Abstract
Background: Septic hip revision arthroplasty is a complex procedure associated with significant perioperative risks. This study aimed to analyze perioperative and follow-up risk factors in patients undergoing septic hip revision arthroplasty. Methods: A retrospective analysis was conducted on 96 patients who underwent septic revision total hip arthroplasty between 2018 and 2021 at a university hospital. Demographic data, surgical details, pathogen analyses, and complication data were collected and analyzed. The first and second hospitalizations were investigated. Data analyses were conducted with SPSS Version 29.0. Results: The mean age of patients was 69.06 ± 11.56 years, with 59.4% being female. On average, 1.3 ± 0.8 pathogens were detected per patient. Staphylococcus species were the most common pathogens. Women experienced significantly more complications during the first revision hospitalization (p = 0.010), including more surgical (p = 0.022) and systemic complications (p = 0.001). Anemia requiring transfusion was more common in women (70.1% vs. 43.5%, p = 0.012). A higher BMI was associated with a higher count of pathogens (p = 0.019). The number of pathogens correlated with increased wound healing disorders (p < 0.001) and the need for further revision surgeries (p < 0.001). Conclusions: This study identifies gender as a significant risk factor for complications in septic hip revision arthroplasty. Female patients may require more intensive perioperative management to mitigate risks. The findings underscore the need for personalized approaches in managing these complex cases to improve outcomes.
Keywords: age, blood transfusion, hip, pathogens, perioperative complications, gender differences, septic revision THA
1. Introduction
Periprosthetic joint infection (PJI) remains one of the most challenging complications following total hip arthroplasty (THA), often necessitating revision surgery [1]. Septic revision THA is a complex procedure associated with significant morbidity and mortality risks [2,3]. While a two-stage revision has traditionally been considered the gold standard for treating chronic PJI, some specialized centers have reported comparable outcomes with one-stage exchange arthroplasty in carefully selected patients [4]. The management of septic hip revisions requires careful perioperative planning and risk stratification. However, there remains a need for a comprehensive analysis of the perioperative and long-term risks specific to septic hip revisions [5,6]. Understanding the risk profile and outcomes of septic hip revisions is crucial for optimizing surgical protocols, managing patient expectations, and potentially reducing the substantial economic burden associated with these complex cases. Previous research has identified several factors that influence the outcomes of septic hip revisions, including patient comorbidities, causative organisms, the timing of the intervention, and the surgical technique. Factors such as advanced age, obesity, diabetes, and immunosuppression have been associated with an increased risk of complications and treatment failure [2,3,7,8]. The microbiology of the infection can play a crucial role as well, with certain organisms like methicillin-resistant Staphylococcus aureus (MRSA) and Gram-negative bacteria posing challenges for eradication and successful revision [9,10]. Many existing studies focus on either the short-term outcomes or long-term survival rates, but few provide a detailed examination of the entire patient journey from initial presentation through follow-up [11,12]. Understanding the risk profile and outcomes of septic hip revisions is crucial for several reasons. First, it can inform preoperative risk stratification and patient counseling, allowing for more accurate prognostication and management of expectations. Second, identifying modifiable risk factors may guide the development of targeted interventions to improve outcomes. This study aims to conduct a detailed perioperative and follow-up risk analysis of septic hip revision arthroplasty cases at a single academic center in Germany. By examining a wide range of factors including patient demographics, surgical approach, microbiology, complications, and functional outcomes, we hope to provide valuable insights to guide clinical decision-making and improve patient care. Our analysis will encompass both the initial revision procedure and subsequent hospitalizations, allowing for a comprehensive assessment of the challenges and outcomes associated with septic hip revisions.
2. Materials and Methods
2.1. Study Design
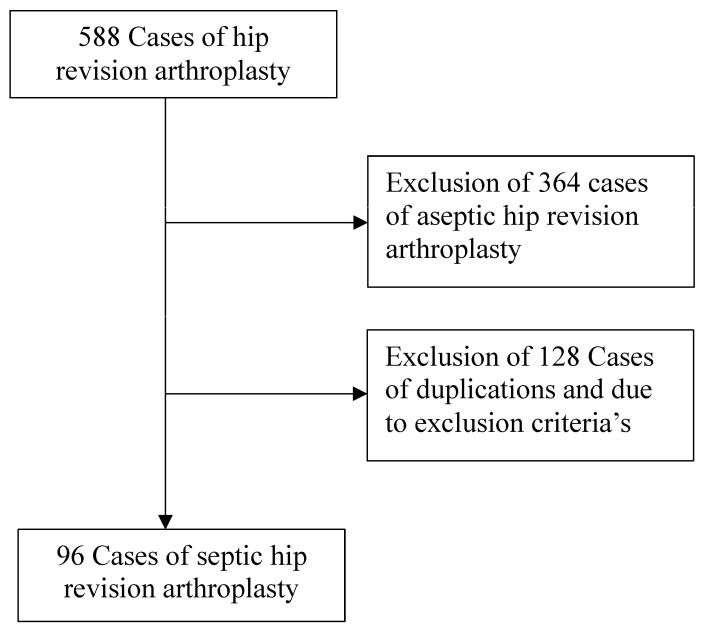
The present study was performed according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [13]. This study was conducted in the Department of Orthopedic Surgery of a university hospital in Germany. The study was conducted in accordance with the Declaration of Helsinki and approved by the local Ethics Committee of the university hospital. For more details, see Figure 1 below.
Figure 1.
Flow chart of study design.
Data from patients who underwent septic revision THA from 2018 to 2021 were retrieved. The data were retrieved using Pegasos 7 (Nexus Marabu GmbH, Berlin, Germany) and collected in Microsoft Excel Version 16.89.1 (Microsoft Corporation, Redmond, WA, USA). The following data were collected at admission: age, sex, side, body mass index (BMI), length of hospital stay, length of intensive care unit stay, and American Society of Anesthesiologists physical status (ASA). The ASA classification counts from 1 to 6 (normal health, mild, severe, severe with life-threatening conditions, moribund diseases, and brain dead) [14]. The following data were collected during the hospitalization: complete knee replacement or partial component replacement (femoral or tibial replacement), preoperative and postoperative hemoglobin (Hb), the incidence of systemic and surgical complications, and the frequency of blood unit transfusions. Systemic complications included pulmonary, cardiac, urogenital, and neurologic complications. Surgical-related complications included early infections, neurologic disorders, fractures, bleeding, aseptic loosening, surgical interventions post-surgery, and post-discharge complications such as infections or instabilities.
Exclusion Criteria
If patient data were not accessible, the patient was excluded from the present investigation.
Patients with aseptic revision hip arthroplasty, including aseptic loosening, periprosthetic fracture, or wear of the prosthetic components, were also excluded. In addition, patients who were admitted to a German university hospital for reimplantation of the hip prosthesis but who had previously had the infected prosthesis removed in another hospital were excluded. Furthermore, patients with low and incomplete data collection were excluded, for example, due to a premature transfer.
2.2. Inclusion Criteria
All patients undergoing septic revision THA were retrieved, and their eligibility was assessed. The inclusion criteria were (1) patients with primary THA and clinical symptoms of a THA infection; (2) patients aged between 40 and 100 years; (3) accessible patient data; (4) revision surgery; (5) patients with a proven positive pathogen test result; and (6) patients with all primary approaches (dorsal, lateral, anterolateral, anterior).
2.3. Perioperative Management
The revision arthroplasties were conducted with the Zimmer Biomet Zweymueller system (Zimmer biomet, Warsaw, IN, USA) Implantcast Mutars RS system (Implantcast, Hamburg, Germany), and Link MP Reconstruction System (Link, Hamburg, Germany). For revision THA, the Bauer approach, Moore approach, and anterolateral approach were used. Every patient received a urinary tract catheter before the revision surgery. Removal was carried out as early as possible and on an individual basis, but at least after sufficient mobilization had been achieved. All patients received general anesthesia and at least short monitoring after the operation. A stationary or ambulant rehabilitation program was organized prior to hospital release.
Blood Unit Supply
The indication for the blood unit transfusion was according to the restrictive Cochrane guidelines: Hb-levels over 8.0 g/dL indicated no transfusion; levels between 7 and 9 indicated concomitant clinical symptoms such as dizziness, nausea, malaise, or loss of appetite; and Hb-levels under 8 g/dL indicated transfusion [15].
2.4. Statistical Analyses
All statistical analyses were performed using the software IBM SPSS version 29 (IBM, Armonk, NY, USA). Metric-scaled data were analyzed by mean, standard deviation, and variance. Nominal, dichotomous data were analyzed by Fisher’s exact test. For the analysis of metric and nominally scaled variables, the T-test for independent samples, variance analyses, the Levene test, and the Welch test were used. Cohen’s d (small 0.20; medium 0.50; large 0.80) and a 95% interval were used as effect sizes. The effect size used was phi (small 0.10; medium 0.30; large 0.50). For correlation analyses of metric and ordinal scales, the bivariate Pearson and Spearman correlation analyses were used. For nominal and ordinal scales, the Mann –Whitney U test and the Kruskal–Wallis test were used. The significance level was set to two-sided with α = 0.05.
3. Results
3.1. Recruitment Process
In total, data from 96 patients with septic revision THA were retrieved from 2018 to 2021.
3.2. Patient Demographics
Patient demographics were sorted from hospital data of the first stay to the follow-up period. See more details in Table 1.
Table 1.
Patient demographics. (d) = days.
| Demographics | |
|---|---|
| Age | 69.06 ± 11.56 years |
| Men | 40.6% (39 of 96) |
| Women | 59.4% (57 of 96) |
| BMI | 30.46 ± 6.6 kg/m2 |
| ASA score | 2.3 ± 0.51 |
| Pre-diseases | 4.9 ± 2.6 |
| Hospital data | |
| Length in days until first revision | 636.8 ± 1224 |
| Surgery time (min) | 123 ± 81.65 |
| Length of hospital stay (d) | 28.3 ± 18.8 |
| Number of surgeries in first hospital stay (mean) |
2.01 ± 1.87 |
| Number of pathogens detected | 1.3 ± 0.82 |
| Detection of the main pathogen in X samples | 3.6 ± 2.42 |
| Duration of antibiotic therapy | 40.33 ± 23.09 |
| Days of intensive care | 2.84 ± 3.80 |
| Number of blood unit transfusions | 3.47 ± 5.59 |
| Follow-up period (d) | 219 ± 290 |
| Number of follow-up stays (mean) | 0.85 ± 0.89 |
| Number of follow-up surgical interventions (mean) | 1.13 ± 1.47 |
The indications for revision were pain (27.1%), positive pathogen detection in punction (12.5%), persistent wound secretion (21.9%), positive inflammation signs (10.4%), persistent fever (6.3%), subcutaneous abscess (2.1%), luxation (7.3%), persistent fistula (5.2%), and periprosthetic fracture (2.1%). For component changes, see Table 2.
Table 2.
Type of operation during first revision hospitalization and second hospitalization.
| Change of mobile components | Direct implantation of spacer | Girdlestone | |||
| 1. hospitalization |
51 (53.1%) | 45 (46.9%) | 0% | ||
| Implantation of spacer | Reimplantation of arthroplasty | Girdlestone | Permanent fistula | Amputation | |
| 2. hospitalization |
7 (7.3%) | 45 (46.8%) | 7 (7.3%) | 2 (2.1%) | 2 (2.1%) |
3.3. Pathogen Analyses
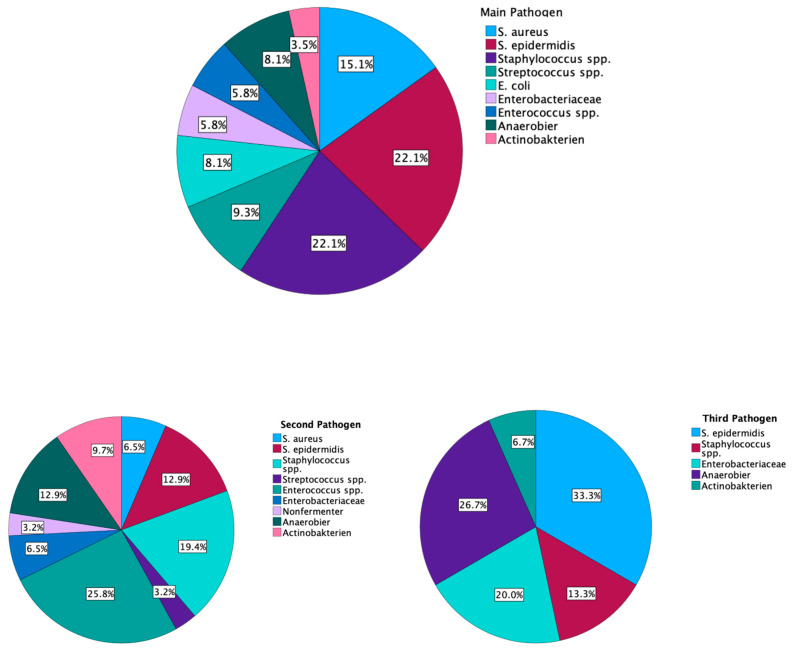
The analyses of pathogens identified up to three pathogens per patient. The main pathogen was found in 3.6 ± 2.4 test samples. The mean proportion of the main pathogen was 69.7 ± 30.9%. On average, 1.3 ± 0.8 pathogens were detected. No gender or age difference was found in the number of pathogens per patient (p = 0.517; d = 0.135/p = 0.308; d = 0.194), whereas a significant difference between a BMI lower than 25 and a BMI higher than 25 could be detected. A high BMI was associated with a higher count of pathogens in the infection (p = 0.019; d = 0.596). No difference was found between the main pathogens and the time to the first revision operation (p = 0.906; η2 = 0.042). In the second hospitalization, in 79.2% of the cases, no pathogen was found; in 2.1% of cases, the same pathogen from the first hospitalization could be found; and in 15.6% of cases, a new pathogen was detected. In 28% (n = 13) of patients with THA reimplantation (in the second hospitalization) (n = 46), a pathogen was detected. The higher the number of pathogens found in the revision surgery, the more often wound healing disorders occurred (p ≤ 0.001; d = 0.900) and the more often further revision surgeries were necessary (p ≤ 0.001; d = 0.910). The pathogen distribution is presented in Figure 2.
Figure 2.
Pathogen distribution in the first hospitalization; Staphylococcus spp. Includes all different staphylococcus except S. aureus and S. epidermidis.
3.4. Gender Analyses
There was no difference between the sexes in the frequency of the change of mobile components (p = 0.417; phi = 0.158), but men were more often implanted with a spacer than women during the first revision surgery (p = 0.022; phi = 0.243). No significant gender difference was found in the frequency of the type of pathogens, although Staphylococcus species were found in women more often in fixed numbers (p = 0.425; phi = 0.311). No significant gender differences were detected in the pre- and postoperative walking distances during the first revision stay. Women experienced more complications including systemic and surgery-related complications during the first revision hospitalization (p = 0.010; phi = 0.285), but no gender differences were revealed for the follow-up complications after the second revision (p = 0.400; phi = 0.095). Additionally, women were significantly more likely to suffer from surgical complications (p = 0.022; phi = 0.251). The same observation was made regarding systemic complications (1. Hospitalization p = 0.001; phi = 0.347; 2. Hospitalization p = 0.674; phi = 0.051). Anemia was significantly higher in women than men in the first hospitalization (p = 0.012; phi = 0.266); in the second hospitalization, no gender differences were found (p = 1.0; phi = 0.022). Men more often received reimplantation in the second hospitalization (p = 0.36; phi = 0.228).See more details in Table 3.
Table 3.
Surgery-related and systemic complications in first and second hospitalization: cardiac disorders included cardiac arrhythmias and decompensation; pulmonary disorders included pneumonia or respiratory dysfunction. * = significantly different.
| Women (n = 57) | Men (n = 39) | p | |
|---|---|---|---|
| 1. Hospitalization | |||
| Intraoperative fracture | 12.2% | 2.5% | 0.13 |
| Intraoperative vascular damage | 3.5% | 2.5% | 1 |
| THA dislocation | 10.5% | 10.2% | 1 |
| Wound healing disorder | 41.1% | 25.8% | 0.03 * |
| Postoperative neurologic disorders | 5.2% | 5.1% | 1 |
| Change of spacer (when implanted in the first surgery) |
15.7% | 18.7% | 0.43 |
| Complete removal of endoprosthesis | 15.7% | 17.9% | 0.787 |
| Permanent fistula tract | 5.2% | 0.0% | 0.269 |
| Anemia requiring transfusion | 70.1% | 43.5% | 0.012 * |
| Blood unit transfusion (mean) | 4.33 | 2.19 | 0.054 |
| Urinary tract infection | 19.2% | 0.0% | 0.003 * |
| Postoperative thrombosis | 0.0% | 2.5% | 0.406 |
| Renal insufficiency | 0.0% | 7.6% | 0.064 |
| Cardiac disorders | 5.2% | 2.5% | 0.644 |
| Pulmonary disorders | 7.0% | 5.1% | 1 |
| Postoperative delirium | 3.5% | 0% | 0.51 |
| 2. Hospitalization | Women (n = 56) | Men (n = 38) | p |
| Intraoperative fracture | 1.7% | 0.0% | 1 |
| Intraoperative vascular damage | 0.0% | 0.0% | / |
| THA dislocation | 12.7% | 5.2% | 0.301 |
| Wound healing disorder | 16.3% | 18.4% | 0.788 |
| Postoperative neurologic disorders | 12.7% | 2.5% | 0.135 |
| Reinfection of the new implant | 16.3% | 18.4% | 0.788 |
| Evidence of new bacteria compared to the last hospitalization | 16.3% | 15.7% | 1 |
| Anemia requiring transfusion | 36.3% | 34.2% | 1 |
| Urinary tract infection | 7.1% | 0.0% | 0.142 |
| Postoperative thrombosis | 3.5% | 2.6% | 1 |
| Renal insufficiency | 0.0% | 0.0% | / |
| Cardiac disorders | 3.5% | 2.6% | 1 |
| Pulmonary disorders | 3.6% | 2.6% | 1 |
| Postoperative delirium | 1.7% | 0.0% | 1 |
| Number of follow-up stays (mean) | 0.78 | 0.94 | 0.391 |
3.5. Survival Rate
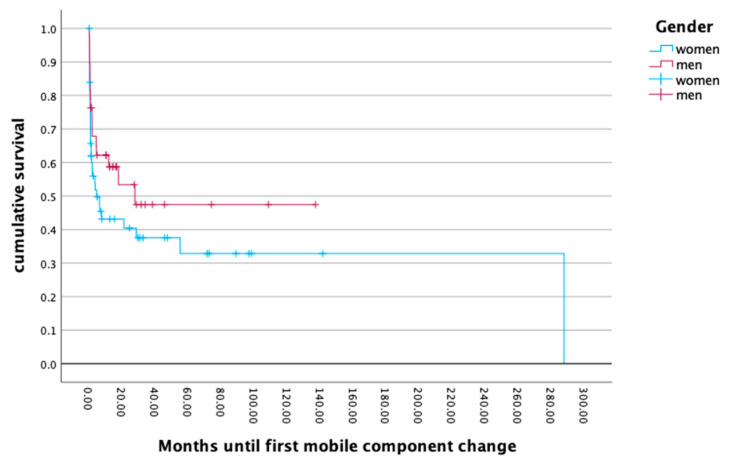
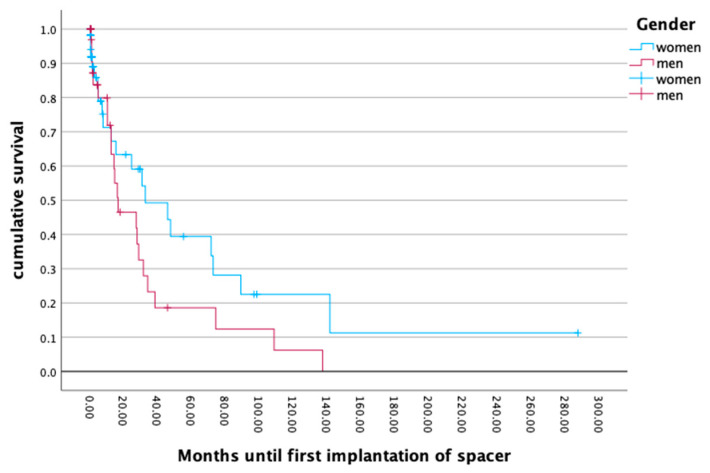
The survival of the first implanted endoprosthesis to the first event of a mobile component change or a full component removal with implantation of a temporary spacer revealed no gender differences (p = 0.173; p = 0.120). The mean survival rate of the endoprosthesis also showed no gender differences (p = 0.704), with a mean for men of 19.26 months and 22.53 months for women. The cumulative survival rate revealed a periprosthetic infection rate of 50.0% at 20 months after primary implantation. An analysis of the differences in the survival rates for low and high body mass indices did not reveal any significant outcomes (p = 0.917). For more details, see Figure 3 and Figure 4.
Figure 3.
Months until first mobile component change.
Figure 4.
Months until first implantation of spacer.
4. Discussion
This study provides valuable insights into the perioperative risks and outcomes associated with septic hip revision arthroplasty. The findings highlight several key factors that influence complications and patient outcomes, with important implications for clinical practice.
One of the most striking findings of this study is the significant gender difference in complication rates. Women experienced more complications during the first revision hospitalization, including higher rates of surgical and systemic complications. Additionally, our study found that a higher BMI was associated with a higher count of pathogens in the infection, whereas gender did not show any differences. This aligns with previous research suggesting that obesity is a risk factor for periprosthetic joint infection and may complicate treatment [16]. Higher pathogen counts were also accompanied by worse wound healing and more frequent revision surgeries. A reason for this could be the difficult intraoperative tackling of the pathogens, especially of the small colony variants. Another factor could be antibiotic therapy, which depends on many factors, like the patient’s weight, allergies, compatibility, and the antibiotic resistogram. The treatment of different pathogens at the same time is a difficult task. Surprisingly, Petrie et al. (2023) claimed that systemic antibiotics are not required for a successful two-stage revision. Aggressive debridement and local antibiotics without prolonged systemic antibiotics were equally successful. There may be a question regarding the missing treatment of biofilm-building bacteria and possible hematogenous spreading [17] Other study groups have shown good results with systemic antibiotic therapy [18,19,20,21]. The microbiology results in our study, with Staphylococcus species being the most common pathogens, are consistent with the literature on periprosthetic joint infections. Gender disparity in outcomes following septic hip revision has not been widely reported in previous studies in the literature [22,23]. While some studies have found gender differences in outcomes following primary total hip arthroplasty, the specific impact on septic revisions has been less clear. Despite women being more prone to complications in the first and second hospitalization, men more often received a direct implantation of a spacer in the first hospitalization. One reason for this could be a worse infection situation or a longer wait until the decision to go to the hospital is made. Another reason could be a sex difference in the immune response. Some studies have revealed different immune responses in favor of women. This allows females to have better pathogen clearance but also leads to faster and worse inflammatory signs [24,25,26]. Offner et al. (1999) observed gender differences in the occurrence of complications after trauma surgery [27]. These results show the complexity of gender differences in clinical medicine. Orthopedic surgery should pay more attention to this factor. In addition, women have been described as an independent risk factor for periprosthetic infections in previous investigations [22,28]. On the other hand, research by Triantafyllopoulos et al. (2015) on risk factors for early PJI after total joint arthroplasty found that the male gender was actually associated with a higher risk of early infection [29]. This is contrary to findings in other studies [30,31,32,33]. Regarding urinary tract infections, women were only affected by the complication (p = 0.003) in the first hospitalization. The complication rate drops clearly during the second hospitalization. This could be due to a long pretreatment with antibiotics and a repaired prosthesis infection before reimplantation of the new implants. A comparison of the bacteria from the urinary tract catheter (UTC) and the pathogen of the joint infection would have been useful to find a connection. Magliano et al. (2012) described that women in the age range of 16–64 experience significantly more urinary tract infections than men. Gram-negative pathogens were found in 90% of cases [34]. The urethra of women is shorter than men, which is proposed as a reason why it is easier for ascending bacteria to reach the bladder. Another problem is the close distance of the anus to the urethra [35]. Other study groups revealed that women were more prone to urinary tract infections with UTCs [36,37]. The fact that urinary tract infections occurred in spite of antibiotic treatment and standardized hospital care allows room for many interpretations. The extended period spent in bed and the extended placement of the catheter, coupled with the female anatomy, are to be seen as the most likely causes. As a consequence, bladder catheters in women have to be removed more quickly, and remobilization should be encouraged. The survival analysis of the first implanted prostheses revealed a concerning trend, with a 50% infection rate at 20 months after primary implantation. It should be added that the patients were presented from any hospital in the region, which could have caused a bias effect. In addition, due to the hospital’s single status specialization and certification in treating prosthesis infections within a wide radius of the region, severe cases are referred directly to it. Further investigations will be carried out to find a reasonable explanation for this effect. Overall, this is substantially higher than rates reported in some previous studies [38]. For instance, other study groups found a re-revision rate of 7–30% within one year after septic revision THA in a large registry study [3,39]. The higher rate in our study may reflect potential differences in patient populations and treatment protocols. During the second hospitalization, the rate of complications decreased significantly, which demonstrates that a standardized procedure is essential for a good outcome.
While this study provides valuable insights, it has several limitations. The retrospective design and relatively small sample size (n = 96) limit the generalizability of the findings. Additionally, the single-center nature of the study may not capture variations in practice across different institutions. Future research should focus on prospective, multi-center studies to validate these findings and explore regional variations in outcomes. Future studies should also investigate the underlying mechanisms for the observed gender differences in complications, as well as evaluate targeted interventions to reduce complication rates, particularly in high-risk groups such as women and patients with a high BMI. There should also be long-term follow-up studies to assess the impact of perioperative factors on long-term outcomes and quality of life.
5. Conclusions
In conclusion, this study highlights the complex nature of septic hip revision arthroplasty and identifies several key risk factors for complications. The findings underscore the need for personalized approaches to perioperative management, particularly for female patients and those with a high BMI, especially in postoperative treatment with possible complications like urinary tract infections. By addressing these risk factors, clinicians may be able to improve outcomes and reduce the burden of complications associated with this challenging procedure.
Author Contributions
Conceptualization, writing—original draft preparation, J.K.; formal analysis, methodology, J.B.; software, data curation, F.M.; validation, writing—review and editing, C.S.; supervision, project administration, C.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of RUB-Bochum University, HDZ Bad Oeynhausen (IDs: 2022-934, ethical approval on 21 April 2022).
Informed Consent Statement
Consent information was not applicable: “retrospective data collection was performed using established approved software for treatment procedures completed in the past with no immediate risk to the patient”—approved by Ethics Committee of RUB-University, HDZ Bad Oeynhausen. This study is considered “Inhouse-research” according to German legislation with no affection to paragraph 203 (StGB).
Data Availability Statement
Data generated or analyzed during this study are included in this published article. No Supplementary datasets were used for the manuscript.
Conflicts of Interest
The authors declare that they have no competing interests.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Vees T., Hofmann G.O. Early periprosthetic infection: Dilution, jet dilution or local antibiotics. Which way to go? A meta-analysis on 575 patients. GMS Interdiscip. Plast. Reconstr. Surg. DGPW. 2020;9:Doc03. doi: 10.3205/iprs000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi H.R., Beecher B., Bedair H. Mortality after septic versus aseptic revision total hip arthroplasty: A matched-cohort study. J. Arthroplast. 2013;28:56–58. doi: 10.1016/j.arth.2013.02.041. [DOI] [PubMed] [Google Scholar]
- 3.Resl M., Becker L., Steinbrück A., Wu Y., Perka C. Re-revision and mortality rate following revision total hip arthroplasty for infection. Bone Jt. J. 2024;106:565–572. doi: 10.1302/0301-620X.106B6.BJJ-2023-1181.R1. [DOI] [PubMed] [Google Scholar]
- 4.Zahar A., Gehrke T.A. One-Stage Revision for Infected Total Hip Arthroplasty. Orthop. Clin. N. Am. 2016;47:11–18. doi: 10.1016/j.ocl.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Bettencourt J.W., Wyles C.C., Osmon D.R., Hanssen A.D., Berry D.J., Abdel M.P. Outcomes of primary total hip arthroplasty following septic arthritis of the hip: A case-control study. Bone Jt. J. 2022;104-b:227–234. doi: 10.1302/0301-620X.104B2.BJJ-2021-1209.R1. [DOI] [PubMed] [Google Scholar]
- 6.Sadoghi P., Liebensteiner M., Agreiter M., Leithner A., Böhler N., Labek G. Revision surgery after total joint arthroplasty: A complication-based analysis using worldwide arthroplasty registers. J. Arthroplast. 2013;28:1329–1332. doi: 10.1016/j.arth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Kilgus S., Karczewski D., Passkönig C., Winkler T., Akgün D., Perka C., Müller M. Failure analysis of infection persistence after septic revision surgery: A checklist algorithm for risk factors in knee and hip arthroplasty. Arch. Orthop. Trauma Surg. 2021;141:577–585. doi: 10.1007/s00402-020-03444-0. [DOI] [PubMed] [Google Scholar]
- 8.Russo A., Cavagnaro L., Alessio-Mazzola M., Felli L., Burastero G., Formica M. Two-stage arthroplasty for septic arthritis of the hip and knee: A systematic review on infection control and clinical functional outcomes. J. Clin. Orthop. Trauma. 2022;24:101720. doi: 10.1016/j.jcot.2021.101720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashkenazi I., Thomas J., Lawrence K.W., Rozell J.C., Lajam C.M., Schwarzkopf R. Positive Preoperative Colonization with Methicillin Resistant Staphylococcus Aureus Is Associated with Inferior Postoperative Outcomes in Patients Undergoing Total Joint Arthroplasty. J. Arthroplasty. 2023;38:1016–1023. doi: 10.1016/j.arth.2023.02.065. [DOI] [PubMed] [Google Scholar]
- 10.Tsikopoulos K., Sidiropoulos K. Is there sufficient evidence to support the use of antibiotic holiday just before the second stage of an infected total hip or knee arthroplasty revision surgery? World J. Orthop. 2024;15:483–485. doi: 10.5312/wjo.v15.i5.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saul H., Deeney B., Cassidy S., Kwint J., Blom A. One-stage hip revisions are as good as two-stage surgery to replace infected artificial hips. BMJ. 2023;381:1087. doi: 10.1136/bmj.p1087. [DOI] [PubMed] [Google Scholar]
- 12.Tohidi M., Grammatopoulos G., Mann S.M., Pysklywec A., Groome P.A. Patient Factors Associated with 10-Year Survival After Arthroplasty for Hip Fracture: A Population-Based Study in Ontario, Canada. J. Bone Joint. Surg. Am. 2024 doi: 10.2106/jbjs.24.00379. [DOI] [PubMed] [Google Scholar]
- 13.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Mayhew D., Mendonca V., Murthy B.V.S. A review of ASA physical status—Historical perspectives and modern developments. Anaesthesia. 2019;74:373–379. doi: 10.1111/anae.14569. [DOI] [PubMed] [Google Scholar]
- 15.Carson J.L., Stanworth S.J., Dennis J.A., Trivella M., Roubinian N., Fergusson D.A., Triulzi D., Dorée C., Hébert P.C. Transfusion thresholds for guiding red blood cell transfusion. Cochrane Database Syst. Rev. 2021;12:Cd002042. doi: 10.1002/14651858.CD002042.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boyer B., Bordini B., Caputo D., Neri T., Stea S., Toni A. What are the influencing factors on hip and knee arthroplasty survival? Prospective cohort study on 63619 arthroplasties. Orthop. Traumatol. Surg. Res. 2019;105:1251–1256. doi: 10.1016/j.otsr.2019.07.020. [DOI] [PubMed] [Google Scholar]
- 17.Petrie J.M., Panchani S., Al-Einzy M., Partridge D., Harrision T.P., Stockley I. Systemic antibiotics are not required for successful two-stage revision hip arthroplasty. Bone Joint. J. 2023;105-B:511–517. doi: 10.1302/0301-620X.105B5.BJJ-2022-0373.R2. [DOI] [PubMed] [Google Scholar]
- 18.Knoll L., Steppacher S.D., Furrer H., Thurnheer-Zürcher M.C., Renz N. High treatment failure rate in haematogenous compared to non-haematogenous periprosthetic joint infection. Bone Jt. J. 2023;105-b:1294–1302. doi: 10.1302/0301-620X.105B12.BJJ-2023-0454.R1. [DOI] [PubMed] [Google Scholar]
- 19.Kurapatti M., Oakley C., Singh V., Aggarwal V.K. Antibiotic Therapy in 2-Stage Revision for Periprosthetic Joint Infection: A Systematic Review. JBJS Rev. 2022;10:e21. doi: 10.2106/JBJS.RVW.21.00143. [DOI] [PubMed] [Google Scholar]
- 20.Ji B., Li G., Zhang X., Xu B., Wang Y., Chen Y., Cao L. Effective single-stage revision using intra-articular antibiotic infusion after multiple failed surgery for periprosthetic joint infection: A mean seven years’ follow-up. Bone Jt. J. 2022;104-b:867–874. doi: 10.1302/0301-620X.104B7.BJJ-2021-1704.R1. [DOI] [PubMed] [Google Scholar]
- 21.Romanò C.L., Romanò D., Logoluso N., Meani E. Septic versus aseptic hip revision: How different? J. Orthop. Traumatol. 2010;11:167–174. doi: 10.1007/s10195-010-0106-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dhanjani S.A., Schmerler J., Wenzel A., Gomez G., Oni J., Hegde V. Racial and Socioeconomic Disparities in Risk and Reason for Revision in Total Joint Arthroplasty. J. Am. Acad. Orthop. Surg. 2023;31:e815–e823. doi: 10.5435/JAAOS-D-22-01124. [DOI] [PubMed] [Google Scholar]
- 23.Klein S.L., Flanagan K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016;16:626–638. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 24.Dias S.P., Brouwer M.C., van de Beek D. Sex and Gender Differences in Bacterial Infections. Infect. Immun. 2022;90:e0028322. doi: 10.1128/iai.00283-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abdullah M., Chai P.S., Chong M.Y., Tohit E.R., Ramasamy R., Pei C.P., Vidyadaran S. Gender effect on in vitro lymphocyte subset levels of healthy individuals. Cell Immunol. 2012;272:214–219. doi: 10.1016/j.cellimm.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 26.Sciarra F., Campolo F., Franceschini E., Carlomagno F., Venneri M.A. Gender-specific Impact of Sex Hormones on the immune System. Int. J. Mol. Sci. 2023;24:6302. doi: 10.3390/ijms24076302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Offner P.J., Moore E.E., Biffl W.L. Male gender is a risk factor for major infections after surgery. Arch. Surg. 1999;134:935–938; discussion 938–940. doi: 10.1001/archsurg.134.9.935. [DOI] [PubMed] [Google Scholar]
- 28.Miley G.B., Scheller A.D., Jr., Turner R.H. Medical and surgical treatment of the septic hip with one-stage revision arthroplasty. Clin. Orthop. Relat. Res. 1982;170:76–82. doi: 10.1097/00003086-198210000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Triantafyllopoulos G., Studner O., Memtsoudis S., Poultsides L.A. Patient, Surgery, and Hospital Related Risk Factors for Surgical Site Infections following Total Hip Arthroplasty. ScientificWorldJournal. 2015;2015:979560. doi: 10.1155/2015/979560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Veghel M.H.W., van der Koelen R.E., Hannink G., Schreurs B.W., Rijnen W.H.C. Survival of cemented short Exeter femoral components in primary total hip arthroplasty. Bone Jt. J. 2024;106-b:137–142. doi: 10.1302/0301-620X.106B3.BJJ-2023-0826.R2. [DOI] [PubMed] [Google Scholar]
- 31.De Leissegues T., Viste A., Fessy M.H. Revision of total hip arthroplasty by long locking stem with fully hydroxyapatite-coated modular metaphysis (Reef™): A continuous series of 78 cases at a minimum 2-year follow-up. Orthop. Traumatol. Surg. Res. 2024;110:103786. doi: 10.1016/j.otsr.2023.103786. [DOI] [PubMed] [Google Scholar]
- 32.Koettnitz J., Migliorini F., Peterlein C.D., Götze C. Same-gender differences in perioperative complications and transfusion management for lower limb arthroplasty. BMC Musculoskelet Disord. 2023;24:653. doi: 10.1186/s12891-023-06788-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deltourbe L., Lacerda Mariano L., Hreha T.N., Hunstad D.A., Ingersoll M.A. The impact of biological sex on diseases of the urinary tract. Mucosal. Immunol. 2022;15:857–866. doi: 10.1038/s41385-022-00549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magliano E., Grazioli V., Deflorio L., Leuci A.I., Mattina R., Romano P., Cocuzza C.E. Gender and age-dependent etiology of community-acquired urinary tract infections. Sci. World J. 2012;2012:349597. doi: 10.1100/2012/349597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abelson B., Sun D., Que L., Nebel R.A., Baker D., Popiel P., Amundsen C.L., Chai T., Close C., DiSanto M., et al. Sex differences in lower urinary tract biology and physiology. Biol. Sex. Differ. 2018;9:45. doi: 10.1186/s13293-018-0204-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saint S., Trautner B.W., Fowler K.E., Colozzi J., Ratz D., Lescinskas E., Hollingsworth J.M., Krein S.L. A Multicenter Study of Patient-Reported Infectious and Noninfectious Complications Associated with Indwelling Urethral Catheters. JAMA Intern. Med. 2018;178:1078–1085. doi: 10.1001/jamainternmed.2018.2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simon S., Martalanz L., Frank B.J.H., Hartmann S.G., Mitterer J.A., Sebastian S., Huber S., Hofstaetter J.G. Prevalence, risk factors, microbiological results and clinical outcome in unexpected positive intraoperative cultures in unclear and presumed aseptic hip and knee revision arthroplasties—A ten-year retrospective analysis with a minimum follow up of 2 years. J. Orthop. Translat. 2024;48:156–162. doi: 10.1016/j.jot.2024.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jeschke E., Gehrke T., Günster C., Heller K.D., Leicht H., Malzahn J., Niethard F.U., Schräder P., Zacher J., Halder A.M. Low Hospital Volume Increases Revision Rate and Mortality Following Revision Total Hip Arthroplasty: An Analysis of 17,773 Cases. J. Arthroplast. 2019;34:2045–2050. doi: 10.1016/j.arth.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 39.Cosseddu F., Shytaj S., Sacchetti F., Capanna R., Manca M., Parchi P.D., Scaglione M., Andreani L. Total hip replacement: A retrospective multicentric analysis on re-intervention rate after single component revision. J. Biol. Regul. Homeost. Agents. 2020;34((Suppl. 3)):191–196. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data generated or analyzed during this study are included in this published article. No Supplementary datasets were used for the manuscript.