MicroNET-covered stent (CGuard) is a self-expandable 2nd-generation carotid dual-layer anti-embolic (“mesh”) stent with level-1 (randomized controlled trial) evidence for a profound reduction of peri-procedural cerebral embolism and elimination of lesion-related post-procedural embolism in carotid artery stenting (CAS) [1]. Clinical data demonstrate a minimized risk of 30-day death/stroke/myocardial infarction (≤ 1%) and optimal long-term outcomes with CGuard, in absence of device-related issues [2–6]. Today, competent CAS has a significant part in primary and secondary stroke prevention [7]. Also, evidence is increasing for an important role of the MicroNET-covered stent in improving the outcomes of emergency CAS in acute carotid-related strokes [8–10].
CGuard consists of a very widely open-cell (laser-cut) metallic frame (free cell area of ~22 mm²) that is wrapped by an outer, single-fiber knitted polyethylene terephthalate MicroNET adaptable sleeve (fiber thickness ~25 μm; cell size ~0.02–0.03 mm2; mesh fixation to the frame on stent edges [11, 12]); for a stent photograph see reference 13. CGuard combines properties of the most open-cell metallic stent frame (and thus very high conformability) with the smallest-cell anti-embolic layer [11, 12]. The MicroNET pore size is similar to that of embolic protection filters, resulting in a dense plaque coverage between the sparse struts, providing not only sequestration of the atherothrombotic plaque material but also a degree of sealing properties [13–17]. The MicroNET-covered stent shows no foreshortening or elongation and exhibits self-adaptability to the artery diameter (within the device nominal diameter; “SmartFit” characteristics) [11, 12]. The neuroprotective [1, 4, 14] stent has an increasing role in emergency management of carotid-related strokes [8–10]. Importantly, when properly implanted (post-dilatation embedded), the MicroNET-covered stent shows a normal healing profile and minimal in-stent restenosis (< 1%) [5, 6, 8, 17].
Embolic protection device use remains important in MicroNET-covered stent CAS because of the need to prevent cerebral embolism at procedural stages prior to protection by the MicroNET that is exerted only after the stent implantation and post-dilatation optimization [14]. Distal filters have several limitations relevant for cerebral safety of CAS [14, 18, 19]. Thus practical knowledge of how to effectively use proximal cerebral protection is crucial in today’s competent CAS [14, 20, 21]. For procedures at the level of carotid bifurcation, double-balloon systems, enabling transient endovascular exclusion of both the external (ECA) and common (CCA) carotid artery – and thus preventing any flow towards the brain in the internal carotid artery – are preferred [13, 14, 22] , as with a mono-balloon catheter the flow exclusion may be limited to CCA-only [13]. This, in some patients, can be insufficient for any effective cerebral protection because of the residual flow from the ECA to the ICA, towards the brain [13]. However, use of the double-balloon catheter [20] is not feasible in case of severe stenosis of the ECA ostium (Figures 1 A–C) and/or when the lesion involves distal CCA [13].
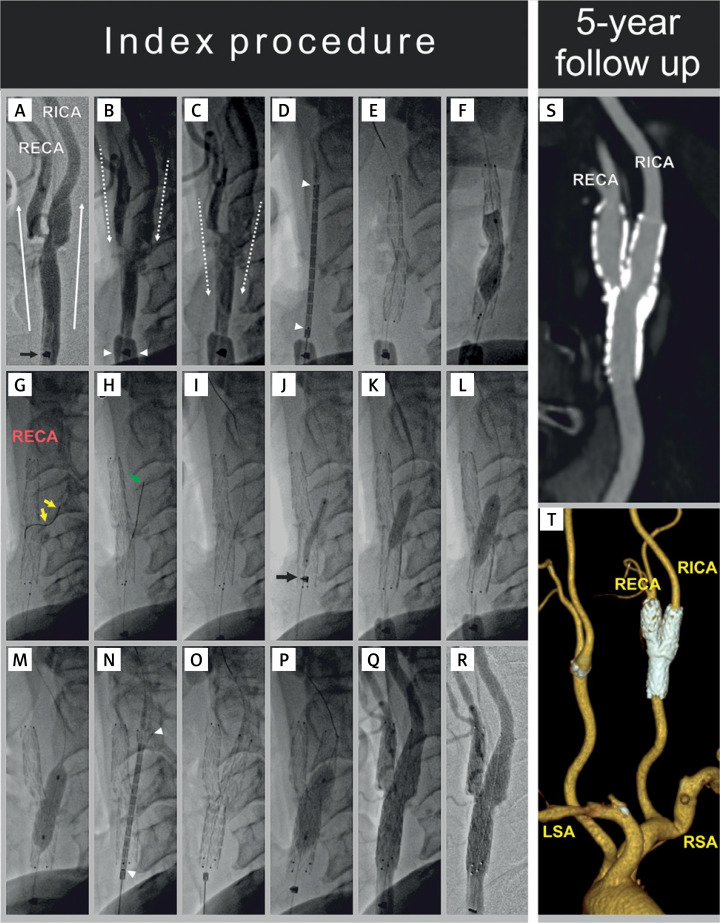
Figure 1.
A 61-year-old man presenting with a recent right-hemispheric transient ischemic attack was treated, in primary prevention of carotid-related stroke, with proximal-protected stenting of the right internal carotid artery. MicroNET-covered 2nd-generation anti-embolic stent was used consistent with the PARADIGM protocol [11]. Proximal cerebral protection – offering a “protected” lesion crossing [14, 20] – was selected due to the lesion morphology (A, note a large ulceration in the right internal carotid artery extending to the distal common carotid artery seen with antegrade contrast injection, white arrows, via a non-inflated mono-balloon catheter, the catheter marker is indicated with a black arrow) and symptomatic presentation, consistent with the ‘tailored’ CAS algorithm [18]. With the external carotid artery (RECA) tight ostial stenosis, and lesion involving also the distal common carotid artery (A), use of a double-balloon proximal neuroprotection system (that is our preference [8, 10, 13]) was not feasible as the balloon-wire ECA exclusion system [22] was no longer available. Contrast injection (common carotid artery, CCA balloon inflated, B, white arrowheads, “back” pressure 68/52 mm Hg) demonstrated – with opening the stopcock of the system – flow reversal (B and C, dotted arrows) in the right internal carotid artery (RICA, target vessel), RECA, and CCA, consistent with an effective cerebral protection. The common carotid artery lesion was crossed with a coronary wire (BMW 0.014 J) and a 10 × 30 mm self-expandable MicroNET-covered stent was positioned (D, white arrowheads indicate the stent edges), released (E), and post-dilated with a 5.5 × 20 mm balloon (F). As post-aspiration visualization demonstrated stent presence in RECA-CCA (rather than ICA-CCA), an attempt was made to cross from the CCA to the ostial-stenosed (cf., A) – and now covered with the dual-layer stent – RICA. Attempts to cross with standard coronary wires (BMW 0.014” and WhisperMS 0.014”) failed but crossing with a V-14 wire (with manually modified tip angulation to resolve the “wire-preferred” entry into the RICA ulcer, yellow arrows in G) was successful (H, green arrow). Effective reaching of the RICA distal extracranial segment with the angioplasty wire is shown in I. Insertion of a small coronary balloon through the 2 stent layers and the RICA ostial stenosis required increased support from the guiding catheter (note the catheter marker within the proximal portion of the 1st stent, J, arrow). Gradual opening of the RICA ostium was performed under resumed (due to extended procedure duration – at key steps) proximal protection, using a semi-compliant coronary balloon (3.5 × 15 mm, K) followed by non-compliant balloons (5.0 × 20 mm and 6.0 × 20 mm, L and M). With the above preparation, a second 10 × 30 mm self-expandable MicroNET-covered stent could be smoothly inserted into the RICA, positioned (N), and released (O). The stent was gradually post-dilatation optimized, up to using (finally) an 8.0 × 20 mm balloon inflated up to 20 atm at the proximal segment (P). No balloon inflations from the CCA to RECA were performed following the 2nd (ie., RICA-RCCA) stent implantation. The final result at the carotid bifurcation is shown in Q (non-subtracted image) and R (digital subtraction angiogram). There was no cerebral embolism and the procedure was clinically uneventful. Annual clinical and duplex ultrasound follow-ups were normal. At 5 years in-stent peak velocities remained normal (RICA – 58/28 cm/s; RECA – 82/21 cm/s; RCCA – 76/31 cm/s), and computed tomography angiography demonstrated – with the “Y” configuration of the stents – a lasting optimal anatomic result of the reconstruction of carotid bifurcation in absence of any restenosis (S, T).
We present procedural imaging demonstrating how to resolve safely and effectively – using the endovascular route – an accidental implantation of the CGuard double-layered stent into the ECA (rather than ICA), covering the (diseased) ICA ostium with the MicroNET and strut structure; this occurred in CAS employing a mono-balloon catheter with transient flow reversal for cerebral protection (Figures 1 A–R). 5-year follow-up showed a maintained excellent anatomic result (Figures 1 S-T) in the context of uneventful clinical follow-up.
In conclusion, with mono-balloon use for proximal protection in CAS/eCAS, landmark separation of the ICA and ECA is critical to avoid accidental stent placement in ECA. We show that inadvertent placement of the dual-layer MicroNET-covered stent can be resolved, using the endovascular route (same, continued procedure), by (1) crossing the MicroNET and stent strut frame and making a step-wise gradual opening onto the ICA, followed by (2) placement and optimization of another MicroNET-covered stent (appropriately positioned in the ICA; “Y” technique). This endovascular resolution was safe and effective, with an optimal clinical and anatomic result at long-term. Today, ensured separation of ICA from the ECA under mono-balloon catheter proximal cerebral protection can be practiced – along with neurovascular interventions – in a novel human stroke model [23].
Funding Statement
Funding Open-access publication of this article was supported by the Cardiovascular Center Foundation in Krakow, Poland.
Ethical approval
Not applicable.
Conflict of interest
PM has proctored and/or consulted for Abbott Vascular, Balton, Gore, InspireMD, Medtronic and Penumbra, and serves on the European Society of Cardiology Stroke Council Scientific Documents Task Force; he has been the Polish Cardiac Society Board Representative for Stroke and Vascular Interventions. PM is Global Co-Principal Investigator in CGUARDIANS FDA IDE Trial of the MicroNET-covered carotid stent system. Other authors declare no conflict of interest.
References
- 1.Karpenko A, Bugurov S, Ignatenko P, et al. Randomized controlled trial of conventional versus MicroNet-covered stent in carotid artery revascularization. JACC Cardiovasc Interv 2021; 14: 2377-87. [DOI] [PubMed] [Google Scholar]
- 2.Mazurek A, Malinowski K, Rosenfield K, et al. Clinical outcomes of second-versus first-generation carotid stents: a systematic review and meta-analysis. J Clin Med 2022; 11: 4819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mazurek A, Malinowski K, Sirignano P, et al. Carotid artery revascularization using second generation stents versus surgery: a meta-analysis of clinical outcomes. J Cardiovasc Surg. 2023; 64: 570-82. [DOI] [PubMed] [Google Scholar]
- 4.Karpenko A, Bugurov S, Ignatenko P, et al. Randomized controlled trial of conventional versus MicroNet-covered stent in carotid artery revascularization: 12-month outcomes. JACC Cardiovasc Interv 2023; 16: 878-80. [DOI] [PubMed] [Google Scholar]
- 5.Mazurek A, Borratynska A, Malinowski KP, et al. MicroNET-covered stents for embolic prevention in patients undergoing carotid revascularisation: twelve-month outcomes from the PARADIGM study. EuroIntervention 2020; 16: e950-2. [DOI] [PubMed] [Google Scholar]
- 6.Musialek P, Mazurek A, Kolvenbach R, et al. 5-year clinical and ultrasound outcomes in CARENET prospective multicenter trial of CGuard MicroNET-covered carotid stent. JACC Cardiovasc Interv 2022; 15: 1889-91. [DOI] [PubMed] [Google Scholar]
- 7.Musialek P, Bonati LH, Bulbulia R, et al. Stroke risk management in carotid atherosclerotic disease: A Clinical Consensus Statement of the ESC Council on Stroke and the ESC Working Group on Aorta and Peripheral Vascular Diseases. Cardiovasc Res 2023. Aug 25:cvad135. doi: 10.1093/cvr/cvad135 (online ahead of print)> [DOI] [PubMed] [Google Scholar]
- 8.Tekieli L, Afanasjev A, Mazgaj M, et al. A multi-center study of the MicroNET-covered stent in consecutive patients with acute carotid-related stroke: SAFEGUARD-STROKE. Adv Interv Cardiol. 2024; 20: 172-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim J, Jaikumar V, Scullen TA, et al. Commentary: a multi-center study of the MicroNETcovered stent in consecutive patients with acute carotid-related stroke: SAFEGUARD-STROKE. Adv Interv Cardiol 2024; 20: 245-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tekieli L, Dzierwa K, Grunwald IQ, et al. Outcomes in acute carotid-related stroke eligible for mechanical reperfusion: SAFEGUARD-STROKE [Acute Stroke of Extracranial CArotid Origin Treated With Use oF the MicronEt-Covered CGUARD Stent] Registry. J Cardiovasc Surg 2024; 65: 231-48. [DOI] [PubMed] [Google Scholar]
- 11.Musialek P, Mazurek A, Trystula M, et al. Novel PARADIGM in carotid revascularisation: prospective evaluation of All-comer peRcutaneous cArotiD revascularisation in symptomatic and Increased-risk asymptomatic carotid artery stenosis using CGuard MicroNet-covered embolic prevention stent system. EuroIntervention 2016; 12: e658-70. [DOI] [PubMed] [Google Scholar]
- 12.Wissgott C, Schmidt W, Brandt-Wunderlich C, et al. Clinical results and mechanical properties of the carotid CGUARD double-layered embolic prevention stent. J Endovasc Ther 2017; 24: 130-7. [DOI] [PubMed] [Google Scholar]
- 13.Tekieli L, Mazgaj M, Ruzsa Z, et al. MicroNET-covered stent (CGuard) routine use in acute carotid-related stroke – SAFEGUARD-STROKE Study: response to the Buffalo Group commentary. Adv Interv Cardiol 2024; 20: 248-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Musialek P, de Donato G. Carotid artery revascularization using the endovascular route. In: Peripheral Arterial Interventions – Practical Guide. Ruzsa Z, Bartus S, Nemes B (eds.). Edizioni Minerva Medica, Turin: 2023; 142-72. [Google Scholar]
- 15.Musialek P, Capoccia L, Alvarez CA, et al. Carotid artery endovascular reconstruction using Micronet-covered stents in patients with symptoms or signs of cerebral ischemia (CGuard OPTIMA Trial Investigators; OPtimal sequestration of high-risk carotid lesions with effecTive lumen reconstruction usIng MicroNet–covered stents And the endovascular route, NCT04234854). TCT Featured Research. Available from: https://d18mqtxkrsjgmh.cloudfront.net/public/2022-09/a355a7ab-6d71-44de-8ecf-6712bd763300.pdf [accessed 21 August 2024]> [Google Scholar]
- 16.Lehmann MF, Musialek P. MicroNET-covered stent use to seal carotid artery perforation. Adv Interv Cardiol 2023; 19: 284-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Musialek P, Tekieli L, Umemoto T. Carotid anti-embolic (“Mesh”) stents: not created equal. J Am Soc Car Ang Interv 2024. (in press)> [Google Scholar]
- 18.Pieniazek P, Musialek P, Kablak-Ziembicka A, et al. Carotid artery stenting with patient- and lesion-tailored selection of the neuroprotection system and stent type: early and 5-year results from a prospective academic registry of 535 consecutive procedures (TARGET-CAS). J Endovasc Ther 2008; 15: 249-62. [DOI] [PubMed] [Google Scholar]
- 19.Chmiel J, Tekieli L, Mazurek A, et al. Filter protection in contemporary carotid artery stenting: consider limited protection. Adv Interv Cardiol 2024; 20: 213-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Musialek P. Proximal embolic protection with the Mo.Ma Ultra device: a “must know how” for competent carotid artery stenting. Endovasc Today 2024; 23: 30-2. [Google Scholar]
- 21.Tekieli L, Banaszkiewicz K, Moczulski Z, et al. Novel large-diameter controlled-expansion stentriever, embolic-prevention stent and flow reversal in large-thrombus-burden ICA proximal occlusion stroke. JACC Cardiovasc Interv 2021; 14: e287-91. [DOI] [PubMed] [Google Scholar]
- 22.Nikas D, Reith W, Schmidt A, et al. Prospective, multicenter European study of the GORE flow reversal system for providing neuroprotection during carotid artery stenting. Catheter Cardiovasc Interv 2012; 80: 1060-8. [DOI] [PubMed] [Google Scholar]
- 23.Grunwald IQ, Tekieli L, Podlasek A, et al. Endovascular treatment of tandem lesions in a novel cadaveric stroke model. EuroIntervention 2024. (in press)> [Google Scholar]