Abstract
Background
Transgender individuals frequently undergo gender-affirming hormone therapy (GAHT) during their gender transition which plays a vital role in gender identity affirmation. Cholelithiasis, a common condition affecting 10-15% of the US population, has been linked to estrogen therapy in cisgender women. Despite the fact that hormonal profiles achieved after GAHT are not always identical to cisgender individuals, the effects of GAHT on gallbladder disease (GBD) risk have not been evaluated in transgender populations. This research aims to address this gap utilizing a large nationwide database.
Methods
The study analyzed medical records data from the TrinetX database from 52,847 trans men and 38,114 trans women. Four cohorts were created: trans women and men either receiving either hormone therapy or no intervention. Descriptive statistics were calculated before matching to estimate disease burden. The groups were then propensity score matched on known risk factors (age, race, BMI, etc.) and rates of GBD were compared.
Results
Before matching, trans women on hormone therapy (TWHT) had a significantly higher 10-year GBD probability than those naïve to therapy (TWNI) (4.69% vs 1.88%). For trans men, there was no significant difference in 10-year rates between those on therapy (TMHT) and those not (TMNI) (3.15% vs 3.87%). Cholecystectomy rates were significantly higher for TWHT than TWNI (1.10% vs. 0.57%), but similar between TMHT and TMNI (0.95% vs. 1.10%). After accounting for risk factors, TWHT had increased GBD risk (HR 1.832), while TMHT showed no significant change.
Discussion
This study suggests a link between estrogen GAHT and increased GBD risk in transgender women. Notably, testosterone GAHT did not offer protection against GBD in transgender men, contrary to expectations. This study is, to our knowledge, the first to describe the burden of GBD in the transgender population and to investigate the effects of GAHT on GBD risk.
Keywords: Cholecystitis, cholelithiasis, estrogen, GAHT, HRT, testosterone
Introduction
Cholelithiasis, also known as gallstones, occurs when solid concretions, usually of cholesterol or bilirubin, form within the gallbladder. In the United States approximately 10–15% of the adult population has gallstones (Everhart et al., 1999). However, only one-third of individuals with gallstones experience symptoms, which occur when a gallstone obstructs the flow of bile into the biliary tree (Ahmed et al., 2000). While the mortality of gallstones is low at 0.6%, obstruction of the biliary tree by gallstones can result in complications including cholecystitis, choledocholithiasis, and cholangitis (Lammert et al., 2016).
Several well-documented risk factors contribute to gallstone formation including sex, age, race/ethnicity, obesity, rapid weight loss, pregnancy, and estrogen therapy (ET)(Pak & Lindseth, 2016). Among other mechanisms, estrogen increases biliary cholesterol secretion, which promotes the formation of cholesterol crystals and therefore gallstone formation (Uhler et al., 2000). Because of this, cisgender women are considered at higher risk of cholelithiasis than cisgender men due to their physiologically higher estrogen levels (Cirillo et al., 2005). The effect of hormone therapy on gallstone risk has not been explored in the context of gender-affirming therapy for transgender individuals.
In recent years, there is a growing recognition of transgender individuals, persons whose gender identity does not correspond with their sex assigned at birth (Meerwijk & Sevelius, 2017). Some transgender individuals choose to undergo gender-affirming interventions such as gender-affirming hormone therapy (GAHT) to align their body with their gender identity. Trans women (assigned male at birth) receive estrogen, often with an anti-androgen, while transgender men (assigned female at birth) are given testosterone. Gender affirming hormone therapy serves as a critical aspect of transgender healthcare and identity affirmation.
While the effect of ET on gallstone development has been extensively studied in cisgender women, with randomized control trials demonstrating an increased risk of gallbladder disease (Cirillo et al., 2005), there is a notable dearth of research exploring the effects of GAHT on gallstone development in trans women. Similarly, there has been no research into the effects of testosterone therapy on gallstone risk in transgender men. To our knowledge, there have been no studies that explored GAHT and gallstone disease in transgender populations.
The present study seeks to address this research gap by investigating the relationship between GAHT and gallbladder diseases in transgender patients. Through analysis of a large database, we aim to provide insights into gallstone-related complications in transgender patients undergoing GAHT, thereby contributing to a better understanding of the implications of hormone therapy in this specific population.
Materials and methods
Data source
We used US-based data from the network TriNetX (TriNetX, Inc., Cambridge, MA, United States), a multinational collaborative clinical research platform, that collects real-time medical records, including demographics, diagnoses, procedures, medications, laboratory values, and vital statuses. This network included 84 healthcare organizations at the time of analysis, including data from around 115.8 million patients. Sources of patient records were relatively evenly distributed across the United States (30% Northeast, 21% Midwest, 21% South and 27% West). The TriNetX platform uses aggregated counts and statistical summaries of de-identified information so that no protected health information or personal data are made available to users of the platform. Individuals with missing values for age at index were omitted from the data set. Data were extracted from the Research Network and analyzed on the TriNetX platform on June 23, 2023.
Study population
We queried the databank to select patients who identified as transgender based on the presence of ICD-10 codes indicating gender identity disorders (ICD-10 codes F64.0-F64.9). While chart review is the gold standard for identifying transgender patients in the medical record, studies demonstrate that ICD-10 based methods show a high specificity for identifying transgender patients in the EHR/EMR (Blosnich et al., 2018; Nik-Ahd et al., 2023; Proctor et al., 2016; Rich et al., 2021). We created 4 cohorts: trans women either receiving estrogen HT or no intervention (TWHT, TWNI) and trans men receiving testosterone therapy or no intervention (TMHT, TMNI). Estrogen and testosterone hormone therapy was defined using prescription codes and ICD-10 codes commonly used to denote GAHT (Appendix A). Patients were excluded from all groups who had a previous diagnosis of gallstone diseases or surgery affecting the biliary system before the index event. The index event for analysis was defined as 6 months past the earliest use of GAHT in the patient’s medical record for the HT groups, or 6 months after the first GID diagnosis in the NI groups.
Outcomes
The primary outcome was the rate of gallbladder disease, determined by ICD-10 codes denoting acute or chronic gallbladder inflammation or gallbladder or biliary tract stone disease (K80.0-8, K83.0-1,K81.0-9) (Cirillo et al., 2005). Secondary outcomes included rates of cholecystectomy, determined by CPT codes (Appendix A). The probability of each outcome was first evaluated in each cohort before matching using 1, 5, and 10 year Kaplan–Meier analysis in order to describe disease and surgical outcome burden. They were then compared between GAHT and non-GAHT groups post-matching to evaluate the potential effects of hormone therapy on gallstone disease risk.
Propensity score matching
Using 1:1 nearest neighbor propensity score matching (PSM) with a caliper of 0.1 times the pooled standard deviation of the propensity score, cohorts were matched on 27 gallstone disease-associated covariates including age, race, BMI, recent weight loss, alcohol and tobacco use, and presence of diabetes, HLD, and liver disease which were identified after comprehensive literature review. These covariates were identified using ICD-10 codes in the medical record prior to the index event. Following matching, standardized mean differences between the groups were < 0.035 for all covariates. Balance tables with full listed covariates are given (Appendix B).
Statistical analysis
The baseline characteristics for each group were compared with the chi-square test for categorical variables and the Student t-test for continuous variables. Before matching, Kaplan–Meier analysis was used to estimate the probability of gallbladder disease and surgical outcomes at 1 year, 5 years, and 10 years past the index event. Propensity score matching was then used to balance cohorts with baseline characteristics. In relation to outcome comparisons, we used the groups naïve to hormone therapy as the reference, comparing them with the hormone therapy groups. After matching, Kaplan–Meier analysis was performed to estimate the probability of outcomes after the index date from 1 day to the first instance of gallstones or the end of each patient’s record (censoring date). Comparisons between cohorts were made using a log-rank test. We calculated hazard ratios (HRs) and their associated 95% confidence intervals (CI) via a Cox proportional hazards model, together with the test for proportionality based on the scaled Schoenfeld residual, using R’s Survival package v3.2-3.
Statistical analyses were done within TriNetX. Statistical significance was set at a two-sided p-value of < 0.05.
Results
Baseline characteristics
We identified 52,847 trans men and 38,114 trans women. Within these groups, we identified 22,786 trans men using testosterone GAHT (TMHT), and 30,061 with no intervention (TMNI). There were 20,188 trans women on GAHT (TWHT) and 17,926 without (TWNI). The average time on treatment for individuals on GAHT was 853.4 d (SD 643.9, Range 1–7039) for trans men and 893.5 d (SD 810.7, Range 1–7353 d) for trans women.
The baseline characteristics of the cohorts are described in Table 1 and Appendix B. There were significant differences between TWHT and TWNI in rates of alcohol and nicotine dependence, as well as hyperlipidemia, cirrhosis, and NAFLD. Between TMHT and TMNI, there were significant differences in age at index, alcohol use disorder, Type 2 diabetes mellitus, hyperlipidemia, and NAFLD.
Outcomes
Before matching, the Kaplan–Meier showed that trans women receiving hormone therapy (TWHT) presented a significantly higher probability of all gallbladder disease outcomes at 1 year (0.38% vs 0.23%), 5 years (1.99% vs 1.08%), and 10 years (4.69% vs 1.88%), and cholelithiasis at 1 year (0.34% vs 0.21%), 5 years (1.83% vs 0.97%), and 10 years (4.26% vs 1.40%) compared to those without intervention (TWNI). For cholecystitis, the difference between TWHT and TWNI was significant only at the 1-year mark (0.10% vs 0.02%). For cholecystectomy, the rates were also significantly higher for TWHT at 1 year (0.11% vs 0.02%), 5 years (0.72% vs 0.34%), and 10 years (1.10% vs 0.57%).
In contrast, trans men on hormone therapy (TMHT) displayed probabilities of 0.30% at 1 year, 1.62% at 5 years, and 3.87% at 10 years for all GBD outcomes, versus 0.30%, 1.39%, and 3.15% respectively for trans men not receiving hormone therapy (TMNI), with no significant differences observed at any time point. There was also no significant difference observed for cholecystectomy at any time point between TMHT and TMNI. The full pre-matching probabilities of gallbladder disease and surgery at 1, 5, and 10 years after the index event are given (Table 2).
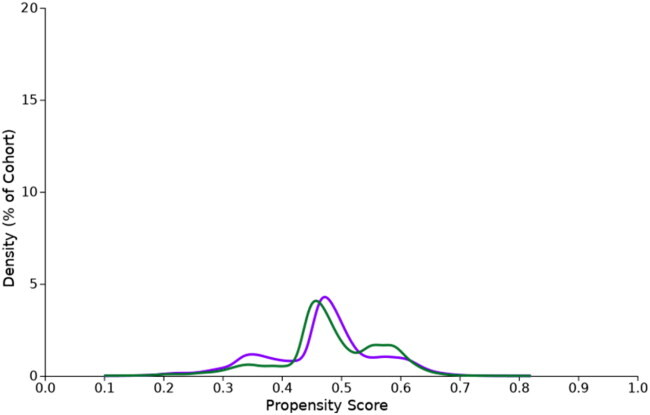
Following propensity score matching, cohort sizes were 15,900 (for both TWHT and TWNI) and 21,406 (for both TMHT and TMNI) with standardized mean differences between groups of below 0.035 for all covariates.
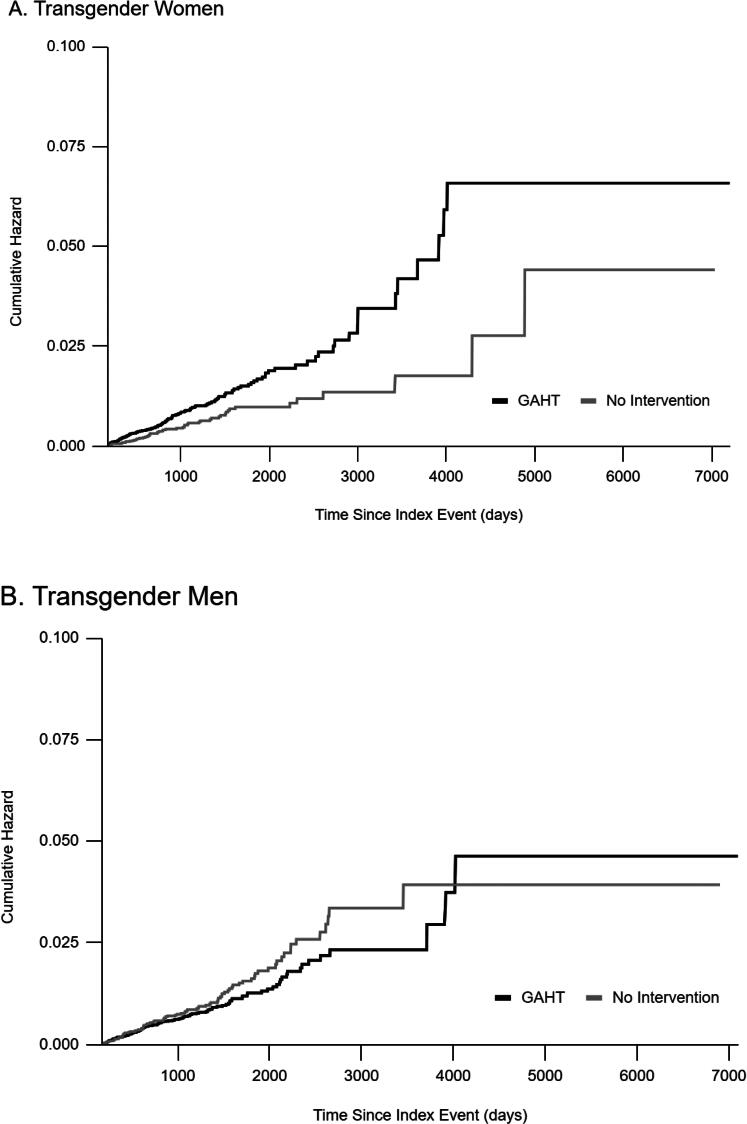
After matching, we observed that trans women who received GAHT were more likely to be diagnosed with gallbladder disease than those who did not receive GAHT (Table 3). Cox proportional hazards models revealed an 83.2% (HR 1.832, 95%CI: 1.324, 2.533) increased hazard for TWHT vs TWNI. The log-rank test revealed a χ2 of 13.795 with p = .0002 (Figure 1).
Among transgender men who received testosterone GAHT, we observed no significant difference in rates of gallbladder disease diagnoses. Cox proportional hazards models revealed an HR of 0.844 (0.95%CI: 0.645, 1.103) for TMHT vs TMNI. The log-rank test revealed a χ2 of 1.547 with p = .214 (Figure 1).
Discussion
In this study, we investigated the impact of Gender-Affirming Hormone Therapy (GAHT) on gallbladder disease rates in transgender patients. Cholelithiasis is common and leads to significant morbidity, mortality, and health care utilization in the United States and worldwide. Gallstones contribute to over 2.2 million ambulatory care visits and direct and indirect costs of over $6.5 billion annually (Unalp-Arida & Ruhl, 2022; Wadhwa et al., 2017). After adjusting for confounders, we found that transgender women on GAHT had a significantly higher likelihood of gallstone disease compared to those not on GAHT, while no such effect was seen in transgender men.
This is the first study to examine the relationship between hormone therapy and gallbladder disease in transgender individuals. To date, there have been two case reports published describing gallstone-related complications in transgender women (Freier et al. 2021, Tirthani et al. 2021). These case reports point to the administration of exogenous estrogen as a possible risk factor leading to the patients’ biliary disease.
The gallstone promoting effects of estrogen hormone therapy may be attributed to the influence of estrogen in lipid metabolism. Estrogen increases the amount of cholesterol relative to bile salts and lecithin in bile, increasing the saturation of bile with cholesterol, which leads to cholesterol crystal formation. Estrogen also alters bile acid composition, increasing the chance of gallstone formation (Uhler et al. 2000).
Our results are consistent with prior studies showing that estrogen therapy (ET) elevates the risk of gallstones in cisgender individuals. In a randomized, doubled-blind, placebo-controlled trial, Cirillo et al. found that ET was associated with a significant excess risk of cholecystitis ((HR, 1.80; nominal 95% CI, 1.42–2.28; p < .001) and cholelithiasis (HR, 1.86; nominal 95% CI, 1.48–2.35; p < .001) in a sample of post-menopausal cis-gender women (Cirillo et al., 2005). Similarly, the HERS-II study found a 48% increased risk of biliary tract surgery in cis women receiving ET (Hulley et al., 2002).
We observed no significant change in gallstone disease burden in transgender men, contradicting our hypothesis that testosterone therapy would lead to lower estrogen levels and therefore lowered gallstone risk. There is limited research on testosterone hormone therapy’s effects on gallbladder disease, although some studies suggest potential correlations between higher free testosterone levels and incident gallstone disease in cis males (Shabanzadeh, 2018; Squarza et al., 2018). One explanation could be that only about a third of trans men receiving GAHT experience a decrease in serum estradiol to cis male levels, indicating that testosterone GAHT alone may not be sufficient to decrease gallbladder disease risk in this group (Deutsch et al., 2015).
Our study’s strengths include a notably large cohort size, which is particularly important given the typically small samples in transgender research. This large sample allows us to examine rare outcomes in this population such as cholangitis. The dataset’s geographic and racial diversity adds to its representativeness. Moreover, our methodology effectively controls for various confounders, offering clearer insights into the relationship between GAHT and gallbladder disease in transgender people.
However, several limitations warrant acknowledgment. Propensity score matching may not entirely offset unmeasured or residual confounding. As with all studies using EMR data, the accuracy and completeness of the medical record is a potential source of error. Furthermore, healthcare access disparities among our population may contribute to underrepresentation of certain covariates and outcomes. An additional limitation is the possible sex assigned at birth misclassification in the TriNetX database. Though TriNetX offers a field denoting sex assigned at birth, it is possible that an individual’s identified gender may have been reported instead. Since sex assigned at birth carries a higher weight biologically when it comes to medical decisions, we believe most EMR systems still register patients with their sex assigned at birth. Due to TriNetX platform limitations, we couldn’t include a robust cisgender comparison group. As a result, our analysis is limited to comparing transgender groups with and without hormone therapy. Different criteria for follow-up between groups could introduce bias as different groups may have longer or shorter follow-up. The ICD-10 codes used offer high specificity but lower sensitivity, potentially omitting some members of the transgender population, though those identified are very likely to be transgender. (Blosnich et al., 2018; Nik-Ahd et al., 2023; Proctor et al., 2016; Rich et al., 2021).
Conclusion
Our study points to a link between estrogen hormone therapy and a heightened risk of gallbladder disease in transgender women. We also found that there is no significant decrease in gallstone risk for transgender men receiving GAHT. Our findings underline the importance of close monitoring for cholelithiasis and other gallbladder diseases in transgender patients receiving hormone therapy. Further research is needed to clarify best practices for early intervention and screening in this population. Our study adds to the growing understanding of GAHT in the trans population, enhancing efforts to improve health and well-being among transgender individuals.
Acknowledgements
Special thanks to A.S. and all members and faculty of the GLMR research group whose support made this paper possible.
Appendix A. Cohort and outcome criteria
Cohort Construction- Terms Denoting Gender Identity Disorders
| ICD-10-CM Code | |
|---|---|
| Transsexualism | F64.0 |
| Dual role transvestism | F64.1 |
| Gender identity disorder of childhood | F64.2 |
| Other gender identity disorders | F64.8 |
| Gender identity disorder, unspecified | F64.9 |
Cohort Construction-Terms Denoting Female-To-Male GAHT:
| ICD-10-CM/RXNORM/VA Class/HCPCS Code | |
|---|---|
| Hormone replacement therapy | ICD10CM:Z79.890 |
| ANDROGENS/ANABOLICS | VA:HS100 |
| Testosterone | RXNORM:10379 |
| Endocrine disorder, unspecified | ICD10CM:E34.9 |
| Injection, testosterone cypionate, 1 mg | HCPCS:J1071 |
| Injection, testosterone enanthate, 1 mg | HCPCS:J3121 |
| Injection, testosterone undecanoate, 1 mg | HCPCS:J3145 |
Cohort Construction-Terms Denoting Male-To-Female GAHT
| ICD-10-CM/RXNORM/VA Class/HCPCS/ATC Code | |
|---|---|
| Hormone replacement therapy | ICD10CM:Z79.890 |
| ESTROGENS | ATC:G03C |
| Estrogens | ATC:L02AA |
| Endocrine disorder, unspecified | ICD10CM:E34.9 |
| ESTROGENS | VA:HS300 |
| estrogens, esterified (USP) | RXNORM:214549 |
| Estrogens | RXNORM:4100 |
Outcome Measures-Terms Denoting Gallbladder Disease
| ICD-10-CM Code | |
|---|---|
| Cholelithiasis | ICD10CM:K80 |
| Cholangitis | ICD10CM:K83.0 |
| Cholecystitis | ICD10CM:K81 |
| Obstruction of bile duct | ICD10CM:K83.1 |
Outcome Measures-Terms Denoting Gallbladder Surgery
| CPT Code: | |
|---|---|
| Cholecystectomy | 1014153 |
| Cholecystectomy with exploration of common duct | 1014154 |
| Laparoscopy, surgical; cholecystectomy | 47562 |
| Laparoscopy, surgical; cholecystectomy with cholangiography | 47563 |
| Laparoscopy, surgical; cholecystectomy with exploration of common duct | 47564 |
Appendix B. Cohort baseline characteristics and propensity score matching
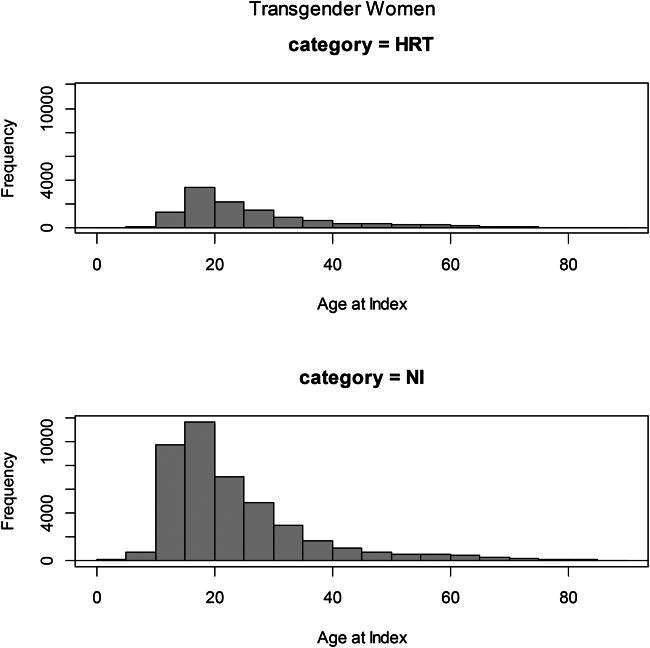
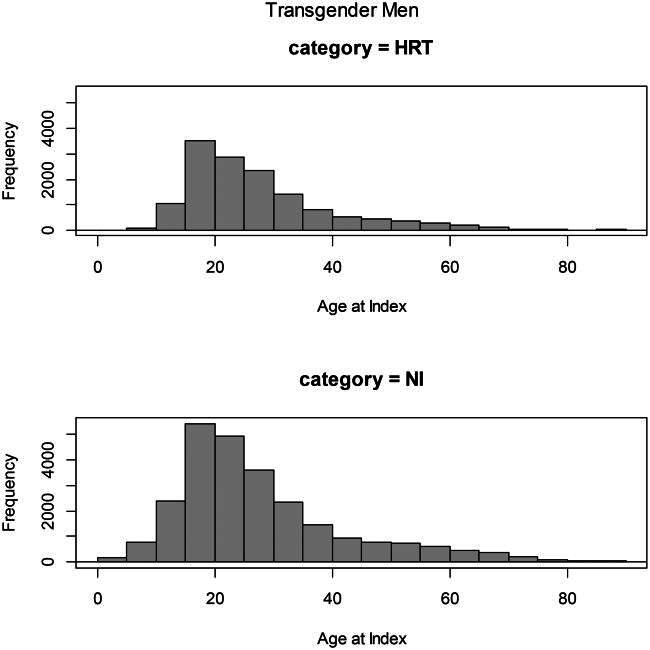
Age histograms
1. Distribution of age at index of transgender women
2. Distribution of age at index of transgender men
Balance tables
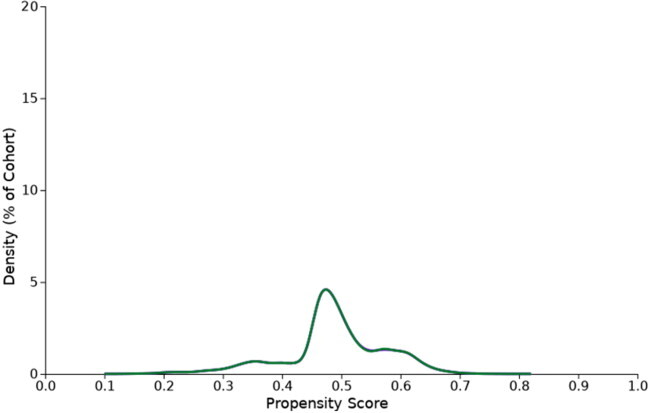
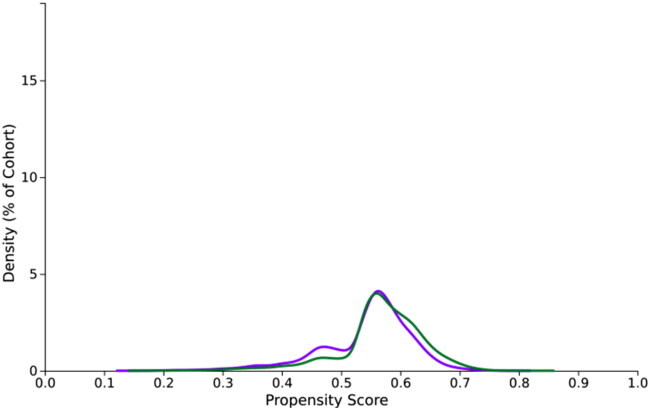
TWHT vs TWNI:
| Cohort 1 and cohort 2 patient count before and after propensity score matching | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort | Patient count before matching | Patient count after matching | ||||||||||
| 1 - TWHT15+ No Biliary | 20,188 | 15,900 | ||||||||||
| 2 - TWNI15 + No Biliary | 17,926 | 15,900 | ||||||||||
| Propensity score density function – Before and after matching (cohort 1 – purple, cohort 2 – green) | ||||||||||||
[
|
|
|||||||||||
| Cohort 1 (N = 20,188) and cohort 2 (N = 17,926) characteristics before propensity score matching | ||||||||||||
| Demographics | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-Value | Std diff. | |||||||
| 1 2 |
Age | Current Age | 32.2 ± 13.5 32.6 ± 15.2 |
20,104 17,735 |
100% 100% |
.005 | 0.029 | |||||
| 1 2 |
AI | Age at Index | 28.5 ± 13.0 28.7 ± 14.7 |
20,104 17,735 |
100% 100% |
.271 | 0.011 | |||||
| 1 2 |
2106-3 | White | 14,350 11,591 |
71.4% 65.4% |
<.001 | 0.130 | ||||||
| 1 2 |
UN | Unknown Ethnicity | 3675 4728 |
18.3% 26.7% |
<.001 | 0.202 | ||||||
| 1 2 |
2186-5 | Not Hispanic or Latino | 14,818 11,631 |
73.7% 65.6% |
<.001 | 0.177 | ||||||
| 1 2 |
2135-2 | Hispanic or Latino | 1611 1376 |
8.0% 7.8% |
.359 | 0.009 | ||||||
| 1 2 |
2054-5 | Black or African American | 1682 1767 |
8.4% 10.0% |
<.001 | 0.055 | ||||||
| 1 2 |
M | Male | 20,104 17,735 |
100% 100% |
-- | -- | ||||||
| 1 2 |
2131-1 | Unknown Race | 3441 3780 |
17.1% 21.3% |
<.001 | 0.107 | ||||||
| 1 2 |
2028-9 | Asian | 398 378 |
2.0% 2.1% |
.299 | 0.011 | ||||||
| Diagnosis | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-Value | Std diff. | |||||||
| 1 2 |
F10.1 | Alcohol abuse | 366 317 |
1.8% 1.8% |
.809 | 0.002 | ||||||
| 1 2 |
F10.2 | Alcohol dependence | 203 219 |
1.0% 1.2% |
.037 | 0.021 | ||||||
| 1 2 |
F17 | Nicotine dependence | 1510 952 |
7.5% 5.4% |
<.001 | 0.087 | ||||||
| 1 2 |
F17.2 | Nicotine dependence | 1510 952 |
7.5% 5.4% |
<.001 | 0.087 | ||||||
| 1 2 |
F17.20 | Nicotine dependence, unspecified | 1071 652 |
5.3% 3.7% |
<.001 | 0.080 | ||||||
| 1 2 |
F17.21 | Nicotine dependence, cigarettes | 712 546 |
3.5% 3.1% |
.012 | 0.026 | ||||||
| 1 2 |
E11 | Type 2 diabetes mellitus | 664 565 |
3.3% 3.2% |
.522 | 0.007 | ||||||
| 1 2 |
E10 | Type 1 diabetes mellitus | 202 154 |
1.0% 0.9% |
.170 | 0.014 | ||||||
| 1 2 |
E78.5 | Hyperlipidemia, unspecified | 964 629 |
4.8% 3.5% |
<.001 | 0.062 | ||||||
| 1 2 |
E78.4 | Other hyperlipidemia | 473 320 |
2.4% 1.8% |
<.001 | 0.038 | ||||||
| 1 2 |
E78.0 | Pure hypercholesterolemia | 349 237 |
1.7% 1.3% |
.002 | 0.032 | ||||||
| 1 2 |
E78.2 | Mixed hyperlipidemia | 318 186 |
1.6% 1.0% |
<.001 | 0.047 | ||||||
| 1 2 |
K74 | Fibrosis and cirrhosis of liver | 48 68 |
0.2% 0.4% |
.011 | 0.026 | ||||||
| 1 2 |
K70 | Alcoholic liver disease | 20 30 |
0.1% 0.2% |
.063 | 0.019 | ||||||
| 1 2 |
K76.0 | Fatty (change of) liver, not elsewhere classified | 228 144 |
1.1% 0.8% |
.002 | 0.033 | ||||||
| 1 2 |
R63.4 | Abnormal weight loss | 350 253 |
1.7% 1.4% |
.015 | 0.025 | ||||||
| Laboratory | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-Value | Std diff. | |||||||
| 1 2 |
9083 | BMI | 26.4 ± 6.9 26.4 ± 7.2 |
6683 3601 |
33.2% 20.3% |
.853 | 0.004 | |||||
| 1 2 |
1–18.40 kg/m2 | 1095 810 |
5.4% 4.6% |
<.001 | 0.040 | |||||||
| 1 2 |
18.50–24.90 kg/m2 | 3506 1864 |
17.4% 10.5% |
<.001 | 0.201 | |||||||
| 1 2 |
25–29.90 kg/m2 | 2330 1306 |
11.6% 7.4% |
<.001 | 0.145 | |||||||
| 1 2 |
30–39.90 kg/m2 | 1854 1003 |
9.2% 5.7% |
<.001 | 0.136 | |||||||
| 1 2 |
40–99 kg/m2 | 467 282 |
2.3% 1.6% |
<.001 | 0.053 | |||||||
| Cohort 1 (N = 15,900) and cohort 2 (N = 15,900) characteristics after propensity score matching | ||||||||||||
| Demographics | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
Age | Current Age | 32.2 + ± 13.6 32.4 ± 15.2 |
15,900 15,900 |
100% 100% |
.277 | 0.012 | |||||
| 1 2 |
AI | Age at Index | 28.5 ± 13.0 28.6 ± 14.7 |
15,900 15,900 |
100% 100% |
.456 | 0.008 | |||||
| 1 2 |
2106-3 | White | 10,949 10,978 |
68.9% 69.0% |
.725 | 0.004 | ||||||
| 1 2 |
UN | Unknown Ethnicity | 3431 3,235 |
21.6% 20.3% |
.007 | 0.030 | ||||||
| 1 2 |
2186-5 | Not Hispanic or Latino | 11,193 11,340 |
70.4% 71.3% |
.070 | 0.020 | ||||||
| 1 2 |
2135-2 | Hispanic or Latino | 1276 1325 |
8.0% 8.3% |
.316 | 0.011 | ||||||
| 1 2 |
2054-5 | Black or African American | 1477 1485 |
9.3% 9.3% |
.877 | 0.002 | ||||||
| 1 2 |
M | Male | 15,900 15,900 |
100% 100% |
-- | -- | ||||||
| 1 2 |
2131-1 | Unknown Race | 2960 2892 |
18.6% 18.2% |
.325 | 0.011 | ||||||
| 1 2 |
2028-9 | Asian | 334 345 |
2.1% 2.2% |
.670 | 0.005 | ||||||
| Diagnosis | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
F10.1 | Alcohol abuse | 253 277 |
1.6% 1.7% |
.293 | 0.012 | ||||||
| 1 2 |
F10.2 | Alcohol dependence | 165 168 |
1.0% 1.1% |
.869 | 0.002 | ||||||
| 1 2 |
F17 | Nicotine dependence | 897 900 |
5.6% 5.7% |
.942 | 0.001 | ||||||
| 1 2 |
F17.2 | Nicotine dependence | 897 900 |
5.6% 5.7% |
.942 | 0.001 | ||||||
| 1 2 |
F17.20 | Nicotine dependence, unspecified | 615 618 |
3.9% 3.9% |
.931 | 0.001 | ||||||
| 1 2 |
F17.21 | Nicotine dependence, cigarettes | 465 499 |
2.9% 3.1% |
.266 | 0.012 | ||||||
| 1 2 |
E11 | Type 2 diabetes mellitus | 498 512 |
3.1% 3.2% |
.654 | 0.005 | ||||||
| 1 2 |
E10 | Type 1 diabetes mellitus | 143 142 |
0.9% 0.9% |
.953 | 0.001 | ||||||
| 1 2 |
E78.5 | Hyperlipidemia, unspecified | 623 606 |
3.9% 3.8% |
.621 | 0.006 | ||||||
| 1 2 |
E78.4 | Other hyperlipidemia | 315 303 |
2.0% 1.9% |
.626 | 0.005 | ||||||
| 1 2 |
E78.0 | Pure hypercholesterolemia | 224 227 |
1.4% 1.4% |
.887 | 0.002 | ||||||
| 1 2 |
E78.2 | Mixed hyperlipidemia | 179 181 |
1.1% 1.1% |
.916 | 0.001 | ||||||
| 1 2 |
K74 | Fibrosis and cirrhosis of liver | 40 46 |
0.3% 0.3% |
.517 | 0.007 | ||||||
| 1 2 |
K70 | Alcoholic liver disease | 16 20 |
0.1% 0.1% |
.505 | 0.007 | ||||||
| 1 2 |
K76.0 | Fatty (change of) liver, not elsewhere classified | 132 140 |
0.8% 0.9% |
.626 | 0.005 | ||||||
| 1 2 |
R63.4 | Abnormal weight loss | 250 239 |
1.6% 1.5% |
.616 | 0.006 | ||||||
| Laboratory | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
9083 | BMI | 26.2 ± 7.1 26.4 ± 7.2 |
3957 3530 |
24.9% 22.2% |
.123 | 0.036 | |||||
| 1 2 |
1–18.40 kg/m2 | 799 770 |
5.0% 4.8% |
.453 | 0.008 | |||||||
| 1 2 |
18.50–24.90 kg/m2 | 1870 1853 |
11.8% 11.7% |
.767 | 0.003 | |||||||
| 1 2 |
25–29.90 kg/m2 | 1378 1284 |
8.7% 8.1% |
.057 | 0.021 | |||||||
| 1 2 |
30–39.90 kg/m2 | 1003 998 |
6.3% 6.3% |
.908 | 0.001 | |||||||
| 1 2 |
40–99 kg/m2 | 280 275 |
1.8% 1.7% |
.830 | 0.002 | |||||||
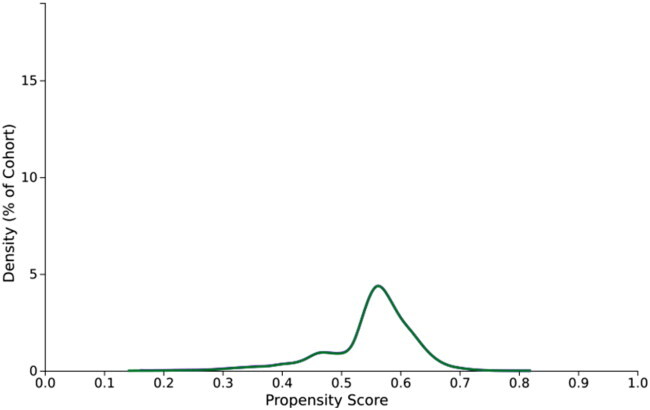
TMHT vs TMNI:
Figure 1.
Kaplan–Meier estimates of cumulative hazards for gallbladder disease outcomes.
| Cohort 1 and cohort 2 patient count before and after propensity score matching | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort | Patient count before matching | Patient count after matching | ||||||||||
| 1 - TMHT15 + No Biliary | 22,786 | 21,406 | ||||||||||
| 2 - TMNI15 + NoBiliary | 30,061 | 21,406 | ||||||||||
| Propensity score density function – Before and after matching (cohort 1 – purple, cohort 2 – green) | ||||||||||||
[
|
|
|||||||||||
| Cohort 1 (N = 22,786) and cohort 2 (N = 30,061) characteristics before propensity score matching | ||||||||||||
| Demographics | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-Value | Std diff. | |||||||
| 1 2 |
Age | Current Age | 27.9 ± 11.7 29.2 ± 14.6 |
22,764 29,864 |
100% 100% |
<.001 | 0.093 | |||||
| 1 2 |
AI | Age at Index | 24.5 ± 11.2 25.4 ± 13.9 |
22,764 29,864 |
100% 100% |
<.001 | 0.074 | |||||
| 1 2 |
2106-3 | White | 15,986 20,257 |
70.2% 67.8% |
<.001 | 0.052 | ||||||
| 1 2 |
UN | Unknown Ethnicity | 4691 7472 |
20.6% 25.0% |
<.001 | 0.105 | ||||||
| 1 2 |
2186-5 | Not Hispanic or Latino | 16,205 20,114 |
71.2% 67.4% |
<.001 | 0.083 | ||||||
| 1 2 |
2135-2 | Hispanic or Latino | 1868 2278 |
8.2% 7.6% |
.015 | 0.021 | ||||||
| 1 2 |
2054-5 | Black or African American | 1555 2133 |
6.8% 7.1% |
.166 | 0.012 | ||||||
| 1 2 |
2131-1 | Unknown Race | 4494 6500 |
19.7% 21.8% |
<.001 | 0.050 | ||||||
| 1 2 |
2028-9 | Asian | 518 672 |
2.3% 2.3% |
.846 | 0.002 | ||||||
| Diagnosis | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
F10.1 | Alcohol abuse | 250 252 |
1.1% 0.8% |
.003 | 0.026 | ||||||
| 1 2 |
F10.2 | Alcohol dependence | 154 149 |
0.7% 0.5% |
.008 | 0.023 | ||||||
| 1 2 |
F17 | Nicotine dependence | 1208 892 |
5.3% 3.0% |
<.001 | 0.117 | ||||||
| 1 2 |
F17.20 | Nicotine dependence, unspecified | 751 566 |
3.3% 1.9% |
<.001 | 0.088 | ||||||
| 1 2 |
F17.21 | Nicotine dependence, cigarettes | 609 482 |
2.7% 1.6% |
<.001 | 0.073 | ||||||
| 1 2 |
E11 | Type 2 diabetes mellitus | 590 685 |
2.6% 2.3% |
.028 | 0.019 | ||||||
| 1 2 |
E10 | Type 1 diabetes mellitus | 210 242 |
0.9% 0.8% |
.167 | 0.012 | ||||||
| 1 2 |
K74 | Fibrosis and cirrhosis of liver | 38 41 |
0.2% 0.1% |
.384 | 0.008 | ||||||
| 1 2 |
K70 | Alcoholic liver disease | 10 17 |
0.0% 0.1% |
.514 | 0.006 | ||||||
| 1 2 |
K76.0 | Fatty (change of) liver, not elsewhere classified | 191 179 |
0.8% 0.6% |
.001 | 0.028 | ||||||
| 1 2 |
R63.4 | Abnormal weight loss | 446 531 |
2.0% 1.8% |
.127 | 0.013 | ||||||
| 1 2 |
E78.1 | Pure hyperglyceridemia | 182 168 |
0.8% 0.6% |
.001 | 0.029 | ||||||
| 1 2 |
E78.2 | Mixed hyperlipidemia | 284 226 |
1.2% 0.8% |
<.001 | 0.049 | ||||||
| 1 2 |
E78.4 | Other hyperlipidemia | 329 374 |
1.4% 1.3% |
.056 | 0.017 | ||||||
| 1 2 |
E78.5 | Hyperlipidemia, unspecified | 793 766 |
3.5% 2.6% |
<.001 | 0.054 | ||||||
| Laboratory | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
9083 | BMI | 27.5 ± 7.7 26.4 ± 7.5 |
8051 6949 |
35.4% 23.3% |
<.001 | 0.149 | |||||
| 1 2 |
1–18.40 kg/m2 | 1433 1857 |
6.3% 6.2% |
.718 | 0.003 | |||||||
| 1 2 |
18.50–24.90 kg/m2 | 4200 3918 |
18.5% 13.1% |
<.001 | 0.147 | |||||||
| 1 2 |
25–29.90 kg/m2 | 2776 2408 |
12.2% 8.1% |
<.001 | 0.137 | |||||||
| 1 2 |
30–39.90 kg/m2 | 2510 1924 |
11.0% 6.4% |
<.001 | 0.163 | |||||||
| 1 2 |
40–99 kg/m2 | 858 586 |
3.8% 2.0% |
<.001 | 0.108 | |||||||
| Cohort 1 (N = 21,406) and cohort 2 (N = 21,406) characteristics after propensity score matching | ||||||||||||
| Demographics | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
Age | Current Age | 28.0 ± 11.8 27.8 ± 13.0 |
21,406 21,406 |
100% 100% |
.344 | 0.009 | |||||
| 1 2 |
AI | Age at Index | 24.5 ± 11.3 24.5 ± 12.6 |
21,406 21,406 |
100% 100% |
.613 | 0.005 | |||||
| 1 2 |
2106-3 | White | 14,998 15,084 |
70.1% 70.5% |
.363 | 0.009 | ||||||
| 1 2 |
UN | Unknown Ethnicity | 4558 4272 |
21.3% 20.0% |
.001 | 0.033 | ||||||
| 1 2 |
2186-5 | Not Hispanic or Latino | 15,121 15,287 |
70.6% 71.4% |
.077 | 0.017 | ||||||
| 1 2 |
2135-2 | Hispanic or Latino | 1727 1847 |
8.1% 8.6% |
.036 | 0.020 | ||||||
| 1 2 |
2054-5 | Black or African American | 1453 1502 |
6.8% 7.0% |
.350 | 0.009 | ||||||
| 1 2 |
2131-1 | Unknown Race | 4271 4113 |
20.0% 19.2% |
.054 | 0.019 | ||||||
| 1 2 |
2028-9 | Asian | 483 522 |
2.3% 2.4% |
.213 | 0.012 | ||||||
| Diagnosis | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
F10.1 | Alcohol abuse | 212 208 |
1.0% 1.0% |
.844 | 0.002 | ||||||
| 1 2 |
F10.2 | Alcohol dependence | 134 130 |
0.6% 0.6% |
.805 | 0.002 | ||||||
| 1 2 |
F17 | Nicotine dependence | 961 872 |
4.5% 4.1% |
.034 | 0.021 | ||||||
| 1 2 |
F17.20 | Nicotine dependence, unspecified | 592 552 |
2.8% 2.6% |
.231 | 0.012 | ||||||
| 1 2 |
F17.21 | Nicotine dependence, cigarettes | 479 471 |
2.2% 2.2% |
.793 | 0.003 | ||||||
| 1 2 |
E11 | Type 2 diabetes mellitus | 529 511 |
2.5% 2.4% |
.572 | 0.005 | ||||||
| 1 2 |
E10 | Type 1 diabetes mellitus | 196 198 |
0.9% 0.9% |
.919 | 0.001 | ||||||
| 1 2 |
K74 | Fibrosis and cirrhosis of liver | 30 27 |
0.1% 0.1% |
.691 | 0.004 | ||||||
| 1 2 |
K70 | Alcoholic liver disease | 10 10 |
0.0% 0.0% |
1 | <0.001 | ||||||
| 1 2 |
K76.0 | Fatty (change of) liver, not elsewhere classified | 168 153 |
0.8% 0.7% |
.401 | 0.008 | ||||||
| 1 2 |
R63.4 | Abnormal weight loss | 411 416 |
1.9% 1.9% |
.861 | 0.002 | ||||||
| 1 2 |
E78.1 | Pure hyperglyceridemia | 161 150 |
0.8% 0.7% |
.531 | 0.006 | ||||||
| 1 2 |
E78.2 | Mixed hyperlipidemia | 228 208 |
1.1% 1.0% |
.336 | 0.009 | ||||||
| 1 2 |
E78.4 | Other hyperlipidemia | 291 281 |
1.4% 1.3% |
.674 | 0.004 | ||||||
| 1 2 |
E78.5 | Hyperlipidemia, unspecified | 666 651 |
3.1% 3.0% |
.675 | 0.004 | ||||||
| Laboratory | ||||||||||||
| Cohort | Mean ± SD | Patients | % of Cohort | p-value | Std diff. | |||||||
| 1 2 |
9083 | BMI | 27.2 ± 7.7 26.9 ± 7.5 |
6847 6283 |
32.0% 29.4% |
.007 | 0.047 | |||||
| 1 2 |
1–18.40 kg/m2 | 1361 1439 |
6.4% 6.7% |
.127 | 0.015 | |||||||
| 1 2 |
18.50–24.90 kg/m2 | 3495 3722 |
16.3% 17.4% |
.003 | 0.028 | |||||||
| 1 2 |
25–29.90 kg/m2 | 2346 2265 |
11.0% 10.6% |
.207 | 0.012 | |||||||
| 1 2 |
30–39.90 kg/m2 | 2012 1875 |
9.4% 8.8% |
.021 | 0.022 | |||||||
| 1 2 |
40–99 kg/m2 | 680 575 |
3.2% 2.7% |
.003 | 0.029 | |||||||
Table 1.
Baseline descriptive characteristics of transgender cohorts before propensity score matching.
| Transgender Women |
Transgender Men |
|||
|---|---|---|---|---|
| Baseline characteristics | TWNI (n = 17926) | TWHT (n = 20188) | TMNI (n = 30061) | TMHT (n = 22786) |
| Age At Index, mean (SD), years | 28.7 (14.7) | 28.5 (13.0) | 25.4 (13.9) | 24.5 (11.2) |
| BMI, mean (SD) | 26.4 (7.2) | 26.2 (7.1) | 26.4 (7.5) | 27.5 (7.7) |
| Alcohol Consumption: | ||||
| Alcohol Use Disorder, Mild | 317 (1.77%) | 366 (1.81%) | 252 (0.84%) | 250 (1.10%) |
| Alcohol Use Disorder, Moderate-Severe | 219 (1.22%) | 203 (1.01%) | 149 (0.50%) | 154 (0.68%) |
| Nicotine Dependence | 952 (5.30%) | 1510 (7.48%) | 892 (2.97%) | 1208 (5.30%) |
| Type 1 Diabetes Mellitus | 154 (0.86%) | 202 (1.00%) | 242 (0.81%) | 210 (0.92%) |
| Type 2 Diabetes Mellitus | 565 (3.15%) | 664 (3.29%) | 685 (2.28%) | 590 (2.59%) |
| Hyperlipidemia | 1372 (7.64%) | 2104 (10.42%) | 1534 (5.10%) | 1588 (6.97%) |
| Fibrosis and Cirrhosis of the Liver | 68 (0.38%) | 48 (0.24%) | 41 (0.14%) | 38 (0.17%) |
| NAFLD | 144 (0.80%) | 228 (1.13%) | 179 (0.60%) | 191 (0.84%) |
| Alcoholic Liver Disease | 30 (0.17%) | 20 (0.10%) | 17 (0.06%) | 10 (0.04%) |
TM: Trans Men; TW: Trans Women; HT: Hormone Therapy; NI: No Intervention. Bold indicates p > .05 between HT and NI groups within the same gender identity before matching.
Table 2.
Kaplan–Meier Estimates of 1, 5, and 10 year probability of gallbladder disease and surgical outcomes before propensity score matching.
| % Patients with outcome |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TWNI (n = 17,926) |
TWHT (n = 20,188) |
TMNI (n = 30,061) |
TMHT (n = 22,786) |
|||||||||
| Outcomes | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year |
| All Gallbladder Disease Outcomes: | 0.23 | 1.08 | 1.88 | 0.38 | 1.99 | 4.69 | 0.30 | 1.62 | 3.87 | 0.30 | 1.39 | 3.15 |
| Cholelithiasis | 0.21 | 0.97 | 1.40 | 0.34 | 1.83 | 4.26 | 0.26 | 1.46 | 3.57 | 0.28 | 1.22 | 2.93 |
| Cholecystitis | 0.02 | 0.29 | 0.92 | 0.10 | 0.44 | 0.56 | 0.09 | 0.42 | 0.78 | 0.07 | 0.38 | 0.79 |
| Choledocholithiasis | 0.03 | 0.07 | 0.17 | 0.02 | 0.13 | 0.40 | 0.03 | 0.08 | 0.08 | 0.01 | 0.10 | 0.10 |
| Cholangitis | 0.00 | 0.03 | 0.20 | 0.01 | 0.08 | 0.12 | 0.01 | 0.03 | 0.03 | 0.00 | 0.05 | 0.05 |
| Surgical Outcomes: | ||||||||||||
| Cholecystectomy | 0.02 | 0.34 | 0.57 | 0.11 | 0.72 | 1.10 | 0.07 | 0.42 | 1.10 | 0.09 | 0.41 | 0.95 |
TM: Trans Men; TW: Trans Women; HT: Hormone Therapy; NI: No Intervention. Bold indicates significant difference between HT and NI within same gender identity at same time point before matching (by K-M log-rank test, p < .05).
Table 3.
Hazard ratio of gallbladder disease risk between propensity score matched cohorts.
| Cohort statistics |
Log Rank Test |
Hazard ratio |
||||
|---|---|---|---|---|---|---|
| Group | Patients in cohort | Patients with Gallstone Disease, No. (%) | X 2 | p | HR | 95% CI |
| TMHT | 21,406 | 118 (0.55%) | 1.547 | .214 | 0.844 | (0.645, 1.103) |
| TMNI | 21,406 | 98 (0.46%) | ||||
| TWHT | 15,900 | 123 (0.77%) | 13.795 | <.0001 | 1.832 | (1.324, 2.533) |
| TWNI | 15,900 | 52 (0.33% | ||||
TM: Trans Men; TW: Trans Women; HT: Hormone Therapy; NI: No Intervention. Bold indicates statistical significance p < .05.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Ahmed, A., Cheung, R. C., & Keeffe, E. B. (2000). Management of gallstones and their complications. American Family Physician, 61(6), 1673–1680. [PubMed] [Google Scholar]
- Blosnich, J. R., Cashy, J., Gordon, A. J., Shipherd, J. C., Kauth, M. R., Brown, G. R., & Fine, M. J. (2018). Using clinician text notes in electronic medical record data to validate transgender-related diagnosis codes. JAMIA, 25(7), 905–908. 10.1093/jamia/ocy022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirillo, D. J., Wallace, R. B., Rodabough, R. J., Greenland, P., LaCroix, A. Z., Limacher, M. C., & Larson, J. C. (2005). Effect of estrogen therapy on gallbladder disease. JAMA, 293(3), 330–339. 10.1001/jama.293.3.330 [DOI] [PubMed] [Google Scholar]
- Deutsch, M. B., Bhakri, V., & Kubicek, K. (2015). Effects of cross-sex hormone treatment on transgender women and men. Obstetrics and Gynecology, 125(3), 605–610. 10.1097/AOG.0000000000000692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everhart, J. E., Khare, M., Hill, M., & Maurer, K. R. (1999). Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology, 117(3), 632–639. 10.1016/s0016-5085(99)70456-7 [DOI] [PubMed] [Google Scholar]
- Freier, E., Kassel, L., Rand, J., & Chinnakotla, B. (2021). Estrogen-induced gallstone pancreatitis in a transgender female. American Journal of Health-System Pharmacy, 78(18), 1674–1680. 10.1093/ajhp/zxab190 [DOI] [PubMed] [Google Scholar]
- Hulley, S., Furberg, C., Barrett-Connor, E., Cauley, J., Grady, D., Haskell, W., Knopp, R., Lowery, M., Satterfield, S., Schrott, H., Vittinghoff, E., & Hunninghake, D. (2002). Noncardiovascular disease outcomes during 6.8 years of hormone therapy heart and estrogen/progestin replacement study follow-up (HERS II). JAMA, 288(1), 58–66. 10.1001/jama.288.1.58 [DOI] [PubMed] [Google Scholar]
- Lammert, F., Gurusamy, K., Ko, C. W., Miquel, J.-F., Méndez-Sánchez, N., Portincasa, P., van Erpecum, K. J., van Laarhoven, C. J., & Wang, D. Q.-H. (2016). Gallstones. Nature Reviews, 2(1), 16024. 10.1038/nrdp.2016.24 [DOI] [PubMed] [Google Scholar]
- Meerwijk, E. L., & Sevelius, J. M. (2017). Transgender population size in the United States: A meta-regression of population-based probability samples. American Journal of Public Health, 107(2), e1–e8. 10.2105/AJPH.2016.303578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nik-Ahd, F., Waller, J., De Hoedt, A. M., Garcia, M. M., Figueiredo, J. C., Carroll, P. R., Cooperberg, M. R., & Freedland, S. J. (2023). Seeing the unseen: How can we best identify transgender women within the veterans affairs healthcare system’s electronic medical record? The Journal of Sexual Medicine, 20(4), 559–567. 10.1093/jsxmed/qdac033 [DOI] [PubMed] [Google Scholar]
- Pak, M., & Lindseth, G. (2016). Risk factors for cholelithiasis. Gastroenterology Nursing, 39(4), 297–309. 10.1097/SGA.0000000000000235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor, K., Haffer, S. C., Ewald, E., Hodge, C., & James, C. V. (2016). Identifying the transgender population in the medicare program. Transgender Health, 1(1), 250–265. 10.1089/trgh.2016.0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich, A. J., Poteat, T., Koehoorn, M., Li, J., Ye, M., Sereda, P., Salway, T., & Hogg, R. (2021). Development of a computable phenotype to identify a transgender sample for health research purposes: A feasibility study in a large linked provincial healthcare administrative cohort in British Columbia, Canada. BMJ Open, 11(3), e040928. 10.1136/bmjopen-2020-040928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shabanzadeh, D. M. (2018). New determinants for gallstone disease? Dan Med J, 65(2):B5438. [PubMed] [Google Scholar]
- Squarza, S., Rossi, U. G., Torcia, P., & Cariati, M. (2018). Association between cholesterol gallstones and testosterone replacement therapy in a patient with primary hypogonadism. Revista de Gastroenterologia de Mexico, 83(2), 205–207. 10.1016/j.rgmx.2017.09.005 [DOI] [PubMed] [Google Scholar]
- Tirthani, E., Said, M., Neupane, B., Quartuccio, M., Tirthani, E., Said, M., Neupane, B., & Quartuccio, M. (2021). An unusual case of the “terrible triad” in a transgender woman. Cureus, 13(8), e16869. 10.7759/cureus.16869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhler, M. L., Marks, J. W., & Judd, H. L. (2000). Estrogen replacement therapy and gallbladder disease in postmenopausal women. Menopause, 7(3), 162–167. 10.1097/00042192-200007030-00006 [DOI] [PubMed] [Google Scholar]
- Unalp-Arida, A., & Ruhl, C. E. (2022). The burden of gallstone disease in the United States population. medRxiv. 10.1101/2022.07.08.22277386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadhwa, V., Jobanputra, Y., Garg, S. K., Patwardhan, S., Mehta, D., & Sanaka, M. R. (2017). Nationwide trends of hospital admissions for acute cholecystitis in the United States. Gastroenterology Report, 5(1), 36–42. 10.1093/gastro/gow015 [DOI] [PMC free article] [PubMed] [Google Scholar]