Abstract
In the warmer lowlands, scorpion stings frequently result in emergencies and are a serious public health issue. Early in the spree, scorpion envenomation is particularly deadly because of respiratory and/or cardiovascular collapse. We report a 4-year-old boy with left middle cerebral arterial territory ischemic infarct within 24 h following scorpionism. He was managed conservatively with prazosin, aspirin, enoxaparin, levetriacetam and other supportive measures.
Key clinical message
Scorpion envenomation is frequently reported from tropical flatlands. In most patients, the manifestations are localized to the site of sting. However, serious presentations are also bound to occur and require early diagnosis and meticulous care.
Keywords: envenomation, ischemia, stroke, vasculitis
Introduction
The scorpion sting is one of the most go to forms of envenomation in countries with tropical climates. There are a variety of scorpions, and some of them have venom that could be detrimental to human beings. Non-fatal symptoms are common, which include pain, burning sensation, and change in color of the skin. Scorpion venom contains neurotoxins, which trigger the body to release endogenous catecholamines and acetylcholine. Systemic envenomation invites autonomic instability with a wide range of manifestations, including cardiovascular (hypertension, tachycardia, arrhythmias, myocarditis, distributive and cardiogenic shock), pulmonary (acute respiratory distress syndrome, pulmonary edema, atelectasis, bronchospasm), acute renal dysfunction, neurological emergencies (seizures, ischemia, hemorrhage, and rarely demyelination), and disseminated intravascular coagulation. A sympathetic storm may or may not follow the initial parasympathetic overdominance phase, which displays emesis, abdominal pain, excessive salivation, bradycardia, and pupillary constriction. Cerebrovascular injury in systemic envenomation is considered very odd. Globally, it has been documented in only 2% to 5% of cases of scorpionism [1–8].
We hereby present the case of a 4-year-old child with features consistent with autonomic storm following scorpion sting who later developed left sided ischemic stroke. However, he lacked features of defibrination syndrome and myocarditis. Therefore, the most speculated cause of stroke in our patient was presumed to be the autonomic storm, vasospasm and toxin associated vasculitis.
Case history/examination
A 4-year male child presented to our emergency department with features of vomiting, abdominal pain, and decreased sensorium following a complaint of pain and noticeable swelling in the right great toe. After a sleep of approximately 10 h, the child woke up in the morning complaining of severe pain in the right lower extremity. The mother of the child noticed swelling in the right great toe, and one of the family members noticed the scorpion on the floor of the room. They envisioned that the child was stung by the arthropod and rushed to our hospital emergency room.
The child presented to our emergency with features consistent with history. On arrival, the child was febrile, with a temperature of 100.8 degrees Fahrenheit, heart rate of 140/min and blood pressure of 125/87 mm Hg. Thorough evaluation revealed that the child was drowsy with Glasgow Coma Scale (GCS) of 12 (E3V3M6) with slurring noted during verbal examination and was unable to move right extremity while giving a command and poking with painful stimuli. Deep tendon reflexes and tone were increased in right upper and lower extremities.
Investigations and work-up
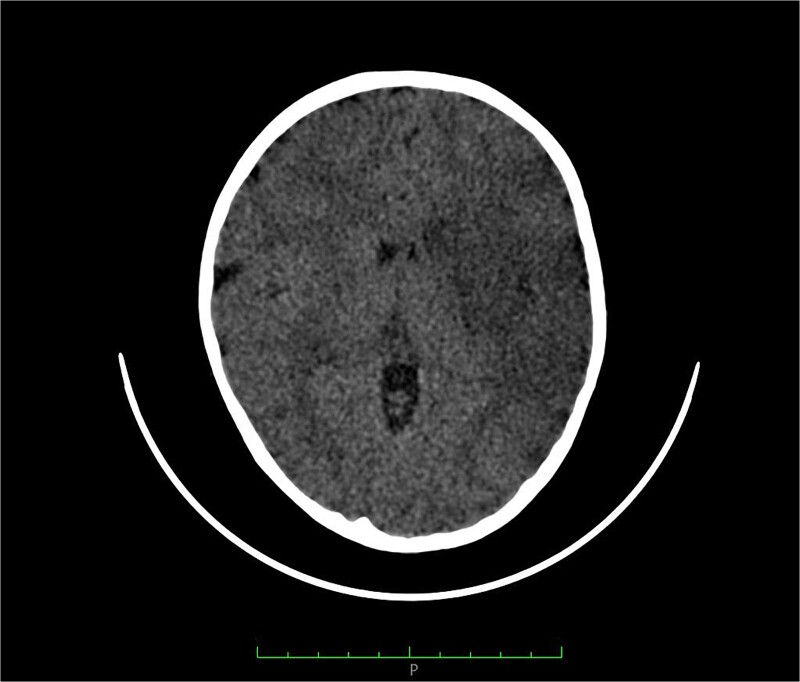
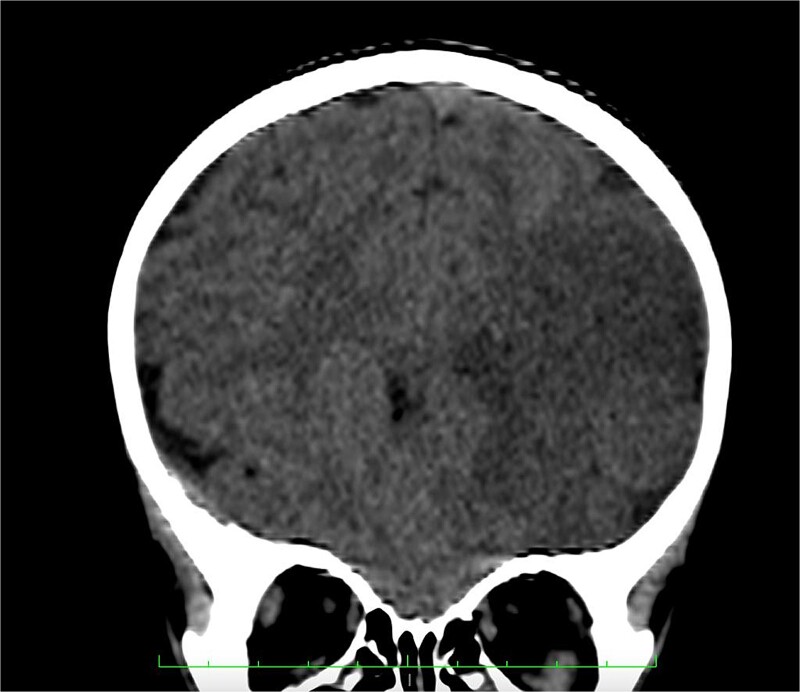
Based on the clinical examination, a computerized tomography (CT) scan of the head and two-dimensional echocardiography was requested. In addition, a blood sample was withdrawn and sent to the lab for estimation of hemoglobin, platelet count, electrolytes, urea, creatinine, and coagulation profile testing. CT scan showed an infarct in the left middle cerebral artery territory (Figs 1–3), and echocardiography showed normal ventricular function. Similarly, all requested lab parameters were in the normal range (Hemoglobin: 12.3 g/dl, Total leukocyte count: 12 300/mm3, sodium: 141 mEq/l, potassium: 3.9 mEq/l, prothrombin time: 15 s, INR:1.0, aPTT: 28 s, fibrin degraded products: 2mcg/ml, D-dimer: 0.1, urea: 25 mg/dl, creatinine: 0.6 mg/dl, ESR: 50 mm 1st h, CRP quantitative: 75 mg/dl).
Figure 1.
CT axial section showing hypodensity in left frontoparietal region with loss of garywhite differentiation suggestive of ischemic infarction.
Figure 2.
CT coronal section showing ischemic infarction in left frontoparietal region.
Figure 3.
CT axial section showing hypodensity in the left fronto-parieto-temporal region with loss of graywhite differentiation suggestive of ischemic infarction.
Treatment and outcome
The child was admitted and managed in the high dependency unit with a combination of antihypertensive (1 mg orally twice a day), antiplatelet (aspirin 37.5 mg orally once a day), anticoagulant (enoxaparin 10 mg by subcutaneous injection), and antiepileptic (levetiracetam 100 mg orally twice a day) medications. Other important aspects focusing on the child’s nutrition, physiotherapy, bedside mobilization, and bowel and bladder care were taken care of during treatment. The child’s physical activity gradually improved (from Modified Rankin Scale 4 at admission to 2 at time of discharge) during the period of treatment and was discharged on day 7 of admission. Physiotherapy and other rehabilitation measures were also addressed during the discharge. On follow-up after the next 10 days there was no significant disability, only little residual weakness was present and dysarthria was not evident (Modified Rankin Scale 1).
Discussion
On an annual basis, more than a million reports of scorpion stings are made across the globe, with a 20 per 100 000 population figures for prevalence. While roughly 5% of reported cases are severe, only about 0.3% of severe cases result in mortality [1].
The Asian Forest scorpion (Heterometrus species) is the most common scorpion found in Nepal, is responsible for non-fatal envenomations, and usually leads to local skin manifestations. The eastern Indian scorpion, or Hottentotta tamulus, is a species of scorpion belonging to the Buthidae family is also found in the tropics of Nepal. It is nocturnal and is reported to be deadly [8].
Patients presenting with scorpion envenomation have been split into three grades: Patients in grade (I) merely have local pain; those in grade (II) have systemic symptoms; and those in grade (III) have significant neurological impairment (coma and/or convulsions) or cardiorespiratory symptoms, primarily cardiogenic shock, and pulmonary edema [1–3].
Depending on the species of arachnid and the toxin’s plasma levels, the clinical symptoms can vary considerably. The release of endothelin, neuropeptide Y, and nitric oxide is prompted by the toxin. It triggers the complement and coagulation systems, which leads to an upward spiral of neurological harm (seizures, cerebral edema), inflammation, and microthrombosis [1, 4–6].
Because venom is hydrophilic, it has low blood–brain barrier permeation. In young kids, the central nervous system may be heavily involved in the envenomation process since the blood–brain barrier remains fragile. The central nervous system outcomes (grade III) resulting from scorpion stings can vary widely and manifest as diminished consciousness, convulsions, subarachnoid hemorrhage, stroke (hemorrhagic and/or ischemic) [3, 6].
Different mechanisms like heart failure, arrhythmias, coagulopathy, vasculitis, cerebral embolism, defibrination has been put forward to describe stroke resulting from scorpion envenomation [6]. The fundamental basis for these etiologies can be described as follows:
Autonomic storm: During an autonomic storm, high blood pressure can cause vessels to burst, notably perforating arteries, leading to hemorrhagic stroke. Catecholamine excess with predominant alpha receptor stimulation brings about the play of endothelin. Endothelin excess causes severe vasoconstriction of cerebral vessels resulting in low flow infarcts. Cholinergic overactivity, and dehydration can cause hypotension, leading to watershed infarcts [1–8].
Vasculitis: The venom is vasculotoxic, potentially capable of disrupting endothelium and causing vasculitis which may culminate in thrombosis. Furthermore, scorpion venom can induce platelet aggregation and enhance process of thrombus generation [1–8].
Toxic myocarditis: Venom induced myocarditis can precipitate into heart failure and arrhythmia, which may lead to stroke [1–8].
Defibrination syndrome: Stroke can also occur due to disseminated intravascular coagulation. Fibrin deposits has been demonstrated by autopsy in vessels of the sufferers of scorpion sting [1–8].
Neurological complications from scorpion stings are well reported in South America, Venezuela, India, and Turkey. Eight percent of patients in a case series drawn from southern India had neurological involvement; of these, four percent had hemorrhagic stroke and four percent had ischemic stroke [2, 5].
Cerebral infarcts typically appear more than 48 to 72 h after the initial scorpion envenomation [2, 3]. Contrary to this, our patient exhibited signs and symptoms of cerebral ischemia in less than 24 h, which made this case more atypical for reporting.
Scorpion stings are a problem in emerging economies, where medical costs are always a concern. The cornerstone of treatment in these areas is typically prazosin and supportive care [1].
Antivenin is theoretically the specific management. Purified anti-venom F(ab)2 is currently in widespread usage. Venom is released into the circulation during the initial cholinergic phase. Antivenom works best during this time and can neutralize free venom in about 5 h. This stops the ensuing sympathetic storm. However, due to unavailability of antivenin in Nepal, we managed the cause with combination of prazosin, anticoagulants, and antiplatelet agents [1, 3]. Owing to the absence of features suggestive of coagulopathy, myocarditis, defibrination, arrhythmias and heart failure, we therefore conclude that the venom induced vasospasm and vasculitis were the main culprits behind the occurrence of cerebral ischemic changes in our patient.
The main takeaway from this case report is that, despite being extremely common, scorpion stings can seldom surface as an ischemic stroke. Various explanations were put forth to delineate the pathophysiology behind the occurrence of cerebral infarction in scorpion envenomation. They can be summarized as briefly due sympathetic storm, myocarditis (left ventricular systolic dysfunction due to myocarditis, causing stagnation of blood and subsequent thromboembolism), venom vasculitis, and defibrination syndrome [6, 7].
Conclusion
In tropical and subtropical climates, scorpion envenomation is typical. Serious systemic effects and end organ damage might result from a severe scorpion sting envenomation. The central nervous system (CNS) can be compromised infrequently, but in a variety of complex ways, because of the toxin’s various neurotoxic effects. Furthermore, medical professionals working in environments where scorpion stings are commonly reported should be aware of the wide range of clinical toxidrome associated with envenomation [1–8].
Consent
Written and informed consent was obtained from the patient father for the publication of the case report, which is available for review by the editor of this journal.
Guarantor
Sunil Bhatta.
Acknowledgements
None.
Contributor Information
Bhatta Sunil, Department of Anesthesia and Critical Care, Nisarga Hospital and Research Center Pvt. Ltd., Dhangadhi-5 10900, Kailali, Nepal.
Awasthi Pusp Raj, Department of Pediatric Critical Care, Nisarga Hospital and Research Center Pvt. Ltd., Dhangadhi-5 10900, Kailali, Nepal.
Pandit Sukriti, Department of Pediatric Critical Care, Nisarga Hospital and Research Center Pvt. Ltd., Dhangadhi-5 10900, Kailali, Nepal.
Author contributions
Sunil Bhatta, Pusp Raj Awasthi and Sukriti Pandit equally involved in the conceptualization, formulation, resources, writing, and editing of the original draft.
Conflict of interest
Non conflict of interests.
Funding
None declared.
Data availability
Data described to support the findings is openly accessible in the article.
Ethical approval
Ethical approval of case reports is not needed in accordance with the local ethical guidelines.
References
- 1. Godoy D, Badenes R, Seifi S. et al. Neurological and systemic manifestations of severe scorpion envenomation. Cureus 2021;13:e14715. 10.7759/cureus.14715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kandan B, Ravi P. Scorpion sting and blindness: a case report. J Family Med Prim Care 2023;12:171–3. 10.4103/jfmpc.jfmpc_808_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Naranjo L, Carrillo-Villaseñor F, D’Suze G. et al. Ischemic stroke in a child after a probable scorpion sting. Am J of Trop Med Hyg 2021;106:959–61. 10.4269/ajtmh.21-0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bordón L, Paredes W, Pacheco R. et al. Intracerebral hemorrhage secondary to scorpion toxin in the northwest of Argentina; a case report. Bull Emerg Trauma 2018;6:253–6. 10.29252/beat-060312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Işik Y, Çegin MB, Kati İ. et al. A rare complication of scorpion sting: hemiplegia: case report. Turkiye Klinikleri J Case Rep 2016;24:127–30. 10.5336/caserep.2015-43728. [DOI] [Google Scholar]
- 6. Brutto OH, Brutto VJ. Scorpion stings: focus on cerebrovascular complications of envenoming. Int J Stroke 2013;8:E8. 10.1111/j.1747-4949.2012.00940.x. [DOI] [PubMed] [Google Scholar]
- 7. Reddy CR, Bompelli N, Khardenavis V. et al. Scorpion bite-induced ischaemic stroke. BMJ Case Rep 2017;2017:bcr-2017-221606. 10.1136/bcr-2017-221606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tripathi M, Sharma S, Pandey R. et al. Scorpion sting envenomation presenting with pulmonary edema in adults: a report of seven cases from Nepal. Indian J Med Sci 2006;60:19–23. 10.4103/0019-5359.19672. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data described to support the findings is openly accessible in the article.