Abstract
Suicide is a significant leading cause of death among young people, particularly those struggling with mental disorders. The present study utilised data from 230 young people (aged 16–18 years) undergoing a transitional care process from Child and Adolescent Mental Health Services to Adult Mental Health Services within the MILESTONE European project (2014–2019), a longitudinal cluster randomised controlled trial. The objectives of this study were to monitor temporal patterns of general health and social functioning over two years, to detect sex differences, and to identify factors associated with Suicidal Thoughts and Behaviours (STB) at the first and last time points. The results demonstrate a decrease in STB over the two-year follow-up period among all participants. Females exhibited a higher prevalence of STB across all time points, whereas males only exhibited STB at the nine-month follow-up. The most influential factors associated with STB were previous suicide attempts and mood disorders at baseline, and mood disorders and relational problems at the end of follow-up. These findings emphasise the importance of monitoring STB and informing young people undergoing a transitional care period about its key risk factors. Moreover, sex differences in STB suggest the need for different preventive strategies for males and females.
Keywords: Suicidal ideation, Suicidal behaviour, Adolescence, Child and adolescent mental health services, Adult mental health services, Care transition
Subject terms: Risk factors, Health services, Psychiatric disorders
Introduction
Suicide represents a major leading cause of death among young people aged between 15 and 29 years old1,2, and the impact of such a tragic event on families and friends is magnified when the individual is a young adolescent3–5. Notably, 90% of people who die by suicide have suffered from mental disorders6,7. Therefore, a deeper understanding of the dynamics leading up to suicide risk in young individuals suffering from a mental disorder is of major clinical and public health interest. Modern suicidology tends to evaluate the causes and underlying mechanism of suicide without considering it as an epiphenomenon of a mental disorder but as a complex combination of risk and protective factors that threaten the stability of the individual8. Academics’ interest in suicide prevention, therefore, focuses on possible antecedents to determine which individuals are at risk of attempting suicide9. The Suicidal Thoughts and Behaviours (STB) continuum encompasses the progression from suicidal thoughts to actions. It begins with suicidal ideation, where an individual contemplates ending their life, which can be passive (wishing one were dead) or active (considering specific methods). If these thoughts advance, they may lead to suicidal planning, where the individual starts detailing the method and means to die by suicide. The continuum culminates in a suicidal attempt, an actual effort to end one’s life, which can vary in severity and intentionality. Recognising where a person is on this continuum is crucial for effective intervention and prevention. The terminology STB will be employed in this paper to align with recent guidelines by De Leo et al.10, which advocate for a standardised and consensus-based nomenclature in suicidology. This approach distinguishes between the aforementioned stages clarifying the continuum from thoughts to actions. The precision in using these terms helps differentiate non-fatal suicidal behaviours from suicide attempts, as well as account for varying degrees of intent, thus enhancing clarity in both academic and clinical contexts. Prior research identified factors such as previous non-fatal suicide attempts, psychiatric symptoms (especially mood disorders), personality or temperamental factors (e.g., aggressive tendencies, impulsivity, low prosociality, and low self-esteem), trauma and abuse, lack of social support, and relational problems among the most significant associated factors for suicidal behaviour11–16. However, the most influential factors related to STB10 in young people during the transition process from Child and Adolescent Mental Health Services (CAMHS) to Adult Mental Health Services (AMHS) remain an unexplored research area. Additionally, some typical characteristics of adolescence, compared to adulthood, such as more frequent high-intensity emotions, with a prospective increase of negative emotions from early to late adolescence, and experiencing higher emotional instability17, highlight the clinical relevance of monitoring STB over time. Though fluctuations in suicidal ideation are even more pronounced among adolescents who struggle with mental disorders, identifying associated factors may improve our understanding of the susceptibility to such variations, and ultimately contribute to the implementation of effective prevention strategies. Additionally, this challenge is compounded by the fact that the absence of previous suicidal acts does not necessarily rule out the risk of suicide, making it difficult to exclude risk for individuals who have never attempted suicide before10,18.
Another aspect that deserves attention relates to potential sex differences in STB, a phenomenon commonly referred to as the 'gender paradox in suicide’19–21, with suicide attempts more common among females, and suicides in males (by suicide, we refer to the act that results in death)22,23. Female prevalence in non-fatal suicidal behaviour among adolescents can be partly explained by emotional instability and behavioural problems typical of this age17,24, but more evidence is needed to verify the gender paradox in young people suffering from a mental disorder. Moreover, no prior research explored sex differences in suicidality in young people facing the transition process from CAMHS to AMHS.
The MILESTONE project (2014–2019) was a longitudinal cluster randomised controlled trial (cRCT) undertaken with the primary objective of enhancing the comprehension of, and thereby strengthening, transitional care processes from CAMHS to AMHS across diverse healthcare systems in different European countries25. It proposed an innovative transitional care model that encompassed an evidence-based decision-making process and managed transition, integrating fundamental principles of continuity of care: adequate information, appropriate collaborative efforts, therapeutic and relational continuity, and engagement with AMHS25. Specifically, the present study was based on the Italian adolescents’ subsample of MILESTONE. In Italy, a comprehensive nationwide cohort study on adolescents aged between 10 and 19 revealed a suicide rate of 1.71 per 100.000 person-years26, while the most up-to-date European statistics registered a suicide rate of 5.9 per 100.000 person-years when considering the whole Italian population27. Therefore, we explored whether the transition process from CAMHS to AMHS, or other treatment providers (e.g., general practitioners, private clinicians, etc.) was related to STB among italian adolescents. Specifically, we aimed to (i) investigate temporal patterns of general health and social functioning before, during, and after the transition from CAMHS to AMHS or other treatment providers; (ii) examine sex differences in STB at baseline (T1), at 9 months (T2), at 15 months (T3), and at 24 (months); (iii) and determine the importance of different factors associated with STB and that might be useful in outlining a risk profile in future research.
We hypothesised that: (i) given the developmental stage of young people’s lives and the treatments received, many of them would show improvements in general health and social functioning over the two years; (ii) females would exhibit higher levels of STB compared to males; (iii) environmental and social factors (such as lack of support and relational problems) would have been more associated with STB at T4 compared to T1, as these factors are more implicated during the transition process rather than stable biopsychosocial factors (such as mood disorders, previous suicide attempts, aggressive tendencies, and trauma and abuse).
Results
Sociodemographic and clinical characteristics of participants
Table 1 shows the sociodemographic characteristics of the 230 adolescents in treatment at 11 Italian CAMHS included in the MILESTONE study. Adolescents aged 16–18 years old were involved in the study, with a mean age of 17.7 years (SD = 0.29). Of them, 88.3% had a white European ethnicity and 53% were females. Over 81% of the participants had utilised CAMHS services for at least 6 months, with 10% undergoing treatment for 5 to 10 years. About a third of participants had been up to one year in CAMHS treatment, while approximately 17% had been 5 years or more in treatment. Regarding household composition, 58.4% of adolescents lived with both parents, while 16.0% lived with a single parent, 7.8% with one parent and a new partner, and only 4.8% were living in residential facilities. Furthermore, 14.3% of participants reported previous suicide attempts, while 9.6% didn’t answer this question.
Table 1.
Sociodemographic characteristics of the sample at baseline.
| Sociodemographic characteristics | N | % |
|---|---|---|
| Sample | 230 | 100 |
| Age (m, SD) | 17.68, 0.29 | 0.3 |
| Sex | ||
| Males | 108 | 47 |
| Females | 122 | 53 |
| Ethnicity | ||
| White | 203 | 88.3 |
| Other ethnic groups | 17 | 7.4 |
| Missing | 10 | 4.3 |
| Education level | ||
| Primary | 3 | 1.3 |
| Secondary school | 213 | 92.6 |
| Further/higher education | 1 | 0.4 |
| Missing | 13 | 5.6 |
| Usual living situation | ||
| Both parents | 134 | 58.3 |
| One parent and new partner | 18 | 7.8 |
| One parent only | 37 | 16.1 |
| Adoptive or foster parents | 5 | 2.2 |
| Independent (alone, roommates, partner) | 2 | 0.9 |
| Residential care | 11 | 4.8 |
| Other | 12 | 5.2 |
| Missing | 11 | 4.8 |
| Time spent under CAMHS care (years) | ||
| 0–1 | 70 | 30.4 |
| 1–2 | 45 | 19.6 |
| 2–5 | 56 | 24.3 |
| 5–10 | 23 | 10.0 |
| 10 + | 16 | 7.0 |
| Missing | 20 | 8.7 |
| Previous suicide attempts | ||
| No | 175 | 76.1 |
| Yes | 33 | 14.3 |
| Missing | 22 | 9.6 |
Regarding clinical characteristics, neurodevelopmental disorders (21.3%) were the most prevalent diagnoses, followed by mood disorders (14.8%), and anxiety disorders (13.9%); 84.3% of the participants reported no other psychiatric diagnosis in comorbidity (Table 2).
Table 2.
Clinical characteristics of the sample at baseline.
| Clinical characteristics | ||
|---|---|---|
| Primary diagnosis | ||
| Neurodevelopmental disorders | 49 | 21.3 |
| Mood disorders (depressive, bipolar and related disorders) | 34 | 14.8 |
| Anxiety disorders | 32 | 13.9 |
| Eating disorders | 24 | 10.4 |
| Personality disorders | 22 | 9.6 |
| Attention deficit hyperactivity disorder | 15 | 6.5 |
| Autistic spectrum disorders | 11 | 4.8 |
| Conduct disorders | 10 | 4.3 |
| Schizophrenia spectrum disorders and other psychotic disorders | 10 | 4.3 |
| Trauma-and stressor-related disorders | 8 | 3.5 |
| Obsessive–compulsive and related disorders | 6 | 2.6 |
| Gender dysphoria | 3 | 1.3 |
| Somatic symptoms & related disorders | 3 | 1.3 |
| Unspecified/other mental disorders | 3 | 1.3 |
| Diagnoses in comorbidity | ||
| None | 194 | 84.3 |
| Anxiety disorders | 15 | 6.5 |
| Mood disorders (depressive, bipolar and related disorders) | 9 | 3.9 |
| Conduct disorders | 2 | 0.9 |
| Obsessive–compulsive and related disorders | 4 | 1.7 |
| Schizophrenia spectrum disorders and other psychotic disorders | 3 | 1.3 |
| Somatic symptoms & related disorders | 3 | 1.3 |
Temporal patterns of general health and social functioning over 24 months-period
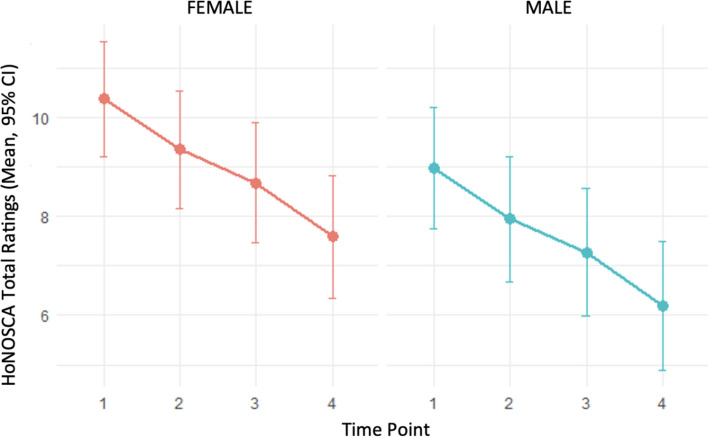
We found a global decrease in HoNOSCA total ratings over the study period, indicating an improvement in general health and social functioning levels. Sex comparisons show that across all time points female subjects had higher HoNOSCA total ratings than male subjects (Fig. 1). A Likelihood Ratio Test (LRT) was performed to evaluate the interaction between sex and time points, revealing no statistical significance (p = 0.265). Sex differences (p = 0.037) and time points (p < 0.001), considered as a continuous variable, showed a significant effect on HoNOSCA total ratings. Moreover, we found a general decreasing trend over time for both sexes. In particular, decreases of 2.78 and 2.77 points in HoNOSCA total ratings mean were observed respectively for female and male subjects. Interestingly, the general improvement was visible both in the subsample of adolescents involved in the experimental Managed Transition (N = 63) and in the rest of the sample assigned to Treatment As Usual (TAU) (N = 167).
Fig. 1.
HoNOSCA total rating trends at the four time points by sex.
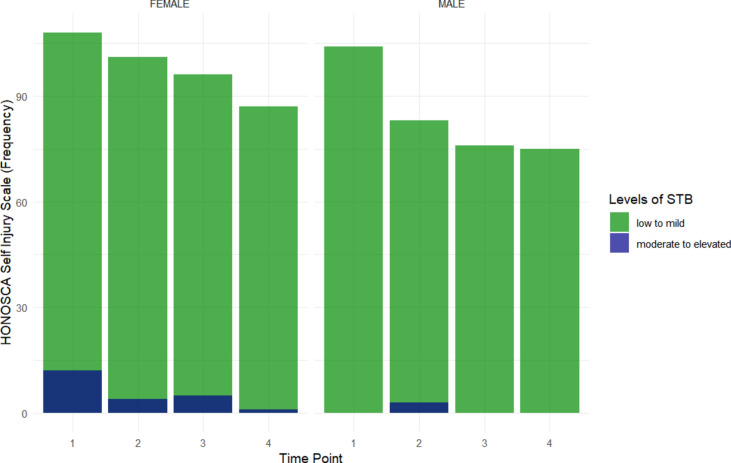
Sex differences in STB over 24 months-period
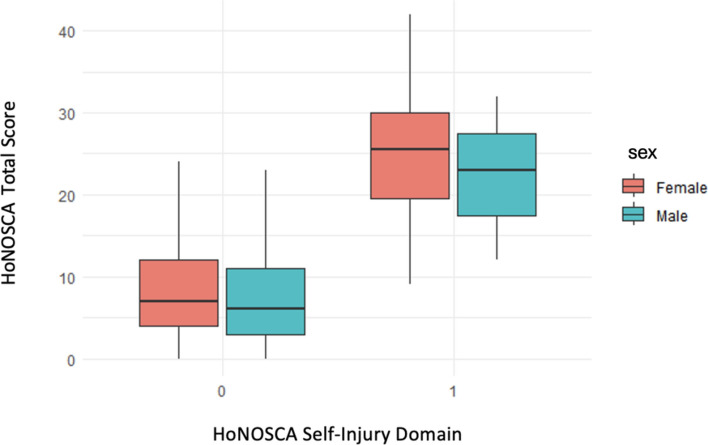
As shown in Fig. 2, female subjects had higher frequencies of STB than males. From T1 to T4, the number of female adolescents exhibiting STB decreased (12 at T1, 4 at T2, 5 at T3, and 1 at T4), according to the HoNOSCA self-injury ratings. Being male was less associated with STB across all time-points, except for T2. Furthermore, the model coefficients applied to determine the relationship among the underlying factors (Table 3) showed a statistically significant coefficient associated with HoNOSCA total ratings ( p < 0.001)—so that an increment of 1 point led to an increase of 27% on the levels of STB severity. Moreover, with an LRT test, no significant interaction was found between sex and time point, considered as a continuous variable, suggesting that the highest female odds of STB compared to males were constant across the entire follow-up period. Differences between HoNOSCA total and self-injury domain ratings by sex are shown in Fig. 3. Low levels of STB were associated with lower HoNOSCA total ratings, while elevated levels of STB were associated with higher HoNOSCA total ratings.
Fig. 2.
Participants who reported different levels of STB based on the HoNOSCA self-injury domain ratings by sex.
Table 3.
STB trends over four time points based on the HoNOSCA self-injury domain ratings.
| Coefficients | OR | 95% CI | p-value |
|---|---|---|---|
| intercept | 0.00018 | 0.00–0.017 | < 0.001 |
| tpoint | 0.829 | 0.434–1.583 | 0.569 |
| HoNOSCApt | 1.374 | 1.178–1.603 | < 0.001 |
| Sex (= Male) | 0.087 | 0.009–0.807 | 0.032 |
Fig. 3.
Differences in STB severity (ratings 3 and 4 of the HoNOSCA self-injury domain) compared to the HoNOSCA total ratings by sex.
Factors associated with STB
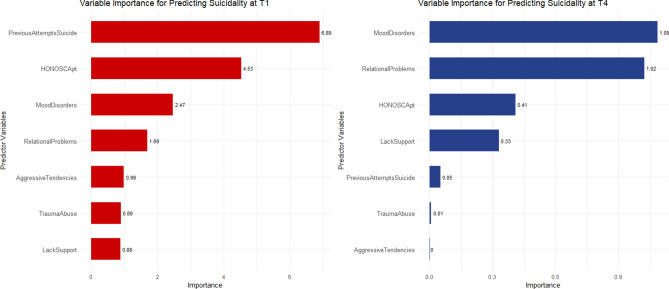
At baseline (T1) the most influential factors associated with STB in the applied model were previous attempts of suicide (importance = 6.89), HoNOSCA total ratings (importance = 4.53), and a diagnosis of mood disorder (importance = 2.47). Similarly, at T4 a diagnosis of mood disorder (importance = 1.09) and HoNOSCA total ratings (importance = 0.41) were identified among the most influential factors associated with higher levels of STB, but also relational problems (importance = 1.02) (Fig. 4).
Fig. 4.
Comparison of factors’ importance in the association with STB at T1 and T4.
Discussion
The present study longitudinally investigated sex differences in general health and social functioning as well as in STB over two years in a large sample of adolescents in treatment at 11 Italian CAMHS. Our findings indicate a consistent improvement in health outcomes over four time points, suggesting that many young people in a developmental stage of their life and in treatment at mental health services show improvements in several life domains, regardless of the type of transitional care they receive25. Significant differences emerged between males and females, with females having higher HoNOSCA ratings compared to males, reflecting worse physical, behavioral, and emotional conditions, and a higher prevalence of STB. Moreover, we identified the most associated factors with STB in young people facing a transition from CAMHS to AMHS (and to other health providers), above all mood disorders, previous suicide attempts, and relational problems.
Females consistently had higher HoNOSCA total ratings than males, indicating worse physical, emotional, and behavioural conditions. These findings align with prior investigations indicating a greater incidence and prevalence of mental health disorders among females compared to males in adolescence and young adulthood28. As a result, it is not surprising that females also exhibit higher levels of STB, highlighting the strong connection between general health, particularly mental health, and domains related to suicidal behaviours and non-fatal self-harm29,30, as well as their well-known propensity for suicide ideation, planning, or attempts compared to males31. These results are in line with the growing need for psychiatric consultations related to STB in Italy before the COVID pandemic, especially among female adolescents29. Moreover, at least partially in line with the sex differences in STB documented in the literature20,21, our findings revealed a higher prevalence of STB among young females compared to males, but no mortality comparison could be done since no suicide deaths were recorded in our adolescent sample during the two years. Prior research showed that in young adolescents, females are three to nine times more likely to attempt suicide, while men are up to four times more likely to die by suicide32,33. Possible explanations for this phenomenon may have to do with means, with females often choosing methods that have less probability of leading to death compared to males34, and with the higher prevalence of mental disorders, especially mood disorders, among female adolescents35,36. According to Tintori et al.37, disparities in suicide attempts between sexes arise from distinct vulnerabilities that affect males and females to varying degrees. These authors highlighted the significant sex-based variability in suicidal ideation, particularly pertinent when addressing adolescents’ demographics, revealing a higher prevalence of mental disorders and suicidal behaviour among females compared to males, consistent with prior research. Importantly, data from the present study were collected before the COVID global pandemic. This aspect is of particular interest since results from the Youth Risk Behavior Survey across 17 countries published by the Centers for Disease Control and Prevention38 revealed a substantial increase in STB among girls before the pandemic, which also worsened due to it39–41.
Moreover, during the MILESTONE 2-year assessment period, there was a consistent increase in the low levels of STB across the four time points examined. This may be due, in part, to growing attention from clinicians towards those who have previously attempted suicide, as previous studies demonstrate that about 20% of those who attempted suicide will attempt again within one year42. In addition, consistent with previous observations43, participants in the MILESTONE project who reported high levels of STB at baseline often continued to receive care from CAMHS over the 24 months. Clinicians, parents, and carers of those particularly at risk of suicide, indeed, may persist in postponing the transition to AMHS due to high levels of emotional distress43.
Regarding factors associated with STB, in our sample neurodevelopmental (21.3%), mood (14.8%), and anxiety disorders (13.9%) accounted for about 50% of primary diagnoses among participants. As Nock et al.44 reported, the majority of young individuals who exhibit suicidal behaviours have pre-existing mental health conditions, which therefore represent one of the most important risk factors42. Even though mood disorders were not the most prevalent in our sample, they revealed the strongest association with STB at both the first and last time points (see Fig. 4). This finding is consistent with previous research highlighting that 50–75% of young individuals who die by suicide had a mood disorder, resulting in adolescents suffering from mood disorders potentially being at a higher risk of attempting suicide than their peers45. Although mood disorders in children and adolescents are often underdiagnosed, misdiagnosed, and undertreated46, they remain significant risk factors for suicide across all age groups, including childhood and adolescence47–49. Moreover, among the 230 participants, 33 had previously (before T1) attempted suicide (14.3%), while 22 did not disclose such information (9.6%). Our findings show that a history of suicide attempts had the strongest association with STB from the first through the last time point (Fig. 4). This finding is consistent with the literature showing that previous suicide attempts represent a major risk factor for completed suicide50. Other studies have shown that around 10% of adolescents who attempt suicide may try again within three months14, and 40–55% of those who attempt suicide have made previous attempts51,52. It is worth noting that the mean lifetime suicide attempt rate among other European countries participating in the MILESTONE project was 25.7%, which is significantly higher than in our Italian sample53. This observation is consistent with the relatively lower suicide rates recorded in Italy (6.7 per 100.000 inhabitants) compared to the rest of the world (9.2 per 100.000 inhabitants)1.
Finally, our investigation confirmed the significance of environmental and social factors as pivotal factors associated with STB in adolescence. In our study, relational problems exhibited a stronger association with STB at the end of the follow-up (T4), a period coinciding with the possible transition to AMHS for the majority of participants, than when all adolescents were seen in CAMHS due to their age below 18 years (T1). This transition to AMHS may have been emotionally taxing, necessitating additional support from family members, peers, and healthcare practitioners. Previous studies have shown that social and interpersonal relationships, parenting processes, family climate factors, and stressors within the family context are significant risk factors for STB among young people54,55. During adolescence, a period characterised by heightened emotional volatility driven by the limbic system’s bottom-up regulation56, individuals may face more profound emotional challenges due to the instability of interpersonal relationships, particularly intimate bonds; and those struggling with mental disorders frequently face stigmatisation and may become targets of peer victimisation and bullying, circumstances that can exacerbate social isolation among adolescents57. Moreover, the transition from CAMHS to AMHS may include additional challenges: these include adjusting to new environments, dealing with social isolation, managing disruptions in treatment continuity, navigating complex healthcare systems, and taking on increased responsibility for their well-being. Other challenges, such as moving away from home for the first time and financial concerns, may also arise58–60.
The current study, compared to previous ones conducted on adolescents with psychiatric health conditions61,62 includes (i) four assessments over two years to monitor suicidality fluctuation, (ii) a larger sample size (who meets the criteria for psychiatric diagnoses according to the ICD-10, DSM-IV, and DSM-5)63, (iii) and the use of standardised assessment tools, such as the HoNOSCA64. Previous studies conducted on the Italian population employed a broader age spectrum65 and did not specifically include adolescents with mental disorders during their transition from CAMHS to AMHS (and to other health providers). Additionally, two of MILESTONE’s Young Project Advisors, both with lived experience of using mental health services, are co-authors of this study. Their experiences and perspective played a crucial role in the comprehension of the relevant factors implicated in the transition from CAMHS to AMHS, and in highlighting the clinical implications of this study.
Nevertheless, our study presents some limitations and future works may contribute to bridging these gaps. Since none of the participants—fortunately—died during our study, within the gender differences in suicide, we were only able to support the assumption that females experienced more non-fatal STB than males. Moreover, for an in-depth investigation of each specific suicide outcome separately (e.g., suicidal ideation, suicidal planning, and/or suicide attempts), longitudinal studies should aim to include a larger number of participants with elevated levels of STB in order to capture a broader spectrum of these phenomena. However, within the MILESTONE project, young people were deemed ineligible if they were considered to be too unwell or too vulnerable by their clinician to participate. Therefore, young people with an imminent risk of suicide might have been excluded from the sample. This is a common limitation in suicidology since both clinicians and researchers must carefully select participants with the well-being and safety of patients as a top priority. Moreover, this study considered the participants’ biological sex dichotomously (male vs. female) according to the tools used, such as DAWBA. Including gender identity as a variable to explore suicide risk in the young LGBTQIA + community, especially among those facing a transitional care process, might be of great relevance and interest, given the high rates of rejection, bullying, and abuse these individuals are subjected to66,67. In general, adolescents are often heavily exposed to issues related to suicidal tendencies and self-harming behaviours on social networking platforms. While these platforms can serve as a means of communication and seeking social support, they can also expose young individuals to negative messages promoting self-harm, which can exacerbate their involvement in such harmful behaviours68. Furthermore, extended use of social networking sites has been linked to elevated levels of psychological distress, unfulfilled mental health requirements, decline in self-assessed mental health, and an increased inclination towards suicidal thoughts. The dual nature of social media, which includes positive elements such as peer support and recovery narratives, as well as negative effects such as dependency, triggers, imitation of harmful behaviours, cyber victimisation, and psychological entrapment, highlights its role as both a contributing factor and a protective mechanism69,70. Longitudinal investigations are necessary to clarify the nature of the association between suicidal behaviours and social media use, given the ambiguity surrounding the precise direction of causality71. Moreover, there is a pronounced tendency among girls towards dependency and imitation, which can lead to the emergence of a “suicidal identity”—an online persona centered around suicidal thoughts and behaviours. This highlights the need for targeted intervention strategies aimed at using social media as a tool for suicide prevention.
In conclusion, this longitudinal study evaluated trends in general health and social functioning, as well as sex differences and factors associated with different levels of severity in STB among young people suffering from mental disorders and undergoing a transition from CAMHS to AMHS in Italy. We found an overall improvement in general health and social functioning over the two-year follow-up. Moreover, sex differences in STB among young people struggling with a mental disorder suggest that females may require the implementation of different preventive strategies than males. Finally, the identification of factors associated with STB has clinical implications as it reinforces the perspective in suicidology that views suicide as the unfortunate combination of various contributing factors, and also suggests that more attention should be paid to environmental and social factors (e.g., relational problems and lack of support). Thus, it would be ideal to approach these phenomena comprehensively and through an interdisciplinary lens to gain a deeper understanding of the underlying causes of suicidal ideation among adolescents. In light of recent NICE recommendations on suicidal behaviors72, it is crucial to recognise that risk assessment tools are ineffective in reliably predicting self-harm or suicide. This study emphasises the importance of focusing on associated factors contributing to STB rather than predictive models. The variability of individual risk calls for a holistic assessment that considers each person’s unique needs and vulnerabilities. Our findings advocate for clinicians to use their clinical judgment, ensuring treatment strategies are developed within a comprehensive framework that addresses both strengths and challenges.
Methods
Participants
The MILESTONE project enrolled 763 young individuals from 52 CAMHS across eight European Countries25. Previous studies43,63 have described in detail the study design and recruitment procedures. In the present study, only data from the Italian sample were analysed, which was the country with the highest number of participants (n = 230). Participants were users of CAMHS and: (i) were up to one year younger than the upper CAMHS age limit (between 16 and 19 years old), or three months older if they were still under CAMHS care at the time of the study (mean = 17.68; SD = 0.29); (ii) had a psychiatric diagnosis or regularly visited CAMHS services; (iii) had an IQ of more than 70 or no intellectual impairment—previously assessed with standardised tools or diagnosed by a clinician—and (iv) were able to complete all the assessments. Of note, in Italy, CAMHS are commonly referred to as “Neuropsychiatry Units” or “Services for Children and Adolescents” (NPIA). However, in this manuscript, we used CAMHS in line with the MILESTONE project rationale, which involves selecting participants from different countries. In Italy, there is no standard policy for determining the age at which patients should transition from CAMHS (or NPIA services) to AMHS. The transition typically occurs around the age of 18, but it depends on individual needs and local healthcare resources. To ensure continuity of care and support at this important time, patients and their families were gradually involved in the planning and execution of this transition. However, specific and regional transition policies may differ depending on the location.
Study design and procedures
After informed consent was obtained, young people and their parents were invited for a baseline assessment at the CAMHS where they received care, for approximately six months before reaching the upper age limit of the service. Interviews to collect information on sociodemographic details and the need for care were conducted. Based on the participants’ preferences, the assessments took place either at their original CAMHS (at baseline for everyone and at other time points for those who had not yet experienced the transition), at AMHS (after the transition from CAMHS), at home, or via telephone. Online questionnaires were completed using HealthTracker™ as a secure web-based platform (https://www.healthtracker.co.uk)25. Clinical information on young people was provided by clinicians or by accessing medical files. Participants completed the baseline assessment between October 2015 and January 2017 and were evaluated four times during the 24-month follow-up period: at 3 months before transitioning from CAMHS to AMHS (T1), 9 months after T1 (T2), 15 months after T1 (T3), and 24 months after T1 (T4). At T1, all participants were receiving treatment in CAMHS, while at T4 some of them had already transitioned to AMHS.
The study protocol (study registration numbers: ISRCTN83240263 and NCT03013595) was approved by the UK National Research Ethics Service Committee West Midlands, South Birmingham (15/WM/0052) and the ethical committee of the Italian coordinating site IRCCS Fatebenefratelli on 4.12.2014 (permission 70/2014). All procedures contributing to this study comply with the Helsinki Declaration of 1975, as revised in 2008.
Measures
General health and social functioning
General Health and social functioning were assessed using the Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA)73,74, a 15-item scale rated on a five-point severity scale, from 0 (no problem) to 4 (severe problem). It is composed of two sections: section A consists of 13 items related to different emotional and behavioural domains, while Section B contains two questions that investigate the young person’s or parents’ awareness of the young person’s difficulties and their knowledge of the available services. Items included in the HoNOSCA are reported in Table S2.
Suicidal thoughts and behaviours (STB)
In the HoNOSCA Non-Accidental Self-Injury subscale participants were asked the question "Have you done anything to injure or harm yourself on purpose?". Scores to this item, ranging from 0 to 4, allowed to differentiate different levels of severity reflecting the STB continuum: 0 = "No problem of this kind during the period rated"; 1 = "Occasional thoughts about death, or of self-harm not leading to injury. No self-harm or suicidal thoughts"; 2 = “Non-hazardous self-harm, such as wrist scratching, whether or not associated with suicidal thoughts”; 3 = “Moderately severe suicidal intent (including preparatory acts e.g. collecting tablets) or moderate non-hazardous self-harm” (e.g. small overdose); 4 = “Serious suicidal attempt (e.g. serious overdose), or serious deliberate self-injury”. This item does not include scratching, picking as a direct result of a physical illness, accidental self-injury due to severe learning or physical disability, and illness or injury as a direct consequence of drug/alcohol use, rated on Physical illness or disability problems subscale.
Factors associated with STB
To determine the importance of the association of different factors with STB at T1 and T4, we utilised five different MILESTONE information: sociodemographic and personal information, clinical diagnosis, the Achenbach System of Empirically Based Assessment (ASEBA), the Development and Well-Being Assessment (DAWBA), and the Transition Readiness and Appropriateness Measure (TRAM), as outlined by Singh et al.25. These standardised tools incorporate a range of items pertinent to factors associated with suicide, including previous suicide attempts, mood disorder diagnoses, aggressive tendencies, trauma and abuse, lack of support from family and friends, and relational problems. Items of each of these factors were grouped into thematic domains to exploit them in the factor analysis. A detailed list of the items included in our analysis is presented in the Supporting Information section (see Supplementary Table 1) and in Singh et al.25.
Statistical analysis
To assess the general health and social functioning over four time-points, we considered the HoNOSCA total ratings employing a repeated measures model with a random effect for each subject to account for within-subject correlations. This approach allowed us to sketch the total rating trajectory over time, considering individual variability. To analyse sex differences in STB trends a generalized linear mixed-effects model was fitted with a binomial family and a logit link function. The HoNOSCA self-injury subscale variable was transformed into a binary variable: a score of 3–4 indicates moderate-to-elevated levels of STB, while a score of 0–1–2 indicates low-to-mild levels. The score of 2 was initially ambiguous since self-harm might be done to avoid suicide impulses75, but it may also represent a predisposition for suicide attempts76. Therefore, we tested two approaches: including it in the low-level category (Table 3), and excluding it entirely (see Table S3). Since the results of these two scenarios were almost identical, we proceeded with the first approach. To account for within-subject correlations we included a random effect for each subject; in addition, sex and HoNOSCA total ratings were considered as covariates. Finally, through an Exploratory Factor Analysis (EFA) using a random forest model77, we identified the importance of the factors associated with STB at the first and last time points. The metric used to evaluate features’ importance was Mean Decrease Gini (MDG), providing an overall indication of how much each feature contributes to the accuracy of the model by increasing the purity of the nodes. The analyses were performed using the R software system version 4.3.2, considering a significance threshold of 0.05.
Supplementary Information
Acknowledgements
The MILESTONE project was funded by the European Union’s Seventh Framework Programme for research, technological development, and demonstration (Grant Agreement: 602442). This work was supported by the Italian Ministry of Health (Ricerca Corrente). We extend our thanks and appreciation to all the study participants, their families and carers, and clinicians for their contribution. We are also grateful to the wider MILESTONE project consortium for their valuable collaboration during the study.
The Italian MILESTONE consortium members include Giovanni Allibrio, M.D. (ASST of Bergamo Ovest, Treviglio), Angelo Bertani, M.D. (ASST Santi Paolo e Carlo, Milan), Sabrina Ferrari, Clin Psych (AUSL of Parma, Parma, Italy), Patrizia Conti, M.D. (ASST of Como, Como), Francesco Margari, M.D. (University of Bari, Bari), Ottaviano Martinelli, M.D. (ASST of Lecco, Lecco), Renata Nacinovich, M.D. (Fondazione IRCCS San Gerardo dei Tintori, Monza), Paolo Scocco, M.D. (formerly ASL of Padua, Padua), Francesco Rinaldi, M.D. (ASST Valcamonica, Esine), Paolo Stagi, M.D. (Azienda USL Toscana Centro, Lucca), Stefano Vicari, M.D. (Child Neuropsychiatric Unit, Department of Neuroscience, IRCCS Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy; Department of Life Sciences and Public Health, Catholic University, Rome). Thanks are also due to the following researchers of the 11 participating centres: Cecilia Ferrari, Alessandro Ferrari, Maria Giulia Cataldo, Elisa Gheza, Lidia Manenti, Flavia Micol Levi, Giorgia Morini, Adriana Pastore, Laura Rivolta, Giulia Signorini, Pamela Stagni.
Author contributions
G.T., S.L., and G.d.G. conceived and designed the study. All people listed below in the acknowledgments collected data at 11 Italian CAMHS. G.T. and S.L. consulted literature and wrote the paper. D. M., D. M., and R.M. performed the statistical data analysis. G.T. and S.L. did the psychosocial interpretation of the results. G.d.G. is the last author, i.e., the Italian group leader in MILESTONE. S.C., G.D., S.G., S.S., R.M., C.S., and G.d.G. contributed to the paper’s review. All authors read and approved the manuscript.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
The original online version of this Article was revised: In the original version of this Article Gabriele Torino and Silvia Leone were omitted as equally contributing authors. Additionally, the first paragraph of the Acknowledgements section was incomplete where a grant fund was omitted. Full information regarding the corrections made can be found in the correction for this Article.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gabriele Torino and Silvia Leone contributed equally to this work.
A list of authors and their affiliations appear at the end of the paper.
Change history
11/27/2024
A Correction to this paper has been published: 10.1038/s41598-024-79680-w
Contributor Information
Giovanni de Girolamo, Email: gdegirolamo@fatebenefratelli.eu.
the Italian MILESTONE Consortium:
Giovanni Allibrio, Angelo Bertani, Sabrina Ferrari, Patrizia Conti, Francesco Margari, Ottaviano Martinelli, Renata Nacinovich, Paolo Scocco, Francesco Rinaldi, Paolo Stagi, and Stefano Vicari
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-76605-5.
References
- 1.WHO. Suicide Worldwide in 2019 Global Health Estimates.
- 2.Shain, B. & COMMITTEE ON ADOLESCENCE. Suicide and suicide attempts in adolescents. Pediatrics 138 (2016). [DOI] [PubMed]
- 3.Hawton, K., Saunders, K. E. A. & O’Connor, R. C. Self-harm and suicide in adolescents. Lancet 379, 2373–2382 (2012). [DOI] [PubMed] [Google Scholar]
- 4.Pitman, A., Osborn, D., King, M. & Erlangsen, A. Effects of suicide bereavement on mental health and suicide risk. Lancet Psychiatry 1, 86–94 (2014). [DOI] [PubMed] [Google Scholar]
- 5.Sveen, C.-A. & Walby, F. A. Suicide survivors’ mental health and grief reactions: A systematic review of controlled studies. Suicide Life Threat Behav. 38, 13–29 (2008). [DOI] [PubMed] [Google Scholar]
- 6.Arsenault-Lapierre, G., Kim, C. & Turecki, G. Psychiatric diagnoses in 3275 suicides: A meta-analysis. BMC Psychiatry 4, 37 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertolote, J. M. & Fleischmann, A. Suicide and psychiatric diagnosis: A worldwide perspective. World Psychiatry 1, 181–185 (2002). [PMC free article] [PubMed] [Google Scholar]
- 8.Pompili, M. Critical appraisal of major depression with suicidal ideation. Ann. Gen. Psychiatry 18, 7 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McMahon, E. M., Cully, G., Corcoran, P., Arensman, E. & Griffin, E. Advancing early detection of suicide? A national study examining socio-demographic factors, antecedent stressors and long-term history of self-harm. J. Affect. Disord. 350, 372–378 (2024). [DOI] [PubMed] [Google Scholar]
- 10.De Leo, D. et al. International study of definitions of English-language terms for suicidal behaviours: A survey exploring preferred terminology. BMJ Open 11, 043409 (2021). [DOI] [PMC free article] [PubMed]
- 11.Brent, D. A. & Mortiz, G. Developmental Pathways to Adolescent Suicide (University of Rochester Press Rochester, 1996). [Google Scholar]
- 12.Qin, P. & Nordentoft, M. Suicide risk in relation to psychiatric hospitalization: Evidence based on longitudinal registers. Arch. Gen. Psychiatry 62, 427–432 (2005). [DOI] [PubMed] [Google Scholar]
- 13.Runeson, B. & Beskow, J. Reactions of survivors of suicide victims to interviews. Acta Psychiatr. Scand. 83, 169–173 (1991). [DOI] [PubMed] [Google Scholar]
- 14.Shaffer, D. Psychiatric diagnosis in child and adolescent suicide. Arch. Gen. Psychiatry 53, 339 (1996). [DOI] [PubMed] [Google Scholar]
- 15.Till, B., Tran, U. S. & Niederkrotenthaler, T. Relationship satisfaction and risk factors for suicide. Crisis 38, 7–16 (2017). [DOI] [PubMed] [Google Scholar]
- 16.Bi, B. et al. Personality traits and suicide attempts with and without psychiatric disorders: Analysis of impulsivity and neuroticism. BMC Psychiatry 17, 294 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bailen, N. H., Green, L. M. & Thompson, R. J. Understanding emotion in adolescents: A review of emotional frequency, intensity, instability, and clarity. Emotion Rev. 11, 63–73 (2019). [Google Scholar]
- 18.Ryan, E. P. & Oquendo, M. A. Suicide risk assessment and prevention: Challenges and opportunities. Focus 18, 88–99 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beautrais, A. Suicide by jumping. Crisis 28, 58–63 (2007). [DOI] [PubMed] [Google Scholar]
- 20.Canetto, S. S. & Sakinofsky, I. The gender paradox in suicide. Suicide Life Threat Behav. 28, 1–23 (1998). [PubMed] [Google Scholar]
- 21.Schrijvers, D. L., Bollen, J. & Sabbe, B. G. C. The gender paradox in suicidal behavior and its impact on the suicidal process. J. Affect. Disord. 138, 19–26 (2012). [DOI] [PubMed] [Google Scholar]
- 22.Fox, K. R., Millner, A. J., Mukerji, C. E. & Nock, M. K. Examining the role of sex in self-injurious thoughts and behaviors. Clin. Psychol. Rev. 66, 3–11 (2018). [DOI] [PubMed] [Google Scholar]
- 23.Miranda-Mendizabal, A. et al. Gender differences in suicidal behavior in adolescents and young adults: Systematic review and meta-analysis of longitudinal studies. Int. J. Public Health 64, 265–283 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaess, M. et al. Explaining gender differences in non-fatal suicidal behaviour among adolescents: A population-based study. BMC Public Health 11, 597 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh, S. P. et al. Protocol for a cohort study of adolescent mental health service users with a nested cluster randomised controlled trial to assess the clinical and cost-effectiveness of managed transition in improving transitions from child to adult mental health services (the MILESTONE study). BMJ Open 7, e016055 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grande, E. et al. Suicide among adolescents in Italy: A nationwide cohort study of the role of family characteristics. Eur. Child Adolesc. Psychiatry 30, 1037–1045 (2021). [DOI] [PubMed] [Google Scholar]
- 27.EUROSTAT. Causes of Death - Standardised Death Rate by NUTS 2 Region of Residence (2024).
- 28.Rihmer, Z., Rihmer, A. & Beltezcki, Z. Psycho-social correlates of suicidal behaviour. Neuropsychopharmacol. Hung. 24, 162–169 (2022). [PubMed] [Google Scholar]
- 29.Castaldo, L., Serra, G., Piga, S., Reale, A. & Vicari, S. Suicidal behaviour and non-suicidal self-injury in children and adolescents seen at an Italian paediatric emergency department. Ann. Ist Super Sanita 56, 303–314 (2020). [DOI] [PubMed] [Google Scholar]
- 30.Akinyemi, O. et al. Factors associated with suicide/self-inflicted injuries among women aged 18–65 years in the United States: A 13-year retrospective analysis of the National Inpatient Sample database. PLoS ONE 18, e0287141 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scocco, P., de Girolamo, G., Vilagut, G. & Alonso, J. Prevalence of suicide ideation, plans, and attempts and related risk factors in Italy: Results from the European Study on the Epidemiology of Mental Disorders-World Mental Health study. Compr. Psychiatry 49, 13–21 (2008). [DOI] [PubMed] [Google Scholar]
- 32.Wunderlich, U., Bronisch, T., Wittchen, H. U. & Carter, R. Gender differences in adolescents and young adults with suicidal behaviour. Acta Psychiatr. Scand. 104, 332–339 (2001). [DOI] [PubMed] [Google Scholar]
- 33.Eaton, D. K. et al. Youth risk behavior surveillance - United States, 2011. MMWR Surveill. Summ. 61, 1–162 (2012). [PubMed] [Google Scholar]
- 34.Lim, M., Lee, S. U. & Park, J.-I. Difference in suicide methods used between suicide attempters and suicide completers. Int. J. Ment. Health Syst. 8, 54 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuehner, C. Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatr. Scand. 108, 163–174 (2003). [DOI] [PubMed] [Google Scholar]
- 36.Mitchell, R. H. et al. Sex differences in brain structure among adolescents with bipolar disorder. Bipolar Disord. 10.1111/bdi.12663 (2018). [DOI] [PubMed] [Google Scholar]
- 37.Tintori, A., Pompili, M., Ciancimino, G., Corsetti, G. & Cerbara, L. The developmental process of suicidal ideation among adolescents: Social and psychological impact from a nation-wide survey. Sci. Rep. 13, 20984 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Youth Risk Behavior Survey Data Summary & Trends Report: 2013–2023 (2024).
- 39.García-Fernández, L. et al. Dramatic increase of suicidality in children and adolescents after COVID-19 pandemic start: A two-year longitudinal study. J. Psychiatr. Res. 163, 63–67 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gracia, R. et al. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls?. J. Affect. Disord. 292, 139–141 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Madigan, S. et al. Comparison of paediatric emergency department visits for attempted suicide, self-harm, and suicidal ideation before and during the COVID-19 pandemic: A systematic review and meta-analysis. Lancet Psychiatry 10, 342–351 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gili, M. et al. Mental disorders as risk factors for suicidal behavior in young people: A meta-analysis and systematic review of longitudinal studies. J. Affect. Disord. 245, 152–162 (2019). [DOI] [PubMed] [Google Scholar]
- 43.Gerritsen, S. E. et al. Leaving child and adolescent mental health services in the MILESTONE cohort: A longitudinal cohort study on young people’s mental health indicators, care pathways, and outcomes in Europe. Lancet Psychiatry 9, 944–956 (2022). [DOI] [PubMed] [Google Scholar]
- 44.Nock, M. K. et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 70, 300–310 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shaffer, D. et al. Psychiatric diagnosis in child and adolescent suicide. Arch. Gen. Psychiatry 53, 339–348 (1996). [DOI] [PubMed] [Google Scholar]
- 46.Sanchez, L. E. & Le, L. T. Suicide in mood disorders. Depress. Anxiety 14, 177–182 (2001). [DOI] [PubMed] [Google Scholar]
- 47.Dilillo, D. et al. Suicide in pediatrics: Epidemiology, risk factors, warning signs and the role of the pediatrician in detecting them. Ital. J. Pediatr. 41, 49 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pelkonen, M. & Marttunen, M. Child and adolescent suicide. Pediatr. Drugs 5, 243–265 (2003). [DOI] [PubMed] [Google Scholar]
- 49.Zhu, S., Li, X. & Wong, P. W. C. Risk and protective factors in suicidal behaviour among young people in Hong Kong: A comparison study between children and adolescents✰. Psychiatry Res. 321, 115059 (2023). [DOI] [PubMed] [Google Scholar]
- 50.Hawton, K. & van Heeringen, K. Suicide. The Lancet 373, 1372–1381 (2009). [DOI] [PubMed] [Google Scholar]
- 51.Rudd, M. D. Suicidality in clinical practice: Anxieties and answers. J. Clin. Psychol. 62, 157–159 (2006). [DOI] [PubMed] [Google Scholar]
- 52.Scoliers, G., Portzky, G., van Heeringen, K. & Audenaert, K. Sociodemographic and psychopathological risk factors for repetition of attempted suicide: A 5-year follow-up study. Arch. Suicide Res. 13, 201–213 (2009). [DOI] [PubMed] [Google Scholar]
- 53.Gerritsen, S. E. et al. Cohort profile: Demographic and clinical characteristics of the MILESTONE longitudinal cohort of young people approaching the upper age limit of their child mental health care service in Europe. BMJ Open 11, e053373 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.King C. A. Suicidal behavior in adolescence. Review of Suicidology 61–97 (1997).
- 55.Diamond, G., Kodish, T., Ewing, E. S. K., Hunt, Q. A. & Russon, J. M. Family processes: Risk, protective and treatment factors for youth at risk for suicide. Aggress Violent Behav. 64 (2022). [DOI] [PMC free article] [PubMed]
- 56.Casey, B. J., Jones, R. M. & Hare, T. A. The adolescent brain. Ann. N. Y. Acad. Sci. 1124, 111–126 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kaushik, A., Kostaki, E. & Kyriakopoulos, M. The stigma of mental illness in children and adolescents: A systematic review. Psychiatry Res. 243, 469–494 (2016). [DOI] [PubMed] [Google Scholar]
- 58.Livanou, M., D’Souza, S., Lane, R., La Plante, B. & Singh, S. P. Challenges and facilitators during transitions from adolescent medium secure units to adult services in England: Interviews with mental healthcare professionals. Adm. Policy Ment. Health 48, 1089–1104 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Medforth, N. & Boyle, C. Challenges, complexity, and developments in transition services for young people with disabilities, mental health, and long-term conditions: An integrative review. Compr. Child Adolesc. Nurs. 46, 180–200 (2023). [DOI] [PubMed] [Google Scholar]
- 60.Hendrickx, G. et al. Challenges during the transition from child and adolescent mental health services to adult mental health services. BJPsych Bull. 44, 163–168 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Poletti, M. et al. Anhedonia and suicidal ideation in young people with early psychosis: Further findings from the 2-year follow-up of the ReARMS program. Psychiatry Res. 323, 115177 (2023). [DOI] [PubMed] [Google Scholar]
- 62.Williams, A. J. et al. A systematic review and meta-analysis of victimisation and mental health prevalence among LGBTQ+ young people with experiences of self-harm and suicide. PLoS ONE 16, e0245268 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tuomainen, H. et al. Managing the link and strengthening transition from child to adult mental health Care in Europe (MILESTONE): Background, rationale and methodology. BMC Psychiatry 18, 167 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gowers, S. G. et al. Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). Glossary for HoNOSCA score sheet. Br. J. Psychiatry 174, 428–431 (1999). [DOI] [PubMed]
- 65.Girardi, P. et al. Suicide mortality among psychiatric patients in Northeast Italy: A 10-year cohort study. Epidemiol. Psychiatr. Sci. 31, e17 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ryan, C., Huebner, D., Diaz, R. M. & Sanchez, J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics 123, 346–352 (2009). [DOI] [PubMed] [Google Scholar]
- 67.Mustanski, B. S., Garofalo, R. & Emerson, E. M. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual, and transgender youths. Am. J. Public Health 100, 2426–2432 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Memon, A. M., Sharma, S. G., Mohite, S. S. & Jain, S. The role of online social networking on deliberate self-harm and suicidality in adolescents: A systematized review of literature. Indian J. Psychiatry 60, 384–392 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Balt, E. et al. Social media use of adolescents who died by suicide: Lessons from a psychological autopsy study. Child Adolesc. Psychiatry Ment. Health 17, 48 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lombardo, C. et al. Why social media could be dangerous? Suicide risk and mental health challenges in adolescents during COVID-19 pandemic. A narrative review of the literature. J. Clin. Dev. Psychol. 10.13129/2612-4033/0110-3631 (2022). [Google Scholar]
- 71.Sedgwick, R., Epstein, S., Dutta, R. & Ougrin, D. Social media, internet use and suicide attempts in adolescents. Curr. Opin. Psychiatry 32, 534–541 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.NICE. Suicidal Behaviour: Evidence and Recommendations. National Institute for Health and Care Excellence (NICE) Guidelines (2022).
- 73.Garralda, M. E., Yates, P. & Higginson, I. Child and adolescent mental health service use. Br. J. Psychiatry 177, 52–58 (2000). [DOI] [PubMed] [Google Scholar]
- 74.Gowers, S. G. et al. Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). Br. J. Psychiatry 174, 428–431 (1999). [DOI] [PubMed] [Google Scholar]
- 75.Klonsky, E. D., May, A. M. & Glenn, C. R. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. J. Abnorm. Psychol. 122, 231–237 (2013). [DOI] [PubMed] [Google Scholar]
- 76.Duarte, T. A. et al. Self-harm as a predisposition for suicide attempts: A study of adolescents’ deliberate self-harm, suicidal ideation, and suicide attempts. Psychiatry Res. 287, 112553 (2020). [DOI] [PubMed] [Google Scholar]
- 77.Breiman, L. Random forests. Mach. Learn. 45, 5–32 (2001). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.