Abstract
Introduction
Acute appendicitis, a prevalent cause of acute abdominal pain and a common indication for emergency surgery, presents a diagnostic challenge due to its diverse clinical presentation and variability in appendix location and symptoms. Traditional diagnostic approaches, including physical examination, clinical scoring systems, and imaging techniques, have limitations. This study introduces the "Amr sign," a new diagnostic indicator characterized by sudden reflex hyperextension of the neck upon palpation of the right iliac fossa, which is hypothesized to reflect local peritoneal irritation from an inflamed appendix.
Methods
We conducted a prospective observational study at Alwakra Hospital from November 2016 to January 2019 that included 195 patients aged 15 years and older with right iliac fossa pain and an Alvarado score of four or more. The "Amr sign" was evaluated alongside standard clinical examination and imaging results. Diagnostic accuracy was assessed via histopathological confirmation, which is the gold standard.
Results
The "Amr sign" had a sensitivity of 68.6% and a specificity of 67.3%. The positive predictive value (PPV) was 89%, whereas the negative predictive value (NPV) was 45%. Receiver operating characteristic (ROC) analysis revealed an area under the curve (AUC) of 0.679 for the "Amr sign" compared with 0.622 for the other imaging modalities, suggesting comparable diagnostic performance. The "Amr sign" demonstrated a higher likelihood ratio of a positive test (2.3) and a lower likelihood ratio of a negative test (0.46).
Conclusion
The "Amr sign" is a promising diagnostic tool for acute appendicitis, offering a simple, reliable, and quick test that can be performed by less experienced physicians. While its sensitivity and specificity are moderate, its high PPV suggests that it is particularly useful in confirming appendicitis. Further research and validation are needed to fully establish its role in clinical practice.
Keywords: acute appendicitis, alvarado score, amr sign, diagnosis, diagnostic reliability
Introduction
Acute appendicitis is one of the most common causes of acute abdomen and the leading indication for emergency abdominal surgery worldwide. In the USA, the annual incidence is 93 per 100,000 people, making it the most frequent acute surgical emergency in the country [1]. A higher incidence has been reported in European populations, with 132 cases per 100,000 in Spain [2]. However, reports from Denmark and the UK have noted a decline in the incidence of acute appendicitis, though no specific cause has been proposed for this trend [3]. Although the management of acute appendicitis is standardized, the diagnosis of appendicitis remains a clinical challenge for physicians. Most medical students and residents learn how to diagnose a hernia within one to two teaching sessions, but it takes months of experience to master the skill of diagnosing the causes of right iliac fossa (RIF) pain. This is due to the multiplicity of pathologies in the RIF, which can manifest themselves in the variability in appendix position, time of presentation, pain tolerance, and the lack of one specific accurate and sensitive clinical sign. For these reasons, surgeons have traditionally accepted a 20% rate of false positive diagnoses of acute appendicitis, leading to a significant number of unnecessary surgeries, particularly in females, to minimize morbidities associated with a missed diagnosis [4]. The false positive diagnosis rate of appendicitis in clinical practice is particularly high in females, with reports reaching up to 42% [5]. While both genders pose diagnostic challenges, women often require additional imaging, such as ultrasonography, to rule out gynecological and obstetric causes, whereas men rely more on repeated physical examinations [6,7].
Since repeated physical examination is the gold standard of diagnosis, and to avoid subjective methods of diagnosis, a number of clinical scoring systems have been devised [8]. They gained popularity as they rendered the diagnosis of appendicitis more objective, though not particularly perfect. Eventually, the scoring systems lost popularity, and we returned to the era of clinical judgment. Although initial reports and studies on the diagnostic power of CT and abdominal ultrasound (AUS) were not promising at the beginning of the third millennium [9], trials of the use of technetium 99 labeled WBCs in the diagnosis of acute appendicitis were introduced, but again, the results were not encouraging, the cost was high, and the feasibility of such techniques in hospital was limited [10]. During the last three decades, with the advent of high-resolution ultrasound and the rise of the learning curve among radiologists, the diagnostic benefit of ultrasound and CT scans has been confirmed, and their use has become almost standard practice in the evaluation of acute appendicitis [11-13].
Several studies have emphasized the efficacy of adding ultrasound to clinical examination or the Alvarado score [14-16]. A careful history and the signs elicited will, in most cases, lead to a diagnosis. However, the diagnostic challenge lies in a significant portion of patients who present with vague symptoms or incomplete clinical signs. At this point, it is up to the physician’s experience to reach a conclusion with respect to operation, observation, investigation, or discharge. For this reason, we present a new sign that we believe has far greater sensitivity and specificity for diagnosing and excluding acute appendicitis than any other clinical sign. We present the “Amr sign,” which is simply a sudden reflex hyperextension of the neck upon palpation of the RIF in patients with acute appendicitis. The explanation for such a jerky reflex is probably the presence of some degree of local peritonitis over the inflamed appendix. This explanation is augmented by the fact that the sign was difficult to elicit in the retrocecal position of the inflamed appendix. It is a very simple, reliable, quick test that is safe to conduct and can be easily performed by even the least experienced physicians.
Materials and methods
During the period from November 2016 to January 2019, we prospectively examined 440 patients above the age of 15 who presented to the Accident and Emergency Department of Alwakra Hospital in the State of Qatar with a complaint of RIF pain. A total of 440 patients were initially examined by the emergency physician, and those who had an Alvarado score of four or more were referred to the surgeon with an initial diagnosis of suspected acute appendicitis. A total of 195 patients were referred and included in the study. To guarantee the consistency of the technique, the eliciting of the sign was performed by the same physician and medical student. The sign was considered positive if sudden hyperextension of the neck occurred in response to pressure on the RIF and negative if no neck movement occurred.
Patient selection
Patients of both sexes, all above the age of 15 years, presenting with RIF pain and an Alvarado score of four or more during the period from November 2016 to January 2019, were included in the study (standard examination plus the "Amr sign"). In addition to the Alvarado score and RIF pain, other clinical factors such as fever, leukocytosis, and localized tenderness were also considered as part of the standard clinical assessment (standard examination plus the "Amr sign").
Exclusion criteria
Patients younger than 15 years of age, those with an Alvarado score below four, and those with a history of appendectomy were excluded from the study. Any of the causes of abdominal pain, such as gastrointestinal disorders, gynecological conditions, or urinary tract infections, were still included in the study to test the specificity of "Amr sign" and its ability to pick up only appendicitis among all patients with RIF pain.
Ethics
A copy of the project was sent to the medical ethics committee and approved.
The study was conducted as an observational study, where the results of the "Amr sign" were not considered a factor in determining the decision to operate or observe.
Blinding
The physician performing the clinical test ("Amr sign") performed a physical examination and recorded whether the test was positive or negative. He was not involved in the patient’s treatment.
The final confirmation of the diagnosis of acute appendicitis was made via histopathological examination of the retrieved appendix. Patients who were discharged without surgery due to a lack of symptoms and signs were considered negative for appendicitis. They were included in the study to test the negative predictive value (NPV) of this sign. At the end of the study, the results were collected and compared against other known signs of appendicitis.
Statistical analysis
The data were compiled, checked, and analyzed using the Statistical Package for Social Sciences (IBM Corp., Armonk, NY) version 26. For each variable and all demographic variables, descriptive statistics (i.e., frequencies, percentages, and measures of central tendency and where applicable) were generated. A chi-square test was implemented to test the significance of the associations of "Amr sign," CT scan, and ultrasound, with other attributes at the 5% level of significance, with the CT scan results and between male and female students. ROC analysis was performed to test the sensitivity and specificity of the "Amr sign" and imaging modalities.
Results
The demographic distribution of patients diagnosed with acute appendicitis is detailed in Table 1. The majority of the cases (64.0%) occurred in the age group of 15-30 years, followed by 31-50 years (33.8%), and a small proportion (2.2%) in patients older than 50 years.
Table 1. Demographics of patients with acute appendicitis.
| Variables/categories | n | % |
| Age groups | ||
| 15-30 years | 87 | 64.0% |
| 31-50 years | 46 | 33.8% |
| >50 years | 3 | 2.2% |
| Gender | ||
| Female | 32 | 16.4% |
| Male | 163 | 83.6% |
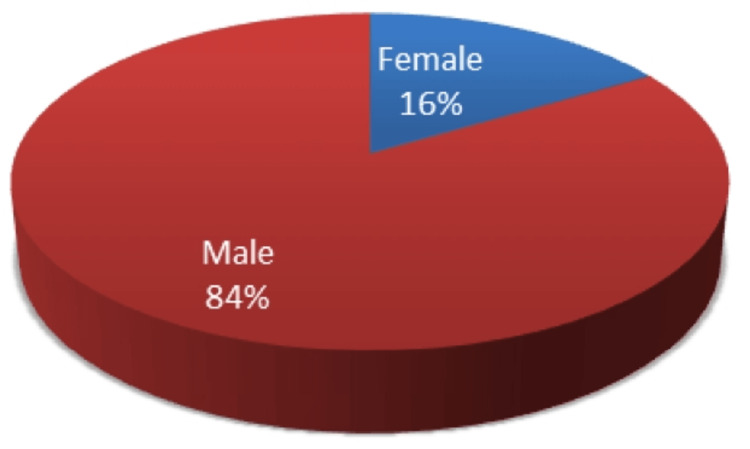
Gender distribution indicated a significantly higher incidence in males, who comprised 83.6% of the cases, compared to females at 16.4% (Figure 1).
Figure 1. Gender distribution of the patients of acute appendicitis included in our study.
The analysis of the frequency distribution of patients with acute appendicitis, as presented in Table 2, reveals several key clinical indicators associated with the condition. Among the 195 patients studied, 59.0% (n = 115) experienced vomiting, and 30.3% (n = 59) presented with fever. A significant majority, 97.4% (n = 190), exhibited tenderness in the RIF, while 66.2% (n = 129) had positive cough signs. Regarding patient outcomes, 77.9% (n = 152) underwent surgical intervention, and 22.1% (n = 43) were observed without immediate surgery. Rebound tenderness and a neutrophil shift to the left were noted in 55.4% (n = 108) and 56.4% (n = 110) of patients, respectively. Rovsing’s sign was positive in 44.1% (n = 86) of cases, while 52.3% (n = 102) reported migrating pain. These findings underscore the prevalence of these symptoms in diagnosing acute appendicitis, with tenderness in RIF and cough signs being particularly prominent indicators. The statistical analysis supports these observations, with a 95% confidence interval (CI) demonstrating the robustness of the results, although specific p-values were not provided for these individual attributes.
Table 2. Conditions of patients with acute appendicitis.
RIF, right iliac fossa
| Attributes/categories | n | % |
| Vomiting | ||
| No | 80 | 41.0 % |
| Yes | 115 | 59.0 % |
| Fever | ||
| No | 136 | 69.7 % |
| Yes | 59 | 30.3 % |
| Tender RIF | ||
| Negative | 5 | 2.6 % |
| Positive | 190 | 97.4 % |
| Cough signs | ||
| Negative | 66 | 33.8% |
| Positive | 129 | 66.2% |
| Disposition | ||
| Total admitted | 195 | 100 % |
| Operated | 152 | 77.9 % |
| Observed | 43 | 22.1 % |
| Rebound tenderness | ||
| Negative | 87 | 44.6 % |
| Positive | 108 | 55.4 % |
| Neutrophil shift to left | ||
| Negative | 85 | 43.6 % |
| Positive | 110 | 56.4 % |
| Rovsing’s sign | ||
| Negative | 109 | 55.9% |
| Positive | 86 | 44.1% |
| Migrating pain | ||
| Negative | 93 | 47.7% |
| Positive | 102 | 52.3% |
The results presented in Table 3 provide a detailed comparison of the "Amr sign" and other clinical findings among patients suspected of having acute appendicitis. The "Amr sign" was positive in 58.5% of the patients (n = 114) and negative in 41.5% (n = 81), indicating a relatively high frequency of this sign among those diagnosed with appendicitis. Of the 195 patients admitted, 77.9% (n = 152) underwent surgery, and 22.1% (n = 43) were observed. Histopathological examination confirmed acute appendicitis in 71.8% (n = 140) of cases, while 8.2% (n = 16) had negative results, and in 20% (n = 39) of the cases, the histopathology was not performed due to discharge of the patient without surgery. The total number of negative histopathology and discharged cases without surgery is 55 (28.2 %). Notably, Rovsing’s sign was positive in 44.1% (n = 86) of the patients, while imaging findings varied, with 48.7% (n = 95) showing positive results on imaging modalities (ultrasound or CT) or negative results in 15.9% (n = 31), while 5.1% (n = 10) were inconclusive, and 30.3% (n = 59) were those where neither ultrasound nor CT was performed. The high positive rate of the "Amr sign" compared to Rovsing’s sign (44.1%) and imaging results suggests its potential utility in diagnosing acute appendicitis. Further statistical analysis with a 95% CI and p-value would be necessary to determine the precise sensitivity and specificity of the "Amr sign" in comparison to other diagnostic methods.
Table 3. "Amr sign" and other clinical findings of patients with acute appendicitis.
| Attributes/categories | n | % |
| "Amr sign" | ||
| Negative | 81 | 41.5% |
| Positive | 114 | 58.5% |
| Disposition | ||
| Total admitted | 195 | 100% |
| Operated | 152 | 77.9% |
| Observed | 43 | 22.1% |
| Histopathology | ||
| Positive | 140 | 71.8% |
| Negative | 16 | 8.2 % |
| Discharged no surgery | 39 | 20.0% |
| Overall negative | 55 | 28.2 % |
| Rovsing’s sign | ||
| Negative | 109 | 55.9% |
| Positive | 86 | 44.1% |
| Image modalities | ||
| Negative | 31 | 15.9% |
| Positive | 95 | 48.7% |
| Inconclusive | 10 | 5.1% |
| Not done | 59 | 30.3% |
The association of the "Amr sign" with various demographic and clinical attributes in patients with acute appendicitis was analyzed, revealing several statistically significant findings (Table 4). Age group showed a significant association with the "Amr sign" (χ² = 4.418, p = 0.041), with a higher prevalence of a positive "Amr sign" in the 15-30 years age group (58.1%) compared to the negative group (74.0%). Gender, vomiting, fever, tender RIF, cough signs, previous admission, rebound tenderness, neutrophil shift to the left, Rovsing’s sign, and migrating pain were not significantly associated with the "Amr sign" (p > 0.05). However, histopathology results showed a highly significant association (χ² = 20.892, p < 0.001), with 84.2% of patients with a positive "Amr sign" having confirmed acute appendicitis, compared to 54.3% in the negative group. The disposition variable approached significance (χ² = 3.244, p = 0.072), suggesting a trend toward more frequent surgical intervention in patients with a positive "Amr sign" (82.5%). These results highlight the potential diagnostic value of the "Amr sign" in acute appendicitis, particularly when considered alongside histopathological findings.
Table 4. Testing significance of the association of "Amr sign" with other demographic and clinical attributes of patients with acute appendicitis.
Highly significant if p < 0.01, significant if p < 0.05, and nonsignificant if p > 0.05.
RIF, right iliac fossa
| Variables/categories | "Amr sign" | Chi-square | p-value | ||||
| Negative | Positive | ||||||
| n | % | n | % | ||||
| Age groups | 15-30 years | 37 | 74.0% | 50 | 58.1% | 4.418 | 0.041 |
| 31-50 years | 13 | 26.0% | 33 | 38.4% | |||
| >50 years | 0 | 0.0% | 3 | 3.5% | |||
| Gender | Female | 15 | 18.5% | 17 | 14.9% | 0.449 | 0.503 |
| Male | 66 | 81.5% | 97 | 85.1% | |||
| Vomiting | No | 30 | 37.0% | 50 | 43.9% | 0.991 | 0.340 |
| Yes | 51 | 63.0% | 64 | 56.1% | |||
| Fever | No | 54 | 66.7% | 82 | 71.9% | 0.622 | 0.430 |
| Yes | 27 | 33.3% | 32 | 28.1% | |||
| Tender RIF | Negative | 9 | 11.1% | 17 | 14.9% | 0.592 | 0.442 |
| Positive | 72 | 88.9% | 97 | 85.1% | |||
| Cough signs | Negative | 30 | 37.0% | 36 | 31.6% | 0.630 | 0.427 |
| Positive | 51 | 63.0% | 78 | 68.4% | |||
| Disposition | Operated | 58 | 71.6% | 94 | 82.5% | 3.244 | 0.072 |
| Observed | 23 | 28.4% | 20 | 17.5% | |||
| Histopathology | Negative | 37 | 45.7% | 18 | 15.8% | 20.892 | 0.000 |
| Positive | 44 | 54.3% | 96 | 84.2% | |||
| Previous admission | No | 49 | 60.5% | 73 | 64.0% | 0.254 | 0.615 |
| Yes | 32 | 39.5% | 41 | 36.0% | |||
| Rebound tenderness | Negative | 36 | 44.4% | 51 | 44.7% | 0.002 | 0.968 |
| Positive | 45 | 55.6% | 63 | 55.3% | |||
| Neutrophil shift to left | Negative | 33 | 40.7% | 52 | 45.6% | 0.457 | 0.499 |
| Positive | 48 | 59.3% | 62 | 54.4% | |||
| Rovsing’s sign | Negative | 44 | 54.3% | 65 | 57.0% | 0.140 | 0.709 |
| Positive | 37 | 45.7% | 49 | 43.0% | |||
| Migrating pain | Negative | 36 | 44.4% | 57 | 50.0% | 0.586 | 0.444 |
| Positive | 45 | 55.6% | 57 | 50.0% | |||
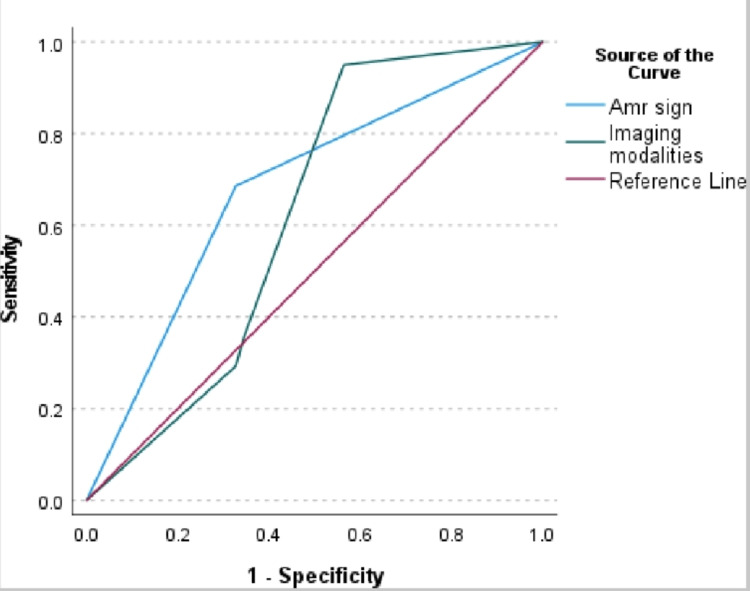
The diagnostic accuracy of the "Amr sign" and imaging modalities in predicting acute appendicitis was assessed using receiver operating characteristic (ROC) analysis, as shown in Table 5. The area under the curve (AUC) for the "Amr sign" was 0.679 (p < 0.001), with a 95% CI ranging from 0.606 to 0.753. This indicates a moderate level of diagnostic accuracy, as values closer to 1.0 suggest higher accuracy. In comparison, imaging modalities yielded a lower AUC of 0.622 (p = 0.017) with a 95% CI of 0.522 to 0.722, indicating a statistically significant but less accurate performance compared to the "Amr sign." These results suggest that the "Amr sign" may offer a more reliable diagnostic tool for acute appendicitis than imaging modalities, although neither approach achieves perfect accuracy.
Table 5. Area under the receiver operating characteristic curve.
The test result variables, "Amr sign" and imaging modalities, have at least one tie between the positive actual state group and the negative actual state group.
Null hypothesis: true area = 0.5
| Test result variable | Area | Standard error | p-value | 95% confidence interval | |
| Lower bound | Upper bound | ||||
| "Amr sign" | 0.679 | 0.038 | 0.000 | 0.606 | 0.753 |
| Imaging modalities | 0.622 | 0.051 | 0.017 | 0.522 | 0.722 |
In the evaluation of the diagnostic performance of the "Amr sign" compared to imaging modalities, the ROC analysis reveals that the "Amr sign" has a Gini index of 0.358 and a corresponding Kolmogorov-Smirnov (K-S) statistic of 0.358, with a maximum K-S cutoff at 0.50 (Table 6). In comparison, imaging modalities show a slightly lower Gini index of 0.244 but a higher K-S statistic of 0.386, also with a maximum K-S cutoff at 0.50. The p-values associated with these metrics indicate the statistical significance of the observed differences. These results suggest that while both diagnostic tools provide valuable information, the "Amr sign" exhibits a slightly better discriminatory power, as reflected by its Gini index, though the K-S statistic for imaging modalities is marginally higher, indicating a potentially stronger separation between true positive and false positive rates at the given cutoff.
Table 6. Classifier evaluation metrics.
| Test result variable | Gini index | K-S statistics | |
| Max K-S | Cutoff | ||
| "Amr sign" | 0.358 | 0.358 | 0.50 |
| Imaging modalities | 0.244 | 0.386 | 0.50 |
The results of the ROC analysis presented in Figure 2 indicate that the "Amr sign" when compared to imaging modalities, has a statistically insignificant difference in diagnostic performance for acute appendicitis.
Figure 2. Receiver operating characteristic curve analysis.
The AUC difference between the "Amr sign" sign and imaging modalities was found to be 0.849, with a standard error difference of 0.057 and a 95% CI ranging from -0.075 to 0.190 (Table 7). The z-value of 0.396 and the corresponding p-value of 0.298 suggest that the observed difference is not statistically significant, failing to reject the null hypothesis that the true area difference is zero. This implies that the "Amr sign" performs comparably to imaging modalities in diagnosing acute appendicitis but without significant superiority.
Table 7. Paired-sample area difference under the receiver operating characteristic curves.
Highly significant if p < 0.01, significant if p < 0.05, and nonsignificant if p > 0.05.
Null hypothesis: true area difference = 0
AUC, area under the curve
| Test result pair | Asymptotic | AUC difference | Standard error difference | 95% confidence interval | ||
| z | p-value | Lower bound | Upper bound | |||
| "Amr sign" - imaging modalities | 0.849 | 0.396 | 0.057 | 0.298 | -0.075 | 0.190 |
The diagnostic performance of the "Amr sign" in detecting acute appendicitis was evaluated by comparing its results against histopathological findings. According to Table 8, the "Amr sign" demonstrated a sensitivity of 68.6% and specificity of 67.3% at a threshold of 0.50. In contrast, imaging modalities display a higher sensitivity of 95.0% but a lower specificity of 43.6% at the same threshold. The ROC analysis reveals that while the "Amr sign" offers a balanced sensitivity and specificity, imaging modalities provide greater sensitivity but at the expense of specificity. The positive predictive value (PPV) of the "Amr sign" was 89%, indicating a high likelihood that patients with a positive "Amr sign" truly have acute appendicitis. Conversely, the NPV was 45%, suggesting a lower likelihood of correctly identifying patients who do not have appendicitis when the test result is negative. The likelihood ratio of a positive test was calculated to be 2.3, indicating that a positive "Amr sign" is 2.3 times more likely to be associated with acute appendicitis than a negative sign. Conversely, the likelihood ratio of a negative test was 0.46, showing that a negative "Amr sign" is less effective in ruling out appendicitis. Overall, while the "Amr sign" has a reasonable PPV, its relatively low sensitivity and NPV suggest that it should be used in conjunction with other diagnostic methods rather than as a standalone test.
Table 8. Coordinates of the receiver operating characteristic curve.
| Test result variable | Positive if greater than or equal to | Sensitivity | 1 - Specificity |
| "Amr sign" | -1.00 | 1.000 | 1.000 |
| 0.50 | 0.686 | 0.327 | |
| 2.00 | 0.000 | 0.000 | |
| Imaging modalities | -1.00 | 1.000 | 1.000 |
| 0.50 | 0.950 | 0.564 | |
| 1.50 | 0.357 | 0.345 | |
| 2.50 | 0.293 | 0.327 | |
| 4.00 | 0.000 | 0.000 |
Table 9 compares the positive and negative likelihood ratios of "Amr sign," RIF tenderness, and leukocytosis in order to show which of the three signs has more reliability to rule in or out acute appendicitis.
Table 9. Results of likelihood ratio test.
RIF, right iliac fossa
| Test | Positive likelihood ratio | Trust when test is positive | Negative likelihood ratio | Trust when test is negative (reliability) |
| "Amr sign" | 2.3 | Small | 0.46 | Small |
| RIF tenderness | 1 | Minimal | 0.4 | Small |
| Leukocytosis | 1.3 | Minimal | 0.24 | Small |
Discussion
One of the strengths of this study is the diversity of the patient population. Qatar, a multinational country, is home to many ethnic groups from different nationalities [17]. The 195 patients included in this study represented 25 nationalities and seven ethnic groups. This diversity enhances the credibility of our study, indicating that the findings are likely to be applicable to populations globally.
In this study, the majority of the cases (64.0%) occurred in the age group of 15-30 years. Our findings are in accordance with previous studies reporting that the majority of the cases (43.3 and 47%) were in the age group of 15-30 years [18,19]. Interestingly, gender distribution revealed a significantly higher incidence in males (83.6%) than in females (16.4%) cases. These findings suggest that acute appendicitis predominantly affects younger individuals, particularly males, which aligns with existing epidemiological data on the condition [18,19]. Our findings underscore the importance of considering demographic factors when diagnosing and managing acute appendicitis in clinical practice.
Our study revealed a strong PPV of the "Amr sign" when tested separately to diagnose appendicitis; although it did not show superiority over imaging, it did show a higher specificity and sensitivity when compared to each clinical sign of the Alvarado score individually. Previously, it has been reported in a recent meta-analysis that the Alvarado score demonstrated low combined sensitivity and specificity in diagnosing acute appendicitis [20]. When the "Amr sign" is compared with the two most important and pivotal signs in the Alvarado score - RIF tenderness and leukocytosis (each weighted at two points instead of one) - RIF tenderness had very high sensitivity (98.5%) but very low specificity (3.7%) compared to the "Amr sign" (68% sensitivity) and (70% specificity). Hence, RIF pain alone, although highly sensitive for appendicitis, does not help in ruling out the disease when the sign is positive simply because a highly sensitive test would be very useful in ruling out a disease when the test is negative. Since it has a very low specificity (3.7%), a positive RIF pain could indicate appendicitis, among many other causes of RIF pain. Thus, a higher specificity test, such as the "Amr sign" (70%), would be more useful in confirming the disease when the test is positive, and to a lesser extent, it might be fairly helpful in ruling out the disease when the sign is negative. Similarly, leukocytosis alone had a sensitivity of 93.6% but a specificity of only 26.4%, meaning it also does little to confirm appendicitis even when the white cell count is elevated. This is further confirmed by the positive likelihood ratio of only 1.3 and the negative likelihood ratio of 0.24, which suggests that leukocytosis, as a standalone test, has minimal importance in definitively ruling in or out the disease.
Our results further revealed that the "Amr sign" is superior to RIF tenderness and leukocytosis when positive. Our results are consistent with those of Iftikhar et al., who reported that the Pediatric Appendicitis Score (PAS) technique is superior to the Alvarado score in diagnosing acute appendicitis in the pediatric population, as indicated by higher diagnostic accuracy values [21]. Considering that when a test’s reliability is minimal, it cannot be used alone in the diagnosis or exclusion of a disease, while a test with “low” reliability can still be effective when combined with other tests. Thus, a more reliable test in diagnosing appendicitis may increase diagnosis certainty, though it remains less reliable when negative for ruling out appendicitis. This leads us to conclude that incorporating the "Amr sign" into the Alvarado score clinical criteria can significantly improve the PPV for diagnosing acute appendicitis. As a result, this combination may reduce the need for expensive, time-consuming, and costly imaging studies to confirm the diagnosis.
Limitations
One limitation of this study is that the "Amr sign," despite its promising PPV, was only compared to the two most pivotal clinical signs of the Alvarado score - RIF tenderness and leukocytosis. A more comprehensive comparison with other established diagnostic criteria and imaging modalities would provide a clearer picture of its diagnostic utility. Additionally, the study did not assess the performance of the "Amr sign" across different age groups or gender distributions, which could affect its generalizability. Lastly, while the study highlights the potential of the "Amr sign" to reduce reliance on imaging, it does not address how the inclusion of this sign might impact the overall clinical decision-making process in real-world settings where resources vary.
Conclusions
In this study, the "Amr sign" has been evaluated as a diagnostic tool for acute appendicitis, showing moderate sensitivity (68.6%) and specificity (67.3%). Although its diagnostic performance is not superior to imaging modalities, the sign's high PPV (89%) and ease of use make it a valuable addition to the diagnostic arsenal. The ROC analysis indicated that the "Amr sign" provides comparable diagnostic accuracy to imaging techniques, with an AUC of 0.679. While it does not achieve perfect accuracy, its simple application and reliability in detecting appendicitis justify its consideration as a supplementary diagnostic method. The relatively low NPV (45%) of the "Amr sign" highlights the importance of using it alongside other diagnostic methods, such as the Alvarado score or imaging, when ruling out appendicitis. On its own, the "Amr sign" is less reliable when negative. However, when positive, it improves diagnostic certainty. This leads us to conclude that incorporating the "Amr sign" into the Alvarado score significantly enhances the PPV of current clinical and imaging methods used for diagnosing acute appendicitis.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Medical Research Center and Research Committee, Hamad Medical Corporation, Doha, Qatar issued approval 8187/08. A copy of the project was sent to the medical ethics committee and approved. The study was conducted as an observational study, where the results of the “AMR sign” were not considered a factor in determining the decision to operate or observe.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Khalil Ahmad, Amr Mohamed F. Aboulwafa, Ali A. Aboulwafa, Mazin Abouzour, Amira Khairallah
Acquisition, analysis, or interpretation of data: Khalil Ahmad, Amr Mohamed F. Aboulwafa, Ali A. Aboulwafa, Mazin Abouzour, Amira Khairallah
Drafting of the manuscript: Khalil Ahmad, Amr Mohamed F. Aboulwafa, Ali A. Aboulwafa, Mazin Abouzour, Amira Khairallah
Critical review of the manuscript for important intellectual content: Khalil Ahmad, Amr Mohamed F. Aboulwafa, Ali A. Aboulwafa, Mazin Abouzour, Amira Khairallah
Supervision: Amr Mohamed F. Aboulwafa
References
- 1.Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. J Surg Res. 2012;175:185–190. doi: 10.1016/j.jss.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 2.Epidemiology of appendectomy and appendicitis in the Valencian community (Spain), 1998-2007. Andreu-Ballester JC, González-Sánchez A, Ballester F, Almela-Quilis A, Cano-Cano MJ, Millan-Scheiding M, del Castillo JR. Dig Surg. 2009;26:406–412. doi: 10.1159/000235956. [DOI] [PubMed] [Google Scholar]
- 3.Changes in the epidemiology of acute appendicitis and appendectomy in Danish children 1996-2004. Andersen SB, Paerregaard A, Larsen K. Eur J Pediatr Surg. 2009;19:286–289. doi: 10.1055/s-0029-1224199. [DOI] [PubMed] [Google Scholar]
- 4.The epidemiology of appendicitis and appendectomy in the United States. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. Am J Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 5.Effect of CT on false positive diagnosis of appendicitis and perforation. Raman SS, Osuagwu FC, Kadell B, Cryer H, Sayre J, Lu DS. N Engl J Med. 2008;358:972–973. doi: 10.1056/NEJMc0707000. [DOI] [PubMed] [Google Scholar]
- 6.The influence of age and gender on the utility of computed tomography to diagnose acute appendicitis. Antevil J, Rivera L, Langenberg B, Brown CV. Am Surg. 2004;70:850–853. [PubMed] [Google Scholar]
- 7.Diagnosis of acute appendicitis. Appendicitis is a separate clinical entity in men and women. Devey L, Henderson J, Wakefield C. https://pubmed.ncbi.nlm.nih.gov/11464830/ BMJ. 2001;323:50. [PMC free article] [PubMed] [Google Scholar]
- 8.A practical score for the early diagnosis of acute appendicitis. Alvarado A. Ann Emerg Med. 1986;15:557–564. doi: 10.1016/s0196-0644(86)80993-3. [DOI] [PubMed] [Google Scholar]
- 9.Has misdiagnosis of appendicitis decreased over time? A population-based analysis. Flum DR, Morris A, Koepsell T, Dellinger EP. JAMA. 2001;286:1748–1753. doi: 10.1001/jama.286.14.1748. [DOI] [PubMed] [Google Scholar]
- 10.The value of 99mTc-HMPAO labelled white blood cell scintigraphy in acute appendicitis patients with an equivocal clinical presentation. Colak T, Güngör F, Ozuğur S, et al. Eur J Nucl Med. 2001;28:575–580. doi: 10.1007/s002590100504. [DOI] [PubMed] [Google Scholar]
- 11.'To have...or not to have'. Should computed tomography and ultrasonography be implemented as a routine work-up for patients with suspected acute appendicitis in a regional hospital? Chiang DT, Tan EI, Birks D. Ann R Coll Surg Engl. 2008;90:17–21. doi: 10.1308/003588408X242259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Predictive value of sphericity index and other multidetector computed tomography findings in perforated acute appendicitis. Akıncı Ö. Ulus Travma Acil Cerrahi Derg. 2023;29:590–595. doi: 10.14744/tjtes.2023.45383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Does CT reduce the rate of negative laparoscopies for acute appendicitis? A single-center retrospective study. Wagner PJ, Haroon M, Morarasu S, Eguare E, Al-Sahaf O. J Med Life. 2020;13:26–31. doi: 10.25122/jml-2019-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diagnostic pathways in acute appendicitis: clinical score plus ultrasound outperform CT scan or upfront surgery, especially in doubtful cases. Coccolini F, Martinez-Perez A, Licitra G, et al. World J Surg. 2024;48:1350–1359. doi: 10.1002/wjs.12160. [DOI] [PubMed] [Google Scholar]
- 15.Efficacy of modified Alvarado score combined with ultrasound in the diagnosis of acute appendicitis: a prospective analytical study. Sirpaili S, Rajthala L, Banmala S, Gautam P, Ranabhat S, Ghatani SR, Shrestha E. Ann Med Surg (Lond) 2024;86:2586–2590. doi: 10.1097/MS9.0000000000001932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assessment of the diagnostic reliability of modified Alvarado scores and abdominal ultrasonography in acute appendicitis. Bhardwaj P, Behura A, Mohapatra I, et al. Cureus. 2023;15:0. doi: 10.7759/cureus.38991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The challenges of migrant employees and its impact on intension to leave. Rangan KR, Rajan KKS. https://d1wqtxts1xzle7.cloudfront.net/59449404/12IJHRMRAPR20191220190530-32463-1hmqjrh-libre.pdf?1559209592=&response-content-disposition=inline%3B+filename%3DTHE_CHALLENGES_OF_MIGRANT_EMPLOYEES_AND.pdf&Expires=1727249477&Signature=DaV-qnhChSJ9RDUkEhSxGtMwFSp6k5o8aARGOKN~g2pYMkPjVYPSVsO3z3KqYDZKbsglYOD1aQlD9Ip9YW1QC20jNRKB1auwFzj-90X~BemGxXI1m2HGM7HSHZj6fmq6kAQ6R4VaoJgINJO05iWjyB86SEaV12DSUPnfbjCaMygKzs5fUN5F6iLsewRULxyjoqyy-RDq-AQI0UM1dKDg6s1LYqnsdzkTnus-psONyy962m09YDSx94lEM02--pS74i6B8-feHwhdY2LesK7hp-cJ7hSr3~LBxxFoRV9WfKkkFh4gkTrwbKFVwrZVKRUfSxAAGlVtCW9wF2WpdsPm0A__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA Int J Hum Resour Manag Res. 2019;9:105–112. [Google Scholar]
- 18.A one year prospective study to compare and evaluate diagnostic accuracy of modified Alvarado score and ultrasonography in acute appendicitis, in adults. Kurane SB, Sangolli MS, Gogate AS. Indian J Surg. 2008;70:125–129. doi: 10.1007/s12262-008-0035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Modified alvarado score in diagnosis of acute appendicitis: a clinicopathological study. Jain S, Gehlot A, Songra M. Int Surg J. 2018;5:878–882. [Google Scholar]
- 20.The value of the Alvarado score for the diagnosis of acute appendicitis in children: a systematic review and meta-analysis. Bai S, Hu S, Zhang Y, Guo S, Zhu R, Zeng J. J Pediatr Surg. 2023;58:1886–1892. doi: 10.1016/j.jpedsurg.2023.02.060. [DOI] [PubMed] [Google Scholar]
- 21.Comparison of Alvarado score and pediatric appendicitis score for clinical diagnosis of acute appendicitis in children—a prospective study. Iftikhar MA, Dar SH, Rahman UA, et al. Ann Pediatr Surg. 2021;17:7. [Google Scholar]