Abstract
Background
The shoulder is a complex joint that has the most extensive range of motion among all joints, resulting in more susceptibility to dislocation. The treatment for acute shoulder dislocation is closed reduction, which should be performed immediately. Arthroscopic Bankart repair (ABR) is a procedure for treating anterior shoulder instability. This systematic review aimed to evaluate the published literature on ABR for anterior shoulder instability.
Material/Methods
We searched electronic databases, including Google Scholar, PubMed, Science Direct, Scopus, and PubMed, to find literature about our topic published between 2018 and 2023. Different keywords were searched, including “ABR, shoulder, instability, dislocation, treatment, management, recurrence, outcomes, and complications”. The inclusion criteria were English original articles with available full text.
Results
Only 8 articles were included; the articles included a total of 398 patients with an age range of 15 to 55 years old. One study was conducted on male patients, and another was conducted on female patients, whereas the remaining studies were conducted on both sexes. Among the 8 studies, 4 studies conducted ABR alone, and all reported significant change with ABR. Four studies compared ABR with Latarjet, concomitant remplissage, and immobilization and reported that ABR is equivalent or better than these interventions.
Conclusions
ABR was effective in the management of shoulder instability, as it resulted in a lower rate of recurrence, low rate of complications, and high rate of return to sport, regardless of the suture type. However, it is superior or similar to other interventions, like Latarjet and concomitant remplissage.
Keywords: Arthroscopy; Outcome Assessment, Health Care; Shoulder; Bankart Lesions
Introduction
The shoulder is a complex joint, where stability has been sacrificed in favor of range of motion [1]. The shoulder joint has the largest range of motion among all joints [2], making the joint more liable to dislocate following the injury of the anterior labrum, which is the master stabilizer of the glenohumeral joint [3,4]. A traumatic shoulder dislocation is often accompanied by a labral lesion, which predisposes the patient to develop chronic shoulder instability [5]. Primary shoulder dislocation incidence varies between 15.3 and 56.3 per 100 000 individual-years [6,7]. In sports medicine, anterior instability of the shoulder joint is quite prevalent, particularly in athletes, young men, and military people, who experience dislocations at a rate as high as 3% per year [8,9]. The incidence of anterior shoulder instability in the general population ranges from 8% to 25% per 100 000 person-years [10].
Shoulder instability occurs when the structures that keep the shoulder joint in place are damaged or weakened, often due to trauma, repetitive strain, or congenital factors, such as hypermobility. More recently, biomechanical research has shown that following a single dislocation of the shoulder joint complex, abnormal biomechanics alter, and the likelihood of recurrent instability rises; these disturbances in the kinetics compound with further dislocations [11,12]. These long-term biomechanical alterations and the dose-dependent effects of numerous instability events support early surgical stabilization to lower recurrence and maximize function [13–15].
Management involves a combination of non-surgical and surgical approaches. Non-surgical treatment typically includes physical therapy to strengthen the shoulder muscles, activity modification, and possibly bracing. If instability persists or is severe, surgical intervention can be required to repair or reconstruct the damaged structures. The acute treatment of shoulder dislocation is closed reduction and should be performed as soon as possible. Stabilization can be indicated following the first dislocation. Most patients with chronic post-traumatic shoulder instability are offered to undergo stabilization surgery [5].
Conservative treatment of anterior instability of the shoulder joint can result in a high recurrence rate of 87% in patients at high risk after the first episode of dislocation [16]. Even in situations with bipolar bone loss, open Bankart repair has been proven to be a durable choice, with a recurrence rate of less than 1% at short and long follow-ups [17,18]. Bankart repair focuses on the anatomical re-attachment of the labrum to the glenoid rim [2].
During the arthroscopic Bankart repair (ABR), small incisions are made around the shoulder, and an arthroscope is inserted to visualize the joint. Using specialized instruments, the surgeon reattaches the torn labrum to the socket, typically with the help of anchors or sutures. Because of its minimally invasive nature and capacity to treat concurrent injuries, ABR has largely replaced open Bankart repair during the past few decades, particularly in cases of minor glenoid or humeral bone loss [19]. Most surgeons favor ABR as the first surgical treatment for anterior shoulder instability, as it is the most frequently performed surgical operation worldwide [20]. ABR has raised concerns since, according to published research, it produced significant rates of instability recurrence of up to 40% [21]. Appropriate patient selection, the state of the preserved soft tissue, and careful surgical technique – including the positioning of suture anchors and the quantity of sutures passed – are all necessary for successful outcomes in ABR [22]. Therefore, this systematic review was performed to evaluate the effects of ABR in the management of anterior shoulder instability and in comparison with other interventions, to study the evidence of its effectiveness.
In this systematic review, we compiled and examined the existing data on ABR, offering a thorough assessment of the treatment’s efficacy. As a result, we can offer healthcare professionals the most recent and trustworthy data to support clinical judgments about the application of ABR. In systematic reviews that gather data, ABR is frequently compared with other therapy options for shoulder instability, such as open Bankart repair, conservative care, or other surgical procedures. By comparing the advantages and disadvantages of various treatment choices, this comparative analysis can aid physicians and patients in making well-informed decisions. In conducting this systematic review, we offer a methodical and thorough way to assess the results of ABR in treating shoulder instability, which will eventually help guide future research, educate clinical judgment, and enhance patient care. Therefore, this systematic review aimed to evaluate the published literature on arthroscopic Bankart repair for anterior shoulder instability.
Material and Methods
Information Sources, Search Strategy and Selection Process
This systematic review follows the PRISMA checklist guidance [23]. We searched via electronic databases, including Google Scholar, PubMed, SciElco, Science Direct, Scopus, and PubMed, to find literature about our topic. A group of different keywords were used for searching purposes, including “ABR, shoulder, instability, dislocation, treatment, management, recurrence, outcomes, complications”, which were used in different combinations to obtain all possible related articles. The search process was restricted to articles published in English from 2018 till 2023.
Eligibility Criteria
The titles generated by this initial investigation were all rewritten using the following criteria: first, duplicate articles and articles on recurrent patients were eliminated as indicated by the titles; second, the study design was reviewed for each article through the titles and abstract to include only the original articles and exclude other types, like reviews, case reports, systematic reviews, meta-analyses, and letters to the editor; third, the articles were checked for language and full-text availability; non-English articles and those not available for full text were excluded; and, lastly, only original English articles with full-text availability were included.
Synthesis Method
The full data of each article was checked, and articles containing incomplete data were excluded. The illustration of the search strategy is shown in Figure 1.
Figure 1.
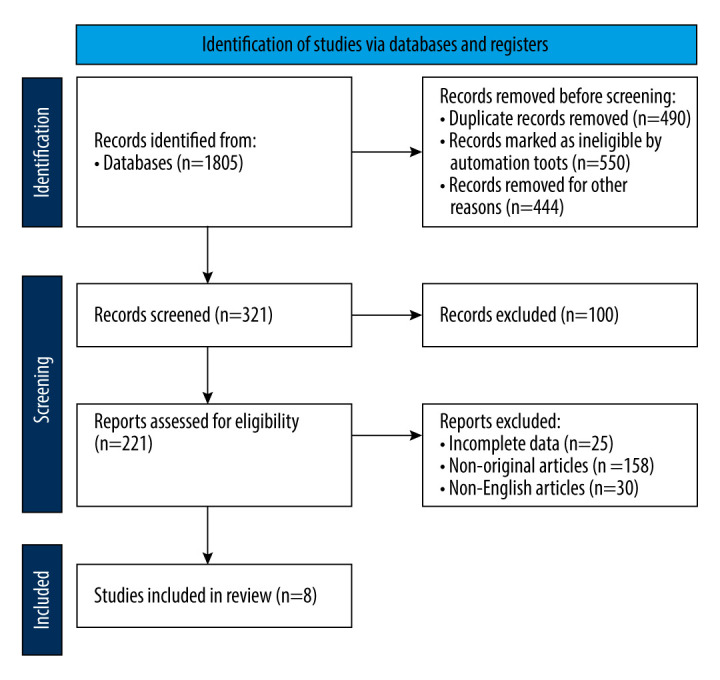
Flowchart demonstrating the identification, screening, and selection of the included studies in this systematic review.
Data Review and Analysis
Using a specially created Excel sheet, a preliminary assessment was conducted to identify the data of relevance for data extraction. After selected data from eligible articles were edited using the Excel sheet, they were moved to a table that had already been prepared for summarization.
Results
Study Selection
This systematic review included 8 studies that met the eligible criteria [24–31] (Table 1). Three studies did not report the study design [25,30,31]; the remaining 5 studies were a prospective randomized trial [24], randomized controlled trials [26,27], longitudinal, observational, and retrospective trial [28], and retrospective review [29]. Four studies [28–31] assessed ABR alone to assess the outcomes and risk factors of recurrence of the procedure [28], assess outcomes, including recurrence among female patients [29], assess the clinical outcomes of 2 types of sutures [30], and assess recurrence rate and risk factors [31], respectively. The remaining 4 studies involved ABR and other interventions [24–27]. The first study compared ABR and open Latarjet [24], the second study compared ABR with and without concomitant remplissage [25], the third study compared ABR and immobilization [26], and the last study compared ABR and immobilization in 60° of external rotation and 30° of abduction [27].
Table 1.
Summary of the included studies, describing authors, publication year, study design, technique, characteristics of the patients, results and main findings.
| Author and publication year | Study design | Techniques/ aim | Characteristics of patients | Results and main findings |
|---|---|---|---|---|
| Genena et al, 2023 [24] | Prospective randomized trial |
|
|
|
| Paul et al, 2023 [25] | ------ |
|
|
|
| Pouges et al, 2021 [26] | Randomized controlled trial |
|
|
|
| Minkus et al, 2021 [27] | Randomized controlled trial |
|
|
|
| Garcia-Vega et al, 2021 [28] | Longitudinal, observational and retrospective |
|
|
|
| Moore et al, 2020 [29] | Retrospective review |
|
|
|
| Arican & Turhan 2019 [30] | ------ |
|
|
|
| Alkhathami et al, 2018 [31] | ------- |
|
|
|
ABR – arthroscopic Bankart repair; F/U – follow-up; ER – external rotation; ABD – abduction; OR – odds ratio; ASES – American Shoulder and Elbow Surgeons.
Study Characteristics
A total of 398 patients were included in the 8 studies. One study included 30 male patients [24], and another study included 31 female patients [29]. The remaining 6 studies included male and female patients. Three studies involved 1 group of patients [28,29,31], whereas the remaining 5 studies included 2 groups of patients for comparison [24–27,30].
One study enrolled patients with traumatic anterior shoulder instability with minimal glenoid bone loss [24], and another 2 studies enrolled patients with traumatic anterior shoulder instability [30,31]. Three studies enrolled patients with anterior instability of shoulder joint [25,28,29], and 2 studies included patients with the first incidence of anterior dislocation of the shoulder joint [26,27]. The age of patients ranged from 15 years [31] to 55 years [25,30]. One study did not report the duration of follow-up [31], whereas in the remaining 7 studies, the minimum duration of follow-up was 13.27 months [24], and the maximum duration was 84 months (7 years) [28].
Results of Individual Studies
The studies reported heterogeneous results, due to their differences in objectives and populations. Therefore, the findings of studies that assessed ABR alone are illustrated first, as follows [28–31]. The study conducted on female patients revealed that 82% of patients returned to sport and 58% of them returned to the same or higher level. The rate of complication was low, as the recurrent rate of instability was 8.8%, recurrence of dislocation was experienced by 2.9%, and 5.9% experienced recurrent subluxation [29]. The other study conducted on ABR reported only a low recurrence rate of 9.8%, and the associated factors by multivariate analysis included large Hill-Sachs lesions (OR=6.75) and less than 4 suture anchors (OR=9.45) [31]. One of the other 2 studies assessed ABR with suture with no mention of the suture type. The study showed a low recurrence rate of 9.4%, whereas 54.3% of the patients achieved excellent or good results. A complete range of motion was achieved among 90% of patients, and the complication rate was low among the 4.88% who experienced advanced osteoarthritis [28]. The last study, which compared all-soft suture anchor and conventional metal anchor, showed that both types resulted in comparable clinical and functional results, and both types resulted in significant increases in American Shoulder and Elbow Surgeons (ASES) and Latarjet scores, concomitant remplissage Latarjet scores, and concomitant remplissage scores after ABR. However, no significant differences were found between the 2 types regarding ASES score (P=0.2), Rowe score (P=0.4), the change in ASES% (P=0.4), and the change in Rowe% (P=0.2) [30].
Results of Syntheses
The other 4 studies compared ABR with other interventions [24–27]. One study comparing ABR and Latarjet found that postoperative range of motion and Rowe scores did not differ between the 2 methods, and none of the patients experienced recurrent dislocation. Latarjet was better than ABR regarding significantly lower time to return to sport (5.2 vs 7 months for Latarjet and ABR, respectively), but ABR was better regarding significantly shorter operative time (43.33 vs 72.33 for ABR and Latarjet, respectively). Additionally, open Latarjet is a more invasive and non-anatomical procedure [24]. ABR with and without concomitant remplissage showed similar results; both methods resulted in the same rate of glenoid bone loss (11%), close rate of recurrence of dislocation with no significant difference, and no difference in the rate of return to sport, range of motion, and complications, including subjective instability, reoperation, or revision (all P values were >0.05). The only significance was regarding the engagement of Hill-Sachs lesions, as they were more prevalent among patients who underwent remplissage than in those without remplissage [25]. The remaining 2 studies compared ABR with immobilization. One study reported that ABR resulted in better outcomes regarding a lower rate of recurrence (P=0.0001), fewer episodes of dislocation, lower complications, including subluxation (P=0.003), and a higher rate of return to sport at the same or better level (P=0.012). Additionally, the ABR group showed a higher Walch-Duplay score (P=0.035), with no surgical complications and no significant difference in range of motion [26]. The last study compared ABR with immobilization, but immobilization was in external rotation and abduction. The recurrence rate was lower in the ABR group (P=0.01), with no significant difference in clinical shoulder score (P>0.05) [27].
Discussion
This systematic review was performed to assess the outcomes of ABR compared with those of other interventions, as well as the recurrence rate. We found that ABR resulted in excellent or good results among more than 50% of the patients, a high return rate to sport with the same or higher level, a low rate of recurrence, and low complication rates. Additionally, it was found that both all-soft suture anchor and conventional metal anchors resulted in comparable functional and clinical outcomes.
A previous systematic review of studies with 10 years of follow-up included 9 studies that enrolled 822 shoulders of patients aged between 15 and 73 years. The return to sports after ABR was 77.6% of athletes, and the overall recurrence rate of instability was 31.2%, with 16% of patients having recurrent dislocations, and an overall revision rate of 17%. The authors concluded that ABR for anterior shoulder instability resulted in excellent long-term functional outcomes [21]. In the present systematic review, despite the heterogeneous findings, the return to sport rate was high among patients who underwent ABR regarding the studies assessed ABR only, and the studies compared ABR with other interventions. The rate of return to sport among patients who underwent ABR was 82% [29] and 89% [26]. Additionally, the recurrence rate among patients who underwent ABR in this systematic review was less than that reported in the previous systematic review (31.2%) [21]; the highest recurrence rate found in our analysis regarding ABR was 10% [26], and some studies even did not report any recurrence within the follow-up duration [24].
ABR is the most appropriate intervention in the setting of a simple Bankart lesion without significant glenoid bone loss [32]. However, one study in our analysis reported patients with instability and minimal glenoid bone loss. The study reported no recurrence observed with the duration of follow-up and returning to sport and work after 7 months [24].
Latarjet is an intervention that enables restoring anterior stability of shoulder joint by 3 different mechanisms, which is known as the triple effect [33]. Latarjet has been shown to be clinically effective, with a re-dislocation rate of 0.8% at 2 years and satisfaction levels over the long run of up to 98% [34]. In our analysis, only one study compared between Latarjet and ABR, finding that Latarjet was superior to ABR regarding the reduced duration required to return to sport (5.2 months); however, ABR consumed significantly less procedural time and was less invasive than Latarjet [24]. It has been claimed that Latarjet significantly improves patients’ reported outcomes and allows them to resume their sport activities [33].
Nonetheless, considering the high reported rate of complications, it was advised that Latarjet be evaluated against the risks of adverse effects, which reached 25% and incorporated mal positioning, arthrosis, graft fracture, and screw breakage [35]. In the present analysis, no complications were found regarding Latarjet; however, this can be attributed to 2 factors. The first is the short mean duration of follow-up (13.27 months), and the second is that only one study reported the outcomes of Latarjet repair. ABR has several advantages, including providing minimally invasive anatomic reconstruction with low rates of operative complications [21], as well as low or no recurrence rate, as found in our analysis.
A systematic review of a minimum follow-up of 5 years revealed that the rate of re-dislocation for ABR was higher (15.1%) than that of Latarjet repair (2.7%). On the contrary, open Latarjet repair resulted in a significantly higher rate of complications (9.4%) than ABR (0%) (P=0.002). The review did not suggest the superiority of any of the interventions. Additionally, it included studies published earlier, with some from 2000; however, now interventions from that time have been improved [2].
In a previous study of patients aged 12 to 40 years who were treated non-operatively, the patients were followed for 25 years after primary anterior dislocation, and 52% of all patients who participated in sports or leisure activities at any level experienced a recurrence or required surgical stabilization during the research period [36]. In our analysis, immobilization vs ABR resulted in a higher recurrence rate of 70% vs 19.1%, which resulted in a significantly lower recurrence rate of 10% vs 2.3%, respectively [26,27].
A systematic review and meta-analysis by Hu et al compared ABR and conservative treatment for first-traumatic anterior shoulder dislocation and included 12 trials. It was demonstrated that ABR showed superiority over conservative management regarding recurrence, return to play, and subsequent instability surgery [37]. These findings were similar to ours. Although the previous systematic review was published in 2023 and included a larger number of studies [37] than the present systematic review, the present systematic review included more recent studies, published between 2018 and 2023. On the other hand, the previous systematic review included the earliest studies, and one of them was published in 1994 [37], when there was less advancement in technology and management than in the more recent studies.
Another systematic review and meta-analysis included 10 studies with 569 patients and compared ABR and conservative treatment for first-time traumatic anterior shoulder instability. ABR resulted in a lower rate of recurrent instability and further surgical treatment (P<0.0001), as well as a higher rate of return to play, compared with conservative management [10]. Kavaja et al, in a systematic review with a network meta-analysis including 22 randomized controlled trials, revealed that there was very low-quality evidence suggesting no benefit of immobilization in external rotation vs internal rotation [5]. In our analysis, one study compared immobilization in external rotation and abduction with ABR; however, there was no significant difference between the 2 groups regarding clinical shoulder score, and immobilization resulted in a higher recurrence rate than did ABR [27]. In actuality, the increased risks of recurring instability with nonoperative treatment compared with surgical treatment is what has caused the trend toward operative treatment of first-time shoulder dislocations [38,39].
The identification and determination of risk-related factors are crucial in the management procedures. The patient-specific demographics risk factors, including younger age and male athletes, can increase the patients’ risk of experiencing recurrent instability, indicating that nonoperative treatment might not be the best option for such groups [40]. Unfortunately, we could not determine the risk factors, as there was a lack of such data in the studies included in this systematic review. One study reported that the identification of risk factors was not possible [28]. Only one study reported 2 factors that were determinants for re-dislocation, and they included large Hill-Sachs lesions, which increased the risk by more than 6-fold and the number of suture anchors by less than 4-fold, which increased the probability of recurrence to more than 9-fold [31]. It was reported that the risk of recurrence is high for ABR alone in situations of concomitant bony injury, incorporating large off-track Hill-Sachs injuries and glenoid fracture [33]. In a case series, it was found that there was an 8.3-fold increase in the recurrence rate among patients with off-track Hill-Sachs injuries managed with isolated ABR [41].
It was discovered in a case series that adding remplissage for off-track Hill-Sachs lesions led to a 90% rate of return to activity, with a failure rate of less than 5% after a minimum of 4 years of follow-up [42]. In our analysis, one study compared between ABR with and without remplissage. However, no difference between the 2 interventions was found regarding return to sport, shoulder range of motion, outcomes reported by the patients, and the rate of re-dislocation, revision, reoperation, and subjective instability [25]. In a recent systematic review on treatment of anterior shoulder instability with bone loss, the authors focused on ABR with remplissage compared with bone block augmentation. Bone block augmentation and Bankart repair with remplissage were found to be effective treatments for recurrent anterior shoulder instability in patients with bipolar bone loss but with subcritical glenoid bone loss. Both approaches yielded similar functional outcomes, although bone block procedures had a higher risk of complications [43].
Limitations of the Study and Future Suggestions
There was a lack of data on risk factors in the studies included in this systematic review. Some studies had a relatively short duration of follow-up, which does not capture long-term outcomes accurately. The systematic review included a limited number of 8 studies, which can restrict the generalizability of the findings and the ability to draw strong conclusions. The included studies had different designs, such as prospective randomized trials, retrospective reviews, and observational studies, which could introduce bias and affect the consistency of the results. Some comparisons, such as between ABR and Latarjet, were based on a single study, which may not provide a comprehensive understanding of the comparative effectiveness of different interventions. Hence, we recommend a systematic review of randomized controlled trials that includes a greater number of studies.
Conclusions
ABR was effective in the management of shoulder instability, as it resulted in a lower rate of recurrence, low rate of complications, and high rate of return to sport, regardless of the suture type. ABR was also superior to the conservative method, as it resulted in lower recurrent rare complications, with no surgical complications. Also, combining concomitant remplissage with ABR showed no superior outcomes. Furthermore, when Latarjet was compared with ABR, Latarjet was superior regarding a reduced time to return to sport, whereas ABR was better regarding a shorter operative time. A shorter operative time is necessary, as a long operative time carries an increased risk of the patient getting infection. The current evidence for the effectiveness and superiority of ABR is weak, due to variations in results. Although the studies reported the superiority of ABR compared with conventional immobilization and other interventions, such as Latarjet and combined concomitant remplissage, there is a lack of recent studies performing such comparisons, and strong evidence will require the analysis of more studies without such heterogeneous variations in study design and other variables.
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Department and Institution Where Work Was Done: Department of Medical Rehabilitation Sciences, King Khalid University, Abha, Saudi Arabia.
Declaration of Figures’ Authenticity: All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
Data Availability Statement
Data are available from the corresponding author mentioned in this research paper.
References
- 1.Adam M, Attia AK, Alhammoud A, et al. Arthroscopic Bankart repair for the acute anterior shoulder dislocation: Systematic review and meta-analysis. Int Orthop. 2018;42(10):2413–22. doi: 10.1007/s00264-018-4046-0. [DOI] [PubMed] [Google Scholar]
- 2.Rollick NC, Ono Y, Kurji HM, et al. Long-term outcomes of the Bankart and Latarjet repairs: A systematic review. Open Access J Sports Med. 2017;8:97–105. doi: 10.2147/OAJSM.S106983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: Long-term evaluation. Arthroscopy. 2005;21(1):55–63. doi: 10.1016/j.arthro.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 4.Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: Long-term evaluation. Arthroscopy. 2005;21(1):55–63. doi: 10.1016/j.arthro.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 5.Kavaja L, Lähdeoja T, Malmivaara A, Paavola M. Treatment after traumatic shoulder dislocation: A systematic review with a network meta-analysis. Br J Sports Med. 2018;52(23):1498–506. doi: 10.1136/bjsports-2017-098539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang NP, Chen HC, Phan DV, et al. Epidemiological survey of orthopedic joint dislocations based on nationwide insurance data in Taiwan, 2000–2005. BMC Musculoskelet Disord. 2011;12:253. doi: 10.1186/1471-2474-12-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fabbriciani C, Milano G, Demontis A, et al. Arthroscopic versus open treatment of Bankart lesion of the shoulder: A prospective randomized study. Arthroscopy. 2004;20(5):456–62. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Waterman B, Owens BD, Tokish JM. Anterior shoulder instability in the military athlete. Sports Health. 2016;8(6):514–19. doi: 10.1177/1941738116672161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Owens BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35(7):1168–73. doi: 10.1177/0363546506295179. [DOI] [PubMed] [Google Scholar]
- 10.Hurley ET, Manjunath AK, Bloom DA, et al. Arthroscopic Bankart repair versus conservative management for first-time traumatic anterior shoulder instability: A systematic review and meta-analysis. Arthroscopy. 2020;36(9):2526–32. doi: 10.1016/j.arthro.2020.04.046. [DOI] [PubMed] [Google Scholar]
- 11.Yoshida M, Takenaga T, Chan CK, et al. Location and magnitude of capsular injuries varies following multiple anterior dislocations of the shoulder: Implications for surgical repair. J Orthop Res. 2021;39(3):648–56. doi: 10.1002/jor.24860. [DOI] [PubMed] [Google Scholar]
- 12.Yoshida M, Takenaga T, Chan CK, et al. Altered shoulder kinematics using a new model for multiple dislocations-induced Bankart lesions. Clin Biomech (Bristol, Avon) 2019;70:131–36. doi: 10.1016/j.clinbiomech.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 13.Buss DD, Lynch GP, Meyer CP, et al. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32(6):1430–33. doi: 10.1177/0363546503262069. [Erratum in: Am J Sports Med. 2004;32(7):1780] [DOI] [PubMed] [Google Scholar]
- 14.Vaswani R, Gasbarro G, Como C, et al. Labral morphology and number of preoperative dislocations are associated with recurrent instability after arthroscopic Bankart repair. Arthroscopy. 2020;36(4):993–99. doi: 10.1016/j.arthro.2019.11.111. [DOI] [PubMed] [Google Scholar]
- 15.Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy. 2007;23(9):985–90. doi: 10.1016/j.arthro.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 16.White AE, Patel NK, Hadley CJ, Dodson CC. An algorithmic approach to the management of shoulder instability. J Am Acad Orthop Surg Glob Res Rev. 2019;3(12):e19.00168. doi: 10.5435/JAAOSGlobal-D-19-00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neviaser RJ, Benke MT, Neviaser AS. Mid-term to long-term outcome of the open Bankart repair for recurrent traumatic anterior dislocation of the shoulder. J Shoulder Elbow Surg. 2017;26(11):1943–47. doi: 10.1016/j.jse.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 18.Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in american football players. J Bone Joint Surg Am. 2002;84(5):711–15. doi: 10.2106/00004623-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 19.van der Linde JA, van Kampen DA, Terwee CB, et al. Long-term results after arthroscopic shoulder stabilization using suture anchors: An 8- to 10-year follow-up. Am J Sports Med. 2011;39(11):2396–403. doi: 10.1177/0363546511415657. [DOI] [PubMed] [Google Scholar]
- 20.Castagna A, Garofalo R, Conti M, Flanagin B. Arthroscopic Bankart repair: Have we finally reached a gold standard? Knee Surg Sports Traumatol Arthrosc. 2016;24(2):398–405. doi: 10.1007/s00167-015-3952-6. [DOI] [PubMed] [Google Scholar]
- 21.Murphy AI, Hurley ET, Hurley DJ, et al. Long-term outcomes of the arthroscopic Bankart repair: A systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg. 2019;28(11):2084–89. doi: 10.1016/j.jse.2019.04.057. [DOI] [PubMed] [Google Scholar]
- 22.Boileau P, Villalba M, Héry JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–63. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 23.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Genena A, Hashem M, Waly A, Hegazy MO. Open latarjet versus arthroscopic Bankart repair for the treatment of traumatic anterior shoulder instability in high-demand patients with minimal glenoid bone loss. Cureus. 2023;15(4):e37127. doi: 10.7759/cureus.37127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paul RW, Reddy MP, Onor G, et al. Bankart repair with or without concomitant remplissage results in similar shoulder motion and postoperative outcomes in the treatment of shoulder instability. Arthrosc Sports Med Rehabil. 2022;5(1):e171–e78. doi: 10.1016/j.asmr.2022.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pougès C, Hardy A, Vervoort T, et al. Arthroscopic Bankart repair versus immobilization for first episode of anterior shoulder dislocation before the age of 25: A randomized controlled trial. Am J Sports Med. 2021;49(5):1166–74. doi: 10.1177/0363546521996381. [DOI] [PubMed] [Google Scholar]
- 27.Minkus M, Königshausen M, Pauly S, et al. Immobilization in external rotation and abduction versus arthroscopic stabilization after first-time anterior shoulder dislocation: A multicenter randomized controlled trial. Am J Sports Med. 2021;49(4):857–65. doi: 10.1177/0363546520987823. [Erratum in: Am J Sports Med. 2022;50(11): NP45] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.García-Vega M, De La Cuadra-Virgil P, Jiménez-Cristobal J, et al. Arthroscopic Bankart repair for the management of anterior shoulder instability: mid-and long-term results. Revista Española de Cirugía Ortopédica y Traumatología (English Edition) 2021;65(4):255–63. [Google Scholar]
- 29.Moore TK, Hurley ET, Rowe DN, et al. Outcomes following arthroscopic Bankart repair in female patients. J Shoulder Elbow Surg. 2020;29(7):1332–36. doi: 10.1016/j.jse.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 30.Arican M, Turhan Y. [Comparison of clinical and functional results after arthroscopic Bankart repair with the all-soft suture anchor and the conventional metal anchor]. Düzce Üniversitesi Sağlık Bilimleri Enstitüsü Dergisi. 2019;9(3):139–44. [in Turkish] [Google Scholar]
- 31.Alkhathami MS, AL-Ahdal AA, Alomari MA, et al. Bankart Repair in Traumatic Anterior Shoulder Instability. Egypt J Hosp Med. 2018 Jan 1;70(4):549–53. [Google Scholar]
- 32.DeFroda S, Bokshan S, Stern E, et al. Arthroscopic Bankart repair for the management of anterior shoulder instability: indications and outcomes. Curr Rev Musculoskelet Med. 2017;10(4):442–51. doi: 10.1007/s12178-017-9435-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nazzal EM, Herman ZJ, Engler ID, et al. First-time traumatic anterior shoulder dislocation: current concepts. J ISAKOS. 2023;8(2):101–7. doi: 10.1016/j.jisako.2023.01.002. [DOI] [PubMed] [Google Scholar]
- 34.Hovelius L, Sandström B, Sundgren K, Saebö M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: Study I – clinical results. J Shoulder Elbow Surg. 2004;13(5):509–16. doi: 10.1016/j.jse.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 35.Shah AA, Butler RB, Romanowski J, et al. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94(6):495–501. doi: 10.2106/JBJS.J.01830. [DOI] [PubMed] [Google Scholar]
- 36.Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am. 2008;90(5):945–52. doi: 10.2106/JBJS.G.00070. [DOI] [PubMed] [Google Scholar]
- 37.Hu B, Hong J, Zhu H, et al. Arthroscopic Bankart repair versus conservative treatment for first-time traumatic anterior shoulder dislocation: A systematic review and meta-analysis. Eur J Med Res. 2023;28(1):260. doi: 10.1186/s40001-023-01160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buss DD, Lynch GP, Meyer CP, et al. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32(6):1430–43. doi: 10.1177/0363546503262069. [Erratum in: Am J Sports Med. 2004;32(7):1780] [DOI] [PubMed] [Google Scholar]
- 39.Dickens JF, Rue JP, Cameron KL, et al. Successful return to sport after arthroscopic shoulder stabilization versus nonoperative management in contact athletes with anterior shoulder instability: A prospective multicenter study. Am J Sports Med. 2017;45(11):2540–46. doi: 10.1177/0363546517712505. [DOI] [PubMed] [Google Scholar]
- 40.Hurley ET, Matache BA, Wong I, et al. Anterior Shoulder Instability International Consensus Group. Anterior shoulder instability part I – diagnosis, nonoperative management, and Bankart repair – an international consensus statement. Arthroscopy. 2022;38(2):214–223e7. doi: 10.1016/j.arthro.2021.07.022. [DOI] [PubMed] [Google Scholar]
- 41.Locher J, Wilken F, Beitzel K, et al. Hill-Sachs off-track lesions as risk factor for recurrence of instability after arthroscopic Bankart repair. Arthroscopy. 2016;32(10):1993–99. doi: 10.1016/j.arthro.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 42.Scanaliato JP, Dunn JC, Fitzpatrick KV, et al. Double-Pulley remplissage in active-duty military population with off-track anterior shoulder instability results in improved outcomes and low recurrence at minimum 4-year follow-up. Arthroscopy. 2022;38(3):743–49. doi: 10.1016/j.arthro.2021.09.003. [DOI] [PubMed] [Google Scholar]
- 43.Gouveia K, Abidi SK, Shamshoon S, et al. Arthroscopic Bankart repair with remplissage in comparison to bone block augmentation for anterior shoulder instability with bipolar bone loss: A systematic review. Arthroscopy. 2021;37(2):706–17. doi: 10.1016/j.arthro.2020.08.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author mentioned in this research paper.


