After elective percutaneous coronary intervention (PCI), patients are frequently observed overnight in the hospital. Same‐day discharge (SDD) after elective PCI is safe, cost‐effective, and traditionally preferred by the patients.1, 2, 3 Although several studies have shown an interest in this practice,1, 2, 3 its feasibility and safety in older patients remains unknown because those patients are generally not included in these studies. 4 Older patients have more comorbidities and less favorable coronary and peripheral anatomy (tortuosity and calcifications), which may compromise SDD after PCI. On the other hand, frailty is also associated with hospitalization‐related complications. Only one study has assessed a 30‐day prognosis of a multicentric cohort of older patients undergoing SDD PCI. 5 This study from 2011 compared patients over 65 undergoing SDD PCI with an overnight stay for the PCI, but most of these patients underwent the procedure using a femoral approach. We aimed to assess the feasibility and safety of SDD post‐PCI in older patients.
From January 2013 to December 2019, we conducted a longitudinal study with retrospective enrolment of all consecutive patients undergoing elective PCI in a single center (Hopital Privé Parly 2). We compared a group of older patients (aged ≥75 years) undergoing SDD after elective PCI with a control group of younger patients (<75 years). To perform a 2:1 comparison, patients <75 years old were randomly included. SDD PCI was defined as having the same day admission and discharge from hospital procedure. Patients with planned hospitalization or acute coronary syndrome were excluded. SDD PCI were performed with a standard angioplasty protocol. Periprocedural treatment with antiplatelet therapy and anticoagulants was left to the discretion of the physician. After PCI, patients were monitored for 1 h in the recovery room. If the clinical and vitals constants were satisfying, patients were able to move back to their rooms. Electrocardiogram and troponin assays were performed four hours after the end of procedure. Patients were able to leave hospital after 6 h of uneventful clinical observation following the procedure. The 2021 ACC Expert Consensus Decision Pathway on Same‐Day Discharge After Percutaneous Coronary Intervention uses pre‐PCI considerations such as clinical factors (physician's input), social factors, and staff/systems factors, post‐PCI considerations such as complications during/after procedure and pre‐discharge checklist for medication, and follow‐up management. In this consensus, no troponin value was mentioned as mandatory for SDD PCI. Nevertheless, in our center, troponin was systematically obtained before discharge. 6 Troponin value was evaluated by the clinician in regard of the complexity of the procedure to allow SDD (Fig. 1a).
Figure 1.
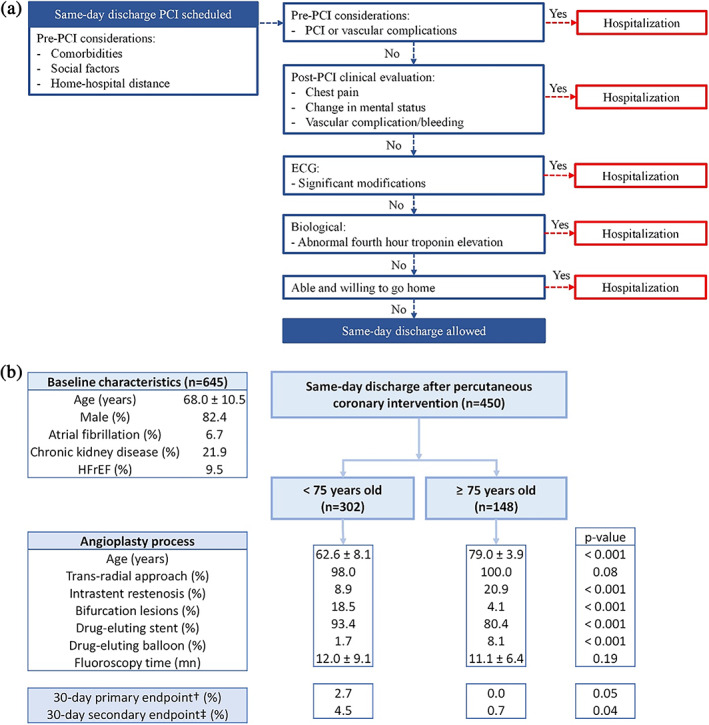
Diagram of same‐day discharge percutaneous coronary intervention (PCI) protocol in the center and comparison of same‐day discharge after elective PCI according to the age. (a) Diagram of same‐day discharge PCI protocol in the center. (b) Comparison of same‐day discharge after elective PCI according to the age. Values are n (%) or mean ± SD. HFrEF, heart failure with reduced ejection fraction. †30‐day primary endpoint: composite of all‐cause death, target lesion revascularization, stroke, myocardial infarction, and unplanned cardiovascular hospitalization. ‡30‐day secondary endpoint: composite of all‐cause death, target lesion revascularization, stroke, myocardial infarction, and unplanned hospitalization from any cause.
The follow‐up consisted of a phone call after 30 days and additional contacts in case of events (medical reports and/or phone call to the referring physicians). The primary endpoint was a composite of all‐cause death, target lesion revascularization, stroke, myocardial infarction, and unplanned cardiovascular hospitalization at 30 days. The secondary endpoint was a composite of all‐cause death, target lesion revascularization, stroke, myocardial infarction, and unplanned hospitalization from any cause at 30 days. The clinical outcome was analyzed with logistic regression.
Among the 645 patients referred for a SDD PCI, 148 (22.9%) were aged ≥75. The mean age of the older patients was 79 years old. Older patients were less likely to be men (74.3% vs. 86.4%, P = 0.002), but presented more frequently with comorbidities: hypertension (74.3% vs. 58.3%, P < 0.001), atrial fibrillation (14.2% vs. 3.0%, P < 0.001), heart failure with reduced ejection fraction (20% vs. 5.2%, P < 0.001), and known coronary artery disease (52.0% vs. 19.8%, P < 0.001). Older patients had significantly more chronic kidney disease Stage 3 or higher (glomerular filtration rate <60 mL/min/m2) (52.0% vs. 19.8%, P < 0.001) and significantly more severe chronic kidney disease stage 4 or higher (glomerular filtration rate <30 mL/min/m2) (5.4% vs. 0.7%, P = 0.002). Moreover, older patients had significantly lower weight and lower body mass index (75.2 ± 12.8 vs. 81.5 ± 14.9 kg, P = 0.03 and 26.1 ± 3.9 vs. 27.8 ± 12.4, P < 0.001 respectively). There were no differences between both groups in the lesions treated with a similar rate of left main coronary artery, left anterior descending artery, circumflex, and right coronary artery (all P‐values non‐significant) and similar number of arteries treated at the same time. Older patients had a higher rate of coronary artery bypass graft lesions (P = 0.001) and intrastent restenosis (P < 0.001) treated, but a lower rate of bifurcation lesions and chronic total occlusions (P < 0.001 and P = 0.02 respectively). The vascular approach was most frequently a radial access (444, 98.7%). Concerning PCI, older patients were less likely treated with drug‐eluting stents (93.4% vs. 80.4%, P < 0.001), but more likely treated with drug‐eluting balloons (8.1% vs. 1.7%, P < 0.001). In the lesions treated, there were no significant differences between fluoroscopy time, volume contrast, stent length, and ultra‐sensitive troponin assay at 4 h post‐PCI (12.0 ± 9.1 in younger group vs. 11.1 ± 6.4 min in older group, P = 0.19, 159.4 ± 55.9 in younger group vs. 153.8 ± 57.2 mL, P = 0.7, 24.2 ± 14.5 in younger group vs. 21.3 ± 14.5 mm in older group, P = 0.06, 24.7 ± 60.4 in younger group vs. 33.4 ± 52.3 ng/L in older group, P = 0.14 respectively) but older patients had significantly smaller stents than younger patients (2.87 ± 0.46 vs. 2.95 ± 0.74 mm, P < 0.001). At 30 days follow‐up, in the whole population, the primary endpoint occurred six times (1.7% including 0.0% all cause death, 0.3% of stroke, 0.3% target lesion revascularization, 0.8% unplanned cardiovascular hospitalization), but there was no significant difference between the two groups at the primary endpoint (2.7% in the younger group vs. 0.0% in the older group, P = 0.05). However, the 30‐day secondary endpoint occurred significantly more in younger patients (4.5% in the younger group vs. 0.7% in the older group, P = 0.04) (Fig. 1b).
This study has several limitations, as anemia, nutritional status, and frailty score were not collected for these patients.
In our cohort of consecutive patients referred for a SDD PCI, selected older patients had similar outcomes as compared with younger patients. SDD PCI seems to be safe and feasible for most patients aged ≥75 years. Although limited by the retrospective nature of the analysis and selection bias in which patients were discharged, it does reinforce SDD PCI as a good option for older patients following PCI.
Funding information
FP reports research, consulting and speaking fees from Astra‐Zeneca, Bayer, BBraun, Biotronik, BMS‐Pfizer Alliance, Boston Scientific, and Sanofi, outside the submitted work.
Author contributions
All of the authors contributed to the manuscript drafts, reviewed and approved the final manuscript.
Léquipar A, Chicheportiche T, Pham V, et al. Same‐day discharge after elective percutaneous coronary intervention in older patients. Geriatr. Gerontol. Int. 2023;23:639–641. 10.1111/ggi.14628
Data availability statement
The data that support the findings of this study are available from the corresponding author, AL, upon reasonable request.
References
- 1. Kiemeneij F, Laarman GJ, Slagboom T, van der Wieken R. Outpatient coronary stent implantation. J Am Coll Cardiol 1997; 29: 323–327. [DOI] [PubMed] [Google Scholar]
- 2. Abdelaal E, Rao SV, Gilchrist IC et al. Same‐day discharge compared with overnight hospitalization after uncomplicated percutaneous coronary intervention: a systematic review and meta‐analysis. JACC Cardiovasc Interv 2013; 6: 99–112. [DOI] [PubMed] [Google Scholar]
- 3. Amin AP, Patterson M, House JA et al. Costs associated with access site and same‐day discharge among Medicare beneficiaries undergoing percutaneous coronary intervention: an evaluation of the current percutaneous coronary intervention care pathways in the United States. JACC Cardiovasc Interv 2017; 10: 342–351. [DOI] [PubMed] [Google Scholar]
- 4. Heyde GS, Koch KT, de Winter RJ et al. Randomized trial comparing same‐day discharge with overnight hospital stay after percutaneous coronary intervention. Circulation 2007; 115: 2299–2306. [DOI] [PubMed] [Google Scholar]
- 5. Rao SV, Kaltenbach LA, Weintraub WS et al. Prevalence and outcomes of same‐day discharge after elective percutaneous coronary intervention among older patients. JAMA 2011; 306: 1461–1467. [DOI] [PubMed] [Google Scholar]
- 6. Rao SV, Vidovich MI, Gilchrist IC et al. 2021 ACC expert consensus decision pathway on same‐day discharge after percutaneous coronary intervention. J Am Coll Cardiol 2021; 77: 811–825. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, AL, upon reasonable request.


