Abstract
Introduction:
Endodontic therapy has been regarded as a safe treatment option with highly promising results in preserving natural teeth. Numerous factors may influence the longevity of endodontically treated teeth (ETT), thus altering their success/survival rate. This study aimed to determine the survival and success rates of endodontically treated premolars and molars with different complex restorative/prosthodontic treatments.
Materials and Methods:
A total of 190 patients with an ETT were included, who had received final coronal restoration up to 14 days after the temporary one and at least one year prior to the enrollment. The investigator evaluated the quality of endodontic filling, coronal restoration, mobility, and proximal contacts. Data were analyzed with multiple binary logistic regression and the Chi-Square test.
Results:
The average duration of follow-up was 28.6±11.9 months. Overall, 89.4% (170/190) of the teeth survived. The overall success rate for the investigated teeth was 70.5% (134/190). Success rates of 100% for crown, 95.7% for post and core crown (PCC), and 94.7% for amalgam build-up with post were achieved. However, the success rates were 75%, 52.5%, and 50% for amalgam build-up, composite build-up, and PCC with crown lengthening, respectively. The Chi-square test revealed that there was a significant difference between the different restorations in terms of success (P<0.001). Multiple binary logistic regression models revealed that coronal leakage (P=0.048), obturation void (P=0.037), obturation length (P=0.020), mobility (P=0.002), type of the restoration (P<0.001), and proximal contact (P<0.001) were significant predictors for success. However, apical lucency, root length, marginal caries, tooth type, and post did not appear to be significant indicators of success (P>0.05).
Conclusions:
ETT with minimal mobility, exhibiting underfilled obturations without visible voids, and having received crown/PCC/amalgam build-up with a post, along with the presence of both proximal contacts, tend to exhibit a significantly high success rate.
Key Words: Dental Amalgam, Dental Restoration Failure, Endodontic Inflammation, Endodontically Treated Tooth, Pain Management, Root Canal Therapy, Survival Analysis
Introduction
Patients with relatively complete dentitions and dental awareness are increasingly turning to endodontic treatment as a conservative treatment option [1]. Survival rates of endodontically treated teeth (ETT) have been very high accompanying extremely high satisfaction [2]. In a systematic review of 33 cross-sectional studies, based on data representing over 300,000 teeth, roughly 10% of all teeth were endodontically treated. Broadly, it is equivalent to two endodontic treatments per patient [3]. Another systematic review showed that the success rates for ETT without and with apical periodontitis were 82.8%-97.3% and 75.6%-87.77%, respectively [4]. This rate of success is comparable with more aggressive treatments such as extraction and implant placement. There are various definitions for endodontic success, focusing on clinical signs and symptoms and/or radiographic findings [5-7].
Moreover, a large number of other studies referred to "survival rate" rather than "success rate" [8-11]. The term "survival" refers to a tooth that is still in situ at the follow-up visit [6]. Exercising survival rate is substantially useful for retrospective records that lack adequate clinical information. For instance, in a population-based cohort study in Korea, more than 3 million teeth were studied between 2010 and 2015 for a 5-year survival rate. It showed a 90.8% and 88.4% of 5-year survival rate for initial root canal therapy (RCT) and re-RCT, respectively [12].
Numerous factors have been reported in the literature that compromise the success and survival of endodontic treatments, such as persistence of intracanal bacteria, inadequate canal cleaning, compromised obturation quality, overextension of root canal filling materials, coronal leakage, missed major and minor canals, and iatrogenic procedural errors [13]. Furthermore, restorative and prosthodontic causes are claimed to be the most prevalent reasons for ETT extraction [14]. Posterior ETT with minimum to moderate structural loss could be restored by direct/indirect restorations with comparable survival rates [15]. Despite several recommendations regarding whether to crown ETT or use more conservative restorations, the evidence on this topic is not conclusive yet [16].
In this retrospective observational study, we aimed to evaluate treatment outcomes of RCT, including survival and success rates of the enrolled teeth, and to clarify the prognostic factors contributing to RCT success and ETT survival in the premolar and molar teeth (including mobility grade, proximal contacts, apical periodontitis, obturation void and length, type of the restoration, presence of post, coronal leakage, and marginal caries). The null hypothesis indicates no significant difference in survival or success rate of ETT based on the endodontic or prosthodontic treatments they received.
Materials and Methods
This study conformed to the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement for observational epidemiology studies [17], and was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.RIDS.REC.1394.137). Participants were fully informed about the advantages and disadvantages of the follow-up X-ray and data confidentiality. Written consent was taken from each patient, containing the authorization to take an X-ray.
With the assumption of a confidence interval of 95% and a standard error of 0.07, a minimum sample size of 170 participants was calculated for the present study using the PASS 11 software (NCSS, LLC. Kaysville, Utah, USA), according to a similar study [18]. It was increased to 190 participants, considering expected losses and refusals of 10%. Using the convenience sampling method, samples were made up of patients attending the Department of Endodontics, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
All enrolled patients had at least one posterior ETT that was carried out by endodontic postgraduate students with inclusion criteria as follows: (1) final restoration was placed up to two weeks after temporary restoration, and (2) passing at least one year after the restoration delivery at the time of enrollment. Exclusion criteria of participants consisted of: (1) exhibition of any underlying diseases, (2) occurrence of root fracture, external or internal resorption, broad periapical lesions (score 4 and 5 of the periapical index [19]), or history of trauma on the tooth, and (3) generalized periodontal disease.
A periapical radiograph with parallel technique (XCP; extension cone paralleling using Rinn system) using the MinRay radiography unit (Sordex, Helsinky, Finland), was taken from each patient and controlled for proper density and contrast and appearance of at least 3 mm of periapical tissues. The data were collected through an oral questionnaire, clinical examination (CE), and radiological assessment (RA). The data were investigated by one examiner. The investigator assessed different variables for each participant in three categories: 1. General factors: mobility grade (through CE) and proximal contacts (through CE). 2. Endodontic-related factors: anatomical root length through RA; using a digital caliper (Mitutoyo, Kawasaki, Japan), apical periodontitis (through RA; considered positive if an increased or sustained lucency was evident in comparison to the X-ray recorded at the time of treatment), and obturation void and length (through RA and a digital caliper). Obturation length was deemed appropriate if the ending was at a distance of 0–2 mm from the apex, underfilled when it was more than 2 mm short of the apex, and overfilled if the material extruded beyond the apex [20]. 3. Restorative- and prosthodontic-related factors: type of the restoration (through CE and RA), presence of post (through RA), coronal leakage (through RA; presence of a gap between the restoration and tooth), and marginal caries (through CE and RA).
Statistical analysis was carried out using SPSS 25 (IBM Statistics for Windows, Version 25.0. Armonk, NY, USA). All statistical tests were interpreted at a 0.05 significance level. Binary logistic regression models were run to explore significant covariates on the success. The covariates comprised apical lucency, obturation length and void, root length, coronal leakage, tooth type, restoration type, presence of post, marginal caries, mobility grade, and proximal contact. Furthermore, Chi-square test was used to compare gender, type of the tooth and restoration, apical lucency, post, coronal leakage, marginal caries, obturation void, and proximal contact between the successful and failed cases.
Results
A total of 190 teeth from 190 patients (96 males and 94 females) were studied in the present study. The mean age of the participants was 33.83±12.51 years (95% CI: 32.04-35.62). The mean follow-up time was 28.62±11.91 months (minimum=12, maximum=65). The total survival rate of the teeth was 89.4% (170/190). Nine, seven, and four teeth were extracted for prosthodontic, periodontal, and endodontic reasons, respectively. Success rate of the survived teeth was 78.8% (134/170). The overall success rate for all investigated teeth was 70.5% (134/190).
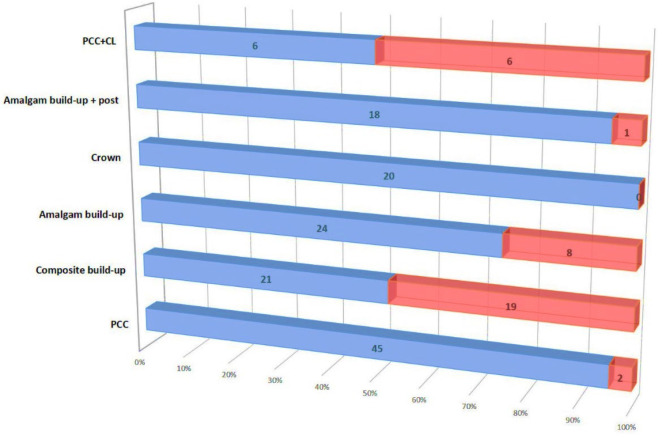
In total, 23% and 18% of the teeth were solely restored with composite and amalgam build-ups, respectively. Post and core crown (PCC), with or without crown lengthening (CL), accounted for 7% and 27% of the teeth, respectively. Single crown and amalgam build-up with post was used for 12% and 11% of the teeth. Success rates were 100%, 95.7%, and 94.7% for crown, PCC, and amalgam build-up with post, respectively. However, for amalgam build-up, composite build-up, and PCC with crown lengthening (CL), the success rates were 75%, 52.5%, and 50%, respectively (Figure 1). The Chi-square test revealed a significant difference between the success rates of different restorations (P<0.001).
Figure 1.
The successful and failed cases of each coronal restoration. CL: crown lengthening; PCC: post and core crown
Chi-Square tests showed that coronal leakage (odds ratio (OR): 0.136, P<0.001), obturation void (OR: 0.326, P=0.003), obturation length (P<0.001), mobility (P<0.001), apical lucency (OR: 0.107, P<0.001), marginal caries (OR: 0.354, P=0.006), post (OR: 3.185, P=0.005), and proximal contact (P<0.001) were significantly different in the successful and failed cases (Table 1).
Table 1.
Success rates, subjects’ number and P-values of Chi-Square tests yielded for each variable
| Study characteristic | n | Success rate | Unadjusted odds ratio (95% CI) for success | P-value | |
|---|---|---|---|---|---|
| Gender | Male | 87 | 75.9% | 0.693 (0.329-1.459) (F/M) | 0.333 |
| Female | 83 | 81.9% | |||
| Tooth type | Mand. molar | 54 | 72.2 % | - | 0.935 |
| Mand. premolars | 31 | 67.7 % | |||
| Max. molars | 58 | 72.4% | |||
| Max. premolars | 47 | 68.1% | |||
| Obturation void | Absent | 98 | 86.7% | 0.326 (0.152-0.701) (P/A) | 0.003* |
| Present | 72 | 68.05% | |||
| Obturation length | Underfilled | 125 | 90.4% | - | <0.001* |
| Flush | 25 | 60% | |||
| Overfilled | 20 | 30% | |||
| Apical lucency | Absent | 32 | 87% | 0.107 (0.054-0.256) (P/A) | <0.001* |
| Present | 138 | 43.8% | |||
| Coronal leakage | Absent | 109 | 90.8% | 0.136 (0.060-0.310) (P/A) | <0.001* |
| Present | 61 | 57.4% | |||
| Marginal caries | Absent | 117 | 84.6% | 0.354 (0.166-0.755) (P/A) | 0.006* |
| Present | 53 | 66% | |||
| Post | Absent | 92 | 70.7% | 3.185 (1.393-7.281) (P/A) | 0.005* |
| Present | 78 | 88.5% | |||
| Number of proximal contacts | Two | 82 | 97.6% | - | <0.001* |
| One | 69 | 66.7% | |||
| None | 19 | 42.1% | |||
| Mobility | Grade 0 | 53 | 90.6% | - | <0.001* |
| Grade 1 | 88 | 81.8% | |||
| Grade 2 | 26 | 53.8% | |||
| Grade 3 | 3 | 0% | |||
*: Statistically significant; 95% CI: 95% confidence interval; Mand; Mandibular; Max.: Maxillary; F/M: Female/Male; P/A: Present/Absent
As shown in Table 2, multiple binary logistic regression models showed that significant covariates on success were as follows: obturation void (P=0.037) and type of restoration (P<0.001) were associated with 13.1 and 3.2 times higher odds of predicting success, respectively. Moreover proximal contact problems (P<0.001), coronal leakage (P=0.048), suboptimal obturation length (P=0.020), and mobility (P=0.002) could significantly reduce the odds of success by 98%, 92%, 77%, and 76%, respectively. However, apical lucency, root length, marginal caries, tooth type and post were not significant predictors for the success (P>0.05).
Table 2.
Results of binary logistic regression models for the included covariates
| Covariate | B | SE of B | Adjusted OR (95% CI) | P-value |
|---|---|---|---|---|
| Tooth type | -0.176 | 0.268 | 0.839 (0.496-1.418) | 0.512 |
| Obturation void | 2.575 | 1.234 | 13.135 (1.168-147.752) | 0.037* |
| Obturation length | -1.464 | 0.631 | 0.231 (0.067-0.797) | 0.020* |
| Apical lucency | -0.273 | 0.862 | 0.761 (0.141-4.118) | 0.752 |
| Coronal leakage | -2.493 | 1.26 | 0.083 (0.007-0.982) | 0.048* |
| Marginal caries | -0.239 | 0.773 | 0.787 (0.173-3.582) | 0.758 |
| Post | -0.159 | 0.771 | 0.853 (0.188-3.864) | 0.837 |
| Proximal contacts | -3.707 | 0.726 | 0.025 (0.006-0.102) | <0.001* |
| Mobility | -1.39 | 0.451 | 0.249 (0.103-0.603) | 0.002* |
| Root length | -0.224 | 0.137 | 0.800 (0.611-1.046) | 0.102 |
| Type of the restoration | 1.185 | 0.331 | 3.272 (1.710-6.259) | <0.001* |
* Statistically significant, B: Unstandardized regression weight, SE: Standard Error, OR: Odds Ratio, CI: Confidence Interval
Discussion
The results of this observational study indicated that general (mobility and proximal contacts), endodontic (obturation void and length), and restorative/prosthodontic (coronal leakage, type of the restoration, and proximal contacts) variables may influence the treatment success. Hence, the null hypothesis was rejected.
The tooth was chosen as the smallest study unit in this study. Using roots/canals as the study unit may introduce bias, as endodontic failure is frequently not due to a single root/canal [21]. Delayed placement of the final restorations has a detrimental effect on the survival of ETT [22]. Hence, only teeth receiving the final restoration ≤ 2 weeks after the temporary ones were included in this study. Findings of this study showed an 89.4% survival rate for posterior ETT with a mean follow-up of more than two years. Amongst extracted teeth in this study, the most common reason for extraction was prosthodontic reasons, concurring with a previous study [14]. Previous studies with follow-up periods ranging from two to ten years reported 86%-93% survival rates for ETT [23]. A population-based cohort study on more than 2.8 million teeth in Korea showed a 90.8% five-year survival rate for ETT [12]. LópezValverde et al. reported a cumulative survival rate of 97%, 81%, 76% and 68% after 10, 20, 30, and 37 years of follow-up, respectively [24]. The relatively high survival rate of nonsurgical endodontic treatment makes it an effective method for maintaining natural teeth. Furthermore, the survival/success rate for vital pulp therapies and regenerative endodontics have been reported high. Success rate of full pulpotomy using CEM cement was reported very high in teeth with calcified or non-calcified pulp chambers [25]. Additionally, the overall survival rates for the endodontic regeneration procedures ranged from 94% and 100% [26].
Endodontic postgraduate students carried out the endodontic treatments in this study. Similarly, a prospective study with a follow-up of two to four years reported a survival rate of 95.4%, with endodontic postgraduate students carrying out the treatments [27]. The difference in the survival rates could be explained by the differences in study designs (i.e., retrospective/prospective/clinical trials), samples (teeth with simple/sophisticated treatments), and treatment features (quality of endodontic treatment and restoration).
Endodontic outcome studies used a variety of different measures to determine the treatment success. The functional theory [5], one of the simplest measures, was used in this study. It refers to the asymptomatic status of a functioning tooth as a success, regardless of any apical pathology revealed on X-rays [5]. The success rate of 78.8% in this study was similar to the previous findings of ~80% to 90% with different follow-up periods [24, 27-29]. This notably high success rate suggests that if a root canal treatment is possible, it may be better than more aggressive treatment options such as an implant [24, 28].
Numerous studies have demonstrated a substantial correlation between poor root filling quality and ETT failure [30-32]. Correspondingly, our findings suggested that an insufficiently obturated root (underfilled) with no discernible void was a strong predictor of success. Even though this finding was consistent with earlier research [33-35], some authors reported contradictory evidence [32, 35]. GarcíaGuerrero et al. found that short length filling was a significant predictor for failure, even when an optimal grade of tapering and homogeneity were present [32].
Interproximal contact areas play a pivotal role in maintaining interdental papilla, which directly affects the level of the underlying crestal bone, and guarantees the survival/success rate of the ETT [36]. As per our findings, higher mobility grades and fewer proximal contacts were associated with a higher failure rate. Grades 0 and 1 mobility were associated with acceptable success rates of 90.6% and 81.8%, respectively. Nevertheless, the success plunged in teeth with grades 2 and 3 mobility to 53.8% and 0%, respectively. Similar to our findings, another retrospective investigation revealed that the absence of mobility was associated with higher rates of periapical healing [37]. Furthermore, when both mesial and distal teeth were present, the success rate was 97.6%. The success, however, fell to 66.7% when one of the mesial or distal adjacent teeth was absent and to 42.1% when both were absent. These results corroborated earlier evidence [38].
The value of the coronal seal in obtaining success is debatable. According to a prospective cohort research, the quality of the coronal restoration did not affect the treatment outcome [35]. Later, another study showed that coronal filling quality influenced the treatment outcome [39]. However, its effect was reported to be of lesser impact than the root canal filling quality. Success rates of 90.8% and 57.4% were found in teeth without and with coronal leakage, respectively. The number of recognized parameters affecting endodontic outcomes exceeds twenty [14, 21, 27, 30, 31, 34, 37]. Controlling these variables is extremely difficult, if not impossible, and this multidimensional aspect of endodontic success may account for the divergent results. Although the difference is statistically significant, neither coronal leakage nor marginal caries were significant indicators of failure in regression models.
Furthermore, the type of restoration was a significant predictor of success. The best results were seen with crown, PCC, and amalgam build-up with post. Amalgam and composite build-ups, on the other hand, did not yield a high success rate. Similar to our findings, a previous study found that teeth with composite/amalgam build-ups were 2.29 times more expected to be extracted than those that received crowns [40]. Moreover, the survival rate of endodontically treated anterior teeth having unrestorable fracture which restored with full coverage crown was significantly higher than teeth restored with direct resin composite [41]. PCC+CL had the worst success amongst different coronal restorations. It has been shown that at 10-year follow-up, ETT that received the CL procedure after the endodontic treatment were roughly 2.3 times more prone to extraction compared with ETT that did not require the CL procedure [42]. According to the regression results, the presence of a post did not predict success in this study. Pontoriero et al. stated that when the placement of a post is related to the residual amount of the crown, its use does not change the final outcome of the ETT [43]. However, the increased retention given by a post must be weighed against the loss of healthy dental tissue, which might further deteriorate the tooth. It is thought that the more coronal tooth structural loss a post compensates, the more valuable it becomes [44]. The decision of when to place a post mainly depends on the coronal hard tissue loss, the tooth type, and the final restoration. However, the current literature does not define the precise level of structure loss at which a post contributes to the survival of an ETT. Nonetheless, when complex restorations are indicated, as in this investigation, current evidence justifies the use of posts [44].
One limitation of this study is the involvement of multiple operators in performing the treatments. Future studies should use the same design and be conducted by a single operator to ensure treatment consistency. Another limitation is the small sample size, which can be addressed by conducting larger-scale studies.
Conclusions
Within the limitations of this study, both endodontic and prosthodontic grounds could play vital roles in achieving treatment success. Underfilled obturation without noticeable void, crown/PCC/amalgam build-up with post, presence of proximal contacts, and absence of high grades of mobility were significant predictors for the success in nonsurgical endodontically treated posterior teeth.
Acknowledgements
This research was based on a thesis No. 3440
Conflict of interest
None.
Funding support
None.
Author contributions
MRV: Writing-original draft and editing, HA: Visualization and Supervision, FJ: Data curation, Investigation, ST: Writing-original draft and editing, AAB: Data analysis, KK: Writing-review and editing, NZ: Conceptualization, Methodology, Project administration. All authors contributed to the study and approved the final manuscript.
References
- 1.Bjørndal L, Laustsen M, Reit C. Root canal treatment in Denmark is most often carried out in carious vital molar teeth and retreatments are rare. Int Endod J. 2006;39(10):785–90. doi: 10.1111/j.1365-2591.2006.01149.x. [DOI] [PubMed] [Google Scholar]
- 2.Hamedy R, Shakiba B, Fayazi S, Pak JG, White SN. Patient-centered endodontic outcomes: a narrative review. Iran Endod J. 2013;8(4):197–204. [PMC free article] [PubMed] [Google Scholar]
- 3.Pak JG, Fayazi S, White SN. Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod. 2012;38(9):1170–6. doi: 10.1016/j.joen.2012.05.023. [DOI] [PubMed] [Google Scholar]
- 4.Chércoles-Ruiz A, Sanchez-Torres A, Gay-Escoda C. Endodontics, endodontic retreatment, and apical surgery versus tooth extraction and implant placement: a systematic review. J Endod. 2017;43(5):679–86. doi: 10.1016/j.joen.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Friedman S, Mor C. The success of endodontic therapy healing and functionality. J Calif Dent Assoc. 2004;32(6):493–503. [PubMed] [Google Scholar]
- 6.Riis A, Taschieri S, Del Fabbro M, Kvist T. Tooth survival after surgical or nonsurgical endodontic retreatment: long-term follow-up of a randomized clinical trial. J Endod. 2018;44(10):1480–6. doi: 10.1016/j.joen.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 7.Kim D, Lee H, Chung M, Kim S, Song M, Kim E. Effects of fast- and slow-setting calcium silicate-based root-end filling materials on the outcome of endodontic microsurgery: a retrospective study up to 6 years. Clin Oral Investig. 2020;24(1):247–55. doi: 10.1007/s00784-019-02937-6. [DOI] [PubMed] [Google Scholar]
- 8.Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30(12):846–50. doi: 10.1097/01.don.0000145031.04236.ca. [DOI] [PubMed] [Google Scholar]
- 9.Skupien JA, Opdam N, Winnen R, Bronkhorst E, Kreulen C, Pereira-Cenci T, Huysmans M-C. A practice-based study on the survival of restored endodontically treated teeth. J Endod. 2013;39(11):1335–40. doi: 10.1016/j.joen.2013.06.028. [DOI] [PubMed] [Google Scholar]
- 10.Borén DL, Jonasson P, Kvist T. Long-term survival of endodontically treated teeth at a public dental specialist clinic. J Endod. 2015;41(2):176–81. doi: 10.1016/j.joen.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Fransson H, Dawson VS, Frisk F, Bjørndal L, Jonasson P, Kvist T, Markvart M, Petersson K, Pigg M, Reit C. Survival of root-filled teeth in the Swedish adult population. J Endod. 2016;42(2):216–20. doi: 10.1016/j.joen.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Kwak Y, Choi J, Kim K, Shin S-J, Kim S, Kim E. The 5-year survival rate of nonsurgical endodontic treatment: a population-based cohort study in Korea. J Endod. 2019;45(10):1192–9. doi: 10.1016/j.joen.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Tabassum S, Khan FR. Failure of endodontic treatment: The usual suspects. Eur J Dent. 2016;10(01):144–7. doi: 10.4103/1305-7456.175682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olcay K, Ataoglu H, Belli S. Evaluation of related factors in the failure of endodontically treated teeth: a cross-sectional study. J Endod. 2018;44(1):38–45. doi: 10.1016/j.joen.2017.08.029. [DOI] [PubMed] [Google Scholar]
- 15.Suksaphar W, Banomyong D, Jirathanyanatt T, Ngoenwiwatkul Y. Survival rates against fracture of endodontically treated posterior teeth restored with full-coverage crowns or resin composite restorations: a systematic review. Restor Dent Endod. 2017;42(3):157–67. doi: 10.5395/rde.2017.42.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atlas A, Grandini S, Martignoni M. Evidence-based treatment planning for the restoration of endodontically treated single teeth: importance of coronal seal, post vs no post, and indirect vs direct restoration. Quintessence Int. 2019;50(10):772–81. doi: 10.3290/j.qi.a43235. [DOI] [PubMed] [Google Scholar]
- 17.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 18.Hommez GM, Coppens CR, De Moor RJ. Periapical health related to the quality of coronal restorations and root fillings. Int Endod J. 2002;35(8):680–9. doi: 10.1046/j.1365-2591.2002.00546.x. [DOI] [PubMed] [Google Scholar]
- 19.Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2(1):20–34. doi: 10.1111/j.1600-9657.1986.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 20.Bürklein S, Schäfer E, Jöhren HP, Donnermeyer D. Quality of root canal fillings and prevalence of apical radiolucencies in a German population: a CBCT analysis. Clin Oral Investig. 2020;24(3):1217–27. doi: 10.1007/s00784-019-02985-y. [DOI] [PubMed] [Google Scholar]
- 21.Stoll R, Betke K, Stachniss V. The influence of different factors on the survival of root canal fillings: a 10-year retrospective study. J Endod. 2005;31(11):783–90. doi: 10.1097/01.don.0000158229.43298.a9. [DOI] [PubMed] [Google Scholar]
- 22.Yee K, Bhagavatula P, Stover S, Eichmiller F, Hashimoto L, MacDonald S, Barkley G. Survival Rates of Teeth with Primary Endodontic Treatment after Core/Post and Crown Placement. J Endod. 2018;44(2):220–5. doi: 10.1016/j.joen.2017.08.034. [DOI] [PubMed] [Google Scholar]
- 23.Ng YL, Mann V, Gulabivala K. Tooth survival following non‐surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010;43(3):171–89. doi: 10.1111/j.1365-2591.2009.01671.x. [DOI] [PubMed] [Google Scholar]
- 24.López-Valverde I, Vignoletti F, Vignoletti G, Martin C, Sanz M. Long-term tooth survival and success following primary root canal treatment: a 5- to 37-year retrospective observation. Clin Oral Investig. 2023;27(6):3233–44. doi: 10.1007/s00784-023-04938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Farhadi A, Safarzadeh A, Nekouei AH, Sabeti M, Manochehrifar H, Shahravan A. Comparative Outcomes of Pulpotomy in Mature Molars with Irreversible Pulpitis: A Non-Randomized Trial Evaluating Calcified and Non-Calcified Pulp Chambers. Iran Endod J. 2024;19(1):13–21. doi: 10.22037/iej.v19i1.43894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rojas-Gutiérrez WJ, Pineda-Vélez E, Agudelo-Suárez AA. Regenerative Endodontics Success Factors and their Overall Effectiveness: An Umbrella Review. Iran Endod J. 2022;17(3):90–105. doi: 10.22037/iej.v17i3.32703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J. 2011;44(7):610–25. doi: 10.1111/j.1365-2591.2011.01873.x. [DOI] [PubMed] [Google Scholar]
- 28.Doyle SL, Hodges JS, Pesun IJ, Law AS, Bowles WR. Retrospective cross sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants. J Endod. 2006;32(9):822–7. doi: 10.1016/j.joen.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Dammaschke T, Steven D, Kaup M, Ott KH. Long-term survival of root-canal-treated teeth: a retrospective study over 10 years. J Endod. 2003;29(10):638–43. doi: 10.1097/00004770-200310000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44(7):583–609. doi: 10.1111/j.1365-2591.2011.01872.x. [DOI] [PubMed] [Google Scholar]
- 31.Santos SM, Soares JA, Costa GM, Brito-Júnior M, Moreira AN, de Magalhães CS. Radiographic parameters of quality of root canal fillings and periapical status: a retrospective cohort study. J Endod. 2010;36(12):1932–7. doi: 10.1016/j.joen.2010.08.050. [DOI] [PubMed] [Google Scholar]
- 32.García-Guerrero C, Delgado-Rodríguez CE, Molano-González N, Pineda-Velandia GA, Marín-Zuluaga DJ, Leal-Fernandez MC, Gutmann JL. Predicting the outcome of initial non-surgical endodontic procedures by periapical status and quality of root canal filling: a cohort study. Odontology. 2020;108(4):697–703. doi: 10.1007/s10266-020-00494-z. [DOI] [PubMed] [Google Scholar]
- 33.Schaeffer MA, White RR, Walton RE. Determining the optimal obturation length: a meta-analysis of literature. J Endod. 2005;31(4):271–4. doi: 10.1097/01.don.0000140585.52178.78. [DOI] [PubMed] [Google Scholar]
- 34.Fernández R, Cardona JA, Cadavid D, Álvarez LG, Restrepo FA. Survival of Endodontically Treated Roots/Teeth Based on Periapical Health and Retention: A 10-year Retrospective Cohort Study. J Endod. 2017;43(12):2001–8. doi: 10.1016/j.joen.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 35.Ricucci D, Russo J, Rutberg M, Burleson JA, Spångberg LS. A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(6):825–42. doi: 10.1016/j.tripleo.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 36.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995–6. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 37.Llena C, Nicolescu T, Perez S, Gonzalez de Pereda S, Gonzalez A, Alarcon I, Monzo A, Sanz JL, Melo M, Forner L. Outcome of Root Canal Treatments Provided by Endodontic Postgraduate Students A Retrospective Study. J Clin Med. 2020;9(6):1994–2007. doi: 10.3390/jcm9061994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caplan DJ, Kolker J, Rivera EM, Walton RE. Relationship between number of proximal contacts and survival of root canal treated teeth. Int Endod J. 2002;35(2):193–9. doi: 10.1046/j.1365-2591.2002.00472.x. [DOI] [PubMed] [Google Scholar]
- 39.Craveiro MA, Fontana CE, de Martin AS, Bueno CE. Influence of coronal restoration and root canal filling quality on periapical status: clinical and radiographic evaluation. J Endod. 2015;41(6):836–40. doi: 10.1016/j.joen.2015.02.017. [DOI] [PubMed] [Google Scholar]
- 40.Pratt I, Aminoshariae A, Montagnese TA, Williams KA, Khalighinejad N, Mickel A. Eight-Year Retrospective Study of the Critical Time Lapse between Root Canal Completion and Crown Placement: Its Influence on the Survival of Endodontically Treated Teeth. J Endod. 2016;42(11):1598–603. doi: 10.1016/j.joen.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 41.Phengudom P, Banomyong D, Jirathanyanatt T, Ngoenwiwatkul Y, Suksaphar W. Survival Rates of Unrestorable Fracture of Endodontically Treated Anterior Teeth Restored with Resin Composites or Crowns: A Retrospective Cohort Study. Iran Endod J. 2021;16(3):176–83. doi: 10.22037/iej.v16i3.30646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patil K, Khalighinejad N, El-Refai N, Williams K, Mickel A. The Effect of Crown Lengthening on the Outcome of Endodontically Treated Posterior Teeth: 10-year Survival Analysis. J Endod. 2019;45(6):696–700. doi: 10.1016/j.joen.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 43.Pontoriero DIK, Grandini S, Spagnuolo G, Discepoli N, Benedicenti S, Maccagnola V, Mosca A, Ferrari Cagidiaco E, Ferrari M. Clinical Outcomes of Endodontic Treatments and Restorations with and without Posts Up to 18 Years. J Clin Med. 2021;10(5):908–19. doi: 10.3390/jcm10050908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhuva B, Giovarruscio M, Rahim N, Bitter K, Mannocci F. The restoration of root filled teeth: a review of the clinical literature. Int Endod J. 2021;54(4):509–35. doi: 10.1111/iej.13438. [DOI] [PubMed] [Google Scholar]