ABSTRACT
Introduction:
Neurological disorders are the leading causes of death and disability globally. In low-middle-income countries such as India, there is a wide treatment gap for neurological disorders. To address this gap, an initiative known as the Karnataka Brain Health Initiative (KaBHI) was developed in collaboration with the public health system of the state of Karnataka in India.
Method:
A structured hybrid training program was conducted for 120 medical doctors working in the Primary Health Centers (PHCs) in the public health system in three districts of Karnataka. Pre- and post-training evaluation was conducted to assess physicians’ knowledge and skills for evaluating patients with common neurological conditions.
Results:
Of 120 PHC doctors, 111 (92%) scored below the passing score of 50 points out of 100 before the training program. After the training, all trainees scored above this cut-off. The study found a significant improvement in knowledge and skills after the training (before training: 40.48 ± 7.92, after training: 66.28 ± 8.98 (P < 0.001) mean difference = 25.81), and was comparable among the PHC doctors in all three districts.
Conclusions:
Our study shows the feasibility of training primary care doctors in the public health system to manage selected common neurological disorders. The training program can potentially help to reduce the treatment gap for neurological disorders in India.
Keywords: Karnataka Brain Health Initiative, KaBHI, neurological disorders, primary healthcare doctors, training program, treatment gap
Introduction
Neurological disorders are a major public health challenge worldwide and a leading cause of disability-adjusted life years (DALYs) lost and mortality in adults. Every year, nearly ten million deaths occur due to neurological disorders worldwide.[1,2] In low-middle-income countries (LMICs) such as India, stroke, headache, dementia, and epilepsy are the predominant contributors to disability from neurological disorders, and among them stroke is the leading cause of mortality.[3] Early diagnosis and treatment of neurological disorders can significantly reduce the burden of neurological disorders in the community.[4] However, there is a wide treatment gap for neurological disorders in India [dementia: 90%,[5] epilepsy: 50% to 90%,[6] stroke: 30%[7]] primarily due to low awareness, limited accessibility to neurological services, especially in remote areas,[3] and unaffordability of specialist services.[7]
Globally, there exists a significant mismatch between the burden of neurological disorders and the availability of neurologists. In LMICs like India, there are reports of one neurologist for every 3,200,000 people in 1998, and this number improved to one neurologist for every 1,250,000 people in 2002.[8] However, despite the progress, there are approximately 2500 neurologists serving a population of more than one billion people in the India.[9] Therefore there is an urgent need to increase service coverage for neurological disorders at the community level.[10] The World Health Organization (WHO) suggests the adoption of capacity-building programs that can enhance the training and education for primary health care professionals to diagnose, treat, and provide care for patients with neurological disorders.[11] Primary health care has been identified as the foundation of effective health systems, as well as the best approach to achieving universal health coverage and meeting sustainable development goals.[12] PHC doctors provide basic health services at the community level and are important components of health delivery systems.[13] To ensure access to neurological services in remote areas, it is important to integrate neurological care into primary care. To the best of our knowledge, currently there are no operational health care delivery models to promote brain health or treat neurological diseases in the public health system in India or other LMICs.
Neurological disorders require early diagnosis, long-term treatment, and rehabilitation to reduce burden and improve patients’ quality of life.[14] Many common neurological disorders can be diagnosed and treated at the PHC level.[15,16] Additionally, these centres can provide timely referrals to specialised centres and continued care for patients. Therefore, it is crucial for PHC doctors to be able to identify, diagnose and treat individuals with neurological disorders, and thereby strengthen primary health care systems.
The major challenge for prevention and treatment of neurological disorders at the PHC level is the lack of adequate knowledge and skills among PHC professionals.[17] In a study carried out in the Northern part of India, to assess the knowledge, attitudes and practices (KAP), one fourth of the medical officers were found to have minimal experience in management of epilepsy and some of them (16%) even considered epilepsy to be a mental illness.[16] Previous studies have focused on the impact of training of health care providers in core clinical skills and treatment of disorders related to mental health, dermatological conditions, and tobacco use/dependence.[18,19,20,21,22] However, there have been few studies evaluating effectiveness of training health care providers for neurological disorders. These studies have focussed on individual diseases such as headache,[23,24,25] epilepsy,[26] dementia[27,28] and stroke.[29] The format of training adopted in these studies included continuing medical education (CMEs), didactic lectures, case discussions, providing education materials, and workshops.[25,26,28,29] A systematic approach to training PHC professionals comprehensively for all major neurological disorders has not been implemented. There is hence a need to develop and implement training programs to strengthen proficiency among PHC professionals to diagnose and manage major neurological disorders and also enable timely referrals to specialist care when required.
In order to address this treatment gap, a public health initiative was developed in the state of Karnataka, India to implement an evidence-based comprehensive model for prevention, diagnosis, and equitable care of neurological disorders across all levels of health care known as Karnataka Brain Health Initiative (KaBHI). This initiative is in collaboration with National Institution for Transforming India (NITI) Aayog, the policy think-tank of the Government of India and the Department of Health and Family Welfare, Government of Karnataka. A major component of the Brain Health Initiative was to systematically build capacity among PHC doctors. In this study, we aimed to assess the effectiveness of training PHC doctors in diagnosis and treatment of major neurological disorders.
Method
The Karnataka Brain Health Initiative (KaBHI) was launched in both urban and rural Karnataka, India in three pilot districts of Chikkaballapura (population-1255104), Kolar (population-1699696), and Bengaluru South region (population-2199888) of Bengaluru urban district [Figure 1]. These districts were selected for convenience as they are located close to the National Institute of Mental Health and Neuroscience (NIMHANS).
Figure 1.
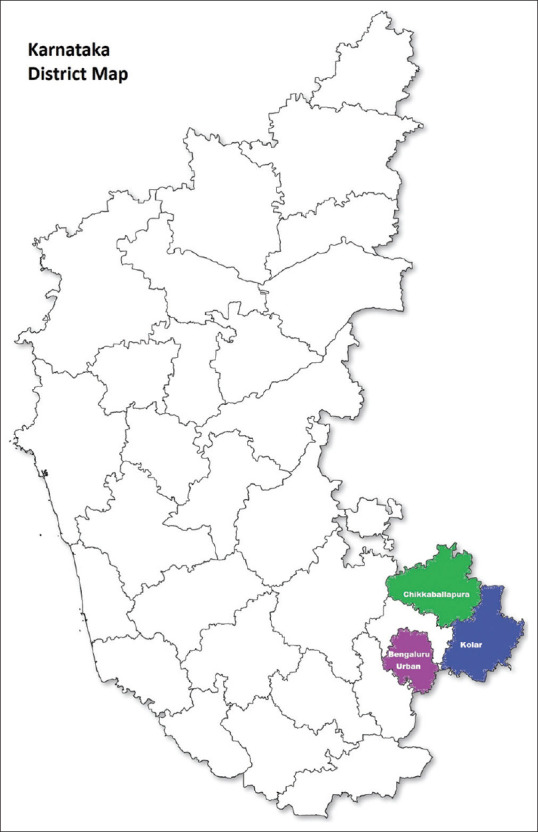
Map of selected districts (Map Source: Government of Karnataka, Official Website)
Participants and sampling
In the public health system, each district has a district hospital which provides tertiary and secondary care. Community health centres provide primary and some secondary level care at the block headquarters and cover a population of about 100,000 and primary health centres (PHCs) cater to a population of about 20000 to 30000. PHCs are present in both urban and rural areas and are the medical facilities closest to the communities where a doctor is present. As An official communication was sent by the Karnataka State Health Commissioner to the District Health Officers and doctors working in the PHCs in three pilot districts to participate in the study. The three districts have a total of 159 PHCs. All the doctors who attended the training program were included in the study. we expected a minimum improvement of knowledge and clinical skills to 10% of the PHC doctors. Assuming a 10% improvement in the scores after the training, a sample size of 120 participants was considered to be adequate with a power of 0.90 at α =0.05.
Study procedure
We adopted a quasi-experimental pre- and post-test study design without a control group. The study was conducted in March and April, 2022. The doctors at the PHC were subjected to a structured training program on diagnosis and treatment of common neurological disorders. In collaboration with the Department of Health and Family Welfare, Government of Karnataka, the training program was developed by expert neurologists from a postgraduate training institute in neurology (NIMHANS) with extensive experience in training doctors.
Structure of training program: A hybrid training program was conducted over a period of two months which included one in-person workshop and total of nine online training sessions for all the three districts. During the in-person workshop (each lasting for 4 to 4.5 hours), specialists in the areas of headache, epilepsy, stroke, and dementia discussed approaches to diagnosis and treatment with the PHC doctors. Three in-person workshops were organised, one each at Chikkaballapura, Kolar, and Bengaluru South in order to facilitate interaction and build rapport between specialists and primary health care doctors. An introduction to history taking and clinical examination in neurology was conducted initially. Following this, the participants were trained in early identification, diagnosis and treatment of these disorders through case-based discussions and evidence-based protocols.
Specialist neurologists subsequently conducted nine weekly interactive online training sessions each lasting for 90 minutes over a period of two months for the PHC professionals. The topics included the following: approaches to neurological history and examination, classification, diagnosis and management of headache, epilepsy, stroke, dementia and neuroinfections. This online training program consisted of didactic lectures, case vignettes, poll-based questions, and interactive discussions between experts and PHC doctors professionals [Table 1]. The focus of the online training program was to reiterate and reinforce the learning and skills of PHC doctors acquired during the in-person workshops. Specialist neurologists also addressed the queries by the PHC doctors in managing patients with the selected neurological problems through telephone calls when required.
Table 1.
Teaching contents and methods
| Mode | Content | Methods | Time allocation |
|---|---|---|---|
| In-person | An introduction to history taking and clinical examination Identification Diagnosis and treatment of common neurological disorders | Didactic lectures interactive case-based discussions and evidence-based protocols | 4 to 4.5 hours each session |
| Clinical Skills Evaluation | OSCE- Objective Structured Clinical Examination (five stations) | 5 minutes/station | |
| Online training | 1. Approach to the Common Neurological Symptoms | Lectures | 90 minutes/session |
| 2. Approach to Neurological Examination | Case vignettes | ||
| 3. Approach to diagnosis and the classification of Epilepsy | Case-based interactive discussions | ||
| 4. Approach to the Classification and Management of Epilepsy | Poll-based questions | ||
| 5. Approach to headache | |||
| 6. Approach and Management of Neuroinfections | |||
| 7. Road Map to Dementia and Examination of Dementia | |||
| 8. Dementia Diagnosis, Management, and Rehabilitation | |||
| 9. Diagnosis and Management of Stroke |
Development and validation of the KaBHI primary healthcare physicians training questionnaire: The KaBHI primary healthcare physicians training questionnaire aimed at assessing the knowledge of common neurological disorders was developed and validated. Series of focussed group meetings/discussions by expert neurologists and public health specialists were conducted to develop the questionnaire. Based on consensus from the expert panel, 50 objective-type questions and 10 descriptive-type questions were developed. Content validation of the questionnaire was carried out by six expert neurologists. A Likert scale which consisted of five options (not at all, a little, moderate, very much, extremely) was employed to evaluate the usefulness of questions for assessing knowledge. Questions rated “very much” and “extremely” from at least five out of the six experts were considered to include in the questionnaire. Appropriate modifications were made based on the suggestions from experts, resulting in a more comprehensive questionnaire. A pilot study was conducted on a sample of ten medical doctors. Two raters administered and scored the adapted questionnaire on pilot participants independently. Inter-rater reliability was determined by Cohen’s kappa and there was 90% agreement between the two raters. The internal consistency of the pilot data was examined using Cronbach’s alpha and the coefficient was 0.93. Based on the modifications from the pilot study, a final version of the questionnaire was finalised which included a total of 32 objective-type questions (2 points/question = 64 points) and 4 descriptive questions (9 points/question = 36 points). The questionnaire also included questions on basic socio-demographic information such as age, gender, education, and years of experience. Based on the pilot study, if a PHC professional scored greater than 50 points out of 100 after the training program, they were considered to have adequate knowledge about neurological disorders.
Evaluation: A pre- and post-training evaluation of 120 PHC doctors was conducted to assess their knowledge of neurological disorders before and after the training program using the KaBHI primary healthcare physicians training questionnaire. Both pre- and post-training evaluation consisted of the same set of descriptive and objective questions to assess the gain in knowledge and skills through training. The questionnaire included objective and descriptive questions deriving a total of 100 points. Pre-training evaluation was conducted during an in-person workshop, whereas post-training evaluations were collected using Google Forms, and the data was matched using participants’ mobile phone numbers.
Additionally, an Objective Structured Clinical Examination (OSCE) was conducted after the training program. The OSCE was conducted at the Brain Health Clinics, located in district level general hospitals by a team of trained general physicians and neurologists from tertiary care centres. The OSCE evaluated doctors’ practical knowledge on headache, epilepsy, stroke, and dementia. Five examination stations were included in OSCE, one for each disorder and a clinical signs demonstration station with a total of 10 points for each station.
Rural/urban definition: We defined rural and urban areas according to Census of India (2011): An urban area was defined as “all places with municipality, corporation, cantonment board or notified town area committee” and a rural area should satisfy the following criteria: (1) population size lesser than 5000; (2) more than 25% of the male workforce engaged in non-agricultural occupations; and (3) population density greater than 400/km2 (National Sample Survey Organization- Ministry of Statistics and Programme implementation, Government of India).[30]
Statistical analysis
Demographic characteristics and test scores are expressed in mean (SD) for continuous variables and frequency (percentage) for categorical variables. Pre- and post-test scores were compared by using the paired t-test. Continuous data was analysed using ANOVA and Tukey test to measure the differences between the OSCE scores across the three districts. The Statistical Package for Social Sciences (SPSS) software version 16.0 was used to analyse the data (SPSS, Chicago, IL). A value of P < 0.05 was considered as statistically significant.
Ethics
The research study was approved by the Institutional Ethics Committee of National Institute of Mental Health and Neurosciences (NIMHANS) and informed consent was obtained from all participants.
Results
A total of 120 PHC doctors participated, representing 75% of the 159 PHCs, in the three districts. Among the three in-person workshops held in Chikkaballapura, Kolar, and Bengaluru South, the participation rates were 53 (44.2%), 41 (34.2%), and 26 (21.6%) respectively. On the other hand, during the online training sessions, the number of participants ranged from 71 to 99 per session out of the total 120 attendees of the in-person workshops. The average age of the participants was 34.9 ± 6.63 years (range: 24-55) and the average years of experience was 7.82 ± 5.62 (range: 0.5-24). There were 67 females (55.8%) and 53 males (44.1%). Among the PHC doctors, a majority were doctors trained in modern medicine (109, 90.8%) while some were trained in traditional medical practice of Unani (11, 9.2%) respectively. The descriptive characteristics of PHC doctors are presented in Table 2.
Table 2.
Demographic and educational characteristics of PHC doctors from three districts of Karnataka
| Mean | |
|---|---|
| Age in years Mean (SD) | 34.95 (6.63) |
| Years of clinical experience Mean (SD) | 7.82 (5.62) |
| Gender | |
| Male | 53 (44.1%) |
| Female | 67 (55.8%) |
| Education | |
| Bachelor in Unani Medicine and Surgery (BUMS) | 11 (9.2%) |
| Bachelor of Medicine and Bachelor of Surgery (MBBS) | 97 (80.8%) |
| Bachelor of Medicine and Bachelor of Surgery, Diploma in Public Health (MBBS, DPH) | 1 (0.8%) |
| Doctor of Medicine (MD) | 11 (9.2%) |
| District Wise | |
| Chikkaballapura | 53 (44.1%) |
| Kolar | 41 (34.2%) |
| Bengaluru South | 26 (21.6%) |
The paired-t test demonstrated that there was a significant increase in the questionnaire test scores before and after the training program (P < 0.001). A significant improvement was also found across specific neurological disorders including headache, epilepsy, stroke, and dementia (P < 0.001). The details of pre- and post-training scores of the PHC doctors on the KaBHI primary health care physicians training questionnaire is presented in Table 3. Consistent improvement was also observed in post-training scores of PHC doctors across all the three districts [Table 4]. Among 120 PHC doctors, 111 (92%) scored below 50 points before the training program. After the training program, a significant improvement was observed. All the PHC doctors (N = 120, 100%) scored above the set cut-off score of 50 points out of 100 on the questionnaire.
Table 3.
Pre- and post-training scores of PHC doctors on the KaBHI primary health care physicians training questionnaire across different neurological disorders
| Pre-training scores (n=120) Mean (SD) | Post-training scores (n=120) Mean (SD) | Mean difference | P | |
|---|---|---|---|---|
| Objective type (Max score: 64) | 25.21 (6.53) | 42.45 (6.48) | 17.23 | <0.001 |
| Descriptive type (Max score: 36) | 15.27 (3.08) | 23.76 (3.63) | 8.48 | <0.001 |
| Total (Max score: 100) | 40.48 (7.92) | 66.28 (8.98) | 25.81 | <0.001 |
|
| ||||
| Scores obtained for different neurological disorders | ||||
|
| ||||
| Headache (Max score: 25) | 12.67 (2.71) | 19.18 (2.77) | 6.52 | <0.001 |
| Epilepsy (Max score: 25) | 10.63 (2.42) | 16.88 (2.69) | 6.24 | <0.001 |
| Stroke (Max score: 25) | 8.96 (2.35) | 17.02 (2.69) | 7.91 | <0.001 |
| Dementia (Max score: 25) | 8.22 (2.01) | 14.65 (2.12) | 6.43 | <0.001 |
Table 4.
Pre- and post-training scores of PHC doctors on the KaBHI primary health care physicians training questionnaire across three districts of Karnataka
| Chikkaballapura | Kolar | Bengaluru South | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Pre-training scores (n=53) Mean (SD) | Post-training scores (n=53) Mean (SD) | Mean difference | P | Pre-training scores (n=41) Mean (SD) | Post-training scores (n=41) Mean (SD) | Mean difference | P | Pre-training scores (n=26) Mean (SD) | Post-training scores (n=26) Mean (SD) | Mean difference | P | |
| Objective type (Max score: 64) | 26.26 (7.15) | 43.94 (5.85) | 17.67 | <.0001 | 24.53 (6.02) | 39.58 (6.47) | 15.05 | <.0001 | 24.12 (5.81) | 43.81 (6.44) | 19.69 | <.0001 |
| Descriptive type (Max score: 36) | 15.26 (3.33) | 23.72 (3.64) | 8.45 | <.0001 | 15.13 (2.89) | 22.78 (2.70) | 7.65 | <.0001 | 15.50 (2.94) | 25.35 (4.34) | 9.84 | <.0001 |
| Total (Max score: 100) | 41.52 (10.48) | 67.66 (9.49) | 26.13 | <.0001 | 39.66 (8.91) | 62.36 (9.17) | 23.02 | <.0001 | 39.62 (8.75) | 69.15 (10.78) | 29.53 | <.0001 |
|
| ||||||||||||
| Scores obtained for different neurological disorders | ||||||||||||
|
| ||||||||||||
| Headache (Max score: 25) | 12.79 (2.93) | 20.02 (2.43) | 7.22 | <.0001 | 12.32 (2.42) | 17.66 (2.76) | 5.341 | <.0001 | 12.96 (2.73) | 19.88 (2.53) | 6.92 | <.0001 |
| Epilepsy (Max score: 25) | 10.98 (2.52) | 17.19 (2.61) | 6.20 | <.0001 | 9.95 (2.04) | 15.59 (2.44) | 5.634 | <.0001 | 11.00 (2.63) | 18.27 (2.40) | 7.26 | <.0001 |
| Stroke (Max score: 25) | 9.25 (2.58) | 15.85 (2.33) | 6.60 | <.0001 | 9.12 (2.12) | 15.05 (1.78) | 6.463 | <.0001 | 8.12 (2.08) | 15.85 (3.39) | 7.73 | <.0001 |
| Dementia (Max score: 25) | 8.51 (2.30) | 14.60 (2.02) | 6.09 | <.0001 | 8.27 (1.39) | 14.39 (1.81) | 6.122 | <.0001 | 7.54 (2.08) | 15.15 (2.70) | 7.61 | <.0001 |
The performance of PHC doctors from three districts of Karnataka on objective structured clinical examination (OSCE) across different neurological disorders was examined. There was no significant difference in the performance of PHC doctors on the OSCE scores between neurological disorders (headache (P = 0.086); epilepsy (P = 0.064); stroke (P = 0.426); dementia (P = 0.141) and in clinical sign demonstration (P = 0.379) [See Table 5].
Table 5.
Post-training Objective Structured Clinical Examination (OSCE) scores of PHC doctors on diagnosis and treatment of common neurological disorders across three districts of Karnataka
| OSCE (n=73) | Chikkaballapura Mean (SD) (n=33) | Kolar Mean (SD) (n=22) | Bengaluru South Mean (SD) (n=19) | P |
|---|---|---|---|---|
| Headache (Max score: 10) | 6.70 (1.78) | 7.55 (2.04) | 6.05 (1.78) | 0.093 |
| Epilepsy (Max score: 10) | 7.70 (.85) | 7.41 (1.05) | 7.47 (.84) | 0.041 |
| Stroke (Max score: 10) | 7.71 (1.02) | 8.09 (1.47) | 7.26 (1.10) | 0.381 |
| Dementia (Max score: 10) | 7.78 (.49) | 7.77 (1.41) | 7.42 (.90) | 0.473 |
| Clinical Sign demonstration (Max score: 10) | 8.03 (.73) | 7.45 (1.29) | 7.63 (1.00) | 0.092 |
| Total OSCE Score (Max score: 50) | 37.92 (4.87) | 38.14 (4.91) | 35.83 (5.62) | 1.08 |
The performance of PHC doctors was compared based on their age and years of experience after acquiring the last degree. The baseline performance was the same across all age groups (<30 years, 30-40 years and ≥ 40 years) and years of experience (<5 years, 5-10 years, 10-15 years, >15 years). [Supplementary Tables 1 and 2]. The improvement following the training program was significantly more (P value = 0.036) in the younger doctors (age < 30 years) as compared to the older doctors (≥40 years) [Figure 2]. The improvement in knowledge remained same across all categories of years of experience.
Figure 2.
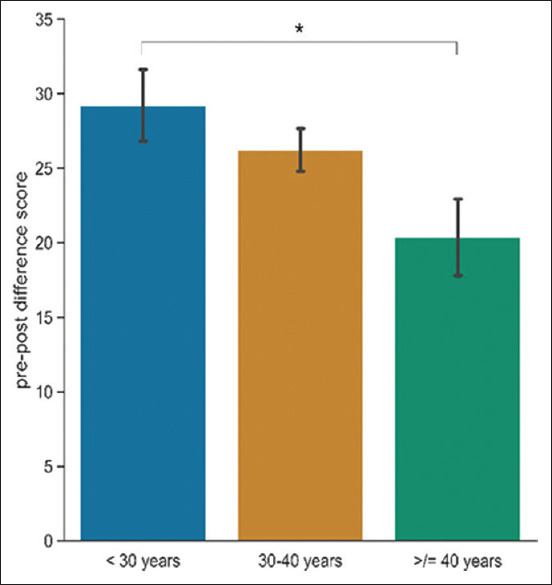
Bar plot showing age wise comparison of PHC doctors in the degree of knowledge improvement. Error bars represent standard error
Discussion
The PHC doctors participating in the study were observed to have limited knowledge about neurological disorders prior to the training program. Following a structured and systematic training program, both the knowledge and the skills to diagnose major neurological disorders such as headache, epilepsy, stroke, and dementia were found to improve significantly.
Additionally, we also observed that the improvement in knowledge and skills was significantly higher among doctors aged less than 30 years. The study shows the feasibility of training doctors at the primary health centres in the public health system in manging common neurological disorders. To our knowledge this is the first of its kind initiative to improve brain health in a low- and middle-income country.
In the background of a rising burden of neurological disorders globally, and a wide treatment gap, WHO advocates capacity building programs for primary health care professionals to diagnose and treat neurological disorders.[11] Previous studies have demonstrated positive outcomes of training of health care providers in the treatment of several non-neurological disorders[18,19,20,21,22] However, the effectiveness of training health care providers for neurological disorders is limited to a few individual diseases.[23,25,31,32] The diagnostic accuracy and choice of proper treatment significantly improved following a training program in the context of headache and migraine disorders in primary healthcare providers and general practitioners.[23,24,31,32] Another study[26] found that the knowledge, attitude and practice towards epilepsy among 50 general practitioners improved after two training modules six months apart, in Bolivia, an LMIC. Furthermore, in Germany, there was a significant gain in knowledge in management of dementia among 166 general practitioners after an interactive dementia training session that included 30 minutes of lecture and 45 minutes of structured case discussion.[27] To the best of our knowledge, this is the first study that has assessed the effectiveness of training of PHC doctors comprehensively on a range of neurological disorders including epilepsy, stroke, headache and dementia from India or any other LMIC.
The current study provides evidence that training PHC doctors in diagnosis and treatment of common neurological disorders is feasible and effective in building capacity of primary care physicians who serve at the grassroot levels of health care. The current study is the first of its kind measuring the effectiveness of training PHC doctors in the public health system in India in diagnosis and management of common neurological disorders. The training program significantly improved the theoretical and practical knowledge of PHC doctors in neurological disorders and will facilitate the reduction of the existing treatment gap for neurological disorders in India.
Our study indicated that a majority of PHC doctors lacked sufficient knowledge to effectively diagnose and manage the common neurological conditions, consistent with earlier studies.[23,26,27] This knowledge gap may lead to incorrect diagnosis and treatment, delaying timely intervention and increasing risk of progression of disability. The lack of adequate knowledge among PHC doctors could also result in unwarranted patient referrals to specialist neurologists, in turn increasing the cost of care. Based on the recommendations from a National Consultation on Strengthening Primary Health Care in Rural India,[33] building, empowering, and training primary health care professionals was identified as one of the factors to improve comprehensive care, especially for health care in rural India. In the background of a huge disparity in access to and utilization of primary health care services between rural and urban areas in India, improving access to health care in the rural areas is a major priority.[33]
In our study, a hybrid training program was organised that incorporated both in-person workshops and online sessions. These workshops, focused on the diagnosis and treatment of common neurological disorders, facilitated by experts using case-based discussions and evidence-based protocols. To additionally enhance knowledge acquired during in-person workshops, an online weekly training program was conducted over a period of two months. This training program featured didactic lectures, case vignettes, poll-based questions, and interactive discussions between PHC doctors and experts. Along with the training, evidence-based protocols were also provided as resources and the mentorship by the experts was continued beyond the training period to address the clinical challenges faced by them in their practice. The training program incorporated in the current study is in line with the recommendations from meta-analyses of studies examining different types of medical education programs and workshops,[34,35] that suggest that the use of interactive learning methods mixed with didactic formats could bring about a major change in practice.
In this study, PHC doctors from both rural (n = 71) and urban (n = 49) areas were trained to diagnose and treat common neurological disorders. There was a significant improvement in knowledge and skills of PHC doctors practicing in both rural and urban regions before and after the training program and this improvement was found to be comparable between rural and urban PHC doctors. This effort of capacity building potentially benefits provision of neurological services at the primary care level, particularly in remote areas, and help bridge the gap in the neurological care between rural and urban areas.[15,16] Our study findings are consistent with a recent study in rural Karnataka that demonstrated a gain in knowledge of common mental disorders (CMDs) among 38 primary health center doctors after undergoing approximately 3 hours of training session on identification and treatment of CMDs.[36]
The global burden of disease study concluded that the increasing prevalence of neurological diseases needs to be addressed with newer strategies of prevention and treatment.[1] According to WHO, better professional education is the best method for implementing change.[37] Neurological disorders are most prevalent in the community and majority of patients make their first contact with PHC doctors. A well-functioning primary healthcare system is a key component to promote coordination among health care levels and ensure patients receive optimal care.[38] During the process of training in the current study, we recognised that the interaction between PHC professionals and neurologists during the in-person workshops helped in building rapport between the specialists and the PHC doctors, and this was reflected in the subsequent online sessions. This rapport laid a strong foundation in development of an effective referral pathway from primary to tertiary levels of health care systems in Karnataka. It is especially important to build an effective long-term working relationship in the context of health center workers and difficult working circumstances at the PHC level.[39]
Several potential challenges were identified in the training program, including the following:
The doctors who participated in this study were operating in extremely busy PHCs where patient care took precedence. As a result, arranging both in-person and online training programs proved to be very challenging.
The highest number of participants in the online training session is 99 (82.5%). The remaining participants were unable to attend the training sessions due to other concurrent training programs.
During the online training sessions, maintaining a consistent number of participants posed difficulties due to network and technical problems.
The above-mentioned challenges may be addressed by integration of brain health initiative program in an existing national health program such as the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) or National Mental Health Programme (NMHP).
There are some limitations to our study. The effectiveness of training was assessed within a short two-month period; hence the long-term retention of knowledge and skills may require future study. Though there was a significant improvement in the knowledge and skills of the PHC doctors, the impact on referral patterns and patient related outcomes like health-related quality of life and disability was not evaluated in this study but will be evaluated in the next phase of KaBHI. The number of PHC doctors who took part in the training program was relatively small as the study involved only three districts from the state of Karnataka.
Conclusions
This study is the first of its kind that assessed the effectiveness of training PHC doctors comprehensively on a range of neurological disorders from India. The results of the evaluation clearly demonstrate that the knowledge and clinical skills of PHC doctors improved significantly following the training. The study establishes the feasibility and effectiveness of incorporating a training component to the development of a public health strategy to integrate care of neurological disorders into existing health care services and other LMIC settings.
Contributors
SA, PM, RP, RD, GNR, GBK, and AP contributed to the study design development. SA, AP, FV, SG, RS, ANVJ and AV contributed towards data collection, verification, and statistical analysis. SA, PM, AP, SG, DB, AV and YK contributed to the manuscript preparation. The manuscript was finalized with considerable input from the Karnataka Brain Health Initiative (KaBHI) Consortium [Supplementary Material].
Data sharing statement
Data supporting the findings of this study are available from the corresponding author [SA] on request.
Ethical policy and Institutional Review board statement
The research study was approved by the Institutional Ethics Committee of National Institute of Mental Health and Neurosciences (NIMHANS).
Patient declaration of consent statement
Informed consent was obtained from all participants.
List of Abbreviations
| Abbreviation | Definition |
|---|---|
| PHCs | Primary Health Centers |
| KaBHI | Karnataka Brain Health Initiative |
| DALYs | Disability-Adjusted Life Years |
| LMICs | Low-Middle-Income Countries |
| WHO | World Health Organization |
| CMEs | Continuing Medical Education |
| NITI | National Institution for Transforming India |
| NIMHANS | National Institute of Mental Health and Neuroscience |
| OSCE | Objective Structured Clinical Examination |
| NPCDCS | National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke |
| NMHP | National Mental Health Programme |
Financial support and sponsorship
This research was supported by funding from the Government of Karnataka [Grant No. Amount (A) PR/07/2022-23] and Shri Nanjangud G. Viswanath (NGV) Foundation [Grant No. IN-KA46180725785629U].
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the Scientific Advisory Group (SAG) of the Karnataka Brain Health Initiative (KaBHI) for their expertise extended towards the project: Suman P N Rao, Jeyaraj Durai Pandian, Giridhar R Babu, Subhash Kaul, Prashant Mathur, N. Sreekumaran Nair, Gururaj G. We also, extend our thanks to Shri Nanjangud G Viswanath Foundation for research support through the Healthcare Access and Innovation Laboratory.
Supplementary Material
Karnataka Brain Health Initiative (KaBHI) Consortium
| First Name | Last Name | Affiliations |
|---|---|---|
| Ajay Asranna | I.P | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Andleeb | Zeba | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Farhan Ansari | Mohammad | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Anush | R | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Bipin | Balakrishnan | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Channabasavaiah | B V | General Physician, Bangalore District, Jayanagar General Hospital |
| Deepak | Menon | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Devendrappa | K R | Physician, Government Hospital, Jayanagar |
| Faheem | Arshad | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Geetha | S | Medical Officer, JP Nagar Urban Primary Health Center, Bangalore |
| Haleema | Sara | Medical Officer, Jayanagar Dispensary, Bangalore |
| Hansashree | P | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Hariprasad | T Nambiar | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Harshvardhan | Palamangalam | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Hemant Kumar | B G | Department of Psychiatry, Chikkbalapur District Hospital |
| Jadhav Prithi | Gokuldasrao | Diplomate of National Board Trainee, Bangalore District, Jayanagar General Hospital |
| Jagdeesh | MA | District Health Officer, Kolar |
| Kavya | K | Medical Officer, Sugatur Primary Health Center, Kolar |
| Kishore | D N | Department of Psychiatry, Chikkbalapur District Hospital |
| Madhu | N | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Mahesh | Kumar | District Health Officer, Chikkbalapur |
| Monisha | V | District Program Coordinator, Chikkbalapur |
| Nalini | A | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Narayan Swamy | A V | Medical Officer, Dargamohalla Primary Health Center, Kolar |
| Narayanaswami | NC | District Leprosy Officer, Kolar |
| Navaneeth | Kunnumbarth | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Netravathi | M | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Nidhi | C | Diplomate of National Board Trainee, Jayanagar General Hospital, Bangalore |
| Prajwal | C S | Medical Officer, Wilson Garden Primary Health Center, Bangalore |
| Pramod | K Pal | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Priya Treesa | Thomas | Department of Psychiatric Social Work, National Institute of Mental Health and Neurosciences |
| Radhika | B V | Medical Officer, Sri Narasimha Raja District Hospital, Kolar |
| Ramakrishnappa | - | Medical Superintendent, Bangalore District, Jayanagar General Hospital |
| Ramesh | P V | Department of Medicine, Chikkbalapur District Hospital |
| Rashmi | M B | General Physician, Bangalore District, Jayanagar General Hospital |
| Raveena | R Nambiar | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Renuka | B R | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Reshma | B V | Pulmonologist, Sri Narasimha Raja District Hospital Hospital, Kolar |
| Sabitha | Romeo | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Sahana | N C | Medical Officer, Jayanagar Urban Primary Health Center, Bangalore |
| Sandeep | M R | General Physician, Bangalore District, Jayanagar General Hospital |
| Saraswathi | Nashi | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Seena | V | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Shayeebulla Khan | C.N | Diplomate of National Board Trainee, Bangalore District, Jayanagar General Hospital |
| Sheethal | Sasi | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Shivkumar | District Leprosy Officer, Chikkaballapur | |
| Sirish Kasyap | K | Medical Officer, Billuru Primary Health Center, Chikkaballapur |
| Srinivas | R | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Subasree | Ramakrishnan | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Suma | Sheelavantar | Non-Communicable Diseases, District Program Coordinator, Kolar District |
| Suresh | Gangully | Health Officer Bruhat Bengaluru Mahanagara Palike South Health Administration |
| Suhas | V P | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Vikram | V Holla | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Veeranna Gowda | K M | Senior Consultant & Diplomate of National Board Trainee, Post Graduate Teacher, Bangalore District |
| Vijaya Kumar | S N | District Surgeon, Sri Narasimha Raja District Hospital, Kolar |
| Vishwanathan | L G | Department of Neurology, National Institute of Mental Health and Neurosciences |
| Yogesh | K | Physician, Sri Narasimha Raja District Hospital, Kolar |
Supplementary Tables
Supplementary Table 1.
Age-Stratified evaluation of scores before and after the training program
| Variables | <30 years (n=26) (mean, SD) | 30-40 years (n=72) (mean, SD) | ≥40 years (n=22) (mean, SD) | P | Post-hoc comparison (Tukey) |
|---|---|---|---|---|---|
| Pre-training score | 39.50 (8.00) | 40.32 (7.55) | 42.14 (9.08) | 0.503 | - |
| Post-training improvement score | 29.23 (12.25) | 26.24 (12.22) | 20.36 (12.05) | 0.042* | <30 years vs ≥40 years (P=0.036*) |
*Significant, P<0.05
Supplementary Table 2.
Experience-Based evaluation of pre- and post-training scores
| Variables | <5 years (n=42) (mean, SD) | 5-10 years (n=41) (mean, SD) | 10-15 years (n=22) (mean, SD) | >15 years (n=14) (mean, SD) | P |
|---|---|---|---|---|---|
| Pre-training score | 40.74 (7.57) | 39.61 (5.45) | 40.64 (10.18) | 41.64 (11.35) | 0.843 |
| Post-training improvement score | 28.00 (12.57) | 27.17 (11.44) | 23.77 (11.73) | 19.43 (14.24) | 0.106 |
References
- 1.Feigin VL, Nichols E, Alam T, Bannick MS, Beghi E, Blake N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:459–80. doi: 10.1016/S1474-4422(18)30499-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ding C, Wu Y, Chen X, Chen Y, Wu Z, Lin Z, et al. Global, regional, and national burden and attributable risk factors of neurological disorders: The Global Burden of Disease study 1990–2019. Front Public Health. 2022;10:952161. doi: 10.3389/fpubh.2022.952161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh G, Sharma M, Kumar GA, Rao NG, Prasad K, Mathur P, et al. The burden of neurological disorders across the states of India: The Global Burden of Disease Study 1990–2019. Lancet Glob Health. 2021;9:e1129–44. doi: 10.1016/S2214-109X(21)00164-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giunti P, Morris S, Relja M, Pastores G, Quoidbach V. Toward earlier diagnosis and treatment of rare neurological disorders: The value of coordinated care and specialist centers. Croat Med J. 2019;60:156–7. doi: 10.3325/cmj.2019.60.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dias A, Patel V. Closing the treatment gap for dementia in India. Indian J Psychiatry. 2009;51((Suppl 1)):S93–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Rathore C, Radhakrishnan K. Epilepsy treatment gap in India: Is it too high a peak to scale? Ann Indian Acad Neurol. 2020;23:580. doi: 10.4103/aian.AIAN_919_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke. 2013;15:128–34. doi: 10.5853/jos.2013.15.3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gourie-Devi M. Organization of neurology services in India: Unmet needs and the way forward. Neurol India. 2008;56:4–12. doi: 10.4103/0028-3886.39304. [DOI] [PubMed] [Google Scholar]
- 9.Singh G, Khadilkar S, Jayalakshmi S. The Future of Neurology in India 2020. [updated 13.01.2020] [[Last accessed on 2023 Jul 31]]. Available from: https://worldneurologyonline.com/article/the-future-of-neurology-in-india/
- 10.Owolabi MO, Leonardi M, Bassetti C, Jaarsma J, Hawrot T, Makanjuola AI, et al. Global synergistic actions to improve brain health for human development. Nat Rev Neurol. 2023;19:371–83. doi: 10.1038/s41582-023-00808-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Organization WH. Atlas: Country resources for neurological disorders 2004: Results of a collaborative study of the World Health Organization and the World Federation of Neurology. World Health Organization. 2004 [Google Scholar]
- 12.Mash R, Almeida M, Wong WC, Kumar R, Von Pressentin KB. The roles and training of primary care doctors: China, India, Brazil and South Africa. Hum Resour Health. 2015;13:1–9. doi: 10.1186/s12960-015-0090-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shidhaye R, Lund C, Chisholm D. Closing the treatment gap for mental, neurological and substance use disorders by strengthening existing health care platforms: Strategies for delivery and integration of evidence-based interventions. Int J Ment Health Syst. 2015;9:1–11. doi: 10.1186/s13033-015-0031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thakur K, Tablante E, Harper M, Shakir R, Bergen D, Dua T. The World Health Organization Atlas 2015: Country Resources for Neurological Disorders (PL01. 001) AAN Enterprises. 2016 [Google Scholar]
- 15.Krishnan A, Chowdhury D. Burden, disability and public health importance of headache disorders in India. Neurol India. 2021;69((Supplement)):S4–9. doi: 10.4103/0028-3886.315984. [DOI] [PubMed] [Google Scholar]
- 16.Buddhiraja R, Sharma S, Sharma S, Bansal RK, Setia RK, Bansal N, et al. Epilepsy knowledge, attitudes, and practices among primary healthcare providers in an Indian district. Epilepsy Behav. 2020;104:106899. doi: 10.1016/j.yebeh.2019.106899. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Draft intersectoral global action plan on epilepsy and other neurological disorders 2022–2031. Geneva: 2022. [DOI] [PubMed] [Google Scholar]
- 18.Kebriaei A, Rothe V, Pitner S, Balluff M, Salama F. Effectiveness of a basic training presentation on infant oral health care for pediatric medicine residents. J Clin Pediatr Dent. 2008;33:143–6. doi: 10.17796/jcpd.33.2.14t3v37277x17q75. [DOI] [PubMed] [Google Scholar]
- 19.Tsai J-C, Liu K-M, Lee K-T, Yen J-C, Yen J-H, Liu C-K, et al. Evaluation of the effectiveness of postgraduate general medicine training by objective structured clinical examination—pilot study and reflection on the experiences of Kaohsiung Medical University Hospital. Kaohsiung J Med Sci. 2008;24:627–33. doi: 10.1016/S1607-551X(09)70027-0. [DOI] [PubMed] [Google Scholar]
- 20.Sheffer CE, Barone CP, Anders ME. Training health care providers in the treatment of tobacco use and dependence: Pre-and post-training results. J Eval Clin Pract. 2009;15:607–13. doi: 10.1111/j.1365-2753.2008.01058.x. [DOI] [PubMed] [Google Scholar]
- 21.Makaula PU, Chateau AV, Hift RJ, Dlova NC, Mosam A. The impact of basic dermatology education and training on primary healthcare providers in KwaZulu-Natal, South Africa. S Afr Fam Pract (2004) 2021;63:e1–5. doi: 10.4102/safp.v63i1.5200. doi: 10.4102/safp.v63i1.5200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayano G, Assefa D, Haile K, Chaka A, Haile K, Solomon M, et al. Mental health training for primary health care workers and implication for success of integration of mental health into primary care: Evaluation of effect on knowledge, attitude and practices (KAP) Int J Ment Health Syst. 2017;11:1–8. doi: 10.1186/s13033-017-0169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patwardhan MB, Samsa GP, Lipton RB, Matchar DB. Changing physician knowledge, attitudes, and beliefs about migraine: Evaluation of a new educational intervention. Headache. 2006;46:732–41. doi: 10.1111/j.1526-4610.2006.00427.x. [DOI] [PubMed] [Google Scholar]
- 24.Karli N, Zarifoglu M, Erer S, Pala K, Akis N. The impact of education on the diagnostic accuracy of tension-type headache and migraine: A prospective study. Cephalalgia. 2007;27:41–5. doi: 10.1111/j.1468-2982.2006.01245.x. [DOI] [PubMed] [Google Scholar]
- 25.Braschinsky M, Haldre S, Kals M, Iofik A, Kivisild A, Korjas J, et al. Structured education can improve primary-care management of headache: The first empirical evidence, from a controlled interventional study. J Headache Pain. 2016;17:1–7. doi: 10.1186/s10194-016-0613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giuliano L, Cicero CE, Padilla S, Camargo M, Sofia V, Zappia M, et al. Knowledge, attitudes, and practices towards epilepsy among general practitioners in rural Bolivia: Results before and after a training program on epilepsy. Epilepsy Behav. 2018;83:113–8. doi: 10.1016/j.yebeh.2018.02.030. [DOI] [PubMed] [Google Scholar]
- 27.Vollmar HC, Mayer H, Ostermann T, Butzlaff ME, Sandars JE, Wilm S, et al. Knowledge transfer for the management of dementia: A cluster-randomised trial of blended learning in general practice. Implement Sci. 2010;5:1–10. doi: 10.1186/1748-5908-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee L, Weston WW, Hillier LM. Developing memory clinics in primary care: An evidence-based interprofessional program of continuing professional development. J Contin Educ Health Prof. 2013;33:24–32. doi: 10.1002/chp.21163. [DOI] [PubMed] [Google Scholar]
- 29.Rababah JA, Al-Hammouri MM, AlNsour EA. Effectiveness of an educational program on improving healthcare providers'knowledge of acute stroke: A randomized block design study. World J Emerg Med. 2021;12:93–8. doi: 10.5847/wjem.j.1920-8642.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hui R, Wescoat JL., Jr Visualizing peri-urban and rurban water conditions in Pune district, Maharashtra, India. Geoforum. 2019;102:255–66. [Google Scholar]
- 31.Vincent MB, de Carvalho JJ. Primary headache care delivery by nonspecialists in Brazil. Brazilian Headache Care Cooperative Group. Cephalalgia. 1999;19:520–4. doi: 10.1046/j.1468-2982.1999.019005520.x. [DOI] [PubMed] [Google Scholar]
- 32.Peters M, Vydelingum V, Abu-Saad HH, Dowson A. Migraine and chronic daily headache management: Implications for primary care practitioners. J Clin Nurs. 2007;16:159–67. doi: 10.1111/j.1365-2702.2006.01562.x. [DOI] [PubMed] [Google Scholar]
- 33.Mohan P, Kumar R. Strengthening primary care in rural India: Lessons from Indian and global evidence and experience. J Family Med Prim Care. 2019;8:2169–72. doi: 10.4103/jfmpc.jfmpc_426_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis D, O'Brien MAT, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–74. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 35.Forsetlund L, O’Brien MA, Forsén L, Reinar LM, Okwen MP, Horsley T, et al. Continuing education meetings and workshops: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2021;9:CD003030. doi: 10.1002/14651858.CD003030.pub3. doi: 10.1002/14651858. CD003030.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salazar LJ, Ekstrand ML, Selvam S, Heylen E, Pradeep JR, Srinivasan K. The effect of mental health training on the knowledge of common mental disorders among medical officers in primary health centres in rural Karnataka. J Family Med Prim Care. 2022;11:994–9. doi: 10.4103/jfmpc.jfmpc_1353_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization. Transforming and scaling up health professionals'education and training: World Health Organization guidelines 2013. World Health Organization. 2013 [PubMed] [Google Scholar]
- 38.Seyed-Nezhad M, Ahmadi B, Akbari-Sari A. Factors affecting the successful implementation of the referral system: A scoping review. J Family Med Prim Care. 2021;10:4364–75. doi: 10.4103/jfmpc.jfmpc_514_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tarannum S, Elshazly M, Harlass S, Ventevogel P. Integrating mental health into primary health care in Rohingya refugee settings in Bangladesh: Experiences of UNHCR. Intervention. 2019;17:130. [Google Scholar]


