Abstract
Background
Identifying depressive subtypes is an important tool in reducing the heterogeneity of major depressive disorder. However, few studies have examined the stability of putative subtypes of depression over time.
Method
The sample included 488 persons from the Netherlands Study of Depression and Anxiety (NESDA) who had major depressive disorder at baseline and at the 2-year follow-up assessment. A latent transition analysis (LTA) was applied to examine the stability of depressive subtypes across time-points. Differences in demographic, clinical, psychosocial and health correlates between subtypes were evaluated in a subsample of persons with stable subtypes.
Results
Three subtypes were identified at each time-point : a moderate subtype (prevalence T0 39%, T1 42%), a severe typical subtype (T0 30%, T1 25%), and a severe atypical subtype (T0 31%, T1 34%). The LTA showed 76% stability across the 2-year follow-up, with the greatest stability in the severe atypical class (79 %). Analyses of correlates in the stable subtypes showed a predominance of women and more overweight and obesity in the severe atypical subtype, and a greater number of negative life events and higher neuroticism and functioning scores in the severe typical subtype.
Conclusions
Subtypes of major depressive disorder were found to be stable across a 2-year follow-up and to have distinct determinants, supporting the notion that the identified subtypes are clinically meaningful.
Keywords: Latent transition analysis, major depressive disorder, stability, subtypes
Introduction
Over the past several decades, there has been substantial research devoted to the identification of depressive subtypes based on distinct symptom profiles, treatment response and clinical correlates. For example, the atypical depression subtype was identified after this subgroup was found to have preferential response to monoamine oxidase (West & Dally, 1959). Depressive subtypes play an important role because differences in symptom profiles are likely to be the result of unique psychobiological underpinnings. Two of the subtypes that are currently included in DSM-IV include melancholic and atypical depression, and are coded as depression specifiers. Different clinical and biologic correlates of these subtypes, including different directions of dysregulation of the stress response system, have been identified (Gold & Chrousos, 2002). Such differences may provide clues to differential etiological pathways and inform the development of therapeutic interventions targeting specific subtypes.
Few studies have investigated the stability of depressive subtypes, an essential requirement for the validity of the delineation of subtypes. Studies that have examined the longitudinal stability of depressive subtypes have shown low to moderate stability of subtypes (Young et al. 1987; Coryell et al. 1994; Angst et al. 2007), with greater stability between adjacent episodes (Coryell et al. 1994). Evidence regarding the stability of individual symptoms has been inconsistent (Paykel et al. 1976; Young et al. 1990; Lewinsohn et al. 2003; Minor et al. 2005), but some research has demonstrated that neurovegetative symptoms of depression are relatively stable (Stunkard et al. 1990; Nierenberg et al. 1996). A small study evaluating the severity score of atypical, melancholic and psychotic subscales found low consistency between two episodes (Oquendo et al. 2004). Instability of subtypes, however, may reflect the role of extrinsic factors (environmental factors) on depression, rather than negating the validity of these subtypes.
Unlike subtype definitions based purely on descriptive clinical data, data-driven analytic techniques, such as latent class analysis (LCA), that group persons with similar symptom profiles have provided empirical evidence for the existence of subtypes such as atypical depression (Sullivan et al. 1998; Lamers et al. 2010). An extension of the cross-sectional LCA model is the latent transition analysis (LTA) model, which can be used to estimate transition patterns among subtypes in longitudinal data. To our knowledge, no previous study has applied such transition models to examine the stability and transitions of depressive subtypes over time.
We previously identified three subtypes of depression using data from the baseline measurement of the large-scale Netherlands Study of Depression and Anxiety (NESDA): a moderate subtype, a severe melancholic/typical subtype, and a severe atypical subtype, each with distinct correlates (Lamers et al. 2010). The aim of the current study was to evaluate the 2-year longitudinal stability and transition patterns of depressive subtypes in a cohort of adults with major depressive disorder from NESDA. Because stable subtypes are possibly more reliable (‘purer’ cases) than subtypes based on cross-sectional data, and analyses of correlates of stable subtypes will therefore give a more accurate picture of the true correlates of a subtype, a second aim of this study was to examine correlates of stable subtypes.
Method
Sample
Data from the baseline measurement and the 2-year follow-up measurement from NESDA were used. NESDA is a longitudinal naturalistic cohort study, consisting of 2981 persons (aged 18–65 years), including those with lifetime and/or current anxiety and/or depressive disorders (n=2329; 78%) and healthy controls (persons without depressive or anxiety disorders, n=652; 22%) (Penninx et al. 2008). Participants were recruited from the community (n=564; 19%), primary care (n=1610; 54%) and specialized mental health care (n=807; 27%) from September 2004 to February 2007 at three study sites (Amsterdam, Groningen, Leiden). Exclusion criteria used were: (1) a primary clinical diagnosis of psychotic disorder, obsessive compulsive disorder, bipolar disorder or severe addiction disorder, and (2) not being fluent in Dutch. A detailed description of the NESDA study design can be found elsewhere (Penninx et al. 2008). At baseline and at the 2-year follow-up, participants were invited to a 4-h interview at one of the three study sites during which information was collected on psychopathology, demographic characteristics, physical and psychosocial functioning. The interview also included a medical assessment, computer tasks and two self-administered questionnaires. The response rate at the 2-year follow-up interview was 87.1% (n=2596), and attrition was associated with younger age, lower educational level, non-North European descent, being recruited in Amsterdam, no previous participation in research and having major depressive disorder (Lamers et al. 2012). For the current study, all patients with a current (12-month) diagnosis of major depressive disorder at both the baseline and 2-year follow-up interviews were selected (n=488).
Depressive symptoms
Ten depressive symptoms were used as indicator variables in the LCAs to identify depression subtypes. The nine key symptoms of depression of the DSM-IV were based on the Dutch version of the Composite International Diagnostic Interview (CIDI), lifetime version 2.1 (WHO, 1997; Andrews & Peters 1998), which was used to diagnose depressive and anxiety disorders according to DSM-IV criteria and conducted by specially trained clinical research staff. Changes in appetite and weight were used as two separate variables. The items were coded as ‘not present’ or ‘present’, except for the items regarding changes in appetite, weight, sleep and psychomotor disturbance, where four categories were created; so, for example, for weight the categories were: absence of symptom, weight loss, weight gain, and both gain and loss.
Correlates of subtypes
All correlates were measured at baseline and using Dutch versions of the listed instrument. Sociodemographic variables were collected during the baseline interview. Clinical characteristics such as age of onset of the depressive disorder and co-morbid anxiety disorders were assessed in the CIDI. The duration of depressive symptoms during the 4 years prior to the baseline measurement was obtained using the Life Chart method (Lyketsos et al. 1994). First, to refresh the respondent’s memory, important life events were recalled and, second, the presence or absence of depressive symptoms was assessed for the 4 years prior to baseline. The percentage of months with depressive symptoms was calculated from this information. The presence of manic symptoms was assessed using the 15-item Mood Disorder Questionnaire (MDQ; Hirschfeld et al. 2000), a positive family history in first-degree family members was assessed with the Family Tree Inventory (Fyer & Weissman, 1999), and severity of depressive symptoms was assessed with the 30-item Inventory of Depressive Symptomatology (IDS; Rush et al. 1996; IDS/QIDS, 2012). We also assessed several psychosocial variables. Overall functioning was measured with the World Health Organization Disability Assessment Schedule II (WHODAS II ; Chwastiak & Von Korff, 2003; Buist-Bouwman et al. 2008). Neuroticism was assessed using the NEO Five-Factor Inventory (NEO-FFI; Costa & McCrae, 1995; Hoekstra et al. 1996). Childhood trauma was assessed using the structured inventory from the Netherlands Mental Health Survey and Incidence Study (NEMESIS), a Dutch longitudinal cohort study (de Graaf et al. 2002), and an index (range 0–4) was constructed incorporating the occurrence and frequency of four types of abuse before age 16 (emotional neglect, psychological abuse, physical abuse, and sexual abuse). The number of negative life events in the past year was assessed with the Brugha questionnaire (Brugha et al. 1985). Physical health indicators were also included. Respondents were asked whether they were currently smoking (yes/no). Pain was measured using a count of pain locations (range 0–7) listed in the Chronic Graded Pain scale (Von Korff, 2001). Objective and standardized assessments of height, weight, waist circumference and blood pressure were performed. Body mass index (BMI) was calculated as kilograms divided by meters squared and categorized as underweight-normal (BMI <25 kg/m2), overweight (25 kg/m2 ≤BMI <30 kg/m2) and obese (BMI ⩾30 kg/m2). No separate category for underweight was formed because only a few participants had a BMI <18.5 kg/m2.
Statistical analyses
An LTA was carried out using Mplus, version 6.1 (Muthén & Muthén, 1998–2010). The first step in the analyses was to perform separate LCAs on the baseline and 2-year follow-up measurements to evaluate the number of classes at each time-point. In an LCA it is assumed that a latent categorical variable explains the associations among a set of observed depressive symptoms. Two sets of parameters are estimated: (1) latent class probabilities or class prevalences and (2) conditional probabilities, that is estimated probabilities of observed variables given that the individual is a member of that class. Model selection was based on Bayesian information criterion (BIC) and sample size-adjusted BIC (ssaBIC; lower values are preferred) (Yang, 2006; Nylund et al. 2007), and interpretability of identified classes.
In the second step, we evaluated whether full or partial measurement invariance could be assumed (Nylund, 2007), as the identified classes in both baseline and 2-year follow-up assessments had very similar symptom profiles with only a few differences in probabilities. Models holding all parameter estimates equal across measurements (full measurement invariance) or holding part of the parameter estimates equal across measurements (partial measurement invariance) were run. To assess differences in model fit between a model without constraints and models with full/partial measurement invariance, we used –2 log likelihood tests. These showed that partial measurement invariance could be assumed (i.e. model fit not significantly different from unrestrained model) and therefore partial measurement invariance was used in the final LTA model.
The third step of the analyses was performing the LTA (Graham et al. 1991; Collins & Wugalter, 1992), which aims to evaluate the probability of a transition from a symptom profile (or class) at one time-point to a profile at a later time-point. It builds on the LCA measurement model, which provides the measurement component of the model to capture the symptom profiles, and adds a longitudinal structural component to estimate changes among the profiles over time. The model estimates latent transition probabilities indicating change and/or stability of classes.
After participants were assigned to their most likely class, based on posterior probabilities, SPSS version 19 (SPSS Inc., USA) was used to evaluate baseline correlates of stable subtypes in univariable and multivariable analyses, including multinomial logistic regression. Analyzing the correlates of stable subtypes may give a more accurate picture of distinct characteristics of subtypes than subtypes derived from cross-sectional LCA, as stable subtypes are possibly more homogeneous and therefore more reliable than the subtypes found in cross-sectional studies.
Results
Cross-sectional models
Table 1 presents the fit indices for the latent class models. For the baseline measurement (T0), BIC indicated a two- or three-class solution and ssaBIC a three- or four-class solution. For the follow-up measurement (T1), both BIC and ssaBIC indicated the three-class solution. As the three-class model was also indicated by both indices at baseline, we adopted the three-class model for the baseline measurement. The same model was previously found to have the best fit using a larger sample of depressed persons at baseline (n=818) (Lamers et al. 2010).
Table 1.
Fit indices for the latent class models at each time-point
| No. of classes | BIC | ssaBIC |
|---|---|---|
| T0 | ||
| 1 | 6426.931 | 6369.800 |
| 2 | 6360.463 | 6243.027 |
| 3 | 6371.164 | 6193.422 |
| 4 | 6430.554 | 6192.507 |
| 5 | 6504.612 | 6206.259 |
| T1 | ||
| 1 | 6647.921 | 6590.790 |
| 2 | 6612.107 | 6494.670 |
| 3 | 6601.903 | 6424.161 |
| 4 | 6666.597 | 6428.550 |
| 5 | 6749.849 | 6451.496 |
BIC, Bayesian Information Criterion ; ssaBIC, sample size-adjusted BIC.
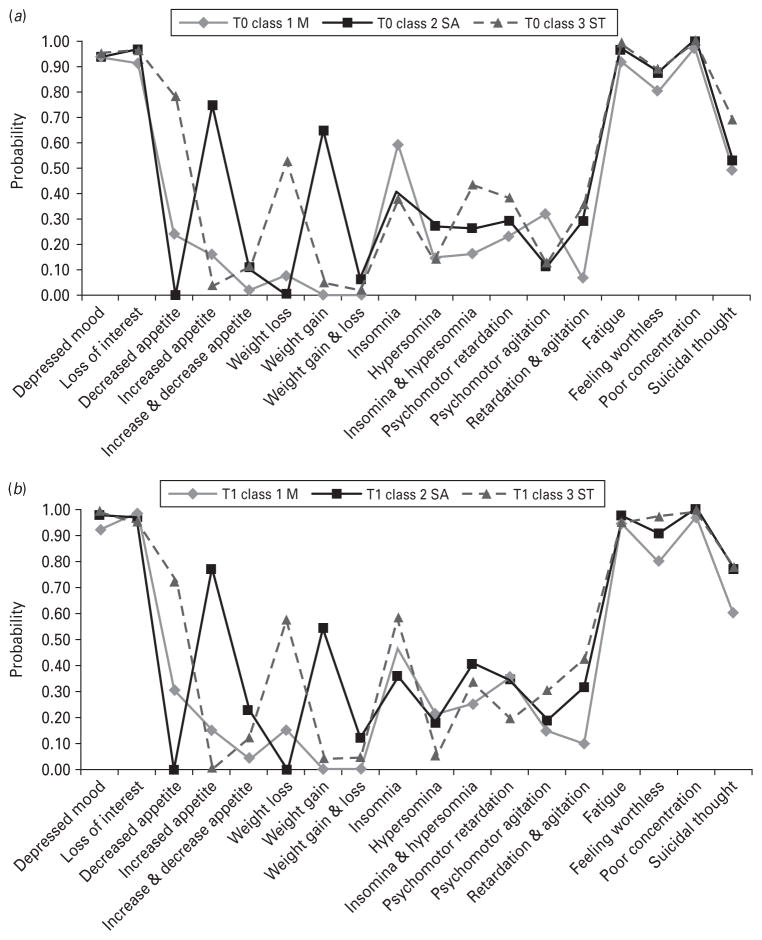
Fig. 1 presents the symptom probabilities across classes at both measurements. The first of the three classes was the severe typical class (estimated prevalence T0 29.6%, T1 24.7%), characterized by typical symptoms such as decreased appetite, weight loss and insomnia. The second class was labeled severe atypical (T0 30.9%, T1 33.7%) and was characterized by atypical symptoms such as increased appetite and weight gain. The third class was labeled moderate (T0 39.4%, T1 41.5%), as its symptom probabilities were overall lower than the other two classes, with lowest endorsement rates on feelings of worthlessness and suicidal thoughts. Small differences between the baseline and 2-year follow-up solutions were observed in the form of different probabilities for the items sleep, psychomotor changes and suicidal thoughts. For all classes, the probability of suicidal thoughts was lower in Wave 3. Overall, the observed differences in probabilities did not change the main interpretation of the three classes across measurements.
Fig. 1.
Symptom probabilities from the latent class models at (a) baseline and (b) the 2-year follow-up. M, Moderate; SA, severe atypical ; ST, severe typical.
LTAs
Table 2 shows the estimated transition probabilities from the LTA model. The estimated probabilities in the diagonal, which can be interpreted as coefficients of class stability, are all above 0.70, indicating relative stability across measurements. Highest stability was achieved in the severe atypical class (probability 0.79). The least stable class, but still with a stability coefficient of 0.70, was the severe typical class. As for change, most transitions seemed to occur from the severe typical to the moderate class (probability 0.24), and to a somewhat lesser extent from the moderate to the severe atypical class (probability 0.19). Of note, there was hardly any change from the moderate to the severe typical class.
Table 2.
Estimated transition probabilities across the latent classes (n=488)
| T0 | T1
|
||
|---|---|---|---|
| Moderate | Severe typical | Severe atypical | |
| Moderate | 0.779 | 0.027 | 0.194 |
| Severe typical | 0.243 | 0.706 | 0.051 |
| Severe atypical | 0.117 | 0.089 | 0.794 |
Correlates of stable subtype groups
Previous analyses of the severe typical, severe atypical and moderate subtypes, using baseline data only, revealed distinct patterns of correlates for the three subtypes (Lamers et al. 2010). Analyzing the correlates of stable subtypes may give a more accurate picture of distinct characteristics of subtypes, as stable subtypes are possibly more homogeneous and therefore more reliable than the subtypes found in cross-sectional studies. Therefore, we evaluated the correlates in the stable subtypes. Table 3 shows the characteristics of the three stable subtypes of depression. Differences in sex, age and years of education were observed between stable subtypes, with the severe atypical subtype showing a preponderance of females and younger age whereas the severe typical subtype had fewer years of education. The prevalence of panic disorder with agoraphobia was considerably lower in the moderate subtype. The moderate subtype also had an older age of onset and the lowest symptom severity. Of the psychosocial characteristics, functioning (WHODAS) score and neuroticism were higher in the severe typical subtype. Differences in physical health indicators were observed for current smoking at baseline, which was highest in the severe typical subtype and lowest in the severe atypical subtype, and number of pain locations, which was lower in the moderate subtype. Furthermore, BMI was highest in the severe atypical subtype, which also had the largest proportion of overweight and obese persons and had a higher number of metabolic syndrome components.
Table 3.
Characteristics of stable subgroups (n=394)
| Moderate (n=161) | Severe typical (n=111) | Severe atypical (n=122) | Overall p value | |
|---|---|---|---|---|
| Sociodemographics | ||||
| Female (%) | 61.5 | 65.8 | 79.5 | <0.01 |
| Age (years), mean (S.D.) | 43.8 (11.4) | 40.2 (12.1) | 39.6 (12.1) | <0.01 |
| Years of education, mean (S.D.) | 12.4 (3.2) | 10.8 (3.1) | 11.3 (3.3) | <0.0001 |
| Clinical characteristics | ||||
| Age of onset (years), median (IQR) | 27.0 (17.0–40.0) | 22.0 (17.0–34.0) | 22.0 (16.0–32.0) | 0.03 |
| Duration of symptoms (% time), median (IQR) | 0.31 (0.14–0.56) | 0.40 (0.19–0.66) | 0.29 (0.15–0.58) | 0.17 |
| Severity of symptoms, mean (S.D.) | 30.5 (11.4) | 39.1 (10.0) | 35.2 (35.2) | <0.0001 |
| MDQ manic symptoms (%) | 9.9 | 15.0 | 10.7 | 0.42 |
| Positive family history of depression (%) | 76.3 | 81.7 | 82.8 | 0.34 |
| Co-morbid diagnosis (%) | ||||
| Panic with agoraphobia | 11.8 | 29.7 | 24.6 | 0.001 |
| Social phobia | 34.2 | 43.2 | 43.4 | 0.19 |
| GAD | 33.5 | 43.2 | 34.4 | 0.22 |
| Psychosocial | ||||
| Functioning, mean (S.D.) | 30.8 (15.5) | 41.7 (15.5) | 37.0 (14.6) | <0.0001 |
| Neuroticism, mean (S.D.) | 41.2 (6.5) | 45.1 (5.1) | 43.8 (6.5) | <0.0001 |
| Extraversion, mean (S.D.) | 32.9 (7.5) | 32.1 (6.9) | 32.3 (6.1) | 0.59 |
| Childhood trauma index, median (IQR) | 1 (0–2) | 1 (0–3) | 1 (0–2) | 0.15 |
| No. of negative life events, median (IQR) | 1 (0–2) | 1 (0–2) | 1 (0–2) | 0.06 |
| Physical health | ||||
| Current smoking (%) | 45.3 | 59.5 | 32.8 | <0.0001 |
| No. of pain locations, mean (S.D.) | 3.7 (1.7) | 4.3 (1.7) | 4.1 (1.7) | 0.01 |
| BMI (kg/m2), mean (S.D.) | 25.5 (5.9) | 24.2 (4.8) | 28.7 (6.0) | <0.0001 |
| BMI categories (%) | ||||
| Normal and underweight (BMI <25 kg/m2) | 60.9 | 60.4 | 28.7 | <0.0001 |
| Overweight (BMI 25.0–29.9 kg/m2) | 22.4 | 27.0 | 37.7 | |
| Obese (BMI ⩾30 kg/m2) | 16.8 | 12.6 | 33.6 | |
MDQ, Mood Disorder Questionnaire; GAD, generalized anxiety disorder; S.D., standard deviation; IQR, interquartile range; BMI, body mass index.
Multi-variable multinomial logistic regression analyses were performed to compare stable subtypes, using all variables with p≤0.10 in univariable analyses, except for symptom severity, which was not included because it was considered to be a distinct component of the classification/subtypes. First, the stable moderate subtype was used as reference in the comparison with the severe atypical and severe typical subtype, and then the two severe stable subtypes where compared, using the severe typical stable subtype as reference (Table 4). For the comparisons with the moderate stable subtype as reference, being female was associated with the severe atypical stable subtype. Years of education was inversely associated with both severe stable subtypes, and having panic disorder with agoraphobia was associated with a twofold higher odds of being in the severe typical stable subtype compared to the moderate stable subtype, although this association was not significant (p=0.06). Age of onset was inversely associated with the severe atypical subtype. Having a higher functioning score was associated with the severe typical stable subtype whereas higher scores on the neuroticism scale were significantly associated with a higher odds of being in a severe stable subtype compared to the moderate stable subtype. The number of negative life events was also associated with a higher odds ratio (OR) of being in the severe typical stable subtype. Of the physical health indicators, current smoking was inversely associated with the severe atypical stable subtype whereas being overweight or obese was associated with a strongly increased OR of having the severe atypical subtype compared to the moderate subtype.
Table 4.
Multivariable analyses of correlates of stable subtypes (n=394)
| Severe typical versus Moderate (=ref.) | Severe atypical versus Moderate (=ref.) | Severe atypical versus Severe typical (=ref.) | |
|---|---|---|---|
| Sociodemographics | |||
| Female | 0.99 (0.55–1.77) | 2.40 (1.29–4.48) | 2.43 (1.24–4.76) |
| Age | 0.98 (0.95–1.00) | 0.98 (0.95–1.00) | 1.00 (0.97–1.03) |
| Years of education | 0.89 (0.82–0.98) | 0.92 (0.84–1.00) | 1.03 (0.93–1.13) |
| Clinical characteristics | |||
| Age of onset | 0.99 (0.97–1.02) | 0.97 (0.95–0.99) | 0.97 (0.95–1.00) |
| Co-morbid diagnosis | |||
| Panic with agoraphobia | 1.98 (0.98–3.99) | 1.61 (0.78–3.34) | 0.82 (0.41–1.62) |
| Psychosocial | |||
| Functioning | 1.02 (1.01–1.04) | 1.01 (0.99–1.03) | 0.99 (0.96–1.01) |
| Neuroticism | 1.06 (1.01–1.12) | 1.06 (1.01–1.11) | 0.99 (0.94–1.05) |
| Childhood trauma index | 1.14 (0.91–1.43) | 0.84 (0.66–1.07) | 0.74 (0.58–0.94) |
| No. of negative life events | 1.25 (1.01–1.55) | 1.18 (0.94–1.47) | 0.94 (0.76–1.17) |
| Physical health | |||
| Current smoking | 1.28 (0.74–2.21) | 0.48 (0.27–0.86) | 0.38 (0.21–0.69) |
| No. of pain locations | 1.12 (0.95–1.31) | 1.01 (0.86–1.19) | 0.91 (0.76–1.08) |
| BMI categories | |||
| Normal and underweight (BMI <25 kg/m2) | 1.00 | 1.00 | 1.00 |
| Overweight (BMI 25.0–29.9 kg/m2) | 1.18 (0.60–2.30) | 4.90 (2.52–9.55) | 4.17 (2.07–8.39) |
| Obese (BMI ⩾30 kg/m2) | 0.58 (0.25–1.33) | 6.03 (2.90–12.56) | 10.38 (4.42–24.35) |
BMI, Body mass index; ref., reference.
Values given as odds ratio (95% confidence interval).
As for the direct comparison of the two severe stable subtypes, we observed that being female and being overweight or obese was associated with having a higher OR of having the severe atypical stable subtype compared to the severe typical subtype, whereas a higher childhood trauma index score and current smoking were inversely associated with the severe atypical subtype. Age of onset was marginally and inversely associated with the severe atypical subtype (p=0.06). In a separate model with all variables from Table 4 except for BMI, we evaluated the associations between metabolic syndrome and its separate component with the severe atypical stable subtype. Having metabolic syndrome was significantly associated with the severe atypical stable subtype [OR 2.58, 95% confidence interval (CI) 1.31–5.08]. Of the separate components, only high waist circumference was significantly associated with the severe atypical subtype (OR 4.47, 95% CI 2.21–9.03) (not tabulated).
Discussion
This study demonstrates that depressive subtypes are relatively stable over 2 years. In our sample of 488 persons with a depressive diagnosis at both baseline and the 2-year follow-up, 76% manifested the same symptom profile at both measurements. The three subtypes identified at each time-point in this study confirm the subtypes that we earlier identified in the baseline data (Lamers et al. 2010). These include moderate and severe typical subtypes with typical symptoms such as decreased appetite and weight loss, but with differential severity, and a severe atypical subtype characterized by overeating and weight gain. The subtypes were characterized by different demographic and clinical correlates. For example, there was a predominance of females, more overweight and obesity, more metabolic syndrome, and less smoking in the severe atypical subtype. The severe typical subtype was also associated with co-morbid panic disorders with agoraphobia and higher functioning and neuroticism scores than the moderate type and also more childhood trauma than the severe atypical subtype.
These findings support the validity of these subtypes of depression. Despite the necessity of selecting persistent cases, the fact that subtypes were similar to those of the full baseline sample demonstrates the generalizability of these findings to depressed patients in general. This study further expands our knowledge of subtypes by looking at the stability of subtypes, an essential requirement for the validity of the delineation of subtypes. The few prior studies that evaluated the stability of subtypes examined psychotic and agitated/retarded subtypes, endogenous depression and melancholic depression. Stability rates from previous studies were 54% for psychotic, 65% agitated/retarded and 50–65% for endogenous depression over an 8-year follow-up period (Young et al. 1987; Coryell et al. 1994). A 15-year follow-up study yielded a stability rate of 29% for melancholia (Angst et al. 2007). These stability rates were substantially lower than the 71% rate for the severe typical subtype, and 79% for the atypical subtype over 2 years in the present study. Differences in stability rates may in part be explained by differences in time-frames, criteria used for subtype definition and statistical methodology. To our knowledge, the present study is the first to evaluate the prospective stability of the atypical subtype. The question of whether a stability rate of 76% is satisfactory is difficult to answer. Perfect stability (no transitions at all) seems impossible as some changes from severe to moderate types are to be expected with the waxing and waning of depression over time. We consider that, in this light, 76% is a very reasonable stability rate ; it is above the cut-off of 50% used by others to indicate relative stability (Geiser et al. 2006; Kleinjan et al. 2010).
The transitions that we observed involved transitions across subtypes of different severity and transitions across types of a different nature of symptoms (typical/atypical). Most of the transitions did occur across types of different severity, but it was notable that hardly anyone changed from the moderate subtype to the severe typical subtype. It seems that if those with a moderate subtype changed to a different subtype, they almost exclusively changed to an atypical subtype, whereas those with a severe typical subtype seemed to change mostly to a moderate subtype. This pattern of transitions was also observed in a sensitivity analysis using only participants with a high classification accuracy, defined as having a posterior probability ⩾0.80 (n=317, data not shown). Overall, the pattern of transitions observed in this study points to a unidirectional transition process, with persons transitioning mainly from moderate to severe atypical, from severe atypical to severe typical and from severe typical to moderate, but with hardly any transitions from moderate to severe typical and from severe typical to severe atypical. Transitions from the severe atypical to severe typical subtype may represent the phenomenon that endogenous/melancholic symptoms increase with increasing age (Brodaty et al. 1997; Parker et al. 2001).
Evaluation of the correlates of depression among those with stable subtypes enabled us to define more homogeneous subgroups of depression. Our finding of a female preponderance and higher rates of overweight and metabolic syndrome in the severe atypical subtype confirms findings of earlier research on correlates of atypical depression (Sullivan et al. 2002; Matza et al. 2003; Angst et al. 2006). Higher BMI and more metabolic syndrome may indicate that those with atypical depression have more obesity and other metabolic abnormalities. A previous study that linked metabolic abnormalities and depression suggested that such a subtype of depression could be labeled as ‘metabolic depression’ (Vogelzangs et al. 2011), but more research is needed to warrant such a label. The specific mechanisms for the higher rates of obesity in those with atypical depression should be investigated systematically in future studies. Atypical depression and metabolic dysregulation leading to obesity may share the same etiologic pathways, but obesity could also be simply the result of the overeating associated with atypical depression. In a recent review evaluating longitudinal associations between depression and BMI and vice versa, obesity was found to increase the risk of depression but depression was also found to be predictive of developing obesity (Luppino et al. 2010). In the only study that considered influence of atypical symptoms, atypical depression was found to mediate the association between childhood depressive symptoms and excessive weight gain in adolescence (Hasler et al. 2005). Recent work involving the fat mass and obesity-associated gene (FTO) has shown that depression moderates the effect of this gene on BMI, thereby suggesting that FTO may contribute to the association between obesity and depression (Rivera et al. 2011). This is a good example of a finding where subtyping of depression into more homogeneous subgroups may lead to discovery of distinct etiologic mechanisms.
The typical subtype’s higher score on childhood trauma compared to the atypical subtype and more negative life events than the moderate subtype highlight the importance of (early) life experiences/environmental factors in the development of typical/melancholic subtypes (Frank et al. 1994; Harkness & Monroe, 2002; Angst et al. 2007). The lesser severity of the moderate subtype was confirmed by lower functioning and neuroticism scores. Some correlates that we previously found to be associated with subtypes (family history, age of onset and duration of symptoms) were not significantly associated with the stable subtypes in the current study. This may be because, in the current analyses, we used stable subtypes instead of subtypes based on cross-sectional analyses, which may be less reliable, although Stoolmiller et al. (2005) found family history to be predictive of a chronic course.
Several researchers have given an overview of depressive subtypes. Recently, Lichtenberg & Belmaker (2010) presented an intuition-based proposal for classifying depressions. In the list of 10 (sometimes overlapping) subtypes, atypical depression was listed as a type whose pathophysiology may involve romantic disappointment, although no evidence for this was presented. In their overview, no other symptom-based types were described. Bech (2010) presented another subtyping schema in which the following types were distinguished : primary depression (melancholia), secondary (to stress) depression, secondary (to medication) depression, and less than major depression subtypes. Atypical depression was categorized under the primary depression, whereas our severe typical subtype may overlap with the unipolar depression listed. Where our moderate subtype would fit is unclear; it may be a milder form of unipolar depression. In a comprehensive review of subtyping models, Baumeister & Parker (2011) conducted a literature search and classified subtypes by symptom-based, etiology-based and time of onset-based subtypes. Female depression and treatment-resistant depression were also mentioned, but judged as too unspecific to qualify as a subtype of depression. The four symptom-based types were melancholic (or typical), psychotic, atypical and anxious depression. We identified typical and atypical subtypes, but not the psychotic or anxious subtypes. The concept of anxious depression may, however, overlap with melancholic and atypical types.
When interpreting the results of this study, several limitations should be taken into consideration. The sample of out-patients may not generalize to in-patient samples. Selection of people with 12-month diagnoses at both measurements may have differentially included those with a chronic course of depression. For some instruments, no official Dutch translation was available (Life Chart, MDQ, Family Tree Inventory, Life events, Pain scale), but these questionnaires were translated into Dutch and then back-translated to English as a check. In addition, as in any prospective study, the differential loss to follow-up of people with depression may have led to some bias in the sample. Some potential limitations of the LTA should be noted. We used only DSM-IV symptoms of depression in our models, which may have limited the analyses. However, a prior LCA based on baseline data only and including more symptoms of depression revealed the same subgroups as were found in the current analyses (Lamers et al. 2010), which suggests that adding more symptoms to the model does not necessarily change the outcome of the model. In the current analyses we also used two time-points and had relative stable subtypes. Although two time-points suffice for LTA analysis, it is possible that if we had had more follow-up measurements, more transitions would have occurred, and that the current results are therefore an overestimation of the true stability. We also evaluated transitions across a period of only 2 years. Although it has been reported that most symptom changes generally occur in the first year after the start of an episode (Penninx et al. 2008), future research should evaluate whether stability of symptomatology is indeed similar when longer time-periods are used. Furthermore, although some have used a cut-off of 50% to indicate relative stability and our stability rates are well above that, the interpretation of stability rates remains somewhat arbitrary. A relevant observation of our study, however, is that transitions between severe typical and severe atypical depression were not frequently occurring (only observed for 5% and 9% respectively), indicating that, when depression is chronic, persons generally present similar subtype symptoms over time. Lastly, we note that because our purpose was to evaluate the stability of subtypes of persons with depression, only those with depression at both time-points could be included. Had we included all respondents, regardless of depression status, more transition would have occurred due to onset and offset of depression.
To conclude, in the past decade there has been increased interest in identifying more homogeneous subtypes of depression but the stability of such subtypes has often been overlooked, even though stability is an important characteristic of a clinically meaningful subtype. This study shows that depressive subtypes are relatively stable over 2 years of follow-up and have partly distinct determinants.
Acknowledgments
The infrastructure for the NESDA (www.nesda.nl) is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development (Zon-Mw, grant no. 10-000-1002) and is supported by participating universities and mental health care organizations: VU University Medical Center, GGZ inGeest, Arkin, Leiden University Medical Center, GGZ Rivierduinen, University Medical Center Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Scientific Institute for Quality of Healthcare (IQ healthcare), the Netherlands Institute for Health Services Research (NIVEL) and the Netherlands Institute of Mental Health and Addiction (Trimbos). Dr Lamers is supported by a Rubicon fellowship from the Netherlands Organization for Scientific Research (NWO).
Footnotes
Declaration of Interest
None.
References
- Andrews G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Social Psychiatry and Psychiatric Epidemiology. 1998;33:80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Benazzi F, Ajdacic V, Rossler W. Melancholia and atypical depression in the Zurich study : epidemiology, clinical characteristics, course, comorbidity and personality. Acta Psychiatrica Scandinavica. 2007;155:72–84. doi: 10.1111/j.1600-0447.2007.00965.x. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Benazzi F, Silverstein B, Ajdacic-Gross V, Eich D, Rossler W. Atypical depressive syndromes in varying definitions. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:44–54. doi: 10.1007/s00406-005-0600-z. [DOI] [PubMed] [Google Scholar]
- Baumeister H, Parker G. Meta-review of depressive subtyping models. Journal of Affective Disorders. 2011 doi: 10.1016/j.jad.2011.1007.1015. Published online : 31 August 2011. [DOI] [PubMed] [Google Scholar]
- Bech P. Struggle for subtypes in primary and secondary depression and their mode-specific treatment or healing. Psychotherapy and Psychosomatics. 2010;79:331–338. doi: 10.1159/000320118. [DOI] [PubMed] [Google Scholar]
- Brodaty H, Luscombe G, Parker G, Wilhelm K, Hickie I, Austin MP, Mitchell P. Increased rate of psychosis and psychomotor change in depression with age. Psycholgical Medicine. 1997;27:1205–1213. doi: 10.1017/s0033291797005436. [DOI] [PubMed] [Google Scholar]
- Brugha T, Bebbington P, Tennant C, Hurry J. The List of Threatening Experiences : a subset of 12 life event categories with considerable long-term contextual threat. Psychological Medicine. 1985;15:189–194. doi: 10.1017/s003329170002105x. [DOI] [PubMed] [Google Scholar]
- Buist-Bouwman MA, Ormel J, De Graaf R, Vilagut G, Alonso J, Van Sonderen E, Vollebergh WA. Psychometric properties of the World Health Organization Disability Assessment Schedule used in the European Study of the Epidemiology of Mental Disorders. International Journal of Methods in Psychiatric Research. 2008;17:185–197. doi: 10.1002/mpr.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chwastiak LA, Von Korff M. Disability in depression and back pain: evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. Journal of Clinical Epidemiology. 2003;56:507–514. doi: 10.1016/s0895-4356(03)00051-9. [DOI] [PubMed] [Google Scholar]
- Collins LM, Wugalter SE. Latent class models for stage-sequential dynamic latent variables. Multivariate Behavioural Research. 1992;27:131–157. [Google Scholar]
- Coryell W, Winokur G, Shea T, Maser JD, Endicott J, Akiskal HS. The long-term stability of depressive subtypes. American Journal of Psychiatry. 1994;151:199–204. doi: 10.1176/ajp.151.2.199. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Domains and facets : hierarchical personality assessment using the revised NEO personality inventory. Journal of Personality Assessment. 1995;64:21–50. doi: 10.1207/s15327752jpa6401_2. [DOI] [PubMed] [Google Scholar]
- de Graaf R, Bijl RV, Smit F, Vollebergh WA, Spijker J. Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders : findings from the Netherlands Mental Health Survey and Incidence Study. American Journal of Psychiatry. 2002;159:620–629. doi: 10.1176/appi.ajp.159.4.620. [DOI] [PubMed] [Google Scholar]
- Frank E, Anderson B, Reynolds CF, III, Ritenour A, Kupfer DJ. Life events and the research diagnostic criteria endogenous subtype. A confirmation of the distinction using the Bedford College methods. Archives of General Psychiatry. 1994;51:519–524. doi: 10.1001/archpsyc.1994.03950070011005. [DOI] [PubMed] [Google Scholar]
- Fyer AJ, Weissman MM. Genetic linkage study of panic : clinical methodology and description of pedigrees. American Journal of Medical Genetics. 1999;88:173–181. [PubMed] [Google Scholar]
- Geiser C, Lehmann W, Eid M. Separating ‘ rotators ‘ from ‘ nonrotators ’ in the Mental Rotations Test : a multigroup latent class analysis. Multivariate Behavioral Research. 2006;41:261–293. doi: 10.1207/s15327906mbr4103_2. [DOI] [PubMed] [Google Scholar]
- Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression : high vs low CRH/NE states. Molecular Psychiatry. 2002;7:254–275. doi: 10.1038/sj.mp.4001032. [DOI] [PubMed] [Google Scholar]
- Graham JW, Collins LM, Wugalter SE, Chung NK, Hansen WB. Modeling transitions in latent stage-sequential processes : a substance use prevention example. Journal of Consulting and Clinical Psychology. 1991;59:48–57. doi: 10.1037//0022-006x.59.1.48. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Monroe SM. Childhood adversity and the endogenous versus nonendogenous distinction in women with major depression. American Journal of Psychiatry. 2002;159:387–393. doi: 10.1176/appi.ajp.159.3.387. [DOI] [PubMed] [Google Scholar]
- Hasler G, Pine DS, Kleinbaum DG, Gamma A, Luckenbaugh D, Ajdacic V, Eich D, Rossler W, Angst J. Depressive symptoms during childhood and adult obesity : the Zurich Cohort Study. Molecular Psychiatry. 2005;10:842–850. doi: 10.1038/sj.mp.4001671. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck PE, Jr, Lewis L, McElroy SL, Post RM, Rapport DJ, Russell JM, Sachs GS, Zajecka J. Development and validation of a screening instrument for bipolar spectrum disorder : the Mood Disorder Questionnaire. American Journal of Psychiatry. 2000;157:1873–1875. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- Hoekstra HA, Ormel J, de Fruyt F. Handleiding NEO persoonlijkheidsvragenlijsten NEO-PI-R en NEO-FFI [Manual NEO personality questionnaires NEO-PI-R and NEO-FFI] Swets Test Services; Lisse: 1996. [Google Scholar]
- IDS/QIDS. Instruments in English and Multiple Translations. 2012. [Accessed 6 January 2012]. ( www.ids-qids.org/tr-dutch.html)
- Kleinjan M, Wanner B, Vitaro F, Van den Eijnden RJ, Brug J, Engels RC. Nicotine dependence subtypes among adolescent smokers: examining the occurrence, development and validity of distinct symptom profiles. Psychology of Addictive Behaviors. 2010;24:61–74. doi: 10.1037/a0018543. [DOI] [PubMed] [Google Scholar]
- Lamers F, de Jonge P, Nolen WA, Smit JH, Zitman FG, Beekman AT, Penninx BW. Identifying depressive subtypes in a large cohort study : results from the Netherlands Study of Depression and Anxiety (NESDA) Journal of Clinical Psychiatry. 2010;71:1582–1589. doi: 10.4088/JCP.09m05398blu. [DOI] [PubMed] [Google Scholar]
- Lamers F, Hoogendoorn AW, Smit JH, van Dyck R, Zitman FG, Nolen WA, Penninx BWJH. Socio-demographic and psychiatric determinants of attrition in the Netherlands Study of Depression and Anxiety (NESDA) Comprehensive Psychiatry. 2012;53:63–70. doi: 10.1016/j.comppsych.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Pettit JW, Joiner TE, Jr, Seeley JR. The symptomatic expression of major depressive disorder in adolescents and young adults. Journal of Abnormal Psychology. 2003;112:244–252. doi: 10.1037/0021-843x.112.2.244. [DOI] [PubMed] [Google Scholar]
- Lichtenberg P, Belmaker RH. Subtyping major depressive disorder. Psychotherapy and Psychosomatics. 2010;79:131–135. doi: 10.1159/000286957. [DOI] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression : a systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Nestadt G, Cwi J, Heithoff K, Eaton WW. The Life Chart Interview : a standardized method to describe the course of psychopathology. International Journal of Methods in Psychiatric Research. 1994;4:143–155. [Google Scholar]
- Matza LS, Revicki DA, Davidson JR, Stewart JW. Depression with atypical features in the National Comorbidity Survey : classification, description, and consequences. Archives of General Psychiatry. 2003;60:817–826. doi: 10.1001/archpsyc.60.8.817. [DOI] [PubMed] [Google Scholar]
- Minor KL, Champion JE, Gotlib IH. Stability of DSM-IV criterion symptoms for major depressive disorder. Journal of Psychiatric Research. 2005;39:415–420. doi: 10.1016/j.jpsychires.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Muthén & Muthén; Los Angeles, CA: 1998–2010. [Google Scholar]
- Nierenberg AA, Pava JA, Clancy K, Rosenbaum JF, Fava M. Are neurovegetative symptoms stable in relapsing or recurrent atypical depressive episodes ? Biological Psychiatry. 1996;40:691–696. doi: 10.1016/0006-3223(96)00029-7. [DOI] [PubMed] [Google Scholar]
- Nylund K. Doctoral dissertation. University of California; Los Angeles: 2007. Latent transition analysis : modeling extensions and an application to peer victimization. [Google Scholar]
- Nylund KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- Oquendo MA, Barrera A, Ellis SP, Li S, Burke AK, Grunebaum M, Endicott J, Mann JJ. Instability of symptoms in recurrent major depression : a prospective study. American Journal of Psychiatry. 2004;161:255–261. doi: 10.1176/appi.ajp.161.2.255. [DOI] [PubMed] [Google Scholar]
- Parker G, Roy K, Hadzi-Pavlovic D, Wilhelm K, Mitchell P. The differential impact of age on the phenomenology of melancholia. Psychological Medicine. 2001;31:1231–1236. doi: 10.1017/s0033291701004603. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Prusoff BA, Tanner J. Temporal stability of symptom patterns in depression. British Journal of Psychiatry. 1976;128:369–374. doi: 10.1192/bjp.128.4.369. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Beekman ATF, Smit JH, Zitman FG, Nolen WA, Spinhoven P, Cuijpers P, de Jong PJ, van Marwijk HWJ, Assendelft WJJ, van der Meer K, Verhaak P, Wensing M, de Graaf R, Hoogendijk WJ, Ormel J, van Dyck RNESDA Research Consortium. The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. International Journal of Methods in Psychiatric Research. 2008;17:121–140. doi: 10.1002/mpr.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera M, Cohen-Woods S, Kapur K, Breen G, Ng MY, Butler AW, Craddock N, Gill M, Korszun A, Maier W, Mors O, Owen MJ, Preisig M, Bergmann S, Tozzi F, Rice J, Rietschel M, Rucker J, Schosser A, Aitchison KJ, Uher R, Craig IW, Lewis CM, Farmer AE, McGuffin P. Depressive disorder moderates the effect of the FTO gene on body mass index. Molecular Psychiatry. 2011 doi: 10.1038/mp.2011.1045. Published online : 19 April 2011. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS) : psychometric properties. Psychological Medicine. 1996;26:477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Stoolmiller M, Kim HK, Capaldi DM. The course of depressive symptoms in men from early adolescence to young adulthood : identifying latent trajectories and early predictors. Journal of Abnormal Psychology. 2005;114:331–345. doi: 10.1037/0021-843X.114.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard AJ, Fernstrom MH, Price A, Frank E, Kupfer DJ. Direction of weight change in recurrent depression. Consistency across episodes. Archives of General Psychiatry. 1990;47:857–860. doi: 10.1001/archpsyc.1990.01810210065009. [DOI] [PubMed] [Google Scholar]
- Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the National Comorbidity Survey. American Journal of Psychiatry. 1998;155:1398–1406. doi: 10.1176/ajp.155.10.1398. [DOI] [PubMed] [Google Scholar]
- Sullivan PF, Prescott CA, Kendler KS. The subtypes of major depression in a twin registry. Journal of Affective Disorders. 2002;68:273–284. doi: 10.1016/s0165-0327(00)00364-5. [DOI] [PubMed] [Google Scholar]
- Vogelzangs N, Beekman AT, Boelhouwer IG, Bandinelli S, Milaneschi Y, Ferrucci L, Penninx BW. Metabolic depression : a chronic depressive subtype ? Findings from the InCHIANTI study of older persons. Journal of Clinical Psychiatry. 2011;72:598–604. doi: 10.4088/JCP.10m06559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Korff M. Epidemiologic and survey methods: chronic pain assessment. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. 2. Guilford Press; New York: 2001. pp. 603–618. [Google Scholar]
- West ED, Dally PJ. Effects of iproniazid in depressive syndromes. British Medical Journal. 1959;1:1491–1494. doi: 10.1136/bmj.1.5136.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Composite International Diagnostic Interview, Core Version 2.1 : Interviewer’s Manual. World Health Organization; Sydney, Australia: 1997. [Google Scholar]
- Yang CC. Evaluating latent class analysis models in qualitative phenotype identification. Computational Statistics and Data Analysis. 2006;50:1090–1104. [Google Scholar]
- Young MA, Fogg LF, Scheftner WA, Fawcett JA. Concordance of symptoms in recurrent depressive episodes. Journal of Affective Disorders. 1990;20:79–85. doi: 10.1016/0165-0327(90)90120-w. [DOI] [PubMed] [Google Scholar]
- Young MA, Keller MB, Lavori PW, Scheftner WA, Fawcett JA, Endicott J, Hirschfeld RM. Lack of stability of the RDC endogenous subtype in consecutive episodes of major depression. Journal of Affective Disorders. 1987;12:139–143. doi: 10.1016/0165-0327(87)90006-1. [DOI] [PubMed] [Google Scholar]