The number of gender-affirming procedures has skyrocketed as awareness of gender dysphoria spreads.1 There have been many studies on transmale gender-affirming top surgery with well-established surgical techniques for chest masculinization.2 However, there is limited information regarding nonbinary patients.3 As acceptance of gender fluidity rises, it is likely there will be more nonbinary patients who seek gender-affirming surgery. We discuss our novel surgical technique for gender-affirming top surgery for a patient who identified as female (preferred pronouns she/her) but desired a nonbinary chest appearance with absence of superomedial fullness and flatter, more uniform contour throughout her chest wall. She initially presented to clinic desiring a reduction mammaplasty due to back, neck, shoulder pain, and erythema intertrigo. During her evaluation, we discussed the procedure and how it would lead to a feminine breast contour with teardrop shape and superomedial volume, which the patient stated she did not want. We then reviewed the standard chest masculinization surgery with mastectomies and free nipple grafts, which she also declined.1 With further discussion, it was apparent that she desired a nonbinary chest and, thus, identified an approach that would best meet her needs.
Our technique was based on an inferior pedicle with Wise pattern skin incisions but incorporated masculine aspects with shortening the vertical limbs to 5 cm and designing the superior portion of the Wise pattern as an oval shape. Additionally, the pedicle was marked more laterally than standard reduction mammaplasties and narrowed in its base width. By marking the pedicle laterally, we achieved a gender-neutral nipple areolar complex position as we lateralized where this typically is in a feminine chest. By narrowing the base width, we were able to achieve a more masculine contour with less volume in the medial and lateral areas of the chest wall.
We performed our markings with the patient standing in the preoperative area. She was then taken to the operating room and underwent timeout, general anesthesia, endotracheal intubation and preparing and draping in standard sterile manner. The areola was made oval and smaller in size by marking it with the base of a 10-mL syringe. Then, the inferior pedicle design was marked with a smaller 6cm width and placed more laterally at 15 cm from midline. The rest of the procedure continued as a standard Wise pattern inferior pedicle breast reduction. The patient had a 5-month postoperative follow-up and voiced satisfaction with the procedure and did not have any complications (Fig. 1).
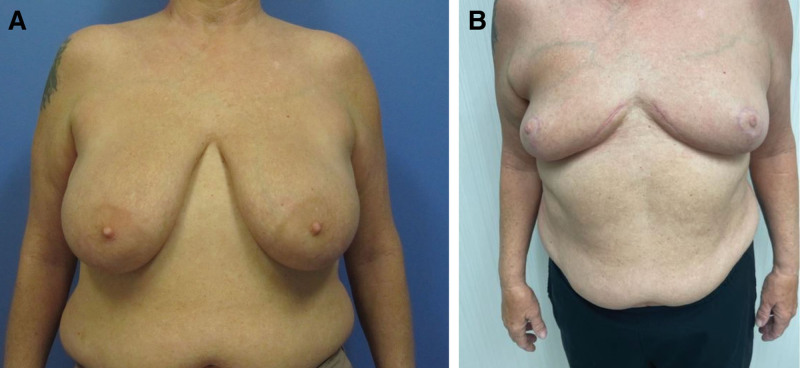
Fig. 1.
Before and after photographs demonstrating a nonbinary chest after our technique. A, Patient’s chest preoperatively. B, Patient’s chest 5 months after top surgery.
Patients desiring a nonbinary chest are a unique population that has not been well studied.1 There are no widely accepted guidelines established for this population in comparison to the established proportions for female or male chest.1 Studies have shown that patients who desire a nonbinary chest appearance also do not share a singular aesthetic goal.1 Accordingly, it is essential to work closely with patients to personalize their procedure to achieve what a nonbinary appearance means for them. As patients embrace their gender identities and seek gender-affirming surgery, plastic surgeons must be able to personalize gender-affirming procedures to accommodate the full spectrum of gender identities.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 24 October 2024.
REFERENCES
- 1.McTernan M, Yokoo K, Tong W. A comparison of gender-affirming chest surgery in nonbinary versus transmasculine patients. Ann Plast Surg. 2020;84:S323–S328. [DOI] [PubMed] [Google Scholar]
- 2.Esmonde N, Heston A, Jedrzejewski B, et al. What is “nonbinary” and what do I need to know? A primer for surgeons providing chest surgery for transgender patients. Aesthet Surg J. 2019;39:NP106–NP112. [DOI] [PubMed] [Google Scholar]
- 3.Friedman R, Garvey SR, Nanda A, et al. Breast reduction as gender-affirming chest surgery in non-binary patients: addressing the needs of a growing population. J Plast Reconstr Aesthet Surg. 2023;76:12–14. [DOI] [PubMed] [Google Scholar]