Abstract
Background
Post-traumatic stress disorder (PTSD) has been shown to predict psychotic symptomology. However, few studies have examined the relative contribution of PTSD compared to broader post-traumatic sequelae in maintaining psychosis. Complex PTSD (cPTSD), operationalized using ICD-11 criteria, includes core PTSD (intrusions, avoidance, hyperarousal) as well as additional “disturbances of self-organisation” (DSO; emotional dysregulation, interpersonal difficulties, negative self-concept) symptoms, more likely to be associated with complex trauma histories. It was hypothesized that DSOs would be associated with positive psychotic symptoms (paranoia, voices, and visions) in daily life, over and above core PTSD symptoms.
Methods
This study (N = 153) employed a baseline subsample of the Study of Trauma And Recovery (STAR), a clinical sample of participants with comorbid post-traumatic stress and psychosis symptoms. Core PTSD, DSO and psychosis symptoms were assessed up to 10 times per day at quasi-random intervals over six consecutive days using Experience Sampling Methodology.
Results
DSOs within the preceding 90 min predicted paranoia, voices, and visions at subsequent moments. These relationships persisted when controlling for core PTSD symptoms within this timeframe, which were themselves significant. The associations between DSOs and paranoia but not voices or visions, were significantly stronger than those between psychosis and core PTSD symptoms.
Conclusions
Consistent with an affective pathway to psychosis, the findings suggest that DSOs may be more important than core PTSD symptoms in maintaining psychotic experiences in daily life among people with comorbid psychosis and cPTSD, and indicate the potential importance of addressing broad post-traumatic sequelae in trauma-focused psychosis interventions.
Keywords: disturbances of self-organization, ecological momentary assessment, experience sampling methodology, paranoia, trauma, visions, voices
Introduction
Traumatic life experiences increase psychosis risk (Bell, Foulds, Horwood, Mulder, & Boden, 2019; Varese et al., 2012), and symptoms of post-traumatic stress mediate this relationship (Alameda et al., 2020; Sideli et al., 2020; Williams, Bucci, Berry, & Varese, 2018). In addition to the high rates of childhood trauma, people with psychosis also have a high risk of re-victimization that compounds the risk of symptoms of post-traumatic stress (De Vries et al., 2019). Comorbid post-traumatic stress disorder (PTSD) is therefore unsurprisingly common among people with psychosis, worsening mental health outcomes (DeTore, Gottlieb, & Mueser, 2021). However, it is unclear which post-traumatic sequelae account for the association between trauma and psychosis. The diagnostic conceptualization of PTSD has been subject to much debate, particularly regarding the extent to which it should focus on ‘core’ symptoms (i.e. intrusions, avoidance, hyperarousal) or those commonly associated with the complex trauma histories typically experienced by people with psychosis, conceptualized as disturbances of self-organization (DSOs; emotional dysregulation, interpersonal difficulties, negative self-concept) (Karatzias et al., 2017; Trauelsen et al., 2015). The newly classified diagnosis of complex PTSD (cPTSD) includes the core symptoms of PTSD as well as DSOs (Maercker et al., 2013).
Whilst the conceptualization of cPTSD in the latest International Classification of Disease (ICD-11; World Health Organisation, 2019) is relatively recent, existing findings on related concepts shed light on the role of DSOs in psychosis. Avoidant attachment, emotion dysregulation and negative self-beliefs have all been shown to predict positive symptoms, demonstrating a potential association between cPTSD and psychosis (Bloomfield et al., 2021; Hardy et al., 2016; Hardy, O'Driscoll, Steel, Van Der Gaag, & Van Den Berg, 2021; Sitko, Bentall, Shevlin, O'Sullivan, & Sellwood, 2014). Epidemiological studies indicate that a sizeable proportion of trauma survivors experience comorbid psychosis and cPTSD symptoms (Frost, Louison Vang, Karatzias, Hyland, & Shevlin, 2019). Preliminary studies suggest cPTSD may be more common than PTSD among people with psychosis, and potentially contribute to maintaining positive and affective symptoms (Panayi et al., 2022). Considering the impact of cPTSD may therefore prove essential to a comprehensive understanding of post-traumatic sequelae in people with psychosis.
One limitation of existing research on core PTSD and DSO difficulties in people with psychosis is the dominant use of cross-sectional designs (Bloomfield et al., 2021), since retrospective designs cannot establish temporal relationships and are subject to recall bias (Blum et al., 2015; Decker, Rosen, Cooney, Schnurr, & Black, 2021). In turn, existing longitudinal studies are typically aimed at detecting developmental change utilizing widely spread assessment points (Ram & Gerstorf, 2009), which may fail to capture the potential confounding effects of contextual factors (McNeish, Stapleton, & Silverman, 2017) and/or dynamic fluctuations in observed variables (Wang, Hamaker, & Bergeman, 2012). An examination of temporal dynamics using intensive longitudinal methods can address these limitations and shed light on the potential interrelatedness of cPTSD and psychosis in daily life.
Experience sampling methodology (ESM), a structured diary technique wherein participants are prompted multiple times per day to complete ambulatory assessments, can assess these temporal dynamics (Trull & Ebner-Priemer, 2009). ESM has increasingly been applied to study the flow and impact of post-traumatic symptoms in the daily lives of people with PTSD (Chun, 2016; Vachon, Viechtbauer, Rintala, & Myin-Germeys, 2019), as well as psychosis (Bell et al., 2024). Brand et al. (2020) investigated the daily impact of PTSD in people with psychosis, and did not find a temporal relationship between core PTSD symptoms and auditory hallucinations. The current study extends prior research by including wider post-traumatic sequelae – namely, DSOs – as well as a wider array of positive psychotic symptoms (i.e. paranoia, voices, and visions) to clarify previous cross-sectional relationships between DSOs and psychosis (Panayi et al., 2022) and aid the identification of further treatment targets of trauma-focused psychological interventions.
To the best of our knowledge, this study is the first to examine the dynamic effects of cPTSD on psychosis symptoms in people meeting ICD-10 criteria for schizophrenia-spectrum disorders and DSM-5 diagnostic criteria for PTSD. We aimed to examine the temporal association between DSOs and positive psychosis symptoms, accounting for concurrent PTSD symptoms. Based on cross-sectional findings that DSO-like difficulties mediate the relationship between childhood trauma and psychosis (Bloomfield et al., 2021; Sideli et al., 2020; Williams et al., 2018), it was hypothesized that daily increases in DSOs would predict subsequent exacerbations in psychotic experiences, and that this relationship would persist when controlling for core PTSD symptoms.
Method
Study design
This study used an ESM design (Myin-Germeys et al., 2018) involving the repeated assessment of positive psychosis symptoms (auditory and visual hallucinations; paranoia), PTSD (intrusions, avoidance, hyperarousal) and DSOs (emotional dysregulation, interpersonal difficulties, negative self-concept), using a mobile app that prompted participants to rate their experiences up to 10 times per day over 6 consecutive days.
Participants
Participants (N = 153) were a subsample of the Study of Trauma and Recovery (STAR trial) (Peters et al., 2022) who consented to additional ESM procedures prior to randomisation. Participants met ICD-10 criteria for schizophrenia-spectrum diagnoses (F20–29) ascertained from the ICD-10 checklist by the research team, following clinical notes review and consultation with the care team, as appropriate, and scored ≥2 (‘moderate’ intensity) on the distress item of at least one psychotic symptom rating scale (see section 2.3.1) to ensure presence of at least one distressing positive symptom. Notably, 31% of the sample were recruited from Early Intervention for Psychosis (EIP) services, where United Kingdom (UK) good practice guidelines stipulate against assigning potentially stigmatizing diagnoses such as schizophrenia to those experiencing a first episode of psychosis, and instead routinely apply ICD-10 F28 (other non-organic psychotic disorder) or F29 (unspecified psychotic disorder) categories. The majority (114[75%]) had at least one other diagnosis, in addition to meeting criteria for psychosis and PTSD, with the most common being depression (58[38%]).
Participants also endorsed at least one traumatic life event on the Trauma and Life Events checklist (Carr, Hardy, & Fornells-Ambrojo, 2018), and met PTSD criteria on the Clinician-Administered PTSD Scale for DSM-5 (Weathers et al., 2018). Participants were excluded if they were <18, their psychotic or PTSD symptoms were primarily organic in etiology, had a primary substance misuse diagnosis, required an interpreter to engage with the trial, or (within the previous 3 months) had major medication changes or received trauma-focussed therapies.
Descriptive demographic and clinical variables are presented in Table 1, split by ESM participants and non-participants. ESM participants had significantly higher rates of ICD-10 F28 diagnoses, and non-participants significantly higher rates of ICD-10 F20 diagnoses. However, the groups did not differ significantly in severity of core PTSD, DSOs, paranoia, voices, or visions (test statistics presented in online Supplementary Table S1).
Table 1.
Demographic and clinical variables for participants who accepted (n = 153) and declined (n = 152) ESM
| Variable | ESM % | No ESM % | |
|---|---|---|---|
| Gender | Male | 39.22 | 44.08 |
| Female | 56.86 | 55.26 | |
| Non-binary | 2.61 | − | |
| Prefer not to say | 1.31 | 0.66 | |
| Ethnicity | White British | 73.86 | 73.03 |
| Black (African or Caribbean) | 9.80 | 7.89 | |
| Mixed heritage | 4.58 | 5.92 | |
| South Asian (Indian or Pakistani) | 2.61 | 1.97 | |
| Other | 9.15 | 10.53 | |
| Relationship status | Single | 58.17 | 65.13 |
| Cohabiting/Married/Civil partnership | 30.07 | 21.71 | |
| Separated/Divorced/Widowed | 11.11 | 12.50 | |
| Prefer not to say | 0.65 | 0.66 | |
| Education | Primary education | 2.61 | 2.63 |
| Secondary education | 30.72 | 43.42 | |
| Vocational education/college | 39.22 | 26.61 | |
| Higher education | 22.88 | 19.08 | |
| Other | 2.61 | 0.66 | |
| Prefer not to say | 1.96 | 3.95 | |
| Employment status | Working | 17.65 | 7.24 |
| Studying | 4.58 | 5.92 | |
| Volunteering | 4.58 | 3.95 | |
| Caregiver | − | 1.32 | |
| Retired | 1.96 | − | |
| Not currently working | 69.93 | 82.24 | |
| Prefer not to say | 1.31 | 1.32 | |
| Schizophrenia spectrum diagnosis (F20-29; ICD-10) | Schizophrenia (F20) | 15.03 | 23.68 |
| Persistent delusional disorder (F22) | 1.31 | 1.32 | |
| Schizoaffective disorder (F25) | 9.80 | 15.79 | |
| Other nonorganic psychotic disorder (F28) | 30.72 | 17.76 | |
| Unspecified nonorganic psychosis (F29) | 43.14 | 41.45 | |
| Hears voicesa | 81.70 | 78.29 | |
| Sees visionsa | 63.40 | 53.95 | |
| Antipsychotic prescription | 81.05 | 75.66 | |
| ITQ Diagnosis | None | 8.55 | 14.09 |
| PTSD | 8.55 | 8.72 | |
| cPTSD | 82.89 | 77.18 | |
| Other diagnoses | Anxiety disorders (Generalized anxiety, OCD, Other anxiety disorders) | 15.69 | 19.08 |
| Autism | 7.84 | 1.97 | |
| Bipolar | 6.54 | 9.87 | |
| Depression (with or without psychotic features) | 37.91 | 26.97 | |
| Personality disorders (including emotionally unstable and other personality disorders) | 30.07 | 22.37 | |
| Substance-related disorders | 6.54 | 9.21 | |
| Other (e.g. ADHD, eating disorders, severe stress, and adjustment disorder) | 9.80 | 12.50 | |
| Multiple trauma exposure | Repeated events (at least 1 TALE item endorsed ‘more than once’) | 100 | 100 |
| Multiple trauma types | 100 | 100 | |
| Trauma timing | Child (endorsed any TALE item < 16) | 92.81 | 95.39 |
| Adult (endorsed any TALE item 16 or over) | 95.42 | 94.74 | |
| Both (endorsed any TALE item < 16 AND 16 or over) | 88.24 | 86.84 | |
| M(s.d.) | M(s.d.) | ||
| Age | 37.00(12.14) | 40.73(12.50) | |
| Number of trauma typesb | 11.52(3.20) | 11.16(3.12) | |
| ITQ-PTSD | 17.93(4.16) | 17.34(4.51) | |
| ITQ-DSO | 18.63(4.52) | 18.13(4.80) | |
| GPTS-Persecution | 23.25(11.38) | 23.39(12.19) | |
| PSYRATS-Visions | 30.82(5.93) | 30.24(6.26) | |
| PSYRATS-Voices | 30.81(5.88) | 31.98(4.54) | |
ESM, Experience Sampling Methodology; M, Mean; s.d., Standard Deviation; PTSD, Post-traumatic Stress Disorder; DSO, Disturbances of Self-Organisation; ICD-10, International Classification of Disease 10th Ed.; ITQ, International Trauma Questionnaire (Cloitre et al., 2018); OCD, Obsessive Compulsive Disorder; ADHD, Attention Deficit and Hyperactivity Disorder; GPTS, Green et al., Paranoid Thoughts Scale (Freeman et al., 2021); PSYRATS, Psychotic Symptom Rating Scales (Haddock et al., 1999); TALE, Trauma and Life Events checklist (Carr et al., 2018).
Based on baseline PSYRATS data.
Based on baseline TALE data.
Measures
Baseline measures
Participants completed the following instruments as part of a larger STAR trial baseline assessment battery (Peters et al., 2022):
Trauma and Life Events Checklist (TALE; (Carr et al., 2018)): 22-item self-report checklist assessing difficult life experiences. Each event is rated according to its occurrence, whether this occurred repeatedly, and its timing (i.e. whether participants were under age 16, 16 or over, or both in instances of repeated events). The number of traumas endorsed may be summed to indicate the number of different types of traumatic experiences. The TALE demonstrates good test-retest reliability and convergent validity with related trauma measures (33).
International Trauma Questionnaire (ITQ; (Cloitre et al., 2018)): 18-item self-report scale assessing presence and severity of PTSD and DSO symptoms within the past month. Both subscales comprise 3 symptom clusters, themselves composed of 2 items each, and 3 items capturing the functional impact of symptoms. Items are scored on a 5-point Likert scale from 0–4 (‘Not at all’–‘Extremely’). The ITQ diagnostic algorithm identifies a probable diagnosis of PTSD when a participant scores ≥2 on at least one item in each PTSD cluster, plus ≥2 on at least one functional impairment item associated with these symptoms. The cPTSD threshold includes that of PTSD plus a score of ≥2 on at least one item in each DSO cluster and of ≥2 on at least one functional impairment item associated with these symptoms. PTSD and DSO items were totaled to derive continuous severity scores from 0–24 on each subscale, with higher scores indicating higher severity. These were used to examine correlations between ESM and baseline measures of PTSD and DSOs. Both subscales demonstrate high internal consistency (both α's ≥0.79; (Cloitre et al., 2018)).
Revised-Green et al., Paranoid Thoughts Scale (R-GPTS; (Freeman et al., 2021)): 18-item self-report scale assessing paranoid ideation in the past month. Composed of two subscales, ideas of reference (8 items) and persecution (10 items), items are scored on a 5-point Likert scale from 0–4 (‘Not at all’–‘Totally’). Higher scores on both the reference (range 0–32) and persecution (range 0–40) subscale suggest higher intensity. Items on the GPTS-persecution subscale were totaled to examine correlations between ESM and baseline paranoia measures. Both subscales demonstrate high internal consistency (all α's >0.9; (Freeman et al., 2021)).
Psychotic Symptom Rating Scales (PSYRATS; (Haddock, McCarron, Tarrier, & Faragher, 1999)): structured clinical interview measuring positive symptoms of psychosis over the past month across two subscales. One measures frequency, intensity, impact and phenomenology of auditory hallucinations (11 items) and the other measures preoccupation, conviction, and impact of distressing beliefs (6 items). Items are scored on a 5-point Likert scale from 0–4, with anchors varying to suit each item; higher scores on both the voices (range 0–44) and beliefs (range 0–24) subscale suggest higher intensity. The PSYRATS displays good inter-rater and test-retest reliability (Drake, Haddock, Tarrier, Bentall, & Lewis, 2007). Average scores on the frequency and duration items of the auditory hallucinations PSYRATS were used to examine associations with the ESM voices item. The STAR trial added an adapted PSYRATs version capturing the presence of hallucinations in other modalities. Items, anchors, and scoring are identical to the voices subscale, but adapted to refer to non-auditory hallucinations (Tsang, 2023). Average scores on frequency and duration of visual hallucinations were used to examine associations with the ESM visions item
ESM measures
The ESM assessment comprised 29 items assessing affective states, contextual information, psychosis, and cPTSD symptoms. Items were scored on a 7-point Likert scale from 1–7 (‘Not at all’–‘Very much so’). Items were based on previous ESM studies of similar populations (Chun, 2016; Kimhy et al., 2006), amended in collaboration with consultants with lived experience of trauma and psychosis.
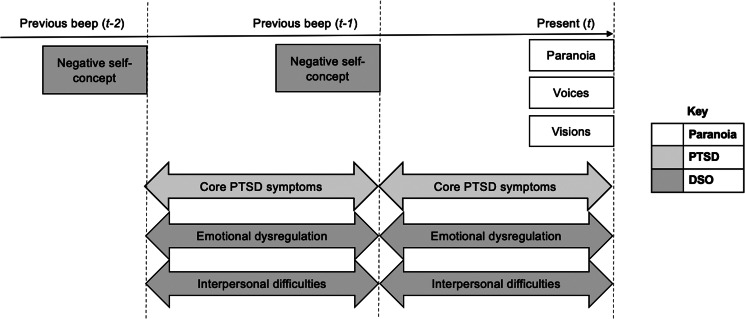
As illustrated in Fig. 1, some items (psychosis symptoms; negative self-concept [DSO]) were phrased to capture the current moment (Right now…, i.e. ‘momentary’ items), whereas others (core PTSD symptoms; emotional dysregulation [DSO]; interpersonal difficulties [DSO]) referred to the timeframe between moments (Since the last beep…, i.e. ‘interval’ items). We considered proximal models based on data from a single timepoint (time t) to nevertheless be longitudinal when interval items were included, since these analyses tested whether symptoms experienced since the previous moment (interval item scores) predicted symptoms at the current moment (momentary item scores). To further corroborate the temporal ordering of effects, we also assessed distal models using lagged predictor variables to test whether interval items at timepoint t − 1, and momentary items at t − 2, predicted momentary items at time t.
Figure 1.
Temporal ordering of ESM items, adapted from (Palmier-Claus, Haddock, & Varese, 2019). Boxes indicate momentary items; arrows indicate interval items.
Current psychotic symptoms: Two items (‘Right now I feel suspicious’; ‘Right now I believe that some people want to hurt me deliberately’) were used to compute momentary paranoia scores. The mean of the two items was used, unless one was missing, in which case the remaining single item was used. Single items measuring voices (‘Right now I hear a voice or voices that other people cannot hear’) and visions (‘Right now I see things that other people cannot see’) were used to assess momentary hallucinatory experiences.
Core PTSD and DSO symptoms: An interval PTSD score was derived from the mean of five items across the three core PTSD symptom domains (intrusions; avoidance; hyperarousal). These items were anchored to the same traumatic experience(s) as the baseline STAR assessment (i.e. that which participants identified as affecting them the most recently). One item captured intrusive memories (‘Unwanted memories about the experience popped into my mind’), two measured avoidance (‘I avoided thoughts, feelings and physical sensations that remind me of the experience’; ‘I avoided people, places or situations that reminded me of the experience’) and two measured hyperarousal (‘I felt super alert, watchful or on guard’; ‘I felt jumpy or easily startled’). All five items were interval items (‘Since the last beep…’, capturing phenomena of interest that might have occurred in the time interval between the previous and current ESM time point) due to the possible insufficient occurrence of specific PTSD symptoms to enable sampling using momentary items (‘Right now..’).
Six items across the three DSO domains (emotional dysregulation; interpersonal difficulties; negative self-concept) were used to derive an interval DSO score. Two items measured emotional dysregulation (‘I found it hard to control my emotions’; ‘I felt spaced out, numb or emotionally shut down’) and another two measured interpersonal difficulties (‘I felt distant or cut off from people’; ‘I found it easy to stay emotionally close to people’ [reverse-scored]). These items were phrased as interval items (‘Since the last beep…’), as the reflective nature of these constructs makes momentary evaluation difficult. The negative self-concept items, however, were momentary (‘Right now, I feel ashamed’; ‘Right now, I believe I am a good person’ [reverse-scored]). An average of all six items would therefore have included momentary and interval items, which may not confer a valid estimate. To account for this, DSO scores were calculated using the mean of negative self-concept item scores from the preceding moment (t − 1; the so-called ‘lagged’ score) and of the emotional dysregulation and interpersonal difficulty item scores at time t (i.e. assessing the interval between the preceding and current moment), to capture DSO severity up to the current assessment point.
ESM item validation: Multilevel confirmatory factor analysis (mCFA) was conducted to verify the factor structure of multi-item ESM constructs whilst accounting for the hierarchical structure of the data (Forkmann et al., 2018). A three-factor solution representing paranoia, PTSD and DSOs demonstrated acceptable fit (CFI = 0.91; RMSEA = 0.05) (Forkmann et al., 2018) that was better (AIC = 203 555.14; BIC = 204 012.59) than a single-factor solution (AIC = 213 402.71; BIC = 213 825.15) at within- and between-participant levels.
Multilevel regressions were used to test whether cross-sectional scores on validated questionnaires at baseline predicted ESM measures of matching constructs. These confirmed that GPTS-persecution scores predicted daily paranoia scores (b = 0.043, p < 0.001, 95% CI 0.028–0.058)<TS: Please check for ‘95% CI’ here and elsewhere>. Additionally, frequency and duration items on the PSYRATS-voices and ‘other modalities’ subscales predicted daily voice and vision frequency among voice hearers and those who experienced visions, respectively (b = 1.174, p < 0.001, 95% CI 0.931–1.417; b = 1.005, p < 0.001, 95% CI 0.566–1.444). Similarly, ITQ-PTSD subscale scores predicted daily PTSD scores (b = 0.035, p = 0.004, 95% CI 0.011–0.059), and ITQ-DSO subscale scores predicted daily DSO scores (b = 0.025, p = 0.012, 95% CI 0.005–0.044).
Owing to the multilevel nature of ESM data, the restrictions placed by Cronbach's alpha on measures of internal consistency are too strict, and Macdonald's omega (ω) is preferred as a more robust estimate (Eisele, Kasanova, & Houben, 2022), yet the dual-item nature of paranoia in our ESM questionnaire prevented a valid calculation of ω. Cronbach's alpha was therefore used to conservatively estimate reliability in this sample, which was acceptable (α = 0.79). The internal reliability of ESM core PTSD and DSO measures was good (ω = 0.83 for both scales). Internal consistency estimates were not suited to the measurement of voices or visions, as they were measured by single items.
Procedure
Participants were recruited from five National Health Service (NHS) Mental Health Trusts across the UK (NHS research ethics committee IRAS ID: 275697). After providing informed consent, participants referred to the trial completed an eligibility assessment administered by a trained research assistant (RA). Those eligible for the trial completed the standardized questionnaire and clinical interview measures used in this study (ITQ, PSYRATS, GPTS-R). The full STAR trial assessment battery and procedures are listed elsewhere (Peters et al., 2022). Following baseline assessment, those who consented to hear about additional studies within the trial were invited to take part in the ESM study, which took place prior to randomization to the trial arms.
The ESM study used a mobile app, m-Path (Mestdagh et al., 2023), to deliver ESM questionnaires up to 10 times a day for six days. Smartphones with preloaded SIM cards were provided for participants without access to either a smartphone or sufficient internet connection. To reduce burden, schedules were adapted to suit the waking hours of participants. Participants with an atypical schedule (e.g. an upcoming holiday or invasive medical procedure) were not onboarded to the study until after the event(s) had passed, to ensure study responses reflected a typical week for participants.
After providing informed consent, participants were supported by a RA to download m-Path onto their personal mobile phone or were provided with a phone for the duration of the study. Participants completed a practice ESM assessment with the RA to clarify understanding of the items and resolve any queries. Next, the RA scheduled up to 10 notifications – as many as the participants' waking hours would allow using 90-min increments – per day. Compliance with the study was monitored throughout, and a monitoring phone call made two days following the practice to ensure the app ran smoothly and items made sense. Participants who missed all notifications in a day were contacted to check for any issues with the app. Following completion of all six days, participants were debriefed, provided feedback on the study procedures, and reimbursed.
Statistical analyses
Linear regression models are unsuitable for ESM data, due to its clustered nature (Carter & Emsley, 2019). Multilevel regressions extend linear models by allowing for variation within and between participants, thereby accounting for ESM clustering (Garson, 2013). This study employed two-level (observations nested within participants) as opposed to three-level models (observations nested within days nested within participants), as the latter has been shown to be suboptimal in the presence of autocorrelation (de Haan-Rietdijk, Kuppens, & Hamaker, 2016), which temporal networks suggest is typical of psychotic experiences (Contreras, Valiente, Heeren, & Bentall, 2020; Jongeneel et al., 2020). Multilevel models were estimated using the XTREG module in STATA 14 (Statacorp, 2015). Multilevel models report standardized regression coefficients (b); their relative sizes were compared using Wald tests of coefficient standard errors (Wald, 1943). As a dimensional experience, analyses involving paranoia included all participants (N = 153). Analyses involving hallucinations only included participants who heard voices (n = 125) or saw visions (n = 97), respectively.
Proximal analyses tested whether DSO symptoms since or at the previous moment (i.e. time t − 1 for momentary item scores [negative self-concept] and time t for interval item scores [emotional dysregulation and interpersonal difficulties]) predict current psychotic symptom scores at time t, and whether this association persisted when controlling for PTSD symptoms since the previous moment (i.e. time t interval item scores).
Distal analyses tested whether lagged DSO scores (i.e. time t − 2 for momentary items and time t − 1 for interval items) predict current psychotic experiences at time t, and whether this association persisted when controlling for PTSD symptoms at time t − 1 (interval items).
The sampling scheme was quasi-random (i.e. beeps sent at random points within each consecutive 90-min interval), meaning the interval between beeps varied. The maximum interval between beeps during which DSO and PTSD items were measured spanned 3 hours in proximal analyses (e.g. if time t was at the end of the 90 min block, and time t − 1 was at the beginning of the previous block), and 6 hours in distal analyses. The average intervals, however, were 90 and 180 min, respectively. Non-consecutive scores were used where immediately preceding observations were missing.
Results
Descriptive statistics
Of a total 8174 data points, 3.326 (40.69%) were missing. On average, participants were scheduled 54 beeps (maximum = 60) over 6 days and responded to 59.26% of these (M = 32; s.d. = 15). Participants who responded to any notifications were included in the analysis, since multilevel models are robust against unbalanced data, though 2.83% of questionnaires were responded to outside a predetermined 15-min window and were excluded from analyses (Delespaul, 1995). A multilevel model including consecutive beeps as a predictor of missingness suggested measurements were increasingly more likely to be missed as the assessment period progressed (OR = 1.01, p < 0.001, 95% CI 1.00–1.01).
An experience was considered present if a participant rated ≥2, since 1 was anchored to ‘not at all’. Any paranoia item was endorsed at 4295 (93.03%) timepoints; voices and visions at 3077 (66.65%) and 2580 (55.88%) timepoints, respectively. Any core PTSD symptom was endorsed at 4397 (95.24%) timepoints, and any DSO at 4600 (99.63%) timepoints. Within-participant means and standard deviations of ESM variables are listed in Table 2.
Table 2.
Means (M) and standard deviations (s.d.) of within-participant means and within-participant standard deviations for all ESM variables
| Variable | M(s.d.) | MSD(s.d.) | |
|---|---|---|---|
| PTSD | Memory intrusions | 4.14 (1.41) | 1.49(0.64) |
| Avoidance | 4.30 (1.51) | 1.10(0.54) | |
| Hyperarousal | 4.11 (1.39) | 1.010(0.57) | |
| DSO | Emotional dysregulation | 4.10 (1.32) | 1.06(0.47) |
| Interpersonal difficulties | 4.61 (0.97) | 1.03(0.43) | |
| Negative self-concept | 3.78 (1.29) | 0.88(0.42) | |
| Psychosis | Paranoia | 4.24 (1.44) | 0.93(0.50) |
| Voices | 3.80 (2.11) | 0.97(0.75) | |
| Visions | 3.07 (1.96) | 0.92(0.71) | |
Note: All variables were measured using a 7-point Likert scale (range 1–7). M (s.d.) refers to means of each item across participants, and s.d.s of those mean scores between participants. MSD (s.d.) refers to the mean s.d. of each participant's own mean, and the s.d. between participants.
Proximal analyses
Multilevel linear regression models indicated that DSO symptoms since or at the previous moment significantly predicted paranoia, voices, and visions at the current moment. This effect of DSOs persisted for all three outcomes when including core PTSD symptoms since the previous moment, themselves also predicting all three outcomes. Wald tests suggested DSOs were a significantly better predictor of paranoia, but not voices or visions, than core PTSD symptoms. Regression and Wald test statistics are listed in Table 3.
Table 3.
Regression statistics of multilevel models
| Analysis | Outcome | Predictor(s) | b | 95% CI | Wald test statistic |
|---|---|---|---|---|---|
| Proximal | Paranoia (n = 153) | Step 1 | |||
| DSO | 0.662*** | 0.618, 0.706 | |||
| Step 2 | 5.55** | ||||
| DSO | 0.457*** | 0.408, 0.505 | |||
| PTSD | 0.285*** | 0.251, 0.319 | |||
| Voices (n = 125) | Step 1 | ||||
| DSO | 0.639*** | 0.576, 0.701 | |||
| Step 2 | 0.82 | ||||
| DSO | 0.382*** | 0.311, 0.453 | |||
| PTSD | 0.333*** | 0.146, 0.382 | |||
| Visions (n = 97) | Step 1 | ||||
| DSO | 0.482*** | 0.413, 0.551 | |||
| Step 2 | 0.04 | ||||
| DSO | 0.293*** | 0.183, 0.343 | |||
| PTSD | 0.275*** | 0.221, 0.328 | |||
| Distal | Paranoia (n = 153) | Step 1 | |||
| DSO | 0.392*** | 0.334, 0.451 | |||
| Step 2 | 2.52* | ||||
| DSO | 0.283*** | 0.216, 0.350 | |||
| PTSD | 0.149*** | 0.103, 0.196 | |||
| Voices (n = 125) | Step 1 | ||||
| DSO | 0.294*** | 0.213, 0.375 | |||
| Step 2 | 0.29 | ||||
| DSO | 0.182*** | 0.087, 0.277 | |||
| PTSD | 0.144*** | 0.079, 0.209 | |||
| Visions (n = 97) | Step 1 | ||||
| DSO | 0.235*** | 0.144, 0.325 | |||
| Step 2 | 0.10 | ||||
| DSO | 0.142** | 0.035, 0.248 | |||
| PTSD | 0.080** | 0.045, 0.187 |
*Significant at p < 0.05 level; **at p < 0.01 level; ***at p < 0.001 level.
Distal analyses
Multilevel linear regression models assessing whether lagged DSO scores (described above) predicted positive psychosis symptoms at the current moment, and whether this association persisted when controlling for lagged PTSD symptoms, showed the same pattern of findings as the proximal analyses. Wald tests suggested that DSOs were a significantly stronger predictor of paranoia, but not voices or visions, than core PTSD symptoms. Regression and Wald test statistics are listed in Table 3.
Discussion
We aimed to ascertain the relationship between cPTSD and psychosis symptoms in the flow of daily life in psychosis individuals who meet criteria for comorbid PTSD. Consistent with our hypotheses, the key findings indicate that both proximal and distal fluctuations in DSOs predicted momentary measures of paranoia, voices, and visions. These temporal associations persisted when controlling for fluctuations in core PTSD symptoms within the same timeframe. Furthermore, they were stronger than those between core PTSD and psychosis symptoms, which were themselves significant, particularly for paranoia.
To our knowledge, this is the first study demonstrating the impact of cPTSD in the daily life of people with psychosis. Our findings imply that cPTSD may play a key role in maintaining psychotic experiences in daily life. In particular, emotional and interpersonal difficulties, and negative self-concept, seem to have a greater influence on psychosis symptoms than traumatic memory intrusions, hypervigilance, and avoidance. These results align with cross-sectional research demonstrating the impact of complex trauma, PTSD, and prevalence of cPTSD in people with psychosis (Campodonico, Varese, & Berry, 2022; Panayi et al., 2022). They further extend those of previous ESM studies demonstrating the daily impact of childhood trauma and core PTSD in people with psychosis (Brand et al., 2020; Dokuz, Kani, Uysal, & Kuşcu, 2022) to include DSOs. In turn, our findings also align with prior ESM studies investigating the impact of constructs consistent with DSOs; for instance, momentary attachment insecurity (consistent with interpersonal difficulties) and emotional instability (consistent with emotional dysregulation) have been shown to increase subsequent paranoia (Nittel et al., 2018; Sitko, Varese, Sellwood, Hammond, & Bentall, 2016). The distal analyses carried out in this study confirmed that the short-term effect of DSOs on psychosis revealed by proximal analyses persists, albeit with smaller effect size, for a period of up to 6 hours. Significant relationships over this period suggest symptoms of cPTSD potentially earlier on in a day may affect subsequent psychotic experiences (especially for paranoia, where our confidence intervals are more robust).
The findings are aligned with an affective pathway to psychosis and multifactorial accounts of trauma in psychosis (Hardy, 2017; Morrison, Frame, & Larkin, 2003). Particularly, they highlight how negative self-beliefs, relationship difficulties, and emotion regulation may be important treatment targets alongside core symptoms of PTSD, since the effect of DSOs was comparatively larger than that of core PTSD symptoms for all positive psychosis symptoms (significantly so for paranoia). Novel statistical innovations may be used to extend the present findings by exploring the symptom overlap between cPTSD and psychosis, and by identifying directed paths between these clusters to support the development of trauma-focused psychosis interventions (e.g. using network analysis; Contreras et al., 2020).
There were a number of limitations in this study. Interval ESM items are standard in ESM questionnaire design (Eisele et al., 2022), but their use to make longitudinal assumptions could be questioned, since retrospective items could be influenced by current states and/or recall bias. However, DSOs by nature are psychologically reflective, such as emotional dysregulation (‘Since the last beep, I found it difficult to control my emotions’) and may occur infrequently enough that momentary items risk experiences being missed, such as interpersonal difficulties not arising due to a participant being alone (Eisele et al., 2022). Furthermore, the distal analyses findings mirrored those of the proximal analyses, providing strong evidence of a temporal relationship between DSOs and psychotic symptoms.
While a strength of this study was the inclusion of both visions and voices, the reliability of single items to measure them is questionable (Eisele et al., 2022). Hallucinations are multidimensional experiences, with disparate temporal dynamics for differing dimensions (Bless et al., 2020). Further, visual and auditory hallucinations can be difficult to distinguish from dissociative post-traumatic flashbacks (Wearne et al., 2022). Future studies should assess how different aspects of psychotic experiences (e.g. content, appraisal, impact/distress) may be affected by DSOs, and capture these experiences using multiple items to maximize precision.
ESM completion rates in this study may appear low at an average of 59%, indicating potential limitations with the sampling scheme. However, 6 days are considered a standard measurement window in ESM studies and participant-level variables more typically predict non-response in ESM than design characteristics (Rintala, Wampers, Myin-Germeys, & Viechtbauer, 2020; Vachon et al., 2019; van Berkel et al., 2020). Indeed, owing to the complexities of research engagement among people with psychosis, data attrition is more common than in control samples. The completion rates in our sample are typical of other ESM datasets in people with psychosis (Bell et al., 2024).
The majority of our sample (79%) met criteria for cPTSD on the ITQ (Cloitre et al., 2018). Our findings demonstrating a stronger relationship between DSOs and psychosis symptoms than those with core PTSD symptoms may have been a result of the preponderance of people with cPTSD relative to PTSD. Nevertheless, this imbalance is consistent with other trauma-exposed samples of people with psychosis (Panayi et al., 2022), and is typical of individuals presenting to mental health services, who overwhelmingly have complex trauma histories (Trauelsen et al., 2015). Additionally, 30% of our sample presented with personality disorder diagnoses alongside higher rates of ‘other non-organic psychosis’ than ESM non-participants. Since there were no significant differences in symptom severity between groups, our sample is likely representative of people with comorbid psychosis and PTSD symptoms. This includes those in EIP services, who show similar rates of clinically significant personality disorder traits (Archer, Shnyien, Mansfield, & Draycott, 2023), making our findings relevant to psychological interventions offered for this population.
Limitations notwithstanding, there are several implications of these findings. The potentially maintaining role of DSO symptoms supports current trauma-focused therapy practices involving stabilization to establish emotion regulation and build positive relationships, such as trauma-focused cognitive-behavioral and eye-movement desensitization and reprocessing therapies (Keen, Hunter, & Peters, 2017; Peters et al., 2022). Therapeutic approaches aimed at addressing intra- and interpersonal wellbeing, such as compassion-focused techniques (Millard, Wan, Smith, & Wittkowski, 2023), may also be a promising avenue for the ongoing development of trauma-focused psychosis interventions, particularly for those who may find trauma reprocessing intolerable (Lewis, Roberts, Gibson, & Bisson, 2020). Our findings also suggest that the assessment of DSOs may be highly relevant for subgroups of people with psychosis and complex trauma histories. This assessment should be sensitive to the potential difficulties associated with cPTSD, including establishing social support and emotional regulation to manage distress associated with trauma disclosure (UK Psychological Trauma Society, 2017). Lastly, the large proportion of participants in our sample endorsing visual hallucinations suggests the assessment of hallucinations in modalities other than auditory could be valuable.
To conclude, this study highlights the profound impact of cPTSD on people with psychosis. Specifically, DSO symptoms (i.e. emotional dysregulation, negative self-concept, and interpersonal difficulties) may maintain psychosis symptoms in the flow of daily life to an even greater extent than core PTSD symptoms. In turn, the exacerbation of distressing psychosis symptoms is in addition to the direct impact of these difficulties on individuals' quality of life and daily functioning. Future research is required to delineate relationships between specific symptoms of psychosis, PTSD and DSOs, as well as mechanisms by which this impact occurs. There are clear clinical implications to this research, namely confirming the need for incorporating therapeutic practices aimed at addressing DSOs in trauma-focused psychosis interventions.
Supporting information
Panayi et al. supplementary material
Acknowledgements
The authors would like to thank the ESRC and NIHR for funding this study. Thank you also to all participants of the STAR trial for their participation. For the purposes of Open Access, the authors have applied a Creative Commons Attribution (CC BY) license to any Accepted Author Manuscript version arising from this submission.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724001934.
Funding statement
This work was supported by the Economic and Social Research Council (2488414 to PP) and the National Institute of Health Research (NIHR) (NIHR128623 and NIHR130971). AH was funded in part by the NIHR Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London.
Collaborators
Affiliated with South London and Maudsley NHS Foundation Trust
Lucy Ring
Christopher Shoulder
Morwennna Rickard
Firat Denizcaglar
Kavita Bains
Freya Meyer
Leilia Jameel
Majella Byrne
Nadine Keen
Sarah Swan
Rachel Frost
Ze Freeman
Gary Ngai
Jess Bird
Constance Harvey
Edward Bickers
Kaisha Santosa
Samantha Mansell
Siamara Goddard
Molly Bird
Harriet Mellotte
Rhea Kohli
Katja Shultz
Antonia Obele
Elizabeth Leahy
Max Dormitontov
Faiza Abbaz
Ho Chak (Milton) Suen
Affiliated with King's College London
Margaret Heslin
Emma Tassie
Sarah Byford
Elizabeth Kuipers
Laura Potts
Inez Verdaasdonk
Affiliated with Greater Manchester Mental Health NHS Foundation Trust
Tony Morrison
Wendy Jones
Eleanor Longden
Aqsa Choudary
Marina Sandys
Kim Towey-Swift
Elizabeth Murphy
Vicky Brooks
Samantha Bowe
Alice Newton-Braithwaite
Elliot Brewer
Leah Orme
Affiliated with University of Manchester
Tony Morrison
Affiliated with Cumbria, Northumberland, Tyne, and Wear NHS Foundation Trust
Rebecca Miskin
Laura McCartney
Marsha Cochrane
Antonia Newman
Sarah White
Nina Cioroboiu
Louise Prentice
Jane Mitchell
Doug Turkington
Kevin Meares
Libby Oakes
Affiliated with Oxford Health NHS Foundation Trust
Amy Langman
Emily Smyth
Georgina Kirtland
Natalie Barnes
Kate Costello
Collins Larrys
Iulia Grabovschi
Charlotte Sagnay de la Bastida
Affiliated with Sussex Partnership NHS Foundation Trust
Kathryn Greenwood
Cat Sacadura
Sarah Mansfield
Ann Steele
Lauren Edwards
Dan Elton
Angie Culham
Nick Grey
Molly Heeger
Lucy Fisher
Krutika Sharma
Chris Scane
Lisa Wood
Joseph Sherborne
Lauren Mose
Guy Emery
Aparajita Pandey
Affiliated with University of Sussex
Kathryn Greenwood
David Fowler
Competing interests
E. P., A. H., F. V., C. S., and R. U. provide psychological therapies for individuals with psychosis and/or PTSD in NHS settings, and E. P. is the Director of a psychological therapies specialist service for psychosis (PICuP). C. S. has written manuals for psychological therapies for psychosis and psychological formulation for which they receive book royalties (from APPI; Guildford Press; Wiley; Routledge; New Harbinger). E. P., A. H., F. V., and C. S. are employed to provide training and/or receive fees (or generate fees for their clinics or research units) for workshops and presentations on psychological therapies for psychosis and/or PTSD; E. P., A. H., F. V., C. S., and R. E. hold or have held grants to carry out trials of psychological therapy for individuals with psychosis. R. E. is a member of the NIHR HTA Clinical Evaluation and Trials Committee.
References
- Alameda, L., Rodriguez, V., Carr, E., Aas, M., Trotta, G., Marino, P., … Murray, R. M. (2020). A systematic review on mediators between adversity and psychosis: Potential targets for treatment. Psychological Medicine, 50(12), 1966–1976. 10.1017/S0033291720002421 [DOI] [PubMed] [Google Scholar]
- Archer, M., Shnyien, A., Mansfield, S., & Draycott, S. (2023). Mentalizing in first-episode psychosis: Correlates with symptomatology and traits of borderline personality disorder. Early Intervention in Psychiatry, 17(6), 617–624. 10.1111/eip.13356 [DOI] [PubMed] [Google Scholar]
- Bell, C. J., Foulds, J. A., Horwood, L. J., Mulder, R. T., & Boden, J. M. (2019). Childhood abuse and psychotic experiences in adulthood: Findings from a 35-year longitudinal study. British Journal of Psychiatry, 214(3), 153–158. 10.1192/bjp.2018.264 [DOI] [PubMed] [Google Scholar]
- Bell, I. H., Eisner, E., Allan, S., Cartner, S., Torous, J., Bucci, S., … Thomas, N. (2024). Methodological characteristics and feasibility of ecological momentary assessment studies in psychosis: A systematic review and meta-analysis. Schizophrenia Bulletin, 50(2), 238–265. 10.1093/schbul/sbad127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bless, J. J., Hjelmervik, H., Torsheim, T., Gudmundsen, M., Larøi, F., Holma, I., … Hugdahl, K. (2020). Temporal signatures of auditory verbal hallucinations: An app-based experience sampling study. Schizophrenia Research, 215, 442–444. 10.1016/J.SCHRES.2019.11.020 [DOI] [PubMed] [Google Scholar]
- Bloomfield, M. A. P., Chang, T., Woodl, M. J., Lyons, L. M., Cheng, Z., Bauer-Staeb, C., … Lewis, G. (2021). Psychological processes mediating the association between developmental trauma and specific psychotic symptoms in adults: A systematic review and meta-analysis. World Psychiatry, 20(1), 107–123. 10.1002/wps.20841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum, L. H., Vakhrusheva, J., Saperstein, A., Khan, S., Chang, R. W., Hansen, M. C., … Kimhy, D. (2015). Depressed mood in individuals with schizophrenia: A comparison of retrospective and real-time measures. Psychiatry Research, 227, 318. 10.1016/J.PSYCHRES.2015.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand, R. M., Bendall, S., Hardy, A., Rossell, S. L., Meyer, D., & Thomas, N. (2020). Moment-to-moment associations between posttraumatic stress symptoms and auditory hallucinations in the flow of daily life. Psychiatry Research, 285, 112838. 10.1016/j.psychres.2020.112838 [DOI] [PubMed] [Google Scholar]
- Campodonico, C., Varese, F., & Berry, K. (2022). Trauma and psychosis: A qualitative study exploring the perspectives of people with psychosis on the influence of traumatic experiences on psychotic symptoms and quality of life. BMC Psychiatry, 22(1), 1–12. 10.1186/S12888-022-03808-3/TABLES/1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr, S., Hardy, A., & Fornells-Ambrojo, M. (2018). The Trauma and Life Events (TALE) checklist: Development of a tool for improving routine screening in people with psychosis. European Journal of Psychotraumatology, 9(1), 1512265. 10.1080/20008198.2018.1512265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter, L. A., & Emsley, R. (2019). The analysis of experience sampling data. In Palmier-Claus J. E., Haddock G., & Varese F. (Eds.), Experience sampling in mental health research (pp. 18–37). New York, NY: Routledge/Taylor & Francis Group. 10.4324/9781315398341-3 [DOI] [Google Scholar]
- Chun, C. A. (2016). The expression of posttraumatic stress symptoms in daily life: A review of experience sampling methodology and daily diary studies. Journal of Psychopathology and Behavioral Assessment, 38(3), 406–420. 10.1007/s10862-016-9540-3 [DOI] [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. 10.1111/acps.12956 [DOI] [PubMed] [Google Scholar]
- Contreras, A., Valiente, C., Heeren, A., & Bentall, R. (2020). A temporal network approach to paranoia: A pilot study. Frontiers in Psychology, 11, 544565. 10.3389/fpsyg.2020.544565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker, S. E., Rosen, M. I., Cooney, N. L., Schnurr, P. P., & Black, A. C. (2021). Correspondence between retrospective and momentary self-reported posttraumatic stress disorder symptoms: Evidence for peak and end effects in veterans. Journal of Traumatic Stress, 34(4), 889–894. 10.1002/JTS.22669 [DOI] [PubMed] [Google Scholar]
- de Haan-Rietdijk, S., Kuppens, P., & Hamaker, E. L. (2016). What's in a day? A guide to decomposing the variance in intensive longitudinal data. Frontiers in Psychology, 7, 891. 10.3389/fpsyg.2016.00891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delespaul, P. A. E. G. (1995). Assessing schizophrenia in daily life: The experience sampling method (Doctoral dissertation). Maastricht University, Maastricht, Netherlands. 10.26481/dis.19950504pd [DOI] [Google Scholar]
- DeTore, N. R., Gottlieb, J. D., & Mueser, K. T. (2021). Prevalence and correlates of PTSD in first episode psychosis: Findings from the RAISE-ETP study. Psychological Services, 18(2), 147–153. 10.1037/ser0000380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vries, B., Van Busschbach, J. T., Van Der Stouwe, E. C. D., Aleman, A., Van Dijk, J. J. M., Lysaker, P. H., … Pijnenborg, G. H. M. (2019). Prevalence rate and risk factors of victimization in adult patients with a psychotic disorder: A systematic review and meta-analysis. Schizophrenia Bulletin, 45(1), 114–126. 10.1093/schbul/sby020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dokuz, G., Kani, A. S., Uysal, Ö., & Kuşcu, M. K. (2022). The impact of childhood trauma and daily life experiences on emotional and psychotic symptom intensity in psychosis: An experience sampling study. Psychiatry Research, 317, 114872. 10.1016/J.PSYCHRES.2022.114872 [DOI] [PubMed] [Google Scholar]
- Drake, R., Haddock, G., Tarrier, N., Bentall, R., & Lewis, S. (2007). The psychotic symptom rating scales (PSYRATS): Their usefulness and properties in first episode psychosis. Schizophrenia Research, 89(1–3), 119–122. 10.1016/j.schres.2006.04.024 [DOI] [PubMed] [Google Scholar]
- Eisele, G., Kasanova, Z., & Houben, M. (2022). Questionnaire design & evaluation. In Myin-Germeys I., & Kuppens P. (Eds.), The open handbook of experience sampling methodology (2nd ed., pp. 71–89). Leuven: The center for Research on Experience sampling and Ambulatory methods Leuven (REAL). [Google Scholar]
- Forkmann, T., Spangenberg, L., Rath, D., Hallensleben, N., Hegerl, U., Kersting, A., & Glaesmer, H. (2018). Assessing suicidality in real time: A psychometric evaluation of self-report items for the assessment of suicidal ideation and its proximal risk factors using ecological momentary assessments. Journal of Abnormal Psychology, 127(8), 758–769. 10.1037/abn0000381 [DOI] [PubMed] [Google Scholar]
- Freeman, D., Loe, B. S., Kingdon, D., Startup, H., Molodynski, A., Rosebrock, L., … Bird, J. C. (2021). The revised Green et al., paranoid thoughts scale (R-GPTS): Psychometric properties, severity ranges, and clinical cut-offs. Psychological Medicine, 51(2), 244–253. 10.1017/S0033291719003155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost, R., Louison Vang, M., Karatzias, T., Hyland, P., & Shevlin, M. (2019). The distribution of psychosis, ICD-11 PTSD and complex PTSD symptoms among a trauma-exposed UK general population sample. Psychosis, 11(3), 187–198. 10.1080/17522439.2019.1626472 [DOI] [Google Scholar]
- Garson, G. D. (2013). Hierarchical linear modeling: Guide and applications. Los Angeles, CA: SAGE Publications Inc. 10.4135/9781483384450 [DOI] [Google Scholar]
- Haddock, G., McCarron, J., Tarrier, N., & Faragher, E. B. (1999). Scales to measure dimensions of hallucinations and delusions: The psychotic symptom rating scales (PSYRATS). Psychological Medicine, 29(4), 879–889. 10.1017/S0033291799008661 [DOI] [PubMed] [Google Scholar]
- Hardy, A. (2017). Pathways from trauma to psychotic experiences: A theoretically informed model of posttraumatic stress in psychosis. Frontiers in Psychology, 8, 697. 10.3389/fpsyg.2017.00697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy, A., Emsley, R., Freeman, D., Bebbington, P., Garety, P. A., Kuipers, E. E., … Fowler, D. (2016). Psychological mechanisms mediating effects between trauma and psychotic symptoms: The role of affect regulation, intrusive trauma memory, beliefs, and depression. Schizophrenia Bulletin, 42(Suppl. 1), S34–S43. 10.1093/schbul/sbv175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy, A., O'Driscoll, C., Steel, C., Van Der Gaag, M., & Van Den Berg, D. (2021). A network analysis of post-traumatic stress and psychosis symptoms. Psychological Medicine, 51(14), 2485–2492. 10.1017/S0033291720001300 [DOI] [PubMed] [Google Scholar]
- Jongeneel, A., Aalbers, G., Bell, I., Fried, E. I., Delespaul, P., Riper, H., … van den Berg, D. (2020). A time-series network approach to auditory verbal hallucinations: Examining dynamic interactions using experience sampling methodology. Schizophrenia Research, 215, 148–156. 10.1016/j.schres.2019.10.055 [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Cloitre, M., Maercker, A., Kazlauskas, E., Shevlin, M., Hyland, P., … Brewin, C. R. (2017). PTSD and complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. European Journal of Psychotraumatology, 8(Suppl. 7), 1418103. 10.1080/20008198.2017.1418103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keen, N., Hunter, E. C. M., & Peters, E. (2017). Integrated trauma-focused cognitive-behavioural therapy for post-traumatic stress and psychotic symptoms: A case-series study using imaginal reprocessing strategies. Frontiers in Psychiatry, 8, 1. 10.3389/fpsyt.2017.00092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhy, D., Delespaul, P., Corcoran, C., Ahn, H., Yale, S., & Malaspina, D. (2006). Computerized experience sampling method (ESMc): Assessing feasibility and validity among individuals with schizophrenia. Journal of Psychiatric Research, 40(3), 221–230. 10.1016/j.jpsychires.2005.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, C., Roberts, N. P., Gibson, S., & Bisson, J. I. (2020). Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1709709. 10.1080/20008198.2019.1709709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Van Ommeren, M., Jones, L. M., … Reed, G. M. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD-11. World Psychiatry, 12(3), 198–206. 10.1002/wps.20057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeish, D., Stapleton, L. M., & Silverman, R. D. (2017). On the unnecessary ubiquity of hierarchical linear modeling. Psychological Methods, 22(1), 114–140. 10.1037/met0000078 [DOI] [PubMed] [Google Scholar]
- Mestdagh, M., Verdonck, S., Piot, M., Niemeijer, K., Tuerlinckx, F., Kuppens, P., … Dejonckheere, E. (2023). M-Path: An easy-to-use and flexible platform for ecological momentary assessment and intervention in behavioral research and clinical practice. Frontiers in Digital Health, 18(5), 1182175. 10.3389/fdgth.2023.1182175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millard, L. A., Wan, M. W., Smith, D. M., & Wittkowski, A. (2023). The effectiveness of compassion focused therapy with clinical populations: A systematic review and meta-analysis. Journal of Affective Disorders, 326, 168–192. 10.1016/J.JAD.2023.01.010 [DOI] [PubMed] [Google Scholar]
- Morrison, A. P., Frame, L., & Larkin, W. (2003). Relationships between trauma and psychosis: A review and integration. British Journal of Clinical Psychology, 42(4), 331–353. 10.1348/014466503322528892 [DOI] [PubMed] [Google Scholar]
- Myin-Germeys, I., Kasanova, Z., Vaessen, T., Vachon, H., Kirtley, O., Viechtbauer, W., & Reininghaus, U. (2018). Experience sampling methodology in mental health research: New insights and technical developments. World Psychiatry, 17(2), 123–132. 10.1002/wps.20513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nittel, C. M., Lincoln, T. M., Lamster, F., Leube, D., Rief, W., Kircher, T., & Mehl, S. (2018). Expressive suppression is associated with state paranoia in psychosis: An experience sampling study on the association between adaptive and maladaptive emotion regulation strategies and paranoia. The British Journal of Clinical Psychology, 57(3), 291–312. 10.1111/BJC.12174 [DOI] [PubMed] [Google Scholar]
- Palmier-Claus, J., Haddock, G., & Varese, F. (2019). Experience sampling in mental health research (1st ed.). New York, NY: Routledge/Taylor & Francis Group. 10.4324/9781315398341 [DOI] [Google Scholar]
- Panayi, P., Berry, K., Sellwood, W., Campodonico, C., Bentall, R. P., & Varese, F. (2022). The role and clinical correlates of complex post-traumatic stress disorder in people with psychosis. Frontiers in Psychology, 13, 700. 10.3389/fpsyg.2022.791996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters, E., Hardy, A., Dudley, R., Varese, F., Greenwood, K., Steel, C., … Morrison, A. (2022). Multisite randomised controlled trial of trauma-focused cognitive behaviour therapy for psychosis to reduce post-traumatic stress symptoms in people with co-morbid post-traumatic stress disorder and psychosis, compared to treatment as usual: Study protocol for the STAR (Study of Trauma and Recovery) trial. Trials, 23(1), 1–26. 10.1186/S13063-022-06215-X/FIGURES/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram, N., & Gerstorf, D. (2009). Time-structured and net intraindividual variability: Tools for examining the development of dynamic characteristics and processes. Psychology and Aging, 24(4), 778–791. 10.1037/a0017915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rintala, A., Wampers, M., Myin-Germeys, I., & Viechtbauer, W. (2020). Momentary predictors of compliance in studies using the experience sampling method. Psychiatry Research, 286, 112896. 10.1016/j.psychres.2020.112896 [DOI] [PubMed] [Google Scholar]
- Sideli, L., Murray, R. M., Schimmenti, A., Corso, M., La Barbera, D., Trotta, A., & Fisher, H. L. (2020). Childhood adversity and psychosis: A systematic review of bio-psycho-social mediators and moderators. Psychological Medicine, 50(11), 1761–1782. 10.1017/S0033291720002172 [DOI] [PubMed] [Google Scholar]
- Sitko, K., Bentall, R. P., Shevlin, M., O'Sullivan, N., & Sellwood, W. (2014). Associations between specific psychotic symptoms and specific childhood adversities are mediated by attachment styles: An analysis of the national comorbidity survey. Psychiatry Research, 217(3), 202–209. 10.1016/j.psychres.2014.03.019 [DOI] [PubMed] [Google Scholar]
- Sitko, K., Varese, F., Sellwood, W., Hammond, A., & Bentall, R.(2016). The dynamics of attachment insecurity and paranoid thoughts: An experience sampling study. Psychiatry Research, 246, 32–38. 10.1016/J.PSYCHRES.2016.08.057 [DOI] [PubMed] [Google Scholar]
- Statacorp. (2015). Statistical software: Release 14. College Station, TX: Statacorp LP. [Google Scholar]
- Trauelsen, A. M., Bendall, S., Jansen, J. E., Nielsen, H. G. L., Pedersen, M. B., Trier, C. H., … Simonsen, E. (2015). Severity and persistence versus type of childhood adversity in non-affective first-episode psychosis. Schizophrenia Research, 168(1–2), 573–574. 10.1016/j.schres.2015.06.020 [DOI] [PubMed] [Google Scholar]
- Trull, T. J., & Ebner-Priemer, U. W. (2009). Using experience sampling methods/ecological momentary assessment (ESM/EMA) in clinical assessment and clinical research: Introduction to the special section. Psychological Assessment, 21(4), 457–462. 10.1037/a0017653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang, W. (2023). Psychometric validation of an adapted self-rated version of the PSYRATS (Doctoral dissertation). King's College London, London, UK. [Google Scholar]
- UK Psychological Trauma Society. (2017). Guideline for the treatment and planning of services for complex post-traumatic stress disorder in adults (McFetridge M., Swan A., Heke S., Karatzias T., Greenberg N., Kitchiner N., & Morley R., Eds.). London, UK: UK Psychological Trauma Society. [Google Scholar]
- Vachon, H., Viechtbauer, W., Rintala, A., & Myin-Germeys, I. (2019). Compliance and retention with the experience sampling method over the continuum of severe mental disorders: Meta-analysis and recommendations. Journal of Medical Internet Research, 21(12), e14475. 10.2196/14475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Berkel, N., Goncalves, J., Hosio, S., Sarsenbayeva, Z., Velloso, E., & Kostakos, V. (2020). Overcoming compliance bias in self-report studies: A cross-study analysis. International Journal of Human-Computer Studies, 134, 1–12. 10.1016/j.ijhcs.2019.10.003 [DOI] [Google Scholar]
- Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., … Bentall, R. P. (2012). Childhood adversities increase the risk of psychosis: A meta-analysis of patient–control, prospective-and cross-sectional cohort studies. Schizophrenia Bulletin, 38(4), 661–671. 10.1093/schbul/sbs050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wald, A. (1943). Tests of statistical hypotheses concerning several parameters when the number of observations is large. Transactions of the American Mathematical Society, 54(3), 426–482. 10.1090/S0002-9947-1943-0012401-3 [DOI] [Google Scholar]
- Wang, L. P., Hamaker, E., & Bergeman, C. S. (2012). Investigating inter-individual differences in short-term intra-individual variability. Psychological Methods, 17(4), 567–581. 10.1037/a0029317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wearne, D., Ayalde, J., Curtis, G., Gopisetty, A., Banerjee, A., Melvill-Smith, P., … Waters, F. (2022). Visual phenomenology in schizophrenia and post-traumatic stress disorder: An exploratory study. BJPsych Open, 8(4), e143. 10.1192/bjo.2022.544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., … Marx, B. P. (2018). The clinician-administered PTSD scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, J., Bucci, S., Berry, K., & Varese, F. (2018). Psychological mediators of the association between childhood adversities and psychosis: A systematic review. Clinical Psychology Review, 65, 175–196. 10.1016/j.cpr.2018.05.009 [DOI] [PubMed] [Google Scholar]
- World Health Organisation. (2019). International classification of diseases-11 (11th ed.). Geneva, Switzerland: World Health Organisation. Retrieved from https://icd.who.int/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Panayi et al. supplementary material