Abstract
Objective
Many women choose to have breast reconstruction after mastectomy; however, decision‐making can be difficult and expectations are often unmet. The PEGASUS intervention (Patient Expectations and Goals: Assisting Shared Understanding of Surgery) was developed to support shared decision‐making by helping women and healthcare professionals to clarify and discuss their individual expectations around surgery. This study aimed to explore patients’ and health professionals’ experiences of using the intervention and its implementation.
Methods
Forty interviews were conducted with participants in a large scale, multi‐site trial of the effectiveness of PEGASUS, from ‘intervention’ (n=16) and ‘usual care’ groups (n=11), and healthcare professionals (n=13). Data were analysed using thematic analysis.
Results
‘Usual care’ participants described feeling overwhelmed in decision‐making (‘bombarded’), often using their own research to break down information (‘process of elimination’). In contrast, intervention group participants described PEGASUS providing focus (‘focus amongst the frenetic’), and increased connection with clinicians (‘more than a number’). Healthcare professionals described increased focus on patient priorities (‘shifting focus’), but stressed the need for whole team buy‐in (‘collective commitment’).
Conclusions
The PEGASUS intervention offered a qualitatively different experience to individuals considering breast reconstruction, with potential to enhance patients’ and healthcare professionals’ feelings of shared decision‐making and patient‐centred care.
Trial registration: ISRCTN 18000391 (https://doi.org/10.1186/ISRCTN18000391) 27/01/2016.
Keywords: breast cancer, breast reconstruction, mastectomy, patient‐centred care, qualitative research, shared decision‐making
1. INTRODUCTION
Every year in the UK, approximately 50,000 women are diagnosed with breast cancer, making it the most common cancer in the UK and accounting for around 15% of new cancer diagnoses (Cancer Research UK. (n.d.), 2019). In England, figures suggest that approximately 13,000 women undergo a mastectomy each year and over 5,000 choose to have reconstructive breast surgery (Jeevan et al., 2014). However, decision‐making regarding breast reconstruction (BR) can be difficult and involve several options regarding the type and timing of surgery. These preference‐sensitive, highly personal decisions involve consideration of medical or physical factors and are often being made at a time of heightened emotional distress (Harcourt & Rumsey, 2004). Information regarding BR options can be complex, and although many women report being satisfied with their decision, research also suggests that almost half experience some regret (Sheehan et al., 2007). This dissatisfaction may be related to unclear expectations (Denford et al., 2011; Snell et al., 2015) and patients’ and healthcare professionals’ different perceptions of the most salient facts and goals (Lee et al., 2010). These findings highlight the need for further support for women making decisions regarding BR and the need for increased focus on both shared decision‐making and patient‐centred care.
In efforts to address the difficulties outlined above, several interventions have been developed to support patient decision‐making relating to BR. A recent systematic review identified seven distinct interventions ((Paraskeva et al., 2018a), including four interactive computer‐based interventions, two booklets, a group education intervention and a printed decision aid, but suggested that the impact of these interventions was mixed. The interventions demonstrated some changes in decisional conflict, decisional regret, patient satisfaction, involvement and treatment choice observed across multiple interventions, and a further systematic review and meta‐analysis by Berlin et al., (2019) suggest that decision aids can improve self‐reported satisfaction with information, reduce decisional conflict and increase patients perceived involvement in the decision‐making process. Both reviews stress the need for further rigorous evaluation of these existing interventions, as well as the development and evaluation of further interventions to support patients when making decisions specifically regarding BR.
In response to this need for further support for women offered BR, and a paucity of rigorously developed and evaluated interventions to facilitate pre‐surgical shared decision‐making, the PEGASUS intervention (Patient Expectations and Goals: Assisting Shared Understanding of Surgery) was developed. This intervention is based on the premise that the facilitation of realistic expectations regarding BR would lead to improvements in patient satisfaction and well‐being (Clarke et al., 2020). PEGASUS is designed to elicit women's individual expectations around surgery, set patient‐centred goals for surgery, and aid discussion of these expectations and goals with the surgical team. The intervention is delivered by a trained decision facilitator (a specialist nurse or psychologist, referred to as the PEGASUS coach) and is recorded on a ‘PEGASUS sheet’, which is then used to facilitate further discussion during the surgical consultation.
Acceptability testing suggested the PEGASUS intervention was acceptable to patients and healthcare professionals; with reports that it helped patients to prepare for the surgical consultation, clarify their expectations and increase their belief that the surgeon was aware of their goals. In addition, healthcare professionals reported that it helped to focus the consultation on the individual patient's needs and expectations, as well as raising their awareness of previously unknown patient expectations (Harcourt et al., 2016). Further to these findings, it was felt necessary to conduct a trial to establish the impact of PEGASUS on patient‐reported outcomes, whether the intervention offered patient benefits over usual care, the economic costs of delivering PEGASUS, and experiences of using the PEGASUS intervention (Harcourt et al., 2017). This latter element has been shown to be particularly important in the evaluation of decision aids in breast reconstruction (Sherman et al., 2017) in order to record user's experiences of using the intervention, as well as patient‐reported outcomes measures. Therefore, this trial also included interviews exploring patients’ and healthcare professionals’ experiences of using the intervention, in order to capture a more in‐depth account of users’ experiences and explore any potential benefits that PEGASUS could offer over usual care. This qualitative study aimed to explore patients’ and health professionals’ experiences of usual care, as well as experiences of using the PEGASUS intervention, and their views on its implementation within BR services.
2. METHODS
2.1. Design
This study is part of a larger project, which utilised a mixed‐methods, multi‐centred, non‐randomised between‐subjects, before‐and‐after design comparing usual care (control) with the intervention (PEGASUS). This paper focuses on a qualitative exploration of patients’ and health professionals’ experiences of using the PEGASUS intervention and its implementation within BR services, with the quantitative outcomes detailed in the study protocol (Harcourt et al., 2017) and reported elsewhere. This study received a favourable ethical opinion from the NRES Committee South Central—Berkshire B (reference 15/SC/0331) and the University of the West of England, Bristol. All participants provided written informed consent to take part in this research.
2.2. Participants
Semi‐structured qualitative interviews explored the experiences of three groups: (1) women recruited into the PEGASUS trial, considering BR, and receiving ‘usual care’ from their clinicians; (2) women recruited into the PEGASUS trial, considering BR and receiving the ‘PEGASUS intervention’ from their clinicians; and (3) healthcare professionals delivering the PEGASUS intervention as part of the trial. Participants were given the choice of taking part via face‐to‐face or telephone interviews, which were all conducted by the first author: an experienced qualitative researcher who has supported close family members with breast cancer, but who has no personal experience of decision‐making regarding breast cancer or BR.
Participants were eligible to take part in the PEGASUS trial, and this qualitative arm of the trial, if they were: female, aged 18 years+ and had been offered the option of immediate or delayed BR of any type, following a diagnosis of breast cancer, ductal carcinoma in situ (DCIS) or a risk‐reducing mastectomy at one of the five NHS recruitment sites. Women who were unsuitable for BR or unable to participate in an intervention and study conducted in English were not eligible.
In total, 40 semi‐structured qualitative interviews were conducted, with 27 trial participants (16 from the ‘usual care’ group; 11 from the ‘intervention group’) and 13 healthcare professionals involved in intervention delivery.
2.3. Procedure
At each of the five NHS sites participating in the trial, eligible participants were identified by clinic staff, before being given a study information sheet, a consent form and the opportunity to ask questions about the study before deciding whether to take part. All participants were asked to complete a self‐report questionnaire at baseline (i.e. pre‐intervention for those in the PEGASUS condition, equivalent timing for those in the control condition), immediately post‐intervention and 3, 6 and 12 months after surgery.
After completing the final 12‐month questionnaire, all patient participants were invited to take part in an interview to explore their experiences of decision‐making around BR. In addition, after baseline recruitment into the intervention arm of the trial was complete, all healthcare professionals who delivered the PEGASUS intervention and were still working at the trial sites were invited to take part in an interview regarding their experiences.
DH, NP and PT developed a separate interview guide for each group in line with the aims of the current study, which was used flexibly depending on relevance to the individual's circumstances (see Figure 1 and Figure 2). All interviews were conducted and audio recorded by PT, before an independent transcriptionist transcribed them verbatim.
FIGURE 1.
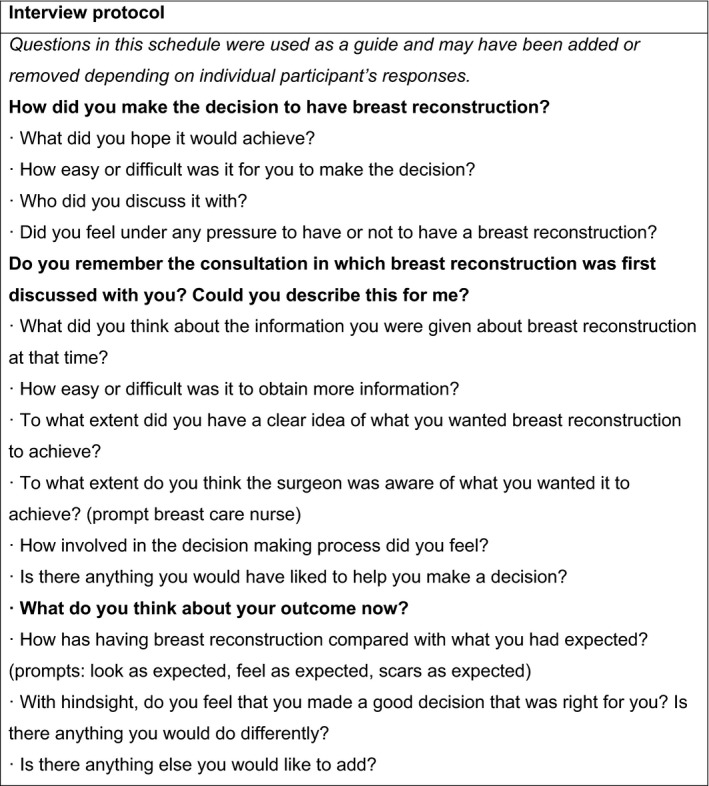
Questions included in the interview schedule with patient participants
FIGURE 2.
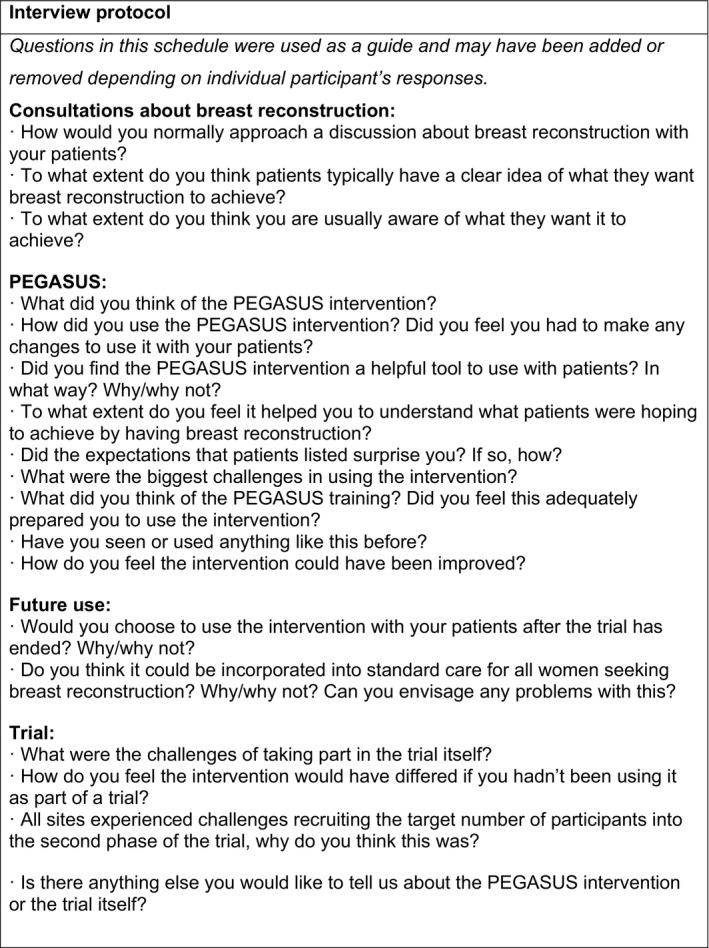
Questions included in the interview schedule with healthcare professionals
2.4. Intervention
Women in the intervention arm attended a consultation with a trained PEGASUS coach, which aimed to clarify their goals and expectations around BR. To aid this discussion, the PEGASUS coach and patient completed the ‘PEGASUS sheet’, which allows space to summarise the conversation, list the patient's surgical and psychosocial expectations for surgery, and rate each expectation in terms of importance (0–10; not at all—extremely). The completed PEGASUS sheet was then used in the subsequent surgical consultation, to facilitate conversation between the patient and surgeon around the patient's expectations. Surgeons were provided with training in how to use the sheet to frame the surgical discussion (see Clarke et al., (2020) for further detail regarding the intervention and its development).
2.5. Data analysis
Thematic analysis of the qualitative data was primarily conducted by PT, in close collaboration with DC and DH, and with feedback from the other authors and a patient representative. Thematic analysis followed five steps, including: ‘data familiarisation’, ‘initial coding generation’, ‘searching for themes’, ‘reviewing and refining themes’ and ‘theme definition and labelling’ (Braun & Clarke, 2006), and was conducted separately for each group before bringing them together for comparison and construction of a broader narrative. Computer Aided Qualitative Data Analysis (CAQDAS) software was used to aid the analysis and all names in this publication are pseudonyms.
3. RESULTS
Sixteen participants from the ‘usual care’ group, 11 participants from the ‘PEGASUS intervention group’ and 13 healthcare professionals (7 PEGASUS coaches, 6 surgeons) took part in interviews; representing participants and healthcare professionals from across the five participating sites (see Table 1 for further demographic information).
TABLE 1.
Participant demographics.
| ‘Usual care’ group participants (n=16) | ‘PEGASUS intervention’ group participants (n=11) | ||
|---|---|---|---|
| Mean age | 52 years | 51 years | |
| Ethnicity | White British | 16 (100%) | 11 (100%) |
| Surgery type | Mastectomy only | 3 (19%) | 0 (0%) |
| Immediate reconstruction | 12 (75%) | 11 (100%) | |
| Delayed reconstruction | 1 (6%) | 0 (0%) | |
| Mean interview duration (minutes) | 30 minutes | 31 minutes | |
Of those 27 participants in the ‘usual care’ and ‘PEGASUS intervention’ groups, 3 participants had a mastectomy only and 1 participant had a delayed reconstruction, with the majority of participants having had an immediate BR. In addition, many participants suggested during interview that they had chosen between one BR option or mastectomy only, due to physical or clinical restrictions; this is discussed further in ‘limitations’ of the study.
Themes and subthemes are presented separately for each group (see Table 2 for a summary of themes and exemplar quotes), and all quotes presented in each section are from the relevant group.
TABLE 2.
Thematic table, with exemplar quotes.
| Group | Theme | Exemplar quote |
|---|---|---|
| Usual care | Bombarded | ‘you're just completely bombarded with information and decision‐making and I think that's a huge thing’. |
| Process of elimination | ‘I think a lot of it is down to the individual because I think if you um … read the information that's given to you and make yourself informed you can actually then drive a better outcome’. | |
| Intervention | Focus amongst the frenetic | ‘I think at that time I was feeling quite confused by things and I wasn't sure what questions to ask and where to go with it and it helped with the decision‐making process’ |
| More than a number | ‘they were aware of who I was as a person, probably things I cope better with than other people and things I don't do as well as other people and what I needed my future to look like compared with somebody else’ | |
| Healthcare professionals | Shifting focus | ‘you could really focus on the area that is important for that patient’ |
| Collective commitment | ‘the CNS [clinical nurse specialist] is pivotal to being able to integrate it’ |
3.1. ‘Usual care’ group: Women recruited into the PEGASUS trial, considering BR and receiving ‘usual care’
Two themes were generated from an analysis of the interviews conducted with women taking part in this group, these are: ‘Bombarded’ and ‘Process of elimination’.
3.1.1. Bombarded
Dominating the decision‐making experience of participants in this group was the description of their initial consultations as overwhelming and difficult to process. Almost all participants in this group suggested that they were unable to take in all the information given to them at this time and many perceived this to be a universal experience:
‘all ladies will tell you when they're first diagnosed that you're just completely bombarded with information and decision‐making and I think that's a huge thing’. (Nicola).
Upon reflection, women appreciated that they needed to be given sufficient information to make an informed decision (‘it's a difficult one because you can swamp people but you've also got to give enough for them to make the right choices’ (Nicola)); however, the means by which information was given to participants appeared to be in stark contrast to the emotional intensity of the experience (‘at that moment in your life, the last thing you want to do is wade through a pile of paperwork’ (Julie)). Although no participant suggested they felt pressure during this process, several women suggested they were tempted to give the decision‐making responsibility to their clinician. Whilst for most this was a brief temptation, one woman did describe adopting a passive role in decision‐making because of this confusion:
‘I think I probably got a little bit confused but then I ultimately thought ‘Oh it doesn't matter too much, you just go with whatever [they] sort of thinks is best really because [they've] got the experience to know’’. (Clare).
Whilst some might argue that feeling overwhelmed when confronted with a cancer diagnosis and a decision of this type is normal or unavoidable, the above example also demonstrates how these feelings might shape an individual's decision and potentially challenge their ability to make an informed decision regarding their care.
3.1.2. Process of elimination
In efforts to counteract the feelings described above and break down the information around their options, an important element of the decision‐making process for many participants was undertaking their own extensive research. Several described reading about what each of the available options would involve, identifying their own priorities (e.g. activity, minimal surgery, appearance), and then asking further questions or making their decision with these priorities in mind. By identifying their own priorities and ruling out incongruent options, women engaged in a self‐driven ‘process of elimination’ (Nicola) to identify their preferred choice.
Importantly, this process of elimination was predominantly patient‐driven. It was not presented as a failure of clinicians to help them, but as something that the women themselves undertook to ensure their choice was right for them and with the aim of gaining the best outcome. However, several participants commented on how the self‐driven nature of the decision‐making process meant that they felt information was often inaccessible to them, feeling unable to seek out further information themselves or make sense of that which they were given.
‘You almost want an idiot's guide because you're just in a … like you're completely blown away by what's going on and you just haven't got the energy’ (Julie).
It is possible that this inaccessibility of information could lead to inequalities in the decision‐making process and, as in the first theme, potentially shape an individual's choice or challenge their ability to make a fully informed decision regarding surgery.
3.2. ‘PEGASUS intervention group’: Women recruited into the PEGASUS trial, considering BR and taking part in the PEGASUS intervention
Two themes were generated from analysis of the interviews conducted with women in this group: ‘Focus amongst the frenetic’ and ‘More than a number’.
3.2.1. Focus amongst the frenetic
When discussing their experiences of decision‐making, participants described the PEGASUS intervention as being a useful tool to focus their mind and frame their discussions regarding BR. Specifically, they suggested that it helped them to process information at a time of heightened emotion:
‘I think at that time I was feeling quite confused by things and I wasn't sure what questions to ask and where to go with it and it helped with the decision‐making process’—(Tracey).
Like the women in the ‘usual care’ group, these participants described the decision‐making process as difficult and stressful, but they also discussed how PEGASUS encouraged them to focus their decision‐making on their own goals and expectations. In addition, some participants suggested that PEGASUS allowed them to reflect on their decision and consider whether this was right for them:
‘It gives you time to look back on it again and think ‘yes, is it right for me?’ […] to think that you're not being rushed into this and at any time I know that I could have changed my mind’—(Elizabeth).
Finally, participants described PEGASUS as enabling them to focus their conversations with healthcare professionals and ensure that they discussed the elements of treatment that were important to them.
‘[PEGASUS] helped frame some of the conversations I could then have with the consultant […] there were some outcomes that we'd identified together as things that […] were most important to me, and that helped me then actually go to the consultant next time and have more of a structured conversation about what I was trying to find out’—(Tracey).
These interactions suggest that the focus provided by the intervention may have allowed participants a level of empowerment and encouraged shared decision‐making between participants and clinicians.
3.2.2. More than a number
During the interview, participants were asked to reflect on the discussions they had had with their clinicians. Many in the intervention group suggested they felt conversations during their consultations were focussed on their wishes (‘everything was solely focussed on me, about what I wanted’ (Elizabeth)) and that clinicians had a good understanding of them as individuals.
‘they were aware of who I was as a person, probably things I cope better with than other people and things I don't do as well as other people and what I needed my future to look like compared with somebody else’—(Alison).
Women in this group suggested that this experience gave them further confidence in their clinicians and trust in their recommendations. They described the conversations that they had with the PEGASUS coach (in most cases a Cancer Nurse Specialist) as being more open and focussed on their needs:
‘I was so relieved to have somebody who I could actually really ask things about. […] she definitely didn't make the decision for me, but things she said prompted me to make a decision’—(Deborah).
Although participants did not directly attribute these feelings to the PEGASUS intervention, the interactions that these participants describe are the appointments where PEGASUS took place and demonstrate the importance of the Cancer Nurse specialists in women's decision‐making experience.
3.3. Healthcare professionals who delivered the PEGASUS intervention as part of the trial
Two themes were generated from analysis of these interviews: ‘Shifting focus’ and ‘Collective commitment’.
3.3.1. Shifting focus
This theme describes a change in the consultations described by healthcare professionals when using the PEGASUS intervention, with both the patient and clinician's focus shifted or broadened during the decision‐making process surrounding BR. Whilst many healthcare professionals described an existing awareness of shared decision‐making and patient‐centred communication, many suggested that PEGASUS encouraged further emphasis on these principles in their practice. The intervention was reported to structure the consultation in a way that ensured conversations were focussed on finding out more about the patient and their priorities when making decisions around reconstructive surgery.
‘It made it more personable […] and really focused on them and their lifestyle […] and what they hope to do in the future. I think sometimes that can get a bit lost’. (PEGASUS Coach (3)).
Not only did the intervention facilitate this more personal communication between patients and clinicians, it was felt to focus the consultation and the decision itself on the patient's goals and expectations.
‘you could really focus on the area that is important for that patient’ (Surgeon (12)).
Acknowledging that logistical arrangements and communicating important information about a patient's curative treatment may sometimes dominate their practice, several clinicians suggested PEGASUS also acted as a reminder to incorporate discussion around a patient's own priorities into the decision‐making process.
‘sometimes it's all too easy to forget that bit, you know, when you're rushing between patients trying to arrange days for surgery and delivering all the stuff about the cancer’. (PEGASUS Coach (4)).
In addition to this focus on patient‐centred discussion, clinicians also described PEGASUS encouraging an increased emphasis on patients’ expectations for the future. Healthcare professionals suggested that many patients are inclined to focus on curative treatment and short‐term outcomes when faced with a cancer diagnosis, which can also dominate conversations relating to BR.
‘It's very easy for the patients initially to focus on the here and now, and not consider long‐term and lifestyle and things’ (PEGASUS Coach (3)).
In comparison, PEGASUS was felt to encourage both patients and clinicians to focus conversation on the future and the patients’ long‐term expectations.
‘A lot of ladies say to us, ‘I just want to recover quickly, I want to move on, I want to get over this’ and actually don't think long term, so I think that was a really good positive from it, that it did focus on home and expectations and plans for the future’ (PEGASUS Coach (3)).
3.3.2. Collective commitment
Clinicians discussed their use of the PEGASUS intervention within the trial, as well as the possibility of using it after the study had finished. In both circumstances, they stressed the importance of having buy‐in from all members of the breast care team, including surgeons and specialist nurses (both of whom are involved in delivering the intervention) and were keen to stress the importance of consistency through the team if the intervention was to be incorporated into the treatment pathway:
‘I don't think it works if you have some members of staff doing it and some not’ (PEGASUS Coach(1)).
Healthcare professionals described this as an important principle in order to provide equitable treatment to all patients and to maintain a unified service, and suggested that the clinical nurse specialists in the team were vitally important to the intervention's success:
‘the CNS [clinical nurse specialist] is pivotal to being able to integrate it’ (Surgeon(4)).
Importantly, surgeons emphasised that their involvement in the intervention was almost entirely dependent on the goals elicited by the PEGASUS coach, as these would frame the conversation that they had with the patient. They stressed that the intervention is ‘heavily reliant on the interaction with the nurse specialist that introduces [PEGASUS]’ (Surgeon (10)) and felt the quality and clarity of the elicited goals were related to the commitment of staff members to the intervention.
4. DISCUSSION
This study aimed to explore patients’ and healthcare professionals’ experiences of using the PEGASUS intervention to aid BR decision‐making. The findings suggest that patients in the intervention group had a qualitatively different experience of decision‐making compared to those in the ‘usual care’ group and suggest several benefits of using the PEGASUS intervention. Patients in the intervention group described how it facilitated focussed conversations that they were able to frame in terms of their own priorities, as well as feeling that their BR team recognised their individual goals and expectations during the decision‐making process. In contrast, whilst participants in the usual care group were complimentary of the treatment they received, they described the decision‐making process as overwhelming and requiring significant independent research to identify their own priorities. Healthcare professionals appeared to echo these findings, suggesting that the intervention encouraged them to alter the focus of their conversations with patients and attend more to the priorities of the individual. Importantly, these findings do not suggest that participants made different decisions as a result of taking part in the intervention or that participants were always entirely satisfied with their decision, but they do appear to suggest that the PEGASUS intervention resulted in a different experience of decision‐making, including increased feelings of shared decision‐making and patient‐centred care taking place.
The findings of this study are in line with conclusions of a previous single‐site acceptability study (Harcourt et al., 2016), demonstrating that both patients and healthcare professionals were accepting of the intervention, but also allowing exploration of how the intervention experience differed from usual care. They echo the findings of previous intervention studies, which have highlighted the utility of exploring benefits, costs/risks and patient attitudes in decision‐making (Paraskeva et al., 2018b), but also reinforce the importance of focussing on communication between patients and healthcare professionals. Importantly, whilst healthcare professionals did report changes to clinician–patient communication because of PEGASUS, they also stressed that this requires the entire clinical team to agree and commit to use of the intervention. These findings reinforce the importance of gaining feedback from healthcare professionals regarding their experience of the intervention, particularly when considering the potential to embed it in clinical practice.
4.1. Study limitations
Many participants in the intervention group described having a limited range of reconstructive options, often choosing between one BR option or mastectomy only. This was revealed during the course of the qualitative interviews, and it is not known to what extent this is representative of the wider population of women considering BR, or how it may have influenced the experiences of those in the intervention group. In addition, the majority of the sample in this study had an immediate BR, and thus, it is not known to what extent the experiences of women having a mastectomy only or a delayed BR are represented in these results.
Whilst all participants in the PEGASUS trial were invited to take part in a qualitative interview, participants with positive experiences of PEGASUS (both patients and healthcare professionals) may have been more likely to take part. It was made clear to all participants prior to the interview that the interviewer was not involved in the development or delivery of the intervention, and all participants were encouraged to be open and honest regarding their experiences; however, there remains a risk that these participants had more positive experiences than those who chose not to take part.
A further challenge of this study concerned the practicalities of incorporating a decision‐making intervention into the breast cancer treatment pathway, and particularly across multiple sites, when decisions regarding immediate BR need to be made in a relatively short period soon after diagnosis. The challenges of conducting this type of intervention trial are discussed further in an additional article (Tollow et al., 2020).
4.2. Clinical implications
These findings support the use of the PEGASUS intervention to assist shared decision‐making for women considering BR and suggest it may influence patients’ and healthcare professionals’ experiences of the decision‐making process, increase the sense of patient‐centred care and shared decision‐making. Future research would usefully explore how we can best identify the women who could most benefit from interventions to support shared decision‐making, as well as the acceptability and effectiveness of an adapted version of PEGASUS for use with different patient groups and other preference‐sensitive surgical decisions.
5. CONCLUSION
The PEGASUS intervention was developed to support shared decision‐making around BR surgery. The findings of this study suggest that PEGASUS may prompt a qualitatively different experience for those using the intervention to support decision‐making, with participants reporting benefits of focussing and framing their conversations with healthcare professionals, as well as increased feelings of patient‐centred care. Healthcare professionals suggested that the intervention encouraged greater focus on individual patient's circumstances and personal priorities, but stressed the importance of collective commitment amongst the clinical team when delivering the intervention. Overall, PEGASUS appears to offer benefits for women considering BR in comparison to usual care, in terms of shared decision‐making and patient‐centred care.
CONFLICT OF INTEREST
PT has no conflict of interest to declare. NP has no conflict of interest to declare. AC has no conflict of interest to declare. PW has no conflict of interest to declare. JP has no conflict of interest to declare. DC has no conflict of interest to declare. DH has no conflict of interest to declare.
ACKNOWLEDGEMENTS
The authors would like to thank: Breast Cancer Now for their support of this study; the University of the West of England for hosting the project; the staff at the NHS sites where the PEGASUS trial took place for their role in recruitment and ongoing support; Sarah Sawyer and Nicola Carson who provided valuable guidance throughout this research project; the project steering group for their advice and guidance; and all the participants for generously giving their time to this research.
Tollow P, Paraskeva N, Clarke A, et al. ‘They were aware of who I was as a person’: Patients’ and health professionals’ experiences of using the PEGASUS intervention to facilitate decision‐making around breast reconstruction. Eur J Cancer Care. 2021;30:e13464. 10.1111/ecc.13464
Funding information
This research was supported by Breast Cancer Now (grant no: 014NovPR415)
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Berlin, N. I. , Tandon, V. J. , Hawley, S. T. , Hamill, J. B. , MacEachern, M. P. , Lee, C. N. , & Wilkins, E. G. (2019). Feasibility and Efficacy of Decision Aids to Improve Decision Making for Postmastectomy Breast Reconstruction: A Systematic Review and Meta‐analysis. Medical Decision Making: an International Journal of the Society for Medical Decision Making, 39(1), 5–20. 10.1177/0272989X18803879 [DOI] [PubMed] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. [Google Scholar]
- Cancer Research UK. (n.d.) (2019). from,https://www.cancerresearchuk.org/health‐professional/cancer‐statistics/statistics‐by‐cancer‐type/breast‐cancer#heading‐Zero
- Clarke, A. , Paraskeva, N. , White, P. , Tollow, P. , Hansen, E. , & Harcourt, D. (2020). The design of a theory based intervention to facilitate shared decision‐making in breast reconstruction. Journal of Cancer Education, 36, 508–518. 10.1007/s13187-019-01656-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denford, S. , Harcourt, D. , Rubin, L. , & Pusic, A. (2011). Understanding normality: a qualitative analysis of breast cancer patients concepts of normality after mastectomy and reconstructive surgery. Psycho‐Oncology, 20(5), 553–558. [DOI] [PubMed] [Google Scholar]
- Harcourt, D. , Griffiths, C. , Baker, E. , Hansen, E. , White, P. , & Clarke, A. (2016). The acceptability of PEGASUS: An intervention to facilitate shared decision‐making with women contemplating breast reconstruction. Psychology, Health and Medicine, 21(2), 248–253. 10.1080/13548506.2015.1051059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt, D. , Paraskeva, N. , White, P. , Powell, J. , & Clarke, A. (2017). A multi‐centred study of the effectiveness of PEGASUS: a multi‐centred study comparing an intervention to promote shared decision making about breast reconstruction with treatment as usual. BMC Medical Informatics and Decision Making, 16, 143. 10.1186/s12911-017-0543-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt, D. , & Rumsey, N. (2004). Mastectomy patients’ decision‐making for or against immediate breast reconstruction. Psycho‐Oncology, 13(2), 106–115. [DOI] [PubMed] [Google Scholar]
- Jeevan, R. , Cromwell, D. A. , Browne, J. P. , Caddy, C. M. , Pereira, J. , Sheppard, C. , Greenaway, K. , & van der Meulen, J. H. P. (2014). Findings of a national comparative audit of mastectomy and breast reconstruction surgery in England. Journal of Plastic, Reconstructive and Aesthetic Surgery, 67(10), 1333–1344. 10.1016/j.bjps.2014.04.022 [DOI] [PubMed] [Google Scholar]
- Lee, C. , Hultman, S. C. , & Karen, S. (2010). Do Patients and providers agree about the most important facts and goals for breast reconstruction decisions? Annals of Plastic Surgery, 64(5), 563–566. [DOI] [PubMed] [Google Scholar]
- Paraskeva, N. , Guest, E. , Lewis‐Smith, H. , & Harcourt, D. (2018a). Assessing the effectiveness of interventions to support patient decision making about breast reconstruction: A systematic review. Breast, 40, 97–105. 10.1016/j.breast.2018.04.020 [DOI] [PubMed] [Google Scholar]
- Paraskeva, N. , Guest, E. , Lewis‐Smith, H. , & Harcourt, D. (2018b). Assessing the effectiveness of interventions to support patient decision making about breast reconstruction: A systematic review. Breast, 40, 97–105. 10.1016/j.breast.2018.04.020 [DOI] [PubMed] [Google Scholar]
- Sheehan, J. , Sherman, K. A. , Lam, T. , & Botages, J. (2007). Association of information satisfaction, psychological distress and monitoring coping style with post‐decision regret following breast reconstruction. Psycho‐Oncology, 16, 342–351. [DOI] [PubMed] [Google Scholar]
- Sherman, K. A. , Shaw, L.‐K. , Jørgensen, L. , Harcourt, D. , Cameron, L. , Boyages, J. , Elder, E. , Kirk, J. , & Tucker, K. (2017). Qualitatively understanding patients’ and health professionals’ experiences of the BRECONDA breast reconstruction decision aid. Psycho‐Oncology, 26(10), 1618–1624. 10.1002/pon.4346 [DOI] [PubMed] [Google Scholar]
- Snell, L. , McCarthy, C. , Klassen, A. , Cano, S. , Rubin, L. , Hurley, K. , & Pusic, A. (2015). Clarifying the expections of patients undergoing breast reconstruction: A qualitative study. Plastic Reconstructive Surgery, 126(6), 1825–1830. 10.1097/PRS.0b013e3181f44580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tollow, P. , Paraskeva, N. , Clarke, A. , White, P. , Powell, J. , Cox, D. , & Harcourt, D. (2020). Challenges and reflections from a multi‐centre trial of a psychosocial oncology intervention. European Journal of Cancer Care, 30(2), 10.1111/ecc.13384 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


