Abstract
Background:
While rotator cuff tears are prevalent in the general population, the natural history of this disease is unclear. Understanding rotator cuff tear progression is crucial for refining surgical indications and evaluating the necessity of early interventions. This study presents an in-depth analysis of the existing literature on the definitions and progression rates of rotator cuff tears, aiming to enhance clinical decision making and patient outcomes.
Methods:
A systematic literature search was conducted based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, using Medline (PubMed), Embase (Elsevier), and Web of Science databases on January 12, 2023. Articles were identified as relevant to the natural history and progression of asymptomatic and symptomatic partial-thickness (PT) and full-thickness (FT) rotator cuff tears. Those written in English reporting rotator cuff progression rates of tears in adults, based on magnetic resonance imaging (MRI) or ultrasound, were included. After reviewing the articles, the data on the rates of tear progression and associated risk factors were extracted, compiled, and analyzed. The risk of bias was determined using the Newcastle-Ottawa Scale.
Results:
Twenty-one articles met the inclusion criteria, with 1,831 tears included. The progression rate for all partial thickness tears was 26.7% ± 12.8% at an average follow-up of 2.2 ± 0.9 years, with 5 definitions for tear progression. For FT tears, the progression rate was 54.9% ± 18.6% at a follow-up time of 3.0 ± 2.0 years, with 8 definitions for tear enlargement. A significant difference (p < 0.0001) was found between the progression rates of PT and FT tears. Patients who were initially asymptomatic and became symptomatic had higher progression rates (33%–63%) than those who remained asymptomatic (4%–38%).
Conclusion:
Further research would benefit by identifying a clinically relevant and standardized definition of rotator cuff tear progression, to describe the natural history of rotator cuff disease, making results more comparable and optimizing treatment planning.
Level of Evidence:
Level II. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Rotator cuff (RC) tears are one of the most common tendinous injuries among adults1, affecting 23% of the population2. As individuals age, the likelihood of rotator cuff injuries escalates, rising to around 40% for those over 60 years and surging to 80% for individuals over 80 years3. The impact of RC tears on patient quality of life is profound, leading to diminished shoulder functionality, pain, weakness, and a significant economic burden4. Approximately 250,000 rotator cuff repairs are performed yearly, exceeding $1.5 billion in outpatient expenditures5.
Numerous studies have explored the natural progression of asymptomatic and symptomatic partial-thickness (PT) and full-thickness (FT) RC tears6-26, reporting a rate of progression for PT tears ranging from 0 to 50% with only a difference in follow-up time of one year. Similarly, the rate of progression of FT tears ranges from 4% to 71% at the same follow-up times. Owing to the differences in definitions, there remains a lack of clarity regarding the likelihood of tear progression.
More importantly, this has resulted in a lack of understanding of the association between tear progression and symptom development. This uncertainty extends to the decision between opting for nonsurgical or surgical treatments. Although surgical intervention has a reported failure rate ranging from 10% to 90%, most studies point to a failure rate of around 25%, often due to the tendon retearing27-35. On the other hand, nonsurgical methods for treating full-thickness tears have shown effectiveness in about 75% of cases, alleviating pain and restoring shoulder function by reinforcing the surrounding rotator cuff muscles36,37. The exact reasons for these failures are unknown, leading to ongoing ambiguity in clinical guidelines for managing RC tears5.
Current literature has highlighted the characteristics associated with the progression of this pathology. Yet, the absence of a universally accepted clinical definition for tear progression has resulted in diverse and, at times, contradictory findings. This systematic review seeks to summarize the available clinical data on RC tear progression and identify the risk factors associated with tear enlargement and symptom development.
Materials and Methods
Search Strategy
A systemic search strategy was developed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocols38,39. This yielded peer-reviewed data and articles for a systematic review in 4 phases. In phase 1, ‘‘identification,” electronic databases were searched to find potentially relevant RC tear progression articles. Medline (PubMed), Embase (Elsevier), and Web of Science were accessed and searched on January 12, 2023, with the following search strategies:
• Medline (PubMed) − ((“Rotator Cuff” [Mesh]) OR (“Rotator Cuff Injuries” [Mesh]) OR (“Rotator Cuff”) OR (“Rotator Cuff Injuries”)) AND (“progression” OR “tear progression”)
• Embase (Elsevier) − (“rotator cuff”/exp OR “cuff, rotator” OR “rotator cuff” OR “rotator cuff”) AND “tear progression”
• Web of Science − (TS = (rotator cuff) OR TS = (rotator cuff injury)) AND (TS = (tear progression) OR TS = (progression))
Eligibility Criteria and Article Review
In phase 2, ‘‘screening,” all search returns were extracted and examined for relevance, and duplicate articles were removed. Titles and abstracts were screened for relevance. Studies were included if they met the following inclusion criteria: (1) reported progression rates on (1a) asymptomatic partial-thickness tears, (1b) symptomatic partial-thickness tears, (1c) asymptomatic full-thickness tears, (1d) symptomatic full-thickness tears; (2) defined tear progression; and (3) reported the follow-up time for tear enlargement. Articles were filtered out by the following exclusion criteria: (1) non-English text, (2) only abstracts available, (3) case reports, (4) systematic reviews, (4) meta-analysis studies, (5) literature guidelines, (6) nonhuman studies, (7) biomechanical studies, and (8) imaging modalities other than magnetic resonance imaging (MRI) or ultrasound (US). Case reports, systematic reviews, meta-analyses, and biomechanical studies were excluded because this review is focused on the clinical research definition of tear progression. In phase 3, ‘‘eligibility,” all articles after the screening phase were evaluated for inclusion criteria and relevant data on RC tear progression. All articles were independently reviewed and assessed by 2 evaluators (M.G. and D.C.), and the results were compared to ensure consistency and accuracy. A third reviewer (J.B.V.) resolved any conflicts or issues independently.
Data Extraction and Assessment
In phase 4, ‘‘included” articles that met the inclusion criteria were analyzed for quality, and data were extracted by 2 independent evaluators (M.G. and J.B.V.). The following data points were extracted from the included articles: author, publication year, journal title, patient type (asymptomatic or symptomatic partial thickness or full thickness), tear progression rates, definition, and associated risk factors (univariate and multivariate analysis). Some studies included nonoperative and operative management of RC tears, where data were extracted for only the nonoperatively managed patients. Furthermore, some studies included data for both partial-thickness and full-thickness asymptomatic tears, and in this case, the data were extracted individually and placed into their respective group. The authors sought to perform both qualitative and quantitative analyses.
Quality Assessment
The Newcastle-Ottawa Scale for cohort studies40 was applied independently by 2 review authors (M.G. and J.B.V.) to assess the risk of bias for the included studies (Table I). A maximum of 9 stars were available for the cohort studies and 8 stars for the cross-sectional studies. Disagreements between the 2 review authors (M.G. and J.B.V.) on the risk of bias ratings were resolved through discussion with a third review author (D.C.). Studies awarded ≥7 stars were deemed at low risk of bias, 4 to 6 stars at high risk, and ≤3 stars at very high risk of bias41. A fourth author (M.V.) evaluated studies to assess the reported reviewer bias.
TABLE I.
Study Characteristics From All Included Studies
| First Author (Year) | Patient Type | # of Patients | Mean Age at Inclusion | Imaging Modality | Follow-up Time (yrs) | Progression Definition | % Progressed | Risk of Bias | Reviewer Bias |
|---|---|---|---|---|---|---|---|---|---|
| Fabbri (2016)6 | FT Symptomatic | 18 | 61 (range 55–71) | MRI | 5.1 (range 3.0–7.3) | Increase in DeOrio-Cofield classification | 67 | Low | Yes |
| Frandsen (2022)7 | FT Symptomatic | 43 | 60 ± 10 | MRI | 1 | (1) Increase in AP or ML tear size ≥5 mm | 72 | Low | Yes |
| 58 | 2 | (2) PT to FT tear | 71 | ||||||
| 20 | 5 | 85 | |||||||
| PT Symptomatic | 31 | 1 | (1) 13 (2) 26 | ||||||
| 40 | 2 | (1) 15 (2) 25 | |||||||
| 14 | 5 | (1) 7 (2) 50 | |||||||
| Fucentese (2012)8 | FT Symptomatic | 24 | 52 (range 39–61) | MRI | 3.5 (range 2.3–7.3) | Any increase in tear area | 25 | Low | Yes |
| Herbert-Davies (2017)9 | FT Asymptomatic | 156 | 63.6 ± 8.5 | US | 4.2 ± 5.4 | Increase in AP or ML tear size ≥5 mm | 67 | Low | Yes |
| Jung (2020)10 | FT Symptomatic | 48 | 69 (range 53–81) | MRI | 1.8 ± 1.2 | (1) Increase in AP tear size ≥5 mm | (1) 54 | Low | No |
| (2) Increase in ML tear size ≥5 mm | (2) 41 | ||||||||
| Keener (2015)11,† | FT Asymptomatic | 118 | 63.8 ± 9 | US | 2.3 (IQR 3.7)* | Increase in AP or ML tear size >5 mm PT to FT tear | 61 | Low | No |
| PT Asymptomatic | 56 | 59.4 ± 10 | 3.3 (IQR 3.1)* | 44 | |||||
| Keener (2015)12 | FT Asymptomatic | 139 | 63.3 ± 8.7 | US | 2.8 (IQR 4.6)* | Increase in AP tear size ≥5 mm | 57 | Low | No |
| Kim (2017)13 | FT Symptomatic PT Symptomatic | 88 | 63.6 ± 10 | MRI | 2.1 ± 1.6 | Increase in AP or ML tear size >2 mm | 82 | Low | Yes |
| 34 | 26 | ||||||||
| Ko (2022)14 | PT Symptomatic | 89 | 55.9 ± 9.6 | MRI | 1.9 ± 0.8 | 20% increase in tear involvement | 14 | Low | Yes |
| Ko (2022)15 | FT Symptomatic | 81 | 61.8 ± 88 | MRI | 1.2 ± 0.8 | Increase in AP or ML tear size >5 mm | 48 | Low | Yes |
| Kong (2018)16 | PT Symptomatic | 81 | 62.3 (range 41–77) | MRI | 1.7 ± 09 | ≥20% increase in tear involvement | 16 | Low | Yes |
| Lo (2018)17 | PT Symptomatic | 37 | 52 ± 10 | MRI | 3.8 ± 0.6 | ≥25% increase in tendon thickness | 24 | Low | Yes |
| Mall (2010)18,† | FT Symptomatic | 34 | 63.3 ± 9 | US | 1.93 ± 1.2 | Increase in AP or ML tear size ≥5 mm | 18 | Low | Yes |
| PT Asymptomatic | 0 | 63.1 ± 11 | 2 | PT to FT tear | 0 | ||||
| PT Symptomatic | 20 | 63 ± 9 | 1.93 ± 1.2 | PT to FT tear | 40 | ||||
| Maman (2009)19 | FT Symptomatic | 33 | 58.8 (range 38–84) | MRI | 1.7 (range 0.6–4.8) | Increase in AP or ML tear size >2 mm Increase in AP or ML tear size >5 mm | 51 | Low | Yes |
| PT Symptomatic | 26 | 8 | |||||||
| Moosmayer (2017)20 | FT Symptomatic | 49 | 61 ± 73 | MRI and US | 8.8 (8.2–11) | Any increase in AP tear size | 76 | Low | Yes |
| Moosmayer (2019)21 | FT Symptomatic | 32 | 61 ± 7.6 | MRI and US | 10 | Increase in AP or ML tear size >10 mm | 41 | Low | Yes |
| Moosmayer(2013)22,† | FT Asymptomatic | 32 | 70 ± 7.5 | US | 3 | (1) Increase in AP tear size >5 mm | (1) 32 (2) 35 | Low | Yes |
| FT Symptomatic | 18 | 68 ± 8.7 | (2) Increase in ML tear size ≥5 mm | (1) 61 (2) 33 | |||||
| Oh (2020)23 | PT Symptomatic | 52 | 57 (range 34–70) | MRI and US | 2.8 (range 1–8.6) | PT to FT tear | 31 | Low | No |
| Ranebo (2021)24 | FT Symptomatic | 24 | 62 (range 46–77) | MRI | 1 | Increase in AP or ML tear size >5 mm | 29 | Low | Yes |
| Yamaguchi (2001)25,† | FT Asymptomatic | 19 | 72.4 (range 58–85) | US | 5.5 (range 3–8) | Increase in AP or ML tear size >5 mm | 22 | Low | Yes |
| FT Symptomatic | 14 | 67.3 (range 52–82) | 50 | ||||||
| Yamamoto (2017)26 | FT Symptomatic | 83 | 66.9 (range 47–83) | MRI | 1.5 (range 1–4.5) | Increase in AP or ML tear size >2 mm | 53 | Low | Yes |
| PT Symptomatic | 91 | 41 |
Follow-up times are reported as mean and standard deviations unless otherwise noted. AP = anterior-posterior, FT = full thickness, ML = medial-lateral, MRI = magnetic resonance imaging, PT = partial thickness, and US = ultrasound.
Indicates the median was reported.
Indicates the study longitudinally assessed patients who were initially asymptomatic and became symptomatic, and data were separated into asymptomatic of symptomatic patients.
Statistical Analysis
The Shapiro-Wilk test was used to assess data distribution, showing a normal distribution for PT and FT tear progression rates. A simple linear regression was used to assess the correlation between reported follow-up times and progression rates. An unpaired t-test with Welches correction was used to assess differences between asymptomatic and symptomatic progression rates. All statistical analysis was performed using GraphPad Prism (version 9.3.1 for Windows; GraphPad Software). Two-tailed p-values less than 0.05 were considered significant.
Results
A total of 21 studies met our inclusion criteria. The PRISMA flow diagram (Fig. 1) details our literature search, showing the results of screening with the included and excluded studies and the rationale for exclusion. The studies reviewed included the assessment of PT symptomatic7,13,14,16-19,23,26, PT asymptomatic11,18, FT symptomatic6-8,10,13,15,18,19,21,24,26,42, FT asymptomatic tears9,11,18,22,25, and evolution from asymptomatic to symptomatic tears11,18,22,25. Data were synthesized by creating a master sheet with all extracted variables for each study (Table I). This resulted in a total of 1,831 tears analyzed, which included 727 FT symptomatic, 531 FT asymptomatic, 507 PT symptomatic, and 66 PT asymptomatic RC tears. All assessed risk factors were separately extracted from the studies that included univariate and multivariate analyses and compiled and tabulated to show both statistically significant and nonsignificant risk factors (Figs. 2 and 3).
Fig. 1.
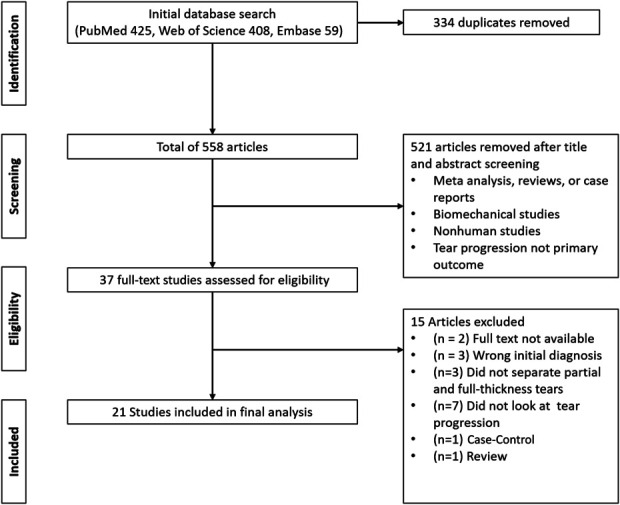
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart exhibiting search strategy to identify articles for inclusion.
Fig. 2.
Reported risk factors for rotator cuff tear progression from univariate analysis across studies including risk factors.
Fig. 3.
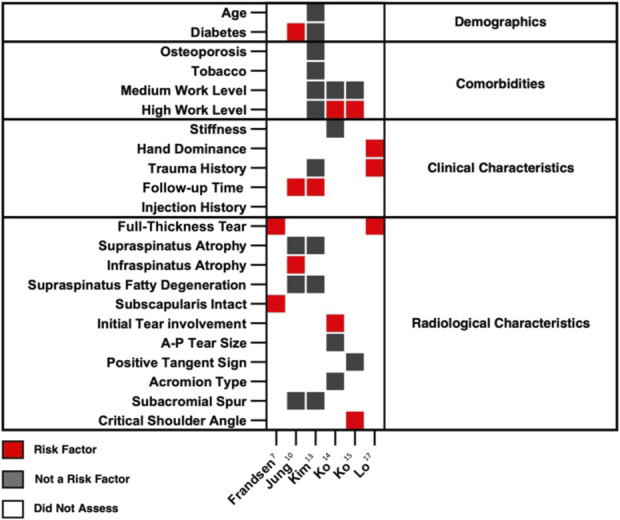
Reported risk factors for rotator cuff tear progression from multivariate analysis across studies including risk factors.
The FT symptomatic tear progression rate was 56.3% ± 19.0% at a follow-up time of 2.8 ± 2.5 years. The FT asymptomatic tear progression rate was 53.1% ± 19.2% at a follow-up time of 3.2 ± 1.0 years. No significant difference (p = 0.72) was observed between progression rates for FT symptomatic and asymptomatic tears (Fig. 4-A). For all PT symptomatic tears, the rate of progression was 25.2% ± 11.5% at a follow-up time of 2.1 ± 0.9 years. For PT asymptomatic tears, the rate of progression was 37.9% ± 20.6% at a follow-up time of 3.1 ± 0.7 years. Similar to FT tears, there was no significant difference (p = 0.56) between the progression of asymptomatic and symptomatic PT tears (Fig. 4-B). Since there was no difference in progression rates between the asymptomatic and symptomatic groups, data were pooled into FT and PT groups regardless of symptomatology. For FT tears, the progression rate was 54.9% ± 18.6% at a follow-up time of 3.0 ± 2.0 years. For PT tears, the progression rate was 26.7% ± 12.8% at a follow-up time of 2.2 ± 0.9 years. FT tears had a significantly higher progression rate compared with PT tears (p < 0.0001) (Fig. 4-C).
Fig. 4.
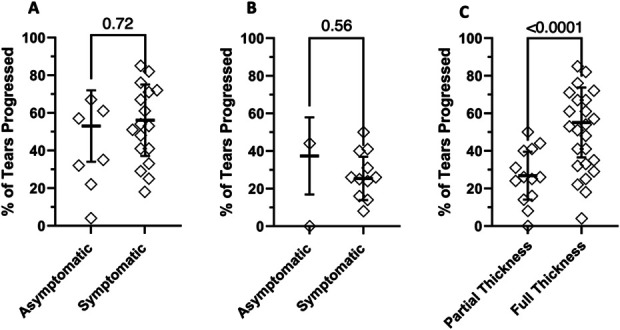
Grouped analysis of (Fig. 4-A) asymptomatic versus symptomatic progression rates for full-thickness tears, (Fig. 4-B) asymptomatic versus symptomatic progression rates for partial-thickness tears, and (Fig. 4-C) partial-thickness (PT) versus full-thickness (FT) progression rates. Error bars represent the reported tear progression rates' weighted mean and standard deviation.
Despite the marked differences in progression between the FT and PT groups, it is important to note the high variability in progression rates and follow-up times, as evidenced by the high standard deviations. A simple linear regression was performed to evaluate the relationship between follow-up time and tear progression and assess whether follow-up time influenced these results. There was no correlation for either FT (R2 = 0.02, p = 0.52) or PT tears (R2 = 0.24, p = 0.09) (Fig. 5). Although time is an established risk factor for tear progression, it does not explain the variability of the results in this data set.
Fig. 5.

Follow-up time versus tear progression rates for (Fig. 5-A) full-thickness tears and (Fig. 5-B) partial-thickness tears. Trendlines are denoted as black lines with 95% confidence bands as dotted lines.
Tear Progression Rates by Definition
Full-thickness Tears
Eight tear progression definitions were used by studies reporting FT tear progression (Fig. 6). The most common definition was the increase in tear size ≥ 5 mm in the anterior-posterior (AP) or medial-lateral (ML) planes. The average progression rate was calculated when there was more than one study for a definition. For ≥2-mm increase in AP or ML tears size, the average progression rate was 64.6% ± 16.8% at a follow-up of 1.8 ± 0.3 years. For ≥5-mm increase in AP or ML tears size, the average progression rate was 54.9% ± 21.7% at a follow-up time of 2.6 ± 1.4 years. For ≥5-mm increase in AP tear size, the average progression rate was 51.2% ± 11.6% at a follow-up time of 2.3 ± 0.6 years. For ≥5-mm increase in ML tear size, the average progression rate was 37.7% ± 4.2% at a follow-up time of 2.4 ± 0.7 years.
Fig. 6.
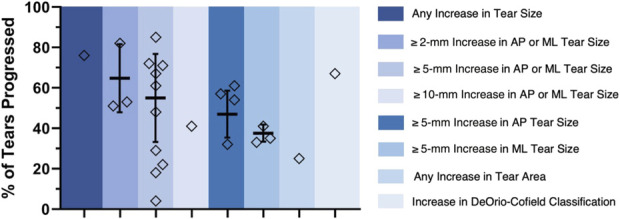
Progression rates for full-thickness tears grouped by tear progression definitions. Weighted means and standard deviation error bars are included for definitions including more than one study.
Partial-thickness Tears
Five definitions were used by studies reporting PT tear progression (Fig. 7). The most common definition was the conversion from PT to FT. The average progression rate was calculated when there was more than one study for a definition. For ≥2-mm increase in AP or ML tears size, the average progression rate was 36.8% ± 9.6% at a follow-up time of 1.7 ± 0.4 years. The average progression rate for conversion from PT to FT was 33.1% ± 11.9% at a follow-up time of 2.6 ± 1 years. For ≥20% increase in tear involvement, the average progression rate was 14.7% ± 1.4% at a follow-up time of 1.8 ± 0.1 years.
Fig. 7.
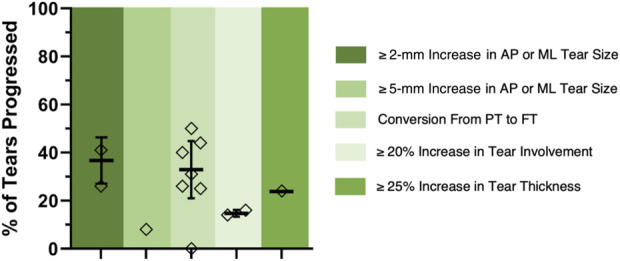
Progression rates for partial-thickness tears grouped by tear progression definitions. Weighted means and standard deviation error bars are included for definitions including more than one study.
Risk Factors for Tear Progression
Although risk factors associated with rotator cuff injury have been extensively studied, there is less clarity on risk factors associated with tear progression. Figure 2 depicts the risk factors analyzed by univariate analysis by the included studies7,10,11,13,14,17,19,23. Even though risk factors such as age, sex, and high body mass index are associated with an increased risk for rotator cuff injury43, they were not unanimously found to be related to tear progression. Regarding clinical characteristics, American Shoulder and Elbow Surgeons score, initial tendinosis, and rotator cable integrity were identified as risk factors for tear progression; however, they were all evaluated by only one study. Other factors, such as tear size, fatty infiltration, tendon retraction, and muscle atrophy, have all been associated with poor healing in rotator cuff repairs44. However, only a few studies assessed these risk factors for tear progression and showed conflicting results (Fig. 2).
Only 6 studies conducted a multivariate analysis of the risk factors associated with tear progression (Fig. 3)7,10,13,15,17. Most of these risk factors were evaluated by one or 2 studies, making it difficult to draw concrete conclusions, along with the already established fact that there are differences in progression definitions across studies. Nonetheless, high work level, hand dominance, follow-up time, FT tear, infraspinatus atrophy, initial tear involvement, intact subscapularis, and a wide critical shoulder angle were all found to be risk factors for tear enlargement.
Discussion
Numerous studies have quantified the progression rates in symptomatic and asymptomatic patients with PT and FT tears. The absence of a clinically relevant definition has resulted in heterogeneous reporting and the need for standardization. Most commonly in literature, it was found that the definition for tear progression was defined as an increase of >5 mm in either the AP or ML plane. We could not determine why 5 mm was determined to be the cutoff value, as there is no evidence as to the clinical relevance of this or any other cutoff point used by the authors. Furthermore, this definition does not distinguish the plane of progression or consider the total tear size (tear area). The marked heterogeneity seen in the reported progression rates demonstrates the need for definition refinement such that it is clinically relevant.
Inconsistency makes it more challenging to establish progression rates and risk factors from multiple studies. While previous studies have attempted to summarize and quantify the progression of RC tears, the studies are limited by a small sample size due to the various definitions of tear progression. Kwong et al. reported on FT tears, finding progression rates of 40.6% in asymptomatic and 34.1% in symptomatic tears44, with an inclusion criterion of progression ≥5 mm in any plane. However, within the examined articles, some reported tear progression as AP or ML tear enlargement11,18, and others only reported AP tear enlargement20. While the results may be similar, the difference in reporting may lead to differences in progression rates, and, as a result, direct comparisons may not provide an accurate representation of the natural history of RC tears. Tsuchiya et al. reported on PT tears and found progression rates of 19.6% in asymptomatic and 5.3% in symptomatic tears45. However, they only included studies that defined the progression of a PT tear as the development of an FT tear. While this definition of progression is clear, only 4 studies used this criterion11,15,17,26. A possible explanation for the higher rate of tear progression in the asymptomatic groups may be that these patients commonly develop new pain, which has been associated with an increase in tear size11,18,22. Our study revealed that there were no significant differences in the progression rates between asymptomatic and symptomatic patients, yielding progression rates of 54.9% ± 18.6% at an average follow-up of 3.0 ± 2.0 years for FT tears and 26.7% ± 12.8% at 2.2 ± 0.9 years for PT tears.
One of the largest uncertainties regarding surgical intervention for RC tears is the association between tear progression and the potential development of symptoms. Two studies have reported no difference in tear size among asymptomatic and symptomatic patients8,16. However, within these studies, all patients were initially symptomatic and those relieved of pain were then denoted as asymptomatic. Thus, this does not fully explain the natural history of tear progression and symptom development as patients were previously symptomatic, limiting the comparison with a true asymptomatic control group. On the contrary, studies that have longitudinally assessed asymptomatic patients found that progressed tears were more likely to have developed symptoms (Fig. 8)11,18,22,25. Keener et al. found that of initially asymptomatic tears that remained asymptomatic, 38% experienced an increase in tear size (45 of 119)11. However, 63% of patients who became symptomatic experienced tear progression (63 of 100)11. Similarly, Mall et al. found that of patients who became symptomatic, 23% of the tears progressed, compared with those who remained asymptomatic, where only 4% progressed18. It is important to note that there was no distinction between PT and FT tears in these 2 studies, as they were grouped. The mean time to symptom development for these studies was 2.6 years and 1.93 years for Keener et al. and Mall et al., respectively. Yamaguchi et al. found that of patients with FT tears who developed symptoms, 50% experienced an increase in tear size, whereas only 22% of the patients who remained asymptomatic experienced tear progression, with a mean symptom development time of 2.8 years25. Similarly, Moosmayer et al. found that of patients with FT tears, 61% of those who developed symptoms experienced tear progression in the AP direction compared with 31% of those who remained asymptomatic at a 3-year follow-up22. Furthermore, they also looked in the ML direction and found that of the tears that became symptomatic, 33% experienced tear progression compared with 35% in the asymptomatic group.
Fig. 8.
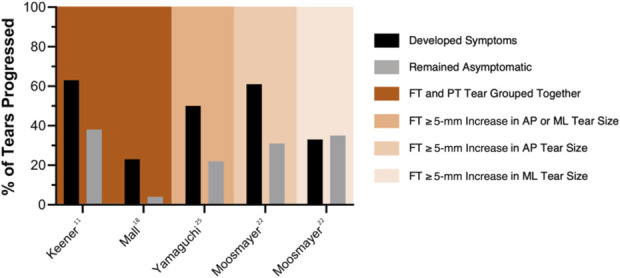
Tear progression rates in longitudinally followed asymptomatic cohorts that either developed symptoms or remained asymptomatic.
Heterogeneous reporting has led to conflicting results when assessing risk factors for RC tear progression, making it difficult to identify patients at an increased risk of tear enlargement. Candela et al. found a steady increase in the quality of reporting results in randomized controlled trials (RCTs) evaluating RC repairs46. However, they identified high levels of variation in scores on reporting quality among RCTs, emphasizing how this issue poses a problem when using studies to create clinical management guidelines. This deficit is also the case for the study of RC tear progression, where variability prohibits accurate comparison of data and robust conclusions to guide clinical management confidently. This results in conflicting data when evaluating the reported risk factors for tear progression, which could be attributed to the lack of a standardized definition of tear progression.
There are conflicting results between studies regarding the characteristics that may or may not be considered a risk factor, leading to a lack of consensus on which characteristics may lead to higher progression rates, making it challenging to identify optimal treatment. More importantly, there is no proof of causality. Many factors have been hypothesized to cause symptoms and portend a higher risk for progression. It has been suggested that cable-intact tears are less likely to progress due to the stress-shielding ability of the rotator cable. However, Keener et al. found no significant difference between the progression rates of cable-intact and cable-disrupted tears12. However, it is important to note that cable-disrupted tears had a higher rate of progression (67%) than cable-intact tears (52%). Given the current scrutiny over the stress-shielding role of the rotator cable47, it is plausible to consider that tears that disrupt the rotator cable may have a higher tendency to worsen simply due to their greater size.
Muscle health has also been linked to RC tear progression, showing muscle degeneration with an increase in tear size and onset of symptoms. Keener et al. found that of the RC tears that did not enlarge, 4% had an increase in muscle degeneration, whereas 30% of progressed tears showed an increase in muscle degeneration11. Moosemayer et al. had similar findings, showing a significant increase in fatty degeneration in the newly symptomatic group (35%) compared with the asymptomatic group (4%)22. On the other hand, Mall et al. reported no significant difference in muscle health between the newly symptomatic and the asymptomatic group18. While associated with poor functional outcomes, muscle atrophy, and fatty degeneration are most likely not risk factors for tear progression, even though they are frequently associated10,11,19. Rather, an RC tear is one of the leading causes of muscle atrophy and fatty infiltration of the RC muscles48,49. As a result, we must consider that these changes may result from the tear progression and may not function as an independent risk factor. Degenerative changes in the muscle are important in assessing surgical outcomes and should be considered part of the natural history of RC tears, especially FT tears. While not yet identified as a risk factor or a result of tear progression, muscle health should be considered when assessing RC tears. Fatty degeneration of the RC muscles has been linked to an increased risk for rerupture after arthroscopic RC repair50.
Although studies that have longitudinally assessed asymptomatic patients who develop symptoms reported an increase in tear size11,18,22,25, data regarding the specific risk for tear progression and symptom development are lacking, limiting clinical decision making for early intervention. In addition, studies exploring the natural history of RC tears are mainly based on data obtained from conservatively treated patients, which limits analysis, as we do not know how patients who had surgical repair would have progressed. Early surgical repair has been reported to achieve better clinical outcomes and mitigate the risk of tear progression42,51. Although surgical intervention is often used to manage RC tears, it is associated with possible rerupture and other postoperative complications52-54. Anatomic characteristics such as tear width, length, and area were all found to be risk factors for rerupture after RC repair50. These characteristics are important to consider in patients who experience tear progression, as they could lead to worse outcomes. Identifying tears at a heightened risk for tear progression could be important for clinical decision making when choosing nonoperative versus operative management and improving the predictability of rerupture and further complications.
Research on shoulder health, focusing on the rotator cuff, has increased due to the aging population and the increasing frequency of repairs. Despite extensive studies in this area, our understanding of the progression of rotator cuff disease remains incomplete, mainly because of the lack of standardized reporting guidelines for rotator cuff tear progression. This gap has resulted in inconsistent data reporting, preventing meaningful study comparisons. To draw more definitive conclusions, we need more comprehensive and precise guidelines and definitions to allow for the comparability of research outcomes.
Limitations
Both prospective and retrospective data were included and analyzed together. Even though prospective data provide better quality results due to higher subject retention and defined follow-up, evidence regarding this topic is limited, and as a result, retrospective data were included. MRI has been proven to correctly predict the size of rotator cuff tears in approximately 75% of cases55; however, the accuracy of this measurement may be limited by the spatial resolution of the MRI protocol. Therefore, cutoff points of tear progression as small as 2 mm may be unreliable. This accuracy may also be affected by the interobserver reliability of MRI measurements when assessing the size of RC tears56. Similarly, US has adequate reliability for both FT and PT, yet interobserver and intraobserver reliability may affect the measured tear size57. Furthermore, this may limit this study as differences in imaging modalities used could cause differences in progression rates due to the accuracy of each method. However, we do see that US-based measurements and MRI measurements at similar follow-up times have comparable progression rates. We should note that few studies used combined imaging modalities (MRI or US), which could further complicate the accuracy of the reported progression rate. Moreover, this highlights the need for standardized reporting methods on the progression of RC tears.
MRI is widely used to measure degenerative changes to muscle58, yet one study included US imaging for the evaluation of degenerative muscle changes, and we included their findings because US is a highly reliable method to assess muscle qualitatively59,60. In addition, although it is known that over time, RC tears are likely to enlarge, our data revealed no clear correlation between progression and time. Most of the studies included in this study reported follow-up times as a means of pooling data in a way that makes it hard to find correlations and specific differences among the cohorts, potentially leading to misleading results of no correlation between time and tear progression. The way of reporting follow-up times in means results in the assumption that all patients in the cohort will progress similarly, which further leads to a heterogeneous way of reporting among studies and inhibits an adequate comparison.
Conclusion
A systematic review and an extensive analysis of the included studies showed that heterogeneous reporting has led to conflicting results on the progression rates and risk factors associated with RC tears. Further insight from more homogenous reporting will improve patient management by understanding which tears are at a greater risk for enlargement. Therefore, we offer the following recommendations to increase comparability and standardize reporting such that a clinically relevant definition of tear progression can be determined. We should note that we recognize that assessing tears down to the mm and considering this tear progression introduces inherent error due to sensitivity and reproducibility when measuring RC tears, but until a clinically relevant definition of tear progression is defined, this will allow standardized methods.
• Tear progression: The AP width should be measured across the anterior and posterior tear margins across the middle of the footprint of the greater tuberosity61. As a result, all increases in AP tear size should be included to determine a clinically relevant progression. Any increased ML progression should be reported as tear retraction in mm. The increase in tear size in the AP and ML planes should be reported separately along with the total tear area. Crescent-shaped tears comprise 54% of RC tears, with U-shaped or L-shaped tears comprising 25% and 21% of RC tears seen clinically, respectively62. Owing to the differences in tear shape, we believe that AP and ML enlargement should be reported separately to determine how different tear types progress.
• Partial tear progression: PT tears should report the conversion from partial thickness to full thickness and the percentage change in depth. Similar to full-thickness tears, the AP and ML sizes of the torn tendon should also be reported.
• Muscle health: Fatty degeneration and muscle atrophy should be included when assessing RC tear progression as muscle quality has been associated with surgical outcomes52 and onset of symptoms11,22. Most commonly used was the Goutallier classification48,63 for fatty infiltration and tangent sign64 for muscle atrophy.
Footnotes
These authors contributed equally to this work.
The Joe Fallon Research Fund and the Dr. Louis Meeks BIDMC Sports Medicine Trainee Research Fund at BIDMC Orthopaedic Surgery Department supported this work.
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A674).
Contributor Information
Mason J. Garcia, Email: mjgarcia@bu.edu.
Daniela Caro, Email: dcaro1095@gmail.com.
Maria Velasquez Hammerle, Email: mvelasq3@bidmc.harvard.edu.
Juan B. Villarreal, Email: bvillarrealesp@gmail.com.
Joseph P. DeAngelis, Email: jpdeange@bidmc.harvard.edu.
Arun J. Ramappa, Email: aramappa@bidmc.harvard.edu.
References
- 1.Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology (Oxford). 2006;45(5):508-21. [DOI] [PubMed] [Google Scholar]
- 2.Reilly P, Macleod I, Macfarlane R, Windley J, Emery RJ. Dead men and radiologists don't lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl. 2006;88(2):116-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J bone Joint Surg. 1995;77(2):296-8. [PubMed] [Google Scholar]
- 4.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699-704. [DOI] [PubMed] [Google Scholar]
- 5.Weber S, Chahal J. Management of rotator cuff injuries. J Am Acad Orthop Surg. 2020;28(5):e193-e201. [DOI] [PubMed] [Google Scholar]
- 6.Fabbri M, Ciompi A, Lanzetti RM, Vadalà A, Lupariello D, Iorio C, Serlorenzi P, Argento G, Ferretti A, De Carli A. Muscle atrophy and fatty infiltration in rotator cuff tears: can surgery stop muscular degenerative changes? J Orthop Sci. 2016;21(5):614-8. [DOI] [PubMed] [Google Scholar]
- 7.Frandsen JJ, Quinlan NJ, Smith KM, Lu CC, Chalmers PN, Tashjian RZ. Symptomatic rotator cuff tear progression: conservatively treated full- and partial-thickness tears continue to progress. Arthrosc Sports Med Rehabil. 2022;4(3):e1091-e1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fucentese SF, von Roll AL, Pfirrmann CW, Gerber C, Jost B. Evolution of nonoperatively treated symptomatic isolated full-thickness supraspinatus tears. J Bone Joint Surg Am. 2012;94(9):801-8. [DOI] [PubMed] [Google Scholar]
- 9.Hebert-Davies J, Teefey SA, Steger-May K, Chamberlain AM, Middleton W, Robinson K, Yamaguchi K, Keener JD. Progression of fatty muscle degeneration in atraumatic rotator cuff tears. J Bone Joint Surg Am. 2017;99(10):832-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jung W, Lee S, Hoon Kim S. The natural course of and risk factors for tear progression in conservatively treated full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2020;29(6):1168-76. [DOI] [PubMed] [Google Scholar]
- 11.Keener JD, Galatz LM, Teefey SA, Middleton WD, Steger-May K, Stobbs-Cucchi G, Patton R, Yamaguchi K. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am. 2015;97(2):89-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keener JD, Hsu JE, Steger-May K, Teefey SA, Chamberlain AM, Yamaguchi K. Patterns of tear progression for asymptomatic degenerative rotator cuff tears. J Shoulder Elbow Surg. 2015;24(12):1845-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim YS, Kim SE, Bae SH, Lee HJ, Jee WH, Park CK. Tear progression of symptomatic full-thickness and partial-thickness rotator cuff tears as measured by repeated MRI. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2073-80. [DOI] [PubMed] [Google Scholar]
- 14.Ko SH, Jeon YD, Kim MS. Progression of symptomatic partial-thickness rotator cuff tears: association with initial tear involvement and work level. Orthop J Sports Med. 2022;10(6):23259671221105471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ko SH, Na SC, Kim MS. Risk factors of tear progression in symptomatic small to medium-sized full-thickness rotator cuff tear: relationship between occupation ratio of supraspinatus and work level. J Shoulder Elbow Surg. 2023;32(3):565-72. [DOI] [PubMed] [Google Scholar]
- 16.Kong BY, Cho M, Lee HR, Choi YE, Kim SH. Structural evolution of nonoperatively treated high-grade partial-thickness tears of the supraspinatus tendon. Am J Sports Med. 2018;46(1):79-86. [DOI] [PubMed] [Google Scholar]
- 17.Lo IK, Denkers MR, More KD, Nelson AA, Thornton GM, Boorman RS. Partial-thickness rotator cuff tears: clinical and imaging outcomes and prognostic factors of successful nonoperative treatment. Open Access J Sports Med. 2018;9:191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mall NA, Kim HM, Keener JD, Steger-May K, Teefey SA, Middleton WD, Stobbs G, Yamaguchi K. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92(16):2623-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maman E, Harris C, White L, Tomlinson G, Shashank M, Boynton E. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91(8):1898-906. [DOI] [PubMed] [Google Scholar]
- 20.Moosmayer S, Gärtner AV, Tariq R. The natural course of nonoperatively treated rotator cuff tears: an 8.8-year follow-up of tear anatomy and clinical outcome in 49 patients. J Shoulder Elbow Surg. 2017;26(4):627-34. [DOI] [PubMed] [Google Scholar]
- 21.Moosmayer S, Lund G, Seljom US, Haldorsen B, Svege IC, Hennig T, Pripp AH, Smith HJ. At a 10-year follow-up, tendon repair is superior to physiotherapy in the treatment of small and medium-sized rotator cuff tears. J Bone Joint Surg Am. 2019;101(12):1050-60. [DOI] [PubMed] [Google Scholar]
- 22.Moosmayer S, Tariq R, Stiris M, Smith HJ. The natural history of asymptomatic rotator cuff tears: a three-year follow-up of fifty cases. J Bone Joint Surg Am. 2013;95(14):1249-55. [DOI] [PubMed] [Google Scholar]
- 23.Oh JH, Lee YH, Lee TH, Jang SI, Kwon J. The natural history of high-grade partial thickness rotator cuff tears: the conversion rate to full thickness tears and affecting factors. Clin Orthop Surg. 2020;12(4):514-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ranebo MC, Björnsson Hallgren HC, Holmgren T, Adolfsson LE. Surgery and physiotherapy were both successful in the treatment of small, acute, traumatic rotator cuff tears: a prospective randomized trial. J Shoulder Elbow Surg. 2020;29(3):459-70. [DOI] [PubMed] [Google Scholar]
- 25.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199-203. [DOI] [PubMed] [Google Scholar]
- 26.Yamamoto N, Mineta M, Kawakami J, Sano H, Itoi E. Risk factors for tear progression in symptomatic rotator cuff tears: a prospective study of 174 shoulders. Am J Sports Med. 2017;45(11):2524-31. [DOI] [PubMed] [Google Scholar]
- 27.Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15(3):290-9. [DOI] [PubMed] [Google Scholar]
- 28.Feng S, Guo S, Nobuhara K, Hashimoto J, Mimori K. Prognostic indicators for outcome following rotator cuff tear repair. J Orthop Surg (Hong Kong). 2003;11(2):110-6. [DOI] [PubMed] [Google Scholar]
- 29.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86(2):219-24. [DOI] [PubMed] [Google Scholar]
- 30.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505-15. [DOI] [PubMed] [Google Scholar]
- 31.Harryman DT, II, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA, III. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73(7):982-9. [PubMed] [Google Scholar]
- 32.Klepps S, Bishop J, Lin J, Cahlon O, Strauss A, Hayes P, Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32(7):1716-22. [DOI] [PubMed] [Google Scholar]
- 33.Mellado JM, Calmet J, Olona M, Esteve C, Camins A, Perez Del Palomar L, Giné J, Saurí A. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005;184(5):1456-63. [DOI] [PubMed] [Google Scholar]
- 34.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;344:275-83. [PubMed] [Google Scholar]
- 35.Zanetti M, Jost B, Hodler J, Gerber C. MR imaging after rotator cuff repair: full-thickness defects and bursitis-like subacromial abnormalities in asymptomatic subjects. Skeletal Radiol. 2000;29(6):314-9. [DOI] [PubMed] [Google Scholar]
- 36.Boorman RS, More KD, Hollinshead RM, Wiley JP, Brett K, Mohtadi NG, Nelson AA, Lo IKY, Bryant D. The rotator cuff quality-of-life index predicts the outcome of nonoperative treatment of patients with a chronic rotator cuff tear. J Bone Joint Surg Am. 2014;96(22):1883-8. [DOI] [PubMed] [Google Scholar]
- 37.Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW, MOON Shoulder Group. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22(10):1371-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vrabel M. Preferred reporting items for systematic reviews and meta-analyses. Oncol Nurs Forum. 2015;42(5):552-4. [DOI] [PubMed] [Google Scholar]
- 40.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P, Ga SW, Zello GA, Petersen JA. The newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014. [Google Scholar]
- 41.Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moosmayer S, Lund G, Seljom US, Haldorsen B, Svege IC, Hennig T, Pripp AH, Smith HJ. Tendon repair compared with physiotherapy in the treatment of rotator cuff tears: a randomized controlled study in 103 cases with a five-year follow-up. J Bone Joint Surg Am. 2014;96(18):1504-14. [DOI] [PubMed] [Google Scholar]
- 43.Song A, Cannon D, Kim P, Ayers GD, Gao C, Giri A, Jain NB. Risk factors for degenerative, symptomatic rotator cuff tears: a case-control study. J Shoulder Elbow Surg. 2022;31(4):806-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kwong CA, Ono Y, Carroll MJ, Fruson LW, More KD, Thornton GM, Lo IKY. Full-thickness rotator cuff tears: what is the rate of tear progression? A systematic review. Arthroscopy. 2019;35(1):228-34. [DOI] [PubMed] [Google Scholar]
- 45.Tsuchiya S, Davison EM, Rashid MS, Bois AJ, LeBlanc J, More KD, Lo IKY. Determining the rate of full-thickness progression in partial-thickness rotator cuff tears: a systematic review. J Shoulder Elbow Surg. 2021;30(2):449-55. [DOI] [PubMed] [Google Scholar]
- 46.Candela V, Longo UG, Di Naro C, Facchinetti G, Marchetti A, Sciotti G, Santamaria G, Piergentili I, De Marinis MG, Nazarian A, Denaro V. A historical analysis of randomized controlled trials in rotator cuff tears. Int J Environ Res Public Health. 2020;17(18):6863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmidt CC, Spicer CS, Papadopoulos DV, Delserro SM, Tomizuka Y, Zink TR, Blake RJ, Smolinski MP, Miller MC, Greenwell JM, Carrazana-Suarez LF, Smolinski PJ. The rotator cable does not stress shield the crescent area during shoulder abduction. J Bone Joint Surg Am. 2022;104(14):1292-300. [DOI] [PubMed] [Google Scholar]
- 48.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78-83. [PubMed] [Google Scholar]
- 49.Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25(1):30-9. [DOI] [PubMed] [Google Scholar]
- 50.Zhao J, Luo M, Pan J, Liang G, Feng W, Zeng L, Yang W, Liu J. Risk factors affecting rotator cuff retear after arthroscopic repair: a meta-analysis and systematic review. J Shoulder Elbow Surg. 2021;30(11):2660-70. [DOI] [PubMed] [Google Scholar]
- 51.Ramme AJ, Robbins CB, Patel KA, Carpenter JE, Bedi A, Gagnier JJ, Miller BS. Surgical versus nonsurgical management of rotator cuff tears: a matched-pair analysis. J Bone Joint Surg Am. 2019;101(19):1775-82. [DOI] [PubMed] [Google Scholar]
- 52.Randelli P, Spennacchio P, Ragone V, Arrigoni P, Casella A, Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2012;96(1):9-16. [DOI] [PubMed] [Google Scholar]
- 53.Scheiderer B, Imhoff FB, Johnson JD, Aglio J, Cote MP, Beitzel K, Imhoff AB, Arciero RA, Mazzocca AD, Morikawa D. Higher critical shoulder angle and acromion index are associated with increased retear risk after isolated supraspinatus tendon repair at short-term follow up. Arthroscopy. 2018;34(10):2748-54. [DOI] [PubMed] [Google Scholar]
- 54.Zakko P, Scheiderer B, Beitzel K, Shoji M, Williams A, DiVenere J, Cote MP, Mazzocca AD, Imhoff FB. Does quality of life influence retear rate following arthroscopic rotator cuff repair? J Shoulder Elbow Surg. 2019;28(6s):S124-S130. [DOI] [PubMed] [Google Scholar]
- 55.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86(4):708-16. [PubMed] [Google Scholar]
- 56.Spencer EE, Jr, Ma CB, Jones G, Safran M, Holloway GB, Kuhn JE, Shoulder Multicenter Orthopaedic Outcomes Network, Dunn WR, Wright RW, Wolf BR, Spindler KP, McCarty E. Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med. 2008;36(1):99-103. [DOI] [PubMed] [Google Scholar]
- 57.Farooqi AS, Lee A, Novikov D, Kelly AM, Li X, Kelly JDt, Parisien RL. Diagnostic accuracy of ultrasonography for rotator cuff tears: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(10):23259671211035106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Somerson JS, Hsu JE, Gorbaty JD, Gee AO. Classifications in brief: goutallier classification of fatty infiltration of the rotator cuff musculature. Clin Orthop Relat Res. 2016;474(5):1328-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Di Matteo A, Moscioni E, Lommano MG, Cipolletta E, Smerilli G, Farah S, Airoldi C, Aydin SZ, Becciolini A, Bonfiglioli K, Carotti M, Carrara G, Cazenave T, Corradini D, Cosatti MA, de Agustin JJ, Destro Castaniti GM, Di Carlo M, Di Donato E, Di Geso L, Elliott A, Fodor D, Francioso F, Gabba A, Hernández-Díaz C, Horvath R, Hurnakova J, Jesus D, Marin J, Martire MV, Mashadi Mirza R, Massarotti M, Musca AA, Nair J, Okano T, Papalopoulos I, Rosa J, Rosemffet M, Rovisco J, Rozza D, Salaffi F, Scioscia C, Scirè CA, Tamas MM, Tanimura S, Ventura-Rios L, Villota-Eraso C, Villota O, Voulgari PV, Vreju FA, Vukatana G, Hereter JZ, Zanetti A, Grassi W, Filippucci E. Reliability assessment of ultrasound muscle echogenicity in patients with rheumatic diseases: results of a multicenter international web-based study. Front Med (Lausanne). 2022;9:1090468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leigheb M, de Sire A, Colangelo M, Zagaria D, Grassi FA, Rena O, Conte P, Neri P, Carriero A, Sacchetti GM, Penna F, Caretti G, Ferraro E. Sarcopenia diagnosis: reliability of the ultrasound assessment of the tibialis anterior muscle as an alternative evaluation tool. Diagnostics (Basel). 2021;11(11):2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ma J, Sahoo S, Imrey PB, Jin Y, Baker AR, Entezari V, Ho JC, Schickendantz MS, Farrow LD, Serna A, Iannotti JP, Ricchetti ET, Polster JM, Winalski CS, Derwin KA. Agreement between intraoperative and magnetic resonance imaging assessments of rotator cuff pathology and 2 magnetic resonance imaging-based assessments of supraspinatus muscle atrophy. JSES Int. 2022;6(6):948-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Watson S, Allen B, Robbins C, Bedi A, Gagnier JJ, Miller B. Does the rotator cuff tear pattern influence clinical outcomes after surgical repair? Orthop J Sports Med. 2018;6(3):2325967118763107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8(6):599-605. [DOI] [PubMed] [Google Scholar]
- 64.Rulewicz GJ, Beaty S, Hawkins RJ, Kissenberth MJ. Supraspinatus atrophy as a predictor of rotator cuff tear size: an MRI study utilizing the tangent sign. J Shoulder Elbow Surg. 2013;22(6):e6-10. [DOI] [PubMed] [Google Scholar]



