Abstract
Background
As antiretroviral therapy (ART) allows the world's 2.3 million human immunodeficiency virus (HIV)–infected children to grow and thrive, these children need to be informed of their HIV status. Neither the prevalence of disclosure to children nor its impact has been evaluated in most resource-limited settings.
Methods
We conducted a prospective assessment of a random sample of HIV-infected children ages 6–14 years enrolled in HIV care at a large referral clinic in Eldoret, Kenya. Clinicians administered questionnaires to children and caregivers independently at routine clinic visits to assess disclosure status, ART adherence, stigma, and depression. Children's demographic and clinical characteristics were extracted from chart review. We calculated descriptive statistics and performed logistic regression to assess the association between disclosure and other characteristics.
Results
Two hundred seventy children–caregiver dyads completed questionnaires. The mean child age was 9.3 years (standard deviation 2.6); 49% were male, and 42% were orphans. 11.1% of children had been informed of their HIV status (N = 30). Of those under 10 years, 3.3% knew their status, whereas 9.2% of 10- to 12-year-olds and 39.5% of 13- to 14-year-olds knew they had HIV. Only age was significantly associated with disclosure status in both bivariate analyses (P < .0001) and multiple logistic regression (odds ratio 1.67, 95% confidence interval 1.36–2.05) when considering social demographics, disease stage variables, adherence, stigma measures, and depression.
Conclusions
Rates of informing children in western Kenya of their HIV status are low, even among older children. Guiding families through developmentally appropriate disclosure processes should be a key facet of long-term pediatric HIV management.
Keywords: Africa, Disclosure, HIV, Pediatrics
(See the Editorial Commentary by Lowenthal and Marukutira on pages 144–6.)
In December 2009, the World Health Organization (WHO) estimated there were more than 2.3 million human immunodeficiency virus (HIV)–infected children worldwide [1], with almost 90% living in sub-Saharan Africa [2]. As increased access to antiretroviral therapy (ART) allows more HIV-infected children to survive into adolescence and adulthood, HIV care systems face new challenges to sustain treatment adherence, provide psychosocial support, and find culturally appropriate methods to disclose HIV status to children [1, 3].
In the context of pediatric HIV infection, disclosure refers to a child gaining knowledge of his or her HIV status [4]. As children develop and progress to adulthood, they need to be informed of their HIV status and transitioned into taking responsibility for their own HIV management [5].
Disclosure involves giving children age-appropriate information regarding their illness, ideally progressing to full disclosure of their HIV infection when the child has the cognitive, emotional, and psychological maturity to process this information [4–7]. Despite recognizing that disclosure is crucial to long-term disease management, including HIV treatment and prevention [7], many care systems in resource-limited settings wrestle with this new challenge.
The prevalence of disclosure varies widely. A 2007 review reported disclosure rates from 10% to 75% among several studies from North America and Europe [4]. The prevalence of disclosure of HIV status to children in sub-Saharan Africa is not well described. The limited existing studies from low- and middle-income countries suggest that disclosure is still relatively rare, with rates of reported disclosure varying from 1.7% to 41% [8–14]. Healthcare providers, parents, and other caregivers of HIV-infected children in resource-limited settings believe that disclosure may have benefits, but weigh these against feared risks. They believe that disclosure could lead to better ART adherence [8–11, 15–21], improve the child's long-term HIV care or clinic adherence [9–12, 15, 17, 18, 20–22], and equip the child to better protect themselves and others [12, 21], preventing HIV transmission [23]. However, parents and caregivers fear that the child will subsequently disclose their HIV status to others [9–12, 17, 21, 24, 25], resulting in stigma and social isolation [10, 11, 17, 21, 22, 24]. They also worry that disclosure will negatively impact the children's psychological or emotional health [9, 10, 16, 17, 19, 25–27].
Information on the appropriate timing for pediatric HIV disclosure and its actual impact is needed to guide a supportive disclosure process within the HIV care systems of sub-Saharan Africa. This study sought to determine the prevalence of disclosure of HIV status among a representative population of HIV-infected children in Kenya and to evaluate whether various sociodemographic, clinical, and emotional factors are associated with disclosure.
METHODS
Study Design
We conducted a cross-sectional, facility-based study to determine the prevalence of disclosure to HIV-infected children enrolled within the Moi Teaching and Referral Hospital (MTRH) pediatric HIV clinic of the United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership. In addition to assessing prevalence of disclosure, we evaluated children's adherence, clinical outcomes, and experiences of stigma. This research occurred over a 5-month period, using prospective sampling with a questionnaire to determine the prevalence of disclosure and the experience of adherence and stigma. Questionnaires were administered to a random sample of HIV-infected children receiving HIV care through the MTRH clinic, as well as to their caregivers (parent or guardian). The questionnaire was administered independently to the child and the child's caregiver by the clinician evaluating the child during a routine HIV clinic visit.
Setting
The AMPATH partnership currently provides care for over 120 000 HIV-infected patients in Kenya, including 15 350 pediatric patients, through 25 parent and 26 satellite clinical sites. The AMPATH partnership was formed out of a collaboration between the Indiana University School of Medicine and the Moi University School of Medicine [28]. The largest AMPATH clinic is based at MTRH in Eldoret, Kenya, which in November 2011 treated 13 400 total patients, including 1578 HIV-infected pediatric patients age 6–14 years. All AMPATH clinics provide comprehensive HIV care for HIV-exposed and HIV-infected children, including free ART, regular clinical follow-up, adherence counseling, nutritional supplementation, and psychosocial support groups through support from the USAID–President's Emergency Plan For AIDS Relief (PEPFAR). Clinicians typically complete standardized paper encounter forms at monthly or bimonthly visits, with these data subsequently entered into the AMPATH electronic medical record system [29]. At the time of this study, the standard AMPATH encounter forms did not incorporate routine questions about pediatric disclosure, nor did AMPATH have a standard disclosure protocol for children, although disclosure to children 10 years and older was encouraged as part of adherence counseling, adolescent psychosocial support, and in the general pediatric care protocols.
Participants and Selection Criteria
The target population was HIV-infected children ages 6– to 14 years who were currently enrolled in the AMPATH MTRH pediatric clinic, with evaluation of both children and their caregivers. HIV infection was defined as having one positive HIV DNA polymerase chain reaction (PCR) test for patients less than 18 months of age and as having either a positive HIV enzyme-linked immunosorbent assay antibody test or a positive HIV DNA PCR test for patients 18 months and older. Six years was selected as the minimal age for inclusion in an attempt to determine the youngest age for disclosure within this population. The choice was made based on qualitative data obtained in this setting, suggesting that very few children less than 10 years of age know their status [26]. The maximum age included was 14 years since adolescents above 14 years are transferred to the adult HIV care system, where disclosure is assumed.
Data Collection
A specialized query of the AMPATH electronic medical record system generated a random sample of 300 patients meeting the inclusion criteria. Then, study disclosure questionnaires were placed on the charts of patients in this random sample. When any of the randomly selected patients presented to the clinic for either routine or unscheduled clinic visits, the AMPATH clinician administered the disclosure questionnaire to the participants and to their caregivers in addition to their usual clinical encounter.
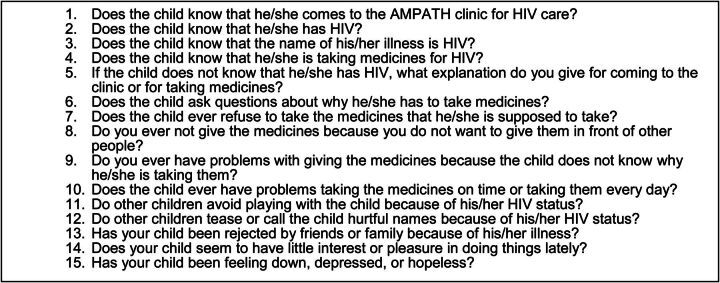
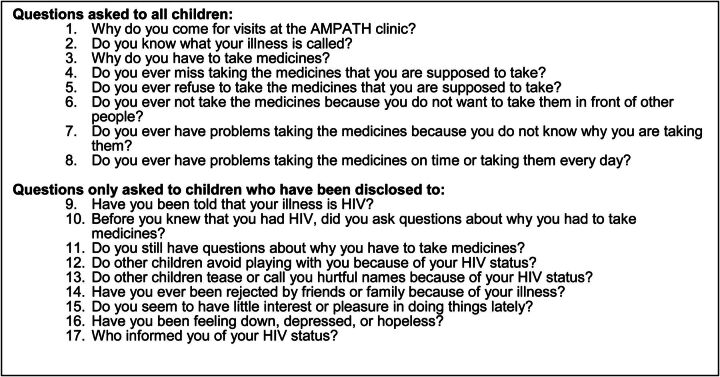
The caregiver and child questionnaires consisted of questions related to the HIV-infected child's disclosure status, their adherence to medications, stigma, and their mental health. (Questionnaire items are summarized in Figures 1 and 2.) Clinicians were chosen to administer the questionnaires for three reasons: (1) AMPATH was trying to incorporate disclosure assessments into routine care, (2) the clinician might already have a therapeutic relationship with the family, and (3) the collected data were potentially useful for the clinical encounter. In order to prevent accidental disclosure to children, the portion of the child questionnaire administered to all children (Figure 2) did not mention HIV specifically. Children who reported knowing their HIV status and children for whom caregivers reported the child knowing their status were asked additional questions specific to disclosure and HIV. In addition, study personnel collected relevant, concurrent clinical information from the participants' charts, including data on patient demographics, HIV progression, and clinical outcomes.
Figure 1.
HIV Disclosure Questionnaire items. Abbreviations: AMPATH, Academic Model Providing Access to Healthcare; HIV, human immunodeficiency virus.
Figure 2.
Child HIV Disclosure Questionnaire items. Abbreviations: AMPATH, Academic Model Providing Access to Healthcare; HIV, human immunodeficiency virus.
The study was approved by the Institutional Review Boards at Indiana University School of Medicine in Indianapolis, Indiana and by the Institutional Review and Ethics Committee at Moi University School of Medicine in Eldoret, Kenya.
Data Analysis
The prevalence of disclosure to children was described for the overall study population, as well as for subcategories divided by age. We performed bivariate analyses to look for associations between disclosure and clinical and demographic attributes. Additionally, we performed multivariable logistic regression to assess the independent association between being disclosed to and the key variables of interest, including HIV disease stage, orphan status, being on ART, adherence to medication and coming to the clinic, positive depression screen, and experienced stigma. We calculated stratified analyses looking for associations between the covariates and tested for statistical significance of interactions using likelihood ratios.
Caregiver-reported disclosure was defined as a positive answer to any of the questions about the child knowing about their HIV status (questions 1, 2, 3, or 4 in Figure 1). Child-reported disclosure was defined as self-reporting HIV as the reason why the child was taking medicines, coming to AMPATH, or as the name of his/her illness (questions 1, 2, or 3 in Figure 2). Perfect 30-day adherence was defined as reporting no missed doses on a single item self- or proxy-report of whether the child has missed any medications over the past 30 days as asked during the clinic encounter. Composite good adherence was defined as reporting no missed doses on 30-day recall, as well as no reports of the child refusing medications, of not giving medications because others are around, or having problems giving ART on time. Caregiver-reported stigma and child-reported stigma were defined through reports of experienced stigma (a positive response to questions 11, 12, or 13 on the caregiver questionnaire or to questions 12, 13, or 14 on the child questionnaire). Caregiver-reported difficulty with taking medicines was defined as any positive answer to questions 7, 8, 9, or 10 on the caregiver questionnaire, while child-reported difficulty with taking medicines was defined as a positive answer to questions 4, 5, 6, 7, or 8 on the child questionnaire.
RESULTS
Participants
Demographic and clinical data for the study participants are shown in Table 1. During the study period, 270 children and their caregivers completed disclosure questionnaires—17.1% of HIV-infected 6–14-year-olds at the clinic. Fifty-one percent of the children were female, and the median age was 9 years (mean age 9.3 years, standard deviation 2.6). Two hundred one (74.4%) of the subjects were on ART. The majority of the children (63.7%) were WHO Stage 3 or 4.
Table 1.
Characteristics of Study Participants by Disclosure Status
| Variable | Disclosure Status |
P Value | |
|---|---|---|---|
| Disclosed | Not Disclosed | ||
| N = 30 (%) | N = 240 (%) | ||
| Sex | N = 30 | N = 240 | .366 |
| Male | 17 (56.7%) | 115 (47.9%) | |
| Female | 13 (43.3%) | 125 (52.1%) | |
| Orphan | N = 30 | N = 238 | .108 |
| Mother deceased | 2 (6.7%) | 26 (10.9%) | |
| Father deceased | 3 (10.0%) | 37 (15.6%) | |
| Both parents deceased | 10 (33.3%) | 31 (13.0%) | |
| Not orphaned | 15 (50.0%) | 140 (58.8%) | |
| Don't know | 0 (0.0%) | 4 (17%) | |
| On ARVs | N = 30 | N = 240 | .132 |
| Yes | 24 (86.7%) | 175 (72.9%) | |
| No | 3 (13.3%) | 65 (27.1%) | |
| On TB meds | N = 30 | N = 240 | 1.000 |
| Yes | 1 (3.3%) | 8 (3.3%) | |
| No | 29 (96.7%) | 231 (96.3%) | |
| Don't know | 0 (0.0%) | 1 (0.4%a) | |
| On PCP prophylaxis | N = 30 | N = 240 | 1.000 |
| Yes | 30 (100%) | 240 (100%) | |
| No | 0 (0%) | 0 (0%) | |
| Caregiver | N = 30 | N = 240 | .103 |
| Mother | 15 (50.0%) | 157 (65.4%) | |
| Father | 3 (10.0%) | 22 (9.2%) | |
| Grandparent | 2 (6.7%) | 13 (5.4%) | |
| Aunt/uncle | 5 (16.7%) | 24 (10.0%) | |
| Children's home | 0 (0%) | 5 (2.1%) | |
| Sibling | 1 (3.3%) | 7 (2.9%) | |
| Cousin | 1 (3.3%) | 6 (2.5%) | |
| Stepmother | 0 (0%) | 4 (1.7%) | |
| Other | 3 (10.0%) | 2 (0.8%) | |
| WHO disease stage | N = 30 | N = 239 | .248 |
| Stage I | 7 (23.3%) | 32 (13.4%) | |
| Stage II | 4 (13.3%) | 54 (22.6%) | |
| Stage III | 18 (60.0%) | 128 (53.6%) | |
| Stage IV | 1 (3.3%) | 25 (10.5%) | |
| Poor adherence on 30-day recall | N = 30 | N = 240 | .104 |
| Yes | 2 (6.7%) | 11 (4.6%) | |
| No | 24 (80.0%) | 217 (90.4%) | |
| Don't know | 4 (13.3%) | 12 (5.0%) | |
| Reports any adherence problem | N = 30 | N = 240 | .356 |
| Yes | 9 (30.0%) | 85 (35.4%) | |
| No | 21 (70.0%) | 155 (64.6%) | |
| Age in years | N = 30 | N = 240 | < .0001 |
| Mean (SD) | 11.87 (2.3) | 8.96 (2.40) | |
| Median (IQR) | 13 (10, 13) | 9 (7, 11) | |
| CD4 % | N = 30 | N = 240 | .7811 |
| Mean (SD) | 0.25 (0.12) | 0.26 (0.09) | |
| Median (IQR) | 0.27 (0.17, 0.34) | 0.27 (0.20, 0.33) | |
| Weight (kg) | N = 30 | N = 239 | .0001 |
| Mean (SD) | 31.08 (9.52) | 23.78 (6.48) | |
| Median (IQR) | 30 (24, 35) | 23 (19, 27) | |
| Ethnic group | N = 30 | N = 239 | .566 |
| Kikuyu | 3 (10.0%) | 42 (17.6%) | |
| Kalenjin | 10 (33.3%) | 91 (38.1%) | |
| Luhya | 11 (36.7%) | 56 (23.4%) | |
| Luo | 5 (16.7%) | 36 (15.1%) | |
| Other | 1 (3.3%) | 14 (5.9%) | |
Bold indicates a statistically significant difference.
Abbreviations: ARVs, antiretroviral medications; IQR, interquartile range; PCP, Pneumocystis jirovecii; SD, standard deviation; TB, tuberculosis; WHO, World Health Organization.
Rates of Disclosure
The overall disclosure rate, based on either the caregiver or child reporting that the child knew they were infected with HIV, was 11.1 % (N = 270). Based on the caregivers' reports, the disclosure rate was 10.2% (N = 266.) Based on the children's self-reports, the disclosure rate was 7.4% (N = 270). For 10 participants, the caregiver stated that the child knew their status, but the child answered that they did not know. One child reported knowing their status even though the caregiver reported the child did not know their status. The proportion of children knowing their status increased with age: 4.2% (2/48) of 6-year-olds, 0% (0/44) of 7-year-olds, 4.0% (1/25) of 8-year-olds, 5.9% (2/34) of 9-year-olds, 10.7% (3/28) of 10-year-olds, 3.9% (1/26) of 11-year-olds, 13.6% (3/22) of 12-year-olds, 39.3% (10/28) of 13-year-olds, and 46.7% (7/15) of 14-year-olds knew their status. (The question of who disclosed to a child was asked to only nine of the children—caregivers informed six of the children, clinicians led disclosure for two children, and one learned their HIV status by reading the information from their medical chart.
Table 2.
Caregiver Reports of Stigma, Depression Symptoms, and Adherence Issues Among Children
| Variable | Child's Disclosure Status |
P Value | |
|---|---|---|---|
| Disclosed | Not Disclosed | ||
| Teased by other children | N = 28 | N = 237a | 1.000 |
| Yes | 0 (0%) | 1 (0.4%) | |
| Been rejected by friends or family | N = 28 | N = 237b | 1.000 |
| Yes | 0 (0%) | 1 (0.4%) | |
| Other children avoid | N = 28 | N = 237c | 1.000 |
| Yes | 0 (0%) | 3 (1.3%) | |
| Has little interest or pleasure in activities | N = 28 | N = 238 | .490 |
| Yes | 1 (3.6%) | 5 (2.1%) | |
| Feeling down or depressed | N = 28 | N = 238b | .638 |
| Yes | 1 (3.6%) | 6 (2.5%) | |
| Asks questions about why taking meds | N = 28 | N = 236b | .743 |
| Yes | 8 (28.6%) | 80 (33.9%) | |
| Child refuses medicine | N = 28 | N = 238c | 1.000 |
| Yes | 1 (3.6%) | 13 (5.5%) | |
| Problems giving child meds since doesn't know status | N = 27 | N = 238 | .618 |
| Yes | 0 (0%) | 12 (5.0%) | |
| Problems taking medicines on time | N = 28 | N = 237 | 1.000 |
| Yes | 1 (3.6%) | 6 (6.8%) | |
| Explanation on coming to clinic for nondisclosed to children | N = 0 | N = 217 | |
| Has another illness | 127 (58.5%) | ||
| We do not talk about it | 58 (26.7%) | ||
| The clinic/meds are to keep them healthy | 32 (14.7%) | ||
The remainder of the responses were “No” with the following number of subjects answering “Don't Know” for marked questions: (a) 4 subjects, (b) 2 subjects, and (c) 1 subject.
Variables Shaping Disclosure Experience
In bivariate analysis, the only factor that was significantly associated with disclosure was age (P < .0001) (Table 1). Caregiver-reported psychological and social variables for the children were reported at similar levels between disclosed and nondisclosed participants (Table 2). Most caregivers reported good adherence to ART, with 95.2% reporting perfect 30-day adherence and 60.8% reporting composite good adherence. In univariate analyses, there were no differences in adherence between the disclosed and nondisclosed groups. In multiple logistic regression, only age (by year of increased age) was significantly associated with disclosure status (odds ratio 1.67, 95% confidence interval 1.36–2.05); however, the model did not fit well due to the small number of disclosed individuals.
Disclosed children did not report any significant differences in missing medications, refusing medications, not wanting to take the medicines in front of other people, problems taking medicines because they did not know why they were taking them, or with taking the medicines on time compared to nondisclosed children. Some nondisclosed children (58.5%) were told they come to the clinic because of other illnesses, including pneumonia, cough, tuberculosis, malaria, and lymphadenopathy. Among the children who knew their HIV status, 84.2% reported asking questions about why they were taking medicines before they knew their HIV status, and 40.9% reported that they still asked questions. None of the children who knew their HIV status reported symptoms of depression or experiences of stigma.
DISCUSSION
Disclosure is a necessary component of the transition from childhood to adulthood for HIV-infected children, yet resource-limited settings may not be prepared for the process of telling HIV-infected children and adolescents that they have HIV. This analysis of a large, representative sample of HIV-infected children and young adolescents in Kenya demonstrates that few children in this setting have been told they have HIV. These findings are similar to smaller assessments from elsewhere in East Africa, and they highlight the need to identify effective strategies to guide families through the process of HIV disclosure to children [8].
Low rates of disclosure are troublesome for a number of reasons. In the Kenyan healthcare system, adolescents typically move to adult care systems by the age of 15, and patients in adult clinics are assumed to know their status. Abrupt and unplanned disclosure upon entrance into the adult clinic is far from the gradual, age-appropriate disclosure process that is highly recommended. Another important concern as youth enter adolescence is the growing possibility of sexual debut. Disclosure before an adolescent is sexually active may enhance the use of appropriate measures to prevent HIV transmission or pregnancy [9, 19].
This evaluation demonstrates that the majority of children have questions about why they are taking medicines and that these questions are not honestly answered. This lack of truthful answers may ultimately impact adherence or a child's mental or emotional health. In other resource-limited settings, parents and guardians feared children's questions and saw them as a motivation to disclose to the children [8–11, 16, 18–21]. In our sample, asking questions was not linked to subsequent disclosure; however, our sample of disclosed children was small. A gradual process in which accurate information is shared with children and their questions are answered in a developmentally appropriate manner is recommended [4–7, 27]. How this process is shaped by the social and cultural context, including whether or not the child is orphaned and cultural beliefs about emerging adulthood, should be evaluated.
While many parents worry that disclosure will negatively impact a child's mental and emotional health [9, 10, 16, 17, 19, 25–27], few studies in resource-limited settings have examined whether these fears are founded. In a univariate analysis of 127 children in Zambia, nondisclosed children were more than twice as likely to experience concerning levels of emotional difficulty compared to disclosed children [30]. Our study included the PHQ-2 depression screening questions, and none of the children answered positively to these screening questions. Seven caregivers reported positive answers for the children on the PHQ-2, but there was no significant difference associated with disclosure status [5]. While the PHQ-2 has not been validated for children or adolescents in Kenya, it has been validated for adults in this setting and among adolescents in other settings [31–33]. The PHQ-2 was used as a general assessment of mental health, because no tool has been validated in this population for clinical depression screening. Despite caregivers' common fears of stigma and discrimination [10, 11, 17, 21, 22, 24], we could not find other studies that measured stigma, social isolation, or discrimination experiences after disclosure. Our study thus provides a first look at whether those fears are supported. Only a small percentage of the parents or caregivers reported that the child had experienced any instances of stigma such as being teased, rejected, or avoided by others, and none of the disclosed children described any experiences of stigma. Since the study was designed to determine prevalence of disclosure, the sample size may not have had the power to reflect differences in depression symptoms or experienced stigma between the groups. Nonetheless, these data from a relatively large sample present no indication that children who know their status have more social or mental health issues.
As a counterpoint to their fears about stigma and a negative mental health impact, many caregivers and healthcare providers believe disclosure will help adherence to ART and to clinical care. One sub-Saharan African setting found better ART adherence, as measured by electronic dose-timing, among children who know their HIV status [34]. Our study did not find a significant association; however, the 30-day caregiver-report or self-report may overestimate adherence [35]. We did find increased reports of problems with adherence with more broad questioning than with the standard 30-day self-report measure, but this did not vary significantly by disclosure status. Incorporating more accurate measures of nonadherence, including questions assessing medication-taking more broadly, objective measures such as electronic dose-timing recordings, and longitudinal measures, may better depict how disclosure and adherence are related.
This study does have some limitations that merit consideration. The study occurred at a single clinic within the AMPATH care system, which may not fully represent the AMPATH catchment area consisting of 2 million people in western Kenya or other resource-limited settings in sub-Saharan Africa. The clinic at MTRH in Eldoret is in an urban environment and may have different clinical procedures than the more rural clinics. Nonetheless, compared to the existing literature on pediatric disclosure in sub-Saharan Africa, this was a large clinical sample, and the Eldoret clinic does have good ethnic diversity. While findings from Kenya may not be generalizable to the rest of the world, they may be more representative for sub-Saharan Africa than many of the other existing studies [13, 36–40]. This study focuses on a limited age range of 6–14 years, with no information for youth aged 15 and older. However, since pediatric clinics in Kenya see patients up to the age of 14, this study was grounded within the local care system and practices for the pediatric population. The disclosure questionnaires were intentionally kept short for ease of use and efficiency in the clinical visit. Thus, we do not have data on some potentially relevant variables, including other mental health symptoms or sexual activity. Within these confines, we did assess characteristics such as experiences of stigma, which have not been measured previously even though qualitative findings suggest their potential importance [8, 9, 11, 15, 18–20]. With this low rate of disclosure, a number of youth may have transitioned to the adult clinic without knowledge of their disease. Future work evaluating their virologic and immunologic parameters, as well as health behaviors and mental health, could provide important information for caring for this population.
Because this study showed a low rate of disclosure at the MTRH AMPATH clinic, AMPATH instituted a disclosure standard operating procedure (SOP) in order to improve the disclosure process. The disclosure SOP initiates a gradual disclosure process for all pediatric patients at the age of 10 years. Implementation of this SOP, involving clinical officers, nurses, physicians, and staff members working in partnership with families, is hoped to improve the rate of disclosure in 10–14-year-olds throughout the AMPATH clinics to nearly 100%. The disclosure SOP follows recommendations for a process of disclosure that assesses the child's age, psychological maturity, and emotional and cognitive capabilities [4–6, 19], and helps patients learn about their HIV status in a controlled and positive environment with the involvement of their families and clinicians. We would recommend that other settings consider how to best implement disclosure protocols and support for the transition to adulthood within their care systems.
In conclusion, we found low rates of informing children about their HIV status in a large referral clinic in western Kenya, with some increase in disclosure as children entered adolescence. Disclosure was not associated with negative effects on emotional health or experienced stigma, although further assessment of these important issues is needed. Guiding families through a gradual, developmentally and culturally appropriate disclosure process should be a key facet of long-term pediatric HIV management.
Acknowledgments
The authors thank the clinical officers and nurses who guide the disclosure processes at the AMPATH clinics, as well as the many families under our care. We also thank Joel Hartsell for his work in implementing this project.
Disclaimer . The views expressed in this article are those of the authors and do not necessarily represent the view of the Indiana University School of Medicine or the Moi University School of Medicine. The authors have no conflicts of interest to disclose.
Financial support. R. C. V. is supported by a grant from the National Institute for Mental Health (1K23MH087225-01.) This work was also supported in part by a grant to the USAID-AMPATH Partnership from the United States Agency for International Development as part of the President's Emergency Plan for AIDS Relief.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Contributor Information
Matthew L. Turissini, Children's Health Services Research, Department of Pediatrics, Indiana University School of Medicine, Indianapolis United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership.
Winstone M. Nyandiko, United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership Department of Child Health and Paediatrics, School of Medicine, College of Health Sciences, Moi University, Eldoret, Kenya.
Samuel O. Ayaya, United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership Department of Child Health and Paediatrics, School of Medicine, College of Health Sciences, Moi University, Eldoret, Kenya.
Irene Marete, United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership; Department of Child Health and Paediatrics, School of Medicine, College of Health Sciences, Moi University, Eldoret, Kenya.
Ann Mwangi, United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership; Department of Child Health and Paediatrics, School of Medicine, College of Health Sciences, Moi University, Eldoret, Kenya.
Victor Chemboi, United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership.
Lucy Warui, United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership.
Rachel C. Vreeman, Children's Health Services Research, Department of Pediatrics, Indiana University School of Medicine, Indianapolis United States Agency for International Development (USAID) Academic Model Providing Access to Healthcare (AMPATH) Partnership.
References
- 1.Geneva, Switzerland: World Health Organization; 2010. Antiretroviral Therapy for HIV Infection in Infants and Children: Towards Universal Access. [PubMed] [Google Scholar]
- 2. UNAIDS. 2010 Report on the Global AIDS Epidemic. 2010;23, 26 The Joint United Nations Programme on HIV/AIDS (UNAIDS) [Google Scholar]
- 3. Lallemant M Chang S et al. Pediatric HIV—a neglected disease? N Engl J Med. 2011;365:581–3. doi: 10.1056/NEJMp1107275. [DOI] [PubMed] [Google Scholar]
- 4. Wiener L et al. Disclosure of an HIV diagnosis to children: history, current research, and future directions. J Dev Behav Pediatr. 2007;28:155–66. doi: 10.1097/01.DBP.0000267570.87564.cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Disclosure of illness status to children and adolescents with HIV infection. American Academy of Pediatrics Committee on Pediatrics AIDS. Pediatrics. 1999;103:164–6. doi: 10.1542/peds.103.1.164. [DOI] [PubMed] [Google Scholar]
- 6. Gerson AC et al. Disclosure of HIV diagnosis to children: when, where, why, and how. J Pediatr Health Care. 2001;15:161–7. doi: 10.1067/mph.2001.114835. [DOI] [PubMed] [Google Scholar]
- 7. Lesch A et al. Paediatric HIV/AIDS disclosure: towards a developmental and process-oriented approach. AIDS Care. 2007;19:811–6. doi: 10.1080/09540120601129301. [DOI] [PubMed] [Google Scholar]
- 8. Bikaako-Kajura W et al. Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS Behav. 2006;10((4 suppl)):S85–93. doi: 10.1007/s10461-006-9141-3. [DOI] [PubMed] [Google Scholar]
- 9. Kallem S et al. Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana. AIDS Behav. 2011;15:1121–7. doi: 10.1007/s10461-010-9741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Oberdorfer P et al. Disclosure of HIV/AIDS diagnosis to HIV-infected children in Thailand. J Paediatr Child Health. 2006;42:283–8. doi: 10.1111/j.1440-1754.2006.00855.x. [DOI] [PubMed] [Google Scholar]
- 11. Punpanich W et al. Understanding the psychosocial needs of HIV-infected children and families: a qualitative study. J Med Assoc Thail. 2008;91((suppl 3)):S76–84. [PMC free article] [PubMed] [Google Scholar]
- 12. Moodley K Myer L Paediatric HIV disclosure in South Africa—caregivers' perspectives on discussing HIV with infected children. S Afr Med J. 2006;96:201–4. [PubMed] [Google Scholar]
- 13. Arun S et al. Disclosure of the HIV infection status in children. Indian J Pediatr. 2009;76:805–8. doi: 10.1007/s12098-009-0177-z. [DOI] [PubMed] [Google Scholar]
- 14. Abebe W Teferra S Disclosure of diagnosis by parents and caregivers to children infected with HIV: prevalence associated factors and perceived barriers in Addis Ababa, Ethiopia. AIDS Care. 2012 doi: 10.1080/09540121.2012.656565. February 9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15. Biadgilign S et al. Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: A qualitative study. SAHARA J J Social Aspects HIV/AIDS Res Alliance SAHARA Hum Sci Res Council. 2009;6:148–54. doi: 10.1080/17290376.2009.9724943. [DOI] [PubMed] [Google Scholar]
- 16. Blasini I et al. Disclosure model for pediatric patients living with HIV in Puerto Rico: design, implementation, and evaluation. J Dev Behav Pediatr. 2004;25:181–9. doi: 10.1097/00004703-200406000-00007. [DOI] [PubMed] [Google Scholar]
- 17. Corneli A et al. The role of disclosure in relation to assent to participate in HIV-related research among HIV-infected youth: a formative study. J Int AIDS Soc. 2009;12:17. doi: 10.1186/1758-2652-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vaz L et al. The process of HIV status disclosure to HIV-positive youth in Kinshasa, Democratic Republic of the Congo. AIDS Care. 2008;20:842–52. doi: 10.1080/09540120701742276. [DOI] [PubMed] [Google Scholar]
- 19. Vaz L et al. Telling children they have HIV: lessons learned from findings of a qualitative study in sub-Saharan Africa. AIDS Patient Care STDS. 2010;24:247–56. doi: 10.1089/apc.2009.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fetzer BC Mupenda B Lusiama J Kitetele F Golin C Behets F Barriers to and facilitators of adherence to pediatric antiretroviral therapy in a sub-Saharan setting: insights from a qualitative study. AIDS Patient Care STDS. 2011;25:611–21. doi: 10.1089/apc.2011.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vreeman RC et al. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDs. 2010;24:639–49. doi: 10.1089/apc.2010.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hejoaka F Care and secrecy: being a mother of children living with HIV in Burkina Faso. Soc Sci Med. 2009;69:869–76. doi: 10.1016/j.socscimed.2009.05.041. [DOI] [PubMed] [Google Scholar]
- 23. Michaud PA et al. To say or not to say: a qualitative study on the disclosure of their condition by human immunodeficiency virus-positive adolescents. J Adolesc Health. 2009;44:356–62. doi: 10.1016/j.jadohealth.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 24. Kouyoumdjian FG Meyers T Mtshizana S Barriers to disclosure to children with HIV. J Trop Pediatr. 2005;51:285–7. doi: 10.1093/tropej/fmi014. [DOI] [PubMed] [Google Scholar]
- 25. Yeap AD et al. Factors influencing uptake of HIV care and treatment among children in South Africa—a qualitative study of caregivers and clinic staff. AIDS Care. 2010;22:1101–7. doi: 10.1080/09540121003602218. [DOI] [PubMed] [Google Scholar]
- 26. Vreeman RC et al. Caregivers' perceptions of the impact of disclosure of pediatric HIV status on antiretroviral therapy adherence in a resource-limited setting. AIDS Patient Care STDs. 2010;24:639–49. doi: 10.1089/apc.2010.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Abadia-Barrero CE Larusso MD The disclosure model versus a developmental illness experience model for children and adolescents living with HIV/AIDS in Sao Paulo, Brazil. AIDS Patient Care STDs. 2006;20:36–43. doi: 10.1089/apc.2006.20.36. [DOI] [PubMed] [Google Scholar]
- 28. Einterz RM Kimaiyo S Mengech HN et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007;82:812–8. doi: 10.1097/ACM.0b013e3180cc29f1. [DOI] [PubMed] [Google Scholar]
- 29. Tierney WM Rotich JK Hannan TJ et al. The AMPATH medical record system: creating, implementing, and sustaining an electronic medical record system to support HIV/AIDS care in western Kenya. Medinfo. 2007;12(pt 1):372–6. [PubMed] [Google Scholar]
- 30. Menon A et al. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. J Acquir Immune Defic Syndr. 2007;26:349–54. doi: 10.1097/QAI.0b013e3181565df0. [DOI] [PubMed] [Google Scholar]
- 31. Monahan PO Shacham E Reece M Kroenke K Ong'or WO Omollo O Yebei VN Ojwang C Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J Gen Intern Med. 2009;24:189–97. doi: 10.1007/s11606-008-0846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Richardson LP et al. Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. 2010;125:e1097–1103. doi: 10.1542/peds.2009-2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Borner I Braunstein JW St. Victor R Pollack J Evaluation of a 2-question screening tool for detecting depression in adolescents in primary care. Clin Pediatr. 2010;49:947. doi: 10.1177/0009922810370203. [DOI] [PubMed] [Google Scholar]
- 34. Haberer JE et al. Excellent adherence to antiretrovirals in HIV+ Zambian children is compromised by disrupted routine, HIV nondisclosure, and paradoxical income effects. PLoS One. 2011;6:e18505. doi: 10.1371/journal.pone.0018505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vreeman RC Wiehe SE et al. A systematic review of pediatric adherence to antiretroviral therapy in low- and middle-income countries. Pediatr Infect Dis J. 2008;27:686–91. doi: 10.1097/INF.0b013e31816dd325. [DOI] [PubMed] [Google Scholar]
- 36. Wiener LS Battles HB Untangling the web: a close look at diagnosis disclosure among HIV-infected adolescents. J Adolesc Health. 2006;38:307–9. doi: 10.1016/j.jadohealth.2005.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bachanas PJ et al. Predictors of psychological adjustment in school-age children infected with HIV. J Pediatr Psychol. 2001;26:343–52. doi: 10.1093/jpepsy/26.6.343. [DOI] [PubMed] [Google Scholar]
- 38. Wiener LS et al. Factors associated with disclosure of diagnosis to children with HIV/AIDS. Pediatr AIDS HIV Infect. 1996;7:310–24. [PubMed] [Google Scholar]
- 39. Cohen J Reddington C Jacobs D Meade R Picard D Singleton K et al. School-related issues among HIV-infected children. Pediatrics. 1997;100:E8. doi: 10.1542/peds.100.1.e8. [DOI] [PubMed] [Google Scholar]
- 40. Funck-Brentano I Costagliola D Seibel N Straub E Tardieu M Blanche S Patterns of disclosure and perceptions of the human immunodeficiency virus in infected elementary school-age children. Arch Pediatr Adolesc Med. 1997;151:978–85. doi: 10.1001/archpedi.1997.02170470012002. [DOI] [PubMed] [Google Scholar]