Video
Introduction
EUS-guided gastrojejunostomy (EUS-GJ) is an effective treatment modality for gastric outlet obstruction (GOO).1,2 A well-known adverse event of this procedure is colonic injury during lumen-apposing metal stent (LAMS) placement.3, 4, 5 Few descriptions are available of delayed colonic injury after successful GJ.6 The following case describes the management of a delayed gastrojejunocolic fistula in a patient with indolent neoplastic disease (Video 1, available online at www.videogie.org).
Case
A 67-year-old man presented with GOO from a large unresectable duodenal GI stromal tumor measuring 12 × 10 × 9 cm in size. The GI stromal tumor was not responsive to imatinib. Surgical and endoscopic options were discussed, and the patient underwent EUS-GJ via the direct method without immediate adverse event. At a follow-up visit, the patient was tolerating a soft diet. He continued to do well for the next couple months, regained 30 lbs, and led a mostly normal life. Four months later, he presented to the hospital with weight loss, abdominal pain, nausea, and feculent emesis.
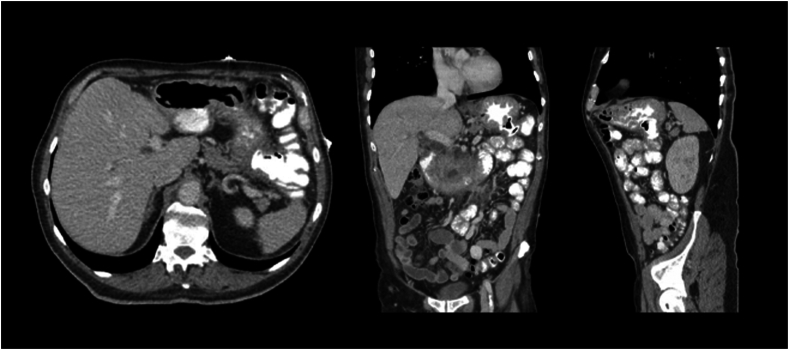
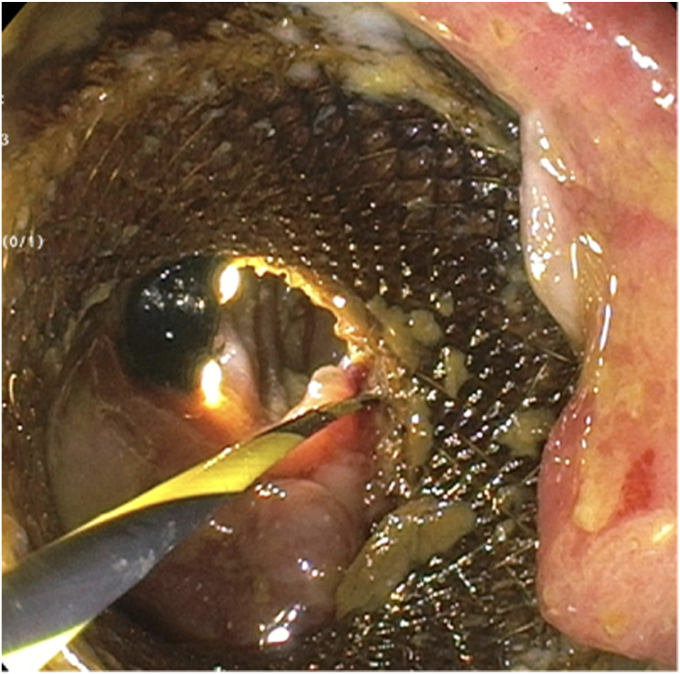
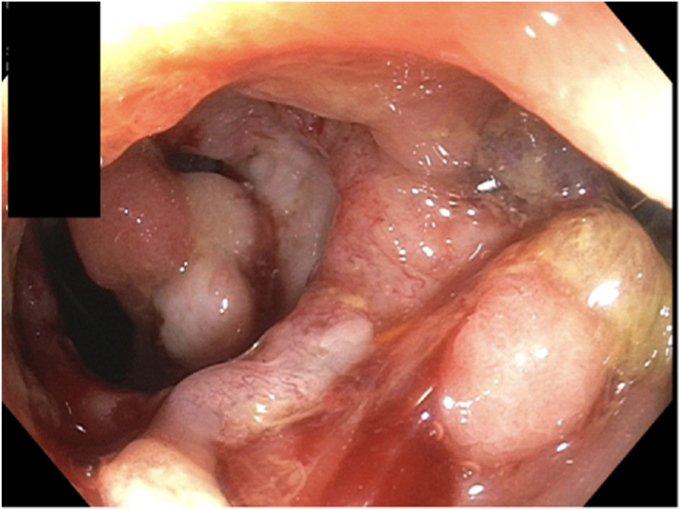
CT showed that the distal flange of the LAMS was displaced. It was in the colon near the splenic flexure, with oral contrast observed entering the jejunum and the colon (Fig. 1). The decision was made to proceed with endoscopic closure of the colonic aspect of the fistula followed by surgical GJ, given the patient's good performance status, lack of metastatic disease, and anticipated life expectancy. The plan was to let the gastrojejunal tract close with secondary intention. During endoscopy, the endoscope could enter both the jejunum and the colon from the stomach through the LAMS. Ulceration was noted where the distal flange had eroded through the jejunal wall into the colon, forming the fistula (Fig. 2). Guidewires were placed through the LAMS to help easily identify each tract (Fig. 3 and 4). With the upper endoscope in the stomach, the colonoscope was introduced. The gastrocolic fistula was found at the splenic flexure.
Figure 1.
CT scan demonstrating the displaced distal flange of the lumen-apposing metal stent in the colon.
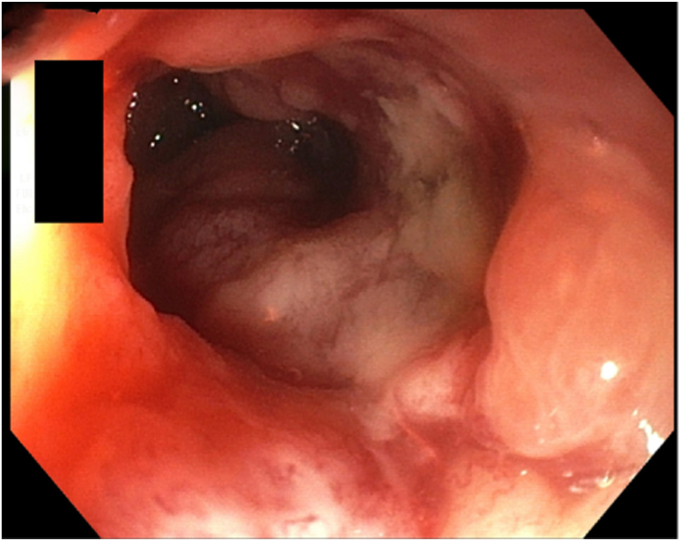
Figure 2.
After entering the jejunum via the lumen-apposing metal stent, ulceration is noted at the distal flange of the stent.
Figure 3.
View of the lumen-apposing metal stent from the stomach, with guidewire placement through the jejunocolic fistula.
Figure 4.
Two guidewires were placed through the lumen-apposing metal stent: one from the stomach into the colon and the second from the stomach into the small bowel.
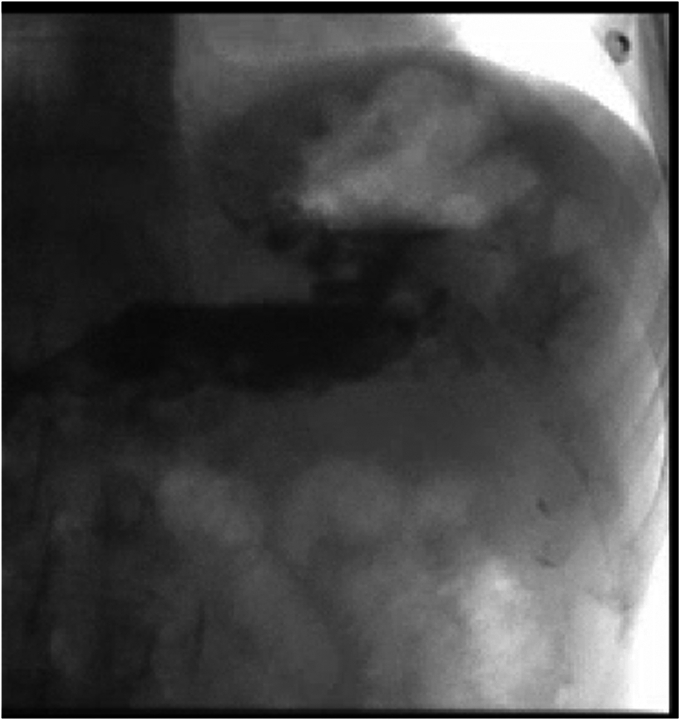
The LAMS was removed (Fig. 5). The colon defect was closed using endoscopic suturing (ES). Contrast mixed with methylene blue was injected from the stomach into the jejunum and did not enter the colon. An upper GI series performed the day after did not show a persistent connection (Fig. 6). CT scan obtained 2 days later showed a small persistent fistula. Given plans for surgery and the need to optimize nutritional status, the patient underwent repeat upper endoscopy to close the fistula and place a nasojejunal tube (Fig. 7). CT confirmed successful closure of the fistula. Clinically, his symptoms and nutritional status improved. Five days later, he underwent surgical GJ. Over the following year, he regained his weight, tolerated a regular diet, and maintained an active lifestyle.
Figure 5.
View of the fistula tract after lumen-apposing metal stent removal.
Figure 6.
Upper GI study after lumen-apposing metal stent removal and closure of jejunoclonic fistula tract, showing absence of leak.
Figure 7.
The second EGD showing small fistula from jejunum to colon along the tract from the stomach to the jejunum.
Conclusions
This case shows a rarely described delayed adverse event of EUS-GJ. Simultaneous upper and lower endoscopies were performed to identify the fistula, and ES was performed with successful closure. Limitations of this therapy include the advanced training and expertise required for ES.6 This case demonstrates that endoscopic management of fistula formation is a viable alternative to surgery.7, 8, 9 Physical health and long-term prognosis of a patient should be considered when determining between endoscopic management and surgical bypass for malignant GOO. Several studies have shown that EUS-GJ has high clinical success with limited adverse events compared with surgical GJ for GOO.10,11 EUS-GJ is associated with earlier resumption of oral intake, decreased length of hospital stay, and shorter time to resumption of chemotherapy, making it an attractive option for patients.11 Randomized studies are needed to evaluate longer-term durability of EUS-GJ in patients with a good performance status and nonmetastatic indolent neoplastic disease.
Disclosure
All authors disclosed no financial relationships.
Supplementary data
Endoscopic management of delayed gastrojejunocolic fistula after successful EUS-GJ.
References
- 1.Khashab M.A., Kumbhari V., Grimm I.S., et al. EUS-guided gastroenterostomy: the first U.S. clinical experience (with video) Gastrointest Endosc. 2015;82:932–938. doi: 10.1016/j.gie.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 2.Tyberg A., Perez-Miranda M., Sanchez-Ocaña R., et al. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: a multicenter, international experience. Endosc Int Open. 2016;4:E276–E281. doi: 10.1055/s-0042-101789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ichkhanian Y., Runge T., Jovani M., et al. Management of adverse events of EUS-directed transgastric ERCP procedure. VideoGIE. 2020;5:260–263. doi: 10.1016/j.vgie.2020.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shrigiriwar A., Mony S., Zhang L.Y., et al. Iatrogenic perforation during lumen-apposing metal stent deployment closed using an over-the-scope stent fixation clip device. VideoGIE. 2023;8:100–103. doi: 10.1016/j.vgie.2022.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghandour B., Bejjani M., Irani S.S., et al. Classification, outcomes, and management of misdeployed stents during EUS-guided gastroenterostomy. Gastrointest Endosc. 2022;95:80–89a. doi: 10.1016/j.gie.2021.07.023. [DOI] [PubMed] [Google Scholar]
- 6.Persaud T., Dawod E., Shah S., et al. Endoscopic management of gastrojejunocolic fistula after endoscopic gastrojejunostomy. VideoGIE. 2022;7:395–397. doi: 10.1016/j.vgie.2022.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Y.I., Itoi T., Baron T.H., et al. EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc. 2017;31:2946–2952. doi: 10.1007/s00464-016-5311-1. [DOI] [PubMed] [Google Scholar]
- 8.Mukewar S., Kumar N., Catalano M., et al. Safety and efficacy of fistula closure by endoscopic suturing: a multi-center study. Endoscopy. 2016;48:1023–1028. doi: 10.1055/s-0042-114036. [DOI] [PubMed] [Google Scholar]
- 9.Sharaiha R.Z., Kumta N.A., DeFilippis E.M., et al. A large multicenter experience with endoscopic suturing for management of gastrointestinal defects and stent anchorage in 122 patients: a retrospective review. J Clin Gastroenterol. 2016;50:388–392. doi: 10.1097/MCG.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 10.Miller C., Benchaya J.A., Martel M., et al. EUS-guided gastroenterostomy vs. surgical gastrojejunostomy and enteral stenting for malignant gastric outlet obstruction: a meta-analysis. Endosc Int Open. 2023;11:E660–E672. doi: 10.1055/a-2098-2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canakis A., Bomman S., Lee D.U., et al. Benefits of EUS-guided gastroenterostomy over surgical gastrojejunostomy in the palliation of malignant gastric outlet obstruction: a large multicenter experience. Gastrointest Endosc. 2023;98:348–359. doi: 10.1016/j.gie.2023.03.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic management of delayed gastrojejunocolic fistula after successful EUS-GJ.