Abstract
Objective
Bowel perforation is a major, yet unstudied complication of ultrasound-guided hydrostatic enema reduction (UGHR). In this study, we aimed to explore the risk factors and determine the clinical characteristics of bowel perforation during UGHR for paediatric intussusception (P-UGHR).
Methods
We retrospectively analysed the medical records of patients who underwent UGHR for intussusception at our institution between January 2011 and December 2021. The patients were divided into the P-UGHR and no P-UGHR groups. Univariate and multivariate logistic regression analyses were performed to analyse the risk factors for P-UGHR, and the clinical characteristics of patients with P-UGHR were determined.
Results
The final analysis included 4961 intussusception episodes. We identified 15 patients [eight male (53.3%); median age, 8.73 months; age range, 3–17 months] with P-UGHR. All P-UGHR cases involved colonic perforations without necrosis distal to the intussusception mass. The perforations were located in the ascending [40% (6/15)], transverse [46.7% (7/15)] or descending colon [13.3% (2/15)]. Age ≤10.5 months [odds ratio (OR), 3.636; 90% confidence interval (CI), 1.274–10.38; P = 0.043], bloody stools (OR, 4.189; 90% CI, 1.352–12.978; P = 0.037) and symptom duration >17.5 h (OR, 0.188; 90% CI, 0.053–0.666; P = 0.03) were independent risk factors for P-UGHR.
Conclusion
Age ≤10.5 months, bloody stools and symptom duration >17.5 h were independent risk factors for P-UGHR. Caution should be exercised during UGHR in patients aged ≤10.5 months, with bloody stools or symptom duration >17.5 h.
Keywords: Infant, intussusception, paediatric perforation, ultrasound-guided hydrostatic enema reduction
1. Introduction
Intussusception is the most common abdominal emergency in infants and toddlers, with an incidence of approximately 1–4 per 2000 infants and children [1,2]. The first-line treatment for uncomplicated paediatric intussusception is enema reduction, which has a great significance in the treatment history of paediatric intussusception.
Ultrasound-guided hydrostatic enema reduction (UGHR) and fluoroscopy-guided air enema reduction are internationally recognized nonsurgical treatment methods for paediatric intussusception [3–5], for which the indications and contraindications are basically the same.
Bowel perforation, the major and most serious complication of attempted enema reduction in paediatric intussusception, can cause life-threatening complications without immediate treatment. Therefore, the possibility of perforation must be anticipated at the time of enema reduction and immediately recognized. Some studies have reported bowel perforation using air and barium to reduce paediatric intussusception [6–8]. However, clinical studies of bowel perforation during UGHR of paediatric intussusception (P-UGHR) are lacking worldwide [9,10].
In this study, we investigated the risk factors and clinical characteristics of P-UGHR.
2. Methods
2.1. Study design
In this single-centre retrospective observational study, we aimed to identify the clinical characteristics and risk factors for P-UGHR. This study was approved by the Institutional Review Board of Shengjing Hospital of China Medical University (No. 2023PS1151K), which waived the requirement for informed consent owing to its retrospective nature. This study had adhered to the principles stated in the ‘Declaration of Helsinki’.
2.2. Participants and data collection
All available medical records of patients who underwent the UGHR for intussusception (ICD-10 code: K56.1) at our institution between January 2011 and December 2021 were reviewed. The inclusion criteria were as follows: age <14 years and intussusception confirmed via ultrasonography conducted by an experienced examiner according to the clinical guidelines for diagnosing acute intussusception.
The patients’ clinical data, including demographic characteristics (sex and age), clinical manifestations, preoperative examination details, UGHR process, surgical procedure performed, surgical findings, histopathological results, postoperative complications and outcomes, were recorded.
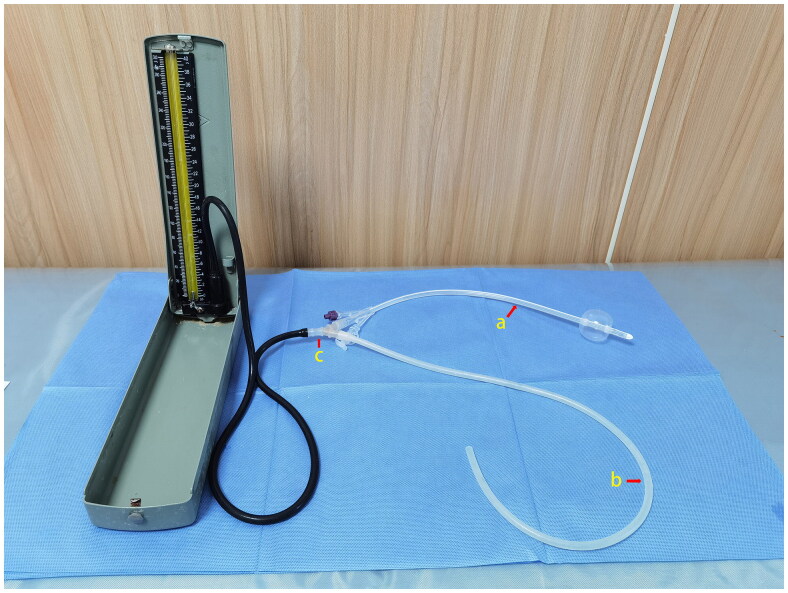
The UGHR [3,9] was performed by two paediatric surgeons under ultrasound guidance. Patients were placed in the supine position. A Foley catheter (Figure 1a) was inserted via the anus, and the buttocks were taped to prevent normal saline (NS) leakage. A rubber tube (Figure 1b) was used to inject NS. The Foley catheter and rubber tube were connected to the sphygmomanometer using a three-way tube (Figure 1c). Thus, the sphygmomanometer measured intracolonic pressure in these patients. Under ultrasound guidance, the NS (37–40 °C) was manually injected through a rubber tube. The hydrostatic pressure was continuously monitored using a sphygmomanometer attached to a Foley catheter. The maximum pressure was maintained at <100 mmHg. Successful reduction was determined based on the disappearance of intussusception and visualization of the NS from the caecum to the ileum through the ileocecal valve or the NS-distended ileum. A maximum of three reduction attempts was allowed.
Figure 1.
The photo of tubes used in the procedure of UGHR. (a) The Foley catheter inserted into the anus; (b) the rubber tube used to inject NS and (c) the three-way tube used for connecting the Foley catheter and the rubber tube with the sphygmomanometer.
2.3. Grouping
The patients were divided into the P-UGHR and non-P-UGHR groups. P-UGHR was defined as bowel perforation recognized during UGHR and confirmed based on surgical records. Age, symptom duration, sex and clinical symptoms (colicky abdominal pain, vomiting, bloody stools, fever and diarrhoea) were evaluated and compared between the groups.
2.4. Statistical analysis
The data were entered into a database by one author and reviewed by another. Data were analysed using IBM SPSS Statistics software for Windows version 20.0 (IBM Corp., Armonk, NY). Continuous and categorical variables were expressed as medians and ranges and as frequencies and proportions, respectively.
The Mann–Whitney U test was performed to compare the age in months and symptom duration in hours between the groups. A chi-square test was performed to compare sex and clinical symptoms (bloody stools, vomiting, colicky abdominal pain, fever and diarrhoea) between the two groups. Differences in continuous parametric and non-continuous data were evaluated using the Mann–Whitney U and chi-squared tests, respectively. Multivariate logistic regression analysis was performed to identify independent risk factors and reduce confounding biases. A receiver operating characteristic (ROC) curve was used to predict the cutoff points for age and symptom duration. Statistical significance was set at P < 0.05.
3. Results
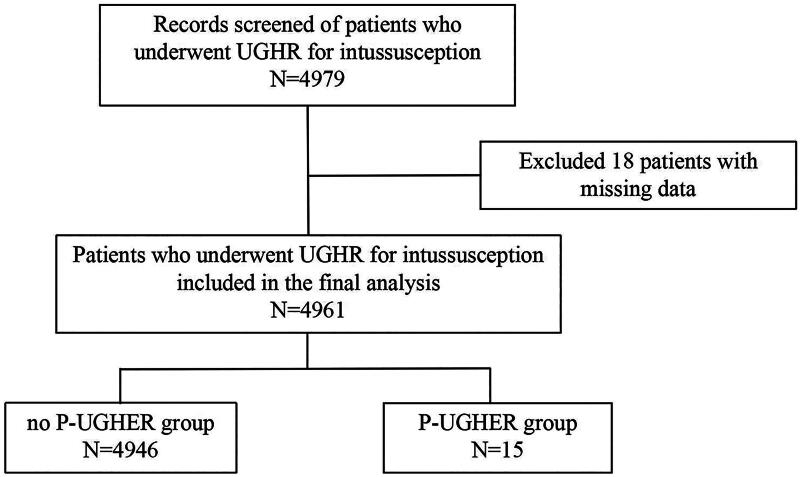
Between January 2011 and December 2021, 4979 paediatric patients with intussusception underwent UGHR at our institution. Missing data elements were identified in 18 records and were excluded. In total, 4961 records of intussusception episodes were collected for the final analysis. Overall, 15 patients [0.3% (15/4961)] underwent P-UGHR (Figure 2).
Figure 2.
Study flowchart.
3.1. Clinical characteristics of patients with P-UGHR
3.1.1. Clinical manifestations
In total, 15 patients [eight male (53.3%); median age, 8.73 months; age range, 3–17 months] with the P-UGHR were identified. The main symptoms included vomiting [93.3% (14/15)], bloody stools [80% (12/15)] and colicky abdominal pain [73.3% (11/15)]. The duration of symptoms was 12–96 h.
3.1.2. UGHR procedure
The maximum enema pressure before perforation was 80–100 mmHg. The NS volume was 400–1200 mL. The number of attempts varied: one [73.3% (11/15)], two [20% (3/15)] and three attempts [6.6% (1/15)].
3.1.3. Surgical findings
All 15 patients underwent emergency surgery and no deaths occurred. Manual reduction of intussusception was performed intraoperatively. Perforation repair [66.7% (10/15)] or partial bowel segment resection [33.3% (5/15)] was performed. The intussusception types were ileocolic [46.7% (7/15)], ileo-ileocolic [33.3% (5/15)] and ileocecal [20% (3/15)]. All perforations were colonic, without necrosis, and were distal to the intussusception mass. The perforations were located in the ascending [40% (6/15)], transverse [46.7% (7/15)] or descending colon [13.3% (2/15)]. The perforations were 0.3–1.5 cm. Intussusceptum bowel necrosis was confirmed in four patients [26.7% (4/15)]. No pathological lead points were identified in any of the 15 patients. The volume of ascites, which is always a clear fluid, was 200–1000 mL. Little or no peritoneal faecal contamination was observed.
3.1.4. Complications and outcomes
Four patients [26.7% (4/15)] showed symptoms of septic shock and were transferred to the paediatric intensive care unit for antishock therapy (antimicrobial therapy, fluid therapy, hemodynamic monitoring, vasoactive medications, ventilation, corticosteroid administration and nutritional support) for 2–5 d. Disruption of the wound occurred in four patients (26.7%) who underwent a second wound-tension suture. No significant sequelae were observed after a 10–60-month follow-up period.
3.2. Risk factor analysis
3.2.1. Univariate analysis of all predictor variables of P-UGHR
The Mann–Whitney U test demonstrated a significant difference in age (P < 0.001) and duration of symptoms (P = 0.01) between the P-UGHR and non-P-UGHR groups. The chi-square test revealed a significant difference in bloody stools (P < 0.001), vomiting (P = 0.005) and colicky abdominal pain (P = 0.034) between the P-UGHR and no P-UGHR groups; sex (P = 0.313), fever (P = 0.094), diarrhoea (P = 0.792) and number of attempts (P = 0.067) did not differ significantly between the two groups (Table 1).
Table 1.
Baseline characteristics of the study population and univariate comparison between the P-UGHR and no P-UGHR groups.
| Characteristics | All, n (%) N = 4961 | P-UGHR group, n (%) N = 15 | No P-UGHR group, n (%) N = 4946 | P value | 90% confidence interval | |||
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Male | 3258 | 65.7% | 8 | 53.3% | 3250 | 65.7% | 0.313 | |
| Female | 1703 | 34.3% | 7 | 46.7% | 1696 | 34.3% | ||
| Age (month) | ||||||||
| Median | 20 | 7 | 20 | |||||
| Average | 24.902 | 8.733 | 24.951 | <0.001 | 24.51–25.37 | |||
| ≤10.5 | 1172 | 23.6% | 11 | 73.3% | 1161 | 23.5% | ||
| >10.5 | 3789 | 76.4% | 4 | 26.7% | 3785 | 76.5% | ||
| Symptoms | ||||||||
| Abdominal pain | 4551 | 91.7% | 11 | 73.3% | 4540 | 91.8% | 0.034 | |
| Vomiting | 2876 | 58.0% | 14 | 93.3% | 2862 | 57.9% | 0.005 | |
| Bloody stools | 1311 | 26.4% | 12 | 80.0% | 1299 | 26.3% | <0.001 | |
| Diarrhoea | 404 | 8.1% | 2 | 13.3% | 402 | 8.1% | 0.792 | |
| Fever | 730 | 14.7% | 5 | 33.3% | 725 | 14.7% | 0.094 | |
| Symptom duration (h) | ||||||||
| Median | 16 | 16 | 24 | |||||
| Average | 26.18 | 34.73 | 26.21 | 0.01 | 25.43–26.94 | |||
| ≤17.5 | 2581 | 52.0% | 2 | 13.3% | 2579 | 52.1% | ||
| >17.5 | 2380 | 48.0% | 13 | 86.7% | 2367 | 47.9% | ||
| Number of attempts | ||||||||
| 1 | 4434 | 89.4% | 11 | 73.3% | 4423 | 89.4% | 0.067 | |
| ≥2 | 527 | 10.6% | 4 | 26.7% | 523 | 10.6% | ||
3.2.2. Multivariate analysis to predict P-UGHR
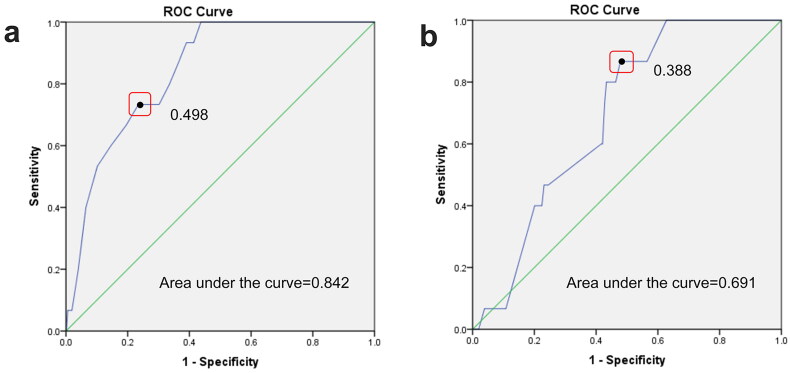
The ROC curve was used to predict the cutoff points for age and symptom duration. Age ≤10.5 months and symptom duration ≤17.5 h were used as the cutoff points for the further multivariate analysis (Figure 3).
Figure 3.
ROC curve analysis for ‘age’ (a) and ‘symptom duration’ (b).
The multivariate analysis to determine the independent risk factors associated with P-UGHR indicated that, out of five factors, age ≤10.5 months [odds ratio (OR), 3.636; 90% confidence interval (CI), 1.274–10.38; P = 0.043], bloody stools (OR, 4.189; 90% CI, 1.352–12.978; P = 0.037) and symptom duration >17.5 h (OR, 0.188; 90% CI, 0.053–0.666; P = 0.03) were independent risk factors for P-UGHR (Table 2).
Table 2.
Multivariate analysis of risk factors of P-UGHR.
| Variables | β | SE | OR | 90% CI | P value |
|---|---|---|---|---|---|
| Age ≤10.5 months | 1.291 | 0.638 | 3.636 | 1.274–10.38 | 0.043 |
| Bloody stools | 1.433 | 0.687 | 4.189 | 1.352–12.978 | 0.037 |
| Symptom duration ≤17.5 h | −1.67 | 0.768 | 0.188 | 0.053–0.666 | 0.03 |
| Vomiting | 1.45 | 1.066 | 4.264 | 0.739–24.618 | 0.174 |
| Colicky abdominal pain | −0.293 | 0.609 | 0.746 | 0.274–2.033 | 0.631 |
CI, confidence interval; OR, odds ratio. Bold values indicate significant differences (P < 0.05).
4. Discussion
To our knowledge, this is the first case–control study of P-UGHR, which includes the largest number of cases worldwide and can provide clinical experience for P-UGHR prevention and treatment. Previous studies on bowel perforation during enema reduction in paediatric intussusception were case reports on the use of air and/or barium conducted at least 25 years ago [6–8].
In this study, we identified several risk factors for the P-UGHR. The multivariate analysis results confirmed that age ≤10.5 months is an independent risk factor for P-UGHR, indicating that intussusception in patients aged ≤10.5 months is more likely to be P-UGHR. Multivariate analysis indicated that bloody stool was another independent risk factor for P-UGHR. The high and low incidences of bloody stools in patients with P-UGHR [80% (12/15)] and in those without P-UGHR [25.19% (1246/4946)], respectively, make it reliable for predicting P-UGHR. In patients with intussusception and bloody stools, a disturbance in blood circulation in the bowel wall decreases colon strength. The colonic wall is weak, perforates easily and cannot tolerate high enema pressures during UGHR. The multivariate analysis indicated that symptom duration >17.5 h is a risk factor for P-UGHR, which is consistent with the results of other studies [7,11–13].
In recent years, several laboratory parameters that are useful for predicting enema reduction failure in paediatric intussusception have been identified [14]. The advantage of these markers is that they are objective and do not depend on parental perceptions, such as the number of hours of symptom evolution, which is sometimes difficult to determine.
P-UGHR is a life-threatening acute colonic perforation that occurs in the paediatric population [15]. Firstly, paediatric surgeons should be aware of the indications and contraindications for the UGHR. Secondly, paediatric surgeons should pay more attention to patients aged ≤10.5 months, with bloody stools or symptom duration >17.5 h. Once this occurs, the P-UGHR should be immediately detected. The most common clinical presentations were abdominal distension and peritonitis. Some of the patients were in poor health. Secondly, a sudden decrease in the enema pressure occurred. Ultrasonographic features include increased fluid volume in the abdominal cavity, sudden decrease or disappearance of fluid volume from the colon and the presence of bowel floating in the fluid-filled upper peritoneal cavity [16,17].
If P-UGHR occurs, enema reduction should be stopped immediately because emergency surgery is the only available treatment. The procedure includes an initial reduction of the intussusception, followed by perforation repair or segmental bowel resection. Surgeons should carefully check the colon distal to the intussusception mass and the intussusceptum for perforation and necrosis. In this study, one patient aged 6 months developed two perforations in the transverse colon, whereas four others developed intussusceptum bowel necrosis. Some studies have supported the active role of paediatric surgeons in enema reduction [18,19]. We also recommend that a paediatric surgeon who can perform UGHR immediately detects P-UGHR and manages abdominal decompression, and that emergency operations be performed during the entire UGHR procedure. During emergency surgery for P-UGHR, peritoneal contamination was relatively mild compared with the severity of colon perforation caused by other reasons. We analysed the possible reasons for this. Firstly, when P-UGHR occurs, the enema is stopped immediately, and most of the NS drains through the Foley catheter. The NS that spilled into the peritoneal cavity was not excessive. Secondly, all patients with P-UGHR were infants aged ≤17 months in whom colon peristalsis was rapid and emptying is easy. Therefore, the colon distal to the intussusception mass is always empty and little colonic content spills into the peritoneal cavity.
This study had several limitations. Firstly, it was retrospective, which increased its potential for bias compared to prospective studies. Owing to the rarity of the P-UGHR, performing a prospective study is challenging. Secondly, the sample size was small because of the low incidence of P-UGHR, despite the 11-year study period. A multicentre study may increase the number of P-UGHR cases and improve the quality of research evidence. Thirdly, the lower end of the CI was very close to 1, likely because of the small number of P-UGHR cases. The 90% CI was very wide, limiting the strength of our conclusions. Finally, we were unable to measure certain risk factors, which should be the focus of future studies. Nevertheless, we believe that our study provides new insights into the P-UGHR.
In conclusion, we identified age ≤10.5 months, bloody stools and symptom duration >17.5 h as independent risk factors for P-UGHR. Further prospective studies and validation are required to confirm these findings. Caution should be taken during UGHR in patients aged ≤10.5 months, with bloody stools or symptom duration >17.5 h.
Acknowledgements
The authors would like to thank Editage (www.editage.cn) for the English language editing.
Funding Statement
This study was supported by the Liaoning Revitalization Talents Program (grant number: XLYC1908008), the Outstanding Scientific Fund of Shengjing Hospital (grant number: Me56) and 345 Talent Project of Shengjing Hospital (grant number: M1403).
Authors contributions
X.T.: study conceptualization, literature search, data collection and analysis, and manuscript preparation; S.L.: study conceptualization, data analysis and manuscript review; Q.W., Y.L. and X.M.: data collection and analysis; manuscript review; Y.B.: study design, collection and analysis of data, manuscript preparation and review. All authors have approved the final manuscript as submitted and agreed to be accountable for all aspects of this work. All authors have read and agreed to the published version of the manuscript.
Consent form
Patient consent was waived because of the retrospective nature of the study.
Disclosure statement
The authors declare no conflict of interest relevant to this article.
Data availability statement
Data are available by request from the corresponding author.
References
- 1.Edwards EA, Pigg N, Courtier J, et al. Intussusception: past, present and future. Pediatr Radiol. 2017;47(9):1101–1108. doi: 10.1007/s00247-017-3878-x. [DOI] [PubMed] [Google Scholar]
- 2.Khorana J, Singhavejsakul J, Ukarapol N, et al. Enema reduction of intussusception: the success rate of hydrostatic and pneumatic reduction. Ther Clin Risk Manag. 2015;11:1837–1842. doi: 10.2147/TCRM.S92169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu ST, Tang XB, Li H, et al. Ultrasound-guided hydrostatic reduction versus fluoroscopy-guided air reduction for pediatric intussusception: a multi-center, prospective, cohort study. World J Emerg Surg. 2021;16(1):3. doi: 10.1186/s13017-020-00346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang H, Wang G, Ding Y, et al. Effectiveness and safety of ultrasound-guided hydrostatic reduction for children with acute intussusception. Sci Prog. 2021;104(3):368504211040911. doi: 10.1177/00368504211040911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie X, Wu Y, Wang Q, et al. A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. J Pediatr Surg. 2018;53(8):1464–1468. doi: 10.1016/j.jpedsurg.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Bramson RT, Blickman JG.. Perforation during hydrostatic reduction of intussusception: proposed mechanism and review of the literature. J Pediatr Surg. 1992;27(5):589–591. doi: 10.1016/0022-3468(92)90454-f. [DOI] [PubMed] [Google Scholar]
- 7.Daneman A, Alton DJ, Ein S, et al. Perforation during attempted intussusception reduction in children-a comparison of perforation with barium and air. Pediatr Radiol. 1995;25(2):81–88. doi: 10.1007/BF02010311. [DOI] [PubMed] [Google Scholar]
- 8.Maoate K, Beasley SW.. Perforation during gas reduction of intussusception. Pediatr Surg Int. 1998;14(3):168–170. doi: 10.1007/s003830050476. [DOI] [PubMed] [Google Scholar]
- 9.Bai YZ, Qu RB, Wang GD, et al. Ultrasound-guided hydrostatic reduction of intussusceptions by saline enema: a review of 5218 cases in 17 years. Am J Surg. 2006;192(3):273–275. doi: 10.1016/j.amjsurg.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 10.Ntoulia A, Tharakan SJ, Reid JR, et al. Failed intussusception reduction in children: correlation between radiologic, surgical, and pathologic findings. AJR Am J Roentgenol. 2016;207(2):424–433. doi: 10.2214/AJR.15.15659. [DOI] [PubMed] [Google Scholar]
- 11.Daneman A, Navarro O.. Intussusception. Part 2: an update on the evolution of management. Pediatr Radiol. 2004;34(2):97–108, quiz 187. doi: 10.1007/s00247-003-1082-7. [DOI] [PubMed] [Google Scholar]
- 12.Ein SH, Mercer S, Humphry A, et al. Colon perforation during attempted barium enema reduction of intussusception. J Pediatr Surg. 1981;16(3):313–315. doi: 10.1016/s0022-3468(81)80687-2. [DOI] [PubMed] [Google Scholar]
- 13.Humphry A, Ein SH, Mok PM.. Perforation of the intussuscepted colon. AJR Am J Roentgenol. 1981;137(6):1135–1138. doi: 10.2214/ajr.137.6.1135. [DOI] [PubMed] [Google Scholar]
- 14.Delgado-Miguel C, García A, Delgado B, et al. Neutrophil-to-lymphocyte ratio as a predictor of the need for surgical treatment in children’s intussusception. Eur J Pediatr Surg. 2023;33(5):422–427. doi: 10.1055/a-1913-4280. [DOI] [PubMed] [Google Scholar]
- 15.Dokucu A, Oztürk H, Yağmur Y, et al. Colon injuries in children. J Pediatr Surg. 2000;35(12):1799–1804. doi: 10.1053/jpsu.2000.19262. [DOI] [PubMed] [Google Scholar]
- 16.Hadidi AT, El Shal N.. Childhood intussusception: a comparative study of nonsurgical management. J Pediatr Surg. 1999;34(2):304–307. doi: 10.1016/s0022-3468(99)90196-3. [DOI] [PubMed] [Google Scholar]
- 17.Wang GD, Liu SJ.. Enema reduction of intussusception by hydrostatic pressure under ultrasound guidance: a report of 377 cases. J Pediatr Surg. 1988;23(9):814–818. doi: 10.1016/s0022-3468(88)80229-x. [DOI] [PubMed] [Google Scholar]
- 18.Kelley-Quon LI, Arthur LG, Williams RF, et al. Management of intussusception in children: a systematic review. J Pediatr Surg. 2021;56(3):587–596. doi: 10.1016/j.jpedsurg.2020.09.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okazaki T, Ogasawara Y, Nakazawa N, et al. Reduction of intussusception in infants by a pediatric surgical team: improvement in safety and outcome. Pediatr Surg Int. 2006;22(11):897–900. doi: 10.1007/s00383-006-1766-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available by request from the corresponding author.