Summary
Objective
To assess completeness and accuracy of children's body mass index (BMI) recorded in general practice electronic health records (GP‐EHRs).
Methods
We linked National Child Measurement Programme (NCMP) records from 29 839 5‐year‐olds and 26 660 11‐year‐olds attending state schools in inner London to GP‐EHRs (95% linked; 49.1% girls). We estimated adjusted odds (aOR) of at least one GP‐BMI record by sex, ethnic background, area‐level deprivation, weight‐status and long‐term conditions. We examined within‐child BMI differences and compared obesity prevalence from these sources.
Results
10.5% (2964/28330) and 26.0% (6598/25365) of 5‐ and 11‐year‐olds respectively had at least one GP‐BMI record. Underweight (aOR;95% CI:1.71;1.34,2.19), obesity (1.45;1.27,1.65), South Asian background (1.55;1.38,1.74), presence of a long‐term condition (8.15;7.31,9.10), and residence in deprived areas (Wald statistic 38.73; P‐value<0.0001) were independently associated with at least one GP‐BMI record. NCMP‐BMI and GP‐BMI differed by +0.45(95% Limits of Agreement −1.60,+2.51) and + 0.16(−2.86,+3.18) in 5‐ and 11‐year‐olds, respectively. The prevalence of obesity based on GP‐BMI was 18.2%(16.1,20.5) and 35.9%(33.9,38.0) in 5‐ and 11‐year‐olds respectively, compared to 12.9%(12.5,13.3) and 26.9%(26.4,27.4) based on NCMP‐BMI.
Conclusion
Child BMI is not comprehensively recorded in urban general practice. Linkage to school measurement records is feasible and enables assessment of health outcomes of obesity.
Keywords: childhood, general practice, BMI, electronic health records
1. INTRODUCTION
Childhood obesity is a major public health concern globally and reflects a complex number of factors, in particular socio‐economic inequalities. 1 In England, more than one‐quarter of children leave primary school with overweight or obesity, at a level of severity defined as in need of clinical intervention. 2 However, evidence to quantify the risk of adverse health outcomes at different overweight and obesity thresholds is lacking, 3 as are evidence‐based interventions to support families and children with obesity to regain a healthy weight. 4
In the United Kingdom (UK), National Health Service (NHS) general practitioner electronic health records (GP‐EHRs) comprise a potentially important source of data on the health outcomes of childhood obesity; however, the quality of the anthropometric data recorded for children remains unclear. Van Jaarsveld et al reported that the prevalence of childhood overweight and obesity estimated using the UK Clinical Practice Research Datalink (CPRD) was broadly similar to that obtained from other national data sources, but did not otherwise report on the representativeness or accuracy of GP‐BMI measurements. 5 Studies reporting the completeness, representativeness or accuracy of child body mass index (BMI) recorded in GP‐EHRs in the UK are lacking. Data quality and assessment of the completeness, representativeness and accuracy of GP‐BMI records are essential to avoid biases in estimates of the prevalence or outcomes of childhood obesity. This is particularly relevant, given the increasing use of data recorded in EHRs.
In this report, we examine the quality of BMI recorded in GP‐EHRs (GP‐BMI) by using pseudonymized data collected as part of a wider research programme on childhood obesity linking data from the National Child Measurement Programme (NCMP) to GP‐EHRs for a geographically‐defined population of children living in an inner city area of high obesity prevalence. 6 The NCMP was established in 2006 and entails annual measurement of the height and weight of all consenting 4‐5‐ and 10‐11‐year‐olds attending state‐maintained primary schools in England by trained observers using standard protocols. This information is used by Public Health England (PHE) to calculate BMI and report the prevalence of childhood obesity at a population level; although optional, parents or carers are also usually informed of their child's weight status. 6 Since 2014, the NCMP record has included the child's NHS number which provides a unique identifier for linkage.
Specifically, we aimed to, firstly, estimate the proportion of children with a GP‐BMI record and its variation by child demographic, anthropometric and clinical characteristics, secondly, to assess the within‐child agreement between BMI values derived from GP and NCMP records and thirdly, to compare weight status assigned using clinical reference standards derived from GP‐ and NCMP‐recorded weights and heights. We also set out to compare estimates of the population prevalence of underweight, overweight and obesity derived from these two sources for the same time period and population.
2. METHODS
2.1. Study population
We included all children (n = 60 891) who participated in the NCMP in the school years 2013/14 to 2016/17 in three inner east London local authorities: City and Hackney (school years included: 2013‐17), Newham (2014‐17) and Tower Hamlets (2015‐17) (median participation 96.1%). We linked NCMP records to GP‐EHRs using pseudonymized NHS numbers created using a study‐specific encryption key as the linkage field with OpenPseudonymiser software. 7
2.2. Height, weight and BMI measurements from GP‐EHRs
General practitioners (GPs) in the study localities are encouraged to use a data entry template to record height and weight in the Egton Medical Information System (EMIS) electronic patient record. BMI is automatically calculated in EMIS from the most recently entered height or weight values recorded. Hence it is possible that BMI may be calculated using a current weight measurement but an earlier height measurement. GPs also have an option to record BMI directly.
We obtained anthropometric data, including actual dates of measurement, from the GP‐EHRs of children participating in the NCMP and who were registered with GPs in City and Hackney, Newham and Tower Hamlets. In order to assess the accuracy of measurements, we included all height, weight and BMI values as recorded in the GP‐EHR, even where these might be considered biologically implausible, for example, measurements falling outside the permitted range or those with “extreme” z‐scores, according to the NCMP validation guidance. 8
2.3. Height, weight and BMI measurements from NCMP
In the NCMP, children are measured without shoes or outdoor clothing by trained teams, with weight recorded to the nearest 0.1 kg, and height to the nearest 0.1 cm. 6 We obtained height, weight and BMI (NCMP‐BMI) measurements and other derived variables from the validated NCMP record created and returned to local authorities by PHE for all NCMP participants for the time periods and areas described above. As the available date of NCMP measurement was restricted to month and year, we randomly assigned a day of measurement within term‐time, excluding weekends and bank holidays to avoid a spurious reduction in variance in age at measurement occasioned by using the same fixed date of measurement for every child (R Studio; version 1.0.153; code available on request).
2.4. Outcome measures
We determined representativeness by estimating the proportion of children with at least one GP‐recorded BMI, defined as the presence in the GP‐EHR of a BMI value greater than zero under Read code “22K..”. We derived a continuous variable to count the number of occasions a non‐zero value was recorded and establish the total number of occasions a GP‐BMI was recorded for each child.
We calculated within‐child differences between NCMP‐BMI and GP‐BMI values, when these were recorded within 1 month of each other, using NCMP‐BMI calculated from measurements made by trained observers as a reference standard.
Weight status was determined according to two reference standards: the UK1990 clinical and UK1990 population reference standards. 9 The UK1990 clinical thresholds are used to categorize BMI as overweight or obese among children deemed to be in need of clinical intervention, and are appropriate to use in both a clinical setting as well as when directly reporting weight status to parents about their child. The UK1990 population thresholds are used for population surveillance of overweight and obesity and are widely used for reporting obesity prevalence in the UK.
We compared NCMP‐ and GP‐derived weight status in individuals with NCMP and GP‐recorded BMI within 1 month of each other using the UK1990 clinical cut‐offs, categorising BMI into one of four mutually exclusive groups: “underweight” (BMI < 2nd centile), “healthy weight” (≥2nd to <91st centile), “overweight” (≥91st to <98th centile) or “obese” (≥98th centile) based on alignment with sex‐ and age‐specific BMI centiles using the LMS growth tool Excel add‐in. 10 , 11
To estimate the population prevalence of each weight status category, we applied the UK1990 population reference standard, which categorizes BMI into one of the four mutually exclusive groups using lower thresholds for overweight and obese categories relative to those used for clinical cut‐offs: “underweight” (BMI < 2nd centile), “healthy weight” (≥2nd to <85th centile), “overweight” (≥85th to <95th centile) or “obese” (≥95th centile). We compared prevalence of these weight status categories based on GP‐BMI and NCMP‐BMI.
2.5. Covariates
Child ethnic background was derived from the NCMP data file 6 and defined using the National Health Service classification. 12 We grouped ethnic background into four mutually exclusive groups: White (“White British”, “White Irish”, or “any other White background”); Black (“Black African”, “Black Caribbean”, or “any other Black background”); South Asian (“Indian”, “Pakistani”, “Bangladeshi” or “Sri Lankan”); and a combination of Mixed and Other (“any other ethnic background”, “mixed ethnicity”, “Chinese” or “Asian other”). Where ethnic background was missing or reported as “not stated” in the NCMP (n = 6486), we used ethnic background as recorded in the GP‐EHR (n = 4672), leaving 1814 children with missing data.
An area‐level measure of relative deprivation—Index of Multiple Deprivation (IMD, 2015) score and an associated decile 13 —was assigned to each NCMP record by PHE, based on the lower super output area (LSOA, 2011) within which the postcode of the child's home address is located. We concatenated IMD decile into five quintiles ranging from most to least deprived.
A binary variable was derived to indicate children with one or more long‐term health conditions, using information from the linked GP‐EHR. This variable was coded “1” if the child had ever had a GP diagnosis of: asthma (Read codes: H33%, 173A.); cystic fibrosis (C370.); type 1 diabetes (C10E., C10EM); attention deficit hyperactivity disorder (ADHD) or autism (Eu9%); or a learning disability (E3%, Eu7%, Eu814, Eu815, Eu816, Eu817, Eu81z, 918e, Eu818, 8HHP). Additionally, this variable was coded “1” if the child was prescribed medications for: epilepsy (British National Formulary [BNF] chapter: 4.8); ADHD (4.4); thyroid disease (6.2.1); or asthma (3.1, 3.2, 3.3 [if the EHR contained both an asthma diagnosis and medication prescription]).
2.6. Statistical analyses
We explored potential linkage biases by examining differences in demographic characteristics of those linked compared to those not linked. We estimated the proportion of 5‐ and 11‐year‐olds with at least one GP‐BMI record and examined its variation by sex, ethnic background, NCMP‐derived weight status, presence of a long‐term condition, IMD quintile and school local authority. We conducted binary logistic regression to estimate the odds (Odds Ratio [OR]), adjusted odds (aOR) and associated 95% Confidence Intervals (CI) of having at least one GP‐BMI record, before and after mutually adjusting for the above covariates. We used Bland‐Altman methods 14 to assess within‐child agreement and estimate 95% limits of agreement between NCMP‐BMI and GP‐BMI. We categorized GP‐BMI and NCMP‐BMI according to the UK1990 clinical cut‐offs 9 and estimated the number of children whose weight status from GP‐BMI would be categorized differently to that derived from NCMP‐BMI. We identified all GP‐BMI entries recorded between September 2013 and August 2017 for children aged 4‐5 and 10‐11 years at the time of measurement. We identified the GP‐BMI entry recorded closest in time to NCMP‐BMI date of measurement among children with more than one instance of GP‐BMI during this period and used these measurements to estimate the prevalence of underweight, healthy weight, overweight and obesity derived from the GP‐EHR using the UK1990 population cut‐offs. 9 We compared this to equivalent NCMP‐derived prevalences for the same time period and age groups. All analyses were conducted using Stata/MP 15 (StataCorp LP).
2.7. Ethics approval
The analyses of linked pseudonymized NCMP and general practice data were approved by the respective data controllers under data processing agreements which allow linkage of pseudonymized NCMP data between the research organisation (Clinical Effectiveness Group, Queen Mary University of London) and each local authority public health team. Ethics approval for this study was not required under Health Research Authority guidelines. 15
3. RESULTS
After removing 4285 records with invalid or missing NHS numbers, 74 records which were exact duplicates, and retaining only the most recent measurement of 33 children measured on two separate occasions, 56 499 (92.8%) of 60 891 NCMP records were available for linkage, comprising, respectively, 20 239, 27 666 and 12 986 children in City and Hackney, Newham and Tower Hamlets. We linked NCMP records to GP‐EHRs for 53 695 children (95.0%; 28 330 5‐year‐olds and 25 365 11‐year‐olds; Figure 1). The proportion of children participating in the NCMP in Tower Hamlets, in the 2016/17 school year, from South Asian ethnic backgrounds, and living in the most deprived IMD quintile were over‐represented among those linked compared to those not (Table S1).
FIGURE 1.
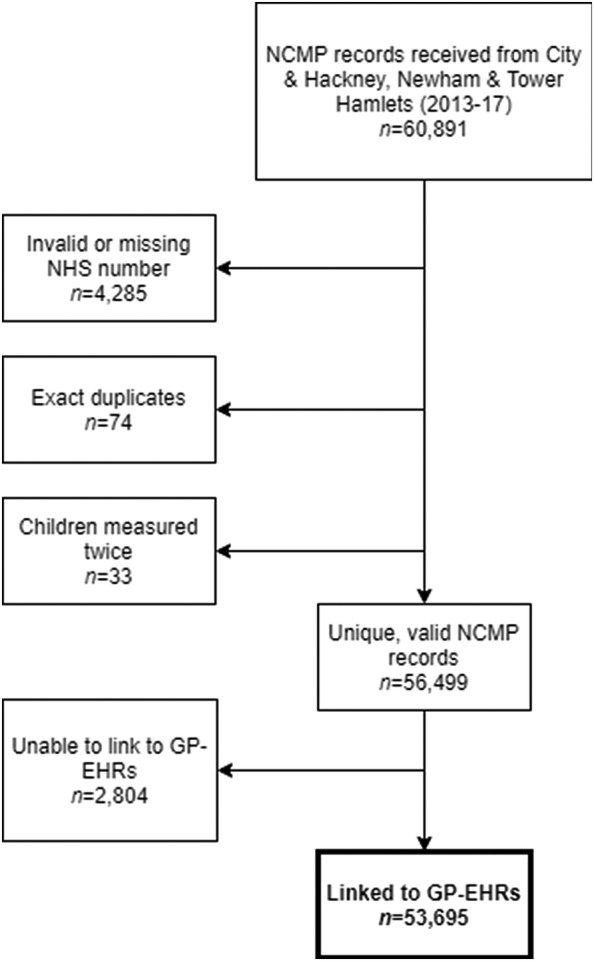
Flow chart to show how study population was derived
There were 53 695 children with linked records, comprising 28 330 5‐year‐olds (13 914 girls; median age [years]; interquartile range [IQR]: 5.07; 4.81,5.33) and 25 365 11‐year‐olds (12 492 girls; 10.93; 10.66,11.21). More than half were from a Black or South Asian ethnic background (20.6% Black, 34.9% South Asian) and almost two thirds (64.7%) were living in the most deprived IMD quintile, reflecting the demographic and socio‐economic characteristics of the population living in the local authorities included (Table 1).
TABLE 1.
Sample characteristics
| Age 5 (n = 28 330) | Age 11 (n = 25 365) | All (N = 53 695) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Local authority a | ||||||
| City and Hackney | 9921 | 35.0 | 8617 | 34.0 | 18 538 | 34.5 |
| Newham | 12 979 | 45.8 | 11 556 | 45.5 | 24 535 | 45.7 |
| Tower Hamlets | 5430 | 19.2 | 5192 | 20.5 | 10 622 | 19.8 |
| School year b | ||||||
| 2013/14 | 2398 | 8.4 | 2001 | 7.9 | 4399 | 8.2 |
| 2014/15 | 6872 | 24.3 | 5864 | 23.1 | 12 736 | 23.7 |
| 2015/16 | 9014 | 31.8 | 8458 | 33.3 | 17 472 | 32.5 |
| 2016/17 | 10 046 | 35.5 | 9042 | 35.7 | 19 088 | 35.6 |
| Sex | ||||||
| Male | 14 416 | 50.9 | 12 873 | 50.8 | 27 289 | 50.8 |
| Female | 13 914 | 49.1 | 12 492 | 49.2 | 26 406 | 49.2 |
| Ethnic background c | ||||||
| White | 6829 | 24.1 | 4866 | 19.2 | 11 695 | 21.8 |
| Mixed and Other | 5166 | 18.2 | 5220 | 20.6 | 10 386 | 19.3 |
| South Asian | 9916 | 35.1 | 8812 | 34.7 | 18 728 | 34.9 |
| Black | 5874 | 20.7 | 5198 | 20.5 | 11 072 | 20.6 |
| Missing | 545 | 1.9 | 1269 | 5.0 | 1814 | 3.4 |
| IMD quintile d | ||||||
| 1 ‐ most deprived | 18 245 | 64.4 | 16 501 | 65.1 | 34 746 | 64.7 |
| 2 | 8950 | 31.6 | 7867 | 31.0 | 16 817 | 31.3 |
| 3 | 828 | 2.9 | 762 | 3.0 | 1590 | 3.0 |
| 4 | 214 | 0.7 | 178 | 0.7 | 392 | 0.7 |
| 5 ‐ least deprived | 49 | 0.2 | 26 | 0.1 | 75 | 0.2 |
| Missing | 44 | 0.2 | 31 | 0.1 | 75 | 0.1 |
| NCMP weight status e | ||||||
| Underweight | 666 | 2.4 | 1013 | 4.0 | 1679 | 3.1 |
| Healthy weight | 22 614 | 79.8 | 15 658 | 61.7 | 38 272 | 71.3 |
| Overweight | 2718 | 9.6 | 4263 | 16.8 | 6981 | 13.0 |
| Obese | 2332 | 8.2 | 4431 | 17.5 | 6763 | 12.6 |
| Long‐term condition f | ||||||
| No | 26 717 | 94.3 | 22 691 | 89.5 | 49 408 | 92.0 |
| Yes | 1613 | 5.7 | 2674 | 10.5 | 4287 | 8.0 |
Note: Asthma was included as a long‐term condition if both GP diagnosis and prescription present.
Local authority which collected the National Child Measurement Programme (NCMP) data.
School year of NCMP measurement: City and Hackney 2013‐17, Newham in 2014‐17, Tower Hamlets 2015‐17.
Ethnic background as recorded in NCMP and supplemented with GP ethnicity for those with missing NCMP ethnic group.
Index of Multiple Deprivation (IMD) quintile based on IMD assigned by Public Health England using child's home address postcode as recorded in NCMP.
Weight status based on NCMP recorded BMI and categorized according to UK1990 clinical reference standard: “underweight” (BMI < 2nd centile), “healthy weight” (≥2nd to < 91st centile), “overweight” (≥91st to < 98th centile) or “obese” (≥98th centile).
Long‐term conditions included GP recorded diagnosis of: cystic fibrosis, type 1 diabetes, attention deficit hyperactivity disorder, autism or learning disability, or GP prescriptions for: epilepsy, attention deficit hyperactivity disorder, or thyroid disease.
The NCMP‐BMI indicated either clinical overweight or obesity in approximately one in five 5‐year‐olds (9.6%, 8.2% respectively) and one in three 11‐year‐olds (16.8%, 17.5%). The distribution of child weight status according to International Obesity Task Force and World Health Organization reference standards are shown in Table S2.
Overall, 16 333 instances of a GP‐BMI record were identified for 9562 children (17.8% of all children), comprising 2964 5‐year‐olds (10.5%) and 6598 11‐year‐olds (26.0%). More than one record was identified for 2.5% of 5‐year‐olds (n = 709) and 9.8% of 11‐year‐olds (n = 2492), with a mean of 1.37 (median; IQR: 1; 1,1) and 1.68 instances per child (1; 1,2), respectively.
Children were more likely to have at least one GP‐BMI recorded if they were: male; from South Asian ethnic backgrounds; living in the most deprived IMD quintile; recorded as having a long‐term condition. Children whose BMI was categorized as underweight or obese in the NCMP were also more likely to have at least one GP‐BMI record (Table 2).
TABLE 2.
Characteristics of children with and without at least one GP‐BMI record, by age group
| Age 5 | Age 11 | |||||||
|---|---|---|---|---|---|---|---|---|
| Never | Ever | Never | Ever | |||||
| n | % (95% CI a ) | n | % (95% CI a ) | n | % (95% CI a ) | n | % (95% CI a ) | |
| Local authority b | ||||||||
| City and Hackney | 8823 |
34.8 (34.2,35.4) |
1098 |
37.0 (35.3,38.8) |
6397 |
34.1 (33.4,34.8) |
2220 |
33.6 (32.5,34.8) |
| Newham | 11 681 |
46.0 (45.4,46.7) |
1298 |
43.8 (42.0,45.6) |
8463 |
45.1 (44.4,45.8) |
3093 |
46.9 (45.7,48.1) |
| Tower Hamlets | 4862 |
19.2 (18.7,19.7) |
568 |
19.2 (17.8,20.6) |
3907 |
20.8 (20.2,21.4) |
1285 |
19.5 (18.5,20.4) |
| Sex | ||||||||
| Male | 12 796 |
50.4 (49.8,51.1) |
1620 |
54.7 (52.9,56.4) |
9370 |
49.9 (49.2,50.6) |
3503 |
53.1 (51.9,54.3) |
| Female | 12 570 |
49.6 (48.9,50.2) |
1344 |
45.3 (43.6,47.1) |
9397 |
50.1 (49.4,50.8) |
3095 |
46.9 (45.7,48.1) |
| Ethnic background c | ||||||||
| White | 6227 |
24.5 (24.0,25.1) |
602 |
20.3 (18.9,21.8) |
3654 |
19.5 (18.9,20.0) |
1212 |
18.4 (17.5,19.3) |
| Mixed and Other | 4677 |
18.4 (18.0,18.9) |
489 |
16.5 (15.2,17.9) |
3954 |
21.1 (20.5,21.7) |
1266 |
19.2 (18.3,20.2) |
| South Asian | 8686 |
34.2 (33.7,34.8) |
1230 |
41.5 (39.7,43.3) |
6230 |
33.2 (32.5,33.9) |
2582 |
39.1 (38.0,40.3) |
| Black | 5279 |
20.8 (20.3,21.3) |
595 |
20.1 (18.7,21.6) |
3911 |
20.8 (20.3,21.4) |
1287 |
19.5 (18.6,20.5) |
| Missing | 497 |
2.0 (1.8,2.1) |
48 |
1.6 (1.2,2.1) |
1018 |
5.4 (5.1,5.8) |
251 |
3.8 (3.4,4.3) |
| IMD quintile d | ||||||||
| 1 ‐ most deprived | 16 161 |
63.7 (63.1,64.3) |
2084 |
70.3 (68.6,71.9) |
12 054 |
64.2 (63.5,64.9) |
4447 |
67.4 (66.3,68.5) |
| 2 | 8151 |
32.1 (31.6,32.7) |
799 |
27.0 (25.4,28.6) |
5906 |
31.5 (30.8,32.1) |
1961 |
29.7 (28.6,30.8) |
| 3 | 768 |
3.0 (2.8,3.2) |
60 |
2.0 (1.6,2.6) |
606 |
3.2 (3.0,3.5) |
156 |
2.4 (2.0,2.8) |
| 4 | 201 |
0.8 (0.7,0.9) |
13 |
0.4 (0.3,0.8) |
156 |
0.8 (0.7,1.0) |
22 |
0.3 (0.2,0.5) |
| 5 ‐ least deprived | 46 |
0.2 (0.1,0.2) |
3 |
0.1 (0.03,0.3) |
19 |
0.1 (0.06,0.2) |
7 |
0.1 (0.05,0.5) |
| Missing | 39 |
0.2 (0.1,0.2) |
5 |
0.2 (0.1,0.4) |
26 |
0.2 (0.09,0.2) |
5 |
0.1 (0.03,0.2) |
| NCMP weight status e | ||||||||
| Underweight | 445 |
1.8 (1.6,1.9) |
92 |
3.1 (2.5,3.8) |
302 |
1.6 (1.4,1.8) |
177 |
2.7 (2.3,3.1) |
| Healthy weight | 20 497 |
80.8 (80.3,81.3) |
2246 |
75.8 (74.2,77.3) |
12 298 |
65.5 (64.8,66.2) |
3894 |
59 (57.8,60.2) |
| Overweight | 2427 |
9.6 (9.2,9.9) |
291 |
9.8 (8.8,10.9) |
3191 |
17 (16.5,17.5) |
1072 |
16.2 (15.4,17.2) |
| Obese | 1997 |
7.9 (7.5,8.2) |
335 |
11.3 (10.2,12.5) |
2976 |
15.9 (15.3,16.4) |
1455 |
22.1 (21.1,23.1) |
| Long‐term condition f | ||||||||
| No | 24 457 |
96.4 (96.2,96.6) |
2260 |
76.2 (74.7,77.7) |
17 940 |
95.6 (95.3,95.9) |
4751 |
72.0 (70.9,73.1) |
| Yes | 909 |
3.6 (3.4,3.8) |
704 |
23.8 (22.3,25.3) |
827 |
4.4 (4.1,4.7) |
1847 |
28.0 (26.9,29.1) |
95% confidence interval.
Local authority which collected the National Child Measurement Programme (NCMP) data.
Ethnic background as recorded in NCMP and supplemented with GP recorded ethnicity for those with missing NCMP ethnic group.
Index of multiple deprivation (IMD) quintile based on the NCMP recorded child's home address postcode.
Weight status based on NCMP recorded BMI categorized according to UK1990 clinical reference standard: “underweight” (BMI < 2nd centile), “healthy weight” (≥2nd to < 91st centile), “overweight” (≥91st to < 98th centile) or “obese” (≥98th centile).
Long‐term conditions included GP recorded diagnosis of: cystic fibrosis, type 1 diabetes, attention deficit hyperactivity disorder, autism or learning disability or GP prescriptions for: epilepsy, attention deficit hyperactivity disorder, or thyroid disease. Asthma was included as a long‐term condition if both GP diagnosis and prescription were present.
Findings were consistent after adjustment for covariates, with the exception of the association with child's sex which attenuated after adjustment. Five‐year‐olds with at least one GP‐BMI record were more likely to: have NCMP‐derived underweight (aOR; 95% CI: 1.71; 1.34,2.19) or obese weight status (1.45; 1.27,1.65); be from South Asian backgrounds (1.55; 1.38,1.74); have a long‐term condition (8.15; 7.31,9.10); and living in the most deprived areas (Wald statistic; P‐value: 38.73; P < 0.0001) (Table S3 for univariable and adjusted odds [and 95% CI] and Figure 2a). Findings among 11‐year‐olds were similar (Table S3 and Figure 2b).
FIGURE 2.
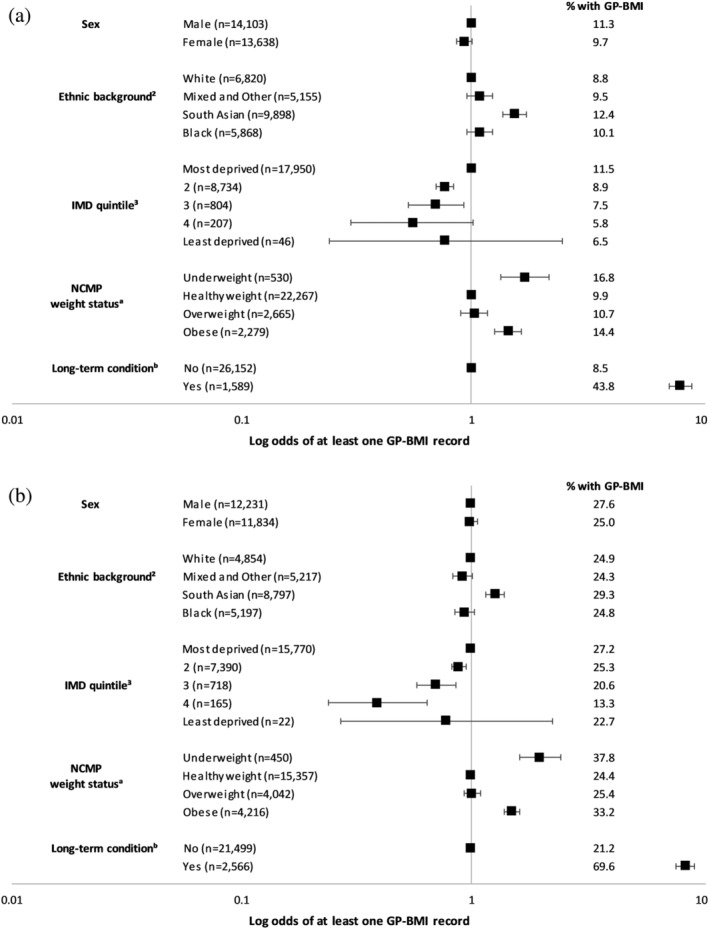
a, Adjusted odds1 of ever having a GP‐BMI record, age 5. 1It illustrates the adjusted odds of at least one GP‐BMI record after mutual adjustment for sex, ethnic background, National Child Measurement Programme (NCMP)‐derived weight status, presence of a long‐term condition, Index of Multiple Deprivation (IMD) quintile, and school local authority (n = 27 741). 2Ethnic background as recorded in the NCMP and supplemented with GP ethnicity for those with missing NCMP ethnic group. 3IMD quintile based on NCMP child's home address postcode. aWeight status based on NCMP recorded BMI and categorized according to UK1990 clinical reference standard: “underweight” (BMI < 2nd centile), “healthy weight” (≥2nd to <91st centile), “overweight” (≥91st to <98th centile) or “obese” (≥98th centile). bLong‐term conditions included GP recorded diagnosis of: cystic fibrosis, type 1 diabetes, attention deficit hyperactivity disorder, autism or learning disability or GP prescriptions for: epilepsy, attention deficit hyperactivity disorder, or thyroid disease. Asthma was included as a long‐term condition if both GP diagnosis and prescription were present. b, Adjusted odds1 of ever having a GP‐BMI record, age 11. 1It illustrates the adjusted odds of at least one GP‐BMI record after mutual adjustment for sex, ethnic background, National Child Measurement Programme‐derived weight status, presence of a long‐term condition, Index of Multiple Deprivation quintile, and school local authority (n = 24 065). 2Ethnic background as recorded in the NCMP and supplemented with GP ethnicity for those with missing NCMP ethnic group. 3IMD quintile based on NCMP child's home address postcode. aWeight status based on NCMP recorded BMI and categorized according to UK1990 clinical reference standard: “underweight” (BMI < 2nd centile), “healthy weight” (≥2nd to <91st centile), “overweight” (≥91st to <98th centile) or “obese” (≥98th centile). bLong‐term conditions included GP recorded diagnosis of: cystic fibrosis, type 1 diabetes, attention deficit hyperactivity disorder, autism or learning disability or GP prescriptions for: epilepsy, attention deficit hyperactivity disorder, or thyroid disease. Asthma was included as a long‐term condition if both GP diagnosis and prescription were present
We identified 15 087 occasions (92.4%) when GP‐BMI was derived from height and weight values recorded on the same date as GP‐BMI (Figure S1). On a further 792 (4.8%) occasions, GP‐BMI was derived from earlier height (n = 645) or weight (n = 79) measurements, or both (n = 68) using height and weight measurements recorded, respectively, a median of 9.25 months (IQR: 3.60,18.28) and 9.92 months (1.82,18.25) prior to GP‐BMI. In the majority of these instances (n = 735, 92.8%) height and weight were recorded on different dates, as well as on a different date to recorded BMI: the median time between height and weight measurement was 9.49 months (3.70,18.74). On 454 occasions (2.8%), we could not identify the height and weight values used to derive the GP‐BMI.
We identified GP‐BMI with dates of measurements within 1 month of the NCMP‐BMI date of measurement for 5.4% (160/2964) and 4.0% (263/6598) of 5 and 11‐year‐olds, respectively. GP‐BMI was on average slightly lower than NCMP‐BMI with wide limits of agreement: mean difference (95% limits of agreement): +0.45 (−1.60,2.51) and + 0.16 (−2.86,3.18) in five and 11‐year‐olds, respectively (Figure 3a,b). Our findings suggest these are meaningful differences, relative to the differences expected in measures made 1 month apart (expected 1 month change in BMI for children following the 50th centile is approximately ±0.009 kg/m2 among 5‐year‐olds and ± 0.043 and ± 0.051 among 11‐year‐old boys and girls, respectively). Among these children, weight status derived from GP‐BMI differed to that derived from NCMP‐BMI for 23 (23/160 = 14.4%) 5‐year‐olds. Based on GP‐BMI, six children's BMI would have been assigned to a weight status one category higher, 16 to a weight status one category lower, and one child's BMI two categories higher (from obese to healthy weight status), compared to that assigned in the NCMP. Among 11‐year‐olds, weight status derived from GP‐BMI differed to that derived from NCMP‐BMI for 35 children (35/263 = 13.3%): 12 children's BMI would have been assigned to a weight status one category higher, one two categories higher (from healthy to obese weight status), 21 one category lower, and one two categories lower (from obese to healthy weight status), compared with that assigned in the NCMP.
FIGURE 3.
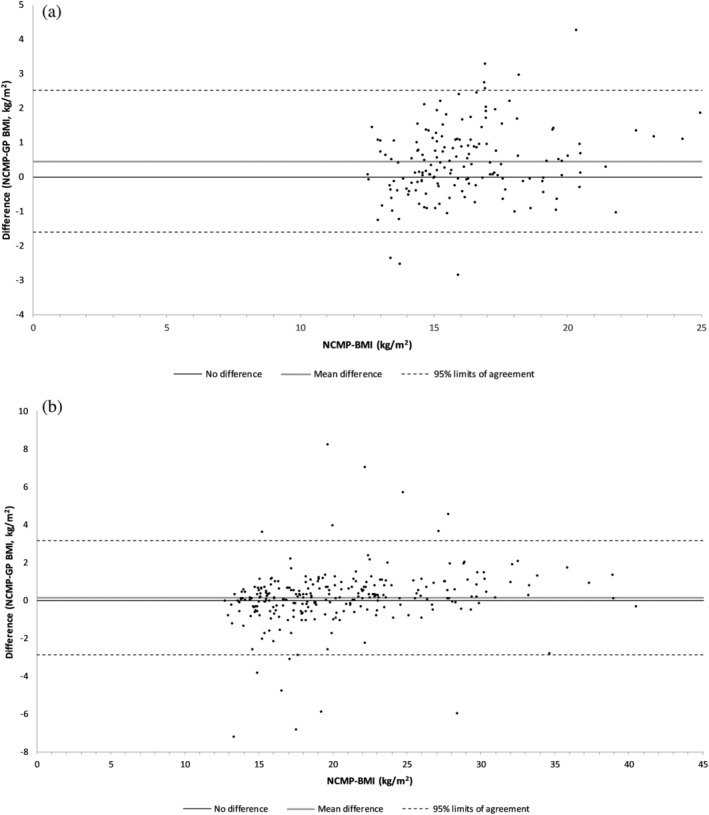
a, Difference between NCMP and GP recorded BMI by NCMP‐BMI, age 5. This figure illustrates the difference between National Child Measurement Programme (NCMP)‐ and GP‐BMI values recorded within 1 month of each other (n = 159) against the NCMP‐BMI value. Mean difference (95% Limits of Agreement): 0.45 (−1.60,2.51). b, Difference between NCMP and GP recorded BMI by NCMP‐BMI, age 11. This figure illustrates the difference between National Child Measurement Programme (NCMP)‐ and GP‐BMI values recorded within 1 month of each other (n = 263) against the NCMP‐BMI value. Mean difference (95% Limits of Agreement): 0.16 (−2.86,3.18)
We identified 1175 and 2091 unique GP‐BMI records between 2013 and 2017 in 5‐ and 11‐year‐olds, respectively. The population prevalence of underweight and obesity estimated from GP‐EHRs was higher, and of healthy weight and overweight lower, in 5‐year‐olds (median age [years]; IQR: 5.03; 4.65,5.40), relative to that estimated from the NCMP (Table S4 and Figure 4). Among 11‐year‐olds (10.92; 10.48,11.34), the prevalence of underweight and obesity derived from GP‐EHRs was higher, and healthy weight lower, relative to that estimated from the NCMP.
FIGURE 4.
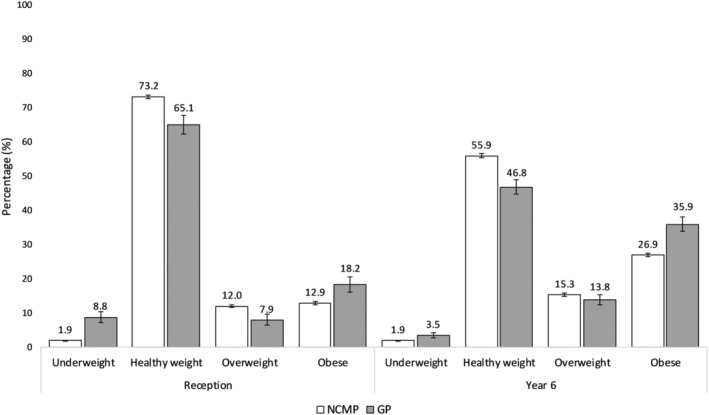
Prevalence (and 95% confidence intervals) of specified weight status1 by data source. 1Weight status based on BMI and categorized according to UK1990 population reference standard: “underweight” (BMI < 2nd centile), “healthy weight” (≥2nd to <85th centile), “overweight” (≥85th to <95th centile) or “obese” (≥95th centile)
4. DISCUSSION
4.1. Key findings
We have found that relatively few children have a BMI record in the GP‐EHR and that this is largely determined by a child's weight and health status and social and demographic factors. Whilst overall the quality of BMI records in the GP‐EHR was good, there was wide within‐child variation between BMI values recorded by the GP and those recorded in the NCMP. Despite this, only a small proportion of these children would have been assigned to a different weight status category on the basis of their GP record to that assigned in the NCMP. At the population level, estimates of underweight and obesity based on GP‐EHRs were significantly higher than those reported in the NCMP, reflecting the fact that children with obesity or underweight were more likely to have their height and weight measured in general practice. This is, to our knowledge, the first time that the completeness, representativeness and accuracy of BMI records in GP‐EHRs have been evaluated and our findings add significant new information about the quality and extent of information about child weight status available to the clinical care team, as well as the potential value of these records as data resources for public health and research purposes.
4.2. Strengths and limitations
We assessed the quality of GP‐BMI records by linking NCMP records to GP‐EHRs at the child level. A high proportion of NCMP records were linked, indicating that the majority of children attending schools in one of the three local authorities were registered with GP practices in the same localities. Whilst ethnic background was missing in a small proportion of NCMP records, we were able to establish ethnic background for a high proportion of these from the GP‐EHR, allowing demographic factors to be evaluated.
We used validated NCMP data returned to the local authorities by PHE and were able to compare this to anthropometry data extracted from the GP‐EHR for children registered with all GPs in City and Hackney, Newham and Tower Hamlets enabling direct comparison between these two data sources in a geographically contiguous population. NCMP data were collected using standardized protocols from all state schools in three local authorities with high participation rates. Whilst data entry and calculation of BMI in the GP‐EHR were standardized, it is possible that scales and stadiometers in general practice are less regularly calibrated and that staff obtaining measurements in general practice do not follow a standardized protocol, including in relation to requirements to remove clothing and shoes when being measured. We only included structured data recorded using defined codes in the GP‐EHR and did not consider codes indicating obesity diagnosis, monitoring or referral, or BMI/weight centile categorisation. Free text was unavailable for analysis.
In assigning weight status from GP‐BMI records using age‐ and sex‐specific BMI centiles, we derived age at measurement from an approximate date of birth and the date GP‐BMI was recorded in the GP‐EHR. Where GP‐BMI was derived from earlier height and/or weight measurements, age on the date GP‐BMI was recorded was used to categorize GP‐BMI. Whilst this was the case for only 4.8% of GP‐BMI records, the calculation of GP‐BMI based on asynchronous measurements is a considerable limitation of GP‐BMI, particularly given that children may be growing rapidly, particularly girls aged 10‐11 years.
Our evaluation applies to two specific age‐groups of children, and only children attending state schools are included in the NCMP, excluding those attending private or faith schools. In City and Hackney, approximately one quarter of school‐aged children attend private or faith schools, compared with equivalent figures of 1.4% and 5.0% for Newham and Tower Hamlets, respectively. 16 We did not have any information about the small proportion of children who opted out of the NCMP in the 2013‐17 school years, however data reporting NCMP non‐measurement in 2017/18 showed that just 2.0% of eligible children opted out or were opted out by their parents. 17
4.3. Comparison with existing literature
We identified an average of 1.4 and 1.8 GP BMI records per child among 5‐ and 11‐year‐olds, respectively, which is consistent with the average of 1.4 BMI observations per child reported by van Jaarsveld based on a national sample of GP records in the UK CPRD for children aged between 2 and 15 years between 1994 and 2013. 5 The authors reported finding a similar prevalence of overweight and obesity in CPRD across a wider age range to that reported by the NCMP, but did not test for potential biases in BMI measurement and recording or adjust for deprivation or ethnic background. Motivation for GP‐BMI recording may differ in disadvantaged areas of England more generally, and whilst we are not able to determine the motivation for recording from routine data recorded in the GP‐EHR, others have reported higher rates of GP consultations among 5‐year‐olds with a BMI considered underweight or obese, 18 and that consultation rates are higher following NCMP measurements for children whose parents would have received a letter reporting their child's BMI was considered underweight or obese. 19
Whilst the National Institute for Health and Care Excellence (NICE) recommends that GPs refer adults with obesity to weight management services and UK general practices are incentivized financially to maintain a register of patients aged over 16 years whose BMI is greater than or equal to 30 kg/m2, 20 similar frameworks for children do not exist. Recording of children's heights, weights and BMI is not routine in general practice, in contrast to well‐child programmes in other countries. 21
Our findings suggest that BMI recording in UK general practice is confounded by clinical indication, as evidenced by the strong association between long‐term health conditions, weight status and the likelihood of BMI measurement in general practice. This finding is in contrast to research findings from the United States, where EHR‐estimated prevalence of overweight and obesity were shown to be similar to estimates generated from population surveys. 22 , 23 Relative to east London, a higher proportion of Canadian school aged children had at least one record of height and weight measurements in primary care EHRs. 24 , 25 These differences reflect between‐country differences in scheduled well‐child visits in primary care which are mandated annually in the United States and Canada but not in the UK.
A systematic review of 17 American and Canadian studies which identified patients with obesity using EHR obesity diagnosis codes found that obesity was usually recorded correctly; however, obesity was underreported in EHRs when compared to a reference standard. 26 Whilst we also found that the majority of children with a BMI considered obese in the NCMP would also be categorized as obese based on their GP‐BMI, the use of obesity diagnosis codes, as opposed to BMI records, to identify patients with obesity is likely to explain our contrasting findings relating to the under and overreporting of obesity based on EHRs.
We found children living in more deprived areas were more likely to ever have a GP‐BMI record, in contrast to findings from a study in Spain where the prevalence of child height and weight records in GP‐EHRs increased with average annual household income. 27
In contrast to earlier studies, 5 , 28 we were able to evaluate associations of BMI recording with ethnic background and found that children from South Asian ethnic backgrounds were more likely to have had a BMI recorded in general practice compared to those from White ethnic backgrounds. Other studies have shown that adults from South Asian ethnic backgrounds have more frequent BMI measurements 29 reflecting recognition of their higher risk of developing type 2 diabetes and cardiovascular disease which are strongly associated with obesity and which begin to develop from childhood. 30 , 31 , 32 , 33 Hence there may be greater community awareness of these risks and parents and GPs may have a lower threshold for measuring height and weight in children from South Asian ethnic backgrounds.
Whilst evidence suggesting that BMI under‐ and overestimates body fat in children from South Asian and Black ethnic backgrounds, respectively, has led to the development of ethnic‐specific adjustments, 34 these are not currently used in either the NCMP or GP‐EHRs. We have previously reported that ethnic‐specific BMI adjustments applied to NCMP data in east London resulted in a significant increase in the prevalence of clinical obesity in areas with a high proportion of children from South Asian ethnic backgrounds, 35 highlighting the importance of ethnic‐adjustment when estimating population prevalence of obesity in ethnically diverse populations.
A previous study of 4‐43‐month‐old children participating in the Avon Longitudinal Study of Parents and Children reported good agreement between the research weight measurements and those made routinely by health visitors. 36 We have not identified other studies which compare BMI values obtained from GP‐EHRs and the NCMP. Although differences in BMI greater than 3 kg/m2 are of sufficient magnitude to result in a difference in weight status, overall relatively few children's BMI would have been categorized into a different weight status to that reported in the NCMP based on UK1990 clinical thresholds. It is worth emphasising, however, that GPs do not have access within EMIS to methods for calculating and hence interpreting weight status using such standards.
4.4. Implications
The Royal College of Paediatrics and Child Health recommends that: “digital capacity in primary care and across child health professionals should be strengthened with the necessary IT systems so that information on a child's weight is accessible to all child health professionals who need it”. 37 Our study has highlighted the limited information about childhood BMI available to GPs. Our findings underscore the potential for linking and making accessible to GPs and parents all child weight and height measurements made in community, hospital, school and primary care settings. Whilst evidence‐based interventions to support weight management for children with obesity and overweight are currently lacking, 4 there is emerging evidence to suggest that, among adults, recording of BMI in GP‐EHRs improves weight management 38 , 39 and is linked to increased guidance about healthier lifestyle choices. 40 , 41 , 42 , 43
In east London, GP‐EHRs do not provide a complete or representative source of data from which to estimate the prevalence of childhood obesity and its associated health outcomes. Linkage to the NCMP enables unbiased estimates of both prevalence of childhood obesity and associated health outcomes. In other countries, where routine measurements of children are made on a regular basis as part of well‐child programmes, primary care EHRs may provide a less biased assessment of obesity prevalence, overcoming some of the limitations of using data based on consultations in primary care.
5. CONCLUSION
In conclusion, we have quantified the completeness and accuracy of BMI records in GP‐EHRs and highlighted significant recording‐biases which preclude their use for estimating the prevalence of childhood obesity at a population level. We have shown that linkage of GP‐EHRs to NCMP records is feasible suggesting that linkage of these two data sources can be used to assess the health outcomes of childhood obesity. Linking all data on children's weight and height is needed to support better recognition of unhealthy childhood weight in clinical practice and enable the consequences of unhealthy childhood weight to be better understood.
CONFLICT OF INTEREST
All authors declare no conflicts of interest.
AUTHORS' CONTRIBUTION
CD obtained funding for the study. NF and CD conceptualized, designed and interpreted the analyses. NF carried out the literature search, conducted the analyses, generated tables and figures and drafted the initial manuscript. All authors contributed to the interpretation of analyses and reviewed and revised the manuscript. All authors were involved in writing the paper and had final approval of the submitted and published manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Supporting information
Appendix S1: Supporting Information
ACKNOWLEDGEMENTS
This research was funded by a grant from Barts Charity ref: MGU0419. This work was supported by Health Data Research UK (award reference: LOND1), which is funded by the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation and Wellcome.
Firman N, Robson J, Ahmed Z, Boomla K, Dezateux C. Completeness and representativeness of body mass index in children's electronic general practice records: Linked cross‐sectional study in an ethnically‐diverse urban population in the United Kingdom. Pediatric Obesity. 2021;16:e12772. 10.1111/ijpo.12772
Funding information Barts Charity, Grant/Award Number: MGU0419; Health Data Research UK, Grant/Award Number: LOND1; Wellcome; British Heart Foundation; Public Health Agency (Northern Ireland); and Social Care Research and Development Division (Welsh Government); Chief Scientist Office of the Scottish Government Health and Social Care Directorates; Department of Health and Social Care (England); Economic and Social Research Council; Engineering and Physical Sciences Research Council; UK Medical Research Council
DATA AVAILABILITY STATEMENT
This work uses data provided by patients and collected by the NHS as part of their care and support. We are grateful to public health colleagues in the London Boroughs of City and Hackney, Newham and Tower Hamlets for access to pseudonymized NCMP data and to general practitioners and colleagues within the Clinical Effectiveness Group for access to general practice data. NCMP data were accessed under data processing agreements with each of the local authorities as data controllers in line with Public Health England guidance. These agreements preclude onward sharing of data. Access to general practice data were accessed by data sharing agreements between the Clinical Effectiveness Group and the general practice data controllers and also precludes onward sharing of data. Data can be obtained by application to respective data controllers.
REFERENCES
- 1. World Health Organisation . Childhood overweight and obesity. https://www.who.int/dietphysicalactivity/childhood/en/. Published 2019. Accessed August 2020.
- 2. NHS Digital . National Child Measurement Programme, England 2018/19 School Year. https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement-programme/2018-19-school-year. Published 2019. Accessed August 2020.
- 3. Wright CM. Are we overdiagnosing obesity in preschool children? Arch Dis Child. 2020. 10.1136/archdischild-2020-318857. [DOI] [PubMed] [Google Scholar]
- 4. Brown T, Moore THM, Hooper L, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019. 10.1002/14651858.cd001871.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Jaarsveld CH, Gulliford MC. Childhood obesity trends from primary care electronic health records in England between 1994 and 2013: population‐based cohort study. Arch Dis Child. 2015;100(3):214‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Public Health England . National Child Measurement Programme: Operational guidance 2020. Public Health England. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/931776/NationaChild_Measurement_Programme_operational_guidance_2020.pdf. Published 2020. Accessed November 2020.
- 7. OpenPseudonymiser [computer program] . University of Nottingham: Hippisley‐Cox, J.; 2011.
- 8. Lifestyles Statistics, NHS Digital . Validation of National Child Measurement Programme data. Health and Social Care Information Centre; 2020.
- 9. Scientific Advisory Committee on Nutrition, Royal College of Paediatrics and Child Health . Consideration of issues around the use of BMI centile thresholds for defining underweight, overweight and obesity in children aged 2‐8 years in the UK. 2012.
- 10. LMSgrowth Microsoft Excel add‐in to access references based on the LMS method [computer program] . Version 2.77 Pan, H. Cole, T. J.; 2012.
- 11. Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child. 1995;73(1):25‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. NHS . Ethnic category code. https://www.datadictionary.nhs.uk/data_dictionary/attributes/e/end/ethnic_category_code_de.asp. Published 2018. Accessed March 2018.
- 13. Department for Communities and Local Government . The English Indices of Deprivation 2015 ‐ Frequently Asked Questions (FAQs). 2016.
- 14. Bland JM, Altman DG. Statistical methods for assessing agreement between 2 methods of clinical measurement. The Lancet. 1986;327(8476):307‐310. [PubMed] [Google Scholar]
- 15. NHS, Health Research Authority . HRA Approval. https://www.hra.nhs.uk/approvals-amendments/what-approvals-do-i-need/hra-approval/. Published 2020. Accessed August 2020.
- 16. Department for Education . Schools and Pupils by Type of School, Borough. https://data.london.gov.uk/dataset/schools-and-pupils-type-school-borough. Published 2020. Accessed August 2020.
- 17. NHS Digital . Non Measurement Reasons for the National Child Measurement Programme by Local Authority 2017/18. NHS Digital. https://digital.nhs.uk/data‐and‐information/find‐data‐and‐publications/supplementary‐information/2018‐supplementary‐information‐files/non‐measurement‐reasons‐for‐the‐national‐child‐measurement‐programme‐by‐local‐authority‐2017‐18. Published 2018. Accessed November 2020.
- 18. Kelly B, West J, Yang TC, Mason D, Hasan T, Wright J. The association between body mass index, primary healthcare use and morbidity in early childhood: findings from the Born In Bradford cohort study. Public Health. 2019;167:21‐27. [DOI] [PubMed] [Google Scholar]
- 19. Dezateux C, Foster N, Ahmed Z, et al. General practice consultations with obese children–a missed opportunity? Cross‐sectional study using linked national child measurement and primary care data. The Lancet. 2017;390:S37. 10.1016/s0140-6736(17)32972-0. [DOI] [Google Scholar]
- 20. British Medical Association , NHS England. Update to the GP Contract Agreement 2020/21 ‐ 2023/24. 2020.
- 21. American Academy of Pediatrics . AAP schedule of Well‐Child care visits. https://www.healthychildren.org/English/family‐life/health‐management/Pages/Well‐Child‐Care‐A‐Check‐Up‐for‐Success.aspx. Published 2020. Accessed November 2020.
- 22. Bailey LC, Milov DE, Kelleher K, et al. Multi‐institutional sharing of electronic health record data to assess childhood obesity. PloS One. 2013;8(6):e66192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gutilla MJ, Davidson AJ, Daley MF, Anderson GB, Marshall JA, Magzamen S. Data for community health assessment in rural Colorado: a comparison of electronic health records to public health surveys to describe childhood obesity. J Public Health Manag Pract. 2017;23:S53‐S62. [DOI] [PubMed] [Google Scholar]
- 24. Carsley S, Birken CS, Parkin P, Pullenayegum E, Tu K. Completeness and accuracy of anthropometric measurements in electronic medical records for children attending primary care. J Innov Health Inform. 2018;25(1):963. [DOI] [PubMed] [Google Scholar]
- 25. Birken CS, Tu K, Oud W, et al. Determining rates of overweight and obese status in children using electronic medical records. Can Fam Physician. 2017;63:e114‐e122. [PMC free article] [PubMed] [Google Scholar]
- 26. Samadoulougou S, Idzerda L, Dault R, Lebel A, Cloutier A‐M, Vanasse A. Validated methods for identifying individuals with obesity in health care administrative databases: A systematic review. Obes Sci Pract. 2020;6(6):677–693. 10.1002/osp4.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sayon‐Orea C, Moreno‐Iribas C, Delfrade J, et al. Inverse‐probability weighting and multiple imputation for evaluating selection bias in the estimation of childhood obesity prevalence using data from electronic health records. BMC Med Inform Decis Mak. 2020;20(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Booth HP, Prevost AT, Gulliford MC. Epidemiology of clinical body mass index recording in an obese population in primary care: a cohort study. J Public Health (Oxf). 2013;35(1):67‐74. [DOI] [PubMed] [Google Scholar]
- 29. Dalton ARH, Bottle A, Okoro C, Majeed A, Millett C. Implementation of the NHS Health Checks programme: baseline assessment of risk factor recording in an urban culturally diverse setting. Fam Pract. 2010;28(1):34‐40. [DOI] [PubMed] [Google Scholar]
- 30. Nightingale CM, Rudnicka AR, Owen CG, et al. Influence of adiposity on insulin resistance and Glycemia markers among United Kingdom children of South Asian, Black African‐Caribbean, and White European origin: child heart and health study in England. Diabetes Care. 2013;36(6):1712‐1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Candler TP, Mahmoud O, Lynn RM, Majbar AA, Barrett TG, Shield JPH. Continuing rise of Type 2 diabetes incidence in children and young people in the UK. Diabet Med. 2018;35(6):737‐744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Whincup PH, Gilg JA, Papacosta O, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. Br Med J. 2002;324(7338):635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Whincup PH, Nightingale CM, Owen CG, et al. Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the child heart and health study in England (CHASE study). PLoS Med. 2010;7(4):e1000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hudda MT, Nightingale CM, Donin AS, et al. Body mass index adjustments to increase the validity of body fatness assessment in UK Black African and South Asian children. Int J Obes (Lond). 2017;41(7):1048‐1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Firman N, Boomla K, Hudda MT, Robson J, Whincup P, Dezateux C. Is child weight status correctly reported to parents? Cross‐sectional analysis of National Child Measurement Programme data using ethnic‐specific BMI adjustments. J Public Health. 2020;42(4):e541‐e550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Howe LD, Tilling K, Lawlor DA. Accuracy of height and weight data from child health records. Arch Dis Child. 2009;94(12):950‐954. [DOI] [PubMed] [Google Scholar]
- 37. Royal College of Paediatrics and Child Health . RCPCH prevention vision for child health. 2019.
- 38. Otero P, Duran P, Setton D, Eymann A, Busaniche J, Llera J. Mismatch between the prevalence of overweight and obese children and adolescents and recording in electronic health records: a cross‐sectional study. Inform Prim Care. 2011;19:75‐82. [DOI] [PubMed] [Google Scholar]
- 39. Rattay KT, Ramakrishnan M, Atkinson A, Gilson M, Drayton V. Use of an electronic medical record system to support primary care recommendations to prevent, identify, and manage childhood obesity. Pediatrics. 2009;123(Suppl 2):S100‐S107. [DOI] [PubMed] [Google Scholar]
- 40. Cook S, Weitzman M, Auinger P, Barlow SE. Screening and counseling associated with obesity diagnosis in a national survey of ambulatory pediatric visits. Pediatrics. 2005;116(1):112‐116. [DOI] [PubMed] [Google Scholar]
- 41. Wald ER, Ewing L, Cluss P, Goldstrohm S, Cipriani L, Colborn K. Establishing a family‐based intervention for overweight children in pediatric practice. Ann Fam Med. 2005;3(Suppl 2):S45‐S47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician's office. Curr Opin Pediatr. 2007;19(3):354‐361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Barlow SE, Bobra SR, Elliott MB, Brownson RC, Haire‐Joshu D. Recognition of childhood overweight during health supervision visits: does BMI help pediatricians? Obesity. 2007;15(1):225‐232. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information
Data Availability Statement
This work uses data provided by patients and collected by the NHS as part of their care and support. We are grateful to public health colleagues in the London Boroughs of City and Hackney, Newham and Tower Hamlets for access to pseudonymized NCMP data and to general practitioners and colleagues within the Clinical Effectiveness Group for access to general practice data. NCMP data were accessed under data processing agreements with each of the local authorities as data controllers in line with Public Health England guidance. These agreements preclude onward sharing of data. Access to general practice data were accessed by data sharing agreements between the Clinical Effectiveness Group and the general practice data controllers and also precludes onward sharing of data. Data can be obtained by application to respective data controllers.


