Abstract
Molecular determinants of virulence in flaviviruses cluster in two regions on the three-dimensional structure of the envelope (E) protein; the base of domain II, believed to serve as a hinge during pH-dependent conformational change in the endosome, and the lateral face of domain III, which contains an integrin-binding motif Arg-Gly-Asp (RGD) in mosquito-borne flaviviruses and is believed to form the receptor-binding site of the protein. In an effort to better understand the nature of attenuation caused by mutations in these two regions, a full-length infectious cDNA clone of Murray Valley encephalitis virus prototype strain 1-51 (MVE-1-51) was employed to produce a panel of site-directed mutants with substitutions at amino acid positions 277 (E-277; hinge region) or 390 (E-390; RGD motif). Viruses with mutations at E-277 (Ser→Ile, Ser→Asn, Ser→Val, and Ser→Pro) showed various levels of in vitro and in vivo attenuation dependent on the level of hydrophobicity of the substituted amino acid. Altered hemagglutination activity observed for these viruses suggests that mutations in the hinge region may indirectly disrupt the receptor-ligand interaction, possibly by causing premature release of the virion from the endosomal membrane prior to fusion. Similarly, viruses with mutations at E-390 (Asp→Asn, Asp→Glu, and Asp→Tyr) were also attenuated in vitro and in vivo; however, the absorption and penetration rates of these viruses were similar to those of wild-type virus. This, coupled with the fact that E-390 mutant viruses were only moderately inhibited by soluble heparin, suggests that RGD-dependent integrin binding is not essential for entry of MVE and that multiple and/or alternate receptors may be involved in cell entry.
Murray Valley encephalitis virus (MVE) is a member of the Flavivirus genus (family Flaviviridae) and is a small, lipid-enveloped virus which contains a single-stranded positive-sense RNA genome. The genome is approximately 11 kb in length and contains a single open reading frame which is posttranslationally cleaved to generate three structural (C, prM, and E) and seven nonstructural (NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5) proteins. Viral genomic RNA also has a methylated cap at its 5′ terminus and forms a highly conserved stem-loop structure at its 3′ end (61). As for many flaviviruses, MVE causes clinically significant disease in humans and, together with Kunjin (KUN) virus, is responsible for almost all cases of flaviviral encephalitis in mainland Australia (41).
In recent years, infectious cDNA clones have been produced for a number of flaviviruses, including MVE (31, 39), enabling manipulation of the genome at the nucleotide level. Such clones have been used to examine the glycosylation, cleavage, and function of the prM and E (4, 20, 28, 33, 55, 57, 68), NS1 (53, 55, 57), NS2B/NS3 (9, 10, 54), and NS5 (34, 35, 36) proteins, as well as to generate viruses with deletions in their 5′ and 3′ untranslated regions (6, 38, 43, 48). More recent work has seen the generation of chimeric yellow fever viruses (YF), containing the prM and E genes of Japanese encephalitis virus (JE) (8) or dengue virus type 2 (DEN-2) (23). In primates, these chimeric viruses provide solid protection against heterologous virus challenge and demonstrate great potential for use as flavivirus vaccines (23, 24, 49, 50).
The envelope (E) protein of flaviviruses plays a significant role in viral entry and possesses an interesting structural and functional biology. It mediates attachment of the virus to host cells, as well as fusion of the viral and cellular membranes after receptor-mediated endocytosis. In addition, it is the major target of neutralizing antibodies in the host and plays a significant role in both viral tropism and pathogenesis. The three-dimensional structure of the ectodomain of the E protein has been determined for tick-borne encephalitis virus (TBE) (60), and it serves as a useful model for other flaviviruses due to the high amino acid sequence homology observed throughout the genus. The protein forms head-to-tail dimers on the virion surface, and each monomer consists of three domains, referred to as domain I (central domain), domain II (dimerization domain), and domain III (immunoglobulin-like domain).
Molecular determinants of virulence on the flavivirus E protein form three distinct clusters and are likely to affect virulence by disrupting the functional biology of the protein (60). The first cluster, located in a putative hinge region linking domains I and II, appears to affect the pH-dependent conformational change required for endosomal fusion. In MVE, mutations in this region at amino acid position 277 [E-277 (Ser→Ile)] inhibit the hemagglutination (HA) and fusion properties of the virus and cause a loss of neuroinvasiveness (NI) in mice (46, 47). Similarly, mutations in the second cluster, located at the tip of domain II in a highly conserved “fusion peptide,” also appear to disrupt fusion. In contrast, mutations in the third cluster, located on the lateral face of domain III, are predicted to disrupt receptor binding. In some mosquito-borne flaviviruses, the presence of an Arg-Gly-Asp (RGD) motif in this region has led some to suggest that integrin binding may be important for virus entry (40). The involvement of an RGD motif in cell entry has been described for a number of viruses, including adenovirus type 2 (18, 73, 74), human rotavirus RV-5 (17), and foot and mouth disease virus (FMDV) (32). Mutations in this motif have been shown to affect virus infectivity and virulence in both MVE (39, 40) and YF (69).
In this study, two panels of mutant MVE viruses with substitutions at E-277 (Ser) or E-390 (Asp) were created to investigate the influence of these mutations on virulence. For each virus, obvious effects on plaque phenotype, growth kinetics in cell culture, genetic stability, and virulence in mice were observed. Interestingly, mutations at E-277 or E-390 did not affect the absorption or penetration rates of any of the viruses nor did they affect the relative rates of inhibition of virus binding by soluble heparin. However, some mutations caused a complete loss of NI and/or a reduced ability to agglutinate red blood cells (RBCs). Furthermore, some mutant viruses displayed either large- or small-plaque phenotypes, correlating with altered growth kinetics in Vero cells.
MATERIALS AND METHODS
Virus and infectious cDNA clone.
All mutant viruses were derived from an infectious cDNA clone of MVE virus prototype strain MVE-1-51 (designated pMVE-1-51). Thorough genotypic and phenotypic characterization of virus derived from this clone (CDV-1-51) has been described previously (31), and its complete genomic sequence is known (GenBank accession no. AF161266). Site-directed mutations of the E protein (E-277 or E-390) were engineered into clone pMVE-1-51 by using the QuikChange Site Directed Mutagenesis (SDM) kit (Stratagene). The nucleotide sequences of polyacrylamide gel electrophoresis-purified sense primers used for SDM are shown in Table 1.
TABLE 1.
Sense primers used to introduce site-directed mutations into clone pMVE-1-51a
| Primer name | Sequenceb | Amino acid mutation |
|---|---|---|
| E-277-a-fwd | 5′-CAGTCGAGTTTTCGAGCATCACACTTAAACTCACTTCAG-3′ | E-277 Ser→Ile |
| E-277-b-fwd | 5′-CAGTCGAGTTTTCGAGCAACACACTTAAACTCACTTCAG-3′ | E-277 Ser→Asn |
| E-277-c-fwd | 5′-CAGTCGAGTTTTCGAGCGTCACACTTAAACTCACTTCAG-3′ | E-277 Ser→Val |
| E-277-d-fwd | 5′-CAGTCGAGTTTTCGAGCCCCACACTTAAACTCACTTCAG-3′ | E-277 Ser→Pro |
| E-390-a-fwd | 5′-TTGTGGTAGGCAGGGGAGAGAAGCAGATCAATCACCACT-3′ | E-390 Asp→Glu |
| E-390-b-fwd | 5′-TTGTGGTAGGCAGGGGAAACAAGCAGATCAATCACCACT-3′ | E-390 Asp→Asn |
| E-390-c-fwd | 5′-TTGTGGTAGGCAGGGGATACAAGCAGATCAATCACCACT-3′ | E-390 Asp→Tyr |
Antisense complementary primers (not shown) were used in combination with sense primers to form primer pairs for site-directed mutagenesis.
Nucleotide substitutions are underlined and affected codons are highlighted in bold.
After SDM and transformation into a bacterial host, three separate cDNA clones of each of the seven mutants were selected and subjected to sequence analysis over the entire E gene (approximately 15% of the entire genome) for comparison to the known sequence of MVE-1-51 (31). This was performed both to confirm the site-specific change and to ensure that other mutations had not been inadvertently introduced during the cycling protocol. In every clone sequenced (n = 21), only the site-specific change was present. No other mutations were identified in any of the clones, confirming the high fidelity of the Pfu DNA polymerase enzyme used in the cycling reaction. One cDNA clone was selected for each mutant and used as a template for the production of RNA and infectious virus.
Virus recovery and stock preparation.
Site-directed mutants of clone pMVE-1-51 were linearized with XbaI and used as templates for subsequent transcription with T7 RNA polymerase. The generation of genome-length RNA and its transfection into BHK-21 cells by electroporation was performed as described previously (31). Four to six days after electroporation, cell culture supernatants showed obvious signs of cytopathic effect and were assayed for virus by plaque assay on Vero cells. In order to generate stocks of sufficient titer for subsequent assays, transfected BHK-21 cell culture supernatants were passaged three times in C6/36 mosquito cells and sequenced across the entire E gene as described below.
Sequence analysis.
Sequencing was performed using an ABI–Perkin-Elmer automated sequencing system, which incorporates fluorescently labeled dideoxynucleotides. All site-directed mutant clones derived from clone pMVE-1-51 were subjected to sequence analysis over the entire E gene. Mutant virus stocks (C6/36 cell culture supernatants), as well as virus present in the brains of two encephalitic mice infected with each mutant virus, were similarly sequenced across the E gene. For these analyses, genomic RNA was purified using QIAamp Viral RNA spin columns (Qiagen) and amplified by reverse transcriptase PCR as described previously (31). Sequencing primers were supplied by Life Technologies (Gibco BRL) and were used at a final concentration of 0.8 pmol/ml. Details of primer sequences are available by request.
Cell culture.
Vero (ATCC CCL81 P130-P145), BHK-21 (ATCC CCL10 P56-P59), and Aedes albopictus C6/36 (ATCC CRL1660 P5-P20) cells were grown in M199 medium supplemented with 2 mM l-glutamine and 10% fetal calf serum and were incubated at either 37°C (Vero, BHK-21) or 28°C (C6/36) in an atmosphere containing 5% CO2. For plaque assays, subconfluent monolayers of Vero cells in 12-well tissue culture trays were inoculated with virus and incubated for 1 h. Virus was then removed, and cells were overlaid with methylcellulose containing 2% fetal calf serum in M199 media. Cells were cultured for 4 to 6 days at 37°C (5% CO2) and stained with methylene blue to visualize plaques (1% [wt/vol] methylene blue, 10% formaldehyde). To test for temperature sensitivity, plaque assays were performed separately at 37°C and at an elevated temperature of 39°C, and the number and morphology of plaques were compared. For virus growth assays, monolayers of Vero cells in 60-mm2 tissue culture dishes were infected with virus at a multiplicity of infection between 1 and 5 (standardized for each assay). Aliquots of cell culture supernatant (500 μl) were then collected at 6, 12, 18, 24, and 30 h postinfection (p.i.) and replaced with an equal volume of fresh media. The titer of virus in each sample was subsequently determined by plaque assay. All virus growth assays were performed in duplicate.
Absorption and penetration assays.
Monolayers of Vero cells were infected in triplicate according to the adsorption assay method described by Khromykh and Westaway (37) or the penetration assay method described by Hung et al. (30). For adsorption assays, approximately 100 PFU of virus was added to each well and allowed to adsorb for 30, 60, or 90 min at 37°C. Cells were then washed twice with phosphate-buffered saline, overlaid with growth medium, and incubated for 4 to 6 days as per standard plaque assay. For penetration assays, approximately 100 PFU of virus was added to each well and allowed to adsorb for 30, 60, or 90 min at 37°C. Cells were then incubated in acid glycine (pH 3.0) for 3 min to inactivate noneclipsed virus. Acid glycine was aspirated, and cells were overlaid with growth medium as outlined for adsorption assays above. The rate of adsorption or penetration was calculated as the ratio of the average number of plaques at 30 or 60 min p.i. relative to the average number of plaques at 90 min p.i. and was expressed as a percentage.
HA assays.
Virus from infected C6/36 cell supernatants was used as a source of hemagglutinin. HA assays were performed using a modified protocol of Clark and Casals (14) as described previously (46). Titers were recorded as the reciprocal of the highest dilution which yielded complete agglutination of gander RBCs.
Heparin inhibition assays.
Inhibition of virus binding by soluble heparin was performed using modified protocols based on those described by Chen et al. (13), Hung et al. (30), and Lee and Lobigs (39). Approximately 100 PFU of virus was preincubated in Hank's borate-buffered saline (Gibco BRL) containing 200 μg of heparin (Sigma)/ml at 4°C for 1 h. Virus was then inoculated onto monolayers of prechilled Vero cells (30 min at 4°C) and incubated for a further 1 h at 4°C to allow virus binding. The inoculum was then removed and cell monolayers were washed with cold phosphate-buffered saline prior to the addition of M199/MC and incubation at 37°C under standard conditions for 4 to 6 days. Plaques were visualized as per standard plaque assay. Percent inhibition by soluble heparin was calculated according to the following formula: (a − b)/a, where a is the number of plaques on cells incubated with untreated virus and b is the number of plaques on cells incubated with heparin-treated virus.
Virulence in mice.
Litters of five 21-day-old ARC/Swiss mice (Animal Resources Centre, Murdoch, Western Australia, Australia) were injected intracranially (i.c.) or intraperitoneally (i.p.) with 10 or 50 μl, respectively, of a 10-fold dilution of virus. Mice were examined daily for signs of morbidity, and deaths were recorded. “Humane end points” were employed to minimize distress in experimental animals, a method which does not significantly alter 50% lethal dose values in models of viral encephalitis (75). The 50% humane end point dose (HD50) was calculated for each group by following the 50% lethal dose method described by Reed and Muench (59). Mean time to death was determined by injecting mice (10 per group) i.c. or i.p. with 103 PFU of virus and recording the survival of mice over a period of 21 days. Statistical significance was determined using a paired Student's t test.
For growth in mouse brain assays, groups of 30 18-day-old ARC/Swiss mice were injected i.c. with 103 PFU of virus. At selected times, three mice from each group were anesthetized (penthrane) and their brains were removed and snap frozen in liquid nitrogen. Tissues were then stored at −80°C until required. Prior to titration by standard plaque assay, tissues were thawed, weighed, and manually homogenized before being prepared as 10% (wt/vol) suspensions in Hanks' borate-buffered saline. Titers were expressed as PFU per gram of tissue.
For protection assays, groups of 21 18-day-old ARC/Swiss mice were mock inoculated or were inoculated with between 104 and 10−1 PFU of clone-derived virus by the i.p. or i.c. route. At 17 days p.i., surviving mice in each group were challenged with 104 i.p. HD50s of clone-derived wild-type virus (CDV-1-51). Mice were observed for a further 21 days for signs of morbidity, and deaths were recorded. All mouse experiments were undertaken using protocols approved by the University of Western Australia Animal Experimentation Ethics Committee. Mice were kept on a clean litter of sawdust and given food and water ad libitum.
Protein structure graphics.
The three-dimensional structure of a soluble ectodomain fragment of the TBE E protein (Brookhaven Protein Databank [PDB] entry 1SVB) (60) was used as the basis for all diagrammatic representations of the E protein. Such representations were made using RASMOL molecular visualization software (version 2.6) (62). Homology modeling of the MVE E protein was performed using Swiss-PDB-Viewer software (version 3.6b3) (21), where the primary amino acid sequence of the MVE E protein was threaded onto the known structure of the TBE E protein and submitted to the Swiss-Model (ExPASy) server in Geneva, Switzerland, for energy minimization and subsequent generation of a final model.
RESULTS
Mutagenesis of the hinge region at E-277.
Four amino acid substitutions at E-277, varying in terms of their size and hydrophobicity, were selected for this study. At E-277, the hydrophilic Ser residue was converted to a strongly hydrophobic Ile residue (S→I) in order to reconstitute the attenuated virus BHv1 from an earlier study (46). This was performed to ascertain whether a single amino acid change in the E protein was responsible for the observed phenotype, which included a low NI in mice and an inability to agglutinate RBCs. In addition, a second mutant from the McMinn et al. study (46) was reconstituted, since the Ser→Asn (S→N) mutation in this virus (BHv2) had no observable effect on viral phenotype and represented a conservative amino acid change. Two other substitutions at E-277 were also made to produce novel viruses not previously reported. These substitutions, Ser→Pro (S→P) and Ser→Val (S→V), were chosen because they were intermediate in terms of their hydrophobicity between the Ile and Asn residues of the first two mutants. It was predicted that such changes would have various effects on virus phenotype and that these effects may correlate with the level of hydrophobicity of the substituted amino acid.
Phenotypes of E-277 (hinge) mutant viruses in vitro.
The in vitro phenotypes of the four hinge mutant viruses (designated CDV-1-51v1, -v2, -v3, and -v4; Table 2) were compared and contrasted to that of clone-derived wild-type virus (CDV-1-51; see reference 31) by a number of means, including plaque morphology, growth kinetics in Vero cells, temperature sensitivity, adsorption and penetration rates, and HA activity. With the exception of CDV-1-51v2 (S→N), no change to the wild-type (CDV-1-51) plaque morphology was observed for any of the E-277 mutant viruses (see notes to Table 2). CDV-1-51v1 (S→I), CDV-1-51v3 (S→V), and CDV-1-51v4 (S→P) all displayed a normal plaque phenotype, contrasting with the large-plaque phenotype observed for CDV-1-51v2 (S→N).
TABLE 2.
Phenotypes of hinge and RGD mutant viruses in vitro
| Virus | Mutation | Plaque phenotypea | Temp sensitivity at 39°C | Virus entryb
|
|||
|---|---|---|---|---|---|---|---|
| Absorption
|
Penetration
|
||||||
| 30:90 | 60:90 | 30:90 | 60:90 | ||||
| CDV-1-51 | None | Normal | None | 46 | 73 | 47 | 78 |
| CDV-1-51v1 | E-277 (S→I) | Normal | None | 43 | 72 | 49 | 75 |
| CDV-1-51v2 | E-277 (S→N) | Large | None | 48 | 81 | 47 | 82 |
| CDV-1-51v3 | E-277 (S→V) | Normal | None | 49 | 79 | 51 | 80 |
| CDV-1-51v4 | E-277 (S→P) | Normal | None | 44 | 77 | 49 | 80 |
| CDV-1-51v5 | E-390 (D→N) | Small | None | 46 | 74 | 50 | 77 |
| CDV-1-51v6 | E-390 (D→E) | Large | None | 50 | 80 | 51 | 82 |
| CDV-1-51v7 | E-390 (D→Y) | Small | None | 44 | 74 | 43 | 77 |
Plaque phenotypes were determined by comparison to those observed for CDV-1-51. CDV-1-51 had a normal plaque phenotype, with a diametric size of approximately 2.2 mm at day 5 p.i. Viruses with small-plaque phenotypes had plaques approximately half this size at the same time p.i. Viruses with large-plaque phenotypes had plaques approximately twice the size of normal plaques at the same time p.i.
Virus entry rates (ratios) for adsorption and penetration assays are expressed as a percentage, i.e., the number of plaques observed at 30 (30:90) or 60 (60:90) min p.i. divided by the number observed at 90 min p.i. (times 100%).
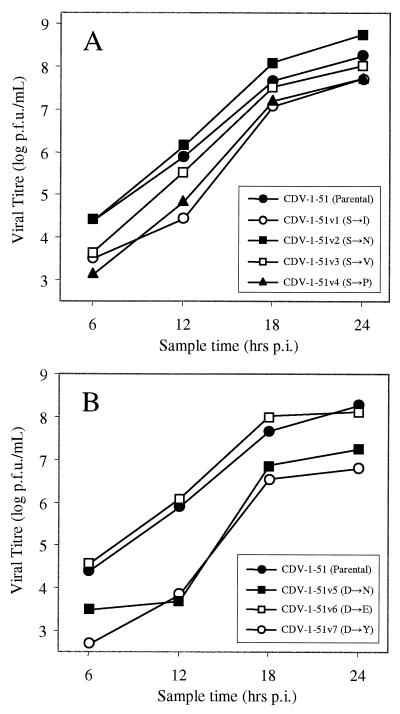
More obvious differences between the phenotypes of the E-277 mutant viruses became apparent when their relative growth kinetics in Vero cells were compared. As shown in Fig. 1a, these differences were most prominent at 12 h p.i., with CDV-1-51v1 (S→I), CDV-1-51v4 (S→P), and CDV-1-51v3 (S→V) exhibiting the lowest titers at this time point. Interestingly, CDV-1-51v2 (S→N) displayed a slightly higher titer than parental virus at this and all other time points, possibly reflecting an improved replicative ability in Vero cells.
FIG. 1.
Growth kinetics of hinge (A) and RGD (B) mutant viruses in Vero cells. Monolayers were infected at a multiplicity of infection of 5, and samples of cell culture supernatant were collected at the times indicated. Viral titers were determined by plaque assay on Vero cells. All assays were performed in duplicate.
To further analyze in vitro phenotype, the temperature sensitivities of each of the hinge mutant viruses were determined by plaque assay at 37 and 39°C (Table 2). Little variability in titer was observed for any of the mutant viruses, suggesting that the introduced mutation had little to no effect on E protein stability at the elevated temperature. To determine if observed differences in growth kinetics were due to altered cell entry, the ability of each of the hinge mutant viruses to bind to and penetrate host cells was determined by adsorption and penetration assay. As shown in Table 2, no significant differences in the ability of E-277 mutant viruses to bind to and penetrate host cells were observed. Adsorption rates (ratios) ranging from 43 to 49% were observed at 30 min p.i., increasing to a range of 72 to 81% by 60 min p.i. Similarly, penetration rates ranging from 47 to 51% were observed at 30 min p.i., increasing to a range of 75 to 82% by 60 min p.i.
Since differences in the binding and penetration of each of the hinge mutant viruses were not evident, the ability of each of these viruses to fuse with RBCs at acidic pH was determined by HA assay. In flaviviruses, HA is a pH-dependent interaction between viral and erythrocyte membranes that is thought to involve the mixing of membrane lipids (56). As such, it serves as a measure of the ability of a virus to fuse efficiently with host cell membranes, specifically those of the endosomal membrane during fusion. Infected C6/36 cell supernatants, ranging in titer between 107 and 108 PFU/ml, were used as a source of HA and assayed for HA activity over the pH range 5.9 to 7.2. Using an optimum pH of 6.6 (determined for CDV-1-51), the HA titers of each of the hinge mutant viruses were determined as shown in Table 3. In addition, the HA titers of two other MVE variants, BHv1 and BHv2 [E-277 (S→I) and E-277 (S→N), respectively; see reference 46], were determined, serving as positive and negative controls for altered HA activity. Interestingly, both CDV-1-51v1 (S→I) and BHv1 (S→I) failed to agglutinate RBCs at the lowest dilution tested (1:2) over the entire pH range examined (data not shown), confirming that a single amino acid substitution at E-277 had been responsible for the observed phenotype of BHv1 in a previous study (46). Furthermore, the HA titers for both CDV-1-51v2 (S→N) and BHv2 (S→N) were also identical at 1:320, similar to that observed for clone-derived wild-type virus (1:160). The HA titers of the remaining two mutants, CDV-1-51v3 (S→V) and CDV-1-51v4 (S→P), were both 1:40; however, the optimal pH for HA was increased from 6.6 to 6.8 for both viruses. Hydrophobic amino acid substitutions at E-277 therefore caused either a complete loss of HA activity [CDV-1-51v1 (S→I)] or a marked reduction of this activity coupled with an increase in optimal pH [CDV-1-51v3 (S→V) and CDV-1-51v4 (S→P)]. In contrast, a hydrophilic amino acid substitution had no effect on HA activity [CDV-1-51v2 (S→N)].
TABLE 3.
HA activity of hinge and RGD mutant viruses
| Virus | Mutation | HA activity
|
|
|---|---|---|---|
| Optimal pH | HA titera | ||
| CDV-1-51 | None | 6.6 | 160 |
| BHv1 | E-277 (S→I) | NAb | <2 |
| BHv2 | E-277 (S→N) | 6.6 | 320 |
| CDV-1-51v1 | E-277 (S→I) | NA | <2 |
| CDV-1-51v2 | E-277 (S→N) | 6.6 | 320 |
| CDV-1-51v3 | E-277 (S→V) | 6.8 | 40 |
| CDV-1-51v4 | E-277 (S→P) | 6.8 | 40 |
| CDV-1-51v5 | E-390 (D→N) | 6.6 | 160 |
| CDV-1-51v6 | E-390 (D→E) | 6.6 | 320 |
| CDV-1-51v7 | E-390 (D→Y) | 6.6 | 160 |
HA titer is expressed as the reciprocal of the highest dilution of virus which yielded complete agglutination of gander RBCs.
NA, not applicable.
Phenotypes of E-277 (hinge) mutant viruses in vivo.
As an extension of the in vitro analyses described above, the in vivo phenotype of each of the hinge mutant viruses was examined by determining HD50 and mortality profiles and comparing average survival times after i.p. or i.c. challenge. In addition, the growth kinetics of each virus in infected mouse brain was also determined.
As shown in Table 4, HD50 values for each of the mutant viruses ranged between 2 and 5 PFU by the i.c. route, resulting in 100% mortality and a mean time to death in the range of 4.4 to 5.5 days. In comparison to the profile for CDV-1-51 (i.c. HD50 of 1 PFU; 100% mortality; time [mean ± standard deviation] to death, 4.6 ± 0.5 days), each of the E-277 mutant viruses was subsequently deemed to be of high neurovirulence (NV). With the exception of CDV-1-51v2 (S→N), the NI (determined by i.p. inoculation) of each of the hinge mutant viruses was found to be markedly different to that of CDV-1-51. The highly neuroinvasive CDV-1-51v2 (S→N) had an i.p. HD50 of 4 PFU, a mortality of 90%, and a mean time to death of 7.3 ± 1.3 days, similar to the profile observed for clone-derived wild-type virus (i.p. HD50 of 5 PFU; mortality of 100%; time to death, 7.2 ± 0.9 days). In contrast, CDV-1-51v1 (S→I) was found to be of low NI, with an i.p. HD50 greater than 104.5 PFU (no observed mortality at the lowest dilution of virus tested). The remaining two mutants, CDV-1-51v3 (S→V) and CDV-1-51v4 (S→P), were found to be of intermediate NI, with HD50 values of 620 and 580 PFU, mortalities of 40 and 50%, and mean times to death of 8.5 ± 1.3 and 10.2 ± 3.6 days, respectively.
TABLE 4.
Phenotypes of hinge and RGD mutant viruses in vivo
| Virus | Mutation | NV parametersa
|
NI parametersb
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| HD50 | % Mortality | Days (mean ± SD) to death | NVc | HD50 | % Mortality | Days (mean ± SD) to death | NId | ||
| CDV-1-51 | None | 1 | 100 | 4.6 ± 0.5 | H | 5.0 | 100 | 7.2 ± 0.9 | H |
| CDV-1-51v1 | E-277 (S→I) | 4 | 100 | 5.5 ± 0.5 | H | >104.5 | 0 | NAe | L |
| CDV-1-51v2 | E-277 (S→N) | 3 | 100 | 4.4 ± 0.5 | H | 4 | 90 | 7.3 ± 1.3 | H |
| CDV-1-51v3 | E-277 (S→V) | 2 | 100 | 4.8 ± 0.8 | H | 620 | 40 | 8.5 ± 1.3 | I |
| CDV-1-51v4 | E-277 (S→P) | 5 | 100 | 4.9 ± 0.3 | H | 580 | 50 | 10.2 ± 3.6 | I |
| CDV-1-51v5 | E-390 (D→N) | 18 | 100 | 4.9 ± 0.6 | H | >104.5 | 0 | NA | L |
| CDV-1-51v6 | E-390 (D→E) | 1 | 100 | 4.3 ± 0.5 | H | 2 | 100 | 6.7 ± 0.8 | H |
| CDV-1-51v7 | E-390 (D→Y) | 10 | 100 | 5.5 ± 0.5 | H | >104.5 | 0 | NA | L |
NV was determined by i.c. inoculation of virus.
NI was determined by i.p. inoculation of virus.
NV was determined according to the criteria described by McMinn et al. (46). H, high (<20 PFU) level of virus.
NI was determined according to the criteria described by McMinn et al. (46). H, high (< PFU); I, intermediate (<103 PFU); L, low (>103 PFU).
NA, not applicable.
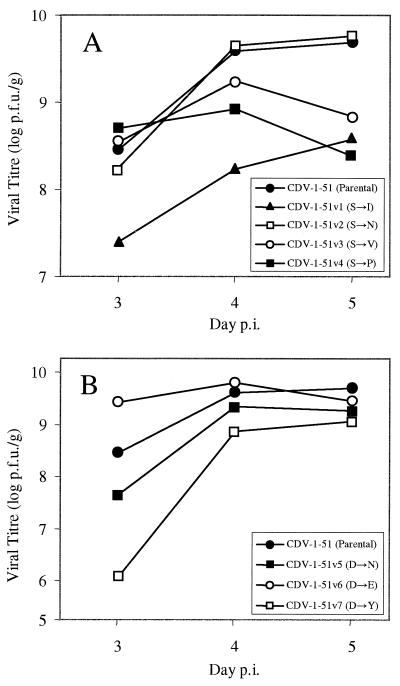
When analysis of the growth kinetics of hinge mutant viruses in infected mouse brain was performed, attenuation was found to be similar to that observed in vitro. As shown in Fig. 2a, mean peak titers ranging from 108.3 to 108.7 PFU/g were obtained for most viruses by day 3 p.i. In contrast, the titer of CDV-1-51v1 (S→I) lagged approximately 10-fold behind that of the other viruses (including CDV-1-51) at the same time point, having a titer of 107.4 PFU/g. On completion of the assay (day 5 p.i.), titers for CDV-1-51v3 (S→V), CDV-1-51v4 (S→P), and CDV-1-51v1 (S→I) were observed to be 20-, 8-, and 13-fold lower, respectively, than those for both CDV-1-51 and CDV-1-51v2 (S→N).
FIG. 2.
Growth kinetics of hinge (A) and RGD (B) mutant viruses in infected mouse brain. Mice were inoculated i.c. with 103 PFU of virus, and brains were collected at the times indicated. Viral titers were determined by plaque assay of 10% homogenates on Vero cells. All assays were performed in duplicate.
Mutagenesis of the RGD motif at E-390.
Three amino acid substitutions at E-390 were selected for this study. At E-390, the negatively charged Asp residue was converted to an uncharged Asn residue [E-390 (D→N)] in order to reconstitute an attenuated virus (P5/Ab10) from a previous study (40). Phenotypic characterization of P5/Ab10 was limited to the observation that the virus had low NI in mice (40). As such, the E-390 (D→N) mutant created in this study was used to further characterize the nature of the attenuation and to ascertain whether a single amino acid change in the E protein was responsible for the observed phenotype. The second mutant, E-390 (D→E), was constructed for two reasons: first, because it represented a conservative amino acid change, and second, because other flaviviruses such as West Nile virus (WNV) (72) and KUN (15) possess an RGE as opposed to an RGD motif in this region of the protein. Substitution of a Glu residue at the third position of an RGD motif has been shown to abolish RGD-dependent integrin binding by a range of viruses, including FMDV (44), chimeric hepatitis B virus (64), and echovirus type 9 (76). The last mutant, E-390 (D→Y), was constructed because it represented the substitution of a large hydrophobic amino acid residue into a strongly hydrophilic region of the protein. Like the D→N and D→E substitutions above, such a mutation would be predicted to significantly disrupt RGD-dependent integrin binding if this were important in the attachment and penetration of MVE into host cells.
Phenotypes of E-390 (RGD) mutant viruses in vitro
As for the panel of hinge mutant viruses, the in vitro phenotypes of each of the RGD mutant viruses (CDV-1-51v5, -v6, and -v7; Table 2) were compared and contrasted in terms of their plaque morphology, growth kinetics in Vero cells, temperature sensitivity, adsorption and penetration rates, and HA activity. All three RGD mutants displayed plaque morphologies different from that of clone-derived wild-type virus. CDV-1-51v5 (D→N) and CDV-1-51v7 (D→Y) exhibited a small-plaque morphology, while CDV-1-51v6 (D→E) exhibited a large-plaque morphology (see notes to Table 2). These differences were found to be reflective of differences in the relative growth kinetics of each virus in Vero cells. As shown in Fig. 1b, obvious differences in replicative ability were evident at 6 h p.i., with CDV-1-51v5 (D→N) and CDV-1-51v7 (D→Y) displaying significantly lower titers at this time point (100- to 500-fold lower titers than CDV-1-51). In contrast, the titer of CDV-1-51v6 (D→E) at this and all other time points was similar to that observed for CDV-1-51. At 12 h p.i., the titers of both CDV-1-51v5 (D→N) and CDV-1-51v7 (D→Y) continued to lag behind those of both CDV-1-51 and CDV-1-51v6 (D→E) by the same order of magnitude, narrowing to 50- and 10-fold differences, respectively, by 24 h p.i.
Further analysis of in vitro phenotype was performed by temperature sensitivity testing of each of the RGD mutant viruses (by plaque assay at 37 and 39°C). As for the panel of hinge mutant viruses, little variability in titer was observed for any of the RGD mutants (Table 2). In addition, no significant differences in the adsorption or penetration rates of these viruses into host cells (Table 2) or their ability to agglutinate RBCs (Table 3) were observed.
Phenotypes of E-390 (RGD) mutant viruses in vivo
As for the hinge mutant viruses described above, the in vivo phenotypes of each of the RGD mutant viruses (CDV-1-51v5, -v6, and -v7) were compared and contrasted to that of CDV-1-51. The results are shown in Table 4. HD50 values ranged between 1 and 18 PFU by the i.c. route, resulting in 100% mortality and a mean time to death between 4.3 and 5.5 days. Each of the E-390 mutant viruses was therefore deemed to be of high NV according to the criteria outlined by McMinn et al. (HD50 of less than 20 PFU) (46).
With the exception of CDV-1-51v6 (D→E), the NI of each of the RGD mutant viruses was found to be markedly different from that of CDV-1-51. The highly neuroinvasive CDV-1-51v6 (D→E) had an i.p. HD50 of 2 PFU, a mortality of 100%, and a mean (± standard deviation) time to death of 6.7 ± 0.8 days, similar to the profile observed for CDV-1-51 (i.p. HD50 of 5 PFU; mortality of 100%; mean time to death of 7.2 ± 0.9 days). In contrast, both CDV-1-51v5 (D→N) and CDV-1-51v7 (D→Y) were found to be of low NI, with i.p. HD50 values of greater than 104.5 PFU (no observed mortality at the lowest dilution of virus tested).
Analysis of the growth kinetics of RGD mutant viruses in infected mouse brain showed a slightly different pattern from that observed in vitro. As shown in Fig. 2b, the titer of CDV-1-51v6 (D→E) had already reached a peak of 109.4 PFU/g by day 3 p.i., approximately eightfold higher than that observed for CDV-1-51 (108.5 PFU/g) at the same time point. In contrast, the titers of CDV-1-51v5 (D→N) and CDV-1-51 (D→Y) lagged behind that of CDV-1-51, reaching 107.7 and 106.1 PFU/g, respectively. On completion of the assay (day 5 p.i.), titers for all three of the RGD mutant viruses were two- to fourfold lower than that of CDV-1-51 (109.7 PFU/g), ranging from 109.1 to 109.5 PFU/g.
Inhibition of virus binding by soluble heparin.
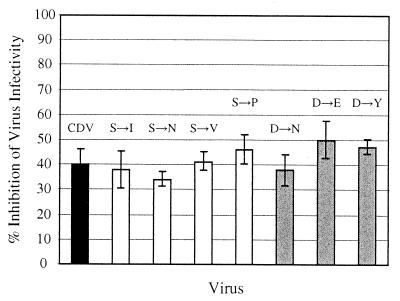
Previous work on DEN-1, DEN-2, and MVE had highlighted a potential role for glycosaminoglycans (GAGs) in host cell entry, based on their ability to inhibit virus binding (13, 27, 30, 39). To ascertain whether clone-derived MVE virus or attenuated variants with mutations at E-277 or E-390 were similarly susceptible to inhibition by GAGs, mutant viruses were preincubated with soluble heparin (200 μg/ml) for 1 h at 4°C prior to their inoculation onto Vero cells for a further 1 h at the same temperature. The inoculum was then removed, and virus titers were determined by plaque assay. As shown in Fig. 3, inhibition of virus infectivity was approximately 40% for CDV-1-51 and ranged between 34 and 46% for the E-277 mutant viruses. Similar inhibition was observed for the E-390 mutant viruses, ranging between 38 and 50%. Given that data generated for DEN-2 (27, 30) had shown a much higher inhibition of virus infectivity (greater than 75%) at the same heparin dose, these results suggested that MVE was only moderately inhibited by heparin. Furthermore, the introduced mutations at E-277 and E-390 appeared to have little to no effect on the heparin binding ability of any of the viruses.
FIG. 3.
Inhibition of virus binding by soluble heparin. Rates of inhibition were calculated using the following formula: (a − b)/a, where a is the number of plaques on cells incubated with untreated virus and b is the number of plaques on cells incubated with heparin-treated virus. CDV-1-51 is shown in black, E-277 mutant viruses are in white, and E-390 mutant viruses are in gray. Average results from two separate experiments are shown.
Stability of introduced mutations during in vitro passage.
Due to selective pressures conferred by an attenuating mutation, it is possible that the amino acid sequence of a mutant virus may revert to that of wild-type virus. Alternatively, second-site mutations may arise, serving in some way to stabilize or compensate for the attenuating mutation. To determine if the attenuation of viruses with mutations at E-277 or E-390 resulted in a selective pressure for reversion (or the appearance of second-site mutations), the stability of each of the mutants produced in this study was determined in vitro by examining the nucleotide sequence of the E protein at different passage levels.
Reverse transcriptase PCR-generated cDNA of each virus was sequenced after one passage (P1) in C6/36 cells and again after two additional passages in the same cell line (P3). In all four of the hinge mutant viruses, the sequence of the E protein was unchanged. Similarly, in two of the three RGD mutants [CDV-1-51v5 (D→N) and CDV-1-51v6 (D→E)], the E protein sequence was also unaffected. Interestingly, the E gene of CDV-1-51v7 (D→Y) contained a single point mutation at E-497, resulting in a Thr→Ile (T→I) substitution. This mutation was found in both the P1 and P3 viruses and must therefore have arisen prior to or during initial amplification of the virus in BHK-21 cells after transfection.
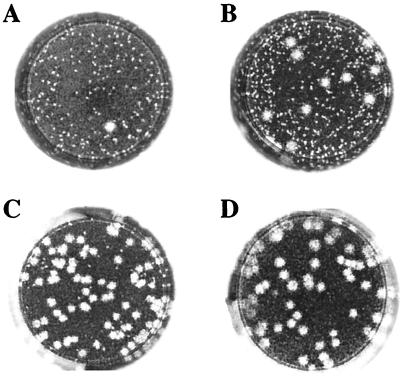
During titration of E-277 and E-390 virus stocks by plaque assay on Vero cells, virus with a normal plaque phenotype was observed at a frequency of approximately 0.5% (1 plaque in 200) in the P3 stock of CDV-1-51v5 (D→N). To ascertain whether this or any other mutant virus stock contained revertants at low frequency, the P3 stock of each virus was passaged three times more in either C6/36 cells (P4-P6) or Vero cells (VP1-VP3). With the exception of CDV-1-51v5 (D→N), all viruses retained their respective plaque phenotypes during passage in both cell lines. As shown in Fig. 4, however, the CDV-1-51v5 (D→N) mutant (which retained its small-plaque phenotype throughout passage in C6/36 cells) reverted over the course of three passages in Vero cells to a normal plaque phenotype. This normal plaque phenotype constituted approximately 10% of the viral population at VP1, 80% of the viral population at VP2, and 100% of the viral population at VP3. Nucleotide sequencing of the E gene of CDV-1-51v5 (D→N) at VP3 confirmed that the Asn (N) residue at E-390 had reverted to the Asp (D) residue of the wild-type virus. Similar sequencing of the VP3 stocks of CDV-1-51v6 (D→E) and CDV-1-51v7 (D→Y) revealed no reversion of the mutated E-390 residue to that of the wild type.
FIG. 4.
Plaque phenotype of CDV-1-51v5 (D→N) after multiple passage in Vero cells. A third passage C6/36 stock was progressively passaged to generate Vero passage 1 (VP1) through passage 3 (VP3) stocks. (A) Original C6/36 P3 stock; (B) CDV-1-51v5 (D→N) VP1; (C) CDV-1-51v5 (D→N) VP2; (D) CDV-1-51v5 (D→N) VP3.
Reversion of the CDV-1-51v5 (D→N) mutant may be suggestive of an overall intolerance of MVE to mutations at E-390, evidenced by reversion of the CDV-1-51v5 (D→N) mutant in cell culture and the appearance of a second-site mutation at E-497 of the CDV-1-51v7 (D→Y) mutant. Such pressure was unlikely for the CDV-1-51v6 (D→E) mutant because the amino acid change was conservative and because the replicative ability of the virus was unaffected (see in vitro and in vivo phenotypes above).
DISCUSSION
Mutations in the hinge region.
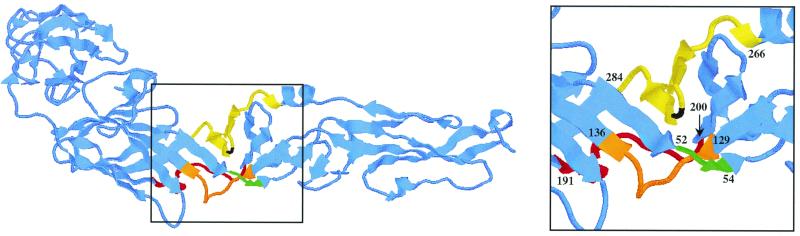
The effects of mutations in the hinge region of the MVE E protein on mouse NI highlight the importance of this region in viral virulence. Previous studies with JE, YF, or JE/YF chimeras have shown that mutations in the polar interface linking domains I and II cause significant attenuation. This interface, shown diagrammatically in Fig. 5, includes residues E-52 to E-54 (hereafter referred to as hinge 1), E-129 to E-136 (hinge 2), E-191 to E-200 (hinge 3), and E-266 to E-284 (hinge 4; MVE numbering based on the TBE model described by Rey et al. [60]). A range of different mutations in these regions can cause a loss of either NI or NV. For example, a mutation in hinge 1 of JE [E-52 (Q→R/K)] causes a loss of NI (26), while a similar mutation in YF [E-52 (G→R)] contributes to a loss of NV (63). Mutations in hinges 2 and 4 also contribute to a loss of NI and/or NV in JE [E-270 (I→S) and E-138 (E→K)] and JE/YF chimeras [E-138 (E→K)] (2, 7, 8, 11, 68).
FIG. 5.
The hinge region of the MVE E protein, based on the known three-dimensional structure of the TBE E protein (60). In MVE, the polar interface linking domains I and II includes residues E-52 to E-54 (hinge 1 [green]), E-129 to E-136 (hinge 2 [orange]), E-191 to E-200 (hinge 3 [red]), and E-266 to E-284 (hinge 4 [yellow]). Hinges 1 through 4 correspond to regions D0-a, e-E0, H0-f, and αB-I0, respectively, according to the nomenclature described by Rey et al. (60). Residue E-277, the residue selected for SDM, is highlighted in black.
In addition to those described above, mutations in hinge 4 also cause a loss or reduction of NI in MVE [E-277 (S→I, V, or P); see reference 46 and work described in this study]. In these cases, the introduction of hydrophobic amino acid residues into an otherwise hydrophilic region of the E protein appears to disrupt the function of the protein at a stage following adsorption and penetration of the host cell. Interestingly, the introduction of a strongly hydrophobic Ile residue into hinge 4 abolishes both HA activity and NI; however, the introduction of a Val residue (which is also strongly hydrophobic but has a smaller side chain) or a Pro residue (weakly hydrophobic) reduces but does not abolish HA activity and NI. Given that adsorption and penetration rates for all hinge mutant viruses were unperturbed and that inhibition of these viruses by soluble heparin was similar to that observed for CDV-1-51, evidence from this and other studies suggests that disruption of E protein function may be caused not by altered binding but by structural instability of the E protein. This instability appears to occur at a point after viral entry and is exacerbated by an increase in the hydrophobicity of the region, as evidenced by the phenotypes of the hinge mutant viruses described above. CDV-1-51v1 (S→I), the most attenuated of the four hinge mutant viruses constructed, contained the most hydrophobic of the substituted amino acids and displayed a complete loss of NI in mice, coupled with reduced replication kinetics in both Vero cells and infected mouse brain. Similarly, CDV-1-51v3 (S→V) and CDV-1-51v4 (S→P) contained substituted amino acids of intermediate hydrophobicity, correlating with intermediate levels of both NI and replication in vitro and in vivo. Concomitantly, the substitution of an Asn residue at E-277 [(CDV-1-51v2 (S→N)], which has little effect on the hydrophobicity of the region, correspondingly had no effect on the phenotype of the virus (high NI and normal growth kinetics in vitro and in vivo).
E-277 forms part of a Ser-Ser-Ser-Thr (SSST) motif at positions E-275 to E-278 of the MVE E protein, a strongly hydrophilic β-turn (linking β-sheets k and l) which is relatively well conserved throughout the JEV serocomplex of flaviviruses. Interestingly, both WNV and KUN contain a hydrophilic Asn residue at E-277, making the resultant SSNT motif identical to that present in CDV-1-51v2 (S→N). All of these viruses are of high NI and NV in mice. It therefore appears likely that the functional basis for attenuation caused by mutations at E-277 is disruption of the β-turn, which on the basis of the three-dimensional structure of the protein appears to form an integral part of the hinge region.
Despite the inferences drawn above, the specific effect of mutations at E-277 is difficult to ascertain. The inability of CDV-1-51v1 (S→I) to hemagglutinate RBCs at low pH and the observed reduction of this ability in both CDV-1-51v3 (S→V) and CDV-1-51v4 (S→P) suggests that a defect in fusion activity suggested by McMinn et al. (47) is responsible for the observed phenotypes. In the aforementioned study, BHv1 [E-277 (S→I)] was also observed to be less efficient in fusion-from-within assays, lending further support for reduced fusion activity in viruses with hydrophobic amino acid substitutions at E-277.
With the three-dimensional structure of the TBE E protein now known (60), it is possible to use this structure as a basis for modeling similar proteins from related flaviviruses, such as MVE. Threading of the MVE E protein sequence onto the known structure of the TBE E protein and subsequent energy minimization of this basic model shows a very high degree of structural similarity between the two proteins. This structural homology is likely to be paralleled by a functional homology which includes a substantial rearrangement of the protein during its transition from dimer to trimer at low pH. In the mechanism proposed by Rey et al. (60), mobility in the hinge region is likely to project the conserved hydrophobic fusion peptide upwards for participation in fusion with the endosomal membrane, a mechanism analogous to that proposed for members of other virus families, including paramyxoviruses (3), orthomyxoviruses (5), and filoviruses (71).
Similarities between the model proposed by Rey et al. (60) for TBE and that observed for other viruses are evident. Viral fusion proteins appear to undergo significant structural rearrangement at low pH, including a shift from dimer to trimer. In addition, mutations in regions which are reorganized during the dimer-to-trimer transition can increase the optimal pH for fusion in both viruses, reflecting a disruption of normal fusion activity. For example, substitutions at positions 55 or 71 of the HA2 subunit of the influenza A virus HA protein are sufficient to shift the optimal pH for fusion 0.6 point up from 5.1 to 5.7 (58, 66). Similarly, mutations at E-153 of DEN-2 have been shown to elevate the pH threshold of fusion (22), as did mutations at E-277 of MVE (S→V and S→P) in this study. It is possible that these substitutions disrupt the stability of the protein, lowering the energy barrier between the metastable native state and the more stable final conformation and allowing conformational change to occur at higher pH.
By combining the model for dimer-to-trimer transition outlined by Allison et al. (1) with that of defective fusion in the endosome at low pH described by McMinn (45), hypothetical models for the basis of attenuation caused by mutations in the hinge region can be postulated. For example, limited mobility in the hinge region (E-277) may prevent correct presentation of the buried fusion peptide on the tip of each protein in the homotrimer. Alternatively, undue stress may be placed on the receptor binding site, causing premature release of the virion from the receptor just prior to fusion. Receptor binding is an important part of the viral entry process and is likely to be essential for holding the viral and cellular membranes in close proximity for initiation of the fusion reaction. In human parainfluenza virus type 3, the binding of hemagglutinin-neuraminidase to its sialic acid receptor is essential for the fusion process (51). Furthermore, increased avidity of the receptor-ligand interaction correlates with increased fusogenicity, as evidenced by the introduction of site-directed mutations into the sialic acid binding site of hemagglutinin-neuraminidase (52). In contrast, cleavage of the hemagglutinin-esterase protein of influenza C virus from its receptor is a prerequisite for the low pH-triggered conformational change required for fusion (67). Whether this is the case in flaviviruses or whether ongoing receptor binding in the endosome is required for fusion to occur remains to be determined. McMinn (45) and Corver et al. (16) have, however, shown that the presence of a receptor is not required for fusion of MVE or TBE with target liposomes. Furthermore, the attenuated BHv1 strain of MVE was able to fuse to liposomes with equal efficiency to wild-type virus, suggesting that the defective fusion phenotype of BHv1 may be influenced by a dynamic interaction between the E protein, the receptor, and the target membrane (45). Given that preexposure of TBE to acidic pH results in a loss of infectivity and fusogenicity (presumably due to an irreversible structural rearrangement of the E protein) (16), evidence suggests that the fusion active state of the E protein is transient and that the receptor, which is dispensable for the fusion process itself, may be required to orient the endosomal membrane with a transitional form of the E protein. If this were the case, premature release of the virion from its receptor would allow the E protein to assume a final “fusion-inactive” conformation before it had a chance to interact with the endosomal membrane.
Mutations in the RGD motif.
Mutations were introduced into the RGD motif at position E-390 of MVE (on the lateral face of domain III of the E protein) to gain further insight into the role of this region in receptor binding. Evidence for the involvement of the lateral face of domain III in receptor binding is compelling but for the most part is based solely on the observed structure of the region (60). Direct experimental evidence is limited to the observation that partial-length C-terminal E protein constructs of DEN-2 (including residues 281 to 423) have potent cell binding activity, while N-terminal constructs do not (12). Whether the RGD motif in mosquito-borne flaviviruses plays an important role in binding to host cell GAGs or integrins and whether these serve as receptors for virus entry is difficult to ascertain. The RGD motif is not present in any of the DEN viruses, and these viruses are able to bind heparin with greater affinity than MVE (see reference 39 and work presented in this study). Integrin binding is further complicated by the fact that motifs other than RGD have been implicated in the process. Motifs such as EILDV (29) and IDAPS (70) are involved in the binding of fibronectin to α4β1 integrins. Similarly, DGEA-containing peptides are capable of inhibiting the binding of collagen to α2β1 integrins, suggesting that this motif may also play a role (65).
Regardless of whether integrins are involved in flavivirus entry, it is clear that RGD-dependent binding to host cell integrins is not an important determinant of virulence in flaviviruses. While the D→N and D→Y substitutions at E-390 of MVE caused a complete loss of NI in the mouse model, coupled with attenuated replication kinetics in vitro and in vivo, the D→E substitution had no effect on viral phenotype. Integrin binding should be severely affected by such a mutation, as evidenced by studies of FMDV where disruption of the RGD motif by R→K and/or D→E substitutions has been shown to disrupt RGD-dependent binding to host cell integrins (44). The presence of an RGE motif in WNV (72) and KUN (15), both of which are highly virulent in mice, plus the observation that all of the E-390 mutants derived in this study were able to adsorb and penetrate host cells with equal efficiency to wild-type virus, suggests that the RGD motif is not essential for virus binding. This does not rule out integrin binding as a means of host cell entry by flaviviruses; rather, it suggests that RGD-dependent binding to host cell integrins is not a major pathway for flavivirus entry.
In contrast to the hinge region of the E protein, the lateral face of domain III is strongly hydrophilic. As such, it is possible that the introduction of a large hydrophobic Tyr residue [CDV-1-51v7 (D→Y)] may destabilize the FG loop (nomenclature of Rey et al. [60]). Alternatively, the replacement of a negatively charged Asp residue with an uncharged Tyr or Asn residue could affect the formation of a functionally important salt bridge. Formation of such a bridge has recently been shown to be an important determinant of virulence in TBE. Based on the three-dimensional structure of the TBE E protein, an Asp residue at E-308 (Asp-308) is believed to form a salt bridge with a Lys residue at E-311 (60). Replacement of Asp-308 with a Lys residue resulted in a virus which was highly unstable, and passage of this virus in baby mouse brain resulted in spontaneous reversion of the replacement Lys to a Glu residue (42). Interestingly, reversion to a negatively charged Glu residue required only a single nucleotide change, while reversion to the wild-type Asp would have required two such changes. It therefore seems evident that the virus took the shortest route possible to restore the salt bridge between residues E-308 and E-311. Confirmation of whether a salt bridge involving E-390 (in MVE) exists will require elucidation of the three-dimensional structure of the MVE E protein; however, at least three positively charged His residues are in close proximity to E-390: His-395, His-396, and His-398. Furthermore, the Arg residue which forms part of the RGD motif is also positively charged. It is entirely possible that one of these four residues could participate in the formation of a functionally important salt bridge in the MVE E protein. The instability of the Asn substitution in CDV-1-51v5 (D→N), as evidenced by its reversion to a wild-type Asp residue after passage in Vero cells, is reminiscent of the reversion observed in the Mandl et al. study (42). Furthermore, if a functionally important salt bridge were playing a role in this region of the MVE E protein, a Glu residue at E-390 would be expected to functionally substitute for an Asp residue, as demonstrated for CDV-1-51v6 (D→E), which had an almost identical phenotype to that of clone-derived wild-type virus.
Since mutations in the RGD motif of MVE do not appear to affect the ability of virus to bind host cells, it seems likely that this motif is not functionally important in receptor binding. Disruption of the motif had little to no effect on the heparin binding ability of the virus, as evidenced by heparin inhibition assays which showed approximately 40% inhibition for all viruses produced during the study. Incomplete inhibition by heparin suggests that receptors other than GAGs can serve as mediators of viral entry.
Variation in the amount of HS expressed on different cell types, as well as the degree of sulfation of HS, may go some way towards explaining the different levels of inhibition by heparin seen in previous studies. Lee and Lobigs (39) have shown that inhibition of MVE binding by soluble heparin is low in Vero cells and high in BHK-21 cells. In addition, Chen et al. (13) have shown that highly sulfated HS is capable of significantly inhibiting the binding of DEN-2, while low-sulfate HS is not. Similar work on respiratory syncytial virus has shown that the interaction of virus with cell surface GAGs is not based on a simple charge interaction but rather a specific GAG structural configuration including N-sulfation and iduronic acid (25). Thus, binding of flaviviruses to host cells is likely to be a complicated process involving multiple receptors with various levels of affinity. The use of such receptors may depend on their relative availability on the host cell, as well as whether these receptors have been posttranslationally modified in a way amenable to virus binding.
Aside from receptor binding, it is possible that mutations at E-390 could affect virulence by disrupting the conformation of the E protein in much the same way as that described for the hinge region. Recent work by van der Most et al. (69), involving SDM of the RGD motif of YF, has shown that viruses containing Arg→Thr, Gly→Ala, or Asp→Glu/Ser substitutions at E-390 are able to bind to and infect both SW-13 and C6/36 cells. In addition, RGD-containing peptides did not inhibit infection of primary chicken embryo fibroblasts by YF-17D (Preugschat and Strauss, unpublished results cited by van der Most et al. [69]). In the van der Most et al. study (69), the explanation for the observed phenotypes was instability in the E protein. Intracellular levels of the E protein were considerably lower in viruses with RGD motif mutations; however, this instability could be overcome by incubation of infected cell cultures at a suboptimal temperature (30°C) (69). This prompted the authors to suggest that the nature of attenuating mutations in the FG loop of flaviviruses may be to cause incorrect folding of the protein at a posttranslational stage. Incorrectly folded E proteins may be defective in their ability to interact with prM or another chaperone protein, resulting in their retention in the endoplasmic reticulum and eventual degradation. Such retention has been observed in cells expressing misfolded HA of influenza A virus (19). The suggestion that attenuation of flaviviruses caused by mutations in the RGD motif are caused not by altered receptor binding but by posttranslational instability of the E protein is an interesting one and warrants further investigation. It may be that the attenuation of MVE mutants with substitutions at E-390 has the same functional basis as that described for similar mutants of YF.
REFERENCES
- 1.Allison S L, Schalich J, Stiasny K, Mandl C W, Kunz C, Heinz F X. Oligomeric rearrangement of tick-borne encephalitis virus envelope proteins induced by an acidic pH. J Virol. 1995;69:695–700. doi: 10.1128/jvi.69.2.695-700.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arroyo J, Guirakhoo F, Fenner S, Zhang Z X, Monath T P, Chambers T J. Molecular basis for attenuation of neurovirulence of a yellow fever virus/Japanese encephalitis virus chimera vaccine (ChimeriVax-JE) J Virol. 2001;75:934–942. doi: 10.1128/JVI.75.2.934-942.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker K A, Dutch R E, Lamb R A, Jardetzky T S. Structural basis for paramyxovirus-mediated membrane fusion. Mol Cell. 1999;3:309–319. doi: 10.1016/s1097-2765(00)80458-x. [DOI] [PubMed] [Google Scholar]
- 4.Bray M, Men R, Tokimatsu I, Lai C J. Genetic determinants responsible for acquisition of dengue type 2 virus mouse neurovirulence. J Virol. 1998;72:1647–1651. doi: 10.1128/jvi.72.2.1647-1651.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bullough P A, Hughson F M, Skehel J J, Wiley D C. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature. 1994;371:37–43. doi: 10.1038/371037a0. [DOI] [PubMed] [Google Scholar]
- 6.Cahour A, Pletnev A, Vazielle-Falcoz M, Rosen L, Lai C J. Growth-restricted dengue virus mutants containing deletions in the 5′ noncoding region of the RNA genome. Virology. 1995;207:68–76. doi: 10.1006/viro.1995.1052. [DOI] [PubMed] [Google Scholar]
- 7.Cecilia D, Gould E A. Nucleotide changes responsible for loss of neuroinvasiveness in Japanese encephalitis virus neutralization-resistant mutants. Virology. 1991;181:70–77. doi: 10.1016/0042-6822(91)90471-m. [DOI] [PubMed] [Google Scholar]
- 8.Chambers T J, Nestorowicz A, Mason P W, Rice C M. Yellow fever Japanese encephalitis chimeric viruses: construction and biological properties. J Virol. 1999;73:3095–3101. doi: 10.1128/jvi.73.4.3095-3101.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chambers T J, Nestorowicz A, Rice C M. Mutagenesis of the yellow fever virus NS2B/3 cleavage site: determinants of cleavage site specificity and effects on polyprotein processing and viral replication. J Virol. 1995;69:1600–1605. doi: 10.1128/jvi.69.3.1600-1605.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chambers T J, Weir R C, Grakoui A, McCourt D W, Bazan J F, Fletterick R J, Rice C M. Evidence that the N-terminal domain of nonstructural protein NS3 from yellow fever virus is a serine protease responsible for site-specific cleavages in the viral polyprotein. Proc Natl Acad Sci USA. 1990;87:8898–8902. doi: 10.1073/pnas.87.22.8898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen L K, Lin Y L, Liao C L, Lin C G, Huang Y L, Yeh C T, Lai S C, Jan J T, Chin C. Generation and characterization of organ-tropism mutants of Japanese encephalitis virus in vivo and in vitro. Virology. 1996;223:79–88. doi: 10.1006/viro.1996.0457. [DOI] [PubMed] [Google Scholar]
- 12.Chen Y, Maguire T, Marks R M. Demonstration of binding of dengue virus envelope protein to target cells. J Virol. 1996;70:8765–8772. doi: 10.1128/jvi.70.12.8765-8772.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Y P, Maguire T, Hileman R E, Fromm J R, Esko J D, Linhardt R J, Marks R M. Dengue virus infectivity depends on envelope protein binding to target cell heparan sulfate. Nat Med. 1997;3:866–871. doi: 10.1038/nm0897-866. [DOI] [PubMed] [Google Scholar]
- 14.Clark D H, Casals J. Techniques for hemagglutination and hemagglutination-inhibition with arthropod-borne viruses. Am J Trop Med Hyg. 1958;7:561–573. doi: 10.4269/ajtmh.1958.7.561. [DOI] [PubMed] [Google Scholar]
- 15.Coia G, Parker M D, Speight G, Byrne M E, Westaway E G. Nucleotide and complete amino acid sequences of Kunjin virus: definitive gene order and characteristics of the virus-specified proteins. J Gen Virol. 1988;69:1–21. doi: 10.1099/0022-1317-69-1-1. [DOI] [PubMed] [Google Scholar]
- 16.Corver J, Ortiz A, Allison S L, Schalich J, Heinz F X, Wilschut J. Membrane fusion activity of tick-borne encephalitis virus and recombinant subviral particles in a liposomal model system. Virology. 2000;269:37–46. doi: 10.1006/viro.1999.0172. [DOI] [PubMed] [Google Scholar]
- 17.Coulson B S, Londrigan S L, Lee D J. Rotavirus contains integrin ligand sequences and a disintegrin-like domain that are implicated in virus entry into cells. Proc Natl Acad Sci USA. 1997;94:5389–5394. doi: 10.1073/pnas.94.10.5389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dmitriev I, Krasnykh V, Miller C R, Wang M, Kashentseva E, Mikheeva G, Belousova N, Curiel D T. An adenovirus vector with genetically modified fibers demonstrates expanded tropism via utilization of a coxsackievirus and adenovirus receptor-independent cell entry mechanism. J Virol. 1998;72:9706–9713. doi: 10.1128/jvi.72.12.9706-9713.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gething M J, McCammon K, Sambrook J. Expression of wild-type and mutant forms of influenza hemagglutinin: the role of folding in intracellular transport. Cell. 1986;46:939–950. doi: 10.1016/0092-8674(86)90076-0. [DOI] [PubMed] [Google Scholar]
- 20.Gualano R C, Pryor M J, Cauchi M R, Wright P J, Davidson A D. Identification of a major determinant of mouse neurovirulence of dengue virus type 2 using stably cloned genomic-length cDNA. J Gen Virol. 1998;79:437–446. doi: 10.1099/0022-1317-79-3-437. [DOI] [PubMed] [Google Scholar]
- 21.Guex N, Peitsch M C. SWISS-MODEL and the Swiss-PdbViewer: an environment for comparative protein modeling. Electrophoresis. 1997;18:2714–2723. doi: 10.1002/elps.1150181505. [DOI] [PubMed] [Google Scholar]
- 22.Guirakhoo F, Hunt A R, Lewis J G, Roehrig J T. Selection and partial characterization of dengue 2 virus mutants that induce fusion at elevated pH. Virology. 1993;194:219–223. doi: 10.1006/viro.1993.1252. [DOI] [PubMed] [Google Scholar]
- 23.Guirakhoo F, Weltzin R, Chambers T J, Zhang Z X, Soike K, Ratterree M, Arroyo J, Georgakopoulos K, Catalan J, Monath T P. Recombinant chimeric yellow fever-dengue type 2 virus is immunogenic and protective in nonhuman primates. J Virol. 2000;74:5477–5485. doi: 10.1128/jvi.74.12.5477-5485.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guirakhoo F, Zhang Z X, Chambers T J, Delagrave S, Arroyo J, Barrett A D T, Monath T P. Immunogenicity, genetic stability, and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (ChimeriVax-JE) as a live, attenuated vaccine candidate against Japanese encephalitis. Virology. 1999;257:363–372. doi: 10.1006/viro.1999.9695. [DOI] [PubMed] [Google Scholar]
- 25.Hallak L K, Spillmann D, Collins P L, Peeples M E. Glycosaminoglycan sulfation requirements for respiratory syncytial virus infection. J Virol. 2000;74:10508–10513. doi: 10.1128/jvi.74.22.10508-10513.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hasegawa H, Yoshida M, Shiosaka T, Fujita S, Kobayashi Y. Mutations in the envelope protein of Japanese encephalitis virus affect entry into cultured cells and virulence in mice. Virology. 1992;191:158–165. doi: 10.1016/0042-6822(92)90177-q. [DOI] [PubMed] [Google Scholar]
- 27.Hilgard P, Stockert R. Heparan sulfate proteoglycans initiate dengue virus infection of hepatocytes. Hepatology. 2000;32:1069–1077. doi: 10.1053/jhep.2000.18713. [DOI] [PubMed] [Google Scholar]
- 28.Hiramatsu K, Tadano M, Men R, Lai C J. Mutational analysis of a neutralization epitope on the dengue type 2 virus (DEN2) envelope protein: monoclonal antibody resistant DEN2/DEN4 chimeras exhibit reduced mouse neurovirulence. Virology. 1996;224:437–445. doi: 10.1006/viro.1996.0550. [DOI] [PubMed] [Google Scholar]
- 29.Humphries M J, Akiyama S K, Komoriya A, Olden K, Yamada K M. Neurite extension of chicken peripheral nervous system neurons on fibronectin: relative importance of specific adhesion sites in the central cell-binding domain and the alternatively spliced type III connecting segment. J Cell Biol. 1988;106:1289–1297. doi: 10.1083/jcb.106.4.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hung S L, Lee P L, Chen H W, Chen L K, Kao C L, King C C. Analysis of the steps involved in dengue virus entry into host cells. Virology. 1999;257:156–167. doi: 10.1006/viro.1999.9633. [DOI] [PubMed] [Google Scholar]
- 31.Hurrelbrink R J, Nestorowicz A, McMinn P C. Characterization of infectious Murray Valley encephalitis virus derived from a stably cloned genome-length cDNA. J Gen Virol. 1999;80:3115–3125. doi: 10.1099/0022-1317-80-12-3115. [DOI] [PubMed] [Google Scholar]
- 32.Jackson T, Sharma A, Abughazaleh R, Blakemore W E, Ellard F M, Simmons D L, Newman J W I, Stuart D I, King A M Q. Arginine-glycine aspartic acid-specific binding by foot-and-mouth disease viruses to the purified integrin alpha-v-beta-3 in vitro. J Virol. 1997;71:8357–8361. doi: 10.1128/jvi.71.11.8357-8361.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kawano H, Rostapshov V, Rosen L, Lai C J. Genetic determinants of dengue type 4 virus neurovirulence for mice. J Virol. 1993;67:6567–6575. doi: 10.1128/jvi.67.11.6567-6575.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khromykh A A, Kenney M T, Westaway E G. trans-Complementation of flavivirus RNA polymerase gene NS5 by using Kunjin virus replicon-expressing BHK cells. J Virol. 1998;72:7270–7279. doi: 10.1128/jvi.72.9.7270-7279.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khromykh A A, Sedlak P L, Guyatt K J, Hall R A, Westaway E G. Efficient trans-complementation of the flavivirus Kunjin NS5 protein but not of the NS1 protein requires its coexpression with other components of the viral replicase. J Virol. 1999;73:10272–10280. doi: 10.1128/jvi.73.12.10272-10280.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khromykh A A, Sedlak P L, Westaway E G. trans-Complementation analysis of the flavivirus Kunjin NS5 gene reveals an essential role for translation of its N-terminal half in RNA replication. J Virol. 1999;73:9247–9255. doi: 10.1128/jvi.73.11.9247-9255.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khromykh A A, Westaway E G. Completion of Kunjin virus RNA sequence and recovery of an infectious RNA transcribed from stably cloned full-length cDNA. J Virol. 1994;68:4580–4588. doi: 10.1128/jvi.68.7.4580-4588.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lai C J, Bray M, Men R, Cahour A, Chen W, Kawano H, Tadano M, Hiramatsu K, Tokimatsu I, Pletnev A, Arakai S, Shameem G, Rinaudo M. Evaluation of molecular strategies to develop a live dengue vaccine. Clin Diagn Virol. 1998;10:173–179. doi: 10.1016/s0928-0197(98)00035-x. [DOI] [PubMed] [Google Scholar]
- 39.Lee E, Lobigs M. Substitutions at the putative receptor-binding site of an encephalitic flavivirus alter virulence and host cell tropism and reveal a role for glycosaminoglycans in entry. J Virol. 2000;74:8867–8875. doi: 10.1128/jvi.74.19.8867-8875.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lobigs M, Usha R, Nestorowicz A, Marshall I D, Weir R C, Dalgarno L. Host cell selection of Murray Valley encephalitis virus variants altered at an RGD sequence in the envelope protein and in mouse virulence. Virology. 1990;176:587–595. doi: 10.1016/0042-6822(90)90029-q. [DOI] [PubMed] [Google Scholar]
- 41.Mackenzie J S, Broom A K. Australian X disease, Murray Valley encephalitis and the French connection. Vet Microbiol. 1995;46:79–90. doi: 10.1016/0378-1135(95)00074-k. [DOI] [PubMed] [Google Scholar]
- 42.Mandl C W, Allison S L, Holzmann H, Meixner T, Heinz F X. Attenuation of tick-borne encephalitis virus by structure-based site-specific mutagenesis of a putative flavivirus receptor binding site. J Virol. 2000;74:9601–9609. doi: 10.1128/jvi.74.20.9601-9609.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mandl C W, Holzmann H, Meixner T, Rauscher S, Stadler P F, Allison S L, Heinz F X. Spontaneous and engineered deletions in the 3′ noncoding region of tick-borne encephalitis virus—construction of highly attenuated mutants of a flavivirus. J Virol. 1998;72:2132–2140. doi: 10.1128/jvi.72.3.2132-2140.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mason P W, Rieder E, Baxt B. RGD sequence of foot-and-mouth disease virus is essential for infecting cells via the natural receptor but can be bypassed by an antibody-dependent enhancement pathway. Proc Natl Acad Sci USA. 1994;91:1932–1936. doi: 10.1073/pnas.91.5.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McMinn P C. Studies on the molecular pathogenesis of Murray Valley encephalitis infection of mice. Ph.D. thesis. Canberra: Australian National University; 1994. [Google Scholar]
- 46.McMinn P C, Lee E, Hartley S, Roehrig J T, Dalgarno L, Weir R C. Murray valley encephalitis virus envelope protein antigenic variants with altered hemagglutination properties and reduced neuroinvasiveness in mice. Virology. 1995;211:10–20. doi: 10.1006/viro.1995.1374. [DOI] [PubMed] [Google Scholar]
- 47.McMinn P C, Weir R C, Dalgarno L. A mouse-attenuated envelope protein variant of Murray Valley encephalitis virus with altered fusion activity. J Gen Virol. 1996;77:2085–2088. doi: 10.1099/0022-1317-77-9-2085. [DOI] [PubMed] [Google Scholar]
- 48.Men R, Bray M, Clark D, Chanock R M, Lai C J. Dengue type 4 virus mutants containing deletions in the 3′ noncoding region of the RNA genome: analysis of growth restriction in cell culture and altered viremia pattern and immunogenicity in rhesus monkeys. J Virol. 1996;70:3930–3937. doi: 10.1128/jvi.70.6.3930-3937.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Monath T P, Levenbook I, Soike K, Zhang Z X, Ratterree M, Draper K, Barrett A D, Nichols R, Weltzin R, Arroyo J, Guirakhoo F. Chimeric yellow fever virus 17D-Japanese encephalitis virus vaccine: dose-response effectiveness and extended safety testing in rhesus monkeys. J Virol. 2000;74:1742–1751. doi: 10.1128/jvi.74.4.1742-1751.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Monath T P, Soike K, Levenbook I, Zhang Z X, Arroyo J, Delagrave S, Myers G, Barrett A D T, Shope R E, Ratterree M, Chambers T J, Guirakhoo F. Recombinant, chimaeric live, attenuated vaccine (ChimeriVax (TM)) incorporating the envelope genes of Japanese encephalitis (SA14-14-2) virus and the capsid and nonstructural genes of yellow fever (17D) virus is safe, immunogenic and protective in nonhuman primates. Vaccine. 1999;17:1869–1882. doi: 10.1016/s0264-410x(98)00487-3. [DOI] [PubMed] [Google Scholar]
- 51.Moscona A, Peluso R W. Fusion properties of cells persistently infected with human parainfluenza virus type 3: participation of hemagglutinin-neuraminidase in membrane fusion. J Virol. 1991;65:2773–2777. doi: 10.1128/jvi.65.6.2773-2777.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moscona A, Peluso R W. Relative affinity of the human parainfluenza virus type 3 hemagglutinin-neuraminidase for sialic acid correlates with virus-induced fusion activity. J Virol. 1993;67:6463–6468. doi: 10.1128/jvi.67.11.6463-6468.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Muylaert I R, Chambers T J, Galler R, Rice C M. Mutagenesis of the N-linked glycosylation sites of the yellow fever virus NS1 protein: effects on virus replication and mouse neurovirulence. Virology. 1996;222:159–168. doi: 10.1006/viro.1996.0406. [DOI] [PubMed] [Google Scholar]
- 54.Nestorowicz A, Chambers T J, Rice C M. Mutagenesis of the yellow fever virus NS2A/2B cleavage site: effects on proteolytic processing, viral replication, and evidence for alternative processing of the NS2A protein. Virology. 1994;199:114–123. doi: 10.1006/viro.1994.1103. [DOI] [PubMed] [Google Scholar]
- 55.Pletnev A G, Bray M, Lai C J. Chimeric tick-borne encephalitis and dengue type 4 viruses: effects of mutations on neurovirulence in mice. J Virol. 1993;67:4956–4963. doi: 10.1128/jvi.67.8.4956-4963.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Porterfield J S, Rowe C E. Haemagglutination with arthropod-borne viruses and its inhibition with certain phospholipids. Virology. 1960;188:160–167. doi: 10.1016/0042-6822(60)90119-7. [DOI] [PubMed] [Google Scholar]
- 57.Pryor M J, Gualano R C, Lin B, Davidson A D, Wright P J. Growth restriction of dengue virus type 2 by site-specific mutagenesis of virus-encoded glycoproteins. J Gen Virol. 1998;79:2631–2639. doi: 10.1099/0022-1317-79-11-2631. [DOI] [PubMed] [Google Scholar]
- 58.Qiao H, Pelletier S L, Hoffman L, Hacker J, Armstrong R T, White J M. Specific single or double proline substitutions in the “spring-loaded” coiled-coil region of the influenza hemagglutinin impair or abolish membrane fusion activity. J Cell Biol. 1998;141:1335–1347. doi: 10.1083/jcb.141.6.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reed L J, Muench H. A simple method of estimating fifty percent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 60.Rey F A, Heinz F X, Mandl C, Kunz C, Harrison S C. The envelope glycoprotein from tick-borne encephalitis virus at 2 Å resolution. Nature. 1995;375:291–298. doi: 10.1038/375291a0. [DOI] [PubMed] [Google Scholar]
- 61.Rice C M. Flaviviridae: the viruses and their replication. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven; 1996. pp. 931–959. [Google Scholar]
- 62.Sayle R A, Milner-White E J. RASMOL: biomolecular graphics for all. Trends Biochem Sci. 1995;20:374. doi: 10.1016/s0968-0004(00)89080-5. [DOI] [PubMed] [Google Scholar]
- 63.Schlesinger J J, Chapman S, Nestorowicz A, Rice C M, Ginocchio T E, Chambers T J. Replication of yellow fever virus in the mouse central nervous system: comparison of neuroadapted and non-neuroadapted virus and partial sequence analysis of the neuroadapted strain. J Gen Virol. 1996;77:1277–1285. doi: 10.1099/0022-1317-77-6-1277. [DOI] [PubMed] [Google Scholar]
- 64.Sharma A, Rao Z, Fry E, Booth T, Jones E Y, Rowlands D J, Simmons D L, Stuart D I. Specific interactions between human integrin alpha v beta 3 and chimeric hepatitis B virus core particles bearing the receptor-binding epitope of foot-and-mouth disease virus. Virology. 1997;239:150–157. doi: 10.1006/viro.1997.8833. [DOI] [PubMed] [Google Scholar]
- 65.Staatz W D, Fok K F, Zutter M M, Adams S P, Rodriguez B A, Santoro S A. Identification of a tetrapeptide recognition sequence for the alpha 2 beta 1 integrin in collagen. J Biol Chem. 1991;266:7363–7367. [PubMed] [Google Scholar]
- 66.Steinhauer D A, Martin J, Lin Y P, Wharton S A, Oldstone M B, Skehel J J, Wiley D C. Studies using double mutants of the conformational transitions in influenza hemagglutinin required for its membrane fusion activity. Proc Natl Acad Sci USA. 1996;93:12873–12878. doi: 10.1073/pnas.93.23.12873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Strobl B, Vlasak R. The receptor-destroying enzyme of influenza C virus is required for entry into target cells. Virology. 1993;192:679–682. doi: 10.1006/viro.1993.1087. [DOI] [PubMed] [Google Scholar]
- 68.Sumiyoshi H, Tignor G H, Shope R E. Characterization of a highly attenuated Japanese encephalitis virus generated from molecularly cloned cDNA. J Infect Dis. 1995;171:1144–1151. doi: 10.1093/infdis/171.5.1144. [DOI] [PubMed] [Google Scholar]
- 69.van der Most R G, Corver J, Strauss J H. Mutagenesis of the RGD motif in the yellow fever virus 17D envelope protein. Virology. 1999;265:83–95. doi: 10.1006/viro.1999.0026. [DOI] [PubMed] [Google Scholar]
- 70.Wayner E A, Garcia-Pardo A, Humphries M J, McDonald J A, Carter W G. Identification and characterization of the T lymphocyte adhesion receptor for an alternative cell attachment domain (CS-1) in plasma fibronectin. J Cell Biol. 1989;109:1321–1330. doi: 10.1083/jcb.109.3.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weissenhorn W, Dessen A, Calder L J, Harrison S C, Skehel J J, Wiley D C. Structural basis for membrane fusion by enveloped viruses. Mol Membr Biol. 1999;16:3–9. doi: 10.1080/096876899294706. [DOI] [PubMed] [Google Scholar]
- 72.Wengler G, Castle E, Leidner U, Nowak T, Wengler G. Sequence analysis of the membrane protein V3 of the flavivirus West Nile virus and of its gene. Virology. 1985;147:264–274. doi: 10.1016/0042-6822(85)90129-1. [DOI] [PubMed] [Google Scholar]
- 73.Wickham T J, Carrion M E, Kovesdi I. Targeting of adenovirus penton base to new receptors through replacement of its RGD motif with other receptor-specific peptide motifs. Gene Ther. 1995;2:750–756. [PubMed] [Google Scholar]
- 74.Wickham T J, Mathias P, Cheresh D A, Nemerow G R. Integrins alpha v beta 3 and alpha v beta 5 promote adenovirus internalization but not virus attachment. Cell. 1993;73:309–319. doi: 10.1016/0092-8674(93)90231-e. [DOI] [PubMed] [Google Scholar]
- 75.Wright A J, Phillpotts R J. Humane endpoints are an objective measure of morbidity in Venezuelan encephalomyelitis virus infection of mice. Arch Virol. 1998;143:1155–1162. doi: 10.1007/s007050050363. [DOI] [PubMed] [Google Scholar]
- 76.Zimmermann H, Eggers H J, Nelsen-Salz B. Cell attachment and mouse virulence of echovirus 9 correlate with an RGD motif in the capsid protein VP1. Virology. 1997;233:149–156. doi: 10.1006/viro.1997.8601. [DOI] [PubMed] [Google Scholar]