Abstract
Purpose:
Osteoradionecrosis of the jaw (ORN) can manifest in varying severity. The aim of this study is to identify ORN risk factors and develop a novel classification to depict the severity of ORN.
Methods:
Consecutive head-and-neck cancer (HNC) patients treated with curative-intent IMRT (≥ 45Gy) in 2011–2017 were included. Occurrence of ORN was identified from in-house prospective dental and clinical databases and charts. Multivariable logistic regression model was used to identify risk factors and stratify patients into high-risk and low-risk groups. A novel ORN classification system was developed to depict ORN severity by modifying existing systems and incorporating expert opinion. The performance of the novel system was compared to fifteen existing systems for their ability to identify and predict serious ORN event (jaw fracture or requiring jaw resection).
Results:
ORN was identified in 219 out of 2732 (8%) consecutive HNC patients. Factors associated with high-risk of ORN were: oral-cavity or oropharyngeal primaries, received IMRT dose ≥60Gy, current/ex-smokers, and/or stage III-IV periodontal condition. The ORN rate for high-risk vs low-risk patients was 12.7% vs 3.1% (p<0.001) with an area-under-the-receiver-operating-curve (AUC) of 0.71. Existing ORN systems overclassified serious ORN events and failed to recognize maxillary ORN. A novel ORN classification system, ClinRad, was proposed based on vertical extent of bone necrosis and presence/absence of exposed bone/fistula. This system detected serious ORN events in 5.7% of patients and statistically outperformed existing systems.
Conclusion:
We identified risk factors for ORN and proposed a novel ORN classification system based on vertical extent of bone necrosis and presence/absence of exposed bone/fistula. It outperformed existing systems in depicting the seriousness of ORN and may facilitate clinical care and clinical trials.
Context Summary:
Key Objective:
To develop a novel ORN staging and grading system that is applicable clinically and in a trial setting.
Knowledge generated:
The ClinRad classification system for ORN considers clinical and radiographic features to stage the disease in clinical practice and considers treatment recommendations to grade the disease in trials setting. A high-risk cohort for ORN was identified and consists of patients with oral-cavity or oropharyngeal primaries who received IMRT dose ≥60Gy and who are current/ex-smokers and have a stage III-IV periodontal condition.
Relevance (Knisely):
Osteoradionecrosis consequent to chemoradiotherapy for head and neck cancer is justifiably feared. Along with confirmation of the prognostication scheme on a separate clinical database, steps to lessen the risk of developing osteoradionecrosis should also be initiated and tested to make this complication vanishingly rare.
Relevance section written by Dr. Knisely
INTRODUCTION
Osteoradionecrosis (ORN) is one of the most severe radiation-induced complications for patients with head and neck cancer (HNC). ORN has been loosely defined as non-healing mucosal breakdown and bone injury, occurring spontaneously or after trauma, within the head and neck (HN) radiation volume in absence of recurrent tumor on the affected site. Although these criteria are widely accepted for a clinical diagnosis, they fail to incorporate objective imaging findings[1].
The prevalence of ORN varies widely in the literature (up to 40%) with a substantial decrease in modern era (4–8%)2, attributed to advances in radiotherapy technology3,4 and the use of a strict prophylactic dental care policy among institutions5. Specific ORN events, in particular ORN-related jaw fracture, are associated with high resource utilization at healthcare-system level and significant negative impact on the quality of life of HNC patients, influencing patients’ subjective well-being on physical, emotional, functional, and social levels[6]. In addition to other indications, ORN-related pathological fracture necessitates surgical intervention, a significant additional healthcare-system burden resulting in lengthier hospitalization periods, treatment costs and financial burden for patients[7]. Regardless of the indication, major surgical interventions represent a serious event from both patient and healthcare-system perspectives[8].
The severity of ORN is depicted by various classification-systems, generally defined based on: 1) clinical signs (e.g., exposed bone)), 2) radiographic findings (e.g. pathological fracture), and 3) treatment required and response to therapy, either conservative or surgical ). However, to the best of our knowledge, there currently is no consensus regarding the most appropriate classification-system, which hinders inter-study comparison and clinical trial design. Furthermore, the most well-accepted systems overclassify serious ORN[9–12], fail to acknowledge maxillary ORN[13–16] or rely on subjective findings[17–20].
Therefore, we conducted this single institution study aimed to identify risk factors for ORN in HNC patients treated with IMRT, evaluate the appropriateness of various ORN classification-systems in depicting the severity of ORN, and finally to propose a reproducible and standardized novel ORN classification-system incorporating clinically relevant data that can be used in routine clinical care and future clinical trials.
METHODS
Study population and data compilation
We conducted a retrospective review of all consecutive adult HNC patients treated with curative-intent (definitive, pre-, or post-operative) IMRT ≥ 45Gy in our institution who underwent pre-radiation dental evaluation at our institutional dental oncology clinic from 2011–2017. Patients who did not undergo pre-RT dental assessment at our institution, those with a previous history of HN radiation, a diagnosis of primary tracheal cancer or early-stage laryngeal cancer (T1–2 N0 M0), or edentulous patients were excluded. There was no exclusion based on adequacy of available data. A CONSORT diagram is included as Appendix Figure 1. Instituitional research ethics approval was obtained prior to study initiation.
Clinical information, and incidence and severity of ORN were retrieved from in-house prospective Clinical and Dental databases, and cross checked against individual patient dental charts to ensure the completeness and quality of the data. A full description of the databases is included in Appendix Figure 1 [21].
Assessment and Classification of ORN severity:
Diagnostic criteria for an ORN event was defined using criteria from previous classification-systems and included clinical signs, radiographic findings, treatment required and response to therapy. Indications for jaw resection in patients with ORN at our institution included jaw fracture, persistent draining fistula, and significant exposed bone with basilar bone involvement following failure of conservative management in symptom control. Each individual visit for all patients with ORN was reviewed and ORN events were retrospectively classified according to fifteen clinically utilized ORN classification-systems reported in the literature (Appendix Table 1): Coffin[9], Marx[24], Morton and Simpson[10], Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer (RTOG/EORTC)[25], Glanzmann and Gratz[18], Clayman[11], Late Effects Normal Tissue Task Force Subjective, Objective, Management, Analytic scales (LENT/SOMA)[26], Store and Boysen[27], Schwartz and Kagan[13], Notani18, Tsai19, Karagozoglu[15], Lyons[20], Common Terminology Criteria for Adverse Events (CTCAE)[28], Caparrotti 23 and Shaw[16]. For systems that have a duration component (like the Caparrotti-system), duration was used to appropriately grade the ORN according to each classification-system. All data related to ORN was independently reviewed by two reviewers.
Distributions of classifications of ORN for each system were summarized across all visits. Proportions of visits missing sufficient data to assign a classification in each system were summarized and presented both unweighted (all visits weighted equally) and weighted (mean proportion of missing visits was first calculated for each patient, then aggregated so that each patient contributed equal weight). Proportions of patients with at least one classification in the most severe category for each system were summarized.
Statistical Analysis:
Identifying ORN Risk Factors and Stratifying Risk Groups
Univariable analysis with logistic regression was conducted to assess the association of the following clinical factors with ORN, chosen based on clinical relevance: primary tumor location, stage, gender, smoking status, alcohol intake, HPV status, IMRT dose, concurrent chemotherapy, surgical management, periodontal condition, age at diagnosis, and smoking pack/years. Variables with p<0.1 in univariable analysis were considered for inclusion in a multivariable ORN risk-score model, built using backwards model selection, which classified patients into high and low risk groups [13]. Total risk scores were computed by adding the resulting model coefficients on the log scale (termed “risk-score-coefficients, RSC”). An optimal cut point for classifying patients as high-risk vs low-risk was identified by maximizing Youden’s J[29]. To measure predictive performance of the binary high-risk vs low-risk scores, area under the receiver-operating curve (AUC) was calculated from repeated 10-fold cross-validation with 10 iterations. All tests were two-sided and used p<0.05 to define statistical significance.
Evaluating the Performance of ORN Classification-Systems
The performance of ORN classification-systems were evaluated for “separability”, defined here as the ability of each system to discriminate between patients who would go on to experience a “serious ORN event” (jaw fracture or ORN requiring jaw resection) versus those who would not. First, Kaplan-Meier curves and logrank tests were used to compare time from ORN detection to serious ORN event, stratified by stage/grade at the time of ORN detection. Second, univariable Cox proportional hazards regression models were fit to evaluate time to serious ORN event from ORN stage/grade at any visit post-detection of ORN, treating ORN stage as a time-varying covariate. Finally, predictive performance of each classification-system was evaluated via overall Cox model concordance, as well as time-dependent AUC at several clinically relevant timepoints and corresponding c-indices using the methods described by Bansal and Heagerty25. Time-dependent AUC measures classification accuracy between patients with a serious ORN event vs. no events at a given landmark time. Separability analysis was not performed on systems for which >50% of all visits were missing/non-evaluable. A full description of AUC analysis is found in Appendix Table 225,26. We considered concordance and c-index statistics above 0.7, 0.8, and 0.9 to indicate relevant, excellent, and outstanding predictive performance, respectively.
Proposing a Novel ORN Classification-System
The existing ORN classification-systems used to inform the novel classification-system were those identified as high-performing on our analysis based on proportion of missingness (and most-severe stage or grade), and separability (time to serious negative ORN outcomes assessed by Kaplan-Meier curves from first ORN detection, time-to-event cox regression treating ORN stage as a time-varying covariate, and time-dependent AUC). Final extracted characteristics included: 1) The Notani-system18: cateogirzation of early stage ORN as confined to alveolar bone based on imaging; 2) Shaw-system 23: Addition of Minor Bony Spicules; 3) Store-system: Inclusion of radiographic ORN with intact mucosa[27]; 4) CTCAE[28]: Aligning objective grading criteria with treatment recommendations, and; 5) Multiple systems that recognize fracture and orocutaneous fistula as representing the most severe form of ORN11–13,15–20,22,23,27. In addition, The American Association of Oral and Maxillofacial surgeons (AAOMS) staging system for MRONJ28,29 was utilized, in particular the recognition of ORN detectable radiographically but not clinically[11]
RESULTS
Clinical characteristics
A total of 2732 HNC patients were included. Median age was 61 years; 30% (n=807) were current/ex-smokers; 53% (n=1410) had stage III-IV PC; 18% (n=490) were oral cavity cancer (OCC), and 35% (n= 969) were oropharyngeal cancer (OPC). The median IMRT dose was 70 Gy/35 fractions; 43% (n=1170) received concurrent chemotherapy; and 37% (n=1006) underwent surgery (Table 1). The median follow-up was 5.6 years (interquartile range: 4.4–7.3 years). A total of 219 patients (8%) developed ORN.
Table 1:
Patient, Tumor and treatment characteristics
| Covariate | Full Sample (n=2732) | ORN (No) (n=2508) | ORN (Yes) (n=224) | p-value |
|---|---|---|---|---|
| Insurance Type | <0.001 | |||
| No Insurance | 1160 (42) | 1076 (43) | 84 (38) | |
| Private | 1373 (50) | 1264 (50) | 109 (49) | |
| Public | 199 (7) | 168 (7) | 31 (14) | |
| Teeth-preRT [median (range)] | 25 (1–32) | 25 (1–32) | 25 (2–32) | 0.60 |
| Teeth-PostRT [median (range)] | 24 (0–32) | 24 (0–32) | 23 (0–32) | 0.35 |
| DMFS [median (range)] | 71 (0–160) | 71 (0–160) | 72 (5,160) | 0.86 |
| Smoking | <0.001 | |||
| No | 1925 (70) | 1791 (71) | 134 (60) | |
| Yes | 807 (30) | 717 (29) | 90 (40) | |
| Drinking | 0.006 | |||
| Never-Drinker | 1038 (38) | 973 (39) | 65 (30) | |
| Ever-Drinker | 1528 (56) | 1383 (55) | 145 (66) | |
| Unknown | 166 (6) | 157 (6) | 9 (4) | |
| Chemotherapy | 0.28 | |||
| No | 1563 (57) | 1443 (58) | 120 (54) | |
| Yes | 1169 (43) | 1065 (42) | 104 (46) | |
| Surgery | 1 | |||
| No | 1727 (63) | 1585 (63) | 142 (63) | |
| Yes | 1005 (37) | 923 (37) | 82 (37) | |
| Age at Dx [median (range)] | 61.0 (18.3–96.7) | 61.3 (18.3–96.7) | 59.0 (27.7–88.9) | 0.082 |
| Gender | 0.82 | |||
| Female | 732 (27) | 670 (27) | 62 (28) | |
| Male | 2000 (73) | 1838 (73) | 162 (72) | |
| N category | 0.084 | |||
| N0 | 790 (29) | 722 (29) | 68 (30) | |
| N1 | 351 (13) | 324 (13) | 27 (12) | |
| N2 | 1405 (52) | 1282 (52) | 123 (55) | |
| N3 | 156 (6) | 151 (6) | 5 (2) | |
| Missing | 30 | 29 | 1 | |
| Disease Site | <0.001 | |||
| Other | 1074 (39) | 1037 (41) | 37 (17) | |
| Larynx | 199 (7) | 197 (8) | 2 (1) | |
| Lip & Oral Cavity | 490 (18) | 415 (17) | 75 (33) | |
| Oropharynx | 969 (35) | 859 (34) | 110 (49) | |
| HPV status | 0.06 | |||
| Negative | 448 (16) | 408 (16) | 40 (18) | |
| Positive | 856 (31) | 775 (31) | 81 (37) | |
| Unknown/Not Tested | 1428 (52) | 1330 (53) | 98 (45) | |
| Teeth Removed | 0.2 | |||
| Mean (sd) | 1.3 (3.0) | 1.3 (2.9) | 1.7 (3.6) | |
| Median (Min,Max) | 0 (0,28) | 0 (0,26) | 0 (0,28) | |
| Missing | 1 | 1 | 0 | |
| Proportion Teeth Removed | 0.23 | |||
| Mean (sd) | 0.1 (0.2) | 0.1 (0.2) | 0.1 (0.2) | |
| Median (Min,Max) | 0 (0,1) | 0 (0,1) | 0 (0,1) | |
| Missing | 1 | 1 | 0 | |
| Smoking PY [median (range)] | 26 (1–89) | 21 (1–89) | 35 (1–86) | <0.001 |
| PC | 0.012 | |||
| I | 270 (10) | 252 (10) | 18 (8) | |
| II | 504 (19) | 466 (19) | 38 (17) | |
| III | 747 (28) | 673 (27) | 74 (33) | |
| IV | 663 (25) | 596 (24) | 67 (30) | |
| O | 489 (18) | 463 (19) | 26 (12) | |
| Missing | 59 | 58 | 1 | |
| Pre-RT Extraction | 0.3 | |||
| No | 1776 (65) | 1638 (65) | 138 (62) | |
| Yes | 956 (35) | 870 (35) | 86 (38) | |
| RT Dose [median (range)] | 70.0 (2.0–76.7) | 70.0 (2.0–76.7) | 70 (50–70) | 0.16 |
Abbreviations: DMFS: Decayed, missing, filled surfaces according to DMFS160; Pre-RT: before commencement of radiotherapy; post-RT: after completion of radiotherapy; PY: pack-years; PC: Periodontal Condition
ORN Risk Factors and Risk Groups
Multivariable analysis (Table 2) identified the following ORN risk factors: current/ex-smoker (RSC=0.4), stage III-IV PC (RSC=0.4), primary OCC (RSC=1.7), primary OPC (RSC=1.4), and IMRT dose prescription ≥60Gy (RSC=1.3). Patients were classified into ORN risk groups according to the sum of their RSC (High-risk group: sum of RSC≥3.5; low-risk group: sum of RSC <3.5). Applying the generated model, the high-risk group included OCC or OPC patients who received IMRT≥60Gy and current/ex- smoker with stage III-IV PC. The overall rate of ORN for high-risk patients was 12.7% (95% CI 11–14.5%) versus 3.1% (95% CI: 2.1–4%) in the low-risk group (p<0.001). Model Performance from 10-fold cross-validation showed an AUC of 0.71 (95% CI: 0.61–0.81).
Table 2:
Multivariable analysis of risk factors for osteoradionecrosis.
| Odds Ratio (95%CI) | p-value | Global p-value | N | |
|---|---|---|---|---|
| Smoking | 0.010 | 2673 | ||
| No | Reference | 1896 | ||
| Yes | 1.48 (1.10, 1.99) | 777 | ||
| Primary Site | <0.001 | 2673 | ||
| Larynx/Other | Reference | 1246 | ||
| Oral Cavity | 5.66 (3.74, 8.55) | <0.001 | 476 | |
| Oropharynx | 4.05 (2.75, 5.96) | <0.001 | 951 | |
| Dose | 0.03 | 2673 | ||
| <60 | Reference | 144 | ||
| >=60 | 3.59 (1.12, 11.51) | 2529 | ||
| Periodontal Classification | 0.004 | 2673 | ||
| 0–2 (Mild) | Reference | 1263 | ||
| 3–4 (Moderate-severe) | 1.55 (1.15, 2.08) | 1410 |
Comparison of ORN Classification-systems
Missingness (the average proportion of visits where an ORN stage could not be generated per patient by each grading system) is summarized in Table 3. The following ORN grading systems showed less than 25% missingness: Clayman (5.4%), CTCAE (20.6%), Notani (20.9%), RTOG/EORTC (19.3%) and Store-systems (7.5%). The proportion of patients with at least one most-severe stage is summarized in Table 3. The following ORN classification-systems detected less than 5% of patients as having the most severe stage or grade of ORN: RTOG/EORTC (1.1%), SOMA (4.7%), Store (4.9%) and Schwartz-systems (2.5%).
Table 3:
Count and proportion of visits missing staging information in each system and proportion of all patients with at least one visit with most-severe stage
| Classification System | Total visits | Number of staged visits | Number of non-evaluable† visits | Proportion of all visits non-evaluable | Average Proportion Missing Per Patient†† | Most Severe Stage | Proportion of Patients with at least one most-severe score | Proportion all patients with at least one most-severe score, excluding patients with only non-evaluable stages |
|---|---|---|---|---|---|---|---|---|
| CAPARROTTI | 1063 | 626 | 437 | 0.411 | 0.423 | 4 | 0.151 | 0.182 |
| CLAYMAN | 1063 | 989 | 74 | 0.070 | 0.054 | 2 | 0.835 | 0.847 |
| COFFIN | 1063 | 202 | 861 | 0.810 | 0.783 | Major | 0.057 | 0.152 |
| CTCAE | 1063 | 867 | 196 | 0.184 | 0.206 | 3 | 0.057 | 0.066 |
| GLANZMANN | 1063 | 379 | 684 | 0.643 | 0.794 | 2 | 0.165 | 0.449 |
| KARAGOZOGLU | 1063 | 637 | 426 | 0.401 | 0.434 | 3 | 0.061 | 0.088 |
| LYONS | 1063 | 355 | 708 | 0.666 | 0.712 | 4 | 0.071 | 0.176 |
| MARX | 1063 | 160 | 903 | 0.849 | 0.926 | 3 | 0.024 | 0.185 |
| MORTON | 1063 | 170 | 893 | 0.840 | 0.800 | Major | 0.057 | 0.164 |
| NOTANI | 1063 | 878 | 185 | 0.174 | 0.209 | 3 | 0.113 | 0.132 |
| ClinRad | 1063 | 1063 | 0 | 0.000 | 0.000 | 3 | 0.057 | 0.057 |
| RTOG/EORTC | 1063 | 872 | 191 | 0.180 | 0.193 | 4 | 0.009 | 0.011 |
| SCHWARTZ | 1063 | 728 | 335 | 0.315 | 0.323 | 3b | 0.019 | 0.025 |
| SOMA | 1063 | 763 | 300 | 0.282 | 0.313 | 3 | 0.075 | 0.116 |
| STORE | 1063 | 983 | 80 | 0.075 | 0.065 | 4 | 0.038 | 0.047 |
| SHAW | 1063 | 574 | 489 | 0.460 | 0.501 | 3 | 0.047 | 0.049 |
| TSAI | 1063 | 699 | 364 | 0.342 | 0.362 | 4 | 0.042 | 0.057 |
Non-evaluable: missing sufficient data to determine stage from medical chart review.
average proportion of visits where no stage could be generated, per patient
Separability of different classification-systems is illustrated in Figure 1. A total of 168 patients had sufficient ORN staging and follow-up data for separability analysis, 32 patients had a serious ORN event (i.e. jaw fracture or surgery). For the Notani, Shaw (stages 2–3 grouped), RTOG/EORTC (grades 2–4 grouped), Store (grades 2–3 grouped), Schwartz and Karagozoglu-systems (grades 1–3 grouped), patients with a more severe grade at time of ORN detection were more likely to develop a serious ORN event (fracture or surgery) at an earlier timepoint than patients with each successively less severe grade. On Univariable Cox regression (Table 4), diagnosis with most severe stages of the Notani (stage 2–3), Shaw (stage 2–3) and RTOG/EORTC-systems (grades 2–4) significantly associated with risk of serious ORN event (fracture or surgery) when compared to patients only diagnosed with the least severe stage/grade(s).
Figure 1:
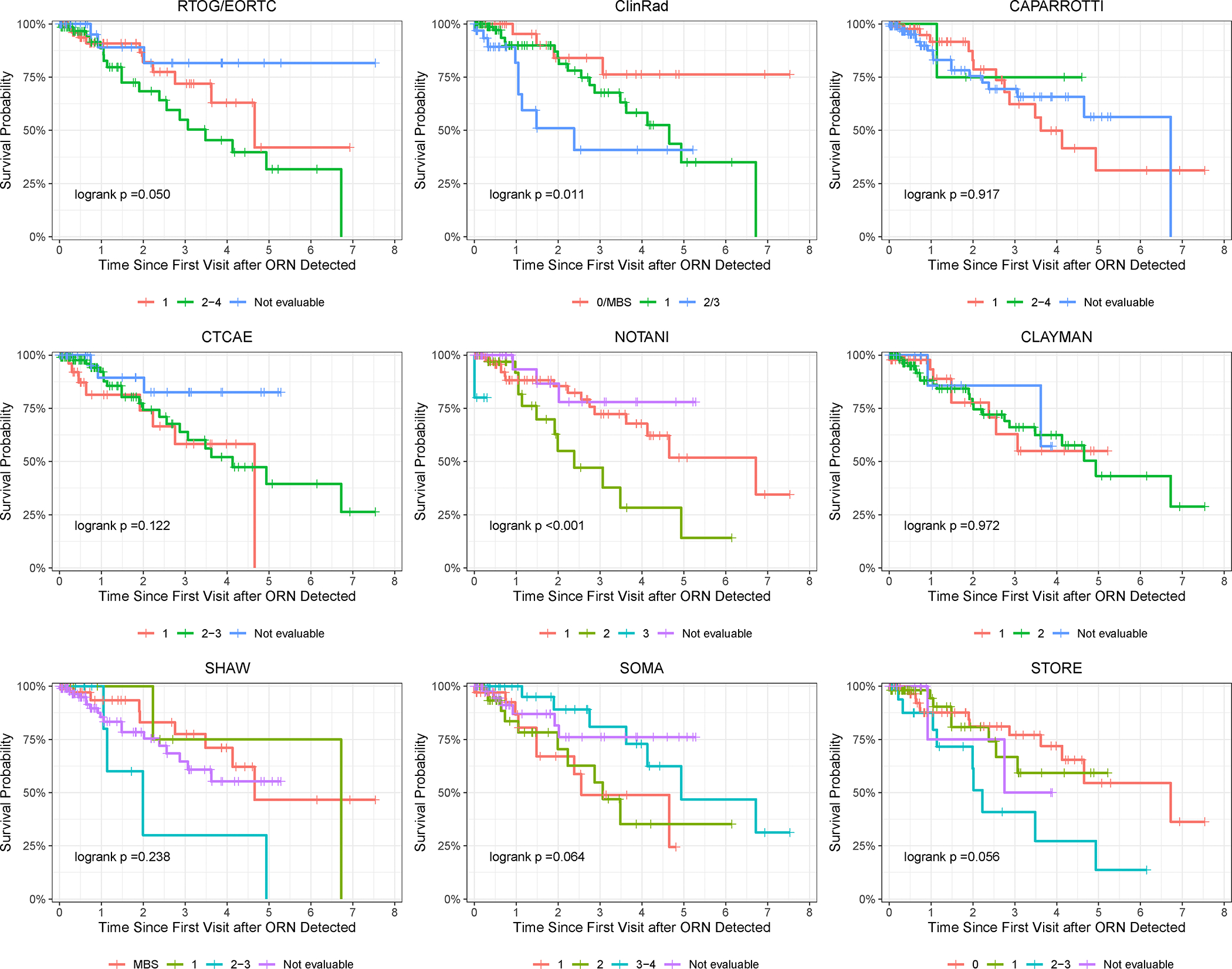
Kaplan-Meier curves for time-to-jaw-fracture or jaw surgery, stratified by stage or grade at baseline (time of ORN detection) within each classification system
Table 4:
Univariable Cox time-to-event regression models: Time to jaw fracture or surgery by stage at all visits prior to fracture, as a time-varying covariate
| Covariate | HR (95%CI) | p-value | Concordance (95% CI) |
|---|---|---|---|
| ClinRad | 0.73 (0.64,0.83) | ||
| MBS/0/1 | Reference | ||
| 2 | 4.90 (2.12, 11.31) | <0.001 | |
| 3 | 11.46 (3.34, 39.32) | <0.001 | |
| Notani | 0.69 (0.58,0.81) | ||
| 1 | Reference | ||
| 2 | 2.50 (1.02, 6.14) | 0.05 | |
| 3 | 9.85 (3.51, 27.69) | <0.001 | |
| Shaw | 0.67 (0.55,0.79) | ||
| MBS-1 | Reference | ||
| 2 | 2.54 (0.97, 6.64) | 0.06 | |
| 3 | 7.02 (2.47, 19.96) | <0.001 | |
| CAPARROTTI | 0.67 (0.56,0.78) | ||
| 1 | Reference | ||
| 2 | 1.07 (0.19, 5.94) | 0.94 | |
| 3 | 2.75 (0.85, 8.92) | 0.09 | |
| 4 | 5.79 (1.67, 20.04) | 0.006 | |
| CTCAE | 0.64 (0.54,0.73) | ||
| 1 | Reference | ||
| 2 | 1.29 (0.54, 3.08) | 0.57 | |
| 3 | 13.88 (4.19, 45.92) | <0.001 | |
| RTOG/EORTC | 0.70 (0.62,0.78) | ||
| 0–1 | Reference | ||
| 2 | 2.67 (1.16, 6.14) | 0.02 | |
| 3–4 | 12.99 (3.78, 44.65) | <0.001 | |
| SOMA | 0.64 (0.51,0.76) | ||
| 0–1 | Reference | ||
| 2 | 1.85 (0.64, 5.37) | 0.26 | |
| 3 | 1.02 (0.35, 3.01) | 0.97 | |
| 4 | 25.60 (6.37, 102.91) | <0.001 | |
| STORE | 0.67 (0.55,0.79) | ||
| 0 | Reference | ||
| 1 | 1.46 (0.52, 4.09) | 0.47 | |
| 2 | 2.05 (0.78, 5.43) | 0.15 | |
| 3 | 24.85 (7.22, 85.52) | <0.001 | |
| SCHWARTZ | 0.67 (0.55,0.79) | ||
| 0–1 | Reference | ||
| 2 | 1.87 (0.78, 4.48) | 0.16 | |
| 3 | 7.31 (2.50, 21.36) | <0.001 | |
| TSAI | 0.65 (0.53,0.77) | ||
| 1 | Reference | ||
| 2 | 0.57 (0.22, 1.46) | 0.24 | |
| 3 | 1.40 (0.44, 4.44) | 0.57 | |
| 4 | 15.31 (4.80, 48.82) | <0.001 | |
| KARAGOZOGLU | 0.60 (0.46,0.73) | ||
| 0 | Reference | ||
| 1 | 1.19 (0.30, 4.66) | 0.80 | |
| 2 | 1.65 (0.45, 6.09) | 0.45 | |
| 3 | 4.43 (1.01, 19.48) | 0.05 |
MBS = Minor bony spicules HR = Hazard Ration CI = Confidence Interval
Development and evaluation of novel ORN grading system:
The proposed ORN classification-system categorizes ORN based on vertical extent of necrosis on imaging and objective clinical findings of bone exposure or fistula formation and is named ClinRad to reflect reliance on objective clinical and imaging findings. The system recognizes 4 different Stages of ORN in addition to Minor Bony Spicules (Table 5):
Table 5:
ClinRad – A Novel Classification system for ORN
| Description | Stage | Radiographic Findings | Clinical Findings | Intervention | ClinRad clinical trial grade proposal |
|---|---|---|---|---|---|
| Distinct from ORN, occurs more often in patients with history of RT | Minor Bone Spicules | None, aside from superficial sequestra | Superficial mobile spicules/sequestra within mucosa | None indicated | Grade 0 |
| Radiographic evidence of bone necrosis confined to alveolar bone with no clinical signs of ORN | Stage 0 | Bone necrosis confined to alveolar bone including: • Bone lysis/sclerosis • Widening periodontal ligament (PDL) space • Absence of osseous filling of extraction sockets |
Intact Mucosa | None indicated | Grade 1 |
| Clinical signs of ORN with or without radiographic evidence of bone necrosis confined to alveolar bone | Stage 1 | None or as stage 0 | Exposed boneA | Minor surgical interventionB and or medical managementC may be indicated with or without adjunctive conservative managementD | Grade 2 |
| Radiographic evidence involving basilar bone with or without clinical signs of ORN | Stage 2 | Bone necrosis involving the basilar bone or maxillary sinus | Intact mucosa or Exposed boneA | Intermediate surgical intervention may be indicatedE, with or without adjunctive conservative and medical management | Grade 3 |
| Advanced ORN | Stage 3 | One or more of the following, ○ Pathological fracture ○ Orocutaneous fistula ○ Oral antral communication/Oral nasal communication |
One or more of the following, ○ Pathological fracture ○ Orocutaneous fistula ○ Oral antral communication/Oral nasal communication |
Reconstructive surgical intervention is indicatedF, with or without adjunctive conservative and medical management | Grade 4 |
: Including pin-point mucosal breach (intra-oral fistula) that probes to bone and/or probing to bone along periodontal tissues
: Examples include sequestrectomy
: Examples include pentoxifylline-tocopherol, hyperbaric oxygen
: Examples include chlorhexidine rinses, antibiotics
: Examples include transoral surgical intervention and debridement, alveolectomy, soft tissue closure
: Examples include segmental maxillectomy/mandibulectomy with vascularized free tissue reconstruction
Applying the ClinRad-system, we were able to classify all visits with ORN (0.0% missingness) and detected 5.7% of patients with the most severe stage of ORN. Patients with a more severe stage at time of ORN detection were more likely to develop serious ORN event (fracture or requiring surgical resection) at an earlier timepoint than patients with each successively less severe stage (Figure 1), with the caveat that stages 2 and 3 were grouped for statistical purpose due to low numbers of patients with stage 3 ORN at time of ORN detection. In addition, diagnosis of stage 2 ORN (HR 4.9, 95%CI 2.12–11.31, p<0.001) or stage 3 ORN (HR 11.45, 95%CI 3.34–39.32, p<0.001) significantly associated with risk of serious ORN event when compared to patients only diagnosed with the least severe stages. The ClinRad-system demonstrated good concordance in Cox modelling, with the highest concordance statistic across all systems (0.73, 95%CI 0.64–0.83), though confidence intervals overlapped with concordance results from other systems (Table 4).
Results of time-dependent AUC analysis are presented in Appendix Table 2. Though no system met the threshold for good performance with respect to c-indices, the ClinRad-system had numerically the highest c-index of all classification-systems in time-dependent AUC analysis, though there was overlap in confidence intervals of the ClinRad-system versus other commonly-used systems such as Notani and Shaw. The ClinRad-system performed similarly, or better than, other grading-systems when predicting serious ORN events at 1-, 2- and 3-years post-detection of ORN.
DISCUSSION
This single institution study identified a high-risk group for ORN. A novel ORN classification system, “ClinRad”, is proposed to addresse the limitations of existing systems. The ClinRad-system also harmonizes with the CTCAE classification to produce a grading-system that can be used in clinical trials.
The overall rate of ORN at the current study was 8%, slightly higher than that reported in the “IMRT era”. This can be attributed to several factors, including: 1) inclusion of minor bony spicules and early radiographic changes as ORN events in this analysis; 2) the utilization of prospectively maintained databases, contrary to the majority of ORN studies which are retrospective in nature and therefore inherently prone to underestimating rates of disease; 3) the detection of ORN events based on multidisciplinary assessments including radiation, surgical and dental oncologists; and 4) inclusion of medical and dental imaging to capture ORN events that might otherwise go undetected.
With a renewed interest in hypofractionation for HNC, risk models for ORN based on conventional radiotherapy dose parameters cannot be directly applied to hypofractionated or stereotactic body radiation therapy (SBRT). Verduijn et al 2023 performed a retrospective study in 334 HNC patients treated with either SBRT boost or conventional IMRT[34]. SBRT and IMRT dose distributions were converted into equivalent dose in 2Gy fractions (a/b = 0.85 Gy) and analyzed using equivalent uniform doses. In multivariable analysis, equivalent uniform dose (a=8) was significantly associated with ORN (AUC=0.71, p < 0.001). Therefore, equivalent uniform dose can be incorporated into ORN risk prediction models across different fractionation schemes[34].
The current analysis excluded edentulous patients because at our institution, edentulous patients are not routinely referred to dental oncologists prior to RT. However, this does not mean the ClinRad-system can only be applied to dentate regions or patients. Some patients seen for pre-radiation dental assessment were rendered edentulous by the time of radiation. In addition, partially-dentate patients with edentulous spans and ORN developing in an edentulous regions were included. In these cases, diagnosis of ORN depends on the stage of resorption of the tooth socket in the edentulous patient or edentulous span, where it is still possible to assign bone exposure or radiographic bone lysis as occurring within alveolar bone or basilar bone.
When considering the performance of previously proposed systems, the Notani-system performed well across multiple domains. A major limitation of the Notani-system is the inclusion of bone lysis beyond the inferior alveolar canal as stage 3 disease. This means a patient with longstanding radiographic evidence of bone lysis beyond this landmark who then progress to fracture will not see an advancement in stage18. In fact, this characteristic resulted in the Notani-system classifying 13.2% of patients as having the most severe form of disease. In addition, Notani-system neglects to include the maxilla, a region where ORN is known to occur[35]. The Shaw-system also performed well, predictable given that it is essentially the Notani-system where some stage 1 cases are re-categorized as Minor Bony Spicules. The concept of Minor Bony Spicules has been included is several previous classification-systems 9,11 and represents an entity distinct from ORN, known to occur in 0.2% of healthy patients following third molar extraction[36].
The CTCAE-system performed well, as it characterizes ORN according to treatment need. However, criteria for classification are a post-hoc function of applied interventions, and availability of treatment locally or local treatment paradigms therefore influences severity of ORN. In addition, Grade 4 ORN - life-threatening consequences, and Grade 5 ORN - Death due to ORN, were not observed to occur in this study. Despite this, the CTCAE-system remains the preferred grading-system for clinical trials, which present a unique challenge. Those recording outcomes in trials may not be dental specialists and therefore ill-equipped to probe for exposed bone, limiting the detecting of stage I disease. Clinical trials favour medical imaging as opposed to dental plain films. Where CT scans are used to assess response to therapy and monitor for recurrence, scatter from metallic restorations can significantly impede interpretation of regions surrounding teeth, making it difficult for medical imaging to diagnose Stage 0 disease. For these reasons, we harmonized the ClinRad-system with the favoured clinical trials-system, the CTCAE, to provide a grading-system for use in clinical trials (Table 5).
The AAOMS-system for MRONJ was heavily consulted when developing the ClinRad-system, as the AAOMS-system is used almost universally by dental professionals to classify MRONJ. As a result, the system is used to stage MRONJ in real-time, and there is overt harmonization across studies on MRONJ. This has allowed for the creation of high-quality evidence to guide decision making in patients at risk of MRONJ, an outcome we hope the ClinRad-system will achieve [33, 37]. To encourage uptake of a single system, we felt it important to incorporate characteristics favoured by both medical and dental professionals involved in management of ORN. By aligning the ClinRad-system with features of the AAOMS-system, this makes the ClinRad-system familiar to dentists, in particular oral and maxillofacial surgeons. While most medical professionals will not be equipped with a dental probe and are unable to detect some cases of Stage I disease, ORN can still be effectively staged according to common radiographic appearance, including subtle changes on dynamic contrast enhanced MRI.
Notably, the system does not include duration of exposure, size of bone exposure, symptoms, or response to treatment. Analysis of systems that included a time or size component generally resulted in over-estimation of severity of ORN, higher missingness and non-significant performance on univariable analysis. While patient symptoms will dictate treatment, this is poorly correlated with extent of bone necrosis, and we instead tied symptoms to management suggestions. Finally, response to therapy requires a patient to have completed a therapy before a stage can be generated, limiting its utility in treatment decision making and standardized data capture.
While the missingness for the ClinRad-system was zero, this is not surprising as 1) The system was designed using existing systems with low missingness, and 2) it was tested and adjusted using patient cases with high missingness across various systems. The ClinRad-system categorized 5.7% of patients with ORN as having the most severe form. This is similar to the proportion in systems that classify ORN in terms of functional deficits or required therapy, like CTCAE (6.6%). Systems that categorize spread of ORN beyond the inferior alveolar canal (Notani- 13.2%, Shaw – 11.6%) appeared to over-estimate the proportion of patients with severe ORN, while simple binary systems or those with high missingness had artificially elevated results.
When analyzing separability, Kaplan-Meier analysis demonstrated that the ClinRad-system performed as well as the Notani, Shaw, RTOG/EORTC and Store-systems. Only Schwartz and Notani-systems required no grouping of stages for statistical power. Given the high proportion of missingness for Karagozoglu and Schwartz-systems, the results for these systems should be interpreted with caution.
Our study has several limitations. The identified risk factors for development of ORN are based on a single-centre retrospective review. The prescribed IMRT dose was incorporated in the ORN risk-score model, however the details on the delivered “rather than planned” IMRT dose was not available to be added. As expected, the ClinRad-system performed well when applied to data used to develop the system but has not been tested outside of this retrospective data set. In addition, though Cox models demonstrated good concordance, time-dependent AUCs had wide confidence intervals and c-indices were not high, potentially due to the relatively low number of post-ORN jaw fracture or surgical intervention events. Future studies will be needed to demonstrate the performance in a prospective clinical setting and datasets from outside of our institution.
Conclusion:
Our study identified a high risk group for ORN and proposed the ClinRad-system that classifies ORN based on clinical and radiographic findings. The ClinRad-sytem outperformed existing systems in depicting the seriousness of ORN and may facilitate clinical care and clinical trials.
Supplementary Material
Acknowledgements:
We acknowledge the generous support by the Bartley-Smith/Wharton, the Gordon Tozer, the Wharton Head and Neck Translational, Dr. Mariano Elia, the Joe’s Team, and the Petersen Funds at the Princess Margaret Foundation of author’s (SHH) academic activity.
We acknowledge the efforts of the dental summer research students, Linnaea Halpert, Josh Moyal, Mariam Ghobrial, Ahuva Plonka, Lila Shapiro and Afisu Oladega.
References:
- 1.Singh A, Huryn JM, Kronstadt KL, Yom SK, Randazzo JR, Estilo CL. Osteoradionecrosis of the jaw: A mini review. Front Oral Health. 2022;3:980786. doi: 10.3389/froh.2022.980786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Studer G, Bredell M, Studer S, Huber G, Glanzmann C. Risk profile for osteoradionecrosis of the mandible in the IMRT era. Strahlenther Onkol. Jan 2016;192(1):32–9. doi: 10.1007/s00066-015-0875-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang W, Zhang X, Yang P, et al. Intensity-modulated proton therapy and osteoradionecrosis in oropharyngeal cancer. Radiother Oncol. Jun 2017;123(3):401–405. doi: 10.1016/j.radonc.2017.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moon DH, Moon SH, Wang K, et al. Incidence of, and risk factors for, mandibular osteoradionecrosis in patients with oral cavity and oropharynx cancers. Oral Oncol. Sep 2017;72:98–103. doi: 10.1016/j.oraloncology.2017.07.014 [DOI] [PubMed] [Google Scholar]
- 5.Ben-David MA, Diamante M, Radawski JD, et al. Lack of osteoradionecrosis of the mandible after intensity-modulated radiotherapy for head and neck cancer: likely contributions of both dental care and improved dose distributions. Int J Radiat Oncol Biol Phys. Jun 01 2007;68(2):396–402. doi: 10.1016/j.ijrobp.2006.11.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong K, Huang SH, O’Sullivan B, et al. Point-of-care outcome assessment in the cancer clinic: audit of data quality. Radiother Oncol. Jun 2010;95(3):339–43. doi: 10.1016/j.radonc.2010.03.015 [DOI] [PubMed] [Google Scholar]
- 7.Watson E, Eason B, Kreher M, Glogauer M. The DMFS160: A new index for measuring post-radiation caries. Oral Oncol. Sep 2020;108:104823. doi: 10.1016/j.oraloncology.2020.104823 [DOI] [PubMed] [Google Scholar]
- 8.Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Periodontol. Jun 2018;89 Suppl 1:S1–S8. doi: 10.1002/JPER.18-0157 [DOI] [PubMed] [Google Scholar]
- 9.Coffin F The incidence and management of osteoradionecrosis of the jaws following head and neck radiotherapy. Br J Radiol. Nov 1983;56(671):851–7. doi: 10.1259/0007-1285-56-671-851 [DOI] [PubMed] [Google Scholar]
- 10.Marx RE, Johnson RP. Studies in the radiobiology of osteoradionecrosis and their clinical significance. Oral Surg Oral Med Oral Pathol. Oct 1987;64(4):379–90. doi: 10.1016/0030-4220(87)90136-8 [DOI] [PubMed] [Google Scholar]
- 11.Morton ME, Simpson W. The management of osteoradionecrosis of the jaws. Br J Oral Maxillofac Surg. Oct 1986;24(5):332–41. doi: 10.1016/0266-4356(86)90018-5 [DOI] [PubMed] [Google Scholar]
- 12.Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. Mar 30 1995;31(5):1341–6. doi: 10.1016/0360-3016(95)00060-C [DOI] [PubMed] [Google Scholar]
- 13.Glanzmann C, Grätz KW. Radionecrosis of the mandibula: a retrospective analysis of the incidence and risk factors. Radiother Oncol. Aug 1995;36(2):94–100. doi: 10.1016/0167-8140(95)01583-3 [DOI] [PubMed] [Google Scholar]
- 14.Clayman L Clinical controversies in oral and maxillofacial surgery: Part two. Management of dental extractions in irradiated jaws: a protocol without hyperbaric oxygen therapy. J Oral Maxillofac Surg. Mar 1997;55(3):275–81. doi: 10.1016/s0278-2391(97)90542-5 [DOI] [PubMed] [Google Scholar]
- 15.LENT SOMA tables. Radiother Oncol. Apr 1995;35(1):17–60. [PubMed] [Google Scholar]
- 16.Støre G, Boysen M. Mandibular osteoradionecrosis: clinical behaviour and diagnostic aspects. Clin Otolaryngol Allied Sci. Oct 2000;25(5):378–84. doi: 10.1046/j.1365-2273.2000.00367.x [DOI] [PubMed] [Google Scholar]
- 17.Schwartz HC, Kagan AR. Osteoradionecrosis of the mandible: scientific basis for clinical staging. Am J Clin Oncol. Apr 2002;25(2):168–71. doi: 10.1097/00000421-200204000-00013 [DOI] [PubMed] [Google Scholar]
- 18.Notani K, Yamazaki Y, Kitada H, et al. Management of mandibular osteoradionecrosis corresponding to the severity of osteoradionecrosis and the method of radiotherapy. Head Neck. Mar 2003;25(3):181–6. doi: 10.1002/hed.10171 [DOI] [PubMed] [Google Scholar]
- 19.Tsai CJ, Hofstede TM, Sturgis EM, et al. Osteoradionecrosis and radiation dose to the mandible in patients with oropharyngeal cancer. Int J Radiat Oncol Biol Phys. Feb 01 2013;85(2):415–20. doi: 10.1016/j.ijrobp.2012.05.032 [DOI] [PubMed] [Google Scholar]
- 20.Lyons A, Osher J, Warner E, Kumar R, Brennan PA. Osteoradionecrosis--a review of current concepts in defining the extent of the disease and a new classification proposal. Br J Oral Maxillofac Surg. May 2014;52(5):392–5. doi: 10.1016/j.bjoms.2014.02.017 [DOI] [PubMed] [Google Scholar]
- 21.Common Terminology Criteria for Adverse Events (CTCAE) Version 5 (Nov 27, 2017). [Google Scholar]
- 22.Caparrotti F, Huang SH, Lu L, et al. Osteoradionecrosis of the mandible in patients with oropharyngeal carcinoma treated with intensity-modulated radiotherapy. Cancer. Oct 01 2017;123(19):3691–3700. doi: 10.1002/cncr.30803 [DOI] [PubMed] [Google Scholar]
- 23.Shaw R, Tesfaye B, Bickerstaff M, Silcocks P, Butterworth C. Refining the definition of mandibular osteoradionecrosis in clinical trials: The cancer research UK HOPON trial (Hyperbaric Oxygen for the Prevention of Osteoradionecrosis). Oral Oncol. Jan 2017;64:73–77. doi: 10.1016/j.oraloncology.2016.12.002 [DOI] [PubMed] [Google Scholar]
- 24.Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. Jun 2008;50(3):419–30. doi: 10.1002/bimj.200710415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bansal A, Heagerty PJ. A Tutorial on Evaluating the Time-Varying Discrimination Accuracy of Survival Models Used in Dynamic Decision Making. Med Decis Making. Nov 2018;38(8):904–916. doi: 10.1177/0272989X18801312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamarudin AN, Cox T, Kolamunnage-Dona R. Time-dependent ROC curve analysis in medical research: current methods and applications. BMC Med Res Methodol. Apr 07 2017;17(1):53. doi: 10.1186/s12874-017-0332-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marx RE. A new concept in the treatment of osteoradionecrosis. J Oral Maxillofac Surg. Jun 1983;41(6):351–7. doi: 10.1016/s0278-2391(83)80005-6 [DOI] [PubMed] [Google Scholar]
- 28.Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw––2014 update. J Oral Maxillofac Surg. Oct 2014;72(10):1938–56. doi: 10.1016/j.joms.2014.04.031 [DOI] [PubMed] [Google Scholar]
- 29.Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, Kademani D. American Association of Oral and Maxillofacial Surgeons’ Position Paper on Medication-Related Osteonecrosis of the Jaws-2022 Update. J Oral Maxillofac Surg. May 2022;80(5):920–943. doi: 10.1016/j.joms.2022.02.008 [DOI] [PubMed] [Google Scholar]
- 30.Shokri T, Wang W, Vincent A, Cohn JE, Kadakia S, Ducic Y. Osteoradionecrosis of the Maxilla: Conservative Management and Reconstructive Considerations. Semin Plast Surg. May 2020;34(2):106–113. doi: 10.1055/s-0040-1709144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. Dec 2003;61(12):1379–89. doi: 10.1016/j.joms.2003.04.001 [DOI] [PubMed] [Google Scholar]
- 32.Baumann DP, Yu P, Hanasono MM, Skoracki RJ. Free flap reconstruction of osteoradionecrosis of the mandible: a 10-year review and defect classification. Head Neck. Jun 2011;33(6):800–7. doi: 10.1002/hed.21537 [DOI] [PubMed] [Google Scholar]
- 33.Chang DW, Oh HK, Robb GL, Miller MJ. Management of advanced mandibular osteoradionecrosis with free flap reconstruction. Head Neck. Oct 2001;23(10):830–5. doi: 10.1002/hed.1121 [DOI] [PubMed] [Google Scholar]
- 34.O’Connell JE, Brown JS, Rogers SN, Bekiroglu F, Schache A, Shaw RJ. Outcomes of microvascular composite reconstruction for mandibular osteoradionecrosis. Br J Oral Maxillofac Surg. Nov 2021;59(9):1031–1035. doi: 10.1016/j.bjoms.2020.11.013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


