Abstract
Prospective university students experience substantial academic stressors and psychological vulnerabilities, yet their mental health literacy (MHL) remains inadequately explored. This study investigates four dimensions of MHL – help-seeking behaviors, stigma, knowledge about mental health and understanding of mental illnesses. Besides, Geographic Information System (GIS) techniques are employed to analyze spatial disparities in MHL, which is the first in the context of MHL research. A total of 1,485 students were assessed for sociodemographic characteristics, admission-related variables, health behaviors and family histories of mental health issues. Data were analyzed using SPSS and ArcGIS software. Multivariable linear regression analyses unveiled predictors of the MHL dimensions, with gender, family income, admission test performance, smoking, alcohol and drug use, physical and mental health history, current depression or anxiety and family history of mental health and suicide incidents emerging as common predictors. GIS analysis unraveled notable regional disparities in MHL, particularly in knowledge of mental health and mental illness, with northern and some southern districts displaying higher literacy levels. In conclusion, these findings accentuate significant gender and sociodemographic inequalities in MHL among prospective university students, highlighting the imperative for targeted interventions to enhance MHL and foster mental well-being in this cohort.
Keywords: mental health literacy, stigma, help-seeking, mental illness, students, spatial analysis
Impact statement
The findings of this study have far-reaching implications for various stakeholders, including policymakers, educators, mental health practitioners and the public. By exploring the mental health literacy levels among prospective university students, it highlights the urgent need for targeted interventions to address gaps in knowledge and attitudes mental health. Locally, this study provides valuable insights for university administrators and counselors to develop tailored mental health literacy programs to better support students’ well-being during their transition to higher education. Understanding the predictors of mental health literacy, allows institutions to implement targeted interventions to enhance help-seeking behaviors, reduce stigma and improve knowledge about mental health and illness. Regionally, the findings can inform public health policies aimed at promoting mental health literacy among young adults, not only within educational settings but also in community-initiatives. Addressing disparities in mental health literacy across regions, helps policymakers allocate resources more effectively to reach underserved populations and reduce the burden of mental health issues. Internationally, this study contributes to the growing body of evidence highlighting mental health literacy as a global public health priority. Emphasizing sociodemographic factors, lifestyle choices and regional disparities, this study adds nuance to understanding cultural, social and economic factors shape perceptions and behaviors related to mental health. Overall, the findings emphasize the importance of mental health literacy in promoting mental well-being and reducing the stigma. By raising awareness and fostering a better understanding of mental health issues among prospective university students and beyond, this study can contribute to positive societal change and improve outcomes for individuals facing mental health challenges.
Introduction
Mental health literacy (MHL) has emerged as a crucial component in addressing the global burden of mental health disorders, facilitating early intervention and promoting well-being among diverse populations. Extensive research has underscored the multifaceted nature of MHL, encompassing individuals’ knowledge, attitudes and behaviors related to mental health issues. A seminal framework proposed by Jorm et al. (1997a) delineated four key dimensions of MHL: recognition of mental disorders, knowledge of risk factors and causes, understanding of self-help interventions and knowledge of professional help-seeking (HS) avenues. Subsequent studies have further refined this framework, emphasizing additional aspects such as stigma (ST) reduction and promotion of positive mental health practices (Jorm et al., 1997b; Kutcher et al., 2015).
Adolescent MHL has garnered increasing attention as a crucial determinant of mental health outcomes and HS behaviors. Adolescence represents a critical developmental period characterized by rapid physical, cognitive and socioemotional changes, during which individuals navigate various challenges that can significantly impact their mental well-being. Studies focusing on adolescent MHL have illuminated the complex interplay between knowledge, attitudes and behaviors related to mental health issues (Rickwood et al., 2005; Wei et al., 2013). For instance, Rickwood et al. (2005) emphasized the importance of addressing MHL deficits among adolescents, highlighting the potential of targeted interventions to improve HS behaviors and reduce ST. Subsequent research has expanded upon this foundation, exploring various dimensions of adolescent MHL across diverse cultural contexts and demographic groups.
Recognition of mental disorders is a fundamental aspect of adolescent MHL. Studies have documented adolescents’ ability to identify symptoms of common mental health disorders such as depression, anxiety and substance abuse, underscoring the importance of early detection and intervention (Gulliver et al., 2010). The influence of sociocultural factors, peer relationships and media portrayals on adolescents’ perceptions of mental health issues is also considerable (Lee et al., 2023). Knowledge of effective coping strategies and HS behaviors is another key component of adolescent MHL. Adolescents who possess greater knowledge of mental health resources and support services are more likely to seek help when experiencing emotional distress or mental health challenges (O’Neill et al., 2023). However, barriers such as ST, lack of awareness and doubts about the effectiveness of available services impede HS efforts, while positive past experiences and encouragement from peers and caregivers facilitate the process, highlighting the necessity for targeted and tailored interventions to overcome these challenges among youths (Gulliver et al., 2010).
Studies on adolescent MHL have been conducted across diverse demographic groups of secondary school students, college students and young adults in various geographic regions, providing valuable insights into the factors influencing mental health outcomes and HS behaviors among young people. For instance, Sokolová (2024) examined MHL and HS behavior among secondary school students in Slovakia. Similarly, Al-Shannaq et al. (2023) investigated MHL among high school and university students in Jordan, revealing high levels of depression ST, low depression literacy and negative attitudes toward seeking psychological help. Goodfellow et al. (2023) identified distinct dimensions of MHL in Scotland, with knowledge of treatment efficacy positively associated with seeking formal and informal help from adolescents. In an Indian study, only one-fifth of adolescents correctly identified depression and anxiety vignettes, with prevalent stigmatizing attitudes toward these conditions (Ahmad et al., 2022). While Singh et al. (2022) found that being female, older, nonsmoking, non-alcohol-consuming and not feeling lonely were associated wsith adequate MHL among Malaysian high school students. Media exposure and familiarity were crucial factors influencing mental health knowledge and attitudes among Malaysian secondary school students as reported in another study (Lee et al., 2023). Besides, a study in Turkey found that age, gender and grade explained a 5.5% of the variance in MHL (Özbıçakçı and Salkim, 2024). In a Chinese population-based study, moderate to severe depression was associated with inadequate MHL (Lam, 2014), whereas investigating the relationship between physical literacy, mental health and resilience in Chinese college students, suggested that physical literacy enhances mental health through improved resilience (Ma et al., 2021). These studies collectively emphasize the multidimensional nature of adolescent mental health outcomes and highlight the importance of addressing MHL across diverse populations.
Among the demographic cohorts under scrutiny, prospective university students represent a population characterized by unique stressors and vulnerabilities. The transition from secondary to tertiary education often coincides with heightened academic pressures, social adjustments and concerns about future prospects, contributing to increased susceptibility to mental health challenges (Stallman, 2010). Studies conducted among university entrance test-taking students have highlighted their vulnerability to mental health problems. For instance, half of them were found to be suffering from depression and burnout, while 28.9% reported anxiety, and 17.7% had suicidal thoughts (Mamun et al., 2022). Consequently, understanding the MHL profile of this cohort assumes paramount significance in developing targeted interventions and support mechanisms. However, there is a notable gap in understanding MHL within this demographic, with only a small study assessing depression literacy (Bhuiyan et al., 2020), thus highlighting the need for further investigation, which this study aims to address.
Building upon this foundational knowledge, the present study aims to expand the discourse on MHL among prospective university students. Utilizing the Universal MHL Scale for Adolescents (UMHL-A), this comprehensive research assesses four distinct dimensions of MHL: HS behaviors, ST reduction, KMH and knowledge about mental illnesses (KMI). Besides, the study employs Geographic Information System (GIS) techniques to offer a novel perspective on MHL through spatial visualization across the country. The use of GIS is particularly paramount as it enables the identification of geographical disparities in MHL, allowing for more targeted and localized interventions. GIS mapping provides a visual representation of MHL distribution, highlighting areas with lower literacy levels that may require more focused public health efforts. This approach not only adds depth to the existing literature on MHL but also serves as a valuable tool for policymakers aiming to design and implement nationwide health literacy programs effectively. By synthesizing empirical evidence with advanced methodologies, this study sets the stage for exploring MHL among prospective university students, thereby promoting mental health awareness, resilience and support within educational contexts and broader society.
Methods
Study participants and procedure
This cross-sectional study targeted prospective university students preparing for entrance tests at Jahangirnagar University, located in Dhaka, Bangladesh. Data collection coincided with the entrance test period, spanning from February 22 to 29, 2024. Participants were recruited from university dormitories during this timeframe. The inclusion criteria for participation in this study were as follows: (1) prospective university students aged 18–20 years, (2) attending entrance tests at Jahangirnagar University, (3) residing in university dormitories during the data collection period and (4) able to provide informed consent. Individuals were excluded if they (1) were not present in the dormitory during the survey period or (2) provided incomplete responses to the survey. However, utilizing a convenience survey approach, all eligible participants residing in designated dormitory rooms were approached and invited to participate. Prior to survey administration, participants received comprehensive information about the study’s objectives, procedures, and their rights, ensuring informed consent. Initially, 1,509 responses were obtained, with data from 1,485 participants considered complete for analysis after excluding incomplete questionnaires.
Measures
Sociodemographic factors
The survey collected sociodemographic information including gender, residence location (urban or rural), monthly family income and religious affiliation. Socioeconomic status was categorized based on monthly family income into lower class (earning <15,000 Bangladeshi Taka [BDT]), middle class (earning between 15,000 and 30,000 BDT) and upper class (earning >30,000 BDT).
Health and behavioral variables
Participants were queried about their engagement with smoking, drug and alcohol use, as well as their history of mental health challenges and physical health. They also reported any instances of personal mental health problems, suicide attempts or occurrences of suicide within their family circle, with responses recorded as ’yes’ or ’no’.
Admission-related variables
Information regarding students’ admission journey encompassed test-taking status (first-time or repeat test-takers), educational background, Grade Point Average (GPA), involvement of professional guidance or coaching centers in preparation, performance in mock tests, monthly expenditure related to preparation and program preference for admission.
Mental health problems
To evaluate mental health conditions, the Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001) and the Generalized Anxiety Disorder (GAD-7) (Spitzer et al., 2006) were utilized to assess depression and anxiety, respectively. Besides, participants self-rated their experience of suicidal thoughts with a response of Yes/No (Mamun et al., 2022; Turecki and Brent, 2016). Ratings were based on experiences over the past 2 weeks for depression and anxiety, while suicidal thoughts were assessed over the past year. A cutoff score of 10 or higher on both the PHQ-9 and GAD-7 scales was used to identify depression and anxiety, respectively. The internal consistency of the PHQ-9 and GAD-7 was measured using Cronbach’s alpha coefficient as follows 0.875 and 0.890.
Mental health literacy
The UMHL-A is a comprehensive tool designed to evaluate MHL among children and young adolescents (Kågström et al., 2023). It comprises four distinct domains: HS, ST, KMH and KMI. The HS and ST dimensions are assessed using a 5-point Likert scale, including an additional ’do not know’ option, while the KMH and KMI dimensions employ a True and False scale, also with an extra ’do not know’ option. The UMHL-A Likert scale is coded as follows: Strongly disagree (1), Disagree (2), Neither agree nor disagree (3), Agree (4), Strongly agree (5) and I do not know (3). Conversely, the UMHL-A True and False scale is coded as: Yes (1), I do not know (0) and No (0). The score ranges vary for each dimension: HS scores range between 5 and 25, ST scores range between 3 and 15, KMH scores range between 0 and 5 and KMI scores range between 0 and 4. Higher scores indicate more positive attitudes or greater knowledge about the respective dimensions. The internal consistency of the domains was as follows: 0.786 for HS, 0.710 for ST, 0.748 for KMH and 0.736 for KMI, and 0.843 for overall scale.
Statistical analysis
Data collection for this study was conducted through Google Forms, followed by formatting for analysis in SPSS. Descriptive statistics, including frequency, percentage, mean and standard deviation, were utilized alongside inferential statistics such as the independent t test, ANOVA and linear regression to examine associations between variables and MHL subdivisions. ArcGIS 10.8 software facilitated spatial analysis of MHL subdivisions, presenting participant data geographically by district. Maps were generated using freely accessible government mapping sites. A significance level of p < 0.05 and a standard 95% confidence interval were applied to all statistical tests.
Results
Description of the study participants
Table 1 presents the characteristics of the study participants. A total of 1,485 university test-taking students took part in the study, comprising 54.3% males and 45.7% females. The majority of participants hailed from rural areas (62.1%), identified as Muslim (74.8%) and belonged to nuclear families (72.9%). Moreover, over half of the participants (53.1%) reported a monthly family income exceeding 30,000 BDT. In terms of admission-related variables, 53.8% of participants were fresher test-takers, while 65.4% had achieved a high Secondary School Certificate (SSC) GPA of 5. Participation in coaching from professional coaching centers was prevalent, with 72.1% of students reporting such involvement. Besides, 71.1% of the participants expressed a desire to gain admission to university departments. A considerable portion of the sample reported not engaging in unhealthy lifestyle behaviors such as smoking cigarettes (79.2%), using drugs (89.9%), or consuming alcohol (90.1%). However, a notable proportion reported experiencing mental health issues, with 21.1% reporting a history of mental health problems and 51.9% indicating experiences of depression. A large percentage reported familial challenges, including histories of mental health issues (11.8%) and suicide abttemptsb (12.1%) (Table 1).
Table 1.
Associations of the studied variables with dimensions of mental health literacy
| Variables | Total sample | Mental health literacy | |||
|---|---|---|---|---|---|
| n; (%) | MHL-HS | MHL-ST | MHL-KMH | MHL-KMI | |
| Sociodemographic variables | |||||
| Gender | |||||
| Male | 867; 58.4% | 16.93 ± 3.90 | 10.94 ± 2.40 a | 3.61 ± 1.60 a | 3.09 ± 1.30 c |
| Female | 618; 41.6% | 16.24 ± 3.90 | 10.63 ± 2.50 | 3.38 ± 1.70 | 2.75 ± 1.40 |
| Permanent residence | |||||
| Rural | 922; 62.1% | 16.73 ± 3.90 | 10.84 ± 2.50 | 3.55 ± 1.60 | 3.03 ± 1.30 c |
| Urban | 555; 37.4 | 16.53 ± 3.90 | 10.77 ± 2.40 | 3.45 ± 1.63 | 2.81 ± 1.40 |
| Religion | |||||
| Muslim | 1,111; 74.8% | 16.50 ± 3.90 | 10.74 ± 2.43 a | 3.52 ± 1.61 | 2.96 ± 1.30 a |
| Others | 366; 24.6% | 17.16 ± 3.90 | 11.01 ± 2.32 | 3.51 ± 1.61 | 2.93 ± 1.40 |
| Family type | |||||
| Nuclear | 1,083; 72.9% | 16.68 ± 3.91 | 10.83 ± 2.41 | 3.54 ± 1.63 | 2.97 ± 1.30 |
| Joint | 363; 24.4% | 16.63 ± 3.70 | 10.88 ± 2.27 | 3.48 ± 1.53 | 2.96 ± 1.33 |
| Monthly family income (BDT) | |||||
| <15,001 | 194; 13.1% | 16.80 ± 4.32 c | 11.15 ± 2.61 b | 3.55 ± 1.70 c | 3.03 ± 1.40 c |
| 15,001–30,000 | 381; 25.7% | 17.45 ± 3.81 | 11.14 ± 2.32 | 3.85 ± 1.51 | 3.23 ± 1.14 |
| >30,000 | 789; 53.1% | 16.40 ± 3.70 | 10.66 ± 2.30 | 3.39 ± 1.61 | 2.85 ± 1.32 |
| Admission-related variables | |||||
| Appearance in the admission test | |||||
| Fresher test-takers | 799; 53.8% | 16.77 ± 3.80 | 10.88 ± 2.34 a | 3.57 ± 1.60 | 2.94 ± 1.30 b |
| Repeat test-takers | 686; 46.2% | 16.49 ± 3.40 | 10.73 ± 2.48 | 3.45 ± 1.62 | 2.95 ± 1.37 |
| Secondary School Certificate (SSC) grade point average | |||||
| Poor (<4.51) | 250; 16.8% | 16.07 ± 3.31 b | 10.57 ± 2.10 | 2.99 ± 1.70 c | 2.52 ± 1.40 c |
| Moderate (4.51–4.99) | 236; 15.9% | 17.18 ± 3.90 | 11.04 ± 2.50 | 3.76 ± 1.50 | 3.13 ± 1.30 |
| High (5) | 971; 65.4% | 16.68 ± 3.95 | 10.83 ± 2.42 | 3.60 ± 1.60 | 3.02 ± 1.30 |
| Higher secondary certificate (HSC) grade point average | |||||
| Poor (<4.51) | 236; 15.9% | 15.85 ± 3.75 c | 10.37 ± 2.30 c | 3.06 ± 1.70 c | 2.60 ± 1.42 c |
| Moderate (4.51–4.99) | 315; 21.2% | 17.50 ± 3.33 | 11.23 ± 2.08 | 3.57 ± 1.60 | 3.01 ± 1.20 |
| High (5) | 907; 61.1% | 16.56 ± 4.00 | 10.80 ± 2.48 | 3.63 ± 1.60 | 3.03 ± 1.30 |
| Coached by professional coaching centers | |||||
| Yes | 1,070; 72.1% | 16.72 ± 3.90 | 10.77 ± 2.42 | 3.55 ± 1.60 | 2.94 ± 1.30 |
| No | 399; 26.9% | 16.35 ± 3.90 | 10.87 ± 2.33 | 3.42 ± 1.64 | 3.00 ± 1.34 |
| Desired institute/department for admission | |||||
| Varsity | 1,056; 71.1% | 16.81 ± 3.90 | 10.81 ± 2.44 | 3.53 ± 1.60 a | 3.00 ± 1.30 c |
| Medical | 261; 17.6% | 16.35 ± 3.70 | 10.82 ± 2.30 | 3.36 ± 1.73 | 2.74 ± 1.50 |
| Engineering | 118; 7.9% | 16.19 ± 4.42 | 10.90 ± 2.50 | 3.78 ± 1.50 | 3.13 ± 1.20 |
| Agriculture | 43; 2.9% | 16.16 ± 2.72 | 10.70 ± 1.80 | 3.05 ± 1.63 | 2.40 ± 1.60 |
| Satisfied with previous mock tests | |||||
| No | 756; 50.9% | 16.61 ± 3.70 b | 10.88 ± 2.30 c | 3.52 ± 1.52 c | 3.00 ± 1.30 c |
| Yes | 585; 39.4% | 16.60 ± 4.02 | 10.55 ± 2.52 | 3.40 ± 1.71 | 2.80 ± 1.40 |
| Average monthly expenditure (BDT) | |||||
| >5,000 | 568; 38.2% | 16.86 ± 3.80 c | 10.84 ± 2.35 a | 3.50 ± 1.61 a | 2.93 ± 1.32 c |
| 5,001–10,000 | 550; 37.0% | 17.09 ± 3.90 | 11.10 ± 2.34 | 3.75 ± 1.53 | 3.16 ± 1.17 |
| > 10,000 | 222; 14.9% | 15.67 ± 3.70 | 10.40 ± 2.46 | 3.35 ± 1.61 | 2.71 ± 1.42 |
| Educational background | |||||
| Science | 955; 64.3% | 16.35 ± 4.05 c | 10.64 ± 2.56 c | 3.50 ± 1.62 c | 2.94 ± 1.33 a |
| Arts | 309; 20.8% | 17.23 ± 3.80 | 11.25 ± 2.21 | 3.76 ± 1.50 | 3.13 ± 1.20 |
| Commerce | 217; 14.6% | 17.14 ± 3.16 | 10.93 ± 1.85 | 3.17 ± 1.70 | 2.71 ± 1.35 |
| Health and behavioral variables | |||||
| Cigarette smoking status | |||||
| No | 1,176; 79.2% | 16.89 ± 3.81 | 10.95 ± 2.33 a | 3.58 ± 1.60 | 3.01 ± 1.30 a |
| Yes | 309; 20.8% | 15.70 ± 4.08 | 10.28 ± 2.62 | 3.26 ± 1.70 | 2.70 ± 1.40 |
| Drug usage status | |||||
| No | 1,335; 89.9% | 16.80 ± 3.90 a | 10.92 ± 2.40 | 3.62 ± 1.60 | 3.04 ± 1.30 c |
| Yes | 150; 10.1% | 15.27 ± 3.54 | 9.80 ± 2.50 | 2.60 ± 1.70 | 2.06 ± 1.45 |
| Alcohol usage status | |||||
| No | 1,338; 90.1% | 16.84 ± 3.90 | 10.93 ± 2.40 | 3.61 ± 1.60 b | 3.03 ± 1.30 c |
| Yes | 147; 9.9% | 14.82 ± 3.80 | 9.68 ± 2.53 | 2.66 ± 1.72 | 2.22 ± 1.50 |
| History of mental health problem | |||||
| No | 1,171; 78.9% | 16.96 ± 3.81 | 10.90 ± 2.40 a | 3.56 ± 1.60 | 2.98 ± 1.30 a |
| Yes | 314; 21.1% | 15.42 ± 4.00 | 10.54 ± 2.54 | 3.37 ± 1.63 | 2.81 ± 1.40 |
| History of physical health problem | |||||
| No | 1,167; 78.6% | 16.91 ± 3.80 a | 10.84 ± 2.32 c | 3.53 ± 1.61 | 2.98 ± 1.31 |
| Yes | 314; 21.0% | 15.64 ± 4.14 | 10.68 ± 2.70 | 3.44 ± 1.62 | 2.82 ± 1.34 |
| History of mental health problem in family | |||||
| No | 1,300; 87.5% | 16.84 ± 3.90 a | 10.95 ± 2.40 | 3.61 ± 1.60 a | 3.03 ± 1.30 c |
| Yes | 175; 11.8% | 15.20 ± 3.57 | 9.90 ± 2.50 | 2.82 ± 1.70 | 2.30 ± 1.50 |
| History of suicide attempt in family | |||||
| No | 1,304; 87.8% | 16.90 ± 3.85 | 10.96 ± 2.40 | 3.60 ± 1.60 | 3.03 ± 1.30 b |
| Yes | 179; 12.1% | 14.88 ± 3.85 | 9.70 ± 2.43 | 2.90 ± 1.60 | 2.33 ± 1.40 |
| History of suicide completion in family | |||||
| No | 1,326; 89.3% | 16.91 ± 3.82 | 10.96 ± 2.35 | 3.63 ± 1.60 | 3.05 ± 1.25 c |
| Yes | 153; 10.3% | 14.50 ± 3.63 | 9.62 ± 2.35 | 2.50 ± 1.62 | 2.03 ± 1.50 |
| Depression status | |||||
| No | 715; 48.1% | 16.92 ± 4.30 c | 10.85 ± 2.64 b | 3.89 ± 1.45 c | 3.16 ± 1.20 c |
| Yes | 770; 51.9% | 16.38 ± 3.50 | 10.77 ± 2.20 | 3.16 ± 1.70 | 2.75 ± 1.40 |
| Anxiety status | |||||
| No | 992; 66.8% | 16.76 ± 4.13 c | 10.81 ± 2.53 b | 3.69 ± 1.54 c | 3.05 ± 1.25 c |
| Yes | 493; 33.2% | 16.40 ± 3.40 | 10.81 ± 2.15 | 3.16 ± 1.70 | 2.73 ± 1.43 |
<0.05.
<0.01.
<0.001.
Associations between sociodemographic variables and MHL
Female participants exhibited a nonsignificantly lower mean MHL-HS score of 16.24 (SD = 3.90) compared to males (16.93 ± 3.90). However, significant differences were observed in MHL-ST (t = 5.734, p = 0.017), MHL-KMH (t = 6.401, p = 0.012) and MHL-KMI (t = 34.500, p < 0.001) scores, with females scoring lower. Participants hailing from urban areas reported lower literacy levels of MHL-KMI (2.809 ± 1.389 vs. 3.032 ± 1.263; t = 17.014, p < 0.001). Muslim participants showed slightly lower MHL-ST scores compared to other religious groups, while the opposite trend was observed for MHL-KMI scores. Similarly, participants belonging to income groups other than middle-income families reported significantly higher scores in all dimensions of MHL (Table 1).
Associations between admission-related variables and MHL
Repeat test-takers exhibited marginally significantly lower MHL-ST scores compared to freshers, with the opposite finding observed for MHL-KMI. Participants with moderate results in SSC and HSC consistently reported lower MHL scores across all domains compared to those with lower and higher GPAs. Participants aiming for institutes of study showed comparable MHL scores, albeit with significant variations in MHL-KMH and MHL-KMI scores. Participants who were not satisfied with previous mock tests exhibited slightly significantly lower MHL scores in all dimensions than those who were satisfied. Similarly, participants with an expenditure other than moderate displayed significantly lower scores for all dimensions of MHL compared to other expenditure groups. Students from science backgrounds exhibited lower MHL scores compared to those from arts and commerce backgrounds in MHL-KMH and MHL-KMI (Table 1).
Associations between health and behavioral variables and MHL
Nonsmokers reported significantly higher MHL-ST and MHL-KMI scores compared to their counterparts, whereas it was MHL-HS and MHL-KMI for nondrug users, and MHL-KMH and MHL-KMI for non-alcohol users. Those with a history of psychiatric problems reported lower MHL-ST and MHL-KMI scores compared, while it was MHL-HS and MHL-ST for participants with a history of physical illness. Participants with a history of these issues in their families displayed lower MHL-KMI scores compared to those without such histories, but the family history of mental health problems was significantly associated with MHL-HS and MHL-KMH. Students currently suffering from depression and anxiety reported lower MHL scores across all domains compared to their counterparts (Table 1).
Linear regression analysis of MHL: HS
The final predictive model for MHL related to HS behavior among yielded an adjusted R 2 of 0.103, indicating that approximately 10.3% of the variance in HS attitudes was accounted for by the predictor variables. The overall model was statistically significant, F = 15.088, p < 0.001. Among the predictors, gender (β = −0.125, p < 0.001), religion (β = 0.081, p = 0.005), appearance in the admission test (β = −0.081, p = 0.007), being coached by professional coaching centers (β = −0.072, p = 0.016), alcohol usage status (β = −0.106, p = 0.001), history of physical health problems (β = −0.068, p = 0.038), history of mental health problems (β = −0.080, p = 0.015) and history of suicide completion in the family (β = −0.124, p < 0.001) emerged as significant predictors of MHL-HS (Table 2).
Table 2.
Final predictive models for dimensions of mental health literacy
| Variables | B | S.E. | β | t | p |
|---|---|---|---|---|---|
| MHL: Help-seeking | R 2 = 0.111, adjusted R 2 = 0.103, F = 15.088, p < 0.001; DW value = 1.892 | ||||
| (Constant) | 23.293 | .821 | 28.368 | <.001 | |
| Gender a | −.940 | .217 | −.125 | −4.332 | <.001 |
| Religion b | .693 | .245 | .081 | 2.830 | .005 |
| Appearance in the admission test c | −.602 | .223 | −.081 | −2.697 | .007 |
| Coached by professional coaching centers d | −.655 | .272 | −.072 | −2.409 | .016 |
| Education background e | .254 | .128 | .057 | 1.977 | .048 |
| Alcohol usage status f | −1.351 | .395 | −.106 | −3.424 | .001 |
| History of physical health problem f | −.625 | .302 | −.068 | −2.073 | .038 |
| History of mental health problem f | −.735 | .301 | −.080 | −2.442 | .015 |
| History of suicide completion in family f | −1.491 | .365 | −.124 | −4.084 | <.001 |
| MHL: Stigma | R 2 = 0.069, adjusted R 2 = 0.061, F = 8.968, p < 0.001; DW value = 1.908 | ||||
| (Constant) | 14.090 | .488 | 28.846 | <.001 | |
| Gender a | −.277 | .142 | −.059 | −1.960 | .050 |
| Monthly family income (BDT) g | −.262 | .100 | −.081 | −2.618 | .009 |
| Appearance in the admission test c | −.258 | .136 | −.056 | −1.907 | .057 |
| Average monthly expenditure (BDT) h | .175 | .098 | .055 | 1.787 | .074 |
| Education background e | .168 | .081 | .060 | 2.061 | .040 |
| Drug usage status f | −.576 | .243 | −.076 | −2.368 | .018 |
| History of mental health problem in family f | −.493 | .241 | −.069 | −2.051 | .041 |
| History of suicide attempt in family f | −.443 | .253 | −.063 | −1.752 | .080 |
| History of suicide completion in family f | −.637 | .266 | −.086 | −2.392 | .017 |
| MHL: Knowledge about mental health | R 2 = 0.127, adjusted R 2 = 0.119, F = 15.811, p < 0.001; DW value = 1.911 | ||||
| (Constant) | 6.139 | .355 | 17.270 | <.001 | |
| Monthly family income (BDT) g | −.228 | .067 | −.103 | −3.431 | .001 |
| HSC grade point average b | .179 | .061 | .084 | 2.936 | .003 |
| Coached by professional coaching centers d | −.188 | .112 | −.049 | −1.670 | .095 |
| Average monthly expenditure (BDT) h | .137 | .065 | .062 | 2.100 | .036 |
| Cigarette smoking status f | .245 | .130 | .063 | 1.877 | .061 |
| Drug usage status f | −.380 | .198 | −.073 | −1.922 | .055 |
| Alcohol usage status f | −.442 | .194 | −.081 | −2.273 | .023 |
| History of mental health in family f | −.271 | .158 | −.055 | −1.713 | .087 |
| History of suicide completion in family f | −.697 | .165 | −.136 | −4.209 | <.001 |
| Depression f | −.543 | .093 | −.172 | −5.857 | <.001 |
| MHL: Knowledge about mental illness | R 2 = 0.137, adjusted R 2 = 0.128, F = 15.657, p < 0.001; DW value = 1.964 | ||||
| (Constant) | 4.665 | .321 | 14.531 | <.001 | |
| Gender a | −.290 | .078 | −.110 | −3.703 | <.001 |
| Monthly family income (BDT) g | −.127 | .054 | −.070 | −2.329 | .020 |
| SSC grade point average i | .140 | .053 | .081 | 2.616 | .009 |
| HSC grade point average i | .124 | .055 | .071 | 2.259 | .024 |
| Desired institute/department for admission d | .108 | .061 | .051 | 1.783 | .075 |
| Satisfied with previous mock tests f | −.132 | .076 | −.050 | −1.734 | .083 |
| Average monthly expenditure | .154 | .054 | .085 | 2.843 | .005 |
| Drug usage status f | −.481 | .150 | −.112 | −3.209 | .001 |
| Alcohol usage status f | −.266 | .155 | −.060 | −1.723 | .085 |
| History of suicide completion in family f | −.755 | .130 | −.179 | −5.815 | .000 |
| Depression f | −.174 | .077 | −.068 | −2.280 | .023 |
B: unstandardized regression coefficient; β: standardized regression coefficient.
1 = male, 2 = female.
1 = Muslim, 2 = others.
1 = fresher test-takers, 2 = repeat test-takers.
1 = yes, 2 = no.
1 = science, 2 = commerce, 3 = arts.
1 = no, 2 = yes.
1 = <15,000, 2 = 15,000–30,000, 3 = > 30,000.
1 = <5,000, 2 = 5,000–10,000, 3 = > 10,000.
1 = poor, 2 = moderate, 3 = high.
Linear regression analysis of MHL: ST
The final predictive model for MHL related to ST among university test-taking students showed an adjusted R 2 of 0.061, indicating that approximately 6.1% of the variance in ST-related attitudes was explained by the predictor variables. The overall model was statistically significant, F = 8.968, p < 0.001. Significant predictors of MHL-ST included gender (β = −0.059, p = 0.050), monthly family income (β = −0.081, p = 0.009) and history of suicide completion in the family (β = −0.086, p = 0.017) (Table 2).
Linear regression analysis of MHL: KMH
The final predictive model for MHL related to knowledge of mental health exhibited an adjusted R 2 of 0.119, indicating that approximately 11.9% of the variance in knowledge of mental health was accounted for by the predictor variables. The overall model was statistically significant, F = 15.811, p < 0.001. Notable predictors of MHL-KMH were monthly family income (β = −0.103, p = 0.001), HSC GPA (β = 0.084, p = 0.003), average monthly expenditure (β = 0.062, p = 0.036), cigarette smoking status (β = 0.063, p = 0.061), alcohol usage status (β = −0.081, p = 0.023), history of mental health in the family (β = −0.055, p = 0.087) and history of suicide completion in the family (β = −0.136, p < 0.001) (Table 2).
Linear regression analysis of MHL: KMI
The final predictive model for MHL related to knowledge of mental illness exhibited an adjusted R 2 of 0.128, indicating that approximately 12.8% of the variance in knowledge of mental illness was accounted for by the predictor variables. The overall model was statistically significant, F = 15.657, p < 0.001. Significant predictors of MHL-KMI included gender (β = −0.110, p < 0.001), monthly family income (β = −0.070, p = 0.020), SSC GPA (β = 0.081, p = 0.009), average monthly expenditure (β = 0.085, p = 0.005), drug usage status (β = −0.112, p = 0.001), alcohol usage status (β = −0.060, p = 0.085) and history of suicide completion in the family (β = −0.179, p < 0.001) (Table 2).
MHL across districts
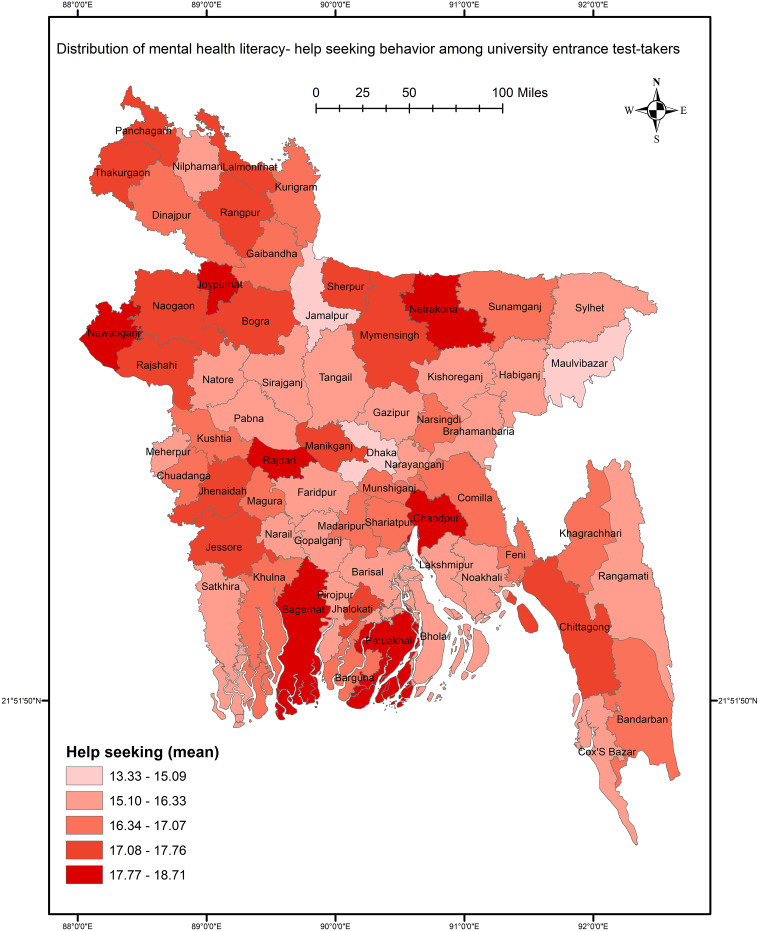
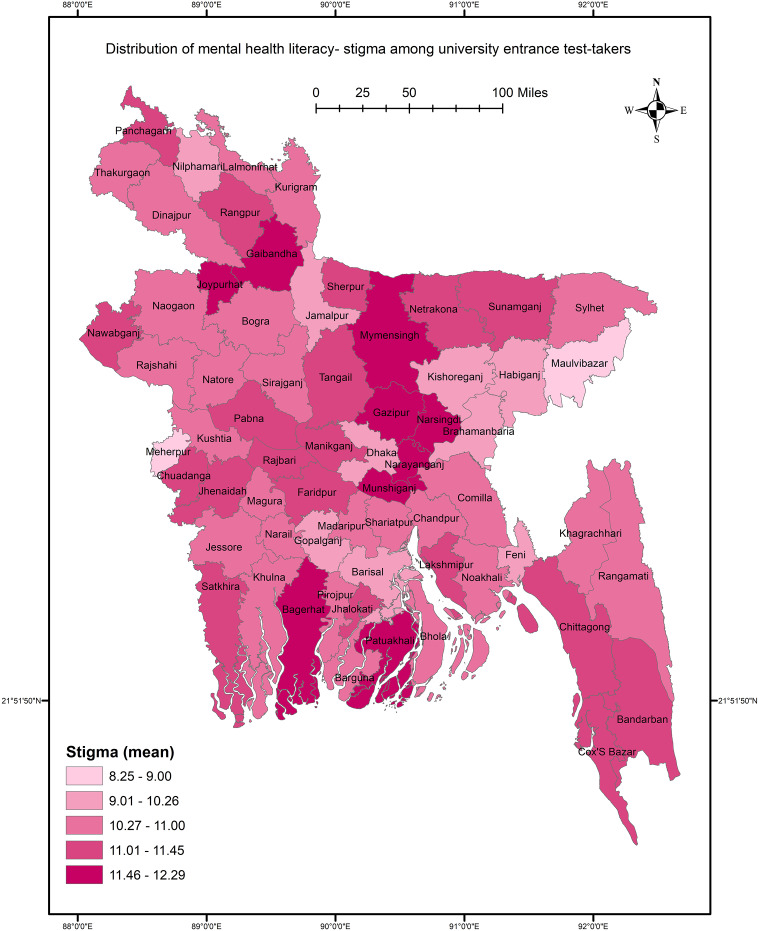
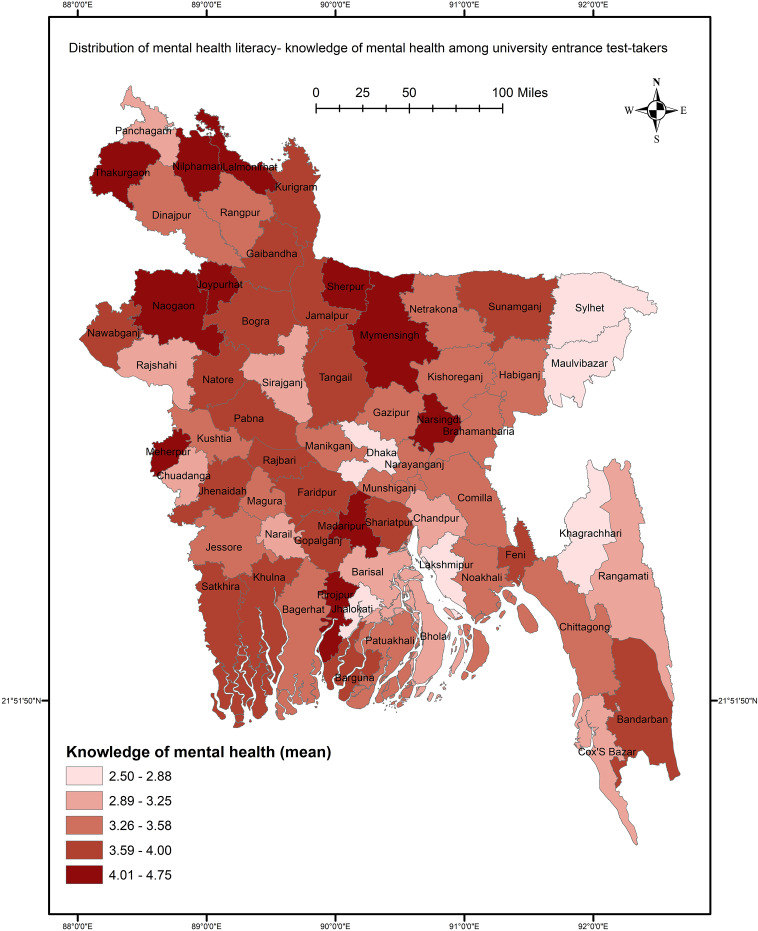
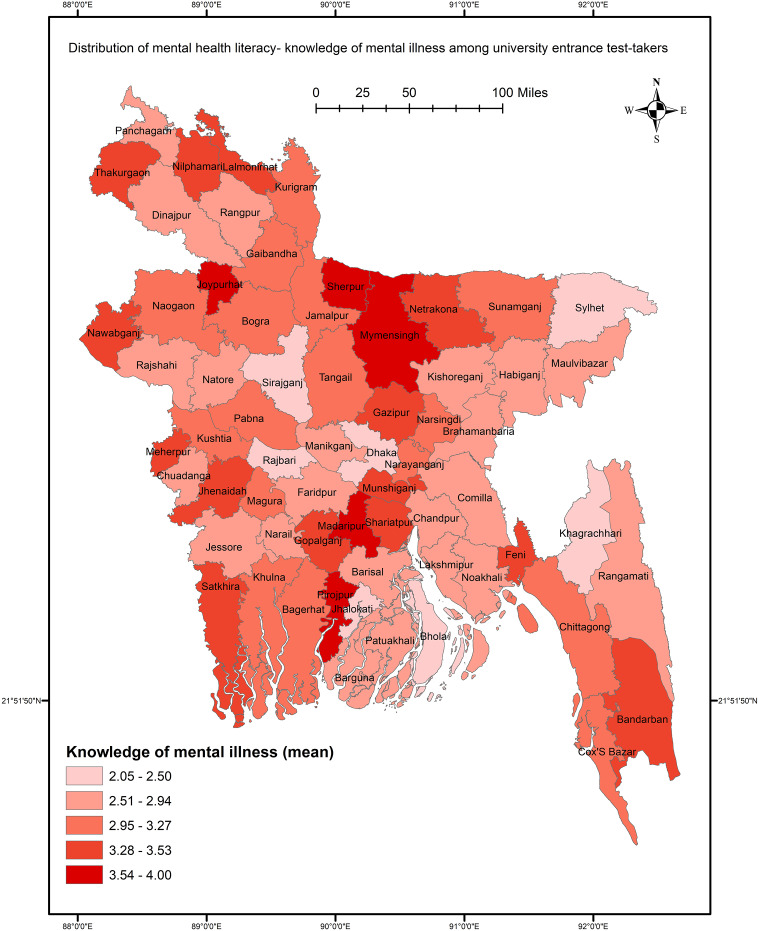
Spatial analysis revealed significant nationwide variations in different dimensions of MHL, particularly in knowledge of mental health and mental illness across districts (F = 1.646, p = 0.001; and F = 2.009, p < 0.001, respectively). However, disparities in the distribution of HS attitudes and ST did not show significant associations with districts. Notably, certain regions exhibited distinct patterns: northern districts like Joypurhat, Chapainawabganj and Rangpur, as well as southern districts like Chandpur, Bagerhat and Patuakhali, demonstrated high levels of HS behavior (Figure 1). Conversely, participants from northern districts such as Gaibandha, Joypurhat and Panchagarh reported positive ST scores (Figure 2). Moreover, mental health knowledge scores were notably elevated in the northern regions compared to other areas (Figure 3). Particularly pronounced knowledge of mental illness was observed among participants from Nilphamari, Thakurgaon, Sherpur and Mymensingh (Figure 4).
Figure 1.
GIS-based distribution of mental health literacy – help-seeking.
Figure 2.
GIS-based distribution of mental health literacy – stigma.
Figure 3.
GIS-based distribution of mental health literacy – knowledge about mental health.
Figure 4.
GIS-based distribution of mental health literacy – knowledge about mental illness.
Discussion
This exploratory study adds to the discourse on MHL among prospective university students by shedding light on the complex associations between sociodemographic, admission-related and health-related variables and literacy levels. The integration of GIS techniques has added a unique dimension to the understanding of MHL by revealing spatial variations across different regions. However, synthesizing the findings with recent literature allows us to offer an updated discussion that reflects the evolving landscape of MHL research and its implications for educational interventions and support services.
The study highlights significant gender disparities in MHL domains, revealing that females tend to exhibit higher levels of ST and lower comprehension of mental health and illness compared to males, despite similar HS attitudes. Evidence from Bangladesh found no significant gender differences in depression literacy conducted among university students (Mamun et al., 2020). It is worth noting that the previous study conducted with prospective university students found that females were more likely to report higher depression literacy (Bhuiyan et al., 2020). Similarly, Malaysian female adolescents were more likely to recognize depression, exhibit adequate MHL and express an intention to seek help compared to their male counterparts (Singh et al., 2022). However, a study involving high school and bachelor’s students in Jordan reported disproportionately higher levels of personal and perceived ST related to depression among female students (Al-Shannaq et al., 2023). These differences may stem from unequal exposure to mental health education and varying access to resources, contributing to females’ relatively lower awareness compared to males. Societal norms and gender expectations can exacerbate ST, hindering open discussions and HS behaviors, while factors like hormonal fluctuations, societal pressures and gender-based violence may increase females’ vulnerability to mental health challenges (Bhatia and Goyal, 2020). Furthermore, global research highlights a higher prevalence of mental health problems among females (Seedat et al., 2009), emphasizing the critical need for targeted interventions to enhance MHL and reduce ST, particularly within educational settings.
The study highlights lower levels of MHL, specifically regarding KMI, among participants from urban areas compared to those from rural areas. This difference may be influenced by distinct cultural norms and attitudes toward mental health in urban settings, potentially shaping how individuals perceive and seek information about mental illness, especially in the technological era (Rickwood et al., 2015). Besides, disparities in access to mental health resources and services between urban and rural areas could contribute to varying levels of MHL. While urban areas typically offer more specialized mental health facilities and resources, challenges such as long wait times and ST associated with seeking help for mental health issues may hinder accessibility and contribute to lower literacy levels. Furthermore, the finding that Muslim participants exhibit positive attitudes toward ST and higher scores in KMI raises questions about the intersection of religious affiliation and MHL. Sometimes religion can provide social support but may also perpetuate ST and misconceptions surrounding mental illness. However, cultural and religious beliefs may shape attitudes toward mental health, influencing HS behaviors and access to services (Rickwood et al., 2015). In addition, socioeconomic disparities were evident in MHL levels, revealing nuanced differences across income brackets. Participants from middle-income families exhibited positive levels of HS behavior and understanding of mental health and illness compared to those from lower-income households. The challenges faced by individuals from lower-income backgrounds, including financial instability, limited access to healthcare services and restricted educational opportunities, contribute to heightened levels of mental health ST. Conversely, higher-income families typically enjoy greater access to educational resources, healthcare services and mental health information, potentially enhancing their MHL levels. However, the observation that participants from high-income families reported lower literacy levels in this study warrants further investigation to uncover underlying factors contributing to this discrepancy.
Lifestyle factors played a crucial role in shaping individuals’ MHL, as evidenced by the significant associations observed in this study. Participants with various lifestyle choices and behaviors, such as smoking, alcohol consumption, drug use and a history of medical conditions, were linked to reporting lower levels of different dimensions of MHL (Singh et al., 2022). This may be attributed to the detrimental effects of smoking on mental health, as research indicates that smoking is not only linked to physical health problems but also contributes to psychological distress and exacerbates symptoms of mental illness (Fluharty et al., 2017). Substance abuse is known to impair cognitive function and judgment, making it more challenging for individuals to comprehend and engage with information about mental health (Al-Shannaq et al., 2023). Engaging in regular exercise and maintaining a balanced diet can enhance cognitive function, reduce stress levels and improve overall well-being, all of which have been linked to improving both physical and mental health outcomes and may contribute to higher levels of MHL (McDowell et al., 2018), which is advised for promoting within the youths. Ma et al. (2021) demonstrated that physical literacy is positively associated with mental health, mediated by resilience, suggesting that holistic approaches to promoting student well-being can have significant benefits. Integrating physical and MHL initiatives within educational settings can enhance resilience and support mental health among students.
The association between family history of mental health problems and MHL is evident in this study, aligning with findings from previous studies (Anbesaw et al., 2024). Individuals with a familial background of mental health issues exhibited lower literacy scores across all dimensions compared to those without such a history. This suggests that individuals with a familial background of mental health problems may have limited exposure to or understanding of mental health concepts, leading to lower levels of MHL. Similarly, the presence of a history of suicide attempts or completions in the family was associated with lower MHL scores across all dimensions. These findings highlight the potential impact of familial experiences on individuals’ attitudes, perceptions and knowledge regarding mental health, highlighting the importance of considering family history in interventions aimed at improving MHL and promoting mental well-being. Further research is needed to explore the mechanisms underlying the link between family history and MHL, to develop targeted interventions for individuals with familial risk factors for mental health issues.
Individuals with a history of psychiatric problems often exhibit lower levels of MHL, particularly concerning ST and understanding mental illness. This highlights the reciprocal relationship between mental health challenges and literacy; those grappling with mental health issues may face obstacles in accessing and comprehending information about their condition (Dardas et al., 2017). This association is notably pronounced for depression and anxiety, as evidenced by previous studies. For instance, Chinese adolescents experiencing moderate to severe depression were found to have a 1.52 times higher risk of poor MHL (Lam, 2014), contrasting with Iranian high school students where no direct relationship between overall health, including psychological aspects, and depression literacy was observed (Bahrami et al., 2019). Individuals with mental health disorders frequently struggle to recognize and comprehend their symptoms, leading to delays in seeking professional help (Gulliver et al., 2010). ST surrounding mental illness compounds these challenges, often dissuading individuals from seeking assistance (Corrigan et al., 2014). Lower MHL scores among those with depression and anxiety underscore the critical need for targeted interventions to enhance literacy and reduce ST. By improving understanding of mental health and fostering HS behaviors, timely access to support services and treatments can be facilitated, ultimately enhancing outcomes for individuals navigating mental health challenges (Rickwood et al., 2005). Furthermore, integrating MHL into educational settings can equip individuals with the knowledge and skills necessary to effectively address mental health issues (Kutcher et al., 2015).
The spatial analysis conducted in this study unveiled significant nationwide variations in different dimensions of MHL, with notable implications for understanding regional disparities and informing targeted interventions. Specifically, the analysis revealed pronounced differences in the levels of knowledge regarding mental health and mental illness across districts, as evidenced by statistically significant findings. Interestingly, while disparities in the distribution of HS attitudes and ST were observed, they did not show significant associations with districts, suggesting that other factors beyond geographic location may influence these aspects of MHL. This insight highlights the complexity of MHL and the need for multifaceted approaches to address it. Thus, further exploration is warranted to elucidate the underlying factors contributing to these disparities and to develop strategies for fostering more uniform attitudes toward seeking mental health support and reducing ST across regions. Notably, certain regions exhibited distinct patterns in terms of HS behavior, ST and mental health knowledge. Northern districts such as Joypurhat, Chapainawabganj and Rangpur, as well as southern districts like Chandpur, Bagerhat and Patuakhali, demonstrated high levels of HS behavior. Conversely, participants from northern districts such as Gaibandha, Joypurhat and Panchagarh reported positive ST scores, indicating a greater prevalence of stigmatizing attitudes toward mental health issues in these areas. Interestingly, mental health knowledge scores were notably elevated in the northern regions compared to other areas, suggesting variations in access to mental health education and resources across different geographical regions. Particularly pronounced knowledge of mental illness was observed among participants from Nilphamari, Thakurgaon, Sherpur and Mymensingh, highlighting potential areas of success in MHL initiatives or indicating specific educational interventions that have been effective in these regions.
The use of GIS in this study is particularly valuable as it goes beyond traditional analyses by providing a visual and spatial representation of MHL levels. This approach not only highlights regional disparities but also offers practical insights for policymakers and mental health professionals. By identifying regions with lower literacy levels, targeted and localized interventions can be designed to address the specific needs of these areas, ultimately leading to more effective MHL programs. However, the spatial disparities observed in this study indicate that MHL is not uniformly distributed across the country, and that interventions need to be tailored to address the unique challenges faced by different regions. Future research could further explore the factors contributing to these geographical disparities, such as access to mental health resources, cultural attitudes and the availability of mental health education, to develop more targeted and effective interventions.
The findings of this study resonate with existing research highlighting the importance of educational interventions in enhancing MHL among students. Interventions aimed at enhancing adolescent literacy have employed various approaches, including school-based programs, online resources and peer-led initiatives. Sokolová (2024) suggested the role of mental health education in secondary schools in promoting MHL and reducing self-stigmatization related to HS behaviors. School-based MHL programs (e.g., Teen Mental Health First Aid) have demonstrated efficacy in improving adolescents’ knowledge of mental health issues, attitudes toward HS and confidence in providing support to peers as found in a randomized control trial (Hart et al., 2018). In a systematic literature review, Liang et al. (2023) demonstrated the effectiveness of mental health first aid programs in increasing students’ knowledge and confidence in supporting adolescents with mental health issues. Similarly, online interventions utilizing interactive platforms and multimedia content have shown promise in engaging adolescents and disseminating mental health information in accessible formats. Despite advancements in adolescent mental literacy research, challenges such as limited access to mental health resources, disparities in service provision and cultural barriers persist (Patel et al., 2018). The evolving landscape of digital technology presents both opportunities and challenges for disseminating mental health information and interventions among adolescents, necessitating ongoing research and adaptation of strategies to suit changing needs and preferences (Rickwood et al., 2015).
Strengths of this study include its comprehensive analysis of MHL among prospective university students, covering various demographic and lifestyle factors that influence literacy levels. By incorporating insights from diverse literature, the discussion enriches the understanding of how factors such as gender, socioeconomic status, lifestyle choices, family history and cultural backgrounds impact MHL. Moreover, the study integrates GIS techniques, providing spatial analysis that elucidates regional variations in MHL, thus offering a nuanced understanding of the geographical distribution of MHL levels among students. This multidimensional approach enhances the credibility and validity of the findings by contextualizing them within geographical landscapes. Additionally, the discussion provides evidence-based insights supported by recent and relevant literature, further bolstering the study’s credibility. Furthermore, the study identifies potential areas for targeted interventions to improve MHL among university students, offering practical implications for educators, policymakers and mental health professionals to develop strategies aimed at reducing ST and promoting MHL in educational settings.
Limitations of the study include its cross-sectional design, which limits the establishment of causality between variables as it captures data at a single point in time. Furthermore, the convenience sampling method used may introduce selection bias, and reliance on self-reported data for variables such as lifestyle choices and family history may lead to response bias and inaccuracies. The findings’ generalizability may be limited to the study’s geographical location and cultural context, and potential confounding variables such as prior exposure to mental health education were not fully accounted for. Addressing these limitations through longitudinal designs, random sampling methods, objective measures and consideration of additional variables can enhance the validity and reliability of future research on MHL among university students.
Conclusions
In conclusion, this study sheds light on the complex interplay of demographic, socioeconomic, lifestyle and cultural factors influencing MHL among prospective university students. Through comprehensive analysis and integration of diverse literature, the study provides valuable insights into the disparities in MHL levels and highlights the need for targeted interventions to reduce ST and enhance literacy, particularly in educational settings. The application of GIS techniques enriches the study by enabling spatial analysis and visualization of regional patterns in MHL, offering valuable guidance for policymakers and healthcare providers. Despite its strengths, the study has limitations that warrant consideration in future research endeavors. Overall, this study contributes to the growing body of knowledge on MHL and highlights the importance of fostering a supportive environment for mental health education and awareness among prospective and general university students.
Acknowledgments
The authors thank all the participants and team members involved in the project. MMA has to acknowledge that the funding support from currently receiving as Princess Nourah Bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R563), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2024.115.
Data availability statement
The datasets will be made available to appropriate academic parties upon request from the corresponding author.
Author contribution
This study was conceptualized by MAM and FAM. The project was implemented and managed, including data collection to data entry, by TI, MKT, MHL, NBM, TBKC and NPS, with direct support from MAM and FAM. It is worth noting that TI, MKT, MHL, NBM, TBKC and NPS were trained in data analysis using the SPSS and were required to submit assignments, which were reviewed and finalized by MAM and FAM. The project was supervised by MMA, ACA, NR, MBH and MSH. The initial draft of this study was written by MAM, whereas subsequent contributions were made by other authors. Extensive edits and reviews were done by all authors in the drafts. MAM addressed the reviewer’s and editor’s comments, and all authors reviewed the final version. All authors have approved the final version.
Financial support
MMA has to acknowledge that the funding support from currently receiving as Princess Nourah Bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R563), Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia.
Competing interest
The authors declare none.
Ethical standard
This study adhered to the Helsinki Declaration of 2013 and obtained ethical approval from the Patuakhali Science and Technology University review board [Ref: PSTU/IEC/2023/85(2)]. Participants provided informed consent and were assured of confidentiality. Their voluntary participation was emphasized, and measures were taken to anonymize data and protect privacy. Participants were informed about support services for mental health concerns and were assured that participation would not affect their academic standing. The study prioritized participant dignity, autonomy and well-being.
References
- Ahmad A, Salve HR, Nongkynrih B, Sagar R and Krishnan A (2022) Mental health literacy among adolescents: Evidence from a community-based study in Delhi. The International Journal of Social Psychiatry 68(4), 791–797. 10.1177/00207640211006155. [DOI] [PubMed] [Google Scholar]
- Al-Shannaq Y, Jaradat D, Ta’an WF and Jaradat D (2023) Depression stigma, depression literacy, and psychological help seeking attitudes among school and university students. Archives of Psychiatric Nursing 46, 98–106. 10.1016/J.APNU.2023.08.010. [DOI] [PubMed] [Google Scholar]
- Anbesaw T, Asmamaw A, Adamu K and Tsegaw M (2024) Mental health literacy and its associated factors among traditional healers toward mental illness in northeast, Ethiopia: A mixed approach study. PLoS One 19(2), e0298406. 10.1371/JOURNAL.PONE.0298406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahrami MA, Bahrami D and Chaman-Ara K (2019) The correlations of mental health literacy with psychological aspects of general health among Iranian female students. International Journal of Mental Health Systems 13(1), 1–7. 10.1186/S13033-019-0315-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia MS and Goyal A (2020) Gender roles in mental health: A stigmatized perspective. In Anand M (ed.), Gender and Mental Health: Combining Theory and Practice. Singapore: Springer, 47–62. 10.1007/978-981-15-5393-6_4. [DOI] [Google Scholar]
- Bhuiyan MAH, Griffiths MD and Mamun MA (2020) Depression literacy among Bangladeshi pre-university students: Differences based on gender, educational attainment, depression, and anxiety. Asian Journal of Psychiatry 50, 101944. 10.1016/j.ajp.2020.101944. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Druss BG and Perlick DA (2014) The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest 15(2), 37–70. 10.1177/1529100614531398. [DOI] [PubMed] [Google Scholar]
- Dardas LA, Silva SG, Smoski MJ, Noonan D and Simmons LA (2017) Personal and perceived depression stigma among Arab adolescents: Associations with depression severity and personal characteristics. Archives of Psychiatric Nursing 31(5), 499–506. 10.1016/J.APNU.2017.06.005. [DOI] [PubMed] [Google Scholar]
- Fluharty M, Taylor AE, Grabski M and Munafò MR (2017) The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine and Tobacco Research 19(1), 3–13. 10.1093/NTR/NTW140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodfellow C, Macintyre A, Knifton L and Sosu E (2023) Associations between dimensions of mental health literacy and adolescent help-seeking intentions. Child and Adolescent Mental Health 28(3), 385–392. 10.1111/CAMH.12608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM and Christensen H (2010) Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 10, 113. 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart LM, Morgan AJ, Rossetto A, Kelly CM, Mackinnon A and Jorm AF (2018) Helping adolescents to better support their peers with a mental health problem: A cluster-randomised crossover trial of teen mental health first aid. The Australian and New Zealand Journal of Psychiatry 52(7), 638–651. 10.1177/0004867417753552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B and Pollitt P (1997a) ‘Mental health literacy’: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. The Medical Journal of Australia 166(4), 182–186. 10.5694/J.1326-5377.1997.TB140071.X. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B and Pollitt P (1997b) Public beliefs about causes and risk factors for depression and schizophrenia. Social Psychiatry and Psychiatric Epidemiology 32(3), 143–148. 10.1007/BF00794613. [DOI] [PubMed] [Google Scholar]
- Kågström A, Pešout O, Kučera M, Juríková L and Winkler P (2023) Development and validation of a universal mental health literacy scale for adolescents (UMHL-A). Psychiatry Research 320, 115031. 10.1016/J.PSYCHRES.2022.115031. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL and Williams JBW (2001) The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutcher S, Bagnell A and Wei Y (2015) Mental health literacy in secondary schools: A Canadian approach. Child and Adolescent Psychiatric Clinics of North America 24(2), 233–244. 10.1016/J.CHC.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Lam LT (2014) Mental health literacy and mental health status in adolescents: A population-based survey. Child and Adolescent Psychiatry and Mental Health 8(1), 1–8. 10.1186/1753-2000-8-26/TABLES/4.24444351 [DOI] [Google Scholar]
- Lee JE, Goh ML and Yeo SF (2023) Mental health awareness of secondary schools students: Mediating roles of knowledge on mental health, knowledge on professional help, and attitude towards mental health. Heliyon 9(3), e14512. 10.1016/J.HELIYON.2023.E14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang M, Chen Q, Guo J, Mei Z, Wang J, Zhang Y, He L and Li Y (2023) Mental health first aid improves mental health literacy among college students: A meta-analysis. Journal of American College Health 71(4), 1196–1205. 10.1080/07448481.2021.1925286. [DOI] [PubMed] [Google Scholar]
- Ma R, Liu T, Raymond Sum KW, Gao T, Li M, Choi SM, Huang Y and Xiang W (2021) Relationship among physical literacy, mental health, and resilience in college students. Frontiers in Psychiatry 12, 767804. 10.3389/FPSYT.2021.767804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun MA, Misti JM, Hosen I and Al Mamun F (2022) Suicidal behaviors and university entrance test‐related factors: A Bangladeshi exploratory study. Perspectives in Psychiatric Care 58(1), 278–287. 10.1111/ppc.12783. [DOI] [PubMed] [Google Scholar]
- Mamun MA, Naher S, Moonajilin MS, Jobayar AM, Rayhan I, Kircaburun K and Griffiths MD (2020) Depression literacy and awareness programs among Bangladeshi students: An online survey. Heliyon 6(9), e04901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell CP, Dishman RK, Vancampfort D, Hallgren M, Stubbs B, MacDonncha C and Herring MP (2018) Physical activity and generalized anxiety disorder: Results from the Irish longitudinal study on ageing (TILDA). International Journal of Epidemiology 47(5), 1443–1453. 10.1093/IJE/DYY141. [DOI] [PubMed] [Google Scholar]
- O’Neill A, Stapley E, Rehman I and Humphrey N (2023) Adolescent help-seeking: An exploration of associations with perceived cause of emotional distress. Frontiers in Public Health 11, 1183092. 10.3389/FPUBH.2023.1183092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özbıçakçı Ş and Salkim ÖÖ (2024) The predictors of mental health literacy among adolescents students. Archives of Psychiatric Nursing 50, 1–4. 10.1016/J.APNU.2024.03.002. [DOI] [PubMed] [Google Scholar]
- Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, Herrman H, Herzallah MM, Huang Y, Jordans MJD, Kleinman A, Medina-Mora ME, Morgan E, Niaz U, Omigbodun O, Prince M, Rahman A, Saraceno B, Sarkar BK, De Silva M, Singh I, Stein DJ, Sunkel C and UnÜtzer J (2018) The Lancet Commission on global mental health and sustainable development. Lancet (London, England) 392(10157), 1553–1598. 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- Rickwood D, Deane FP, Wilson CJ and Ciarrochi J (2005) Young people’s help-seeking for mental health problems. Australian E-Journal for the Advancement of Mental Health 4(3), 218–251. 10.5172/JAMH.4.3.218. [DOI] [Google Scholar]
- Rickwood DJ, Mazzer KR and Telford NR (2015) Social influences on seeking help from mental health services, in-person and online, during adolescence and young adulthood. BMC Psychiatry 15, 40. 10.1186/S12888-015-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, Demyttenaere K, De Girolamo G, Haro JM, Jin R, Karam EG, Kovess-Masfety V, Levinson D, Medina Mora ME, Ono Y, Ormel J, Pennell BE, Posada-Villa J, Sampson NA, Williams D and Kessler RC (2009) Cross-national associations between gender and mental disorders in the World Health Organization world mental health surveys. Archives of General Psychiatry 66(7), 785–795. 10.1001/ARCHGENPSYCHIATRY.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S, Zaki RA, Farid NDN and Kaur K (2022) The determinants of mental health literacy among young adolescents in Malaysia. International Journal of Environmental Research and Public Health 19(6), 3242. 10.3390/IJERPH19063242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokolová L (2024) Mental health literacy and seeking for professional help among secondary school students in Slovakia: A brief report. Frontiers in Public Health 12, 1333216. 10.3389/FPUBH.2024.1333216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW and Löwe B (2006) A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine 166(10), 1092–1097. 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stallman HM (2010) Psychological distress in university students: A comparison with general population data. Australian Psychologist 45(4), 249–257. 10.1080/00050067.2010.482109. [DOI] [Google Scholar]
- Turecki G and Brent DA (2016) Suicide and suicidal behaviour. Lancet (London, England) 387(10024), 1227–1239. 10.1016/S0140-6736(15)00234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei Y, Hayden JA, Kutcher S, Zygmunt A and McGrath P (2013) The effectiveness of school mental health literacy programs to address knowledge, attitudes and help seeking among youth. Early Intervention in Psychiatry 7(2), 109–121. 10.1111/EIP.12010. [DOI] [PubMed] [Google Scholar]