Abstract
Background and Objective:
When the uterus is or more than 18 to 20 weeks in size, laparotomy but not minimally invasive surgery (MIS) is commonly performed for hysterectomy. It is, however, acknowledged that MIS carries numerous benefits to patients compared to laparotomy. The uterine size should therefore not be an excluding factor for MIS. This study aims to demonstrate the feasibility and benefits of MIS for hysterectomy for large uterus and explain specific techniques employed.
Methods:
Data from 73 laparoscopic and robotic hysterectomy cases were collected. Cases were divided in two groups based on uterine weight (≥500 g vs <500 g). Estimated blood loss (EBL), operative time, length of hospital stays, and perioperative complications were compared between the groups.
Results:
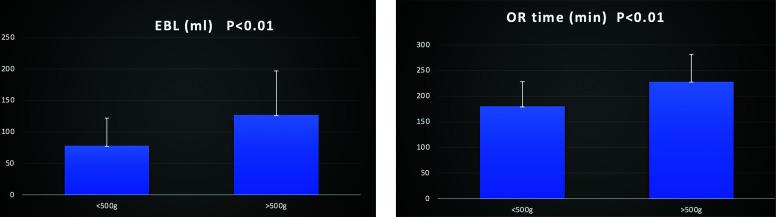
The average specimen weight in two groups was 244 ± 102.75 g vs 903 ± 438.18 g (P < .01). There was no statistically significant difference in length of hospital stay between the two groups. Only 3 patients were hospitalized for more than one day. There were no instances of conversion to laparotomy, intraoperative or postoperative blood transfusion. There was a statistically significant difference in the EBL (78.19 ± 43.8 ml vs 127.88 ± 69.76 ml, P < .01) and operative time (180.68 ± 48.36 vs 228.85 ± 53.04 minutes, P < .01) between the two groups. There were two cases of bladder laceration in the group with uterine weight exceeding 500 g.
Conclusion:
With advanced surgical skills and the adoption of specific techniques, hysterectomy for large uterus can be performed safely and efficiently by MIS.
Keywords: Hysterectomy, Laparoscopy, Large uterus, Minimally invasive surgery, Robot
INTRODUCTION
Since the first laparoscopic hysterectomy was performed by Dr. Harry Reich in 1989,1 the removal of the uterus by a minimally invasive approach has been rapidly adopted world-wide in gynecology. As the performance of conventional laparoscopic hysterectomy remained stable over the past twenty years, the approval of use of the da Vinci Surgical system for gynecological procedures by the FDA in 2005 has accelerated this trend more dramatically. Consequently, the percentage of all hysterectomies for benign indications that were performed abdominally has declined from 59% to 22% between 2005 and 2013.2 It is well recognized that minimally invasive surgery (MIS) carries numerous benefits for patients compared to laparotomy, including less pain, less blood loss, shorter hospitalization, faster recovery and higher patient satisfaction. There is, however, always an argument as to whether we should perform MIS for hysterectomy, especially with consideration of large uterine size. There are currently no universally adopted criteria for selection of laparoscopic or robotic hysterectomy based on uterine size. Many gynecological surgeons will, however, avoid a minimally invasive approach if the uterus is considered “large,” for example, exceeding 15–18 weeks in size or a weight over 500 g due to potential technical difficulties.3
We believe it is more beneficial for patients to undergo MIS for large uterus owing to multiple factors. If an abdominal approach is chosen for this group, it is highly likely a vertical incision will be utilized versus a Pfannenstiel incision. Vertical incisions are associated with increased complications not limited to postoperative pain, higher risk of infection, wound dehiscence, evisceration, and subsequent bowel obstruction. It is more cost-effective if such potential complications and length of hospital stay are minimized. Most patients with large uterus are severely anemic, so choosing of laparotomy often increase the chance of blood transfusion or the delay of surgery.
Several studies have shown the feasibility of minimally invasive hysterectomy for large uterus, however, most of these are limited to small cases reports in which no details of surgical technique were provided.3–11 In this retrospective study, we demonstrate our experience and the outcomes of laparoscopic and robotic hysterectomy for large uterus. Our data indicates that hysterectomy for large uterus through a minimally invasive approach can be completed as successfully as with small uterus if in experienced hands and conducted with proper surgical techniques.
MATERIALS AND METHODS
Institutional Review Board (IRB) approval was obtained and a retrospective chart review was conducted between September, 2022 and September, 2023. Chart review was performed on all laparoscopic and robotic hysterectomy for benign disease performed by one surgeon across the one-year study period.
All cases were divided into two groups based on the threshold uterine weight of 500 g. Patients’ age, body mass index (BMI), race, history of Cesarean section, abdominoplasty, myomectomy, and other surgeries were studied. The primary outcomes of the study are estimated blood loss (EBL) and length of hospital stays. The secondary outcomes are operative time and complications. The χ2 test was used for the comparison of age, BMI, race, rate of Cesarean section, myomectomy, abdominoplasty and other surgeries between the two groups. The student t test was used for EBL, operative time, and rate of lysis of adhesion between two groups.
Preoperative Counseling
All patients were counselled on the possibility of occult uterine sarcoma. The rate of occurrence, diagnosis and prognosis of uterine sarcoma were explained extensively preoperatively.12,13 All patients were informed that power morcellation is not being used in our practice and contained manual morcellation is applied if possible. For cases of extremely large specimens exceeding the size for containment, manual morcellation without containment would be performed if the patient proceeded to opt for minimally invasive hysterectomy.
Intraoperative Techniques
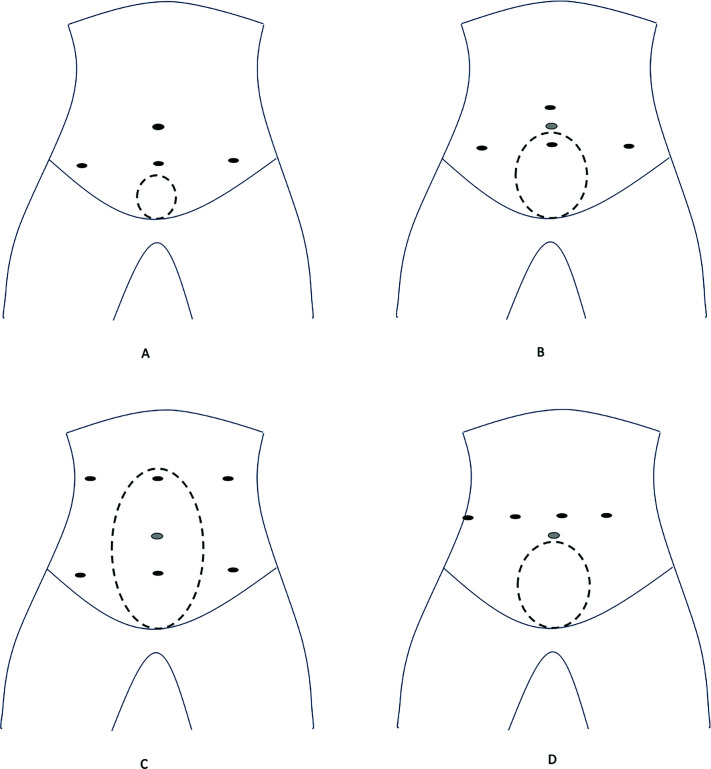
Patients were placed in supine lithotomy position. A urinary Foley catheter and an appropriately sized uterine manipulator, such as V-Care (ConMed USA), were placed. The first trocar was usually placed at Palmer’s point, followed by 4–6 abdominal trocars for laparoscopic hysterectomy and 4–5 trocars for robotic hysterectomy (Figure 1). Trendelenburg position at 20 to 30°F was then adopted. It is important to acknowledge that adequate exposure was achieved through use of a laparoscopic myoma screw, usually placed at the uterine cornua, rather than utilization of the uterine manipulator via the vagina. Hysterectomy usually started at the adnexa permitting the greatest exposure, with ample desiccation and resection of the utero-ovarian ligament and fallopian tube. Salpingectomy was deferred to the end of case.
Figure 1.
Trocar placement. (A) Laparoscopic trocar placement for small uterus. (B) Laparoscopic trocar placement for large uterus. (C) Laparoscopic trocar placement for extremely large uterus. (D) Robotic trocar placement for large uterus.
A key surgical technique is full desiccation prior to cutting. In cases of large specimens especially, the blood vessels supplying the uterus are enlarged and it is extremely difficult to achieve hemostasis once hemorrhage occurs. From our experience, commonly used disposable vessel sealers such as LigaSure (Ethicon, US) are not the most effective tools during hysterectomy for large uterus. We prefer traditional bipolar forceps, such as Richard Wolf bipolar forceps (Richard Wolf Medical Instruments) which can execute thorough and adequate desiccation. Although the risk of energy spread from such instruments may be higher, confidence in knowledge of the patient’s anatomy and leaving adequate space for safe desiccation renders the risk of thermal injury rare.
In cases where the whole uterus is large and the presence of multiple fibroids can distort surrounding structures, it is pivotal to identify both ureters during the entire procedure of the hysterectomy. Ureterolysis was sometimes a necessary precaution to avoid inadvertent injury. Another technique to aid in identification of the ureters bilaterally is to perform preoperative cystourethroscopy with ureteral catheterization to inject Indocyanine Green (Seaford Pharmaceuticals, Canada). The ureters can be clearly visualized by green fluorescence under the XI da Vinci robot or some commercially available laparoscopic cameras.
The function of the uterine manipulator in the vagina is to facilitate dissection, skeletonization, desiccation and transection of the uterine vessels, as well as development of the bladder flap. The ring of the V-Care also serves as a landmark to identify the uterine vessels and bladder. The posterior sheath of the broad ligament is dissected and retracted inferiorly below the level of the ring to protect the ureters.
Another key surgical technique is accurate colpotomy to avoid injury to critical structures. With guidance of the V-Care, anterior and bilateral colpotomy can be performed whilst leaving the posterior portion in situ. In cases of large uterus, there is usually insufficient space to achieve posterior colpotomy with the V-Care safely. We therefore recommend that the V-Care is removed, and the cervix is elevated using a laparoscopic tenaculum. This enables adequate exposure and isolation of the rectum such that posterior colpotomy can be performed safely.
The final step of hysterectomy is retrieval of specimen. If the specimen can be removed through the vagina with the assistance of manual morcellation, a Malleable should be placed along the posterior vaginal wall to retract and protect any bowel present. In cases of larger specimens, a 2–3 cm suprapubic minilaparotomy can be performed to accommodate removal.
RESULTS
Patient Population and Characteristics
The chart of 73 cases of laparoscopic and robotic hysterectomy were reviewed. Uterine weight was recorded on the pathology report. The weight in 47 cases was less than 500 g and in 26 cases more than 500 g. There was no statistically significant difference between the two groups (uterine size <500 g vs >500 g) based on ethnicity, age, BMI or past surgical history (Table 1). Fifty-one patients were of Hispanic ethnicity and 22 patients were African-American. Most patients were obese with an average BMI in the two groups of 31.67 ± 5.71 vs 30.55 ± 5.78. It is also of note that 41 of the 73 (56%) patients had history of at least one Cesarean section and 12 of 73 (16%) patients had a history of abdominoplasty surgery. Forty-five out of 73 (61%) patients underwent other intraabdominal surgeries such as cholecystectomy, appendectomy, gastric by-pass or exploratory laparotomy. As a result, a significant portion of operative time was spent on lysis of adhesions in 23 of 73 (31.5%) cases (Table 2).
Table 1.
Patient Demography and Characters
| <500 g (47) | >500 g (26) | P value | |
|---|---|---|---|
| Age | 46.04 ± 5.54 | 47.61 ± 5.55 | .25 |
| BMI | 31.67 ± 5.71 | 30.55 ± 5.78 | .43 |
| Ethnic Background | |||
| Hispanic | 35 (74.5%) | 16 (61.5%) | .24 |
| African Americans | 12 (25.5%) | 10 (38.5%) | .24 |
| C-section | 30 (63.8%) | 11 (42.3%) | .07 |
| Myomectomy | 1 (2.1%) | 2 (7.7%) | .25 |
| Abdominoplasty | 8 (17.0%) | 4 (15.4%) | .85 |
| Other surgeries | 32 (68.1%) | 13 (50.0%) | .12 |
Table 2.
Intraoperative and Postoperative Results
| <500 g (47) | >500 g (26) | P value | |
|---|---|---|---|
| EBL (ml) | 78.19 ± 43.81 | 127.88 ± 69.76 | <.01 |
| OR time (min) | 180.68 ± 48.36 | 228.85 ± 53.04 | <.01 |
| Lysis of adhesion | 16 (34.0%) | 7 (26.9%) | .53 |
| Intra-OP injury | |||
| Bladder injury | 0 | 2 | |
| Conversion to laparotomy | 0 | 0 | |
| Blood transfusion | 0 | 0 | |
| Hospital stay (day) | 1.02 ± 0.39 | .96 ± .34 | .5 |
| Specimen weight (gram) | 244.34 ± 102.75 | 903.00 ± 438.18 | <.01 |
| Pathology | |||
| Leiomyoma | 17 (36.1%) | 16 (61.6%) | <.05 |
| Adenomyosis | 6 (12.8%) | 0 | |
| Leiomyoma and adenomyosis | 24 (51%) | 10 (38.4%) |
Intraoperative and Postoperative Data
The average specimen weight in two groups was 244 ± 102.75 g vs 903 ± 438.18 g (P < .01). There was a statistically significant difference in the EBL between two groups. Absolute EBL volume in both groups, however, was low (78.19 ± 43.8 ml vs 127.88 ± 69.76 ml, P < .01). There were no instances of intraoperative or postoperative blood transfusion. The length of operative time in both groups was relatively long and there was a statistically significant difference between the two groups (180.68 ± 48.36 minutes vs 228.85 ± 53.04 minutes, P < .01). There were no instances of conversion to laparotomy. There were, however, two cases complicated by a bladder laceration. One case was a patient with history of one prior Cesarean section and a uterine specimen weighing 540 g. The other case was a patient with two prior Cesarean sections and a uterine specimen weighing 570 g. Seventy of 73 patients were discharged home on postoperative day one. One patient stayed a further day for pain management and two patients stayed for more than one day owing to logistical issues surrounding discharge (Table 2, Figure 2). There was no incidence of occult uterine sarcoma. The pathology reported was mainly leiomyoma and adenomyosis, while adenomyosis was more predominant in <500-g group (Table 2).
Figure 2.
The difference of EBL and OR time between two groups.
DISCUSSION
We present here our experience and the outcomes of minimally invasive hysterectomy for large uterus. Our results demonstrate that if a minimally invasive approach can be successfully performed on patients with large uterus, such patients will benefit from the surgery in terms of fast recovery similar to patients with small uterus. This is significant, as patients with a uterus exceeding 500 g will most often be subjected to a vertical incision if an abdominal approach is taken. We believe that minimally invasive hysterectomy on large uterus is feasible, secondary not only to a surgeon’s advanced skills but also to several techniques which can be adopted to conduct the surgery safely.
Choice of Patient
For cases of large uterus, the specimen requires morcellation to enable removal either vaginally or through a minilaparotomy. It is pertinent to counsel patients that contained morcellation may not be feasible if the specimen is extremely large, and that even in cases of contained morcellation it may not be possible to completely prevent cell spillage.14–16 Although the incidence of uterine sarcoma is rare, laparotomy should be performed following shared decision making and in cases where there are risk factors for malignancy such as postmenopausal bleeding, a personal or family history of cancer or suspicious signs on imagining studies.16–18
Laparoscopic versus Robotic Surgery
Laparoscopic surgery can be performed on almost all cases and most hysterectomy on large uterus were actually performed laparoscopically.3–8 There are several reasons for this due to the unique advantages of laparoscopy. (1) For convenience, additional trocars can be placed at different locations during laparoscopic surgery. (2) A laparoscopic camera can be inserted from various directions and a large uterus can be manipulated via different trocars. (3) In addition, the surgical bed can be adjusted during laparoscopic surgery as needed. However, robotic platform provides several advantages that laparoscopy is lack of, such as 3-D surgical field, clear visualization, instrumental stability, fatigue reduction, etc. Sinha et al19 compared the utilization of robot and laparoscopy on hysterectomy for average of 17.4 week size uterus. It is a retrospective study and there was bias in the choosing of robot versus laparoscopy in that robotic hysterectomy was chosen for patients with expected surgical challenges and financially affordability. Overall, however, both modalities were found to be feasible for cases of large uterus with minor differences in trocar number, operative time and EBL. Bahadur et al20 also reported the feasibility of robotic hysterectomy on uterus more than 14 week size with similar results as on uterus less than 14 week size. Considering all the advantages and disadvantages of the robotic platform, we prefer the robotic approach for patients with uterus less than 20 weeks uterus and BMI more than 35–40, providing the robot was available.
Surgical Techniques
The details of surgical techniques were described, which enable us to successfully perform hysterectomy on large uterus. We emphasize ample hemostasis because the bleeding can be massive and is extremely difficult to control if a branch of a vessel is cut without adequate prior desiccation. The exposure is challenging and adequate exposure can only be achieved through uterine manipulation from “top” but not “below.” Without adequate exposure, surgery should be converted to laparotomy for safety. Although the uterine manipulator is not used for manipulation, it is critical for the aid of uterine vessel dissection, bladder flap development and colpotomy. At last, the posterior colpotomy should be performed after removal of the uterine manipulator and elevating of the cervix. As the consequence of these techniques, EBL even in the group >500 g was only 127.88 ml on average and the maximum EBL was 300 ml in one case. There was no case of conversion to laparotomy and 70/73 patients were discharged home on postoperative day one. The operative time was relatively long in both groups, mainly because 31.5% of all cases accompanied with the procedure of extensive lysis of adhesions, secondary to multiple previous surgeries. Compared to the group <500 g, the operative time in the group >500 g was 48 minutes longer on average, with the major contributing factor might be the time for morcellation, although morcellation time was not recorded in our study. Serur et al21 reported their experience of manual contained morcellation on uterine weight exceeding 500 g. The median duration of morcellation was 14.8 minutes (range, 4.5–21.6 minutes) for the abdominal route and 11.7 minutes (range, 5.2–16.8 minutes) for the vaginal route. But the time on morcellation for us were definitely more than Dr. Serur’s experience sine the morcellation were performed by inexperienced residents for most of our cases. There were two cases with bladder laceration in group >500 g. The uteri were not extremely large (540 g and 570 g), but both cases had significant adhesion at the anterior cul-de-sac from previous Cesarean sections. The bladder laceration was more likely a complication of lysis of adhesion, instead of limited exposure secondary to a large uterus. In both cases, the bladder laceration was repaired laparoscopically in two layers. The first layer was sutured with 2-0 vicryl (Ethicon) in a running fashion to close the bladder mucosa, followed by a second layer of interrupted sutures with 0 vicryl (Ethicon) to close the bladder muscle. The bladder was subsequently inflated retrograde to confirm integrity of the seal. An indwelling Foley catheter was left in situ for one week and was removed following imaging with cytogram to reconfirm the bladder integrity. The two patients with bladder laceration had an uncomplicated postoperative course following the repair and healed well. Despite the minor differences and rare complications described, our results of a relatively minimal absolute EBL and fast patient recovery after hysterectomy exemplify the benefits of MIS.
Current and Next Generation of Gynecologic Surgeons
We admit it is difficult for most generalist OBGYN doctors to perform hysterectomy in the same fashion. There is a need, however, for further education in the matter that it is feasible to perform MIS on patients with large uterus, which carries numerous benefits for patients. Such patients should therefore be referred to specialists in MIS, rather than offered laparotomy by default. It also remains pertinent to focus on training the next generation of gynecological surgeons in MIS and the techniques here presented. With advanced surgical skills and adoption of our methods, more surgeons will be able to perform hysterectomy for large uterus safely with minimal injuries for our patients.
Footnotes
Conflicts of interest: The authors report no conflict of interest.
Contributor Information
Pengfei Wang, Department of OB/GYN, BronxCare Health System, Bronx, New York. (Drs. Wang, Uzianbaeva, Hughes, and Mehdizadeh); Department of Obstetrics and Gynecology and Reproductive Science, the Icahn School of Medicine at Mt Sinai, New York, New York. (Drs. Wang and Mehdizadeh).
Liaisan Uzianbaeva, Department of OB/GYN, BronxCare Health System, Bronx, New York. (Drs. Wang, Uzianbaeva, Hughes, and Mehdizadeh).
Noemi Hughes, Department of OB/GYN, BronxCare Health System, Bronx, New York. (Drs. Wang, Uzianbaeva, Hughes, and Mehdizadeh).
Alireza Mehdizadeh, Department of OB/GYN, BronxCare Health System, Bronx, New York. (Drs. Wang, Uzianbaeva, Hughes, and Mehdizadeh); Department of Obstetrics and Gynecology and Reproductive Science, the Icahn School of Medicine at Mt Sinai, New York, New York. (Drs. Wang and Mehdizadeh).
References:
- 1.Reich H, DeCaprio J, McGlynn F. Laparoscopic hysterectomy. J Gynecol Surg. 1989;5(2):213–216. [Google Scholar]
- 2.Pasic RP, Rizzo JA, Fang H, Ross S, Moore M, Gunnarsson C. Comparing robot-assisted with conventional laparoscopic hysterectomy: impact on cost and clinical outcomes. J Minim Invasive Gynecol. 2010;17(6):730–738. [DOI] [PubMed] [Google Scholar]
- 3.Jahan S, Jahan A, Joarder M, Habib SH, Sharmin F, Nayer R. Laparoscopic hysterectomy in large uteri: experience from a tertiary care hospital in Bangladesh. Asian J Endosc Surg. 2015;8(3):323–327. [DOI] [PubMed] [Google Scholar]
- 4.Cesta M, Kennedy B, Pasic R. Total laparoscopic hysterectomy of a 7400 g uterus. J Minim Invasive Gynecol. 2021;28(4):748–749. [DOI] [PubMed] [Google Scholar]
- 5.Dolanbay M, Kutuk MS, Ozgun MT, Uludag S, Sahin Y. Laparoscopically-assisted vaginal hysterectomy for enlarged uterus: operative outcomes and the learning curve. Ginekol Pol. 2016;87(5):333–337. [DOI] [PubMed] [Google Scholar]
- 6.Krentel H, De Wilde RL. Factors for a successful laparoscopic hysterectomy in very large uteri. Case Rep Med. 2017;2017:1637472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macciò A, Chiappe G, Kotsonis P, et al. Feasibility and safety of total laparoscopic hysterectomy for uteri weighing from 1.5 kg to 11.000 kg. Arch Gynecol Obstet. 2021;303(1):169–179. [DOI] [PubMed] [Google Scholar]
- 8.McGurk L, Oliver R, Odejinmi F. Laparoscopic supracervical hysterectomy for the larger uterus (>500 g): a case series and literature review. Arch Gynecol Obstet. 2017;295(2):397–405. [DOI] [PubMed] [Google Scholar]
- 9.Orhan A, Ozerkan K, Kasapoglu I, et al. Laparoscopic hysterectomy trends in challenging cases (1995-2018). J Gynecol Obstet Hum Reprod. 2019;48(10):791–798. [DOI] [PubMed] [Google Scholar]
- 10.Uccella S, Kho RM, Garzon S, Casarin J, Zorzato PC, Ghezzi F. The large uterus classification System: a prospective observational study. BJOG. 2021;128(9):1526–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uccella S, Casarin J, Marconi N, et al. Laparoscopic versus open hysterectomy for benign disease in women with giant uteri (>/=1500 g): feasibility and outcomes. J Minim Invasive Gynecol. 2016;23(6):922–927. [DOI] [PubMed] [Google Scholar]
- 12.Wright JD, T AI, Cui R, et al. Use of electric power morcellation and prevalence of underlying cancer in women who undergo myomectomy. JAMA Oncol. 2015;1(1):69–77. [DOI] [PubMed] [Google Scholar]
- 13.ACOG Committee Opinion No. 770 summary: uterine morcellation for presumed leiomyomas. Obstetr Gynecol. 2019;133(3):604–605. [DOI] [PubMed] [Google Scholar]
- 14.Uterine Morcellation for Presumed Leiomyomas: ACOG Committee Opinion, Number 822: correction. Obstetr Gynecol. 2021;138(2):313–313. [DOI] [PubMed] [Google Scholar]
- 15.Committee Opinion No. 701 summary: choosing the route of hysterectomy for benign disease. Obstetr Gynecol. 2017;129(6):1149–1150. [DOI] [PubMed] [Google Scholar]
- 16.Zullo F, Venturella R, Raffone A, Saccone G. In-bag manual versus uncontained power morcellation for laparoscopic myomectomy. Cochrane Database Syst Rev. 2020;5(5):CD013352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ip PP, Cheung AN. Pathology of uterine leiomyosarcomas and smooth muscle tumours of uncertain malignant potential. Best Pract Res Clin Obstet Gynaecol. 2011;25(6):691–704. [DOI] [PubMed] [Google Scholar]
- 18.Zhao WC, Bi FF, Li D, Yang Q. Incidence and clinical characteristics of unexpected uterine sarcoma after hysterectomy and myomectomy for uterine fibroids: a retrospective study of 10,248 cases. Onco Targets Ther. 2015;8:2943–2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinha R, Bana R, Sanjay M. Comparison of robotic and laparoscopic hysterectomy for the large uterus. JSLS. 2019;23(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bahadur A, Kumawat M, Chawla L, Kapur D, Bahurupi Y, Mundhra R. Robotic-assisted hysterectomy for benign indications of uteri less than fourteen weeks size versus more than fourteen weeks size: a comparative study. Cureus. 2021;13(5):e15263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Serur E, Zambrano N, Brown K, Clemetson E, Lakhi N. Extracorporeal manual morcellation of very large uteri within an enclosed endoscopic bag: our 5-year experience. J Minim Invasive Gynecol. 2016;23(6):903–908. [DOI] [PubMed] [Google Scholar]