Dear Editor,
Near-total mechanical obstruction of the larynx due to laryngeal papillomas with stridor warrants surgical airway access due to its safety and success.[1] However, it remains invasive and carries a risk of spreading the human papillomavirus to the lower respiratory tract and distal recurrence of tracheal papilloma.[1,2] We report a case of laryngeal papillomatosis with near-total obstruction, managed successfully by orotracheal intubation using the Seldinger technique.
A 52-year-old female was scheduled for emergency debulking of the papillomas under general anaesthesia (GA). Tele-laryngoscopic examination revealed a right false vocal cord exophytic growth bulge and multiple papillomatous exophytic growths arising from the entire length of the right vocal cord, which moved up and down with respiration with possible subglottic extension [Figure 1a]. Computerised tomography scan of the neck showed no evidence of subglottic extension [Figure 1b]. She refused to undergo tracheostomy under local anaesthesia despite explaining its safety and need. However, she agreed to undergo awake airway management by the oral route. She was administered intramuscular glycopyrrolate 0.4 mg premedicated 30 min before shifting to the operation room. Under standard monitoring, the patient was nebulised with 4 ml of 4% lignocaine in a semi-recumbent position. She received oxygen supplementation via a nasal cannula throughout the procedure. Intravenous midazolam 1 mg and fentanyl 30 mg were administered and titrated to achieve a Ramsay sedation score of 2–3. She received transtracheal injection of 3 ml of 4% lignocaine through a 20-G angiocath. A 3.8-sized video bronchoscope (Ambu aScope, Ambu A/S, Ballerup, Denmark) was railroaded with a 5.5 internal diameter micro-laryngeal surgery tracheal tube (MLST) and inserted into her oral cavity. Upon visualising the glottis, 2 ml of 4% lidocaine was sprayed through the bronchoscope’s working channel. To facilitate the entry of the bronchoscope across the near-totally closed glottis, a blunt, straight-tipped polytetrafluoroethylene guide wire 150 cm, 0.038” (Biored Medisys Pvt Ltd, Bangalore, India) was threaded through the working channel of the bronchoscope [Figure 1c]. Then, the tip of the guidewire was inserted through the tiny gap between the vocal cords into the trachea during the inspiratory phase. Subsequently, the bronchoscope was inserted into the trachea over the guidewire. The MLST tube was railroaded over the bronchoscope into the trachea. Chest auscultations and capnography further confirmed the correct tracheal tube position. After induction of GA with intravenous propofol, fentanyl and vecuronium, the surgeon debrided the laryngeal papillomas using a microdebrider, and the glottic opening appeared adequate for extubation at the end of debridement [Figure 1d]. Intravenous dexamethasone 8 mg and, after extubation, nebulised 2 ml of 1:1000 adrenaline were administered to reduce the vocal cord oedema. Since the glottic opening after the debridement was adequate, an airway exchange catheter for extubation was not required and extubation was performed uneventfully. In the postoperative period, oxygen was supplemented by the facemask and was weaned off gradually.
Figure 1.
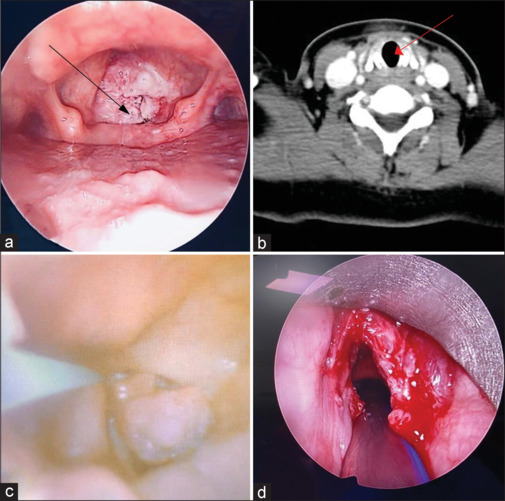
(a) Near-total obstruction of the glottis (black arrow mark showing papilloma). (b) Coronal section of computed tomography scan of the neck at the subglottic level (red arrow showing no subglottic invasion of papilloma). (c) Bronchoscopic image showing guidewire-assisted intubation; (d) Vocal cords after debulking surgery
Our patient was breathing through a narrowed glottis, and the gap was insufficient to pass the bronchoscope freely. Based on our previous experience of managing a similar case of near-total tracheal obstruction by invasive thyroid malignancy, we decided to utilise the wire-guided technique.[3] The advantages of wire-guided techniques include unhurried instrumentation of the airway and the ability to guide the endoscope through the narrow and distorted airway.[4] The risks of airway bleeding and dislodgement of papilloma during tracheal intubation are remote. To avoid tracheostomy, the awake wire-assisted bronchoscope technique can be considered one of the airway management techniques for laryngeal obstruction due to papillomatosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient consented to her images and other clinical information being reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wang J, Han DM, Ma LJ, Ye JY, Xiao Y, Yang QW. Risk factors of juvenile-onset recurrent respiratory papillomatosis in the lower respiratory tract. Chin Med J (Engl) 2012;125:3496–9. [PubMed] [Google Scholar]
- 2.Li SQ, Chen JL, Fu HB, Xu J, Chen LH. Airway management in pediatric patients undergoing suspension laryngoscopic surgery for severe laryngeal obstruction caused by papillomatosis. Paediatr Anaesth. 2010;20:1084–91. doi: 10.1111/j.1460-9592.2010.03447.x. [DOI] [PubMed] [Google Scholar]
- 3.Anguraj J, Panneerselvam S, Rudingwa P, Sivakumar RK. Guidewire-assisted fiberoptic bronchoscope-guided tracheal intubation: A novel airway management in an invasive thyroid malignancy. Saudi J Anaesth. 2019;13:160–2. doi: 10.4103/sja.SJA_729_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heier JM, Schroeder KM, Galgon RE, Arndt GA. Wire-guided (Seldinger technique) intubation through a face mask in urgent, difficult and grossly distorted airways. Saudi J Anaesth. 2012;6:292–4. doi: 10.4103/1658-354X.101226. [DOI] [PMC free article] [PubMed] [Google Scholar]


