Abstract
Serotonergic neurons in the central nervous system control behavior and mood, but knowledge of the roles of serotonergic circuits in the regulation of immune homeostasis is limited. Here, we employ mouse genetics to investigate the functions of enteric serotonergic neurons in the control of immune responses and find that these circuits regulate IgA induction and boost host defense against oral, but not systemic Salmonella Typhimurium infection. Enteric serotonergic neurons promote gut-homing, retention and activation of intestinal plasmacytoid dendritic cells (pDC). Mechanistically, this neuro-immune crosstalk is achieved through a serotonin-5-HT receptor 7 (HTR7) signaling axis that ultimately facilitates the pDC-mediated differentiation of IgA+ B cells from IgD+ precursors in the gut. Single-cell RNA-seq data further reveal novel patterns of bidirectional communication between specific subsets of enteric neurons and lamina propria DC. Our findings thus reveal a close interplay between enteric serotonergic neurons and gut immune homeostasis that enhances mucosal defense.
Subject terms: Mucosal immunology, Enteric nervous system, Infection, Cell signalling
Roles of serotonergic neurons in immune homeostasis and host defense are largely unexplored. Here the authors show that in mice enteric serotonergic neurons regulate immune homeostasis and host defense against Salmonella infection by orchestrating gut homing and activation of plasmacytoid dendritic cell, ultimately promoting the differentiation of protective IgA+ B cells.
Introduction
Serotonin, also known as 5-hydroxytryptamine (5-HT), can be produced by several cell types and has diverse functions1. In central nervous system (CNS) neurons, where 5-HT synthesis depends on the enzyme tryptophan hydroxylase 2 (Tph2)2, serotonin acts as a neurotransmitter whose activity is associated with regulation of emotion and mood3. Mutations in Tph2 have been associated with depression, anxiety, impulsivity, and aggression in both humans and mice4,5. Outside the nervous system, cells use Tph1 to produce 5-HT. Studies using knockout mice have shown that this enzyme creates the majority of the serotonin found in blood and in the gut6. This non-neuronal derived serotonin, which is primarily produced by intestinal enterochromaffin cells, plays important roles in diverse processes, including hemostasis, vascular tone, and immune modulation7.
While the importance of serotonin produced by neurons in the CNS in the control of emotion and mood is well-established8, the functions of serotonin produced by enteric neurons are not as well understood. In the gut, the existence of enteric serotonergic neurons was initially proposed by Gershon et al. in 19659 and recent single-cell RNA sequencing data confirm this idea10. Enteric serotonergic neurons are thought to promote mucosal homeostasis and influence neurogenesis and gut motility11. However, studies of the functions of serotonin produced by enteric neurons have been hindered by the absence of conditional knock-out (KO) mice specifically deficient in Tph2 in enteric neurons, with intact CNS Tph2.
Connections between neuronal serotonin and the immune system have not been experimentally investigated, despite the recent marked expansion in knowledge of the compounds and mechanisms that mediate the communication between the nervous system and immune system. Neuronal circuits are now known to influence both innate and adaptive immune responses12. For example, neurons within the sympathetic and vagus nerves and dorsal root ganglion as well as nociceptive neurons have been shown to regulate innate immune cells, including macrophages, mast cell, and innate lymphoid cells (ILCs)13. In these pathways, compounds traditionally associated with communication between neurons, such as norepinephrine (NE), calcitonin gene-related peptide (CGRP), substance P, and neuromedin U (NMU) have been shown to modify immune cell function and play roles in immune development and homeostasis and host defense14. Since serotonergic neuronal circuits have been strongly associated with the control of emotion/mood, we wondered whether neuronal serotonin could also modify immune responses and host defense, given the extensive reports of associations between emotion/mood and susceptibility to disease15. Interestingly, a recent report suggested an association between a human Tph2 variant and sensitivity to infection16.
Here, using mice lacking neuronal serotonin synthesis, we address whether serotonergic circuits regulate immune homeostasis and host defense. Employing whole-body Tph2 KO and a conditional KO mouse model (Tph2fl/fl; Hand2-Cre) lacking Tph2 in intestinal neurons, we show that enteric serotonergic neurons support the gut homing and/or retention and activation of plasmacytoid dendritic cells (pDC) via serotonin - HTR7 signaling, and that defects in pDC likely underlie the reduction in IgA B cell differentiation in the small intestine in the absence of neuronal serotonin. Collectively, our findings suggest that enteric neuronal 5-HT signaling to HTR7+ pDC regulates intestinal immune homeostasis and mucosal defense.
Results
Serotonergic neurons regulate gut immune homeostasis and mucosal defense
To begin to address whether serotonin impacts host defense, we used mice deficient in serotonin transporters (Sert). In Sert−/− animals, serotonin signaling is heightened due to the absence of serotonin reuptake17. Following oral infection with Salmonella enterica serovar Typhimurium, a model enteric pathogen, Sert−/− mice had decreased pathogen burdens in the spleen and liver (Supplementary Fig. 1A) and increased survival compared with co-housed littermate controls (Supplementary Fig. 1B). These findings are consistent with a role for serotonin in host defense as suggested by a previous study18. However, given the expression of Sert in several cell types besides neurons19, these data do not provide conclusive evidence for the action of neuronal serotonin in gut defense.
To more directly address the role of neuronal serotonin in host defense, we challenged Tph2−/− animals, which lack serotonin production in neurons, with Salmonella. These animals have often been used to model a set of emotional disorders20,21, but the integrity of their mucosal defense has not been explored. Following oral infection with Salmonella, Tph2−/− mice had ~100-fold higher pathogen burdens in the spleen and liver (Fig. 1A) and accelerated death and reduced survival compared with co-housed littermate controls (Fig. 1B). In contrast, when the pathogen was administered intravenously to WT and Tph2−/− mice, there was no difference in survival and both groups succumbed to infection with similar kinetics (Supplementary Fig. 1C). Together, these observations suggest that Salmonella dissemination from the intestine is elevated in Tph2−/− mice.
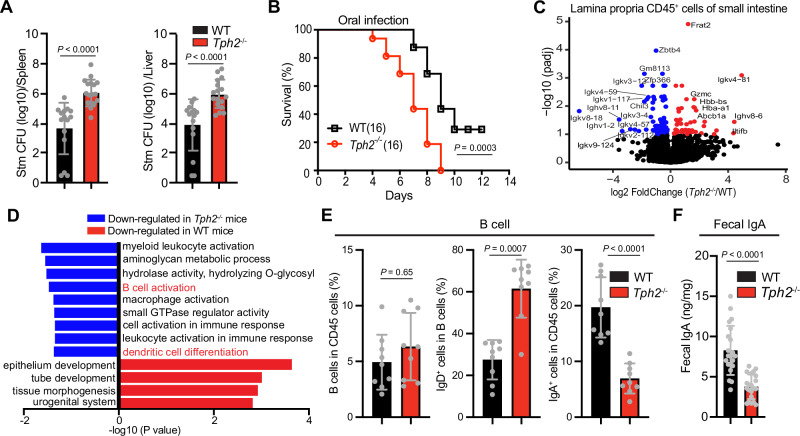
Fig. 1. Neuronal serotonin is important for IgA B cell differentiation and host defense against oral Salmonella infection.
A Salmonella Typhimurium (STm) CFU burdens in spleens and livers of WT and Tph2−/− mice 5 days post oral inoculation (WT, n = 15; Tph2−/−, n = 17). B Kaplan–Meier plot of survival of WT and Tph2−/− mice following oral STm inoculation (n = 16). C Differential gene expression of CD45+ cells isolated from the lamina propria of the small intestine from co-housed WT and Tph2−/− mice. Red points indicate increased expression and blue points indicate decreased expression in Tph2−/− mice compared to WT mice. D Gene Ontology pathway analysis of data from Fig. 1C. E Flow cytometry analyses of frequency of total B cells, IgD+ fraction of total B cells, and IgA+ cells in the lamina propria CD45+ cells from the small intestine of WT and Tph2−/− mice (n = 9). F Fecal IgA levels in WT and Tph2−/− mice (n = 21). Data shown are means ± SD. Statistical analysis was performed by two-tailed Mann–Whitney test in A, E, F; and by a Log-rank test in B.
To address the possibility that serotonergic circuits modify intestinal immune cell function, we analyzed the gene expression profiles of lamina propria-derived immune cells (CD45+) in co-housed littermate WT and Tph2−/− mice. In CD45+ cells derived from the small intestines of Tph2−/− mice, there was reduced expression of genes linked to B cell activation compared to WT animals (Fig. 1C, D). However, the transcription profiles of CD45+ cells isolated from the colons of Tph2−/− and WT mice were similar (Supplementary Fig. 1D). In contrast to the changes in gene expression profiles in small intestinal CD45+ cells that were observed in Tph2−/− animals, transcriptional profiles of epithelial cells isolated from the small and large intestines of WT and Tph2−/− mice were similar (Supplementary Fig. 1E, F). Thus, Tph2-dependent processes appear to specifically modulate gene expression of small intestinal lamina propria immune cells.
FACS-based immune profiling of CD45+ cells isolated from the lamina propria of the small intestines from Tph2−/− mice also revealed that serotonergic neurons modify immune cell composition in the small intestine. Even though the total fraction of B cells was similar in Tph2−/− and control animals, there were increased IgD+ B cells and decreased IgA+ B cells in Tph2−/− animals (Fig. 1E, Supplementary Figs. 1G and 2), consistent with a defect in the differentiation of IgD+ to IgA+ B cells. Furthermore, there was a reduction of fecal IgA in the Tph2−/− mice (Fig. 1F). These data suggest that serotonergic circuits promote the development of IgA+ B cells from IgD+ precursors in the lamina propria of the small intestine; however, defects in B cell trafficking and recirculation cannot be excluded. The fecal microbiota in Tph2−/− and control animals were similar, likely due to coprophagic behavior in the co-housed littermate animals (Supplementary Fig. 3A, B).
Enteric serotonergic neurons control intestinal IgA B cell development
The Tph2−/− animals lack serotonin production by both central and peripheral neurons. The potential immune functions of serotonin produced by intestinal neurons have received relatively little attention. Since enteric serotonergic neurons (ESN) could underlie the association between serotonergic neurons and the intestinal immune system, we initially quantified this neuronal population. FACS was used to sort cells bearing the neuronal marker Uchl122 from the small intestines of infant mice, and then single-nucleus RNA-seq was carried out to determine the frequency of Tph2-expressing neurons. These analyses revealed that a small proportion (~2%) of cells expressed Tph2 as well as Ret (Fig. 2A and Supplementary Fig. 4A–C), an established marker of enteric neurons23, consistent with previous estimates24. Tph2 transcripts were observed in various subtypes of enteric neurons (Fig. 2A). Tph2 transcripts were also present in sorted enteric neurons from the small intestines of adult mice but not in the intestinal epithelium or lamina propria immune cells (Fig. 2B). In contrast, Tph1 transcripts were detected in the latter two small intestinal cell populations but not in enteric neurons (Fig. 2B).
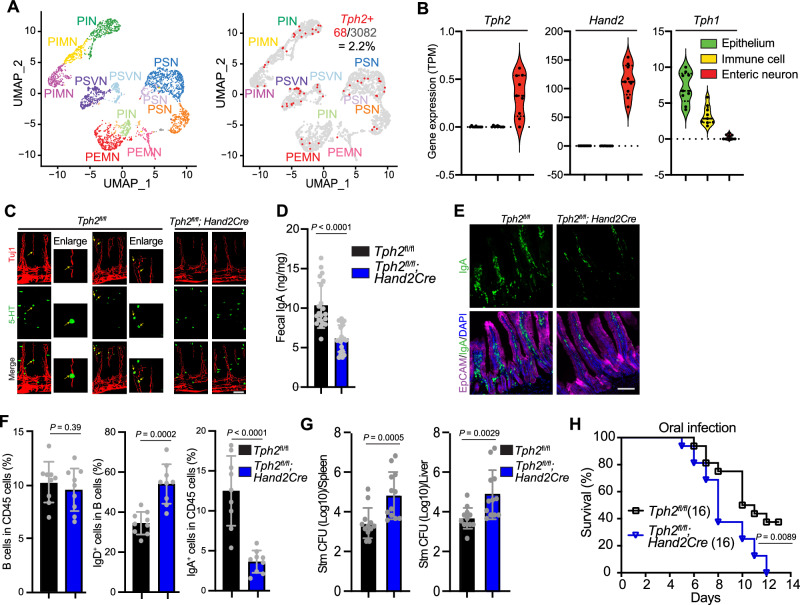
Fig. 2. Serotonin derived from enteric neurons contributes to the development of IgA B cells and mucosal defense in the intestine.
A scRNA-seq uniform manifold approximation and projection (UMAP) of Tph2+ enteric neurons from the small intestine of infant mice. Left, subtypes of enteric neurons according to ref. 61; PSN, putative sensory neurons; PIN, putative inhibitory neuron; PIMN, putative inhibitory motor neurons; PEMN, putative excitatory motor neurons; PSVN, putative secretomotor/vasodilator neurons were defined according to61. Right, distribution of Tph2 transcripts among subsets of enteric neurons. B Detection of Tph2, Hand2, and Tph1 in bulk RNA-seq analysis of the intestinal epithelium, lamina propria immune cells, and enteric neurons (n = 9 mice); TPM, Transcripts Per Million. C Representative whole-mount staining of small intestine from Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. Neurons are detected with Tuj1 (red) and 5-HT positive cells with anti-serotonin antibody (green). Yellow arrows point to enteric serotonergic neurons (round-shaped cells) in the lamina propria, where serotonin co-localizes with Tuj1. The triangular-shaped serotonin positive cells observed in both Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice likely represent enterochromaffin cells. Scale bar, 100 μm. Similar results were obtained in at least 5 animals. D Fecal IgA levels in Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice (n = 21). E Representative immunostaining of small intestine sections from Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. Epithelial cells are detected with EpCAM (magenta), IgA cells with anti-IgA antibody (green), and nuclei with DAPI (blue). Scale bar, 100 μm. F Flow cytometry analyses of frequency of total B cells, IgD+ fraction of total B cells, and IgA+ cells in the lamina propria CD45+ cells from the small intestine of Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice (n = 9). G STm CFU burdens in spleens and livers of Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice 5 days post oral inoculation (n = 12). H Kaplan–Meier plot of survival of Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice following oral STm inoculation (n = 16). Data shown are means ± SD. Statistical analysis was performed by two-tailed Mann–Whitney test in D, F, G; and by a Log-rank test in H.
To investigate the functions of enteric serotonergic neurons, we generated a conditional knockout mouse (Tph2fl/fl; Hand2-Cre), leveraging the Hand2 promoter (Fig. 2B), which is active in neural crest-derived cells including enteric neurons and other neurons in the PNS25–27, but not in the brain28. We confirmed that Tph2 transcripts were absent in the gut but preserved in the brain in Tph2fl/fl; Hand2-Cre mice (Supplementary Fig. 4D), establishing that these animals are deficient in the expression of serotonin synthesis gene Tph2, at least in the enteric neurons. To further demonstrate the presence of enteric serotonergic neurons, we carried out whole-mount staining of cleared small intestine. Colocalization of serotonin and Tuj1, a neuronal cell marker, was observed within lamina propria neurons in Tph2fl/fl but not in Tph2fl/fl; Hand2-Cre animals (Fig. 2C and Supplementary movie 1). Moreover, previous research utilizing a radioenzymatic method29 also reported the detection of enteric serotonergic neurons. The network of neuronal fibers in the myenteric plexus in Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice appeared similar (Supplementary Fig. 4E), and comparable neuronal gene expression patterns were found in Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice (Supplementary Fig. 4F). Together, these results suggest that serotonin produced by enteric neurons is not essential for the formation of the myenteric plexus and are consistent with studies of Tph2−/− mice that showed the absence of Tph2-expressing neurons in the brain does not grossly influence brain development30,31.
Like the Tph2−/− mice, a reduction of fecal IgA (Fig. 2D) and small intestinal IgA+ B cells was also observed in the Tph2fl/fl; Hand2-Cre mice (Fig. 2E and Supplementary Fig. 4G). FACS analysis revealed that there were increased IgD+ B cells and decreased IgA+ B cells in the conditional KO animals (Fig. 2F and Supplementary Fig. 4H). The reduced abundance of IgA+ B cells seemed to be restricted to the small intestinal lamina propria, as the number of IgA+ B cells was similar in Peyer’s Patches (PP) and mesenteric lymph nodes (MLN) from Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice (Supplementary Fig. 4I). These data suggest that intestinal serotonergic neurons promote the development of IgA+ B cells from IgD+ precursors in the lamina propria of the small intestine.
Finally, we sought to investigate the role of intestinal serotonergic neurons in host defense. After oral infection with Salmonella, Tph2fl/fl; Hand2-Cre mice had increased pathogen burdens in the spleen and liver (Fig. 2G) and reduced survival compared with co-housed littermate controls (Fig. 2H), suggesting that intestinal serotonergic neurons inhibit pathogen dissemination by augmenting the defense of intestinal barriers. Although direct comparison of the increased susceptibility to Salmonella in Tph2−/− and Tph2fl/fl; Hand2-Cre animals is not possible due to differences in their microbiota (Supplementary Fig. 3), the similarity in their phenotypes suggests that the absence of serotonin derived from intestinal neurons may largely account for the intestinal immune deficits observed in the whole-body Tph2 KO animals.
Serotonin remodels lamina propria DC function via the HTR7 receptor
To begin to assess how intestinal serotoninergic neurons modulate immune cell function, we analyzed the gene expression profiles of sorted small intestinal lamina propria (SiLP) immune cells (CD45+) and found that HTR7 is the predominant serotonin receptor expressed in these cells (Fig. 3A). Re-analyses of single-cell RNA-seq data of SiLP immune cells32 revealed that Htr7 expression is primarily restricted to lamina propria dendritic cells (LPDC) (Fig. 3B), which was further confirmed by our FACS analysis of surface HTR7 expression in the SiLP-derived T cells, B cells and DC (Fig. 3C). Thus, this G-protein coupled receptor likely enables LPDC to respond to serotonin produced by serotonergic neurons. Consistent with this idea, the gene expression profiles of SiLP CD45+ cells showed that Tph2−/− mice exhibited lower expression of genes linked to DC differentiation compared to controls (Fig. 1C, D). Furthermore, FACS-based immune profiling revealed that both whole-body and conditional KO animals had a reduced abundance of LPDC compared to the respective littermate controls (Fig. 3D and Supplementary Fig. 5A).
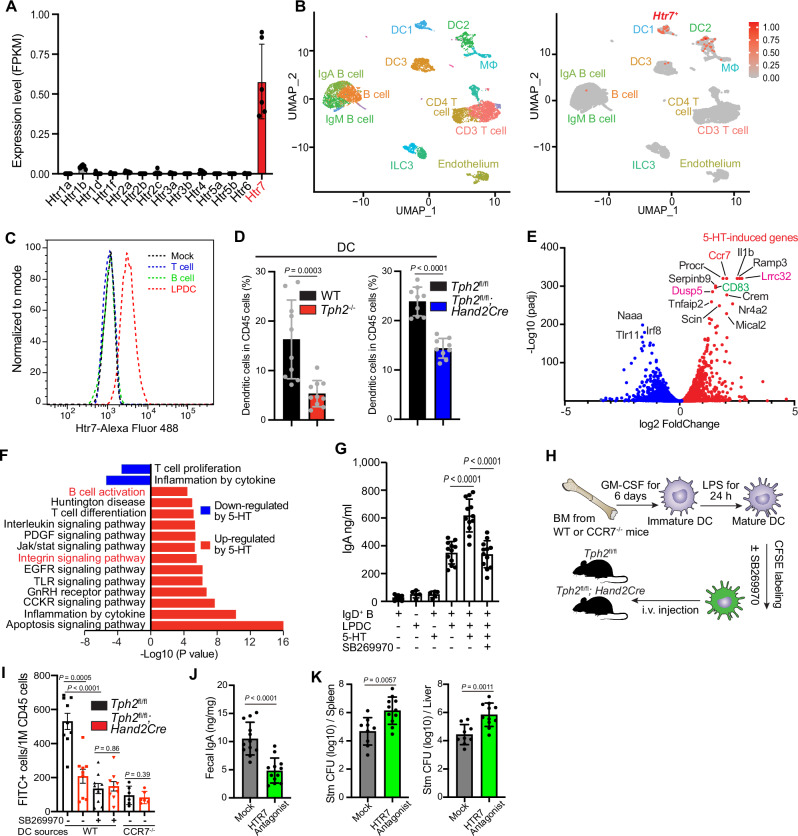
Fig. 3. Serotonin promotes retention and remodeling of DC function through HTR7 signaling and stimulates DC-dependent IgA B cell development.
A HTR7 is the dominant serotonin receptor in lamina propria CD45+ cells. FPKM (Fragments Per Kilobase of transcript per Million fragments mapped) values of all serotonin receptors in lamina propria CD45+ cells. n = 6 mice. B UMAP plot of single-cell transcriptome data32 of small intestinal lamina propria immune cells showing that expression of the Htr7 gene is restricted to LPDC cells. C Flow cytometry analyses of HTR7 expression in small intestinal lamina propria T cells, B cells, and DC. D Flow cytometry analyses of frequency of DC (Live, CD45+, MHC-II+, CD64−, CD11c+) in lamina propria CD45+ cells from the small intestine of mice with the indicated genotypes (n = 10 in WT and Tph2−/− group, n = 9 in Cre+/−; Tph2fl/fl group). E Differential gene expression in LPDCs treated with serotonin ±HTR7 antagonist SB269970. DESeq2 was used to calculate fold-change and adjusted p-value. Red points represent genes that exhibited significantly increased expression in the serotonin treatment group compared to the group treated with serotonin along with the HTR7 antagonist, while blue points indicate genes that showed significantly decreased expression in the serotonin treatment group compared to the group treated with serotonin along with the HTR7 antagonist. F Gene Ontology pathway analysis of data from E. G Tissue culture assay of IgA production from IgD+ B cells that were cocultured with LPDC, serotonin, and a HTR7 antagonist (SB269970) as indicated. The levels of IgA in the supernatants were measured by ELISA after 6 days of coculture (n = 12). Data are representative of three independent experiments. H Schematic of the system used to analyze BMDC homing to the gut in Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. Equal numbers of CFSE-labeled mature WT or CCR7−/− BMDC were transplanted into Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice and the CFSE+ cells in different tissues were analyzed 18 h post-transplantation. I Frequency of CFSE+ BMDC among CD45+ cells in the lamina propria of Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. HTR7 antagonist SB269970 was used to inhibit the HTR7 signaling pathway (n = 9), while CCR7−/− cells were employed to block CCR7-dependent signaling (n = 6). J Fecal IgA levels in mock and HTR7 antagonist-treated mice. The mice were treated with either i.p PBS or an HTR7 antagonist every other day for 10 days. Fecal IgA measurements were carried out after the 10-day HTR7 antagonist treatment. n = 12 mice per group. K STm CFU burdens in spleens and livers of mock and HTR7 antagonist-treated mice 5 days post oral inoculation. The mice were treated as described in J before oral Salmonella infection. n = 9 mice in the mock and n = 11 mice in the treated group. Data shown are means ± SD. Statistical analysis was performed by a two-tailed Mann–Whitney test in D, G, and I–K.
To further characterize the effect of serotonin on LPDC, we treated FACS-isolated LPDC33 in tissue culture with either 5-HT or a combination of serotonin and the serotonin receptor HTR7 antagonist SB269970 and analyzed their gene expression profiles. The abundance of 160 transcripts was increased >2-fold (adjusted p-value < 10−5) in a HTR7-dependent manner (Fig. 3E). Many of the serotonin-induced, HTR7-dependent pathways were associated with immune regulation (Fig. 3F). Consistent with our findings of reduced B cell maturation and LPDC abundance in the Tph2fl/fl; Hand2-Cre mice, these genes and pathways included loci linked to DC activation, such as Cd8334 (Fig. 3E and Supplementary Fig. 5B), integrin signaling (Fig. 3F), which is associated with immune cell adhesion35, as well as genes linked to DC-mediated activation and/or differentiation of B cells. The latter set of genes included Cd4036, Il637, and Lrrc32 (Fig. 3E and Supplementary Fig. 5C), a protein that promotes TGF-β activity38,39 that is linked to stimulation of IgA class switching40.
Co-culture experiments were used to test the hypothesis that serotonin-treated LPDC can promote the differentiation of IgD+ B cells to IgA-secreting cells. Co-culture of IgD+ B cells with LPDC triggered IgA production as described37; furthermore, the addition of serotonin augmented the abundance of IgA measured in supernatants (Fig. 3G). Serotonin stimulation of LPDC-mediated IgA production was ablated by an HTR7 antagonist, demonstrating that the effect of this neurotransmitter relies on HTR7-dependent signaling pathways. Together, these observations suggest that serotonin remodels LPDC function to promote IgA class switching.
The reduced abundance of LPDC in the Tph2fl/fl; Hand2-Cre mice could at least in part be due to reduced homing/retention of circulating DC in the intestine41. We used an in vivo DC homing assay (Fig. 3H), to test the hypothesis that enteric serotonergic neurons (ESN) promote DC homing/retention to the small intestine lamina propria as well as to PP and MLN. There was a greater abundance of labeled DC in the lamina propria of Tph2fl/fl vs Tph2fl/fl; Hand2-Cre mice (Fig. 3I and Supplementary Fig. 5D), suggesting the presence of ESN in the lamina propria may promote the retention of DC in this site. In contrast, no difference in the recruitment of labeled bone-marrow derived DC to the MLN or PP of Tph2fl/fl vs Tph2fl/fl; Hand2-Cre mice (Supplementary Fig. 5E) was observed, indicating that the lymphoid tissue homing of DC is intact in the conditional KO mice. Furthermore, pretreatment of DC with an HTR7 antagonist prior to their intravenous injection reduced their abundance in the lamina propria (Fig. 3I and Supplementary Fig. 5D), suggesting that serotonin signaling through HTR7 on DC promotes the residency of these cells in the small intestine lamina propria. Since CCR7, which has been associated with DC homing to MLN and potentially to ectopic lymphoid tissue in the mucosa as well42, was significantly induced by serotonin treatment of LPDC (Fig. 3E), we evaluated the role of this chemokine receptor in DC gut retention in the lamina propria. DCs derived from the bone marrow of CCR7-deficient animals had deficient homing and/or retention to the lamina propria of both WT and conditional KO mice, suggesting that this serotonin-induced receptor plays a crucial role in DC gut homing and/or retention to the lamina propria. This mechanism could account for the reduced abundance of LPDC in mice deficient in Tph2 in ESN. Together, these observations suggest a new axis of interaction between ESN and the immune system: serotonin derived from enteric neurons promotes both retention and remodeling of DC function through HTR7 signaling, which in turn could induce IgA+ B cell development.
We also measured the effect of the HTR7 antagonist on IgA B cell differentiation and Salmonella infection, to use a non-genetic approach to probe the importance of serotonin-HTR7 interactions in vivo. We found that animals treated with the HTR7 antagonist phenocopied the conditional Tph2 KO mice in that they exhibited decreased levels of fecal IgA (Fig. 3J) and increased susceptibility to Salmonella infection (Fig. 3K). Although the HTR7 antagonist could also block the effects of serotonin produced by cells other than neurons, these findings provide additional support for the role of the HTR7 signaling pathway in the pDC-IgA-Salmonella susceptibility circuitry.
Intestinal serotonergic neurons control the abundance and function of lamina propria pDC
We hypothesized that in vivo ESN-derived serotonin remodels LPDC function in an HTR7-dependent manner. To test this idea, LPDC from Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice were isolated by positive selection for single-cell RNA-seq (Supplementary Fig. 6A). While the fraction of MHCII+ cells was similar in the Tph2fl/fl; Hand2-Cre mice and WT controls, there was a lower proportion of LPDC in the conditional KO animals (Supplementary Fig. 6B–D), as observed above by FACS-based analysis (Fig. 3D). Seven clusters of CD11c+ cells were identified (Fig. 4A), including plasmacytoid dendritic cell (pDC), conventional DC type 1 (cDC1) and conventional DC type 2 (cDC2) based on marker gene expression43(Fig. 4B). Both pDC and cDC1 were found to express Htr7, whereas cDC2 cells expressed very low levels of this serotonin receptor (Fig. 4C). Among LPDC, the proportion of pDC was reduced in Tph2fl/fl; Hand2-Cre mice vs Tph2fl/fl animals (44% to 25%), but the fraction of cDC1 was similar in the two groups (Fig. 4D). Together, these findings suggest that interactions between 5-HT produced by ESN and the HTR7 serotonin receptor on pDC promote the homing to and/or survival of pDC in the lamina propria of the small intestine.
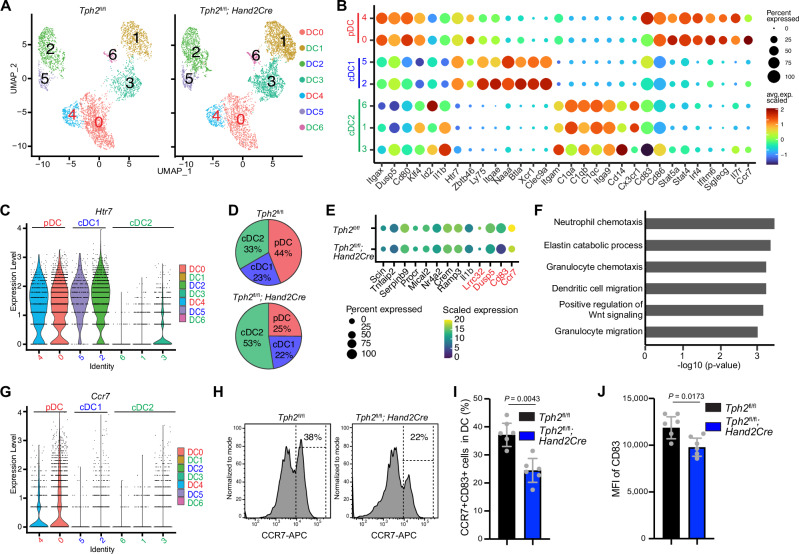
Fig. 4. Enteric serotonergic neurons remodel pDC function in vivo.
A UMAP plot of single-cell transcriptome data of small intestinal LPDC from Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. B Marker gene expression used for annotation of LPDC subsets. C Violin plots depicting the range of expression levels of Htr7 in distinct LPDC clusters. D Pie charts showing the proportion of pDC is decreased in Tph2fl/fl; Hand2-Cre vs Tph2fl/fl mice. E Comparison of the expression of the indicated genes in pDC between Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. The dot color reflects the level of gene expression, and the dot size represents the percentage of cells expressing the indicated gene. The genes labeled in red exhibit decreased expression in pDC from Tph2fl/fl; Hand2-Cre mice and are consistent with the serotonin-induced genes observed in vitro. F GO Pathway analysis of genes that exhibited decreased expression in pDCs of Tph2fl/fl; Hand2-Cre vs Tph2fl/fl mice. G Violin plots depicting the range of expression levels of Ccr7 in distinct LPDC clusters. H Representative histogram plots showing the percentage of pDC (Live, CD45+, MHC-II+, CD64−, CD11c+, CCR7+) in LPDC from the small intestine of Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice by flow cytometry. I Flow cytometry analyses of frequency of pDC in LPDC from the small intestine of Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. n = 6 mice per group. J Flow cytometry analyses of CD83 expression on pDC from the small intestine of Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. MFI mean fluorescence intensity. n = 6 mice per group. Data shown are means ± SD. Statistical analysis was performed by a two-tailed Mann–Whitney test in I and J.
Additional comparisons of the sc-RNA-seq data showed that some of the most highly serotonin-induced genes in LPDC in vitro (Fig. 3E) exhibited reduced expression in pDC in vivo in Tph2fl/fl; Hand2-Cre mice vs control animals; these genes included TGF-β activator Lrrc32, DC activation marker Cd83, Dusp5 as well as Ccr7 (Fig. 4E). These comparisons of gene expression in pDC from Tph2fl/fl; Hand2-Cre vs Tph2fl/fl mice also uncovered reduced expression of genes implicated in chemotaxis and migration, further buttressing the idea that ESN play critical roles in pDC homing and/or retention (Fig. 4F). Among LPDC, only pDC expressed Ccr7 (Fig. 4G), a chemokine receptor that plays a critical role in cell-cell interaction44,45. Thus, the reduced homing/retention of pDC in the lamina propria may, in part, be attributable to reduced Ccr7 expression in these cells (Figs. 3E, I, 4E, F). CCR7 is also a useful cell surface marker for pDC46 and FACS analysis of CCR7+ LPDC confirmed the reduction in the abundance of pDC in the Tph2fl/fl; Hand2-Cre mice compared to the control animals (Fig. 4H, I and Supplementary Fig. 6E–G). Similar FACS analysis confirmed the reduction of the pDC activation marker CD83 in the Tph2fl/fl; Hand2-Cre mice (Fig. 4J), providing further verification of the scRNA-seq results. Collectively, these observations are consistent with the idea that serotonin derived from ESN stimulates the expression of genes linked to the homing/retention and differentiation of a specific subset of LPDC, plasmacytoid dendritic cells, supporting the concept that there are functionally important interactions between ESN and pDC in vivo.
Bidirectional communication between enteric neurons and LPDC
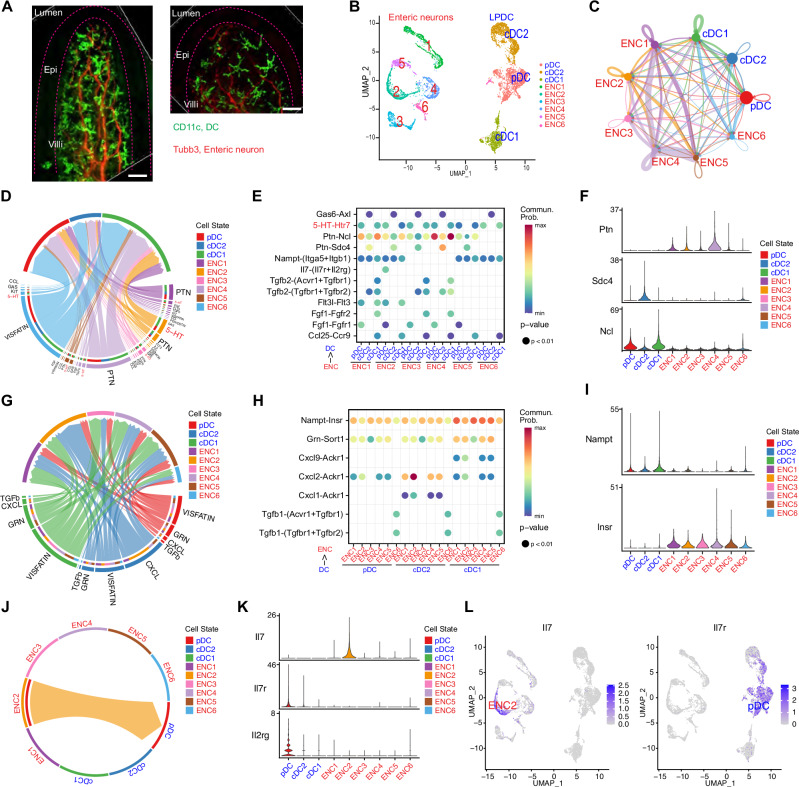
Our understanding of how interactions between the ENS and the gut innate immune system contribute to intestinal homeostasis is limited. Whole-mount immunofluorescence imaging of small intestinal villi was used to first address whether DC are found in close proximity to enteric neurons. Neuronal projections ramifying within the lamina propria were often observed in close proximity to LPDC, suggesting that interactions between these cell types are plausible (Fig. 5A).
Fig. 5. Bidirectional communication between enteric neurons and LPDC.
A Representative whole-mount immunostaining of small intestine villi from CD11c-DTR/GFP mice. LPDC are marked with CD11c (green), and neuronal projections are labeled with anti-Tubb3 antibody (Red). Scale bar, 20 μm. Similar results were obtained in at least 5 animals. B UMAP plot of single-cell transcriptome data of enteric neurons and LPDC generated in this study that was used for analyzing cell-cell communication with CellChat. C Circle network diagram of significant cell-cell interaction pathways. Arrows and line color indicate direction (ligand: receptor) and line thickness indicates the strength of the predicted interaction. The round loops represent the interactions within the same cell type. D–F Enteric neurons to LPDC communication pathways. D Chord diagram showing all the significant interactions from enteric neurons to LPDC. E Dot plot showing the key ligand-receptor interactions in inferred communication pathways between subsets of enteric neurons and LPDC. Empty spaces indicate that the communication probability is zero. p-values were computed with a one-sided permutation test. The color scale represents communication probability as calculated in CellChat. F Violin plots illustrating the gene expression levels of the PTN signaling pathway, with ligand expression in enteric neuron clusters and receptor expression in LPDC clusters. G–I LPDC to enteric neurons communication pathways. G Chord diagram showing all the significant interactions from LPDC to enteric neurons. H Dot plot showing the key ligand-receptor interactions in inferred communication pathways between subsets of LPDC and enteric neurons. Empty spaces indicate that the communication probability is zero. p-values were computed with a one-sided permutation test. The color scale represents communication probability as calculated in CellChat. I Violin plots illustrating the gene expression levels of the Nampt-Insr signaling pathway, with ligand expression in LPDC clusters and receptor expression in enteric neuron clusters. J Chord diagram displaying the communication network between putative enteric sensory neurons and pDC, highlighting the targeting of Il7 from enteric sensory neurons to the Il7r located on the pDC. K Violin plots illustrating the gene expression levels of the IL7 signaling pathway, with ligand expression in enteric sensory neurons and receptor (a heterodimer of Il7r and Il2rg) expression in pDC. L UMAP plot derived from single-cell transcriptome data showing expression of Il7 in enteric sensory neurons (left) and Il7 receptor in pDC (right).
We used CellChat47 to infer and analyze the potential intercellular communication networks within the ENS-innate immune axis. For these analyses, the scRNA-seq data from the 4347 enteric neurons and 3284 LPDC sequenced in this study were utilized (Fig. 5B and Supplementary Fig. 7A). While most of the cell-cell interaction pathways detected in these analyses were between neuron subtypes, predicted interactions between neurons and DCs and between DC subtypes were also found (Fig. 5C). Generally, enteric neurons and LPDCs appeared to rely on distinct pathways for communication (Supplementary Fig. 7B).
Among the ligand-receptor interactions between enteric neurons and DCs respectively inferred by these analyses (Fig. 5D, G), we uncovered significant interactions driven by neuronal production of ‘immune’ ligands such as Il7, Flt3l and Ccl25 and expressed DC receptors, Il7R, Flt3, and Ccr9, that are known to regulate DC function48 (Fig. 5D, E). Interactions between neuronal Ptn, a ligand linked to growth and cytokine regulation49, and Ncl and Sdc4 receptors on LPDC were the most significant interaction detected (Fig. 5E, F and Supplementary Fig. 7C), suggesting that enteric neurons play a role in controlling proliferation/activation of LPDC. Notably, these analyses independently predicted the ENS-DC interaction through the serotonin-HTR7 pathway (Fig. 5D, E).
LPDC produced ligands, including several chemokines were predicted to interact with chemokine receptors, such as Ackr1, on enteric neurons (Fig. 5G, H), suggesting that innate immune cells regulate ENS function. LPDC also appear to control neuronal energy homeostasis, since the Nampt/Visfatin-Insulin receptor pathway was the most significant predicted interaction (Fig. 5H, I and Supplementary Fig. 7D).
Finally, these analyses identified putative interactions between specific neuron and LPDC clusters. For example, Il7 expression was restricted to enteric neuron cluster 2, putative sensory neurons, while IL7 receptors expression was exclusive to pDC (Fig. 5J–L), suggesting that enteric sensory neurons may control the development of this DC subset50. Although additional studies to validate this interaction and to elucidate its significance are necessary, this computational approach strongly suggests that there is a larger range of bidirectional crosstalk between enteric neurons and innate immune cells than was appreciated.
Discussion
Here, we uncovered a new role of neuronal serotonin in immune homeostasis at the intestinal mucosal barrier. Our findings suggest that serotonergic neuronal circuits, which are thought to function in regulation of emotion, also play a role in governing intestinal innate immune defense. Mechanistic studies showed that serotonin produced by neurons in the intestine targets the HTR7 receptor on LPDC. Interactions between 5-HT and HTR7 appear to promote the homing/retention and differentiation of a specific subset of DC, pDC, which are known to promote B cell class switching51. Thus, deficiencies in pDC abundance and function in the absence of intestinal neuronal serotonin signaling likely account for the reduction in IgA B cells and fecal IgA observed in the Tph2fl/fl; Hand2-Cre mice. Deficiencies in pDC and reduced IgA could both contribute to the increased susceptibility of the conditional KO mice to oral infection with Salmonella; deficiencies in other cell types could also impact susceptibility to Salmonella. Thus, these studies begin to uncover molecular pathways by which serotonergic neuronal circuits, which have been linked to the control of emotion, also impact immune function.
Whole-body and conditional Tph2 KO animals exhibit decreased gut motility52,53. It is possible that reduced gut motility could potentially contribute to the increased Salmonella burden observed in the livers and spleens of the Tph2 deficient animals. Interestingly, we found that Salmonella infection increased intestinal motility in WT mice and that Tph2 KO animals also exhibited a similar increase in gut motility with Salmonella infection (Supplementary Fig. 8A). However, even in the setting of infection, the Tph2 KO animals had reduced gut motility compared to the WT mice. Thus, the gut motility defect observed in Tph2 KO animals could contribute to their susceptibility to Salmonella. To further investigate whether changes in gut motility account for increased Salmonella burdens in distal organs, we measured the effect of an HTR7 antagonist on gut motility. Mice treated with the HTR7 antagonist did not display reduced gut motility (Supplementary Fig. 8B) but showed increased susceptibility to Salmonella infection (Fig. 3K), suggesting that gut motility is not the only factor that explains the elevated susceptibility to Salmonella infection in Tph2 KO animals.
Recent research has demonstrated that enteric neurons play roles in regulating various immune cell types, including macrophages, innate lymphocyte cells, and Treg cells14,54. Our findings illuminate a novel gut neuro-immune interaction in which serotonin, a neurotransmitter, controls LPDC function to promote IgA B cell differentiation. The HTR7 on lamina propria pDC appears to be critical for ESN to activate pDCs, suggesting that serotonin derived from enteric serotonergic neurons may account for some of the diverse immune phenotypes linked to HTR755. Notably, human scRNA-seq studies have revealed that, like mice, HTR7 is the only serotonin receptor expressed on intestinal DCs (Supplementary Fig. 8C)56,57. Thus, our findings, along with other studies58,59, raise the possibility that drugs that activate or inhibit HTR7 may be useful as immunomodulatory agents for treating human enteric infections as well as for managing inflammatory bowel disease. Furthermore, our findings may explain some of the observed adverse outcomes in patients with Tph2 gene variants, including susceptibility to viral infection16.
Additional studies are required to decipher whether signaling between ESN and pDC is through a synapse-like mechanism, where there is a direct interaction between pDC and ESN, or via a less direct pathway that ultimately promotes pDC retention and activation in the small intestinal lamina propria (Supplementary Fig. 8D). Whole mount immunofluorescence imaging revealed that there is close apposition of intestinal neurons and DC, suggesting that a direct ESN-pDC interaction is possible. Regardless of the precise mechanism through which serotonergic neurons in the intestine control pDC function, the absence of Tph2-derived serotonin in the intestine impaired mucosal defense against Salmonella, demonstrating the importance of these neuronal circuits in host defense. Furthermore, it will be intriguing to investigate whether serotonin derived from enterochromaffin cells affects DC and B cell function.
Gene expression profiling uncovered the cell-type specificity of the expression of serotonin receptors. Enteric sensory neurons expressed Htr3a (Supplementary Fig. 7E, F), whereas Htr4 was expressed in intestinal epithelial cells (Supplementary Fig. 7G, H), and Htr7 in LPDC (Fig. 3A–C). Although further investigation is warranted, it may be possible to develop drugs that specifically bind these receptors, enabling precise targeting of specific cell types in the intestine. Engineering these compounds so that they are unable to penetrate the blood-brain barrier could prevent untoward central nervous system-related side effects.
Bioinformatic analyses using CellChat and similar pipelines60 to systematically and quantitatively infer intercellular communication networks will be invaluable for deciphering neuro-immune interactions. The predicted interactions between enteric neurons and innate immune cells that we uncovered suggest that there is a complex bidirectional dialogue between specific subsets of enteric neurons and DC. Functional analyses based on these inferences will reveal new insights into the roles of the enteric nervous system in innate immune regulation, as well as the potential remodeling of enteric neuronal function by innate immune cells.
Methods
Mice
C57BL/6 (Strain #:000664), Tg(Uchl1-HISTH2BE/mCherry/EGFP*)Fsout/J (Strain #:016981), CD11c-DTR/GFP (Strain #:004509), Sert−/− (Strain #:008355), Ccr7−/− (Strain #:006621) and Tph2flox/flox mice (Strain #:027590) were purchased from the Jackson Laboratory (Bar Harbor, ME, USA); Tph2−/− mice were a generous gift from Dr. Gerard Karsenty (Columbia University, NY, USA); Hand2-Cre transgenic mice were a generous gift from Dr. Ruaidhrí Jackson (Harvard Medical School, MA, USA). Tph2flox/flox mice were backcrossed to C57BL/6J background for at least six generations. All the experimental and control animals were co-housed, maintained on a 12-hour light/dark cycle and a standard chow diet at the Harvard Institute of Medicine specific pathogen-free (SPF) animal facility. The mice were euthanized by cervical dislocation following an overdose of isoflurane inhalation. Both male and female mice, 6–8 weeks old, were used unless otherwise specified in the figure legend. Animal experiments were performed according to guidelines from the Center for Animal Resources and Comparative Medicine at Harvard Medical School. All protocols and experimental plans were approved by the Brigham and Women’s Hospital Institutional Animal Care and Use Committee (Protocol #2016N000416).
Isolation and purification of nuclei from enteric neurons
The isolation of enteric neurons from Tg(Uchl1-HISTH2BE/mCherry/EGFP*) Fsout/J mice was performed as previously described61. Briefly, fresh-frozen intestinal tissues were disaggregated in 1 mL of CST buffer (0.49% (w/v) CHAPS (220201, EMD Millipore), 146 mM NaCl (S6546, Sigma), 1 mM CaCl2 (97062-820, VWR), 21 mM MgCl2 (M1028, Sigma), 10 mM Tris pH 8.0 (AM9855G, Thermo Fisher) with mild chopping using scissors for 10 minutes on ice. Large debris was removed with a 40 μm strainer (Falcon). The isolated nuclei were stained with 4’,6-diamidino-2-phenylindole (DAPI, D1306, Thermo Fisher Scientific) and sorted as DAPI+, mCherry+ nuclei using an SH800 Cell Sorter (Sony Biotech). The purified nuclei were used for single-nucleus RNA-seq or bulk RNA-seq analysis.
Intestinal epithelium and immune cell isolation and purification
Colonic and small intestinal tissues were dissected, and Peyer’s patches were discarded. The epithelium was isolated by 250 g stirring at 37 °C in RPMI medium (61870036, Gibco) containing 5 mM EDTA (AM9260G, Invitrogen), 1 mM dithiothreitol (10197777001, Sigma) and 2% (vol/vol) FBS (10082147, Gibco) for 15 min. The isolated epithelium was used for bulk RNA-seq analysis.
To isolate lamina propria lymphocytes, the epithelium-depleted intestinal tissues were washed in RPMI medium with 5% (vol/vol) FBS, further minced into small pieces, and then digested by 250 rpm stirring at 37 °C in RPMI medium containing collagenase D (0.5 mg/ml, 11088866001, Sigma), Dispase II (0.5 mg/ml, 17105041, Gibco), DNase I (50 ug/ml, 10104159001, Roche) and 5% (vol/vol) FBS for 40 min. The digested tissues were filtered, and lamina propria cells were collected by centrifugation. The pellets were resuspended, and the lamina propria lymphocytes were isolated by Percoll (40%/80%, GE17-0891-01, GE Healthcare) gradient centrifugation. Mesenteric lymph nodes and Peyer’s patches were mechanically disrupted. The purified immune cells were used for FACS analysis and sorting. The sorted CD45+ cells were used for bulk RNA-seq analysis.
FACS analysis and cell sorting
All the antibodies used in this study are listed in Supplementary Table 1. Single-cell suspensions were blocked with an antibody against CD16/32 (2.4G2, Becton Dickinson) and then stained with LIVE/DEAD™ fixable aqua cell stain kit (L34957, Invitrogen), and antibodies against CD45 (30-F11), MHC-II (M5/114.15.2), CD64 (X54-5/7.1), CD11c (HL3), CCR7 (4B12), CD83 (Michel-19), B220 (RA3-6B2), IgD (11-26c), and IgA (C10-3) all from Becton Dickson. Anti-HTR7 polyclonal antibody is from MyBiosource, stained cells were analyzed with a FACSymphony analyzer (Becton Dickson) or sorted on an SH800 Cell Sorter; analyses were performed with FlowJo software (v10.8).
Single nucleus RNA-Seq
The 10× Genomics protocol was performed on a single sorted enteric nucleus as described61. Libraries were generated using Chromium Next GEM Single Cell 3ʹ Reagent Kits v3.1 (10×) according to the manufacturer’s protocol; library quality was assessed by the Tapestation High Sensitivity D5000 ScreenTape (Agilent) and sequenced using a NextSeq 500 sequencer (Illumina). Data analysis was performed using the 10× Genomics Cloud Analysis Cell Ranger pipeline and Seurat v4.3.0 with the SCT normalization method. Low-quality cells were removed by the parameters nfeature_RNA > 500, nCount_RNA > 2000 & nCount_RNA < 50000, and percent.mt <5. To generate UMAPs, we integrated our data with published small intestine data in Drokhlyansky et al.61 and performed a principal component analysis (PCA) using RunPCA function (npcs = 50), and then cell clusters were identified using FindNeighbors (dims = 1:15) and FindClusters (resolution = 0.4) functions. RunUMAP function (dims = 1:15, n.neighbors = 15, min.dist = 0.3, spread = 1) was used to create UMAP plots. The cell-type assignment was performed using the clustifyr R package (v1.8.0, clustifyr62) based on the cell-types presented in Drokhlyansky et al.61.
Single-cell RNA-Seq of LPDC
Lamina propria lymphocytes were purified on percoll gradients from Tph2fl/fl and Tph2fl/fl; Hand2Cre mice and then DC were isolated using the EasySep™ Mouse CD11c Positive Selection Kit II (18781, StemCell). Library generation, sequencing, and data analysis were performed as described above. MHCII-negative cell clusters were computationally removed prior to analyses of MHCII+ cell clusters. LPDC cell clusters specific analyses were carried out after the computational removal of CD11c negative cell clusters.
Bulk RNA-seq and data analysis
Purified epithelial and immune cells were lysed in Trizol (15596018, Invitrogen), and RNA was extracted with the RNeasy mini Kit (74106, Qiagen) according to the manufacturer’s instructions. RNA-seq libraries were prepared using the KAPA mRNA HyperPrep kit (50-196-5308, Roche) or NEBNext Multiplex Oligos for Illumina kit (E7335L, NEB). Libraries were analyzed using a High Sensitivity D1000 ScreenTape (Agilent) and sequenced on a NextSeq 550 or 1000/2000 (Illumina). For data analysis, reads were trimmed using Trim Galore with automatic adapter sequence detection. Then, trimmed reads were mapped to the mouse reference genome (mm10) and annotated using STAR v2.7.3a with default parameters. The number of mapped reads to each gene was counted by featureCounts of the Subread package using mouse GENCODE annotation M25 (GRCm38.p6). Transcripts Per Kilobase Million (TPM) were calculated by dividing the number of read counts by the length of the gene in kilobases to yield reads per kilobase. Fragments Per Kilobase of transcript per Million fragments mapped (FPKM) were also calculated as described63. Differentially expressed genes were identified using the R-package DESeq2 (v1.36.0) with an adjusted p-value < 0.05.
Histology, whole-mount staining and tissue immunofluorescence
For immunofluorescence analysis, samples from the small intestine were collected and flushed with PBS and fixed in 4% PFA followed by washing with PBS. Tissue samples were then soaked in 30% sucrose and embedded in Optimal Cutting Temperature Compound (23-730-571, Fisher Scientific) and stored at −80 °C before sectioning on a CM1860 UV cryostat (Leica). 8 μm-thick slides were stained with FITC-anti IgA (C10-3, Becton Dickson) and Percp/cy5.5 anti-EpCAM (G8.8, Biolegend) antibodies at 4 °C overnight in PBS. Nuclei were stained with DAPI at RT for 5 min in the dark. For whole-mount staining of villi, a small segment of the proximal small intestine of CD11c-DTR/GFP mice was removed and placed in ice-cold PBS and then transferred to a Sylgard (Dow-Corning)-coated Petri dish. The intestine was opened along the mesenteric border and pinned flat, the tissue was stained overnight with Alexa Fluor 568 anti-Tubulin β3 antibody (TUJ1, Biolegend) as well as Alexa Fluor 488 anti-GFP antibody and rinsed in PBS before imaging. For staining of myenteric plexuses, the intestine was opened along the mesenteric border and pinned flat, and then the mucosa and submucosa were removed with forceps to expose the muscularis propria layer. The resulting muscularis propria preparation was stained overnight with Alexa Fluor 647 anti-Tubulin β3 antibody (TUJ1, Biolegend) and rinsed in PBS before imaging with an Eclipse Ti confocal microscope with a 20× objective (Nikon).
For whole-mount staining, freshly dissected small intestine was fixed with 4% PFA overnight on ice. The tissues were bleached by 6% hydrogen peroxide in methanol in 4 °C for 1 h and blocked by 1% donkey serum in PBSGT (0.5%Triton X-100, 0.2% Gelatin in PBS) for 2 days with shaking in a 37 °C incubator. After incubating with primary antibodies against Tuj1 and 5-HT in PBSGT for 1 day in the dark at 37 °C incubator with shaking, samples were washed and cleared by Dichloromethane and Ethyl. Tissues were then laid on slides and sealed under a coverslip. Z stack images were acquired on an Olympus Stella Confocal microscope.
ELISA for fecal IgA
Fresh mouse feces were homogenized in 10× volume (v/w) of PBS containing the protease inhibitor cocktail Complete EDTA-free (11836153001, Roche), using a bead-beater (Biospec, Bartlesville, OK, USA) for 20 s, and then centrifuged at 5000 g for 15 min at 4 °C. Supernatants were further spun down at 15,000 g for 5 min at 4 °C, and the IgA level in the final supernatant was determined using the Mouse IgA ELISA kit (88-50450-86, Thermo Fisher Scientific) according to the manufacturer’s protocol.
RT-qPCR quantification of gene expression
The brainstem and small intestine muscularis propria were isolated and lysed in Trizol (15596018, Invitrogen). RNA was purified with the RNeasy mini Kit (74106, Qiagen) according to the manufacturer’s instructions. RNA samples were treated for residual DNA contamination using Ambion Turbo DNA-free DNase (AM1907, Invitrogen). Purified RNA was reverse transcribed for quantitative RT-PCR (RT-qPCR) by adding 10 μg of total RNA to a mixture containing oligo dT (N8080128, Thermo Fisher Scientific), 25 mM dNTPs (R0191, Thermo Fisher Scientific), 0.01 M dithiothreitol, reaction buffer and 200 units of SuperScript III reverse transcriptase (18080085, Invitrogen). cDNA was diluted 1:50 in dH2O and mixed with an equal volume of target-specific primers and Roche SYBR master mix (04707516001, Roche) or TaqMan™ Gene Expression Master Mix (4369016, Applied Biosystems). Primer pairs were designed to minimize secondary structures and a melting temperature of 60 °C using the primer design software Primer 3. Primer sequences are listed in Supplementary Table 2. For data normalization, quadruplicate Ct values for each sample were averaged and normalized to Ct values of the control gene Gapdh. The relative gene expression level was determined by normalizing expression in the WT.
16S rRNA profiling of the gut microbiota
Fecal DNA was extracted from mouse fecal pellets with the QIAGEN QIAamp Fast DNA Stool Mini Kit (51604, Qiagen) according to the manufacturer’s instructions. Purified DNA samples were amplified with barcoded primer pairs: 341F and 805R. The amount of PCR products were quantified with the Qubit kit (Q32854, Invitrogen) and then the same amount of DNA from each sample was pooled for sequencing on MiSeq (Illumina). Raw sequencing data were analyzed by QIIME264. In brief, the data were imported into QIIME2 and demultiplexed and the DADA2 pipeline was used for sequencing quality control, and a feature table was constructed. The feature table was used for alpha and beta diversity analysis as well as for taxonomic analysis and differential abundance testing.
BMDC gut homing assay
Bone marrow-derived dendritic cells (BMDCs) were generated from a flushed bone marrow suspension from WT or Ccr7−/− mice as previously described65. In brief, 5 × 106 bone marrow cells from the femurs of C57BL/6J mice were cultured in 10 ml medium containing RPMI 1640 (11875093, Gibco) with 10% FBS (10082147, Gibco), β-Mercaptoethanol (21985023, Gibco), GlutaMAX (35050061, Gibco) and penicillin-streptomycin (10378016, Gibco) supplemented with 100 ng/ml granulocyte-macrophage colony-stimulating factor (GM-CSF; 315-03, PeproTech). Another 10 ml of GM-CSF-supplemented medium was added every 3 days. To generate mature BMDCs, 1 µg/ml lipopolysaccharide (LPS; LPS25, Sigma) was added to the cell suspensions on day 8 for 24 h. At day 9, mature BMDCs were harvested, and labeled with CellTrace CFSE (C34554, Thermo Fisher Scientific) and then injected intravenously into Tph2fl/fl and Tph2fl/fl; Hand2-Cre mice. Recipient mice were euthanized 18 h after injection, and lymphocytes from tissues were harvested. The number of FITC+ cells in the spleen was used to normalize the amount of input and MLN, PP and lamina propria FITC+ cells were normalized to splenic FITC to compare DC gut homing to different organs in different animals as described66.
LPDC and IgD+ B cell isolation and co-culture
C57BL/6J mice were subcutaneously injected with B16 cells secreting Flt3-L as described67. After 12 to 14 days, mice were euthanized and the small intestine lamina propria was digested as described above. Single-cell suspensions were incubated with mAbs to CD11c and IgA. Sorted LPDC (>95% CD11c+ IgA-) were resuspended at 2 × 106/ml and used immediately in co-culture assays. Naïve B cells were purified from the spleen by sorting IgD+ IgA− cells (>95% IgD+ IgA− cells). Sorted LPDC were treated with 100 uM serotonin (14927, Sigma) +/− 1uM HTR7 antagonist SB 269970 hydrochloride for 4 h and then lysed in Trizol for RNA extraction.
For co-cultures of sorted IgD+ and LPDC cells, IgD+ B cells were activated with 10 μg/ml anti-mouse IgM F(ab’)2 (Poly21571, Biolegend), either alone or plus LPDC (1:1 ratio), treated with or without 100 uM serotonin (14927, Sigma) and/or 1uM HTR7 antagonist SB 269970 hydrochloride (1612, Tocris) for 7 days. DMSO was used as a mock treatment. Then the supernatant was collected for IgA measurement as above.
In vivo HTR7 antagonist treatment
Co-housed C57BL/6J WT mice were treated with either intraperitoneal (i.p.) PBS or an HTR7 antagonist (SB269970, 10 mg/kg) every other day for 10 days. Fecal IgA measurements were carried out after the 10-day HTR7 antagonist treatment. After this treatment period, the mice were infected with Salmonella.
In vivo STm infection
Salmonella Typhimurium (SL1344, STm) were grown for ∼16 h at 37 °C with shaking and then subcultured (1:33) in lysogeny broth (LB) without antibiotics for 3 h until the cultures reached an optical density at 600 nm of 0.8. To prepare the inoculum, cultures were first pelleted at 5000 × g for 5 min. The pellets were resuspended in PBS. For oral infection, mice were fasting for 4 h before being infected orogastrically with 5 × 108 STm suspended in 100 μl PBS. For intravenous infection, mice were infected with 1 × 102 STm suspended in 100 μl PBS via the lateral tail vein. Survival was monitored by daily observation and Kaplan–Meier survival graphs were generated by Prism software (GraphPad, version 9.4.1). STm colony-forming units (CFU) in the spleen and liver were measured 5 days after infection by plating serial dilutions of homogenized tissue samples on LB plates containing 100 μg/ml streptomycin.
Cell-cell interaction analysis
We used the single-cell RNA-seq data generated from this study to analyze enteric neuron and LPDC interactions using the CellChat package47. Data analysis was performed with Seurat v4.3.0 as above except when the data was combined the resolution was set to 0.1 for FindClusters. CellChat identified differentially expressed ligands and receptors from each cell group and associated each interaction with a communication probability. Significant interactions were identified using default settings in CellChat. The results were visualized using bubble and chordal plots through the netVisual_bubble and chordDiagram functions in CellChat. The CommunicationPatterns function in the CellChat package was used to identify and visualize receptor repertoires.
Statistical methods
Statistical analyses were carried out using the two-tailed Student’s t test, two-tailed Mann–Whitney test, or Kaplan–Meier Log-rank test on GraphPad Prism5 (version 9.4.1).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Source data
Acknowledgements
We thank the members of the Waldor lab and Drs. Brandon Sit, Meenakshi Rao, Subhash Kulkarni, and Susan M. Dymecki for helpful discussions on all aspects of this project, Dr. Gerard Karsenty at Columbia University for Tph2−/− mice, Dr. Ulrich H. Von Andrian at Harvard Medical School for the B16-FLT3L cell line. Schematics and model figures in Fig. 3H and supplementary Fig. 8D were generated with BioRender.com. Research in the M.K.W. laboratory is supported by HHMI and NIH grant R01 AI-042347.
Author contributions
Conceptualization: H.L.Z., R.P.J. and M.K.W. Methodology: H.L.Z., Y.H., M.S., T.Z., and D.R.L. Investigation: H.L.Z., Y.H., M.S., T.Z., and D.R.L. Visualization: H.L.Z., Y.H., M.S., T.Z., and D.R.L. Funding acquisition: M.K.W. Supervision: M.K.W. Writing – original draft: H.L.Z. Writing – review & editing: H.L.Z. and M.K.W.
Peer review
Peer review information
Nature Communications thanks Kylie James, Javier Ochoa-Repáraz and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Data availability
All scRNA-seq, bulk RNA-seq datasets and 16S sequencing data generated here have been deposited into the NCBI Gene Expression Omnibus database under accession number GSE227340. https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=%20GSE227340 Source data are provided with this paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-024-53545-2.
References
- 1.Berger, M., Gray, J. A. & Roth, B. L. The expanded biology of serotonin. Annu. Rev. Med.60, 355–366 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walther, D. J. et al. Synthesis of serotonin by a second tryptophan hydroxylase isoform. Science299, 76 (2003). [DOI] [PubMed] [Google Scholar]
- 3.Teissier, A. et al. Activity of Raphe Serotonergic Neurons Controls Emotional Behaviors. Cell Rep.13, 1965–1976 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang, X., Beaulieu, J. M., Gainetdinov, R. R. & Caron, M. G. Functional polymorphisms of the brain serotonin synthesizing enzyme tryptophan hydroxylase-2. Cell Mol. Life Sci.63, 6–11 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mosienko, V. et al. Exaggerated aggression and decreased anxiety in mice deficient in brain serotonin. Transl. Psychiatry2, e122 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brommage, R. et al. Adult Tph2 knockout mice without brain serotonin have moderately elevated spine trabecular bone but moderately low cortical bone thickness. Bonekey Rep.4, 718 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amireault, P., Sibon, D. & Cote, F. Life without peripheral serotonin: insights from tryptophan hydroxylase 1 knockout mice reveal the existence of paracrine/autocrine serotonergic networks. ACS Chem. Neurosci.4, 64–71 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salvan, P. et al. Serotonin regulation of behavior via large-scale neuromodulation of serotonin receptor networks. Nat. Neurosci.26, 53–63 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gershon, M. D., Drakontides, A. B. & Ross, L. L. Serotonin: Synthesis and Release from the Myenteric Plexus of the Mouse Intestine. Science149, 197–199 (1965). [DOI] [PubMed] [Google Scholar]
- 10.Morarach, K. et al. Diversification of molecularly defined myenteric neuron classes revealed by single-cell RNA sequencing. Nat. Neurosci.24, 34–46 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Del Colle, A., Israelyan, N. & Gross Margolis, K. Novel aspects of enteric serotonergic signaling in health and brain-gut disease. Am. J. Physiol. Gastrointest. Liver Physiol.318, G130–G143 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chu, C., Artis, D. & Chiu, I. M. Neuro-immune Interactions in the Tissues. Immunity52, 464–474 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoo, B. B. & Mazmanian, S. K. The Enteric Network: Interactions between the Immune and Nervous Systems of the Gut. Immunity46, 910–926 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chavan, S. S., Pavlov, V. A. & Tracey, K. J. Mechanisms and Therapeutic Relevance of Neuro-immune Communication. Immunity46, 927–942 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fairbrass, K. M. et al. Bidirectional brain-gut axis effects influence mood and prognosis in IBD: a systematic review and meta-analysis. Gut71, 1773–1780 (2022). [DOI] [PubMed] [Google Scholar]
- 16.Meng, Y. et al. Genome-wide association study identifies TPH2 variant as a novel locus for severe CV-A6-associated hand, foot, and mouth disease in Han Chinese. Int. J. Infect. Dis.98, 268–274 (2020). [DOI] [PubMed] [Google Scholar]
- 17.Chen, X. et al. Disruption of Transient Serotonin Accumulation by Non-Serotonin-Producing Neurons Impairs Cortical Map Development. Cell Rep.10, 346–358 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar, A. et al. The Serotonin Neurotransmitter Modulates Virulence of Enteric Pathogens. Cell Host Microbe28, 41–53 e48 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu, N. et al. The Mechanism of Secretion and Metabolism of Gut-Derived 5-Hydroxytryptamine. Int. J. Mol. Sci.22, 7931 (2021). [DOI] [PMC free article] [PubMed]
- 20.Gutknecht, L. et al. Tryptophan hydroxylase-2 gene variation influences personality traits and disorders related to emotional dysregulation. Int J. Neuropsychopharmacol.10, 309–320, (2007). [DOI] [PubMed] [Google Scholar]
- 21.Lesch, K. P., Araragi, N., Waider, J., van den Hove, D. & Gutknecht, L. Targeting brain serotonin synthesis: insights into neurodevelopmental disorders with long-term outcomes related to negative emotionality, aggression and antisocial behaviour. Philos. Trans. R. Soc. Lond. B Biol. Sci.367, 2426–2443 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Osaka, H. et al. Ubiquitin carboxy-terminal hydrolase L1 binds to and stabilizes monoubiquitin in neuron. Hum. Mol. Genet12, 1945–1958 (2003). [DOI] [PubMed] [Google Scholar]
- 23.Heanue, T. A. & Pachnis, V. Ret isoform function and marker gene expression in the enteric nervous system is conserved across diverse vertebrate species. Mech. Dev.125, 687–699 (2008). [DOI] [PubMed] [Google Scholar]
- 24.May-Zhang, A. A. et al. Combinatorial Transcriptional Profiling of Mouse and Human Enteric Neurons Identifies Shared and Disparate Subtypes In Situ. Gastroenterology, 160, 755–770.e26 (2021). [DOI] [PMC free article] [PubMed]
- 25.Morikawa, Y. et al. The basic helix-loop-helix factor Hand 2 regulates autonomic nervous system development. Dev. Dyn.234, 613–621 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hendershot, T. J. et al. Expression of Hand2 is sufficient for neurogenesis and cell type-specific gene expression in the enteric nervous system. Dev. Dyn.236, 93–105 (2007). [DOI] [PubMed] [Google Scholar]
- 27.Jarret, A. et al. Enteric Nervous System-Derived IL-18 Orchestrates Mucosal Barrier Immunity. Cell180, 813–814 (2020). [DOI] [PubMed] [Google Scholar]
- 28.Okaty, B. W. et al. A single-cell transcriptomic and anatomic atlas of mouse dorsal raphe Pet1 neurons. Elife9, e55523 (2020). [DOI] [PMC free article] [PubMed]
- 29.Gershon, M. D. & Tamir, H. Release of endogenous 5-hydroxytryptamine from resting and stimulated enteric neurons. Neuroscience6, 2277–2286 (1981). [DOI] [PubMed] [Google Scholar]
- 30.Gutknecht, L. et al. Deficiency of brain 5-HT synthesis but serotonergic neuron formation in Tph2 knockout mice. J. Neural Transm.115, 1127–1132 (2008). [DOI] [PubMed] [Google Scholar]
- 31.Montalbano, A. et al. Cellular resilience: 5-HT neurons in Tph2(−/−) mice retain normal firing behavior despite the lack of brain 5-HT. Eur. Neuropsychopharmacol.25, 2022–2035 (2015). [DOI] [PubMed] [Google Scholar]
- 32.Xu, H. et al. Transcriptional Atlas of Intestinal Immune Cells Reveals that Neuropeptide alpha-CGRP Modulates Group 2 Innate Lymphoid Cell Responses. Immunity51, 696–708 e699 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shi, G. P. et al. Cathepsin S required for normal MHC class II peptide loading and germinal center development. Immunity10, 197–206 (1999). [DOI] [PubMed] [Google Scholar]
- 34.Lechmann, M., Berchtold, S., Hauber, J. & Steinkasserer, A. CD83 on dendritic cells: more than just a marker for maturation. Trends Immunol.23, 273–275 (2002). [DOI] [PubMed] [Google Scholar]
- 35.Luo, B. H., Carman, C. V. & Springer, T. A. Structural basis of integrin regulation and signaling. Annu. Rev. Immunol.25, 619–647 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fayette, J. et al. Human dendritic cells skew isotype switching of CD40-activated naive B cells towards IgA1 and IgA2. J. Exp. Med.185, 1909–1918 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mora, J. R. et al. Generation of gut-homing IgA-secreting B cells by intestinal dendritic cells. Science314, 1157–1160 (2006). [DOI] [PubMed] [Google Scholar]
- 38.Dedobbeleer, O., Stockis, J., van der Woning, B., Coulie, P. G. & Lucas, S. Cutting Edge: Active TGF-beta1 Released from GARP/TGF-beta1 Complexes on the Surface of Stimulated Human B Lymphocytes Increases Class-Switch Recombination and Production of IgA. J. Immunol.199, 391–396 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang, R. et al. GARP regulates the bioavailability and activation of TGFbeta. Mol. Biol. Cell23, 1129–1139 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reboldi, A. et al. IgA production requires B cell interaction with subepithelial dendritic cells in Peyer’s patches. Science352, aaf4822 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Worbs, T., Hammerschmidt, S. I. & Forster, R. Dendritic cell migration in health and disease. Nat. Rev. Immunol.17, 30–48 (2017). [DOI] [PubMed] [Google Scholar]
- 42.Koscielny, A. et al. Impact of CCR7 on the gastrointestinal field effect. Am. J. Physiol. Gastrointest. Liver Physiol.300, G665–675, (2011). [DOI] [PubMed] [Google Scholar]
- 43.Wang, Y. C. et al. Intestinal cell type-specific communication networks underlie homeostasis and response to Western diet. J. Exp. Med.220, e20221437 (2023). [DOI] [PMC free article] [PubMed]
- 44.Hashizume-Takizawa, T., Kobayashi, R., Tsuzukibashi, O., Saito, M. & Kurita-Ochiai, T. CCR7-deficient mice exhibit a delayed antigen-specific mucosal IgA antibody response to an oral recombinant Salmonella strain. Pathog. Dis.77, ftz024 (2019). [DOI] [PubMed]
- 45.Jang, M. H. et al. CCR7 is critically important for migration of dendritic cells in intestinal lamina propria to mesenteric lymph nodes. J. Immunol.176, 803–810 (2006). [DOI] [PubMed] [Google Scholar]
- 46.Seth, S. et al. CCR7 essentially contributes to the homing of plasmacytoid dendritic cells to lymph nodes under steady-state as well as inflammatory conditions. J. Immunol.186, 3364–3372 (2011). [DOI] [PubMed] [Google Scholar]
- 47.Jin, S. et al. Inference and analysis of cell-cell communication using CellChat. Nat. Commun.12, 1088 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Persson, E. K., Scott, C. L., Mowat, A. M. & Agace, W. W. Dendritic cell subsets in the intestinal lamina propria: ontogeny and function. Eur. J. Immunol.43, 3098–3107 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sorrelle, N., Dominguez, A. T. A. & Brekken, R. A. From top to bottom: midkine and pleiotrophin as emerging players in immune regulation. J. Leukoc. Biol.102, 277–286 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vogt, T. K., Link, A., Perrin, J., Finke, D. & Luther, S. A. Novel function for interleukin-7 in dendritic cell development. Blood113, 3961–3968 (2009). [DOI] [PubMed] [Google Scholar]
- 51.Tezuka, H. et al. Prominent role for plasmacytoid dendritic cells in mucosal T cell-independent IgA induction. Immunity34, 247–257 (2011). [DOI] [PubMed] [Google Scholar]
- 52.Zhang, H., Leitner, D. R., Hasegawa, Y. & Waldor, M. K. Peripheral serotonergic neurons regulate gut motility and anxiety-like behavior. Curr. Biol.34, R133–R134 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li, Z. et al. Essential roles of enteric neuronal serotonin in gastrointestinal motility and the development/survival of enteric dopaminergic neurons. J. Neurosci.31, 8998–9009 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jacobson, A., Yang, D., Vella, M. & Chiu, I. M. The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes. Mucosal Immunol.14, 555–565 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Quintero-Villegas, A. & Valdes-Ferrer, S. I. Role of 5-HT(7) receptors in the immune system in health and disease. Mol. Med.26, 2 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pelka, K. et al. Spatially organized multicellular immune hubs in human colorectal cancer. Cell184, 4734–4752 e4720 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jaeger, N. et al. Single-cell analyses of Crohn’s disease tissues reveal intestinal intraepithelial T cells heterogeneity and altered subset distributions. Nat. Commun.12, 1921 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim, J. J. et al. Targeted inhibition of serotonin type 7 (5-HT7) receptor function modulates immune responses and reduces the severity of intestinal inflammation. J. Immunol.190, 4795–4804 (2013). [DOI] [PubMed] [Google Scholar]
- 59.Guseva, D. et al. Serotonin 5-HT7 receptor is critically involved in acute and chronic inflammation of the gastrointestinal tract. Inflamm. Bowel Dis.20, 1516–1529 (2014). [DOI] [PubMed] [Google Scholar]
- 60.Efremova, M., Vento-Tormo, M., Teichmann, S. A. & Vento-Tormo, R. CellPhoneDB: inferring cell-cell communication from combined expression of multi-subunit ligand-receptor complexes. Nat. Protoc.15, 1484–1506 (2020). [DOI] [PubMed] [Google Scholar]
- 61.Drokhlyansky, E. et al. The Human and Mouse Enteric Nervous System at Single-Cell Resolution. Cell182, 1606–1622.e1623 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fu, R. et al. clustifyr: an R package for automated single-cell RNA sequencing cluster classification. F1000Res9, 223 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhao, Y. et al. TPM, FPKM, or Normalized Counts? A Comparative Study of Quantification Measures for the Analysis of RNA-seq Data from the NCI Patient-Derived Models Repository. J. Transl. Med.19, 269 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bolyen, E. et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol.37, 852–857 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Czeloth, N., Bernhardt, G., Hofmann, F., Genth, H. & Forster, R. Sphingosine-1-phosphate mediates migration of mature dendritic cells. J. Immunol.175, 2960–2967 (2005). [DOI] [PubMed] [Google Scholar]
- 66.Zhang, H. L. et al. Regulatory T-cell depletion in the gut caused by integrin beta7 deficiency exacerbates DSS colitis by evoking aberrant innate immunity. Mucosal Immunol.9, 391–400 (2016). [DOI] [PubMed] [Google Scholar]
- 67.Mach, N. et al. Differences in dendritic cells stimulated in vivo by tumors engineered to secrete granulocyte-macrophage colony-stimulating factor or Flt3-ligand. Cancer Res.60, 3239–3246 (2000). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
All scRNA-seq, bulk RNA-seq datasets and 16S sequencing data generated here have been deposited into the NCBI Gene Expression Omnibus database under accession number GSE227340. https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=%20GSE227340 Source data are provided with this paper.