Abstract
CONVENTIONAL ANTIPSYCHOTIC DRUGS, used for a half century to treat a range of major psychiatric disorders, are being replaced in clinical practice by modern “atypical” antipsychotics, including aripiprazole, clozapine, olanzapine, quetiapine, risperidone and ziprasidone among others. As a class, the newer drugs have been promoted as being broadly clinically superior, but the evidence for this is problematic. In this brief critical overview, we consider the pharmacology, therapeutic effectiveness, tolerability, adverse effects and costs of individual modern agents versus older antipsychotic drugs. Because of typically minor differences between agents in clinical effectiveness and tolerability, and because of growing concerns about potential adverse long-term health consequences of some modern agents, it is reasonable to consider both older and newer drugs for clinical use, and it is important to inform patients of relative benefits, risks and costs of specific choices.
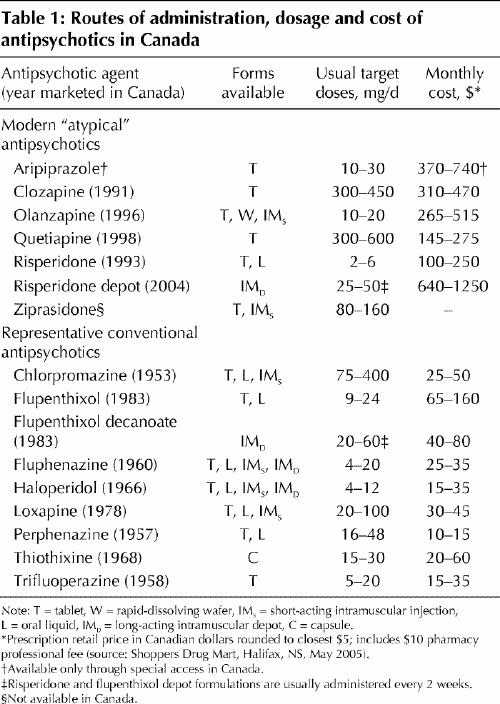
Antipsychotic drugs are useful for treating a range of severe psychiatric disorders. Applications include the short-term treatment of acute psychotic, manic and psychotic-depressive disorders as well as agitated states in delirium and dementia and the long-term treatment of chronic psychotic disorders including schizophrenia, schizoaffective disorder and delusional disorders. Newer, “second-generation” antipsychotic drugs have largely replaced older phenothiazine, thioxanthene and butyrophenone neuroleptics in clinical practice (Table 1).1,2 The development of modern antipsychotic drugs was stimulated by a landmark 1988 study that showed clozapine to be superior in efficacy to chlorpromazine in schizophrenia patients resistant to high doses of haloperidol and to have none of the adverse neurologic effects typical of older antipsychotic agents.3 Clozapine was considered “atypical” in having a very low risk of adverse extrapyramidal symptoms. This term has since been applied broadly and uncritically to antipsychotic drugs marketed in the past decade, despite their striking chemical, pharmacologic and clinical heterogeneity.4 In this overview we consider the neuropharmacology, efficacy and adverse effects of conventional antipsychotics and specific modern antipsychotic drugs.
Table 1
Neuropharmacology
The venerable hypothesis that schizophrenia is caused by increased cerebral activity of the neurotransmitter dopamine was based primarily on the finding that dopamine agonists produced or worsened psychosis and that antagonists were clinically effective against psychotic and manic symptoms.5 Blocking dopamine D2 receptors may be a critical or even sufficient neuropharmacologic action of most clinically effective antipsychotic drugs, especially against hallucinations and delusions, but it is not necessarily the only mechanism for antipsychotic activity. Moreover, this activity, and subsequent pharmacocentric and circular speculations about altered dopaminergic function, have not led to a better understanding of the pathophysiology or causes of the several still idiopathic psychotic disorders, nor have they provided a non-empirical, theoretical basis for the design or discovery of improved treatments for psychotic disorders.
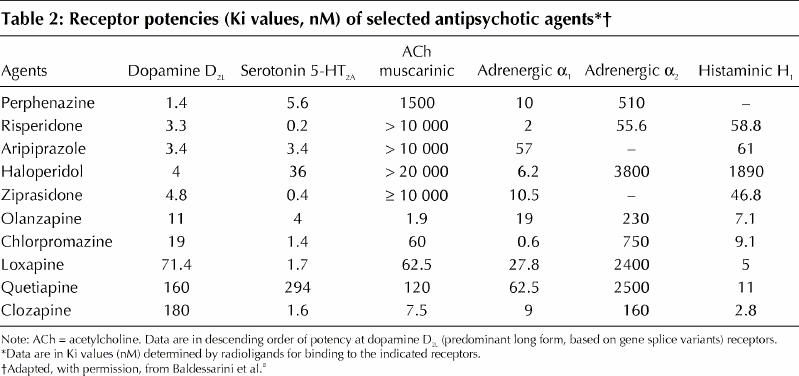
The neuropharmacodynamics of specific modern antipsychotic drugs vary greatly, with little evidence for a unifying theory of antipsychotic activity or of drug design (Table 2). Clozapine in particular is complex: it binds loosely and transiently to D2 receptors and interacts at dopamine (D1, D3 and D4), histamine (H1), acetylcholine muscarinic (M1) and serotonin (5-HT2A, 5-HT2C, 5-HT6 and 5-HT7) receptors and α1 adrenoceptors.6,7,8 This complexity leaves the very low risk of extrapyramidal symptoms and unexcelled antipsychotic effectiveness of clozapine unexplained.9 Postural dizziness, sedation and increased appetite may reflect actions of clozapine and some other antipsychotic agents at α1, H1 and 5-HT2C receptors respectively. Olanzapine demonstrates significant anti-M1 and moderate H1 affinity. Risperidone is a potent antagonist at 5-HT2A, D2 and α1 receptors. Ziprasidone is a potent antagonist at D2, D3, 5-HT1D, 5-HT2A, 5-HT2C and 5-HT7 receptors; it also has 5-HT1A-agonist actions that may alleviate anxiety and depression, and a moderate inhibitory effect on neuronal transport inactivation of serotonin like that of selective serotonin reuptake inhibitor antidepressants.10 Aripiprazole has a particularly low risk of acute extrapyramidal symptoms despite high levels of occupation of D2 receptors (> 90%) at therapeutic doses, which probably reflects its partial-agonist activity at those receptors.11
Table 2
Conventional antipsychotic drugs, especially those of high potency with high affinity and avidity for D2 receptors (e.g., haloperidol and fluphenazine), markedly interfere with dopaminergic neurotransmission and carry relatively high risks of extrapyramidal symptoms, even at moderate doses. These adverse neurologic responses include distressing motor restlessness (akathisia), acute dystonias and dyskinesias and gradually evolving parkinsonian bradykinesia as well as tardive dyskinesias and dystonias. Although the pathophysiology of these extrapyramidal syndromes is ill-defined, parkinsonism, at least, is probably related to decreased dopaminergic transmission in the forebrain basal ganglia.8 Clinical computed positron-emission tomography (PET) studies have indicated that 60%– 80% occupation of D2 receptors is associated with antipsychotic efficacy and that higher occupation levels are associated with an increased risk of acute extrapyramidal symptoms as well as with hyperprolactinemia from the blocking of D2 receptors on anterior-pituitary mammotrophic cells that normally are tonically inhibited by dopamine produced in the hypothalamic arcuate nucleus.12,13,14,15
The atypically low risk of extrapyramidal symptoms associated with some modern antipsychotic agents (e.g., clozapine, olanzapine, ziprasidone) may reflect their greater affinity for 5-HT2A receptors over dopamine D2 receptors.16,17 However, this pattern is not followed by all modern agents and is found in some older drugs (e.g., loxapine).18,19 Also, PET studies have shown that some modern antipsychotic agents (including clozapine, olanzapine, quetiapine and ziprasidone, but not aripiprazole or risperidone) have moderate affinity and relatively low avidity (rapid dissociation) at basal ganglia D2 receptors (Table 2).18,19 The anticholinergic effects of some modern agents (e.g., clozapine, olanzapine) may also limit the risk of extrapyramidal symptoms and avoid the need to add an antimuscarinic-antiparkinsonism agent (e.g., benztropine, biperiden, procyclidine or trihexyphenidyl), as is often required with older antipsychotic agents to rebalance critical dopaminergic – cholinergic functions in the basal ganglia.8,20
Efficacy: modern versus older antipsychotic agents
So-called “positive” psychotic symptoms (particularly agitation, aggression, delusions and hallucinations) are especially responsive to antipsychotic treatment, whereas “negative” symptoms of chronic psychotic illnesses (e.g., social withdrawal, lack of motivation) and impaired cognition (e.g., deficient working memory, verbal fluency) are typically less responsive to treatment and contribute to long-term disability.8,21 To compare individual drugs for their clinical efficacy, tolerability and safety, we examined evidence presented in published systematic reviews that compared modern and conventional antipsychotic drugs22,23,24,25,26,27,28,29,30 (Table 3; a longer version of the table is available online at www.cmaj.ca/cgi/content/full/172/13/1703/DC1). Notable limitations of the findings in many trials included in these reviews are possibly unrepresentative patient samples, relatively brief treatment, high dropout rates, unbalanced dose comparisons, modest clinical effects or outcome measures of sometimes dubious clinical relevance.23,26,31,32 Of particular concern in some clinical trials is the use of relatively high doses of risperidone and standard comparators such as haloperidol, and low doses of quetiapine. High doses can decrease tolerability, and low doses can limit efficacy.22,23,24,33
Table 3
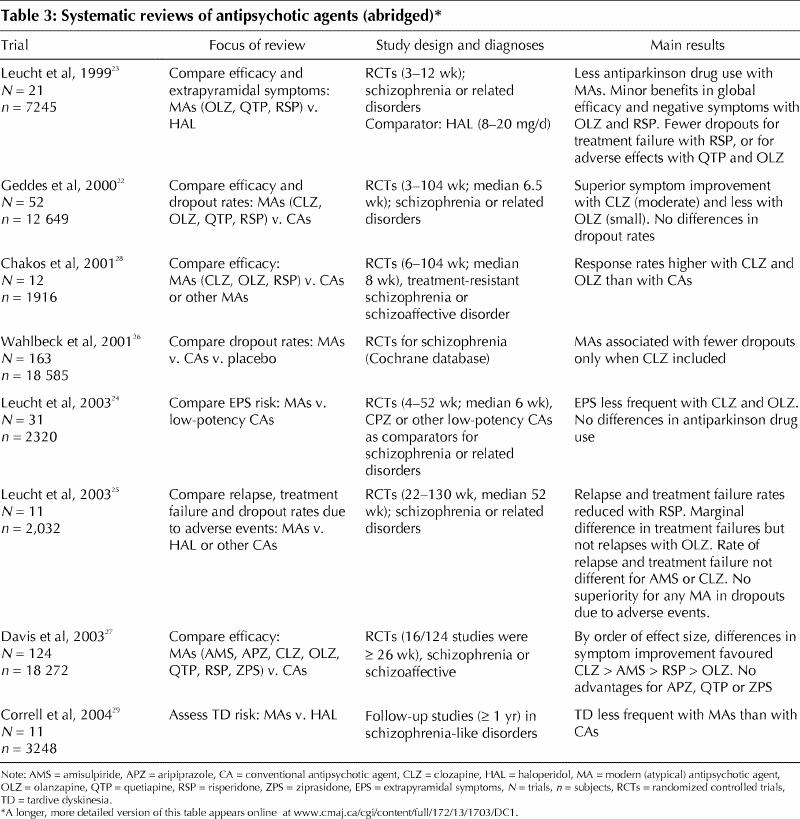
Geddes and associates22 found little advantage in measures of efficacy (improved symptom ratings) or tolerability (dropout rates) of modern antipsychotic agents over moderate daily doses of conventional agents, equivalent to 12 mg or less of haloperidol or 600 mg or less of chlorpromazine, whereas higher doses of comparators were poorly tolerated. Davis and colleagues27 found that some modern antipsychotic drugs (e.g., amisulpride, clozapine, olanzapine, risperidone) but not others (e.g., aripiprazole, quetiapine, ziprasidone) had at least minor efficacy advantages over some older comparators, but they did not find that the dose of conventional antipsychotic drugs influenced outcomes. Leucht and colleagues23 found that the superiority of modern drugs to older ones was variable and limited in terms of treatment dropouts due to inadequate benefits or poor tolerability. For example, quetiapine (at a dose of about 450 mg/d) was associated with 17% fewer dropouts due to adverse effects than various antipsychotic comparators (at haloperidol-equivalent doses of 8–12 mg/d); olanzapine (11–16 mg/d) yielded only 9% fewer dropouts due to treatment failure and 6% fewer due to adverse effects than haloperidol (12–18 mg/d), and risperidone lacked any advantage. These systematic reviews indicate that modern antipsychotic agents are not consistently superior to conventional drugs in efficacy or tolerability and that reported advantages are variable and often minor. The newest antipsychotic agents, ziprasidone and aripiprazole, have undergone fewer comparison trials, and their efficacy compared with that of other antipsychotic drugs remains uncertain.34,35,36
The effects of antipsychotic drugs on negative symptoms of emotional withdrawal and lack of motivation are especially difficult to ascertain because of challenges in rating such features and because of their interactions with depressed mood and reduced motility, both of which can be worsened by antipsychotic drugs.37 In a large pooled comparison of a modern and a conventional antipsychotic agent, involving nearly 2000 subjects given treatment for 6 weeks,38 the advantage (as measured by Cohen's effect size statistic) of olanzapine over haloperidol for negative symptoms was 0.2. Assuming a normal distribution of symptom response, this effect size suggests that 58% of patients taking olanzapine had greater improvement of negative symptoms compared with the mean level of improvement with haloperidol, but it also indicates that 42% did less well with olanzapine.39 Relative efficacy of other modern antipsychotic agents versus older drugs has been similar or even smaller.22 Such findings do not support the hope that modern agents would represent a major advance in the clinical management of negative symptoms.
Impaired cognition is common among patients with chronic psychotic illnesses, but it is also particularly sensitive to dosage of antipsychotic agents and may be worsened by concurrent administration of antiparkinson-anticholinergic drugs. Many studies have compared a newer antipsychotic agent with high doses of haloperidol given with anticholinergics, as needed.40 For example, olanzapine (at a moderate average daily dose of 9.7 mg) was rated superior in several cognitive measures to high daily doses of haloperidol (average dose 27 mg),41 but less so when compared with lower doses of haloperidol (5.5 mg).42 Similarly, a 2-year randomized trial found no difference in cognitive improvements between risperidone (average dose 6 mg/d) and a moderate daily dose of haloperidol (average dose 5 mg/d).43 Such studies do not indicate important advantages of modern over conventional antipsychotics with respect to cognitive function, and any between-drug differences appear to pale in comparison to the often severe cognitive deficits of schizophrenia.42
Positive effects on rates of relapse or readmission to hospital, as well as improvements in occupational and social functioning, quality of life and subjective well-being have been assessed much less consistently than have symptom ratings in most trials comparing treatments of psychotic disorders, even though such outcomes are important from clinical and public health perspectives and may not be predicted well by symptom improvement. In a long-term trial comparing risperidone and haloperidol in patients with chronic psychotic disorders, psychotic symptoms changed little (4.9% improvement and 3.9% worsening respectively), whereas the Kaplan–Meier estimates of relapse risk at the end of the study (34% v. 60% respectively) strongly favoured the modern drug.44 This advantage of risperidone over haloperidol with respect to 1-year relapse risk was replicated in a study of first-episode psychosis (42% v. 55%) despite near identical improvements in symptom measures with low doses (about 3 mg/d) of both agents.45 In contrast, a 12-month study found little difference between treatment with moderate doses of olanzapine (11–16 mg/d) and treatment with haloperidol (11–14 mg/d) combined with benztropine to limit extrapyramidal symptoms in outcomes including psychotic symptoms, negative symptoms, risk of extrapyramidal symptoms or tardive dyskinesia, quality of life and dropout rates.20 Including an antiparkinson agent with moderate doses of haloperidol may have accounted for the lack of difference observed in this trial.46
A striking exception to the inconsistent but generally modest differences between use of a modern antipsychotic drug and appropriately managed treatment with an older drug is clozapine. Patented in 1960, clozapine has shown consistent and substantial superiority to several standard antipsychotic agents in a large number of head-to-head comparisons, with even more striking differences (e.g., in relapse rates and treatment compliance) occurring with prolonged treatment.22,27,28,47 Superiority has been less consistent in comparison with other modern antipsychotic agents,34 except that treatment adherence has been consistently greater with clozapine (60%) than with other modern (41%) or conventional (37%) antipsychotic drugs, perhaps because of the unusually close medical monitoring required for the safe use of clozapine.48 Clozapine remains the drug of choice for treating refractory schizophrenia.49 It also has been associated with reduced or delayed risk of suicide attempts, which led to the precedent-setting approval by the US Food and Drug Administration (FDA) for this effect in 2003.50,51 In a pivotal 18-month comparison of clozapine and olanzapine among 450 patients with schizophrenia who were at relatively high risk of suicide but not necessarily unresponsive to treatment, the risk of suicide attempts and interventions to prevent suicide was moderately lower in the clozapine group (relative risk [RR] 1.32, 95% confidence interval [CI] 1.03– 1.72).50,51
Tolerability and safety of modern antipsychotic agents
The validity of the claim that modern antipsychotic agents carry lesser risks of adverse effects than conventional antipsychotic drugs is challenged by findings from randomized studies that have shown similar rates of treatment discontinuation due to adverse events. The much promoted advantage of reduced risk of extrapyramidal symptoms with modern antipsychotic drugs needs to be balanced against other adverse effects.22,24,25,26
Adverse neurologic effects
The risk of extrapyramidal symptoms varies with specific agents, doses and particular neurologic syndromes. The superiority of the modern agents is clearest for reducing the risk of acute dystonia and late parkinsonian bradykinesia (Table 3). Not surprisingly, in clinical trials, the largest differences in risk have been demonstrated in comparisons between moderate doses of modern antipsychotic drugs and large doses of potent conventional antipsychotic agents without use of a prophylactic anticholinergic. When compared with low-potency antipsychotic drugs (e.g., chlorpromazine) or low to moderate doses of high-potency agents (e.g., haloperidol), or when high-potency agents are combined with anticholinergic drugs at regular doses, the advantage of modern agents of reduced extrapyramidal symptoms is lessened or eliminated.24,46Clozapine and possibly quetiapine appear to be relatively well tolerated by patients with Parkinson's disease who become psychotic with treatment. Risperidone and olanzapine are not well tolerated, and other modern agents have not been adequately investigated.52
Potential superiority of modern antipsychotics is less clear for acute or late dyskinesias, akathisia or neuroleptic malignant syndrome.53,54,55 Regarding tardive dyskinesia, the 1-year incidence was 17 times lower with olanzapine than with haloperidol, each at a dose of about 14 mg/d (0.5% v. 7.4% respectively), but it was not avoided altogether.54 The annualized risk in a randomized trial comparing risperidone (4.9 mg/d) and haloperidol (11.7 mg/d) with a follow-up of at least 1 year was 0.6% and 4.1% respectively. There are no blinded, randomized, long-term follow-up trials comparing other modern agents.29,54
Akathisia, marked by restlessness and anxious agitation, has been associated with virtually all antipsychotic agents, including clozapine.56,57 This clinically distressing idiopathic syndrome is often misdiagnosed as psychotic agitation, typically persists as long as antipsychotic treatment continues and invites mistreatment with more antipsychotic therapy. Lack of an association with antidopaminergic potency suggests that D2-receptor blockade does not explain akathisia, whereas beneficial effects of lipophilic, centrally active β-adrenoceptor antagonists (e.g., propranolol) suggest adrenergic involvement.58
Neuroleptic malignant syndrome is an uncommon, potentially life-threatening cerebrotoxic delirium, with variable fever, autonomic instability, and muscle rigidity with release of circulating creatine kinase and myoglobinuria.59 It is important to emphasize that incomplete forms of neuroleptic malignant syndrome may occur: for example, in patients who are taking clozapine, the syndrome may present with less pronounced muscle rigidity.60,61
Endocrine and metabolic effects
Weight gain is a common adverse effect of several modern and some conventional antipsychotic drugs. In a review of the literature, Allison and coauthors62 found the following mean increases in weight at 10 weeks of treatment: clozapine 4.45 kg, olanzapine 4.15 kg, chlorpromazine 2.58 kg, quetiapine 2.18 kg (at 6 weeks), risperidone 2.10 kg, haloperidol 1.08 kg and ziprasidone 0.04 kg. Weight gain associated with olanzapine tends to plateau over 8–12 months.63 Weight gain is often considered to be clinically significant in antipsychotic drug trials at increases of at least 7%. In a systematic review, Taylor and McAskill64 found the risk of such increases associated with olanzapine, quetiapine and risperidone to be 14%–27% at 6–8 weeks and as high as 40% by 3.5 years. The rates of increases of 10% or more associated with clozapine, olanzapine and risperidone were, respectively, 27%–60% at 3–12 months, 15% at 8 weeks and 6% at 8 weeks.64 Lack of direct long-term comparisons precludes more reliable estimates of the rate and severity of weight gain with specific antipsychotic agents. However, the available data suggest that the risk of weight gain is greatest with clozapine and olanzapine, probably intermediate with quetiapine and low-potency conventional antipsychotic drugs, less with high-potency antipsychotic drugs including risperidone, and minimal with aripiprazole, molindone and ziprasidone. Many patients experience moderate weight gain, but some experience rapid and potentially massive increases that are very difficult to control.65 Children are at particularly high risk of weight gain.66 Mechanisms involved in weight gain and associated adverse metabolic changes probably include sedation and inactivity, perhaps more specific effects of central blockade of H1 and 5-HT2C receptors, as well as specific factors associated with the psychiatric disorder.8,67,68
Hyperlipidemia and hyperglycemia with resultant type 2 diabetes mellitus have been associated with modern antipsychotic agents. Their rates, although not well quantified, probably vary among specific antipsychotic drugs. Using a general practice research database in the United Kingdom, Koro and colleagues69,70 estimated the risk of hyperlipidemia and diabetes associated with olanzapine to be 3.4 (95% CI 1.8–6.4) and 4.2 (95% CI 1.5–12.2) times the risk associated with conventional antipsychotic agents, and 4.6 (95% CI 2.4–8.9) and 5.8 (95% CI 2.0–16.7) times the risk associated with no antipsychotic use. The risk associated with risperidone was much lower, at 0.81 (95% CI 0.4–1.5) and 1.6 (95% CI 0.7–3.8) times the risk of conventional antipsychotic agents, and 1.1 (95% CI 0.6–2.1) and 2.2 (95% CI 0.9–5.2) times the risk associated with no antipsychotic use. In another study, Lambert and colleagues also found an increased risk of diabetes associated with olanzapine (odds ratio [OR] 1.36, 95% CI 1.20-1.53) compared with conventional antipsychotic drugs, but it was less than the risk reported by Koro and colleagues.71 They found a similar increase in risk associated with clozapine (OR 1.34, 95% CI 1.16-1.55). The risks associated with quetiapine (OR 1.2) and risperidone (OR 1.0) were not statistically different from those associated with conventional antipsychotic agents. Overall, the risk of disturbances in both glucose and lipid metabolism appears to be greatest with clozapine and olanzapine, possibly intermediate with quetiapine and the low-potency conventional agents chlorpromazine and thioridazine, and lowest with aripiprazole, risperidone and ziprasidone and with haloperidol and other high-potency conventional antipsychotic agents.72,73,74,75,76 Risks of hyperlipidemia and hyperglycemia are associated with, but not necessarily dependent on, weight gain.76,77 The health implications of long-term therapy with antipsychotic agents that increase the risk of medical morbidity are of growing concern and may well be more dangerous than the extrapyramidal symptoms typically associated with older antipsychotic agents.8,78,79
Moderate hyperprolactinemia is common with conventional antipsychotic drugs. Among the modern antipsychotic agents, the effect is seen only with risperidone, which can elevate prolactin levels at least as much as haloperidol can at comparable doses.80,81 The mean reported prevalence of hyperprolactinemia among patients taking older antipsychotic agents or risperidone is 60% among women and 40% among men.80 The rate of related complications, such as amenorrhea, galactorrhea, and erectile and ejaculatory dysfunction, is about 10%–15%. Aripiprazole, clozapine and quetiapine virtually lack this effect and can be useful for use in patients with prolactin-related adverse effects (amenorrhea, galactorrhea, gynecomastia or sexual dysfunction) or prolactin-dependent metastatic carcinoma of the breast.81
Cardiovascular effects
Several antipsychotic agents are associated with worsening of cardiovascular risk factors, including the previously described weight gain, hyperglycemia and hyperlipidemia. In addition to acute hypotensive effects (Table 4), elevated blood pressure has been reported in patients with weight gain due to antipsychotic use.63 A post hoc analysis involving 113 patients with bipolar disorder taking olanzapine for several months revealed an increase of 13.1% (11 mm Hg) and 9.4% (5.9 mm Hg) in systolic and diastolic blood pressures respectively in those who had above-median changes in body mass index (BMI). Blood pressure was not changed in patients with below-median changes in BMI.63
Table 4

Some antipsychotic drugs are associated with prolongation of ventricular repolarization, which is reflected as a prolongation of the QT interval on an electrocardiogram. Prolongation of the QT interval is associated with an increased risk of polymorphic ventricular tachycardia (torsades de pointes) and sudden cardiac death, especially when the QT interval corrected for rate (QTc) exceeds 500 ms.82 The precise risks for prolonged QT interval are unknown for particular antipsychotic drugs but can occur with both older and modern agents. Among older agents, thioridazine and mesoridazine have been virtually abandoned as a result of this association.83 Among modern agents, ziprasidone may be dangerous when combined with other drugs that result in prolonged QT intervals,84 but when used alone it has not been associated with an increased risk of cardiac arrhythmia or death.85 The effects on the QT interval are likely to be more pronounced when antipsychotic drugs are used in combination with other drugs that prolong the QT interval. The list of such drugs is extensive, although common agents include class I and III antiarrhythmic drugs, tricyclic antidepressants and some antibiotics.
Of great concern are findings associating modern antipsychotic drugs with increased risks of death and cerebral ischemia or stroke among elderly patients receiving therapy for psychotic disorders or the agitation of dementia. On the basis of findings from 17 placebo-controlled trials of modern antipsychotic drugs (aripiprazole, olanzapine, quetiapine and risperidone) involving a total of 5106 elderly patients with dementia-related psychosis, the US FDA issued a warning of a 1.6- to 1.7-fold increase in the risk of death associated with all modern antipsychotics, including clozapine and ziprasidone.86,87,88 Collectively, the mean rate of death was 4.5% with modern antipsychotic drugs and 2.6% with placebo over 10 weeks. The attributable risk of death in this population with conventional antipsychotic drugs remains unknown. Regarding stroke or transient cerebral ischemia, the incidence in 4 placebo-controlled trials was 3.3% with risperidone versus 1.1% with placebo (RR 3.30, 95% CI 1.43– 7.70).89 In 5 other trials, the risk of cerebrovascular events was 1.3% with olanzapine and 0.4% with placebo (RR 3.04, 95% CI 0.70– 13.3; p = 0.043 when controlling for sex, age and type of dementia).90 However, a large retrospective analysis found negligible differences between 14 865 elderly patients taking older antipsychotic drugs and 13 503 taking risperidone (RR 1.04, 95% CI 0.82– 1.31), 3459 taking olanzapine (RR 0.91, 95% CI 0.62– 1.32) or 883 taking quetiapine (RR 0.78, 95% CI 0.38– 1.57).2 Without untreated control groups, these findings are inconclusive about the potential risks of older antipsychotic agents, and comparisons with other modern antipsychotic agents are not available.
Clozapine
Despite its considerable advantages in treating psychosis, clozapine's value is limited by potentially life-threatening agranulocytosis, which has an incidence of about 1% without close monitoring of leukocyte counts, especially during the initial months of treatment.91 In addition, clozapine has a dose-dependent risk of epileptic seizures (about 5% at a daily dose of 600 mg or more);91 potentially massive weight gain;92 possible cardiac damage, including early myocarditis (≤ 19 per 10 000) or late cardiomyopathy (≤ 10 per 10 000);93,94 cerebral intoxication such as that seen with neuroleptic malignant syndrome, with delirium and fever but not muscle rigidity or elevated creatine kinase levels;60 and severe depression of intestinal motility.8,95
Conclusions
Modern antipsychotic drugs (Table 1) offer useful therapeutic options, and the risk of some extrapyramidal symptoms is generally lower with these drugs than with older antipsychotic drugs (Table 3, Table 4). As a group, modern antipsychotic drugs vary greatly in their pharmacology (Table 2) and in their risks of specific adverse effects (Table 4). With the exception of clozapine, they do not represent major gains in effectiveness or tolerability (Table 4). Some present potentially important adverse effects associated with weight gain, including diabetes, hyperlipidemia and hypertension. As a group, they are much more expensive than older antipsychotic drugs, some of which are available as generic drugs (Table 1). It seems reasonable to consider an antipsychotic drug from either group, conventional or modern, for the treatment of psychotic disorders and to inform patients of the relative benefits, risks and costs associated with specific choices.
Supplementary Material
Acknowledgments
We thank Elizabeth Foy and Warren Meek for their valuable contributions to the preparation of this report.
Footnotes
This article has been peer reviewed.
Contributors: Each author contributed meaningfully to the manuscript. David Gardner wrote the original and subsequent drafts of the manuscript. Ross Baldessarini made substantial changes to each draft and identified numerous references. With each draft, Paul Waraich provided input in terms of content, citations and style. All of the authors approved the final version to be published.
Ross Baldessarini was supported, in part, by the Bruce J. Anderson Foundation and the McLean Private Donors Psychopharmacology Research Fund.
Competing interests: None declared for Paul Waraich. David Gardner has received research funding from Janssen-Ortho, Eli Lilly, Novartis, Pfizer and AstraZeneca. Ross Baldessarini is a consultant with Auritec Laboratories, Eli Lilly Laboratories, IFI SpA, Janssen Pharmaceuticals, JDS Corporation and NeuroHealing Pharmaceuticals, is a research collaborator with Auritec Laboratories and has received research grants from Eli Lilly and Janssen Pharmaceuticals.
Correspondence to: Dr. David M. Gardner, Queen Elizabeth II Health Sciences Centre, Rm. AJLB 7517, 5909 Veterans Memorial Lane, Halifax NS B3H 2E2; david.gardner@dal.ca
References
- 1.Leslie DL, Rosenheck RA. From conventional to atypical antipsychotics and back: dynamic processes in the diffusion of new medications. Am J Psychiatry 2002;159:1534-40. [DOI] [PubMed]
- 2.Gill SS, Rochon PA, Herrmann N, Lee PE, Sykora K, Gunraj N, et al. Atypical antipsychotic drugs and risk of ischaemic stroke: population based retrospective cohort study. BMJ 2005;330:445. [DOI] [PMC free article] [PubMed]
- 3.Kane J, Honigfeld G, Singer J, Meltzer HY. Clozapine for the treatment resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1988;45:789-96. [DOI] [PubMed]
- 4.Moller HJ. State of the art of drug treatment of schizophrenia and the future position of the novel/atypical antipsychotics. World J Biol Psychiatry 2000;1:204-14. [DOI] [PubMed]
- 5.Matthysse S. Antipsychotic drug actions: A clue to the neuropathology of schizophrenia? Fed Proc 1973;32:200-5. [PubMed]
- 6.Schotte A, Janssen PFM, Gommeren W, Luyten WHML, Van Gompel P, Lesage AS, et al. Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology (Berl) 1996;124:57-73. [DOI] [PubMed]
- 7.Meltzer HY. An overview of the mechanism of action of clozapine. J Clin Psychiatry 1994;55(Suppl B):47-52. [PubMed]
- 8.Baldessarini RJ, Tarazi FI. Drugs and the treatment of psychiatric disorders: Antipsychotic and antimanic agents. In: Hardman JG, Limbird LE, Gilman AG, editors. Goodman and Gilman's the pharmacological basis of therapeutics. 10th ed. New York: McGraw-Hill Press; 2001. p. 485–520.
- 9.Remington G. Understanding antipsychotic “atypicality”: a clinical and pharmacological moving target. J Psychiatry Neurosci 2003;28:275-84. [PMC free article] [PubMed]
- 10.Goodnick PJ. Ziprasidone: profile on safety. Expert Opin Pharmacother 2001;2:1655-62. [DOI] [PubMed]
- 11.Grunder G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications. Arch Gen Psychiatry 2003;60:974-7. [DOI] [PubMed]
- 12.Farde L, Nordstrom AL, Wiesael FA. Pauli S, Halldin C, Sedvall G. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine: relation to extrapyramidal side effects. Arch Gen Psychiatry 1992;49:538-44. [DOI] [PubMed]
- 13.Suhara T, Okauchi T, Sudo Y, Takano A, Kawabe K, Maeda J, et al. Clozapine can induce high dopamine D(2) receptor occupancy in vivo. Psychopharmacology (Berl) 2002;160:107-12. [DOI] [PubMed]
- 14.Kapur S, Zipursky R, Jones C, Remington G, Houle S. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry 2000;157:514-20. [DOI] [PubMed]
- 15.Baldessarini RJ, Tarazi FI. Brain dopamine receptors: a primer on their current status, basic and clinical. Harv Rev Psychiatry 1996;3:301-25. [DOI] [PubMed]
- 16.Roth BL, Meltzer HY. The role of serotonin in schizophrenia. In: Bloom FE, Kupfer DJ, editors. Psychopharmacology: the fourth generation of progress. New York: Raven Press; 1995. p. 1215-27.
- 17.Meltzer HY. Mechanism of action of atypical antipsychotic drugs. In: Davis KL, Charney D, Coyle JT, Nemeroff C, editors. Neuropsychopharmacology: the fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins; 2002. p. 819-33.
- 18.Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry 2002;47:27-38. [PubMed]
- 19.Kapur S, Seeman P. Does fast dissociation from the dopamine D2 receptors explain the action of atypical antipsychotics? Am J Psychiatry 2001;158:360-9. [DOI] [PubMed]
- 20.Rosenheck R, Perlick D, Bingham S, Liu-Mares W, Collins J, Warren S, et al. Effectiveness and cost of olanzapine and haloperidol in the treatment of schizophrenia: a randomized controlled trial. JAMA 2003;290:2693-702. [DOI] [PubMed]
- 21.Green M. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 1996;153:321-30. [DOI] [PubMed]
- 22.Geddes J, Freemantle N, Harrison P, Bebbington P. Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ 2000;321:1371-6. Additional data available at http://bmj.bmjjournals.com/cgi/content/full/321/7273/1371/DC1/5 (accessed 2004 June 14). [DOI] [PMC free article] [PubMed]
- 23.Leucht S, Pitschel-Walz G, Abraham D, Kissling W. Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo. A meta-analysis of randomized controlled trials. Schizophr Res 1999;35:51-68. [DOI] [PubMed]
- 24.Leucht S, Wahlbeck K, Hamann J, Kissling W. New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 2003;361:1581-9. [DOI] [PubMed]
- 25.Leucht S, Barnes TRE, Kissling W, Engel RR, Correll C, Kane JM. Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and exploratory meta-analysis of randomized, controlled trials. Am J Psychiatry 2003;160:1209-22. [DOI] [PubMed]
- 26.Wahlbeck K, Tuunainen A, Ahokas A, Leucht S. Dropout rates in randomized antipsychotic drug trials. Psychopharmacology (Berl) 2001;155:230-3. [DOI] [PubMed]
- 27.Davis JM, Chen N, Glick ID. A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 2003;60:553-64. [DOI] [PubMed]
- 28.Chakos M, Lieberman J, Hoffman E, Bradford D, Sheitman B. Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: a review and meta-analysis of randomized trials. Am J Psychiatry 2001;158:518-26. [DOI] [PubMed]
- 29.Correll CU, Leucht S, Kane JM. Lower risk for tardive dyskinesias associated with second-generation antipsychotics: a systematic review of 1-year studies. Am J Psychiatry 2004;161:414-25. [DOI] [PubMed]
- 30.Bagnall AM, Jones L, Ginnelly L, Lewis R, Glanville J, Gilbody S, et al. A systematic review of atypical antipsychotic drugs in schizophrenia. Health Technol Assess 2003;7:1-193. [DOI] [PubMed]
- 31.Lewis DA. Atypical antipsychotic medications and the treatment of schizophrenia. Am J Psychiatry 2002;159:177-9. [DOI] [PubMed]
- 32.Mohr P, Czobor P. Subject selection for the placebo- and comparator-controlled trials of neuroleptics in schizophrenia. J Clin Psychopharmacol 2000;20:240-5. [DOI] [PubMed]
- 33.Waraich PS, Adams CE, Roque M, Hamill KM, Marti J. Haloperidol dose for the acute phase of schizophrenia. Cochrane Database Syst Rev 2002;(3):CD001951. [DOI] [PubMed]
- 34.Tuunainen A, Wahlbeck K, Gilbody SM. Newer atypical antipsychotic medication versus clozapine for schizophrenia. Cochrane Database Syst Rev 2000;(2):CD000966. [DOI] [PubMed]
- 35.Addington DE, Pantelis C, Dineen M, Benattia I, Romano SJ. Efficacy and tolerability of ziprasidone versus risperidone in patients with acute exacerbation of schizophrenia or schizoaffective disorder: an 8-week, double-blind, multicenter trial. J Clin Psychiatry 2004;65:1624-33. [DOI] [PubMed]
- 36.El-Sayeh HG, Morganti C. Aripiprazole for schizophrenia [Cochrane review]. In: The Cochrane Library; Issue 2, 2004. Oxford: Update Software.
- 37.Möller HJ. Management of the negative symptoms of schizophrenia: new treatment options. CNS Drugs 2003;17:793-823. [DOI] [PubMed]
- 38.Tollefson GD, Beasley CM, Tran PV, Street JS, Krueger A, Tamura RN, et al. Olanzapine versus haloperidol in the treatment of schizophrenia and schizoaffective and schizophreniform disorders: results of an international collaborative trial. Am J Psychiatry 1997;154:457-65. [DOI] [PubMed]
- 39.Coe R. What is an effect size: a guide for users. Durham (UK): Evidence-Based Education UK; 2000. Available: www.cemcentre.org/ebeuk/research/effectsize/ESguide.htm (accessed 2005 May 19).
- 40.Harvey PD, Keefe RSE. Studies of cognitive change in patients with schizophrenia following novel antipsychotic treatment. Am J Psychiatry 2001;158:176-84. [DOI] [PubMed]
- 41.Bilder RM, Goldman RS, Volavka J, Czobor P, Hoptman M, Sheitman B, et al. Neurocognitive effects of clozapine, olanzapine, risperidone, and haloperidol in patients with chronic schizophrenia or schizoaffective disorder. Am J Psychiatry 2002;159:1018-28. [DOI] [PubMed]
- 42.Keefe RS, Seidman LJ, Christensen BK, Hamer RM, Sharma T, Sitskoorn MM, et al. Comparative effect of atypical and conventional antipsychotic drugs on neurocognition in first-episode psychosis: a randomized, double-blind trial of olanzapine versus low doses of haloperidol. Am J Psychiatry 2004;161:985-95. [DOI] [PubMed]
- 43.Green MF, Marder SR, Glynn SM, McGurk SR, Wirshing WC, Wirshing DA, et al. The neurocognitive effects of low-dose haloperidol: a two-year comparison with risperidone. Biol Psychiatry 2002;51:972-8. [DOI] [PubMed]
- 44.Csernansky JG, Mahmoud R, Brenner R. The Risperidone-USA-79 Study Group. A comparison of risperidone and haloperidol for the prevention of relapse in patients with schizophrenia [published erratum in N Engl J Med 2002;346:1424]. N Engl J Med 2002;346:16-22. [DOI] [PubMed]
- 45.Schooler N, Rabinowitz J, Davidson M, Emsley R, Harvey PD, Kopala L, et al; Early Psychosis Global Working Group. Risperidone and haloperidol in first-episode psychosis: a long-term randomized trial. Am J Psychiatry 2005;162:947-53. [DOI] [PubMed]
- 46.Rosenheck RA. Effectiveness vs. efficacy of second-generation antipsychotics: haloperidol without anticholinergics as a comparator. Psychiatr Serv 2005;56:85-92. [DOI] [PubMed]
- 47.Wahlbeck K, Cheine M, Essali A, Adams C. Evidence of clozapine's effectiveness in schizophrenia: systematic review and meta-analysis of randomized trials. Am J Psychiatry 1999;156:990-9. [DOI] [PubMed]
- 48.Gilmer TP, Dolder CR, Lacro JP, Folsom DP, Lindamer L, Garcia P, et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry 2004;161:692-9. [DOI] [PubMed]
- 49.Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry 2004;161(2 Suppl):1-56. [PubMed]
- 50.Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003;60:82-91. [DOI] [PubMed]
- 51.Hennen J, Baldessarini RJ. Reduced suicidal risk during treatment with clozapine: A meta-analysis. Schizophr Res 2005;73:139-45. [DOI] [PubMed]
- 52.Tarsy D, Baldessarini RJ, Tarazi FI. Atypical antipsychotic agents: effects on extrapyramidal functions. CNS Drugs 2002;16:23-45. [DOI] [PubMed]
- 53.Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull 2003;29:547-58. [DOI] [PubMed]
- 54.Beasley CM, Dellva MA, Tamura RN, Morgenstern H, Glazer WM, Ferguson K, et al. Randomised double-blind comparison of the incidence of tardive dyskinesia in patients with schizophrenia during long-term treatment with olanzapine or haloperidol. Br J Psychiatry 1999;174:23-30. [DOI] [PubMed]
- 55.Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T. Neuroleptic malignant syndrome and atypical antipsychotic drugs. J Clin Psychiatry 2004;65:464-70. [DOI] [PubMed]
- 56.Tarsy D, Baldessarini RJ, Tarazi FI. Effects of newer antipsychotics on extrapyramidal function. CNS Drugs 2002;16:23-45. [DOI] [PubMed]
- 57.Gogtay N, Sporn A, Alfaro CL, Mulqueen A, Rapoport JL. Clozapine-induced akathisia in children with schizophrenia. J Child Adolesc Psychopharmacol 2002;12:347-9. [DOI] [PubMed]
- 58.Lima AR, Bacalcthuk J, Barnes TR, Soares-Weiser K. Central action beta-blockers versus placebo for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev 2004 Oct 18;(4):CD001946. [DOI] [PMC free article] [PubMed]
- 59.Chandran GJ, Mikler JR, Keegan DL. Neuroleptic malignant syndrome: case report and discussion. CMAJ 2003;169(5):439-42. [PMC free article] [PubMed]
- 60.Karagianis JL, Phillips LC, Hogan KP, LeDrew KK. Clozapine-associated neuroleptic malignant syndrome: two new cases and a review of the literature. Ann Pharmacother 1999;33:623-30. [DOI] [PubMed]
- 61.Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T. Neuroleptic malignant syndrome and atypical antipsychotic drugs. J Clin Psychiatry 2004;65:464-70. [DOI] [PubMed]
- 62.Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999;156:1686-96. [DOI] [PubMed]
- 63.Hennen J, Perlis RH, Sachs G, Tohen M, Baldessarini RJ. Weight gain during treatment of bipolar I patients with olanzapine. J Clin Psychiatry 2004;65:1679-87. [DOI] [PubMed]
- 64.Taylor DM, McAskill R. Atypical antipsychotics and weight gain–a systematic review. Acta Psychiatr Scand 2000;101:416-32. [DOI] [PubMed]
- 65.Bryden KE, Kopala LC. Body mass index increase of 58% associated with olanzapine. Am J Psychiatry 1999;156:1835-6. [DOI] [PubMed]
- 66.Safer DJ. Comparison of risperidone-induced weight-gain across the age-span. J Clin Psychopharmacol 2004;24:429-36. [DOI] [PubMed]
- 67.Wirshing DA. Schizophrenia and obesity: impact of antipsychotic medications. J Clin Psychiatry 2004;65(Suppl 18):13-26. [PubMed]
- 68.Allison DB, Casey DE. Antipsychotic-induced weight gain: a review of the literature. J Clin Psychiatry 2001;62(Suppl 7):22-31. [PubMed]
- 69.Koro CE, Fedder DO, L'Italien GJ, Weiss S, Magder LS, Kreyenbuhl J, et al. An assessment of the independent effects of olanzapine and risperidone exposure on the risk of hyperlipidemia in schizophrenia patients. Arch Gen Psychiatry 2002;59:1021-26. [DOI] [PubMed]
- 70.Koro CE, Fedder DO, L'Italien GJ, Weiss SS, Magder LS, Kreyenbuhl J, et al. Assessment of independent effect of olanzapine and risperidone on risk of diabetes among patients with schizophrenia: population based nested case-control study. BMJ 2002;325:243-7. [DOI] [PMC free article] [PubMed]
- 71.Lambert BL, Chou CH, Chang KY, Tafesse E, Carson W. Antipsychotic exposure and type 2 diabetes among patients with schizophrenia: a matched case-control study of California Medicaid claims. Pharmacoepidemiol Drug Saf 2005; [Epub ahead of print] [DOI] [PubMed]
- 72.Cassidy F, Ahearn E, Carroll BJ. Elevated frequency of diabetes mellitus in hospitalized manic-depressive patients. Am J Psychiatry 1999;156:1417-20. [DOI] [PubMed]
- 73.Gianfrancesco F, White R, Wang R, Nasrallah HA. Antipsychotic-induced type 2 diabetes: evidence from a large health plan database. J Clin Psychopharmacol 2003;23:328-35. [DOI] [PubMed]
- 74.Meyer JM, Koro CE. The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophr Res 2004;70:1-17. [DOI] [PubMed]
- 75.Jin H, Meyer JM, Jeste DV. Atypical antipsychotics and glucose dysregulation: a systematic review. Schizophr Res 2004;71:195-212. [DOI] [PubMed]
- 76.Casey DE. Dyslipidemia and atypical antipsychotic drugs. J Clin Psychiatry 2004;65(Suppl 18):27-35. [PubMed]
- 77.Newcomer JW. Abnormalities of glucose metabolism associated with atypical antipsychotic drugs. J Clin Psychiatry 2004;65(Suppl 18):36-46. [PubMed]
- 78.Casey DE, Haupt DW, Newcomer JW, Henderson DC, Sernyak MJ, Davidson M, et al. Antipsychotic-induced weight gain and metabolic abnormalities: Implications for increased mortality in patients with schizophrenia. J Clin Psychiatry 2004;65(Suppl 7):4-18. [PubMed]
- 79.Fontaine KR, Heo M, Harrigan EP, Shear CL, Lakshminarayanan M, Casey DE, et al. Estimating the consequences of anti-psychotic induced weight gain on health and mortality rate. Psychiatry Res 2001;101:277-88. [DOI] [PubMed]
- 80.Kleinberg DL, Davis JM, de Coster R, Van Baelen B, Brecher M. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61. [DOI] [PubMed]
- 81.Haddad PM, Wieck A. Antipsychotic-induced hyperprolactinaemia: mechanisms, clinical features and management. Drugs 2004;64:2291-314. [DOI] [PubMed]
- 82.Zareba W, Moss AJ. QT interval and its drug-induced prolongation. In: Gussak I, Antzelevitch C, editors. Cardiac repolarization bridging basic and clinical science. Totowa (NJ): Humana Press; 2003. p.311-28.
- 83.Haddad PM, Anderson IM. Antipsychotic-related QTc prolongation, torsades de pointes and sudden death. Drugs 2002;62:1649-71. [DOI] [PubMed]
- 84.Pfizer Inc. FDA Psychopharmacological Drugs Advisory Committee Briefing document for Zeldox® capsules (ziprasidone HCl). Pfizer Inc.; 2000. Available: www.fda.gov/ohrms/dockets/ac/00/backgrd/3619b1a.pdf (accessed 2005 May 19).
- 85.Kutcher S, Brooks SJ, Gardner DM, Honer B, Kopala L, Labelle A, et al. Expert Canadian consensus suggestions on the rational, clinical use of ziprasidone in the treatment of schizophrenia and related psychotic disorders. Neuropsychiatr Dis Treat 2005;1(2):89-108. [DOI] [PMC free article] [PubMed]
- 86.FDA issues public health advisory for antipsychotic drugs used for treatment of behavioral disorders in elderly patients [FDA Talk Paper]. Rockville (MD): US Food and Drug Administration; 2005. Available: www.fda.gov/bbs/topics/ANSWERS/2005/ANS01350.html (accessed 2005 May 19).
- 87.Risperdal (risperidone) tablets/oral solution [product monograph]. Titusville (NJ): Janssen Pharmaceutica Products, LP; 2005. Available: www.janssen.com/active/janus/en_US/assets/jan/risperdal.pdf (accessed 2005 May 19).
- 88.Olanzapine (marketed as Zyprexa): increased mortality in patients with dementia-related psychosis [FDA Alert 4/11/05]. Rockville (MD): US Food and Drug Administration; 2005. Available: www.fda.gov/cder/drug/InfoSheets/HCP/olanzapineHCP.pdf (accessed 2005 May 10).
- 89.Summary of clinical trial data on cerebrovascular adverse events (CVAEs) in randomized clinical trials of risperidone conducted in patients with dementia. London (UK): Medicines and Healthcare products Regulatory Agency; 2004. Available: http://medicines.mhra.gov.uk/ourwork/monitorsafequalmed/safetymessages/risperidoneclinicaltrialdata_final.pdf (accessed 2005 May 19).
- 90.Health Canada endorsed important safety information on Zyprexa (olanzapine) [Dear Healthcare Professional letter]. Toronto: Eli Lilly Canada Inc.; 2004 May 10. Available: www.hc-sc.gc.ca/hpfb-dgpsa/tpd-dpt/zyprexa_hpc_e.html (accessed 2005 May 19).
- 91.Clozaril [product monograph]. Compendium of pharmaceutical specialties. Ottawa: Canadian Pharmacists Association; 2004.
- 92.Theisen FM, Cichon S, Linden A, Martin M, Remschmidt H, Hebebrand J. Clozapine and weight gain. Am J Psychiatry 2001;158:816. [DOI] [PubMed]
- 93.Wehmeier PM, Heiser P, Remschmidt H. Myocarditis, pericarditis and cardiomyopathy in patients treated with clozapine. J Clin Pharm Ther 2005;30:91-6. [DOI] [PubMed]
- 94.Killian JG, Kerr K, Lawrence C, Celermajer DS. Myocarditis and cardiomyopathy associated with clozapine. Lancet 1999;354:1841-5. [DOI] [PubMed]
- 95.Levin TT, Barrett J, Mendelowitz A. Death from clozapine-induced constipation: case report and literature review. Psychosomatics 2002;43:71-3. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


