Diagnosis: Naevus lipomatosus cutaneous superficialis
Naevus lipomatosus cutaneous superficialis (NLCS) is a rare skin hamartoma characterized by the growth of mature adipocytes in the dermis and was first described by Hoffman and Zurhelle in 1921 (1–6). There is no sex predilection or heredity (1). NLCS is divided into 2 clinical forms: multiple (classic) and solitary (1–5). Multiple forms are usually inborn or occur in adolescence, with multiple soft, yellowish to skin-coloured, pedunculated papules or nodules that may coalesce into plaques, often on the buttocks or upper thighs. The solitary form usually presents in adulthood as a papule or nodule anywhere on the body, mimicking a soft fibroma. In the current case, multiple nodules were clustered on the lateral skin of the giant mass, suggesting multiple forms.
NLCSs rarely grow to large sizes. Therefore, the number of reported cases is limited. To our knowledge, 14 cases of giant NLCS (over 15 cm), including our case, have been reported; a literature search was performed on PubMed in August 2024, using the search term “giant NLCS”. Giant NLCS predominantly affected males (64%). The onset age ranged from 0 to 30 years (mean: 14.5 years). The time from disease onset to diagnosis was long (mean: 20 years). This might be due to the asymptomatic slow progression of the lesions. In cases where a medical or family history was documented, no abnormalities were noted. The largest NLCS mass was 106 × 30 cm in the back and sacral regions (2). The most common site was the buttocks, but lesions also occurred in other parts of the body, including the neck (2), back (2, 3), and vulva (4), or in more than 2 body regions (2, 3). In addition, most cases showed multiple forms, and there are 2 growth patterns of lesions: 1 pattern in which only some parts of the lesions grow (4), as in the current case, and another pattern in which the entire lesion grows (2, 3, 5, 6).
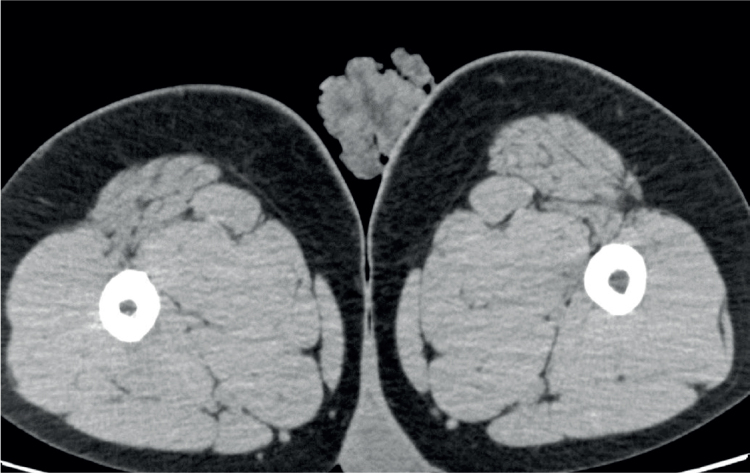
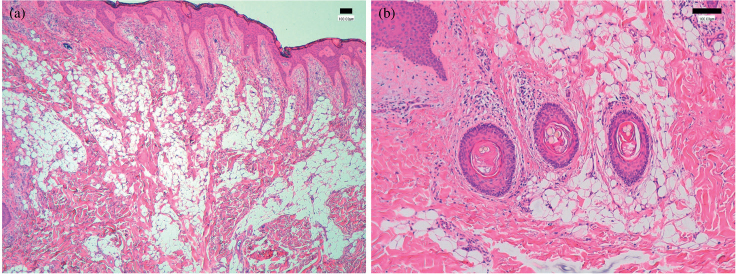
The histological feature of NLCS is mature adipocytes filling more than 10% of the dermis (1–6). The adipocytes most commonly form aggregates around blood vessels, but may also be present as solitary adipocytes between collagen bundles (1). The lesions may contain skin appendages, including hair follicles; in the current case, the hair follicles contained some vellus hairs, indicating a feature of hamartoma. Moreover, the epidermis may show acanthosis, hyperkeratosis, basal pigmentation, and elongation of the rate ridges (1). Although rare, 2 cases of giant NLCS with muscular lipomatosis have been reported (5, 6). In 1 case, magnetic resonance imaging (MRI) showed fat infiltration in the gluteal muscle and a 5 cm mass was completely resected; however, NLCS and muscular lesions recurred simultaneously and grew to a large size (5). The remaining patient underwent complete excision of a 10 × 5 cm mass in the sacral region, but NLCS subsequently recurred and the muscular lesion grew large enough to compress the sciatic nerve, causing neuropathy (6). These facts suggest that a giant NLCS is associated with fat infiltration into the muscle and postoperative recurrence of lesions. Therefore, it is important, especially in patients with giant NLCS, to confirm the presence of muscular lesions using imaging tests such as computed tomography (CT) or MRI before surgery and to plan complete resection to avoid postoperative recurrence.
Although conservative therapeutic interventions for NLCS include CO2 ablative lasers, sodium deoxycholate, and cryotherapy (2, 4), recurrence may occur (4). Surgical excision of the entire lesion is the preferred approach when treatment is required for functional or cosmetic reasons (1–6). All reported cases of giant NLCS underwent surgical excision combined with flap transfer or skin grafting if extensive surgical excision was required (2, 6). In the current case, CT images confirmed the absence of muscular lesions, and no recurrence has occurred for 4 months after complete excision.
REFERENCES
-
1.Lima CDS, Issa MCA, Souza MB, Góes HFO, Santos TBPD, Vilar EAG. Nevus lipomatosus cutaneous superficialis. An Bras Dermatol
2017; 92: 711–713. 10.1590/abd1806-4841.20175217
[DOI] [PMC free article] [PubMed] [Google Scholar]
-
2.Li S, Xiao Y, Wang H, Liu Z. Giant nevus lipomatosus cutaneous superficialis with cerebriform surfaces on the back and sacral region: a case report. Clin Cosmet Investig Dermatol
2022; 15: 981–985. 10.2147/CCID.S366432 [DOI] [PMC free article] [PubMed] [Google Scholar]
-
3.Khandpur S, Nagpal SA, Chandra S, Sharma VK, Kaushal S, Safaya R. Giant nevus lipomatosus cutaneous superficialis. Indian J Dermatol Venereol Leprol
2009; 75: 407–408. 10.4103/0378-6323.53149
[DOI] [PubMed] [Google Scholar]
-
4.Martinez-Ortega JI, Perez-Hernandez FJ, Soto Ortiz JA, Guillermo-Herrera JC. Giant nevus lipomatosus cutaneous superficialis in the vulva: finding the best treatment. Cureus
2023; 15: e50388. 10.7759/cureus.50388
[DOI] [PMC free article] [PubMed] [Google Scholar]
-
5.Jung ST, Park HW, Yun SJ. Giant nevus lipomatosus cutaneous superficialis with intramuscular lipomatosis. J Am Acad Dermatol
2012; 67: e168–e170. 10.1016/j.jaad.2012.01.025
[DOI] [PubMed] [Google Scholar]
-
6.Taş S, Top H. Giant nevus lipomatosus cutaneous superficialis with intramuscular lipomatosis caused sciatic nerve compression. J Cutan Med Surg
2014; 18: 221–222. 10.2310/7750.2013.13161
[DOI] [PubMed] [Google Scholar]