Abstract
Context: Exercise-associated muscle cramps (EAMCs) are common among physically active individuals and are temporarily disabling; therefore, prevention is of great interest.
Objective: To determine the role of hydration and electrolyte supplementation in the prevention of EAMCs.
Design: Each subject completed 2 counterbalanced trials in a repeated-measures design.
Setting: University of Alabama.
Patients or Other Participants: College-aged men (n = 13) with a history of EAMCs.
Intervention(s): In each trial, participants performed a calf-fatiguing protocol to induce EAMCs in the calf muscle group. Each trial was performed in a hot environment (dry bulb temperature of 37°C, relative humidity of 60%). In the carbohydrate-electrolyte trial, subjects consumed, at a rate similar to sweat loss, a carbohydrate-electrolyte beverage with sodium chloride added. In the hypohydration trial, subjects were not allowed to consume any fluids.
Main Outcome Measure(s): We measured the incidence and time to onset of EAMCs.
Results: Nine participants experienced cramps in the carbohydrate-electrolyte trial, compared with 7 in the hypohydration trial. Of the 7 individuals who had EAMCs in both trials, exercise duration before onset was more than doubled in the carbohydrate-electrolyte trial (36.8 ± 17.3 minutes) compared with the hypohydration trial (14.6 ± 5.0 minutes, P < .01).
Conclusions: Consumption of a carbohydrate-electrolyte beverage before and during exercise in a hot environment may delay the onset of EAMCs, thereby allowing participants to exercise longer. However, it appears that dehydration and electrolyte loss are not the sole causes of EAMCs, because 69% of the subjects experienced EAMCs when they were hydrated and supplemented with electrolytes.
Keywords: hypohydration, heat stress, fatigue, environmental physiology, cramping protocol
Skeletal muscle cramps are common among physically active individuals.1–4 Cramps that occur as a result of physical activity have been termed exercise-associated muscle cramps (EAMCs) and defined as a “painful, spasmodic contraction of the skeletal muscle that occurs during or immediately after muscular exercise.”5
Muscle cramps have affected 67% of triathletes during or after training or racing1 and 18% to 70% of marathoners or endurance cyclists, most often in the plantar-flexor muscle group.2,3,6,7 In endurance events, these cramps tend to occur toward the end of races.2,6 In studies of American football players, 30% to 53% experienced cramps.8,9
Because EAMCs are a temporarily debilitating condition, prevention is of great interest. Identifying the causes of EAMCs will likely lead to more effective prevention. The most commonly proposed causes for EAMCs are related to dehydration, abnormal serum electrolyte concentrations, and environmental stress.5,10–15
The dehydration theory suggests that decreases in body mass, blood volume, and plasma volume contribute to EAMCs.5,13,14 The serum electrolyte theory suggests decreases in the concentration of sodium, potassium, magnesium, chloride, and/or calcium as a result of sweating (or overconsumption of water) during exercise may be causative factors in the development of EAMCs.5,11,12,15,16 The environmental theory suggests that exercising in the heat, which may result in electrolyte imbalance and dehydration, is a potential cause of EAMCs.5,11,13,15,16
A more recent theory suggests that EAMCs are related to sustained neural activity that results from fatigue.5 This idea is supported by studies of distance runners, who are most likely to experience cramps toward the end of a race.2,6 McGee17 found that 1 to 2 hours of activity usually precipitate EAMCs.
The literature indicates a distinction between EAMCs that result from fatigue and those that result from heat (in which fluid and electrolyte losses result in a contraction of the extracellular fluid space).5,11,17,18 Fatigue-induced EAMCs tend to be muscle specific, whereas heat-related EAMCs may be more widespread.3,5,11,19 Although muscular fatigue may predispose the muscles to EAMCs, the role played by environmental heat, dehydration, and/or electrolyte loss in conjunction with muscular fatigue is unclear.
Much of the research in this area examines physiologic values after exercise to determine differences between those who experience cramps and those who do not experience cramps. In addition to stretching, the current recommended treatment and prevention of EAMCs include administration of fluids and/or table salt. Anecdotal remedies include pickle juice and mustard. Together these treatments suggest that dehydration and electrolyte balance are associated with EAMCs.3,11,17,20,21 The use of a saline solution for the prevention and treatment of muscle cramps was reported as early as 1898.13 However, limited published research supports these theories.
No known studies have been performed in a controlled environment to consider which conditions are most likely to reduce the occurrence of EAMCs. Therefore, our purpose was to determine the effect of hydration and electrolyte supplementation on the incidence of EAMCs and duration of exercise before the onset of EAMCs.
METHODS
Subjects
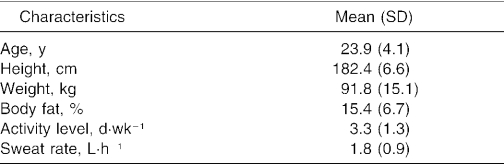
Thirteen healthy men (age, 23.9 ± 4.1 years) with a history of EAMCs that resulted from physical activity participated in this study. All participants completed a medical questionnaire and provided written informed consent. This research protocol was approved by the local institutional review board for the protection of human subjects. Subjects also completed a questionnaire regarding their history of muscle cramps (ie, frequency, muscle affected, activity that caused the cramps). All participants reported having had a cramp in the plantar-flexor muscle group as a result of exercise within the past year. Participant characteristics are given in Table 1.
Table 1. Participant Characteristics (n = 13).
Participants were not heat acclimatized but were moderately physically active (3.3 ± 1.3 d·wk−1), as determined by a questionnaire. They were required to refrain from physical activity for 24 hours before experimental trials. Subjects were asked to arrive at each experimental trial in a state of normal hydration, although this was not quantified (ie, they were instructed to consume beverages and food that were similar to their normal diet and to refrain from dehydration-inducing substances, such as alcohol and caffeine). In an attempt to standardize hydration at the onset of each of the trials, participants consumed 500 mL of water 2 hours before the exercise session.22 Participants were required to refrain from ingestion of any food for the 3 hours before each exercise session.
Testing Protocol
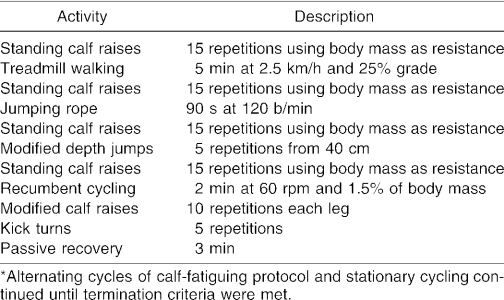
During the initial visit, we obtained measurements of height, body mass, and estimation of body fat using 3 skinfold sites (chest, abdomen, thigh). Each participant completed 2 trials: a hypohydration trial and a carbohydrate-electrolyte trial. The initial trial for the first participant was determined by the investigators. The order of trials for the remaining subjects was counterbalanced, with every other participant performing the hypohydration trial first. Trials were separated by at least 48 hours. Each trial was performed in a hot environment (dry bulb temperature of 37°C, relative humidity of 60%, wet bulb globe temperature of 32°C). During each trial, subjects performed a calf-fatiguing protocol (Table 2) that has been successful in inducing muscle cramps in 56% of participants in our laboratory.
Table 2. Cramping Protocol*.
During the treadmill walking, participants were required to walk on their toes and not allow the heels to make contact with the treadmill. Calf raises were performed on a 9-cm platform. Subjects were required to have their feet move below parallel on each eccentric phase of the exercise.
During the modified depth jump, participants stepped off a 40-cm bench, with both feet hitting the ground simultaneously. After recovery from the eccentric muscle action, subjects performed an explosive calf raise (as if jumping without leaving the ground). The static concentric position was then held for 5 seconds.
During the recumbent cycling, participants were instructed to maintain maximal plantar flexion while pressing down on the pedals. This technique stimulated greater use of the gastrocnemius than in traditional cycling while also loading the gastrocnemius in the shortened position.
During the modified calf raises, subjects assumed a supine position. From this position, they fully extended their elbows and raised their torsos off the floor while supporting their weight with their hands (shoulders in hyperextension). One leg (knee) was flexed to approximately 90° of knee flexion. The foot of the flexed leg was placed on a standard aerobics step bench, with only the ball of the foot on the step bench (9 cm high). In this position, body weight was supported by both hands and the foot of the flexed leg. The contralateral leg was maintained in full knee extension. In this position, participants performed 10 calf raises with each leg.
For the simulated kick turn, subjects sat in a standard office chair with wheels. Participants sat on the chair facing a wall and placed both feet on the wall at a height of approximately 45 cm (hip height). They leaned forward slightly, held onto the front of the chair, and pushed against the wall with both feet using maximal force. Participants held their legs in an extended position and feet in a plantar-flexed position for 5 seconds. This action was repeated 5 times. The action simulated a kick turn in swimming (eccentric action followed by concentric action), while maintaining a shortened gastrocnemius-soleus complex.
If no cramps occurred during the calf-fatiguing exercises, participants rode a mechanically braked cycle ergometer (model 868; Monark, Varberg, Sweden) for 12 minutes at 1 kg of resistance at a rate that elicited a heart rate of 140 to 150 beats/ min. Subjects repeated alternate cycles of the calf-fatiguing protocol and cycling until one of the following termination criteria was met: cramps were induced, 3% of body mass was lost due to sweat, exercise duration reached 120 minutes, rectal temperature reached 38.7°C, heart rate was within 10 beats/ min of age-predicted maximum, any sign of the onset of heat injury, or volitional exhaustion. Participants were informed that they could terminate the exercise session anytime they felt uncomfortable.
Experimental Conditions
During the hypohydration trial, subjects performed the alternating cycles of the calf-fatiguing exercises and cycling described herein. Participants were not allowed to consume any beverages during this trial. They were weighed every 30 minutes during exercise to determine the body mass lost to sweat. Rectal temperature and heart rate were monitored continuously and recorded every 10 minutes during exercise. Sweat rate was determined using the change in body weights from preexercise to postexercise.
During the carbohydrate-electrolyte trial, participants performed the identical exercise session as described in the hypohydration trial. However, each participant consumed a carbohydrate-electrolyte beverage at a rate similar to his specific fluid loss due to sweat. The beverage was a standard sports drink made from powder (Gatorade, Barrington, IL), which is reported to help replace electrolytes lost due to sweating. Half a teaspoon of table salt (NaCl) was added to each liter of the sports drink, as recommended by beverage manufacturers and other researchers as a recovery beverage.21–23 In an attempt to standardize hydration and to stimulate gastric emptying, each participant consumed 500 mL of the sports drink with added NaCl 20 minutes before exercise.22
The carbohydrate-electrolyte beverage, which was made from a powder, contained 56 g of carbohydrate (sucrose, glucose, fructose), 1620 mg (70 mmol) of sodium, 120 mg (3 mmol) of potassium, and 1800 mg (51 mmol) of chloride. These concentrations of sodium and potassium were chosen to replace average electrolyte losses in sweat for unacclimatized individuals. Average electrolyte sweat values have been reported as 920 to 2300 mg·L−1 (40–100 mmol·L−1) for sodium and 120 to 160 mg·L−1 (3–4 mmol·L−1) for potassium in unacclimatized individuals.21,23,24
Participants who performed the carbohydrate-electrolyte trial first consumed the fluid at a rate of at least 200 to 250 mL every 10 minutes or approximately 1.0 to 1.5 L·h−1.22 Subjects in the carbohydrate-electrolyte trial were weighed in undergarments before exercise and every 30 minutes during exercise. Fluid consumption was adjusted throughout the trial based on body weight measurements to compensate for fluid lost due to sweat.
When a cramp occurred, the investigators immediately applied force to the plantar surface of the foot to relieve it, while simultaneously massaging the cramped muscle. This procedure has been successful in a previous study.25 Criteria for a valid cramp included visual “knotting” of the muscle, unequivocal pain, and continuation of cramping when active contraction was stopped.25 The incidence of EAMCs and duration of exercise before the onset of EAMCs were recorded.
Statistical Analysis
We calculated a 1-dimensional χ2 test to determine differences in the frequency of cramps between the 2 experimental trials. A repeated-measures analysis of variance was used to determine the difference between duration of exercise before onset of cramp between the hypohydration and carbohydrate-electrolyte trials. Level of significance was set at α = .05.
RESULTS
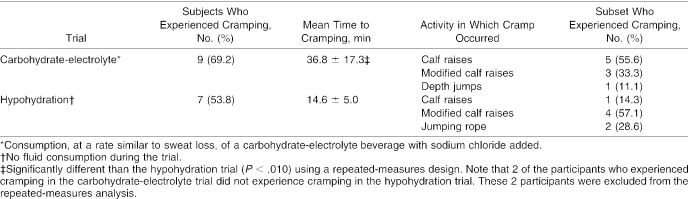
All observed cramps met the criteria set previously. A 1-dimensional χ2 test revealed no significant difference in the frequency of muscle cramps between the 2 trials (P = .42). The number of participants who experienced cramps in each trial, the mean time to onset of cramps, and the activity during which they experienced cramps are given in Table 3. Seven subjects experienced a cramp in both conditions. Two additional participants experienced cramps during the carbohydrate-electrolyte trial but not during the hypohydration trial. Subjects experienced cramps significantly earlier in the hypohydration trial (14.6 ± 5.0 minutes) than in the carbohydrate-electrolyte trials (36.8 ± 17.3 minutes, F6,12 = 14, P < .01).
Table 3. Muscle Cramps During Each Trial and Activity in Which Cramp Was Induced (n = 13).
The difference between preexercise and postexercise weight was significant (t12 = 9.3, P < .001). Mean weight loss during the hypohydration trial due to sweating was 1.0% ± 0.4% of body weight (0.9 ± 0.4 L of sweat). No weight loss occurred during the carbohydrate-electrolyte trial (preexercise weight, 91.8 ± 15.1 kg; postexercise weight, 92.2 ± 15.2 kg). All participants either maintained weight or slightly gained weight in this trial. A significant difference was noted in the sweat rate between those who experienced cramps and those who did not (2.0 ± 0.9 L·min−1 versus 1.3 ± 0.6 L·min−1, P = .01).
Exercise was terminated when the participant reached the maximum allowable core temperature (38.7°C). Mean duration of exercise for those who did not experience cramps was 84.2 ± 8.8 minutes in the carbohydrate-electrolyte trial (n = 4) and 52.3 ± 10.5 minutes for the hypohydration trial (n = 6).
DISCUSSION
As mentioned previously, the proposed explanations of EAMCs include the dehydration theory, electrolyte theory, and environmental theory. We attempted to experimentally address the former 2 theories related to EAMCs in subjects exercising in a hot environment.
In marathoners and cyclists, no difference was noted in hydration status or plasma concentration of electrolytes between those who experienced cramping after a race and those who did not.2,4,5,7,26 Additionally, no association was seen between dehydration and the probability of cramping in Ironman triathletes when dehydration was measured as a percentage of body weight loss.1 Several other groups,12,13 however, have found that EAMCs were associated with a plasma electrolyte deficit. A decrease in urinary sodium chloride, which is associated with muscle cramps, may suggest the body is trying to maintain sodium balance.27,28 In a recent case study, a male tennis player was able to eliminate chronic heat cramps by increasing his daily intake of sodium,11 but most authors assessed differences between those who did and did not experience cramps after exercise. We attempted to find a means of preventing or delaying cramps during exercise by fluid and electrolyte supplementation using a controlled, within-subjects design.
We found that 9 of 13 participants (69%) experienced cramps during exercise when they consumed an electrolyte beverage (carbohydrate-electrolyte trial), whereas 7 of 13 (54%) experienced cramps when they received no fluid or electrolytes (hypohydration trial). All of the subjects who experienced cramps in the hypohydration trial also experienced cramps in the carbohydrate-electrolyte trial. Thus, it would appear that hydration or electrolyte supplementation did not influence the incidence of cramps. It must be noted, however, that because the exercise was so intense, hydration and electrolyte supplementation may not have had the opportunity to play a role in prevention. Sweat rates may have exceeded the ability to absorb the rehydration beverage. It is possible that during less intense exercise, hydration and supplementation might have prevented EAMCs. It is also possible that rehydration beverages have little effect on fatigue-induced EAMCs, which was the focus of this study. Perhaps a rehydration beverage would have a greater preventive effect on heat-related cramps.
Individual variability likely plays a large role in the cause of EAMCs. The participants who experienced cramps had a higher average sweat rate than those who did not experience cramps. This finding supports the theories that EAMCs may be related to dehydration and/or electrolyte imbalance. However, because fluid and electrolytes were provided together, it is difficult to determine which variable may have had the greater influence. It is also possible that those participants who cramped had high levels of electrolytes in their sweat. Neither sweat electrolyte concentrations nor dietary recall was assessed in this study. Consistently low sodium intake has been implicated as related to EAMCs.11 For some participants, the preloading of electrolytes and fluid 30 minutes before exercise may have resulted in an excess of electrolytes over homeostatic values, which may have delayed the onset of cramps. However, because these variables were not measured, it is difficult to evaluate how these factors may have affected the individuals' propensity to cramp.
The average weight loss in this study was approximately 1.0% of total body mass. Although this amount of weight loss may not be substantial, it was achieved rapidly (less than 20 minutes). Additionally, all of the participants in the hypohydration trial lost weight. Subjects cramped regardless of whether they consumed fluids or not, suggesting that fluid intake does not prevent EAMCs.
In the carbohydrate-electrolyte trial, participants were not dehydrated, and they supplemented electrolytes. Nine of the 13 participants experienced a cramp. This finding conflicts with theories suggesting that dehydration and/or electrolyte imbalance may be the primary cause(s) of EAMCs. Additionally, 6 participants did not experience cramps in the hypohydration trial, although these participants lost an average of 1.2% of body mass. This suggests that mild dehydration is not the sole cause of EAMCs. It is also possible that more substantial degrees of dehydration are necessary to develop EAMCs.
Subjects who experienced cramps in both trials in our study were, on average, able to exercise 150% longer before the onset of cramps during the carbohydrate-electrolyte trial, thus indicating a benefit in consuming a carbohydrate-electrolyte beverage. The National Athletic Trainers' Association, among other organizations, suggests that the addition of electrolytes to a beverage will help prevent EAMCs.21–23 Additionally, prehydrating the individuals may have had an effect on cramping.22 Those who were hypohydrated experienced cramps significantly earlier than those who consumed a beverage to maintain hydration, indicating that hydration status may be a contributing factor to EAMCs. Our data support these suggestions; however, due to the nature of the study design, we do not know whether the increased duration of exercise before the onset of muscle cramps was due to the fluid intake, the electrolytes in the beverage, or both. It is also feasible that the carbohydrates delayed fatigue, thereby delaying the onset of EAMCs. Nonetheless, although the mechanism may not yet be defined, the importance of our results is that the carbohydrate-electrolyte beverage did delay the onset of EAMCs.
As mentioned earlier, a more recent theory of EAMC causation involves muscular fatigue. This theory suggests that repetitive contractions may be the precipitating event leading to EAMCs.5,29 Based on our results, it appears that local muscle fatigue may be a precipitating factor for muscle cramps to occur. In our study, cramps were induced in as little as 10 minutes. The high intensity and targeting of a specific muscle group likely predisposed the participants to a cramp after a relatively short duration of exercise compared with the previously stated 1 to 2 hours.
The incidence of muscle cramps was similar between the hypohydration and the carbohydrate-electrolyte trials, suggesting that dehydration and electrolyte imbalance are not the sole causes of EAMCs. However, as mentioned previously, hydration and electrolytes may only aid in the prevention of EAMCs up to a threshold of intensity or muscular fatigue. It is possible that beyond this threshold, hydration and electrolyte supplementation are no longer able to prevent EAMCs.
When considering only the participants who experienced cramps during both trials, the addition of a carbohydrate-electrolyte beverage allowed them to exercise in a hot environment for a longer period before cramping than in the hypohydration trial. These results support the notion that hydration and electrolytes play a role in EAMCs. The constant factor among the trials remains local muscle fatigue, which may ultimately be the primary factor responsible for EAMCs.
There appears to be a distinction between fatigue-induced and heat-related cramps in causation and often in the manifestation of symptoms. Because fluid loss was only 1% of body weight and because the cramps were localized, the EAMCs in this study appear to have been primarily the result of fatigue. This suggests that a carbohydrate-electrolyte beverage has little effect on the incidence of EAMCs when the cramps are fatigue induced. However, because some fluid loss occurred, it appears that the carbohydrate-electrolyte beverage played a role as evidenced by a longer duration of exercise. In some instances, it may be difficult to separate heat-related cramps from fatigue-related cramps, because fatigue is likely a contributing factor in heat-related cramps that occur during extended periods of exercise. Our result is applicable in that exercise and/or athletics often includes both muscle fatigue and factors related to environmental heat.
In general, the occurrence of EAMCs is associated with a multifactor cause. Our findings suggest that carbohydrate-electrolyte beverages possibly mitigate 1 or 2 contributing factors. In doing so, carbohydrate-electrolyte beverages may allow athletes to perform for a longer period before experiencing EAMCs. Thus, one could speculate that a carbohydrate-electrolyte beverage may prevent EAMCs during low-intensity workouts. In situations where sweat production exceeds fluid and electrolyte absorption, carbohydrate-electrolyte beverages may delay the onset of EAMCs, but they are unlikely to prevent EAMCs.
Future researchers need to consider the possibility of a threshold in which hydration and electrolyte supplementation may aid in preventing EAMCs. Because participants experienced cramps while they were hydrated and supplemented with electrolytes, a cause other than dehydration and electrolyte imbalance must be explored. Our results suggest that local muscle fatigue is likely associated with the occurrence of EAMCs. Future investigators also need to address methods of prevention for these different proposed causes of EAMCs.
Acknowledgments
This study was funded in part by the University of Alabama Graduate Student Association, Tuscaloosa, AL.
REFERENCES
- Kantorowski PG, Hiller WDB, Garrett WE, Douglas PS, Smith R, O'Toole M. Cramping studies in 2600 endurance athletes. Med Sci Sports Exerc. 1990;22:S104. (2 suppl) [Google Scholar]
- Maughan RJ. Exercise-induced muscle cramps: a prospective biochemical study in marathon runners. J Sports Sci. 1986;4:31–34. doi: 10.1080/02640418608732095. [DOI] [PubMed] [Google Scholar]
- Miles MP, Clarkson PM. Exercise-induced muscle pain, soreness, and cramps. J Sports Med Phys Fitness. 1994;34:203–216. [PubMed] [Google Scholar]
- O'Toole ML, Douglas PS, Lebrun CM. Magnesium in the treatment of exertional muscle cramps. Med Sci Sports Exerc. 1993;25:S19. et al. (5 suppl) [Google Scholar]
- Schwellnus MP, Derman EW, Noakes TD. Aetiology of skeletal muscle “cramps” during exercise: a novel hypothesis. J Sports Sci. 1997;15:277–285. doi: 10.1080/026404197367281. [DOI] [PubMed] [Google Scholar]
- Manjra S, Schwellnus MP, Noakes TD. Risk factors for exercise associated muscle cramping (EAMC) in marathoners. Med Sci Sports Exerc. 1996;28:S167. (5 suppl) [Google Scholar]
- Williamson SL, Johnson RW, Hudkins PG, Strate SM. Exertion cramps: a prospective study of biochemical and anthropometric variables in bicycle riders. Cycling Sci. Spring 1993:15–20. [Google Scholar]
- Greenwood M, Kreider RB, Greenwood L, Byars A. Cramping and injury incidence in collegiate football players are reduced by creatine supplementation. J Athl Train. 2003;38:216–219. [PMC free article] [PubMed] [Google Scholar]
- Maddali S, Rodeo SA, Barnes R, Warren RF, Murrell GA. Postexercise increase in nitric oxide in football players with muscle cramps. Am J Sports Med. 1998;26:820–824. doi: 10.1177/03635465980260061401. [DOI] [PubMed] [Google Scholar]
- Armstrong LE, Epstein Y, Greenleaf JE. American College of Sports Medicine position stand: heat and cold illnesses during long distance running. Med Sci Sports Exerc. 1996;28:i–x. et al. [PubMed] [Google Scholar]
- Bergeron MF. Heat cramps during tennis: a case report. Int J Sports Nutr. 1996;6:62–68. doi: 10.1123/ijsn.6.1.62. [DOI] [PubMed] [Google Scholar]
- Ladell WSS. Heat cramps. Lancet. 1949;2:836–839. [Google Scholar]
- Talbot JH. Heat cramps. Medicine. 1935;14:323–376. [Google Scholar]
- Mendell JR. The nervous system. In: Strauss RH, ed. Sports Medicine. Philadelphia, PA: WB Saunders; 1984:149–174.
- Levin S. Investigating the cause of muscle cramps. Physician Sportsmed. 1993;21(7):111–116. doi: 10.1080/00913847.1993.11710404. [DOI] [PubMed] [Google Scholar]
- Armstrong LE, Maresh CM. The exertional heat illness: a risk of athletic participation. Med Exerc Nutr Health. 1993;2:125–134. [Google Scholar]
- McGee SR. Muscle cramps. Arch Intern Med. 1990;150:511–518. [PubMed] [Google Scholar]
- Layzer RB. The origin of muscle fasciculations and cramps. Muscle Nerve. 1994;17:1243–1249. doi: 10.1002/mus.880171102. [DOI] [PubMed] [Google Scholar]
- Bergeron MF. Heat cramps: fluid and electrolyte challenges during tennis in the heat. J Sci Med Sport. 2003;6:19–27. doi: 10.1016/s1440-2440(03)80005-1. [DOI] [PubMed] [Google Scholar]
- Anderson S, Eichner R. Preventing muscle cramps in football. School Coach Athl Dir. 2001;70(10):52. [Google Scholar]
- Bergeron MF. Sodium: the forgotten nutrient. Gatorade Sports Sci Exch. 2000;13(3)
- Casa DJ, Armstrong LE, Hillman SK. National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train. 2000;35:212–224. et al. [PMC free article] [PubMed] [Google Scholar]
- Wexler RK. Evaluation and treatment of heat-related illnesses. Am Fam Physician. 2002;65:2307–2314. [PubMed] [Google Scholar]
- Askew EW. Water. In: Ziegler EE, Liler LJ, eds. Present Knowledge in Nutrition. 7th ed. Washington, DC: International Life Sciences Institute Press; 1996:98–108.
- Ross BH, Thomas CK. Human motor unit activity during induced muscle cramp. Brain. 1995;118:983–993. doi: 10.1093/brain/118.4.983. [DOI] [PubMed] [Google Scholar]
- Nicol J, Schwellnus MP, Noakes TD. Serum electrolyte concentrations and hydration status in runners with exercise associated muscle cramps (EAMC) Med Sci Sports Exerc. 1996;28:S59. doi: 10.1136/bjsm.2003.007021. (5 suppl) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard RW, Armstrong LE. The heat illness: biochemical, ultrastructural, and fluid-electrolyte considerations. In: Pandolf KB, Sawka MN, Gonzalez RR, eds. Human Performance Physiology and Environmental Medicine at Terrestrial Extremes. Indianapolis, IN: Benchmark Press; 1988:305–359.
- Hubbard RW, Armstrong LE. Hyperthermia: new thoughts on an old problem. Physician Sportsmed. 1989;17(6):97–113. doi: 10.1080/00913847.1989.11709808. [DOI] [PubMed] [Google Scholar]
- Bentley S. Exercise-induced muscle cramp: proposed mechanisms and management. Sports Med. 1996;21:409–420. doi: 10.2165/00007256-199621060-00003. [DOI] [PubMed] [Google Scholar]