Abstract
Case:
A 44-year-old man sustained a thrombosed popliteal artery after a closed left knee dislocation after a high-energy motor vehicle collision. He underwent emergency open popliteal artery embolectomy, with insertion of endovascular stent. After arthroscopic multiligamentous knee injury reconstruction (MLKI-R) on day 18 after injury, he developed stent thrombosis, which resolved with urgent percutaneous thrombectomy.
Conclusion:
This is the first report of popliteal artery stent thrombosis after MLKI-R. Knee surgery in a revascularized limb has remained controversial, but studies are scarce in the literature. Frequent circulation monitoring and vascular specialist availability postoperatively are still key to detecting this complication and early revascularization.
Keywords: male, trauma, road traffic accident, multiligament knee injury, MLKI-R, popliteal artery injury, popliteal stent thrombosis
Knee dislocation is a rare but serious injury with a reported 0.02% incidence, typically occurring as a result of high-energy polytrauma1, with 5% to 17% presenting as an open injury with associated fractures2. The Schenck classification3 describes the knee injuries based on the ligaments injured, with injuries to both cruciate ligaments and the medial side (KD III-M) being the most common (52.4%)4. There is also a high incidence of 40 to 59% popliteal artery injury5-7, which is likely due to the popliteal artery being tightly adhered to the medial femoral epicondyle at the adductor hiatus and fixed distally to the tendinous arch of the soleus8-10.
Nonetheless, vascular disruption is a limb-threatening emergency with an 86% amputation rate11; thus, ligamentous reconstruction is often delayed to ensure restoration and stabilization of vascular flow. To date, there is no consensus or guideline to manage this complex myriad of injuries because of a paucity of data in the literature12,13.
To the best of our knowledge, this is the first reported case of popliteal artery stent thrombosis after multiligamentous knee injury reconstruction (MLKI-R).
The patient was informed that data concerning the case would be submitted for publication, and he provided consent.
Case Report
A 44-year-old man was brought to a tertiary teaching hospital after a vehicle collision, where he was flung off his motorbike after being hit by an oncoming car at approximately 70 kph. Initial vitals were stable with Glasgow coma scale of 15 and intact neurology in all 4 limbs. Computed tomography (CT) scan showed no injury to his brain, spine, chest, abdomen, and pelvis. He had no medical or surgical history and takes no regular medication.
Examination showed effusion and tenderness over his left knee with ligamentous laxity. Radiographs did not show any fracture, and the joint was enlocated. He likely sustained a closed dislocation of the left knee, with undetectable left popliteal, dorsalis pedis, and posterior tibial pulses. An urgent CT angiography was performed showing an acute cutoff of contrast beyond the distal popliteal artery (Fig. 1).
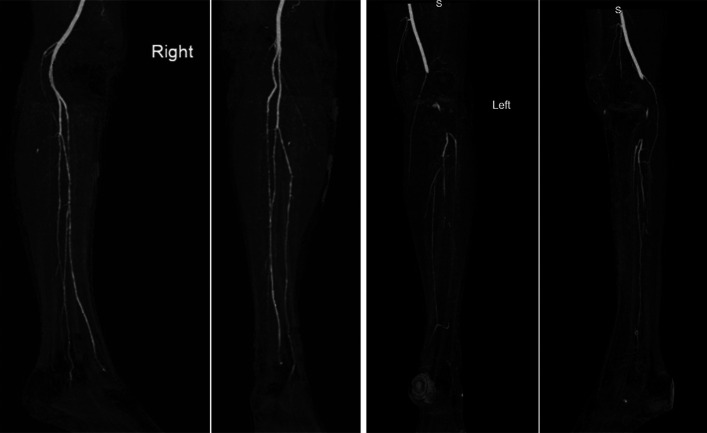
Fig. 1.
CT angiography of right and left legs, showing lack of contrast flow beyond the left popliteal artery. CT = computed tomography.
In addition, he sustained an open fracture-dislocation (Gustilo-Anderson 3B) of his right knee, with distal pulses and sensation intact. Empirical intravenous antibiotics and intramuscular tetanus booster were administered per local protocol.
Initial Revascularization (Day 1 of Admission)
He was brought to operating theater urgently for left lower-limb angiogram and open popliteal artery embolectomy for a 10-cm thrombosed segment, with subsequent insertion of endovascular stent (Viabahn) from P1 to P3 segment of the popliteal artery. His right knee wound and fractures were also extensively debrided in the same operation. Both knees were then stabilized in lower-limb–spanning external fixators. Magnetic resonance imaging of the left knee (Fig. 2) showed complete ruptures of the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), and lateral collateral ligament (LCL), with a partial tear of the medial collateral ligament (MCL). His injuries are summarized in Table I.
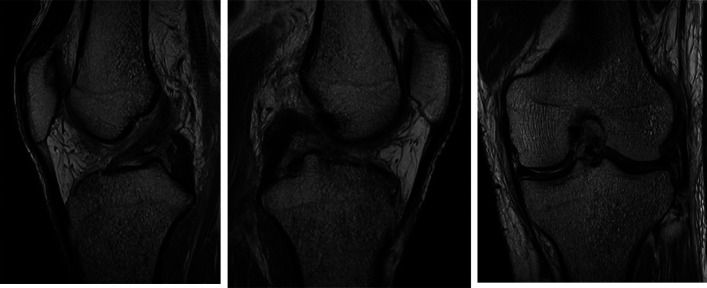
Fig. 2.
Left knee MRIs showing complete ruptures of ACL, PCL, and LCL. ACL = anterior cruciate ligament, LCL = lateral collateral ligament, MRI = magnetic resonance imaging, and PCL = posterior cruciate ligament.
TABLE I.
Summary of Injuries in Both Knees
| Right Knee | Left Knee | |
|---|---|---|
| ACL | Complete rupture | Complete rupture |
| PCL | Complete rupture | Complete rupture |
| LCL | Avulsion fracture at distal femur | Complete tear proximally |
| MCL | Partial high-grade tear >75% | Partial tear |
| Menisci | Medial meniscus capsular tear from posterior horn to anterior horn with roots intact | Medial meniscus posterior horn radial tear with intact root attachment |
| Cartilage | Full-thickness chondral defect over the posterior weight-bearing surface of the MFC | None |
| Bone | Gustilo 3B open in patella comminuted fracture LFC Hoffa fracture (>50%) |
Undisplaced anteromedial tibial plateau fracture |
| Vascular | None | Popliteal artery thrombosis |
| Others | Avulsion tears of the insertional medial and lateral head of the gastrocnemius muscle |
ACL = anterior cruciate ligament, LCL = lateral collateral ligament, MCL = medial collateral ligament, and PCL = posterior cruciate ligament.
His left knee MLKI-R was performed on day 18 of admission, to allow healing time for previous vascular surgery wounds. Preoperative ultrasound Doppler confirmed patent lower-limb vessels and the aforementioned left popliteal endovascular stent. The ACL and PCL reconstruction was performed using harvested semitendinosus and gracilis autograft (quadrupled to 8.5-mm diameter, 6-cm length) and sourced tibialis posterior allograft (quadrupled to 9.5-mm diameter, 7-cm length), respectively, through the arthroscopic “all-inside technique” secured in the femoral and tibial tunnels with Ultrabutton Adjustable Fixation Device (Smith & Nephew). A lateral parapatellar incision split through the iliotibial band is made to visualize the torn LCL remnant, which is plicated using Ultrabraid suture and anchored into its femoral origin footprint in valgus stress using SwiveLock (Arthrex) anchor.
However, while in recovery, the patient’s left foot became cold with no detectable pulses. An urgent CT angiogram showed absent contrast opacification within the popliteal artery endovascular stent (Fig. 3). Urgent vascular consultation was made, and he subsequently underwent percutaneous thrombectomy and thrombolysis, with angioplasty stents inserted into the origin of the anterior tibial artery and tibioperoneal trunk to re-establish left lower-limb circulation. He was started on oral aspirin and prophylactic dose intramuscular enoxaparin, with avoidance of knee flexion. Arterial ultrasound duplex 6 days postoperatively showed triphasic signals in his popliteal artery stent, posterior tibial, and dorsalis pedis arteries.
Fig. 3.
CT angiogram showing absent contrast opacification within the left popliteal artery endovascular stent, after left MLK-R on postinjury day 18. CT = computed tomography.
The patient also underwent right knee fracture fixation and wound closure. Rehabilitation was focused on his upper limb and core muscle strength for bed and chair transfers as both lower limbs were restricted to full extension and non–weight-bearing. He was discharged home on day 33 of admission with no further complications. He subsequently underwent right knee MLKI-R 6 months after injury after the fractures had united. At 1 year postoperatively, both knee wounds have healed with intact pulses. No further ligament laxity was detected in his left knee, and his knee range of movement had recovered to 0 to 130⁰ with full weight-bearing (Fig. 4).
Fig. 4.
Left knee 6 months after MLK-R, showing intact implants on x-ray, healed surgical wounds, and full range of movement.
Discussion
Currently, risk factors for popliteal artery stent thrombosis after MLKI-R are lacking in the literature, with only a single case study reporting stent thrombosis after partial knee replacement14.
The nature of the vascular repair used in such cases may be a factor. Early revascularization involves thrombectomy (open or catheter-based), followed by repair or bypass of the damage section of the artery15,16. However, no randomized controlled trial exists with regard to suitability of popliteal stents in the MLKI-R context. Randomized control trial data 17 had shown similar 5-year patency in both endovascular stenting and open saphenous vein bypass graft in the treatment of popliteal artery aneurysm. Such comparative data will be useful for consideration of vein bypass grafting in the context of knee dislocation multiligament injuries, albeit the longer surgery duration18. Long-term stent patency remains an unsolved issue, particularly in femoropopliteal artery19, which is vulnerable to mechanical compression and kinking from knee articulation. The patency of the popliteal Viabahn stent, which was used in our patient, is reported at 85.6% and 78.5% at 1 and 2 years postoperatively20.
Knee joint immobilization is necessary to prevent damage to the vascular repair5; yet, there has been no consensus on the mode of immobilization. Knee-spanning external fixator confers several advantages especially in the situation of our patient, allowing neurovascular and wound monitoring, while providing a rigid construct to maintain reduction in an unstable knee21.
Knee joint manipulation during MLKI-R can potentially cause stent kinking or even fracture, which is most pronounced when drilling the femoral tunnel in hyperflexion. This can be negated through the use of flexible reamers. A randomized clinical trial by Kosy et al.22 showed no difference in ACL femoral tunnel angles with more anterior lateral femur exit points on 3D-CT analysis between use of conventional rigid reamer in knee maximal hyperflexion and flexible reamer in 100°. Although this can potentially reduce risk of stent fracture and thrombosis, further studies are required to support this hypothesis.
Tourniquet use in a revascularized limb remains controversial because of lack of study, but can potentially damage or dislodge the vascular repair18. When performing arthroscopic MLKI-R, surgeons had reported 3 times better visualization with a tourniquet23; yet, multiple randomized control trials24 and meta-analysis have shown reduced postoperative pain, with no significant difference in surgery time in a tourniquet-less arthroscopic ACL reconstruction. Thus, in a revascularized limb, a tourniquet-less approach may be adopted. Extreme precautions ought to be exercised when operating near the posterior neurovascular bundle, such as during hamstring graft harvest, drilling of the PCL tibial tunnel, and preparation of the PCL tibial footprint.
The optimal timing of MLKI-R after vascular repair remains contentious. Early MLKI-R (within 7 days) is recommended in isolated injury to optimize soft-tissue healing and allow for early rehabilitation9,10. Only a handful of studies have recommended delaying ligamentous repair by at least 2 to 6 weeks until healing of the arterial repair and patency is assured15. Our patient had suffered bilateral knee dislocations, with the right knee arguably more serious with a contaminated open patella fracture (disrupted knee extensor mechanism). Early MLKI-R in his left knee, despite the popliteal artery endovascular stenting, was essential in allowing him to start rehabilitation early.
In our patient, postoperatively regular distal circulation monitoring was vital to early detection of the stent complications or vascular compromise. Availability of CT angiogram modality and vascular specialist was also key to early diagnosis and intervention to restore circulation and salvage his limb.
Conclusion
This is the first report of popliteal artery stent thrombosis after arthroscopic MLKI-R. The frequency of this complication is not well-documented in the literature, and there is a paucity of data on the long-term patency and durability on the different types of endovascular stents deployed in the popliteal artery. Although the authors have recommended a few measures such as early reduction, delayed MLKI-R, tourniquet-less arthroscopy, and reduced joint manipulation, more studies are required to prove a statistical reduction in stent thrombosis. Ultimately, frequent circulation monitoring and vascular specialist availability are key to detecting this complication and salvaging the lower limb.
Footnotes
Investigation performed at Department of Orthopaedic Surgery, Changi General Hospital, Singapore
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSCC/C472).
Contributor Information
Grace I-Ling Tan, Email: Grace.tan@cgh.com.sg.
Siti Mastura Rahim, Email: siti.mastura.rahim@singhealth.com.sg.
References
- 1.Darcy G, Edwards E, Hau R. Epidemiology and outcomes of traumatic knee dislocations: isolated vs multi-trauma injuries. Injury. 2018;49(6):1183-7. [DOI] [PubMed] [Google Scholar]
- 2.King JJ, III, Cerynik DL, Blair JA, Harding SP, Tom JA. Surgical outcomes after traumatic open knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1027-32. [DOI] [PubMed] [Google Scholar]
- 3.Schenck R, Jr. Classification of knee dislocations. Oper Tech Sports Med. 2003;11(3):193-8. [Google Scholar]
- 4.Moatshe G, Dornan GJ, Løken S, Ludvigsen TC, LaPrade RF, Engebretsen L. Demographics and injuries associated with knee dislocation: a prospective review of 303 patients. Orthopaedic J Sports Med. 2017;5(5):2325967117706521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthewson G, Kwapisz A, Sasyniuk T, MacDonald P. Vascular injury in the multiligament injured knee. Clin Sports Med. 2019;38(2):199-213. [DOI] [PubMed] [Google Scholar]
- 6.Kendall RW, Taylor DC, Salvian AJ, O'Brien PJ. The role of arteriography in assessing vascular injuries associated with dislocations of the knee. J Trauma. 1993;35(6):875-8. [DOI] [PubMed] [Google Scholar]
- 7.McCoy GF, Hannon DG, Barr RJ, Templeton J. Vascular injury associated with low-velocity dislocations of the knee. J Bone Joint Surg Br. 1987;69(2):285-7. [DOI] [PubMed] [Google Scholar]
- 8.McDonough EB, Wojtys EM. Multiligamentous injuries of the knee and associated vascular injuries. Am J Sports Med. 2009;37(1):156-9. [DOI] [PubMed] [Google Scholar]
- 9.Dwyer T, Whelan D. Anatomical considerations in multiligament knee injury and surgery. J Knee Surg. 2012;25(4):263-74. [DOI] [PubMed] [Google Scholar]
- 10.Karkos CD, Koudounas G, Giagtzidis IT, Mitka MA, Pliatsios I, Papazoglou KO. Traumatic knee dislocation and popliteal artery injury: a case series. Ann Vasc Surg. 2018;50:298-e13-298.e16. [DOI] [PubMed] [Google Scholar]
- 11.Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59(2):236-9. [PubMed] [Google Scholar]
- 12.Levy BA, Krych AJ, Shah JP, Morgan JA, Stuart MJ. Staged protocol for initial management of the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1630-7. [DOI] [PubMed] [Google Scholar]
- 13.Wascher DC. High-velocity knee dislocation with vascular injury: treatment principles. Clin Sports Med. 2000;19(3):457-77. [DOI] [PubMed] [Google Scholar]
- 14.Hans SS, Hans SS. Management of stent graft thrombosis for popliteal aneurysm following partial knee arthroplasty. Challenging Arterial Reconstructions. 2020:349-53. [Google Scholar]
- 15.Johnson ME, Foster L, DeLee JC. Neurologic and vascular injuries associated with knee ligament injuries. Am J Sports Med. 2008;36(12):2448-62. [DOI] [PubMed] [Google Scholar]
- 16.Hutto JD, Reed AB. Endovascular repair of an acute blunt popliteal artery injury. J Vasc Surg. 2007;45(1):188-90. [DOI] [PubMed] [Google Scholar]
- 17.Antonello M, Frigatti P, Battocchio P, Lepidi S, Dall'Antonia A, Deriu GP, Grego F. Endovascular treatment of asymptomatic popliteal aneurysms: 8-year concurrent comparison with open repair. J Cardiovasc Surg. 2007;48(3):267-74. [PubMed] [Google Scholar]
- 18.Kröger K, Santosa F, Goyen M. Biomechanical incompatibility of popliteal stent placement. J Endovasc Ther. 2004;11(6):686-94. [DOI] [PubMed] [Google Scholar]
- 19.Chang IS, Chee HK, Park SW, Yun IJ, Hwang JJ, Lee SA, Kim JS, Chang SH, Jung HG. The primary patency and fracture rates of self-expandable nitinol stents placed in the popliteal arteries, especially in the P2 and P3 segments, in Korean patients. Korean J Radiol. 2011;12(2):203-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Möllenhoff C, Katsargyris A, Steinbauer M, Tielliu I, Verhoeven ELG. Current status of Hemobahn/Viabahn endografts for treatment of popliteal aneurysms. J Cardiovasc Surg (Torino). 2013;54(6):785-91. [PubMed] [Google Scholar]
- 21.Maslaris A, Brinkmann O, Bungartz M, Krettek C, Jagodzinski M, Liodakis E. Management of knee dislocation prior to ligament reconstruction: what is the current evidence? Update of a universal treatment algorithm. Eur J Orthop Surg Traumatol. 2018;28(6):1001-15. [DOI] [PubMed] [Google Scholar]
- 22.Kosy JD, Walmsley K, Anaspure R, Schranz PJ, Mandalia VI. Flexible reamers create comparable anterior cruciate ligament reconstruction femoral tunnels without the hyperflexion required with rigid reamers: 3D-CT analysis of tunnel morphology in a randomised clinical trial. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1971-8. [DOI] [PubMed] [Google Scholar]
- 23.Kirkley A, Rampersaud R, Griffin S, Amendola A, Litchfield R, Fowler P. Tourniquet versus no tourniquet use in routine knee arthroscopy: a prospective, double-blind, randomized clinical trial. Arthroscopy. 2000;16(2):121-6. [DOI] [PubMed] [Google Scholar]
- 24.Smith TO, Hing CB. A meta-analysis of tourniquet assisted arthroscopic knee surgery. Knee. 2009;16(5):317-21. [DOI] [PubMed] [Google Scholar]