Abstract
Background: Music-based intervention has been advocated as a nonpharmacologic approach for the perioperative control of pain and anxiety in surgical patients. However, its impact on patients with preoperative anxiety has not been clearly established. Our study aimed to examine the impact of music-based intervention administered before, during, and after surgery on postoperative opioid consumption and pain levels, as well as preoperative anxiety, depression, and pain catastrophizing. We hypothesized that, compared to a control group, music-based intervention would be effective in reducing opioid requirements and mood disorders. Methods: This study was a single-center, prospective, single-blinded, randomized controlled trial. Inclusion criteria isame-day or observation surgery. Exclusion criteria included American Society of Anesthesiologists physical status IV, use of spinal anesthesia, PROMIS Anxiety T-scores ≤ 57.4 and ≥74.1, preoperative chronic opioid use, transgender surgery, and history of drug or alcohol abuse. Music-based intervention was developed by a certified music therapist. Each patient was randomized to receive standard of care (SC) or SC plus music-based intervention before, during, and after surgery. The primary end point was postoperative oral morphine equivalents (OMEs) over 5 days following surgery using the area under the curve (AUC)Secondary end points were PROMIS Anxiety, PROMIS Depression scores Pain Catastrophizing Scale scores, postoperative nausea and vomiting, time of hospital discharge, and patient satisfaction (0 = totally unsatisfied to 10 = completely satisfied). Results: A total of 75 patients were randomized to a music-based intervention (n = 33) or control (n = 42) group. Patients in the music-based intervention group consumed 56.7% less opioids than those in the control group (AUC was 2.8 in the music-based intervention group vs. 6.4 in the control group, absolute standardized mean difference (aSMD) = 0.34 (−0.17, 0.85)). No difference in pain scores was recorded between groups. Music-based intervention also reduced anxiety on postoperative day (POD)2 (aSMD = 0.38 (−0.16, 0.91)), depression on POD2 (aSMD = 0.31 (−0.23, 0.84)) and POD4 (aSMD = 0.24 (−0.29, 0.77)), and pain catastrophizing on POD1 (aSMD = 0.24 (−0.3, 0.77)). Conclusions: Our data support the use of music-based intervention to reduce postoperative opioid requirements. Music-based intervention may also reduce anxiety, depression, and pain catastrophizing.
Keywords: music-based intervention, anxiety, depression, catastrophizing, ambulatory surgery
1. Introduction
Up to 50% of patients report experiencing a certain degree of anxiety, depression, or catastrophizing before surgery [1], and up to 80% report pain after surgery [2]. Furthermore, the presence of mood disorders, especially anxiety, has been established as a factor leading to increased postoperative pain and opioid consumption [3,4,5,6,7,8].
In surgical patients, inappropriate management of postoperative pain has been associated with several unfavorable outcomes, including increased morbidity, the development of chronic pain, delayed surgical recovery, and persistence of opioid consumption and opioid use disorder [9]. The current recommended approach to perioperative pain management is multimodal analgesia, which includes non-steroidal anti-inflammatory drugs, acetaminophen, regional nerve blocks, and opioids [10]. A study of 36,177 adults in the US in 2017 reported an approximate 6% incidence of new persistent opioid use after minor and major surgeries. The same study identified anxiety as a significant risk factor [11]. Therefore, considerations have been given to the use of nonpharmacological complementary approaches as a way to control preoperative mood disorders and therefore improve pain control [12,13,14,15,16,17,18,19].
Among nonpharmacologic approaches to the perioperative management of pain and mood disorders, music-based intervention is a method that could be particularly valuable in health care, as it is inexpensive, has no known side effects, and does not require patients to have previous formal experience with music. Music-based interventions are used in health care to help reach various health-promoting goals and are provided by certified music therapists, health care professionals, musicians, and others. Music-based interventions where patients listen to pre-recorded music are a passive method often used by music therapists to relax a patient, regulate activity and tension, and positively influence the patient’s mood and motivation. This is why a licensed music therapist is needed to effectively establish a therapeutic relationship between the music and the patient, while also preventing side effects like anxiety. The current literature suggests that music-based intervention is an effective approach to controlling pain and anxiety [16,20,21,22,23,24,25,26]. Although a meta-analysis reported positive effects of music-based intervention, the high degree of heterogeneity in study designs has led to inconsistent conclusions.
Our study was designed to examine the impact of music-based intervention administered before, during, and after surgery on postoperative opioid consumption and pain levels, as well as preoperative anxiety, depression, and pain catastrophizing. This study also evaluated patient satisfaction and recovery outcomes. We hypothesized that, compared to a control group (standard of care), the use of music-based intervention would be effective in reducing opioid consumption in patients with preoperative anxiety and that a correlation exists between opioid consumption and anxiety.
2. Materials and Methods
2.1. Study Design and Participants
This study was a single-center, prospective, single-blinded, randomized controlled trial. Before subject recruitment was initiated, the study protocol was reviewed and approved by the University of Pittsburgh Institutional Review Board (STUDY21110130) and registered at clinicaltrials.gov (NCT05263635).
The inclusion criteria were patients having same-day surgery including breast surgeries, open inguinal hernia repairs, and laparoscopic or robotic surgeries. The patients received a single nerve block and underwent either general anesthesia or monitored anesthesia care. The patients’ ages ranged from 18 to 80 years old; their American Society of Anesthesiologists (ASA) physical statuses were I, II, or III; and they presented moderate anxiety (PROMIS Anxiety Short Form 8 questionnaire T scores ≥ 57.4 and ≤74.1).
The exclusion criteria were ASA physical status IV, use of spinal anesthesia, significant anxiety with PROMIS Anxiety Short Form 8 T-score of <57.4 or higher than 74.1, preoperative chronic use of opioids, and history of drug or alcohol abuse.
2.2. Enrollment Procedures
In the same-day surgery unit, a trained research coordinator approached patients who met the eligibility criteria at least two hours before surgery. Patients interested in participating were asked to sign a HIPAA-compliant informed consent document. After providing written informed consent, each patient was asked to complete the PROMIS Anxiety Short Form 8 questionnaire. Patients with mild to moderate anxiety (T-scores ≥ 57.4 and ≤74.1) [27] were randomized to either a group who would receive music-based intervention or a control group (no music-based intervention) using a computer-generated randomization scheduled. Baseline data before randomization also included medical history, pain rated using a verbal scale (0 = no pain to 10 = the worst possible pain), and pain medication use (including opioids). In addition, each patient was also asked to complete PROMIS Emotional Distress–Depression Short Form 8 (PROMIS Depression) and a Pain Catastrophizing Scale questionnaire [28].
Computer-generated, blocked randomization was performed with a 1:1 allocation ratio. Information about the allocation was stored in opaque envelopes.
2.3. Music-Based Intervention
The music-based intervention was developed by a certified music therapist (license registered by the medical board of Pennsylvania) and was based on flowing rhythm approximately 60–80 beats/minute, and was played by string instruments [29,30]. Each patient was offered to choose between classical, jazz, piano, guitar, or lo-fi music (music with a laid-back and chilled-out vibe). Lo-fi music often features slow tempos, simple melodies, and a repetitive nature that allows the listener to relax and unwind. Lo-fi music also heavily relies on the use of samples, particularly from vinyl records, to create its signature sound (examples can be found at soundscapehq.com). The music included in each category is listed in Appendix A. An MP3 player connected to headphones played the music-based intervention at a volume of approximately 45 decibels during three sessions: in the preoperative area, immediately following induction of anesthesia in the operating room, and in the post-anesthesia care unit (when subjects were awake and responsive).
2.4. Anesthesia
Surgery was performed under sedation (breast surgery, inguinal hernia repair) or general anesthesia. Prior to surgery, peripheral nerve blocks were performed, either a paravertebral nerve block in patients undergoing breast surgery [31,32] or quadratus lumborum approach (QL 2) in patients undergoing abdominal surgery [33]. The nerve blocks were performed prior to surgery in the same surgery units by a member of the acute interventional pain service. Furthermore, no opioids were administered prior to anesthesia and surgery.
2.5. Follow-Up
In the recovery room, postoperative pain level, analgesics, nausea, and vomiting were recorded until discharge. Prior to discharge, each patient was also asked to complete satisfaction questionnaires. After discharge, each patient was asked to complete questionnaires and report mood symptoms and medication use daily for the first five postoperative days (PODs). Specifically, they were instructed to fill out the PROMIS Anxiety, PROMIS Depression, and PCS surveys and record their levels of pain, anxiety, and pain medication use over the previous 24 h. Research electronic data capture (REDCap) was used to collect all the information.
2.6. Outcome Measurements
The primary end point was opioid consumption. Secondary end points included PROMIS Anxiety, PROMIS Depression, PROMIS sleep interference, and pain catastrophizing scores; pain and opioid consumption on PODs 1, 2, 3, 4, and 5; total opioid consumption over the first 30 days; incidence of postoperative nausea and vomiting (PONV); time of hospital discharge; and patient satisfaction scores (0 = totally unsatisfied to 10 = completely satisfied).
2.7. Statistical Analysis
Descriptive statistics were calculated using means and standard deviations for continuous data and counts and percentages for categorical data. Non-normal continuous data were described using medians and interquartile ranges. Differences between treatment groups prior to starting the treatment were tested on continuous data using T-tests and Mann–Whitney U tests, and categorical differences using Chi-squared tests and Fisher’s exact tests. Missing values were removed from all denominators and statistical testing. p values < 0.05 were considered significant.
Differences between means of the treatment vs. the control group were assessed using the absolute standardized mean difference (aSMD). An aSMD ≥ 0.2 indicates that the standardized means of these two groups are different [33,34]. R software (version 4.3.1, R Core Team, 2023) was used for data management and analysis. The TOSTER package was used to calculate SMDs, DescTools was used to calculate AUCs, and halfmoon was used to construct love plots.
The primary outcome was postoperative (POD) oral morphine equivalents (OMEs) over 5 days following surgery by calculating area under the curves (AUCs) using the trapezoid method. Power analysis indicated that 30 patients per group were required to establish a difference of 30% between the groups. Percent differences of medians and aSMDs were calculated to compare between-group differences. Love plots over time were created to visualize aSMDs over PODs. Secondary outcomes included pain over 5 days following surgery by calculating area under the curves (AUCs) using the trapezoid method, postoperative opioid consumption on POD 1–5, patient’s satisfaction surveys, postoperative length of stay, and level of nausea were compared using aSMDs and percentage differences of medians. Spearman correlations were calculated between total OME in the postoperative period in the hospital, and depression, pain catastrophizing, and anxiety on each POD.
aSMDs ≥ 0.2 were considered our lower bound of effect sizes [34,35]. R software (version 4.3.1, R Core Team, 2023) was used for data management and analysis. The TOSTER package was used to calculate SMDs, DescTools was used to calculate AUCs, and halfmoon was used to construct love plots.
3. Results
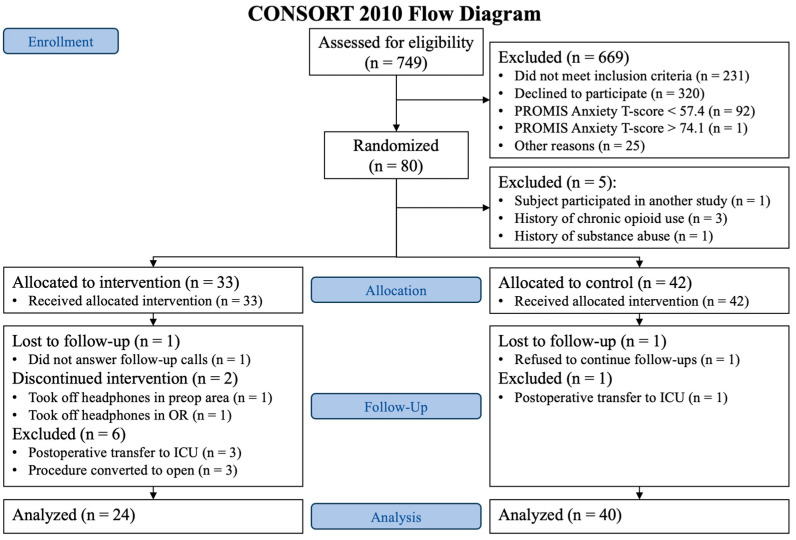
A total of 749 patients were screened from May 2022 to August 2023. We found 493 patients to be eligible; 173 gave informed consent, and 93 patients were considered screen failures because their PROMIS Anxiety T-scores were <57.4 or >74.1. Consequently, 80 patients were randomized. After randomization, five patients were found to be ineligible and removed from the final analysis: one patient participated in another study, one patient had a history of substance abuse, and three patients had a history of chronic opioid use. Out of the 75 remaining patients, 33 were randomized to the music-based intervention group and 42 to the control group. During the follow-up phase in the music-based intervention group, one patient was lost to follow-up, two patients withdrew from the study, and six were excluded due to postoperative transfer to the intensive care unit (ICU) and having their procedure converted from laparoscopic to open. In the control group, one patient was lost to follow-up, and one patient was transferred to the ICU after surgery (Figure 1).
Figure 1.
CONSORT flow diagram.
Table 1 presents patients’ demographics, including age, sex, race, ethnicity, weight, height, body mass index, baseline PROMIS Anxiety, PROMIS Depression, and PCS scores, type of music being played, and the percentage of patients who filled their opioid prescription overall and in each group. These data indicated no observed statistical differences among groups at baseline.
Table 1.
Baseline characteristics of study participants.
| Variable | Total (n = 64) |
Control (n = 40) |
Treatment (n = 24) |
p Value | |
|---|---|---|---|---|---|
| Age, median (IQR) | 54 (42.25–63) | 56 (42.2–61.2) | 49.5 (41.5–66.2) | 0.961 | |
| Sex, No. (%) | 0.778 | ||||
| Female | 45 (70.3%) | 29 (72%) | 16 (67%) | ||
| Male | 19 (29.7%) | 11 (28%) | 8 (33%) | ||
| Race, No. (%) | 0.109 | ||||
| Asian | 3 (4.7%) | 0 (0%) | 3 (12%) | ||
| Black or African American | 11 (17.2%) | 7 (18%) | 4 (17%) | ||
| White | 48 (75%) | 31 (78%) | 17 (71%) | ||
| Other, not specified | 2 (3.1%) | 2 (5%) | 0 (0%) | ||
| Hispanic, No. (%) | 0.137 | ||||
| No | 61 (95.3%) | 39 (98%) | 22 (92%) | ||
| Yes | 2 (3.1%) | 0 (0%) | 2 (8%) | ||
| Not specified | 1 (1.6%) | 1 (2%) | 0 (0%) | ||
| Weight, median (95% CI) in kg | 79.5 (67.5–98) | 84 (67.5–99.5) | 76 (67.7–97.7) | 0.608 | |
| Height, median (95% CI) in cm | 169 (160–175) | 170 (160–175.1) | 168 (159.4–173) | 0.404 | |
| BMI, median in kg/m2 (95% CIU in kg/m2) | 28.6 (24.8–33.5) | 29.2 (24.6–33.8) | 27.9 (52.2–32.9) | 0.906 | |
| Music genre, No. (%) | |||||
| Classical | 3 (4.7%) | 3 (12%) | |||
| Guitar | 8 (12.5%) | 8 (33%) | |||
| Jazz | 9 (14.1%) | 9 (38%) | |||
| Lo-Fi | 2 (3.1%) | 2 (8%) | |||
| Piano | 2 (3.1%) | 2 (8%) | |||
| Opioid prescriptions filled, No. (%) | |||||
| No | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Yes | 33 (100%) | 21 (100%) | 12 (100%) | ||
| Baseline PROMIS Anxiety T-score, median (95% CI) | 62.5 (59.4–66.6) | 62.5 (59.4–64.8) | 63.5 (59.4–69) | 0.452 | |
| Baseline PROMIS Depression T-score, median (95% CI | 53.85 (49.8–57.9) | 54.3 (49.8–57.9) | 53.4 (50.9–57.5) | 0.945 | |
| Baseline PCS score, median (95% CI) | 14 (6.75–21.25) | 16 (8–21.2) | 12.5 (4–21.2) | 0.532 | |
CI (confident interval); BMI—body mass index; PCS—Pain Catastrophizing
Table 2 presents the types of surgery performed on patients included in the study. There were no observed significant differences between the two groups.
Table 2.
Types of surgical interventions among study participants.
| Type of Surgery | Total (n = 64) |
Control (n = 40) |
Treatment (n = 24) |
p Value |
|---|---|---|---|---|
| Mastectomy | 9 (14.1%) | 5 (12.5%) | 4 (16.7%) | 0.953 |
| Breast reconstruction | 17 (26.6%) | 12 (30%) | 5 (20.8%) | |
| Breast fat graft | 2 (3.1%) | 1 (2.5%) | 1 (4.2%) | |
| Laparoscopic prostatectomy | 12 (18.8%) | 7 (17.5%) | 5 (20.8%) | |
| Laparoscopic cholecystectomy | 15 (23.4%) | 10 (25%) | 5 (20.8%) | |
| Laparoscopic appendectomy | 3 (4.7%) | 2 (5%) | 1 (4.2%) | |
| Robotic inguinal hernia repair | 3 (4.7%) | 2 (5%) | 1 (4.2%) | |
| Other laparoscopic procedures | 3 (4.7%) | 1 (2.5%) | 2 (8.3%) |
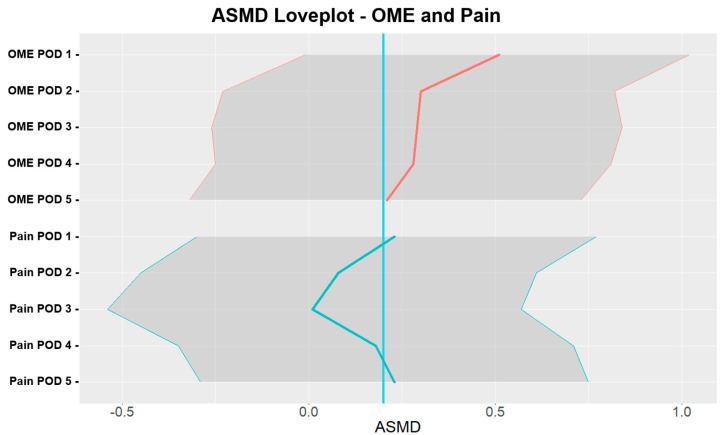
Primary end point: As presented in Table 3 and Figure 2, patients in the intervention music therapy group consumed 56.7% less opioids than those in the control group (median 2.8 in intervention music therapy group vs. 6.4 control group, aSMD = 0.34; 95% confidence interval (CI) = (−0.17, 0.85)). While the estimated aSMD displayed an effect size ≥ 0.2, we noted that the CI contained zero. The greatest difference in opioid consumption was recorded on POD1 (0.51, (−0.01, 1.02)) and decreased after that. On POD5, opioid aSMD was 0.21 (−0.32, 0.73).
Table 3.
Pain score and opioid consumption AUC in the intervention music therapy group vs. those in the control group.
| Variable | Control (n = 40) |
Treatment (n = 24) |
% Difference | aSMD (95% CI) |
|---|---|---|---|---|
| Pain score Median AUC for POD 1–5 |
12.5 | 13.0 | 4% | 0.12 (−0.4, 0.64) |
| Opioid use in OME Median AUC for POD 1–5 |
6.4 | 2.8 | −56.7% | 0.34 * (−0.17, 0.85) |
aSMD—absolute standardized mean difference; AUC—area under the curve; CI—confidence interval; OME—oral morphine equivalent; POD—postoperative day; * aSMD ≥ 0.2.
Figure 2.
aSMD love plot for OME and pain in the intervention music therapy group vs. the control group. aSMD—absolute standardized mean difference; OME—oral morphine equivalent; POD—postoperative day. The blue line represents a reference for aSMD = 0.2.
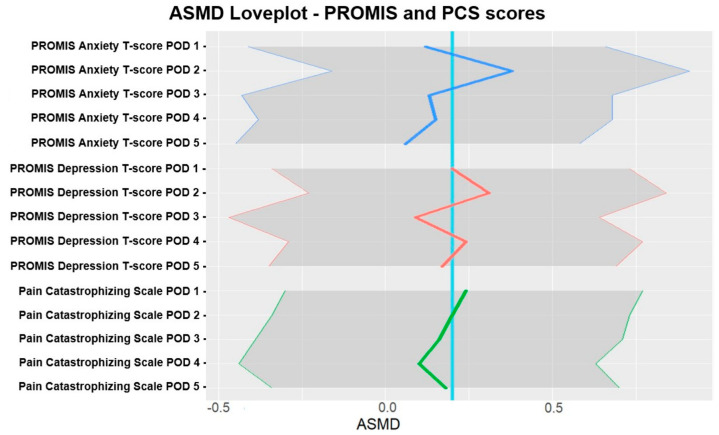
Secondary end point: The greatest difference in opioid consumption was recorded on POD1 (0.51, (−0.01, 1.02)) and decreased after that. On POD5, opioid aSMD was 0.21 (−0.32, 0.73). Pain scores using AUCs from POD1 and POD5 showed no difference between the groups (13.0 vs. 12.5; 0.12 (−0.4, 0.64)). Furthermore, our data demonstrated fluctuating effects of intervention music therapy on anxiety (POD2 0.38 (−0.16, 0.91)), depression (POD2 0.31 (−0.23, 0.84) and POD4 0.24 (−0.29, 0.77)), and pain catastrophizing (POD1 0.24 (−0.3, 0.77)). Table 4 presents the frequency of PONV, satisfaction scores, and length of hospital stay. aSMD sizes were small for satisfaction scores, frequency of PONV, and length of hospital stay (3.6 vs. 4.1 h; 0.11 (−0.4, 0.62)). Correlations between total post-op OME, depression, pain catastrophizing, and anxiety were negligible, with an absolute upper bound of 0.12.
Table 4.
Secondary outcome measures in the intervention music therapy group vs. the control group.
| Variable | Control (n = 40) |
Treatment (n = 24) |
% Difference | aSMD (95% CI) |
|---|---|---|---|---|
| Satisfaction questionnaire score, median 95% CI)) | 10 (10–10) | 10 (10–10) | 0% | 0.05 (−0.48, 0.58) |
| Time to hospital discharge, median in hours (95% CI) | 4.1 (2.8–6.7) | 3.6 (2.9–6) | −11.3% | 0.11 (−0.4, 0.62) |
| Level of nausea, median (95% CI | 0 (0–0) | 0 (0–0) | - | 0.22 (−0.29, 0.73) |
aSMD—absolute standardized mean difference; CI—confidence interval.
Figure 3 presents the difference in PROMIS Anxiety, PROMIS Depression, and PCS scores over five days based on aSMD and pain catastrophizing.
Figure 3.
aSMD love plot for PROMIS and PCS scores in the intervention music therapy group vs. the control group. aSMD—absolute standardized mean difference; POD—postoperative day; PCS—Pain Catastrophizing Scale. The blue line represents a reference for aSMD = 0.2.
Table 4 presents the frequency of PONV, satisfaction scores, and length of hospital stay. aSMD sizes indicated no difference between the group for satisfaction scores, frequency of PONV, and length of hospital stay (3.6 vs. 4.1 h; 0.11 (−0.4, 0.62)). Finally, correlations between total post-op OME, depression, pain catastrophizing, and anxiety were negligible, with an absolute upper bound of 0.12.
4. Discussion
In contrast to other published studies [16,20,21,22,23,24,25,26,27,28], our study focused on the potential benefits of music-based intervention in patients with anxiety prior to surgery. Our data indicates that 46% of the patients included in this study had anxiety scores within the inclusion criteria. This finding is within the percentage of preoperative anxiety reported by Friedrich. In this context, females have been found to have higher levels of preoperative anxiety [36].
Our data suggest that music-based intervention may be an effective technique to reduce opioid requirements in patients undergoing minor surgery. Total opioid consumption for patients in the music-based intervention group was 56.7% lower than that for patients in the control group. The effect was the highest on POD1. Our data also suggest that by POD5, the difference between the groups was minimal (Figure 2), suggesting that in the context of our protocol (administrating music-based intervention prior to, during, and immediately after surgery), the effects of music-based intervention lasted four days. This short-lasting effect of music-based intervention may also be due to the fact that the role of music-based intervention was studied in patients undergoing minor surgery, where pain is expected to last no more than three to four days. [37]. Furthermore, while the aSMD indicated a noteworthy effect of 0.34, the associated 95% CIs (−0.17, 0.85) showed a large difference between the individual effects of music-based intervention on opioid consumption. Postoperative opioid consumption is multifactorial, including not only pain associated with the surgery, but also individual factors such as anxiety, depression, and catastrophizing.
The music protocol used in this study was developed by a licensed music therapist. Patients in this study were offered a choice of classical, jazz, piano, guitar, and lo-fi music. Our protocol is a significant deviation from those in other published studies on the use of music-based intervention in surgical patients. While it is uncertain whether our approach should serve as a reference for future studies, theoretically, involving a certified music therapist could enhance the benefits of music-based intervention in surgical patients.
Music-based intervention has been used in patients undergoing several types of surgery, including ambulatory and inpatient surgery, cancer and cardiac surgery, and total hip, knee, and shoulder arthroplasty. In most cases, music-based intervention has been administered after surgery to treat anxiety and depression and, in a limited number of cases, to reduce post-surgical pain. Juhl et al. (2019) [38] suggested that the mechanism of action of music-based intervention is multifactorial (cognitive function, emotion, and neurobiology). Our data provide additional evidence that music-based intervention is an interesting technique to not only decrease the anxiety and depression associated with surgery, but also decrease opioid requirements in the first five days following surgery. In our study, however, music-based intervention had minimal effects on pain.
Despite the reduction in opioid consumption, there was a lack of differences between the medians of the pain scores, most likely related to the intrinsic variability of the pain scores within each group that is reflected by the large aSMD 95% CI (−0.4, 0.64) and the relatively limited extent of the surgeries that were performed. Although we reported a reduction in both pain levels and postoperative opioid consumption associated with the use of aromatherapy and the NeuroCuple™ device [13,15], this absence of correlation between pain and total opioid consumption can be seen in other studies [39,40]. This absence of correlation might also be related to the temporal independence between the opioid intake and pain level recorded each day.
Secondary outcomes, including patient satisfaction, length of hospital stay, and PONV, were not substantially different between the groups. While music-based intervention may improve some aspects of recovery (such as reducing opioid consumption), it may not be sufficient to influence the overall length of hospital stay or PONV. Other factors, such as type of surgery, type of anesthesia, and the patient’s medical history, may be more determinant factors controlling these outcomes.
Our data suggest that music-based intervention reduced anxiety on POD2, depression on POD2 and POD4, and pain catastrophizing on POD1. While music-based intervention can provide temporary relief, it might be insufficient to consistently affect the emotional and cognitive aspects of these parameters during POD1-POD5, or PROMIS/PCS questionnaires are not designed to capture short-term mood changes. As for depression, the inconsistent effects could also be attributed to the low baseline scores in both treatment groups, showing no further decrease in already low scores.
Several limitations should be noted in our study. First, the sample size was relatively small, which may limit the generalizability of the findings. Second, although each patient was allowed to choose between five playlists with music from various genres, the researcher-selected music may not have covered the type of music preferred by a given patient. Lastly, the unequal distribution of patients between the placebo and the treatment groups may have affected the recorded overall responses between the groups.
Dang et al. [16] reported that the benefits of a combination of aromatherapy and music-based intervention were not greater than the benefits of either therapy alone. This suggests that before adding a combination of complementary techniques to a postoperative protocol to manage anxiety and depression in surgical patients, it is necessary to establish the benefit of that combination. This applies to the use of psychoeducation programs [41,42], acupuncture [43], auriculotherapy [44,45], hypnosis [46], virtual reality [47], aromatherapy [13], nanotechnology [15], and other potential complementary techniques, especially when the technique involves significant training, time, and cost, such as with acupuncture, auriculotherapy, and biofeedback.
In contrast to other published studies [16,20,21,22,23,24,25,26,27,28], our study focused on the potential benefits of music-based intervention in patients with anxiety prior to surgery. Our data indicate that 46% of patients in this study presented anxiety scores within the inclusion criteria. In this context, females have been found to have lower levels of preoperative anxiety [48].
Our study contributes to the growing body of evidence supporting the integration of music-based intervention into perioperative care protocols. Cost-effectiveness and ease of implementation make music-based intervention an attractive option for enhancing patient outcomes. However, variability in the observed effects highlights the need for further research to identify the patient populations that may benefit the most from this intervention.
5. Conclusions
Our study provides evidence to support the effectiveness of music-based intervention as a nonpharmacologic technique to reduce opioid consumption in the postoperative period. There was also a temporary effect on mood disorders. Future studies are necessary to confirm this concept. Further studies should include a larger sample size, assess whether or not music-based intervention should extend beyond the immediate perioperative period, and be applicable to surgeries beyond minor surgeries.
Acknowledgments
The authors would like to acknowledge Christine Burr for editing this manuscript and Jasmin Brown for her administrative assistance.
Appendix A
Table A1.
Music by type (N/A = not available).
| Genre | Song | Composer | Artist |
|---|---|---|---|
| CLASSICAL | Piano Concerto No. 5 in E-Flat Major, Op. 73 | Ludwig van Beethoven | Vienna Philharmonic |
| The Four Seasons Winter, op. 8/4, II Largo | Antonio Vivaldi | Stuttgart Chamber Orchestra | |
| Piano Concerto No 21 in C Major, K. 467 | Wolfgang Amadeus Mozart | Numberg Symphony Orchestra | |
| Romance for Violin and Orchestra in F Major, Op 50 | Ludwig van Beethoven | Badische Staatskapelle | |
| Suite for Orchestra No. 3 in D Major | Johann Sebastian Bach | Mainz Chamber Orchestra | |
| L’estro Armonico No. 8 in A minor, Op. 3 | Antonio Vivaldi | Stuttgart Chamber Orchestra | |
| Andagio for Strings (from Strings Quartet, Op 11) | Samuel Barber | New Zealand Symphony Orchestra | |
| Ellen’s Song III (“Ave Maria”), D. 839 (Op 52/6) | Franz Schubert | Aaron Rosand & Eileen Flissier | |
| Symphony No..6 in B Minor, Op. 74 | Pyotr Ilyich Tchaikovsky | Slovak Philharmonic Orchestra | |
| Symphony No. 6 in F Major, Op 68 | Ludwig van Beethoven | London Symphony Orchestra | |
| Piano Concerto No. 2 in C Minor, Op 18 | Sergei Rachmaninoff | Moscow RTV | |
| Piano Concerto No. 1 in E minor, Op 11 | Frederic Chopin | Hamburg Symphony Orchestra | |
| Violin Concerto in D Major, Op 35 | Pyotr Ilyich Tchaikovsky | Orchestra of Radio Luxemburg | |
| Violin Concerto in D Minor for 2 Violins and Orchestra | Johann Sebastian Bach | Mainz Chamber Orchestra | |
| Symphony No 5 in C-Sharp Minor: IV. Adagietto | Gustav Mahler | London Symphony Orchestra | |
| Songs Without Words, Op 62: Spring Song | Felix Mendelssohn | Hans Kalafusz & Klaus von Wildemann | |
| Concerto No. 20 in D Minor for Piano and Orchestra | Wolfgang Amadeus Mozart | Berlin Symphony Orchestra | |
| Concerto No. 3 in G Major for Violin and Orchestra | Wolfgang Amadeus Mozart | Dalibor Brazda | |
| Carnival of the Animals: XIII The Swan | Camille Saint-Saens | Stockholm Chamber Duo | |
| Thais Meditation (Andante Religioso) | Jules Massenet | Royal Philharmonic Orchestra | |
| String Quartet No 2 in D Major: Notturno | Alexander Borodin | Lucerne String Quartet | |
| Holberg Suite in G Major, Op 40: Sarabande | Edvard Grieg | Slovak Philharmonic Orchestra | |
| Suite Bergamasque, L 75: Clair de lune | Claude Debussy | Mostar Symphony Orchestra | |
| PIANO | Suite Bergamasque: III. Clair de Lune | Claude Debussy | Peter Frankl |
| Reverie, for Piano, L. 68 | Claude Debussy | Peter Frankl | |
| Scenes from childhood, Op 15: VII Traumerei | Robert Schumann | Peter Schmalfuss | |
| 12 Etudes, Op. 10: No. 3 in E major | Frederic Chopin | Abbey Simon | |
| Piano Concerto No 2 in C Minor, Op 18 | Sergei Rachmaninoff | Moscow RTV | |
| Piano Concerto No 1 in E Minor, Op. 11 | Frederic Chopin | Hamburg Symphony Orchestra | |
| Piano Concerto No. 5 in E-Flat Major, Op. 73 | Ludwig van Beethoven | Vienna Philharmonic | |
| 3 Gymnopedies: Gymnopedie No 1 | Erik Satie | Frank Glazer | |
| Melodies for Piano, Op 3: No 1 Melody In F | Anton Rubinstein | Michael Ponti | |
| Waltzes, Op 39: No. 15 in A major | Johannes Brahms | Alfred Bredela dn Walter Klien | |
| Sonata for piano No. 12 in F Major, K 332 | Wolfgang Amadeus Mozart | Carmen Piazzini | |
| Nocturnes, Op. 27, No. 2 in D-flat major | Frederic Chopin | Abby Simon | |
| Concerto No. 20 in D Minor for Piano and Orchestra | Wolfgang Amadeus Mozart | Berlin Symphony | |
| 12 Preludes, Book 1, L 117 | Claude Debussy | Peter Schmalfuss | |
| Trois Gymnopedies: Gynopedie No. 1 | Erik Satie | Frank Glazer | |
| Aria and 30 Variations | Johann Sebastain Bach | Henrik Mawe | |
| Amazing Grace | John Newton William Walker | Relaxing Piano | |
| Sekai no Shazo kara | Nakamura Hachidai | Relaxing Piano | |
| Amaratine | Enya Roma Ryan | Relaxing Piano | |
| Music Room After School | Gonititi Masayo | Relaxing Piano | |
| My Favorite Things/Sound of Music | Rodgers Hammerstein | Relaxing Piano | |
| Give Me a Wing | Kunihiko Murai | Relaxing Piano | |
| Reprise/Spirited Away | Joe Hisaishi | Relaxing Piano | |
| ALWAYS—Sunset on Third Street | Naoki Sato | Relaxing Piano | |
| You Raise Me Up | Brendan Graham Rolf Lovland | Relaxing Piano | |
| Comme au Premier Jour | Ande Gagnon Doug Gamely | Relaxing Piano | |
| Etupirka | Taro Hakase | Relaxing Piano | |
| TAKUMI | Masa Takumi | Relaxing Piano | |
| KAZABUE | Michiru Oshima | Relaxing Piano | |
| JIN—Main Title | Yuu Takami | Relaxing Piano | |
| Let It Go/Frozen | Kristen Anderson Lopez Robert Lopez | Relaxing Piano | |
| Nuovo Cinema Paradiso Tema D’Amore | Andrea Morricone Ennio Morricone | Relaxing Piano | |
| Merry Christmas Mr. Lawrence | Ryuichi Sakomoto | Relaxing Piano | |
| Kaze no Uta | Toshihiko Sahashi | Relaxing Piano | |
| Flowers Will Bloom | Yoko Kanno | Relaxing Piano | |
| Time to Say Good-Bye | Francesco Sartori. Lyricist: Frank Peterson. Lucio Quarantotto | Relaxing Piano | |
| Lost | Jacky Terrasson | Wallace Roney | |
| GUITAR | Gymnopedie No. 1 | Erik Satie | Robert Lunn |
| Clair de Lune | Claude Debussy | Tariq Harb | |
| Cannon in D | Johann Pachelbel | Ines Thome | |
| Gymnopedie No. 3 | Erik Satie | Micharl Christian Durrant | |
| Jeux Interdits (Forbidden Games) | Narciso Yepes | Paco Hernandes | |
| Guitar Concerto de Aranjuez Rodrigo | Joaguin Rodrigo | Julian Bream | |
| Air Jean Baptiste Lully | Jean Lully | Richard Mollenbeek | |
| Pavane Faure | N/A | Pablo Segovia Gardel | |
| Cavatina (Deer Hunter Theme) | Stanky Myers | Mason Wilson | |
| Summertime | Gershwin Heywaard Kuhns | Julio Deranjo | |
| Dance of the Miller | Manuelde Falla | Juan Iniesta | |
| Gran Vals | Francisco Tarrega | Hegovia Juanrez | |
| Una Furtiva Lagrima | Gaetano Donizetti | Pablo Segovia Gardel | |
| Gymnpedie | Erik Satie | Francisco Tores | |
| Malaguena | Ernesto Lecuona | Gypsy Queens | |
| El Mariachi (Once Upon a time in Mexico) | Robert Rodriguez | Leo Sanchez | |
| Moonlight Sonata | Beethoven | Rodrigo Escoba | |
| Valse Criollo | Antonio Lauro | Neo Yepes | |
| Bolero | Ravel | Gipsy Rayes | |
| Granada (Suite Espanola) | Isaac Albeniz | Ricardo Juarez | |
| Prelude, No. 5 | Heitor Villa Lobos | Rodrigo Escoba | |
| Albinoni arr Giazotto: Adagio in G Minor | Tsomaso Albinoni & Remo Giazotto | Dominic Miller, Budapest Film Orchestra | |
| Myers: Cavatina (The Deer Hunter) | Stanley Myers | Goran Sollscher | |
| Guitar Concerto in D—Largo | Antonio Vivaldi | Eduardo Fernandez | |
| Cello Suite No. 1—Prelude | Johann Sebastian Bach | John Williams | |
| Apres un reve | Gabriel Faure | Steve Erquiaga | |
| Pavane pour une infante defunte | Maurice Ravel | Steve Erquiaga | |
| Cello Suite No. 3—Courante | Johann Sebastian Bach | Pepe Romero | |
| Castillos de Espana—Torija | Federico Moreno torroba | Andres Segovia | |
| Prelude No. 1 | Heitor Villa-Lobos | Julian Bream | |
| Andaluza | Enrique Granados | Pepe Romero & Celine Romero | |
| Suite espanola—Granada | Isaac Albeniz | Pepe Romero | |
| Bachianas brasileiras No. 5, W. 389 | Heitor Villa-Lobos | Aleandre Lagoya | |
| Cello Concerto No.6 Andante | Luigi Boccherini | Andres Segovia | |
| 2 Temas Populares Cubanos | Leo Brouwer | Eduardo Fernandez | |
| Cantana No 156—Arioso | Johann Sebastian Bach | Steve Erquiaga | |
| Romane d’amour | Anonymous | goran Sollscher | |
| Mass in B Minor—Qui Tollis | Johann Sebastian Bach | Dominic Miller, Budapest Film Orchestra | |
| Twin Peaks Theme | Angelo Badalamenti | Henrik Janson | |
| Mad World | Roland Orzabal | Sergei Baronin | |
| Be Over Ay | Shazam Footer | John Hanks | |
| Cornfield Chase | Hans Zimmer Alex Gibson | Moldoni | |
| Chi Mai | Ennio Morricon | Henrik Janson | |
| Bibo No Aozora | Ryichi Sakomoto | Henrik Janson | |
| Memories (Top Gun) | Harold Falter-Meyer | Christopher Varela | |
| Deep Forest | Omar Franco Varela | Christopher Varela | |
| Adagio | Henrik Janson | Richard Mollenbeck | |
| Gymnopedie | Erik Satie | Richard Mollenbeck | |
| Hills and Horizons | Evans, Rolls, Leslie and Barlow | John Hanks | |
| Lost and Found | William Puchot | John Hanks | |
| Pavane, Op. 50 | Fauve | Marcel Dopuis | |
| New Moon (The Meadow) | Alexandre Desplat | Miranda Boumedin | |
| Ave Nocturne | John Field | John A. Nilson | |
| Theme from Schindler’s List | John Williams | Moldoni | |
| Pathetique Sonata | Beethoven | Marcel Dopuis | |
| Air on a G String | J. S. Bach | Richard Mollenbeck | |
| Carrousel | Rogers/Hammerstein | N/A John A. Nilson | |
| In Trutina | Carl Orff | Marcel Dopuis | |
| May it Be | Enya/Ryan | Sergei Baronin | |
| Sweden | Getz/Hallberg | Sergei Baronin | |
| River Flows in You | Yiruma | Miranda Boumedin | |
| In My Spanish Hacienda | Rodrigo | Sergio Miguel | |
| The Ludlows | J. Horner | Christopher Varela | |
| Vivaldino | A. Carrilho | John A. Nilson | |
| Braids | Paterson | Enrico Carmona | |
| Transformation | E Menken | Enrico Carmona | |
| JAZZ | Movement I, Pt. I | Bob Belden and Suzanne Severini | Classical Jazz Quartet |
| Movement I, Pt. III | Bob Belden and Suzanne Severini | Classical Jazz Quartet | |
| Movement I, Pt. IV | Bob Belden and Suzanne Severini | Classical Jazz Quartet | |
| Movement II, Pt. II | Bob Belden and Suzanne Severini | Classical Jazz Quartet | |
| Round Midnight | Thelonious Monk and Cootie Williams | Hank Jones | |
| Yesterdays | Jerome Kern Otto Harbach | Larry Coryell | |
| Into the Shadows | John Fedchock | James Moody | |
| Second Time Around | Sammy Cahn-Jimmy Van Heusen | Donald Brown | |
| Yvette | Gigi Gryce | Darrell Grant | |
| Sunny | Bobby Hebb | Les McCann | |
| Sweet & Lovely | Gus Arnheim, Charles N. Daniels and Harry Tobias | Sonny Stitt | |
| A Flower | Kenny Barron | Kenny Barron | |
| My Man’s Gone Now | George Gershwin DuBose Heyward | Mulgrew Miller | |
| When You Wish Upon a Star | Leigh Harline Ned Washington | Eliane Elias | |
| Nature Boy | Eden Ahbez | The Drummonds | |
| This Guy’s In Love with You | Burt Bacharach Hal David | Cedar Walton | |
| Lover Man | Jimmy Davis, Roger Ramirez, James Sherman. | Sonny Stitt | |
| You Better Go Now | Irvin Graham Bix Reichwer | Red Garland | |
| Willow Weep For Me | Ann Ronel | Cannonball Adderley | |
| Love Walked In | George Gershwin | Errol Garner | |
| Summertime | George Gershwin | Duke Jordan | |
| Moonlight in Vermont | John Blackburn Karl Suexxdorf | Marian McPartland | |
| When Darkeness Falls | George Shearing | George Shearing | |
| Solace | S. Joplin | Billy Taylor | |
| Softly as in a Morning Sunrise | Romberg/Hammerstein | The modern Jazz Quartet | |
| Blue in Green | Davis/Evans | Miles Davis | |
| Flamenco Sketches | Davis/Evans | Miles Davis | |
| Fran-Dance | Davis | Miles Davis | |
| Stella By Starlight | Young/Washington | Miles Davis | |
| The Waking Hours | A. Holzwarth | Jeff Bailey | |
| Sweet Sadness | Clary/Bottini | Jeff Bailey | |
| The Only One for Me | McKnight | Jeff Bailey | |
| Precious Few | Kent | Jeff Bailey | |
| Beauty Marks | S. Grey | Jeff Bailey | |
| Make Believe Waltz | Morse/Drislane | Jeff Bailey | |
| Memories | E. Blake | Jeff Bailey | |
| In This Place | T. Thompson | Jeff Bailey | |
| Open Road | Williamson | Jeff Bailey | |
| After Hours | A. Parrish | Jeff Bailey | |
| Lullaby for Lovers | B. Kaempfert | Jeff Bailey | |
| LO-FI | Dreamy Vibe | Loonight, clava & kazuna | Loonight, clava & kazuna |
| Good Night | Loonight, clava & kazuna | Loonight, clava & kazuna | |
| Peaceful | Loonight, clava & kazuna | Loonight, clava & kazuna | |
| Sleepy Tune | Loonight, clava & kazuna | Loonight, clava & kazuna | |
| Sunset Love | Loonight, clava & kazuna | Loonight, clava & kazuna | |
| Blue Bottle | Blue Tumbler | Lofi Blue Tumb | |
| Starbucks | LofiGuy | Lofi LofiGuy | |
| Taylor Coffee | LofiGuy | Lofi LofiGuy | |
| MONACLE | Bruns | Lofi Bruns | |
| % Arabica | Lost Tribe | Lofi Lost Tribe | |
| Intelligentsia | LofiGuy | Lofi LofiGuy | |
| TERAROSA | LofiGuy | Lofi LofiGuy | |
| DOUTOR | LofiGuy | Lofi LofiGuy | |
| Daydreams | Pink Marble | Lofi Pink Marble | |
| Walk in the Blue Mountains | Kitsune | Lofi Kitsune | |
| Endless | LofiBeats | Lofi LofiBeats | |
| Atmosphere | L. Walther | Lofi L. Walther | |
| Nostalgia | Glimlip Sleepermane | Lofi Glimlip Sleepermane | |
| Revenant | Medieval Lofi | Lofi Medieval Lofi | |
| Autumn Breeze | Annata A.I./Zen Vibes | Lofi Annata A.I./Zen Vibes | |
| Inception | Hans Zimmer | Lofi Ender Guney | |
| Chillin in my House | BLK (Kor) | Lofi Antique Sound Lab | |
| Coffee and Cake | ILLIN | Lofi Antique Sound Lab | |
| Song for Lazy bone | ILLIN | Lofi Antique Sound Lab | |
| Smoking After Lunch | ILLIN | Lofi Antique Sound Lab | |
| Sunset | Lukrembo | Lofi Lukrembo | |
| Ocean Sunset | chiro17, Riinholm & Magnoshi Kato | chiro17, Riinholm & Magnoshi Kato | |
| Campfire | chiro17, Riinholm & Magnoshi Kato | chiro17, Riinholm & Magnoshi Kato | |
| Friday | chiro17, Riinholm & Magnoshi Kato | chiro17, Riinholm & Magnoshi Kato | |
| Sunrays | chiro17, Riinholm & Magnoshi Kato | chiro17, Riinholm & Magnoshi Kato | |
| Don’t Worry | chiro17, Riinholm & Magnoshi Kato | chiro17, Riinholm & Magnoshi Kato | |
| Feeling Blue | Menda, loonight & clava | Menda, loonight & clava | |
| Ocean Waves | Menda, loonight & clava | Menda, loonight & clava | |
| Beach Day | Menda, loonight & clava | Menda, loonight & clava | |
| Sunset | Menda, loonight & clava | Menda, loonight & clava | |
| Butterly | Menda, loonight & clava | Menda, loonight & clava | |
| Dim the Lights | Jamania, Menda & Knoodle | Jamania, Menda & Knoodle | |
| Break of Dawn | Jamania, Menda & Knoodle | Jamania, Menda & Knoodle | |
| Sunset Love | Jamania, Menda & Knoodle | Jamania, Menda & Knoodle | |
| So Good | Jamania, Menda & Knoodle | Jamania, Menda & Knoodle | |
| Vacation | Jamania, Menda & Knoodle | Jamania, Menda & Knoodle | |
| Hallucination | Lars Narvike | Lars Narvike | |
| Journey to Jordan | Lars Narvike | Lars Narvike | |
| Mikawa | Lars Narvike | Lars Narvike | |
| Woods of Love | Lars Narvike | Lars Narvike | |
| Sunshine in my heart | finton, Chillski & Narvike | finton, Chillski & Lars Narvike | |
| Golden Hour | finton, Chillski & Narvike | finton, Chillski & Lars Narvike | |
| Peanut Butter Jelly | finton, Chillski & Narvike | finton, Chillski & Lars Narvike | |
| Moonlight | finton, Chillski & Narvike | finton, Chillski & Lars Narvike | |
| The Journey | finton, Chillski & Narvike | finton, Chillski & Lars Narvike | |
| Quiet Thoughts | clava | clava | |
| Anymal | clava | clava | |
| Head to Head | clava | clava | |
| Nights in Rome | clava | clava | |
| Part of This | Bristic, snaate & Riinholm | Bristic, snaate & Riinholm | |
| Bar Night | Bristic, snaate & Riinholm | Bristic, snaate & Riinholm | |
| Dinner for Two | Bristic, snaate & Riinholm | Bristic, snaate & Riinholm | |
| Our History | Bristic, snaate & Riinholm | Bristic, snaate & Riinholm | |
| Love Story | Bristic, snaate & Riinholm | Bristic, snaate & Riinholm | |
| Sao Paolo Sunset | snaate | Snaate | |
| I Miss Home | snaate | Snaate | |
| Good Reputation | snaate | Snaate | |
| Passion | snaate | Snaate | |
| Wonderful Life | kazuna | Kazuna | |
| Waves | kazuna | Kazuna | |
| Morning Flow | kazuna | Kazuna | |
| Spring | kazuna | Kazuna | |
| Sunday Stroll | kazuna | Kazuna | |
| Call Me Please | Lars Narvike | Lars Narvike | |
| Got the Feels | Lars Narvike | Lars Narvike | |
| Salir De Marcha | Lars Narvike | Lars Narvike | |
| Un Flechazo | Lars Narvike | Lars Narvike | |
| Happy Times | Jamania | Jamania | |
| Paris | Jamania | Jamania | |
| Dinner for One | Jamania | Jamania | |
| In the Moment | Jamania | Jamania | |
| Daydreaming | Jamania | Jamania | |
| Blossom | Chillski | Chillski | |
| New York Nights | Chillski | Chillski | |
| Diverted | Chillski | Chillski | |
| Dreamy Clouds | Chillski | Chillski | |
| Happy Day | Chilllski | Chillski | |
| Blue Sky | Jamania | Jamania | |
| Friendship | Jamania | Jamania | |
| Clouds | Jamania | Jamania | |
| Lucky Day | Jamania | Jamania | |
| Late Night Drive | Jamania | Jamania |
Author Contributions
Conceptualization, J.E.C. and S.K.G.; methodology, J.E.C., S.K.G., V.K. and A.E.J.; validation, J.E.C. and S.K.G.; formal analysis, J.E.C. and S.K.G.; investigation, J.E.C., V.K., S.K.G., J.K., L.Z., D.S., C.C. and N.K.; resources, J.E.C. and S.K.G.; data curation, J.E.C., V.K., A.E.J. and S.K.G.; writing—original draft preparation, J.E.C., S.K.G., V.K. and A.E.J.; writing—review and editing, visualization, J.E.C., S.K.G., V.K., L.Z., D.S., C.C., N.K. and A.E.J.; revision, J.E.C., V.K., S.K.G., J.K., L.Z., D.S., C.C., N.K. and A.E.J.; project administration, J.E.C., S.K.G. and V.K.; funding acquisition, J.E.C. and S.K.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was reviewed and approved by the University of Pittsburgh Institutional Review Board (STUDY21110130) and the trial was registered at www.clinicaltrials.gov (NCT05263635) before any eligible patients were recruited and consented. The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Written informed consent was obtained from all patients involved in the study after IRB approval and registration with Clinicaltrials.gov.
Data Availability Statement
Data are available on http://www.ClinicalTrials.gov (NCT05263635).
Conflicts of Interest
The authors declare no conflicts of interest. Funding agencies played no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
Funded in part by the UPMC Shadyside Foundation and the Department of Anesthesiology and Perioperative Medicine, UPMC Shadyside Hospital, Pittsburgh, PA.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Abate S.M., Chekol Y.A., Basu B. Global prevalence and determinants of preoperative anxiety among surgical patients: A systematic review and meta-analysis. Int. J. Surg. Open. 2020;25:6–16. doi: 10.1016/j.ijso.2020.05.010. [DOI] [Google Scholar]
- 2.Institute of Medicine. Board on Health Sciences Policy. Committee on Advancing Pain Research, Care, and Education . Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. National Academy of Sciences; Washington, DC, USA: 2011. The National Academies Collection: Reports funded by National Institutes of Health. National Academies Press (US) Copyright © 2011. [DOI] [Google Scholar]
- 3.Azizoddin D.R., Wilson J.M., Flowers K.M., Beck M., Chai P., Enzinger A.C., Edwards R., Miaskowski C., Tulsky J.A., Schreiber K.L. Daily pain and opioid administration in hospitalized patients with cancer: The importance of psychological factors, recent surgery, and current opioid use. Pain. 2023;164:1820–1827. doi: 10.1097/j.pain.0000000000002880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ip Hui Y.V., Abrishami A., Peng Philip W.H., Wong J., Chung F. Predictors of Postoperative Pain and Analgesic Consumption: A Qualitative Systematic Review. Anesthesiology. 2009;111:657–677. doi: 10.1097/ALN.0b013e3181aae87a. [DOI] [PubMed] [Google Scholar]
- 5.Gorkem U., Togrul C., Sahiner Y., Yazla E., Gungor T. Preoperative anxiety may increase postcesarean delivery pain and analgesic consumption. Minerva Anestesiol. 2016;82:974–980. [PubMed] [Google Scholar]
- 6.Yang M.M., Hartley R.L., Leung A.A., Ronksley P.E., Jetté N., Casha S., Riva-Cambrin J. Preoperative predictors of poor acute postoperative pain control: A systematic review and meta-analysis. BMJ Open. 2019;9:e025091. doi: 10.1136/bmjopen-2018-025091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valencia L., Becerra Á., Ojeda N., Domínguez A., Prados M., González-Martín J.M., Rodríguez-Pérez A. Effect of Preoperative Anxiety on Postoperative Pain after Craniotomy. J. Clin. Med. 2022;11:556. doi: 10.3390/jcm11030556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tadesse M., Ahmed S., Regassa T., Girma T., Hailu S., Mohammed A., Mohammed S. Effect of preoperative anxiety on postoperative pain on patients undergoing elective surgery: Prospective cohort study. Ann. Med. Surg. 2022;73:103190. doi: 10.1016/j.amsu.2021.103190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gan T.J. Poorly controlled postoperative pain: Prevalence, consequences, and prevention. J. Pain. Res. 2017;10:2287–2298. doi: 10.2147/JPR.S144066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mariano E.R., Dickerson D.M., Szokol J.W., Harned M., Mueller J.T., Philip B.K., Baratta J.L., Gulur P., Robles J., Schroeder K.M., et al. A multisociety organizational consensus process to define guiding principles for acute perioperative pain management. Reg. Anesth. Pain. Med. 2021;47:118–127. doi: 10.1136/rapm-2021-103083. [DOI] [PubMed] [Google Scholar]
- 11.Brummett C.M., Waljee J., Goesling J., Moser S., Lin P., Englesbe M.J. New Persistent Opioid Use after Minor and Major Surgery in US Adults. JAMA Surg. 2017;152:e170504. doi: 10.1001/jamasurg.2017.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dimitriou V., Mavridou P., Manataki A., Damigos D. The Use of Aromatherapy for Postoperative Pain Management: A Systematic Review of Randomized Controlled Trials. J. Perianesth Nurs. 2017;32:530–541. doi: 10.1016/j.jopan.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Chelly J.E., Klatt B., O’Malley M., Groff Y., Kearns J., Khetarpal S., Sadhasivam S. The Role of Inhalation Aromatherapy, Lavender and Peppermint in the Management of Perioperative Pain and Opioid Consumption Following Primary Unilateral Total Hip Arthroplasty: A Prospective, Randomized and Placebo-Controlled Study. J. Pain. Relief. 2023;12((Suppl. 1)):3. [PMC free article] [PubMed] [Google Scholar]
- 14.Fan M., Chen Z. A systematic review of non-pharmacological interventions used for pain relief after orthopedic surgical procedures. Exp. Ther. Med. 2020;20:36. doi: 10.3892/etm.2020.9163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chelly J.E., Klatt B.A., Groff Y., O’Malley M., Lin H.S., Sadhasivam S. Role of the NeuroCuple™ Device for the Postoperative Pain Management of Patients Undergoing Unilateral Primary Total Knee and Hip Arthroplasty: A Pilot Prospective, Randomized, Open-Label Study. J. Clin. Med. 2023;12:7395. doi: 10.3390/jcm12237394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deng C., Xie Y., Liu Y., Li Y., Xiao Y. Aromatherapy Plus Intervention music therap Improve Pain Intensity and Anxiety Scores in Patients with Breast Cancer During Perioperative Periods: A Randomized Controlled Trial. Clin. Breast Cancer. 2022;22:115–120. doi: 10.1016/j.clbc.2021.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Rizzo M.G., Jr., Costello J.P., II, Luxenburg D., Cohen J.L., Alberti N., Kaplan L.D. Augmented Reality for Perioperative Anxiety in Patients Undergoing Surgery: A Randomized Clinical Trial. JAMA Netw. Open. 2023;6:e2329310. doi: 10.1001/jamanetworkopen.2023.29310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tola Y.O., Chow K.M., Liang W. Effects of non-pharmacological interventions on preoperative anxiety and postoperative pain in patients undergoing breast cancer surgery: A systematic review. J. Clin. Nurs. 2021;30:3369–3384. doi: 10.1111/jocn.15827. [DOI] [PubMed] [Google Scholar]
- 19.Álvarez-García C., Yaban Z. The effects of preoperative guided imagery interventions on preoperative anxiety and postoperative pain: A meta-analysis. Complement. Ther. Clin. Pract. 2020;38:101077. doi: 10.1016/j.ctcp.2019.101077. [DOI] [PubMed] [Google Scholar]
- 20.Lee J.H. The Effects of Music on Pain: A Meta-Analysis. J. Music. Ther. 2016;53:430–477. doi: 10.1093/jmt/thw012. [DOI] [PubMed] [Google Scholar]
- 21.Lu G., Jia R., Liang D., Yu J., Wu Z., Chen C. Effects of intervention music therap on anxiety: A meta-analysis of randomized controlled trials. Psychiatry Res. 2021;304:114137. doi: 10.1016/j.psychres.2021.114137. [DOI] [PubMed] [Google Scholar]
- 22.Bojorquez G.R., Jackson K.E., Andrews A.K. Intervention music therap for Surgical Patients: Approach for Managing Pain and Anxiety. Crit. Care Nurs. Q. 2020;43:81–85. doi: 10.1097/CNQ.0000000000000294. [DOI] [PubMed] [Google Scholar]
- 23.Kakar E., Billar R.J., van Rosmalen J., Klimek M., Takkenberg J.J.M., Jeekel J. Music intervention to relieve anxiety and pain in adults undergoing cardiac surgery: A systematic review and meta-analysis. Open Heart. 2021;8:e001474. doi: 10.1136/openhrt-2020-001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bradt J., Dileo C., Myers-Coffman K., Biondo J. Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst. Rev. 2021;10:Cd006911. doi: 10.1002/14651858.CD006911.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kühlmann A.Y.R., de Rooij A., Kroese L.F., van Dijk M., Hunink M.G.M., Jeekel J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br. J. Surg. 2018;105:773–783. doi: 10.1002/bjs.10853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin C.L., Hwang S.L., Jiang P., Hsiung N.H. Effect of Intervention music therap on Pain after Orthopedic Surgery-A Systematic Review and Meta-Analysis. Pain Pract. 2020;20:422–436. doi: 10.1111/papr.12864. [DOI] [PubMed] [Google Scholar]
- 27.Baker M., Albelo F., Zhang T., Schneider M.B., Foster M.J., Aneizi A., Hasan S.A., Gilotra M.N., Henn R.F., 3rd PROMIS Depression and Anxiety in shoulder surgery patients. Bone Jt. J. 2022;104:479–485. doi: 10.1302/0301-620X.104B4.BJJ-2021-1089.R1. [DOI] [PubMed] [Google Scholar]
- 28.Sullivan M., Bishop S., Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 1995;7:524–532. doi: 10.1037/1040-3590.7.4.524. [DOI] [Google Scholar]
- 29.Poulsen M.J., Coto J. Nursing Music Protocol and Postoperative Pain. Pain Manag. Nurs. 2018;19:172–176. doi: 10.1016/j.pmn.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 30.Kühlmann A.R., van Rosmalen J., Staals L.M., Keyzer-Dekker C.M., Dogger J., de Leeuw T.G., van der Toorn F., Jeekel J., Wijnen R.M., van Dijk M. Music Interventions in Pediatric Surgery (The Music Under Surgery In Children Study): A Randomized Clinical Trial. Anesth. Analg. 2020;130:991–1001. doi: 10.1213/ANE.0000000000003983. [DOI] [PubMed] [Google Scholar]
- 31.Chelly J.E. Paravertebral blocks. Anesthesiol. Clin. 2012;30:75–90. doi: 10.1016/j.anclin.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Stein M.J., Waltho D., Ramsey T., Wong P., Arnaout A., Zhang J. Paravertebral blocks in immediate breast reconstruction following mastectomy. Breast J. 2019;25:631–637. doi: 10.1111/tbj.13295. [DOI] [PubMed] [Google Scholar]
- 33.Liu X., Song T., Chen X., Zhang J., Shan C., Chang L., Xu H. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020;20:53. doi: 10.1186/s12871-020-00967-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuck K., Naik B.I., Domino K.B., Posner K.L., Saager L., Stuart A.R., Johnson K.B., Alpert S.B., Durieux M.E., Sinha A.K., et al. Multicenter Perioperative Outcomes Group Enhanced Observation Study Investigator Group for the Multicenter Perioperative Outcomes Group Enhanced Observation Study Collaborator Group: Prolonged opioid use and pain outcome and associated factors after surgery under general anesthesia: A prospective cohort association multicenter study. Anesthesiology. 2023;138:462–476. doi: 10.1097/ALN.0000000000004510. [DOI] [PubMed] [Google Scholar]
- 35.Mann D.L. Is it Time to Abandon the Use of P-Values in Early Phase Translational Trials: Why (Effect) Size Matters. JACC Basic Transl. Sci. 2024;9:278–279. doi: 10.1016/j.jacbts.2024.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Friedrich S., Reis S., Meybohm P., Kranke P. Preoperative anxiety. Curr. Opin. Anaesthesiol. 2022;35:674–678. doi: 10.1097/ACO.0000000000001186. [DOI] [PubMed] [Google Scholar]
- 37.Svensson I., Sjöström B., Haljamäe H. Assessment of Pain Experiences after Elective Surgery. J. Pain. Symptom Manag. 2000;20:193–201. doi: 10.1016/S0885-3924(00)00174-3. [DOI] [PubMed] [Google Scholar]
- 38.Juhl Lunde S., Vuust P., Garza-Villarreal E.A., Vase L. Music-induced analgesia: How does music relieve pain? Pain. 2019;441:989–993. doi: 10.1097/j.pain.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 39.Thompson K.A., Klein D., Alaia M.J., Strauss E.J., Jazrawi L.M., Campbell K.A. Opioid Use Is Reduced in Patients Treated with NSAIDs after Arthroscopic Bankart Repair: A Randomized Controlled Study. Arthrosc. Sports Med. Rehabil. 2021;3:e15–e22. doi: 10.1016/j.asmr.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Olausson A., Svensson C.J., Andréll P., Jildenstål P., Thörn S.-E., Wolf A. Total opioid-free general anaesthesia can improve postoperative outcomes after surgery, without evidence of adverse effects on patient safety and pain management: A systematic review and meta-analysis. Acta Anaesthesiol. Scand. 2022;66:170–185. doi: 10.1111/aas.13994. [DOI] [PubMed] [Google Scholar]
- 41.Medina-Garzón M. Effectiveness of a Nursing Intervention to Diminish Preoperative Anxiety in Patients Programmed for Knee Replacement Surgery: Preventive Controlled and Randomized Clinical Trial. Investig. Educ. Enferm. 2019;37:e07. doi: 10.17533/udea.iee.v37n2e07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oliveira P., Porfírio C., Pires R., Silva R., Carvalho J.C., Costa T., Sequeira C. Psychoeducation Programs to Reduce Preoperative Anxiety in Adults: A Scoping Review. Int. J. Environ. Res. Public Health. 2022;20:327. doi: 10.3390/ijerph20010327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abadi F., Abadi F., Fereidouni Z., Amirkhani M., Karimi S., Najafi Kalyani M. Effect of Acupressure on Preoperative Cesarean Section Anxiety. J. Acupunct. Meridian Stud. 2018;11:361–366. doi: 10.1016/j.jams.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 44.Chelly J.E., Orebaugh S.L., Rodosky M.W., Groff Y.J., Norton B.E., Monroe A.L., Alimi D., Sadhasivam S.K., Vogt K.M. The Effect of Cryo-auriculotherapy on Post-Operative Pain Management following Rotator Cuff Surgery: A Randomized, Placebo-Controlled Study. MedRxiv. 2022 doi: 10.1101/2022.02.05.22270330. [DOI] [Google Scholar]
- 45.Tong Q.Y., Liu R., Gao Y., Zhang K., Ma W., Shen W.D. Effect of Electroacupuncture Based on ERAS for Preoperative Anxiety in Breast Cancer Surgery: A Single-Center, Randomized, Controlled Trial. Clin. Breast Cancer. 2022;22:724–736. doi: 10.1016/j.clbc.2022.04.010. [DOI] [PubMed] [Google Scholar]
- 46.Saadat H., Drummond-Lewis J., Maranets I., Kaplan D., Saadat A., Wang S.-M., Kain Z.N. Hypnosis reduces preoperative anxiety in adult patients. Anesth Analg. 2006;102:1394–1396. doi: 10.1213/01.ane.0000204355.36015.54. [DOI] [PubMed] [Google Scholar]
- 47.Rousseaux F., Dardenne N., Massion P.B., Ledoux D., Bicego A., Donneau A.F., Faymonville M.E., Nyssen A.S., Vanhaudenhuyse A. Virtual reality and hypnosis for anxiety and pain management in intensive care units: A prospective randomised trial among cardiac surgery patients. Eur. J. Anaesthesiol. 2022;39:58–66. doi: 10.1097/EJA.0000000000001633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lai C.H., Chandak S., Karlapudi P., Tokis J. Sex-related differences in PROMs prior to the outcome: Comparison of preoperative PROMIS physical function scores in female vs. male patients undergoing shoulder arthroplasty. JSES Int. 2023;7:2473–2475. doi: 10.1016/j.jseint.2023.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on http://www.ClinicalTrials.gov (NCT05263635).