Abstract
Dermoid cysts represent the most frequent type of orbital cystic lesions observed in children. While superficial orbital dermoid cysts manifest early in life as slowly growing masses, deep dermoid cysts typically remain clinically undetectable until adolescence or adulthood, at which point they enlarge and induce proptosis. Imaging studies play a pivotal role in precisely determining location and size, excluding intracranial and intraorbital extensions, and facilitating the planning of management strategies for complex cases.
We present a case of a 5-year-old boy admitted for slowly developing of ocular motility limitation of the right eye, observed by the parents. The imaging revealed a well-circumscribed extraconal cystic mass, with radiological characteristics primarily suggesting a dermoid cyst. The cyst was surgically excised without complications, and the histopathological examination of the operative specimen confirmed our diagnosis.
Keywords: Dermoid cyst, Orbital, Imaging, Children
Introduction
Dermoid cysts are benign, congenital cystic teratomas [1], characterized as developmental cystic lesions originating from the inclusion of ectodermal elements during the closure of the neural tube adjacent to fetal suture lines [2]. They are the most common orbital cystic lesions encountered in children, typically classified as superficial or deep types based on their relationship to the orbital septum [1]. Computed tomography and magnetic resonance imaging assist in precisely measuring the location, size, and extension of dermoid cysts, distinguishing cystic from solid lesions, identifying cyst type, and aiding in planning the management approach for challenging cases [3]. The timing of surgical excision is a matter of debate. Indications for surgical excision include functional impairment by the cyst, cosmetic concerns of the patient or parents, and the risk of trauma, rupture, and subsequent severe inflammation [4].
Case report
We report the case of a 5-year-old boy with no significant medical history, admitted for a slowly developing limitation in ocular motility of the right eye, as observed by his parents. The condition evolved without orbital pain, inflammation, or fever, and his general health remained unaffected. There was no history of trauma or ocular infection. Clinical examination revealed restricted ocular motility, particularly in right eye abduction, with no signs of inflammation, proptosis, strabismus, or visual impairment. The rest of the physical examination was unremarkable, and the infectious work-up was negative.
Due to the unavailability of immediate MRI, an initial orbital CT scan was performed, showing a well-circumscribed extraconal mass in the right superolateral orbital wall with smooth bone remodeling and fluid-attenuating content, without bone invasion (Fig. 1). Subsequent MRI confirmed a cystic mass in the right superior extraconal compartment, hyperintense on T2-weighted images and hypointense on FLAIR, without diffusion restriction or enhancement with Gadolinium (Fig. 2, Fig. 3). The mass caused slight compression of the external and superior right oculomotor muscles, resulting in a limitation of abduction in the right eye, but without involving surrounding structures like the optic nerve and intraconal fat; or show signs of intracranial extension. These imaging features strongly suggested a dermoid cyst.
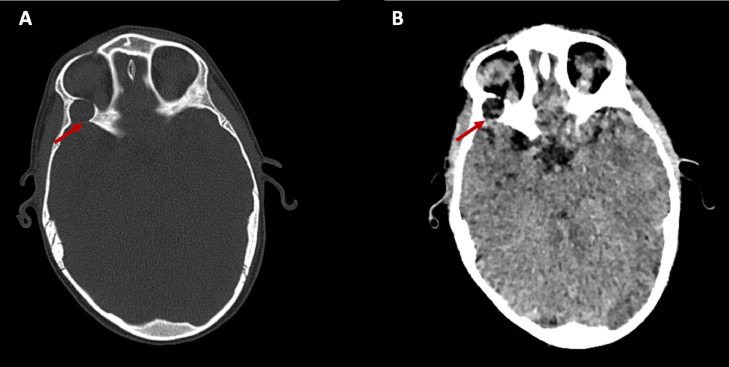
Fig. 1.
Axial CT scan sections with bone (A) and parenchymal(B) windows reveal a well-circumscribed extraconal fluid mass (arrow) located at the right superolateral orbital wall, adjacent to the left frontozygomatic suture. The bone exhibits smooth remodeling without signs of invasion.
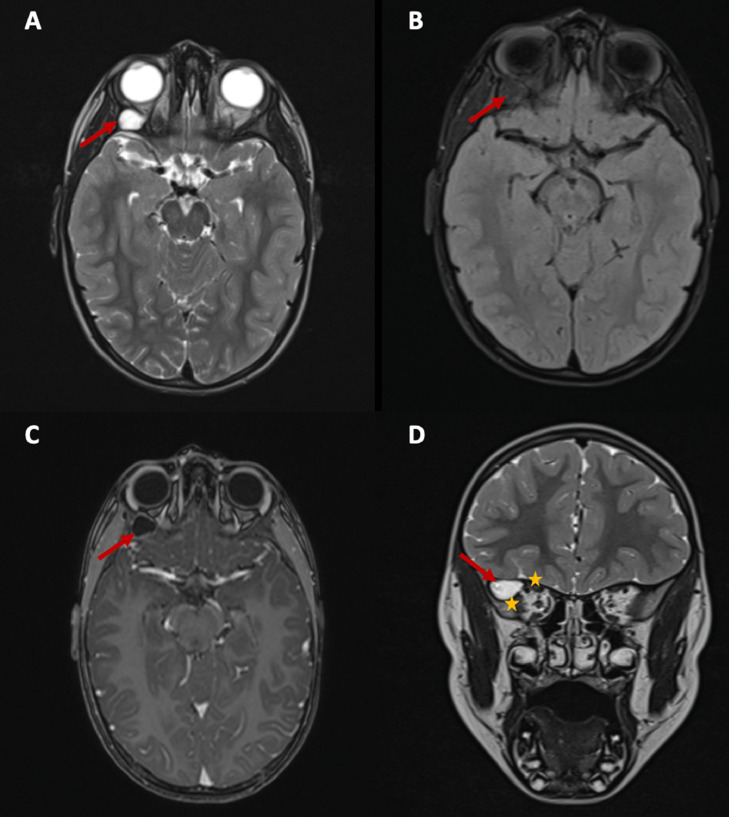
Fig. 2.
Orbital MRI images on axial T2-weighted (A) and FLAIR (B) sections, axial Gadolinium section (C), and coronal T2-weighted section (D) illustrating the presence of a cystic mass (arrow) within the right superior extraconal compartment. The mass exhibits hyperintensity on T2-weighted images and hypointensity on FLAIR imaging. Furthermore, there is enhancement of the wall and a nonenhancing lumen following Gadolinium administration. Note the slight mass effect observed on the external and superior right oculomotor muscles (asterix), along with the absence of invasion into neighboring structures.
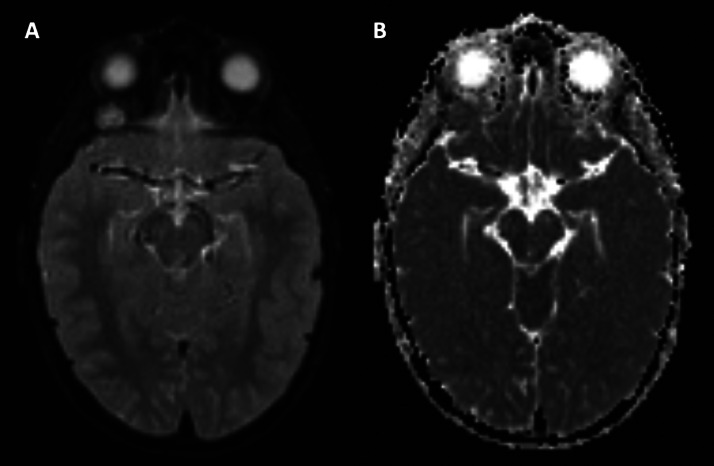
Fig. 3.
Axial sections of orbito-cerebral MRI on Diffusion sequence (A) and ADC mapping (B) shows the absence of diffusion restriction within the orbital mass, indicating its benign nature.
The patient underwent successful microsurgical cystectomy, and histopathology confirmed the diagnosis, showing a cyst wall lined with squamous epithelium and keratin, supported by fibrous tissue (Fig. 4). The postoperative course was uneventful, with favorable recovery.
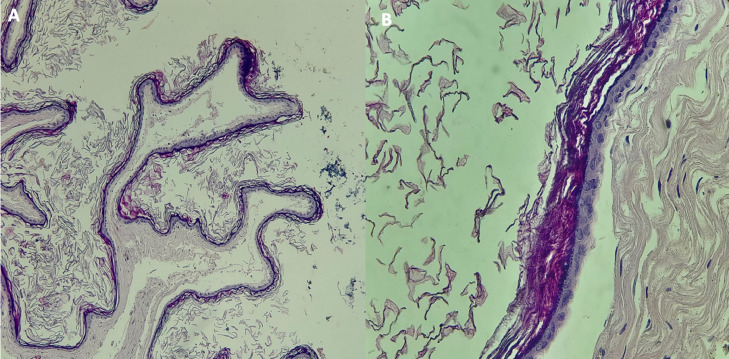
Fig. 4.
Histological examination of the excised specimen at ×10 magnification (A) and with Hematoxylin-Eosin staining at ×40 (B) reveals a cystic wall lined by regular squamous epithelium, covered with keratin, and resting on fibrous tissue with a discrete mononuclear inflammatory infiltrate, consistent with a dermoid cyst.
Discussion
Dermoid cysts are the most common cystic lesions in the orbit, particularly among the pediatric population, accounting for 3 to 9% of orbital tumors [4]. Nearly all are congenital developmental abnormalities resulting from the inclusion of ectodermal elements during the closure of the neural tube adjacent to fetal suture lines [5].
Orbital dermoid cysts are classified into superficial and deep types. Literature indicates that more than 50% of reported cases in the head and neck region involve the periorbital location of dermoid cysts [6,7]. Most periorbital cysts were identified in relation to the frontozygomatic suture, especially in the superotemporal area. Similarly, many orbital cysts are found in the temporal or superotemporal quadrant [8].
Clinical manifestations depend on cyst location and size. Superficial cysts are often noticed in the first year of life as painless, smooth, firm, and mobile masses along the orbital rim [9,10]. In contrast, deeper lesions may not be diagnosed until later, typically presenting as insidious, painless proptosis [8].
Imaging studies are crucial for ruling out intracranial and intraorbital extensions [11]. In CT scans, an orbital dermoid cyst may manifest as a well-defined mass with an enhancing wall and a nonenhancing lumen [12]. Secondary bony remodeling of the adjacent orbital wall is common, with about 20% of cysts being subperiosteal and associated with extensive remodeling [9]. MRI typically shows dermoid cysts as well-defined round or ovoid masses of variable size. The mass's homogeneity influences its signal intensity; cysts can be iso- or hypointense on T1-weighted images or exhibit a bright, fat-like signal intensity, typically appearing hyperintense on T2-weighted images. Occasionally, the cyst margin may show calcification, and the cyst wall may enhance if inflamed. Reduced diffusivity is expected, and a small sinus tract may lead from the cyst to the skin surface [9]. MRI is particularly valuable for delineating the extent of deep orbital cysts, which pose significant surgical challenges [5].
The differential diagnoses for dermoid cysts include orbital cellulitis, pseudotumor, epithelial inclusion cyst, hydatid cyst, and cold abscess [8]. When differentiating these conditions, imaging plays a critical role. Orbital cellulitis typically shows diffuse soft tissue inflammation with contrast enhancement, which contrasts with the more well-defined, nonenhancing nature of dermoid cysts. Pseudotumors may display heterogeneous enhancement and infiltrative characteristics, unlike the localized and well-circumscribed appearance of dermoid cysts. Epithelial inclusion cysts can resemble dermoid cysts but often lack the characteristic fat content visible on imaging. Hydatid cysts, on the other hand, are often identified by the presence of a multilayered membrane or daughter cysts, features that are absent in dermoid cysts. Cold abscesses typically show rim enhancement and may be accompanied by signs of inflammation, further distinguishing them from dermoid cysts. Finally, malignant tumors may present as irregular, enhancing masses with potential bone involvement, which differs from the benign, noninvasive nature of dermoid cysts; but it is crucial to bear in mind that they may mimic orbital dermoid cysts [5].
Histologically, most cysts present with stratified squamous keratinized epithelium lining the cyst wall. Occasionally, the cyst wall may feature nonkeratinized conjunctival epithelium [13,14].
To prevent rupture and secondary inflammation, it is crucial to excise the cyst along with its capsule. This approach also aids in obtaining a pathological diagnosis and achieving a better cosmetic result [12]. Superficial cysts with distinct, palpable margins and no sutural involvement can be easily excised [15]. In contrast, anteriorly located cysts that involve sutures require careful dissection to release adhesions to surrounding structures before addressing any bony extensions [4,16]. Deep orbital cysts are more challenging and necessitate imaging studies for surgical planning. The primary goal during surgery is to achieve complete excision without rupturing the cyst while protecting delicate orbital structures, including ocular tissues, vessels, and nerves [5]. Surgical approaches for deep cysts may include supero-nasal orbitotomy or lateral orbitotomy [4]. In cases of intracranial extension, a multidisciplinary approach involving head and neck surgeons and neurosurgeons is essential [5].
Conclusion
Deep orbital dermoid cysts are less common than superficial types in children. They typically manifest later in life and present greater diagnostic and treatment complexities. Imaging plays a crucial role in their diagnosis, assisting in assessing their extent. It is crucial to raise public awareness about the importance of early presentation and timely management of such benign lesions.
Author contributions
All authors contributed to this work. All authors have read and approved the final version of the manuscript.
Ethical approval and informed consent
Ethics approval does not need to be obtained: This is a case report, based on the editor Guidelines-Ethics Approval and Informed Consent Statements: Ethics committee/IRB approval is often not required.
Patient consent
Written informed consent was obtained from the legal authorized representative (LAR) of the patient for the publication of this case report.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Fasina O, Ogun OG. Giant deep orbital dermoid cyst presenting early in infancy in a nigerian child: a case report and review of the literature. J Med Case Rep. 2012;6:320. doi: 10.1186/1752-1947-6-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bekibele CO, Oluwanisola AO. A clinicopathological study of orbito-ocular diseases in Ibadan between 1991–1999. Afr J Med Med Sci. 2003;32:197–202. [PubMed] [Google Scholar]
- 3.Eldesouky MA, Elbakary MA. Orbital dermoid cyst: classification and its impact on surgical management. Sem Ophthalmol. 2016;31(1):1–5. doi: 10.1080/08820538.2016.1182636. [DOI] [PubMed] [Google Scholar]
- 4.Dave TV, Gupta Rathi S, Kaliki S, Mishra D. Orbital and periorbital dermoid cysts: comparison of clinical features and management outcomes in children and adults. Eur J Ophthalmol. 2021;31(5):2631–2638. doi: 10.1177/1120672120964686. [DOI] [PubMed] [Google Scholar]
- 5.Ahuja R, Azar NF. Orbital dermoids in children. Sem Ophthalmol. 2006;21(3):207–211. doi: 10.1080/08820530500353963. [DOI] [PubMed] [Google Scholar]
- 6.Pollard ZF, Harley RD, Calhoun J. Dermoid cysts in children. Pediatrics. 1976;57:379–382. [PubMed] [Google Scholar]
- 7.Pryor SG, Lewis JE, Weaver AL, Orvidas LJ. Pediatric dermoid cysts of the head and neck. Otolaryngol Head Neck Surg. 2005;132:938–942. doi: 10.1016/j.otohns.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Pushker N, Meel R, Kumar A, Kashyap S, Sen S, Bajaj MS. Orbital and periorbital dermoid/epidermoid cyst: a series of 280 cases and a brief review. Can J Ophthalmol. 2020;55(2):167–171. doi: 10.1016/j.jcjo.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Joseph AK, Guerin JB, Eckel LJ, Dalvin LA, Keating GF, Liebo GB, et al. Imaging findings of pediatric orbital masses and tumor mimics. RadioGraphics. 2022;42(3):880–897. doi: 10.1148/rg.210116. [DOI] [PubMed] [Google Scholar]
- 10.Shields JA, Shields CL. Orbital cysts of childhood: classification, clinical features, and management. SurvOphthalmol. 2004;49(3):281–299. doi: 10.1016/j.survophthal.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Shepherd GP, Lewis JE, Weaver AL, Orvidas LJ. Pediatric dermoid cysts of the head and neck. Otolaryngol Head Neck Surg. 2005;132:938–942. doi: 10.1016/j.otohns.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Cavazza S, Laffi GL, Lodi L, Gasparrini E, Tassinari G, Conti GC, et al. Orbital dermoid cyst of childhood: clinical pathologic findings, classification and management. Int Ophthalmol. 2011;31:93–97. doi: 10.1007/s10792-011-9419-y. [DOI] [PubMed] [Google Scholar]
- 13.McCollough ML, Glover AT, Grabski WJ, Kelley GJ, Jones RL, Henson DD, et al. Orbital dermoid cysts showing conjunctival epithelium. Am Dermatopathol. 1991;13(6):611–615. doi: 10.1097/00000372-199113060-00012. [DOI] [PubMed] [Google Scholar]
- 14.Abou-Rayyah Y, Rose GE, Konrad H, Adams GG, Collin JR, Moseley IF, et al. Clinical, radiological and pathological examination of periocular dermoid cysts: evidence of inflammation from an early age. Eye. 2002;16(5):507–512. doi: 10.1038/sj.eye.6700045. [DOI] [PubMed] [Google Scholar]
- 15.Hachach-Haram N, Benyon S, Shanmugarajah K, Kirkpatrick WNA, Smith JD, Taylor CJ, et al. Back to basics: a case series of angular dermoid cyst excision. J PlastReconstrAesthet Surg. 2013;66(1):57–60. doi: 10.1016/j.bjps.2012.07.030. [DOI] [PubMed] [Google Scholar]
- 16.Sathananthan N, Moseley IF, Rose GE, Wright JE, Lee AJ, Hamed M. The frequency and clinical significance of bone involvement in outer canthus dermoid cysts. Br J Ophthalmol. 1993;77(12):789–794. doi: 10.1136/bjo.77.12.789. [DOI] [PMC free article] [PubMed] [Google Scholar]