Abstract
Background
Suprascapular nerve decompression (SSND) remains a controversial procedure. In 2018, Momaya et al published the first systematic review of SSND noting satisfactory outcomes with low rates of complications; however, numerous studies published since have noted no benefit in routinely adding SSND to other arthroscopic surgeries, contributing to existing contention regarding the procedure. The purpose of this study is to provide an updated assessment of outcomes after SSND.
Methods
To conduct this updated systematic review, a search of PubMed (MEDLINE) for relevant studies published prior to January 21, 2023 was conducted. Outcomes including patient-reported clinical outcomes, return to sport, preoperative and postoperative electrodiagnostic testing, and adverse events were collected and pooled for assessment. Studies were eligible for inclusion if they met Momaya et al’s inclusion criteria and/or reported outcomes following SSND at either the suprascapular notch or spinoglenoid notch.
Results
In total, 730 patients from 33 studies were eligible for inclusion. All patient-reported outcome measure scores including American Shoulder Elbow Surgeon Standardized Shoulder Assessment; Constant-Murley score; Disabilities of the Arm, Shoulder, and Hand; Subjective Shoulder Value; University of California–Los Angeles shoulder; and visual analog scale pain scores improved significantly postoperatively, with improvements ranging from 53.5% to 102.6% of preoperative values. Ultimately, 98% (n = 90/92) of patients returned to sport or military duty and 96% of these patients returned at their previous level of activity (n = 48/50) without heterogeneity among rates between studies (P = .176, P = .238, respectively). Preoperative electrodiagnostic testing was conducted in 93% of patients, and 90% had associated abnormal findings. Continued symptoms were noted among 12% of patients (n = 39/322) with significantly different rates observed between studies. Complications from operative management not limited to SSND occurred in 11% of patients (n = 64/576) and reoperations occurred in 3.3% of patients (n = 15/455).
Conclusion
Suprascapular neuropathy treated with SSND significantly improves patient-reported outcomes and is noninferior to similar procedures without SSND. Appropriate clinical diagnosis of suprascapular neuropathy is required as opposed to a routine adjunct procedure with other arthroscopic shoulder surgery. Ultimately, SSND is associated with high rates of return to sport and relatively low rates of adverse events; however, the risk of continued symptoms and electrodiagnostic test-related complications is an important point on preoperative counseling.
Keywords: Rotator cuff, Shoulder arthroscopy, Suprascapular nerve, Suprascapular neuropathy, Spinoglenoid notch, Suprascapular notch
Suprascapular neuropathy was first described nearly a century ago5,25,26,50 and, as advancements in diagnostic modalities evolve, has been increasingly recognized as an underlying cause of pain and shoulder dysfunction. Compression of the suprascapular nerve (SSN) can occur secondary to a variety of etiologies including, but not limited to, repetitive overhead activities,6,29,34,41 space occupying cysts (sometimes associated with an adjacent superior labral tear),19,34,38,54 dysmorphic anatomy,4,15,51 and retracted rotator cuff tears2,12,34,44 and leads to posterior shoulder pain with supraspinatus and/or infraspinatus dysfunction. Chronic injuries can also lead to muscle wasting with underlying fatty infiltration on magnetic resonance imaging. Collectively, the patient’s physical examination, magnetic resonance imaging, and electromyography7,37 findings can facilitate the diagnosis of suprascapular neuropathy. Athletes, especially those participating in overhead sports, are at an increased risk of developing suprascapular neuropathy, with spinoglenoid notch (SGN) compression more common than SSN compression.9,48
The first line of treatment for suprascapular neuropathy involves an initial trial of nonoperative management; however, surgical decompression via suprascapular nerve decompression (SSND) may be indicated in patients with space-occupying lesions or compression from concomitant extrinsic pathologies such as a large rotator cuff tear with retraction.6,35,48 Recently, interest in SSND has skyrocketed due to conflicting findings in emerging literature: while a systematic review by Momaya et al37 demonstrated significant improvement in patient-reported outcome measures (PROMs) and a 92% return to sport (RTS) rate following SSND among 275 patients, recent studies on the role of SSND as an adjunct to rotator cuff repair (RCR) have shown no additional benefit to routine SSND21,32,56 with a prospective, randomized observational trial by Gerber et al21 reporting early termination due to electromyographic complications in 3 patients coupled with an absence of clinical benefit associated with SSND.
The recent revitalization of interest in the role of SSND both independently and as an adjunct to RCR has warranted reassessment after the 2018 systematic review by Momaya et al37 given that the number of patients eligible for inclusion has nearly tripled. Subsequently, this study seeks to provide an updated systematic review with the primary objective to determine the PROMs and RTS associated with SSND. The secondary objectives were to characterize current utilization of preoperative electrodiagnostic testing (EDT) as well as rates of adverse events following SSND and concomitant procedures.
Materials and methods
Search strategy and study selection
Systematic review and meta-analysis were performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The authors used the search algorithm “suprascapular OR spinoglenoid OR (shoulder and “entrapment neuropathy”) OR (shoulder and “ganglion cyst”) OR (shoulder and “transverse scapular ligament”) based on the search used by Momaya et al37 to search the PubMed (MEDLINE) database for all articles published between September 2016 and January 2023 to prevent duplication of articles searched by Momaya et al.37 Two investigators (A.B.S. and M.E.W.) independently screened abstracts and performed full-text review. Data collection was performed by 3 independent investigators (A.B.S., C.T., and R.A.) with disputes between data collection discussed and by a separate independent investigator (A.B.S. or M.E.W.).
Inclusion criteria
To provide a direct and effective update to the systematic review by Momaya et al,37 the authors elected to maintain identical inclusion criteria, specifically including studies that reported outcomes following SSND at the SSN or SGN (Table I). To be included, studies had to report at least 1 outcome in the jurisdiction of PROMs, rates of RTS, or EDT results. Articles that did not specify the relevant outcome measures as well as commentaries, editorials, reviews, technical guides, case reports with less than 3 patients, and studies published in languages other than English were excluded.
Table I.
Inclusion criteria adjusted from Momaya et al.37
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
EDT, electrodiagnostic testing; SSN, suprascapular notch; SSND, suprascapular nerve decompression; SGN, spinoglenoid notch.
Data analysis and data extraction
Data regarding patient demographics, PROMs, RTS and/or return to military duty, EDT results, and adverse events were collected and pooled for analysis. PROMs included the following: American Shoulder Elbow Surgeons Standardized Shoulder Assessment (ASES) score; Constant-Murley score; Disabilities of the Arm, Shoulder, and Hand (DASH) score; Subjective Shoulder Value (SSV) score; University of California–Los Angeles shoulder score; and the visual analog scale (VAS) pain score. Concomitant procedures were collected based on procedure-specific details specified in the study methodology and were classified as RCR, labral or superior labrum from anterior to posterior lesion repair, subacromial bursectomy/decompression, labral or rotator cuff débridement, acromioplasty, distal clavicle excision, or other. Methodological Index for Non-Randomized Studies (MINORS) criteria were used to assess study quality, although case reports with less than 5 patients and randomized studies did not undergo MINORS criteria calculation given variation in reporting of methodology not thoroughly assessed by the criterion.47
Statistical analysis
Independent 2-tailed t-tests were used to evaluate for significant changes based on calculations of weighted means with standard deviations and/or confidence intervals. Chi-squared tests were used to determine significant differences between categorical variables. Multivariate linear regressions were used to assess the impact of concomitant procedures on outcomes following SSND. Statistical significance was set at α less than or equal to 0.05.
Results
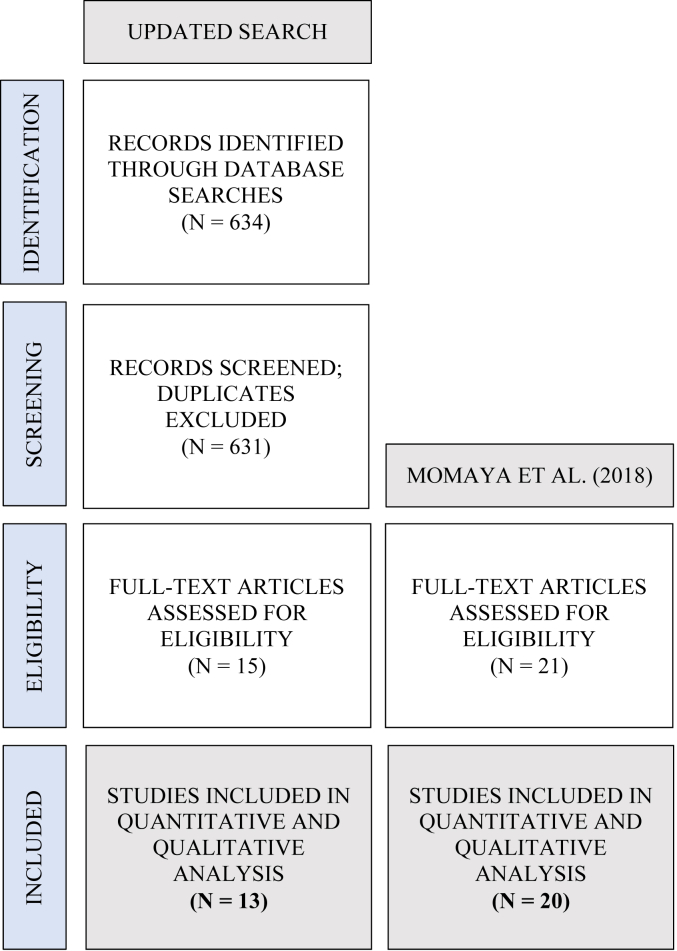
To complete the updated search, an additional 634 abstracts were screened, 15 full-text manuscripts reviewed, and ultimately 13 studies with level I-IV evidence deemed eligible for inclusion (Fig. 1). Quantitative and qualitative data were extracted from the additional 13 studies and combined with data extracted from the 20 articles included in prior systematic review,37 totaling data extraction from 33 studies published between 1992 and 2021 (Table II).1,3,8,10,12, 13, 14,16, 17, 18,20, 21, 22, 23, 24,28,30,31,33,38, 39, 40,42, 43, 44,46,52,54,55,57 Following data extraction, 488 patients from the updated search were pooled with 242 from the Momaya article,37 resulting in a total of 730 patients.
Figure 1.
PRISMA flow diagram.
Table II.
Study characteristics.
| Study | Journal | Level of evidence | Location of decompression | Technique | Shoulders (n) | Safety concerns warranted termination | MINORS score |
|---|---|---|---|---|---|---|---|
| Cano-Martínez (2021)8 | Rev Esp Cir Ortop Traumatol | IV | SSN | Arthroscopic | 75 | N | 11/16 |
| Nolte (2021)38 | Arthroscopy | IV | SSN/SGN | Arthroscopic | 42 | N | 11/16 |
| Sachinis (2021)42 | Am J Sports Med | I | SSN | Arthroscopic | 37 | N | N/A∗ |
| Yang (2021)57 | BMC Musculoskelet Disord | III | SGN | Arthroscopic | 20 | N | 19/24 |
| Davis (2020)13 | J Orthop | IV | SSN | Arthroscopic | 111 | N | 13/16 |
| Gerber (2020)21 | JSES | II | SSN | Arthroscopic | 9 | Y | N/A∗ |
| Katsuura (2020)24 | Clin Med Insights Arthritis Musculoskelet Disord | III | SSN | Arthroscopic | 100 | N | 15/24 |
| Feinberg (2019)17 | Muscle Nerve | II | SSN/SGN | Arthroscopic | N | 11/16 | |
| Yamakado (2019)55 | Int Orthop | III | SSN | Arthroscopic | 31 | N | 21/24 |
| Perry (2018)39 | Mil Med | IV | SSN/SGN | Arthroscopic | 7 | N | 11/16 |
| Tsikouris (2018)52 | Arthroscopy | III | SSN | Arthroscopic | 35 | N | 17/24 |
| Kim (2017)25 | Arthroscopy | IV | SGN | Arthroscopic | 21 | N | 11/16 |
| Hashiguchi (2016)23 | SICOT J | IV | SGN | Arthroscopic | 6 | N | 9/16 |
| Savoie (2016)44 | Orthop J Sports Med | II | SSN | Arthroscopic | 22 | N | 17/24 |
| Bilsel (2014)5 | Knee Surg Sports Traumatol Arthrosc | III | SGN | Arthroscopic | 16 | N | 19/24 |
| Leclere (2014)30 | Arthroscopy | IV | SSN/SGN | Arthroscopic | 4 | N | N/A† |
| Arriaza (2013)3 | Am J Sports Med | IV | SSN | Arthroscopic | 4 | N | N/A† |
| Mall (2013)33 | J Shoulder Elbow Surg | IV | SGN | Open | 29 | N | 11/16 |
| Kim (2012)26 | J Shoulder Elbow Surg | II | SGN | Arthroscopic | 14 | N | 21/24 |
| Garcia Jr. (2011)20 | Rev Bras Ortop | IV | SSN | Arthroscopic | 10 | N | 13/16 |
| Pillai (2011)40 | Clin Orthop Relat Res | IV | SGN | Arthroscopic | 6 | N | 16/24 |
| Shah (2011)46 | J Shoulder Elbow Surg | IV | SSN/SGN | Arthroscopic | 24 | N | 10/16 |
| Costouros (2007)12 | Arthroscopy | IV | SSN | Arthroscopic | 6 | N | 13/16 |
| Lafosse (2007)28 | Arthroscopy | IV | SSN | Arthroscopic | 10 | N | 13/16 |
| Abboud (2006)1 | Clin Orthop Relat Res | III | SGN | Arthroscopic | 16 | N | 10/16 |
| Westerheide (2006)54 | Arthroscopy | IV | SGN | Arthroscopic | 14 | N | 11/16 |
| Dramis (2005)14 | Acta Orthop Belg | IV | SSN | Open | 4 | N | N/A† |
| Lichtenberg (2004)31 | Knee Surg Sports Traumatol Arthrosc | IV | SGN | Arthroscopic | 8 | N | 10/16 |
| Chen (2003)10 | Arthroscopy | IV | SGN | Arthroscopic | 3 | N | N/A† |
| Fabre (1999)16 | J Bone Joint Surg Br | IV | SSN/SGN | Open | 35 | N | 9/16 |
| Ferretti (1998)18 | Am J Sports Med | IV | SGN | Open | 3 | N | N/A† |
| Sandow (1998)43 | J Shoulder Elbow Surg | IV | SSN/SGN | Open | 5 | N | N/A† |
| Hama (1992)22 | J Shoulder Elbow Surg | IV | SSN/SGN | Open | 3 | N | N/A† |
SSN, suprascapular notch; SGN, spinoglenoid notch.
Randomized study.
Case report with 3-5 studies.
A majority of patients underwent arthroscopic intervention (n = 651, 89.2%) versus open intervention (n = 79, 10.8%). Thirteen studies were specific to SSND performed at the SSN (n = 454 shoulders), while 12 were specific to SSND performed at the SGN (n = 156 shoulders). The remaining 8 studies (n = 128 shoulders) involved a combination of SSND at either the SSN and/or the SGN. The most frequently performed concomitant procedures included RCR (n = 126/638, 19.7%), labral/superior labrum from anterior to posterior lesion repair (n = 98/638, 15.4%), subacromial bursectomy/decompression (n = 49/638, 7.7%), and biceps tenotomy/tenodesis (n = 45/638, 7.1%). Specific concomitant procedures are presented in Table III.
Table III.
Concomitant procedures.
| Author | Rotator cuff repair |
Labral/SLAP lesion repair |
Subacromial bursectomy/decompression |
Biceps tenodesis/Tenotomy |
Other |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | Description | |
| Cano-Martínez (2021)8 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Nolte (2021)38 | 0 | 0.0% | 0 | 0.0% | 15 | 35.7% | 8 | 19.0% | 8 | Distal clavicle excision (3), rotator cuff healing response (1), os acromial fixation (1), hardware removal (1), axillary nerve decompression (1), musculocutaneous nerve decompression (1) |
| Sachinis (2021)42 | 18 | 48.6% | 0 | 0.0% | 0 | 0.0% | 18 | 48.6% | 18 | Acromioplasty (18) |
| Yang (2021)57 | 10 | 50.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Davis (2020)13 | 27 | 24.3% | 5 | 4.5% | 0 | 0.0% | 23 | 20.7% | 0 | - |
| Gerber (2020)21 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 14 | 74.7% | 18 | Acromioplasty (14), acromioclavicular joint resection (2), calcium deposit decompression (1), humeral head microfracturing (1) |
| Katsuura (2020)24 | ||||||||||
| Feinberg (2019)17 | 0 | 0.0% | 8 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Yamakado (2019)55 | 31 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Perry (2018)39 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 7 | 100.0% | 0 | - |
| Tsikouris (2018)52 | 27 | 77.1% | 16 | 45.7% | 31 | 88.6% | 0 | 0.0% | 0 | - |
| Kim (2017)25 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Hashiguchi (2016)23 | 2 | 33.3% | 6 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Savoie (2016)44 | 22 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Bilsel (2014)5 | 0 | 0.0% | 16 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Leclere (2014)30 | 0 | 0.0% | 0 | 0.0% | 2 | 50.0% | 0 | 0.0% | 0 | - |
| Arriaza (2013)3 | 0 | 0.0% | 0 | 0.0% | 4 | 100.0% | 0 | 0.0% | 0 | - |
| Mall (2013)33 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Kim (2012)26 | 0 | 0.0% | 14 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Garcia Jr. (2011)20 | 0 | 0.0% | 0 | 0.0% | 9 | 90.0% | 0 | 0.0% | 0 | - |
| Pillai (2011)40 | 0 | 0.0% | 6 | 100.0% | 1 | 16.7% | 0 | 0.0% | 0 | - |
| Shah (2011)46 | 0 | 0.0% | 3 | 12.5% | 0 | 0.0% | 1 | 4.2% | 2 | Capsular release (1), distal clavicle excision (1) |
| Costouros (2007)12 | 6 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 6 | Acromioplasty (6) |
| Lafosse (2007)28 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 3 | Distal clavicle excision (3) |
| Abboud (2006)1 | 0 | 0.0% | 9 | 56.3% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Westerheide (2006)54 | 0 | 0.0% | 7 | 50.0% | 2 | 14.3% | 0 | 0.0% | 1 | Distal clavicle excision (1) |
| Dramis (2005)14 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Lichtenberg (2004)31 | 0 | 0.0% | 5 | 62.5% | 0 | 0.0% | 0 | 0.0% | 2 | Capsular release (2) |
| Chen (2003)10 | 0 | 0.0% | 3 | 100.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Fabre (1999)16 | 1 | 2.9% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Ferretti (1998)18 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 1 | Shaved scapular spine (1) |
| Sandow (1998)43 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | - |
| Hama (1992)22 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 2 | Shaved scapular spine (2) |
| Total | 126 | 19.7% | 98 | 15.4% | 49 | 7.7% | 45 | 7.1% | 61 | - |
SLAP, superior labrum from anterior to posterior.
Patient-reported outcome measures (PROMs)
Significant postoperative improvements in PROMs were observed among all PROM scores with increases in ASES, Constant-Murley score, SSV, and University of California–Los Angeles scores with concurrent decreases in DASH and VAS scores (Table IV). Changes in preoperative to postoperative PROM scores ranged from 53.5% to 102.6% improvement. Multiple linear regression revealed no statistically significant effects of rates of associated RCR, labral repair, and biceps tenodesis/tenotomy on postoperative VAS scores (P = .583) with insufficient data available to test other PROM measures.
Table IV.
Patient-reported outcome measure (PROM) scores.
| Score | Mean (SD) | Included studies (patients), n | PROM change, points (95% CI) | PROM change, % | T-statistic | P value | |
|---|---|---|---|---|---|---|---|
| ASES | Preoperative | 47.5 (2.0) | 113 (6) | +25.4 (21.5-29.4) | +53.5% | +12.8 | <.001 |
| Postoperative | 72.9 (16.5) | 114 (6) | |||||
| Constant | Preoperative | 54.7 (18.0) | 208 (9) | +29.6 (27.1-32.2) | +54.1% | +22.8 | <.001 |
| Postoperative | 84.3 (6.9) | 222 (9) | |||||
| DASH | Preoperative | 67.8 (21.0) | 95 (3) | −50.3 (46.0-54.7) | −74.2% | −22.9 | <.001 |
| Postoperative | 17.5 (4.3) | 95 (3) | |||||
| SSV | Preoperative | 48.4 (12.0) | 58 (4) | +32.0 (27.3-36.6) | +64.8% | +13.6 | <.001 |
| Postoperative | 80.4 (13.3) | 58 (4) | |||||
| UCLA | Preoperative | 15.3 (4.6) | 131 (7) | +15.7 (14.8-16.6) | +102.6% | +35.2 | <.001 |
| Postoperative | 31.0 (2.3) | 131 (7) | |||||
| VAS | Preoperative | 6.8 (1.3) | 481 (15) | −4.2 (4.0-4.4) | −61.8% | −39.4 | <.001 |
| Postoperative | 2.6 (1.9) | 463 (13) | |||||
ASES, American Shoulder Elbow Surgeons Standardized Shoulder Assessment score; CI, confidence interval; Constant, Constant-Murley score; DASH, Disabilities of the Arm, Shoulder, and Hand score; SSV, Subjective Shoulder Value score; UCLA, University of California–Los Angeles shoulder score; VAS, visual analog scale pain score; PROM, patient-reported outcome measures; SD, standard deviation.
Return to sport
The vast majority of patients were able to RTS or military duty (n = 90/92, 98%, Table V) without significant differences observed among rates between studies (X2 [10, n = 92] = 2.658, P = .988). Furthermore, 96% (n = 48/50) were able to RTS or duty at their previous level of function without significant differences observed among rates between studies (X2 [8, n = 50] = 11.48, P = .176). The only specified athlete unable to RTS at previous level of play was a javelin thrower reported by Fabre et al.16 On a broader level, 94% (n = 123/131) of patients reported return to function to include sport participation, military duty, work, and activity following SSND without significant differences observed among rates between studies (X2 [11, n = 131] = 13.90, P = .238). Pooled specific sports and military occupations demonstrated the largest cohort to be volleyball players, at 25 athletes (Table VI).
Table V.
Return to sport/military duty by study.
| Author | Total population, athletes or Military, n | Rates of return to sport/Duty, % | Rates of return to sport/Duty at prior level, % | Specific sports activities |
|---|---|---|---|---|
| Perry (2018)39 | 7 | 100% | - | Navy sea, air, and land (2), Navy diver (1), AD Navy other (3), AD Marine (1) |
| Tsikouris (2018)52 | 35 | 97.1% | - | Volleyball (33), water polo (8), weightlifting (9), javelin throw (6) |
| Arriaza (2013)3 | 4 | 100% | 100% | Swimming (4) |
| Kim (2012)26 | 14 | 92.9% | 92.9% | Unspecified |
| Westerheide (2006)54 | 10 | 100% | 100% | Unspecified |
| Dramis (2005)14 | 4 | 100% | 100% | Volleyball (4) |
| Chen (2003)10 | 3 | 100% | 100% | Modern dance (1), softball (1), tennis (1) |
| Fabre (1999)16 | 4 | 100% | 75% | Javelin throw (1), swimmer (2), volleyball (1) |
| Ferretti (1998)18 | 3 | 100% | 100% | Volleyball (3) |
| Sandow (1998)43 | 5 | 100% | 100% | Volleyball (5) |
| Hama (1992)22 | 3 | 100% | 100% | Volleyball (2), tennis (1) |
| Total | 92 | 97.8% (n = 90/92) | 96% (n = 48/50) |
AD, Active duty.
Patients could report more than 1 sport.
Table VI.
Specific pooled sports and military occupations.
| Activity | N |
|---|---|
| Return to sport | 111 |
| Volleyball | 52 |
| Weightlifting | 9 |
| Water polo | 8 |
| Javelin throw | 7 |
| Swimming | 6 |
| Tennis | 3 |
| Dance | 1 |
| Softball | 1 |
| Unspecified | 24 |
| Military occupations | 7 |
| Active-duty Navy, other | 3 |
| Navy sea, air, and land | 2 |
| Navy diver | 1 |
| Active-duty Marine, other | 1 |
Electrodiagnostic testing (EDT)
In total, 25 studies reported preoperative EDT (n = 678, 92.9%), while only 13 reported postoperative EDT (n = 361, 49.5%). Of the pooled patients undergoing both preoperative and postoperative EDT irrespective of whether it was a study requirement, 90.0% (n = 190/211) were noted to have abnormal findings on preoperative EDT. Of these, 31.6% (n = 60/190) continued to have some degree of EDT abnormality on latest recorded follow-up in the study period.
Adverse events
Continued symptoms were noted among 12% of patients (n = 39/322) with significantly different rates observed between studies (X2 [12, 322] = 81.45, P < .001). In total, 29 patients presented with continued pain or discomfort, 5 with weakness or atrophy, 3 with EDT-related complications, and 2 with continued dissatisfaction with ultimate functional outcomes. The 3 patients with EDT-related complications reported by Gerber et al21 warranted premature termination of the study. Complications from operative management not limited to SSND occurred in 11% of patients (n = 64/576) and reoperations in 3.3% of patients (n = 15/455, Table VII).
Table VII.
Adverse events.
| N (%) | |
|---|---|
| Suprascapular nerve decompression complications | |
| Continued pain or discomfort | 29 (9.0%) |
| Muscle weakness or atrophy | 5 (1.6%) |
| Dissatisfaction with outcomes | 2 (<1%) |
| Associated procedure complications | |
| Rotator cuff retear | 16 (2.8%) |
| Sympathetic dystrophy | 14 (2.4%) |
| Worsened spine-mediated radicular pain | 11 (1.9%) |
| Repair failure | 4 (0.7%) |
| Shoulder arthritis | 4 (0.7%) |
| Superficial soft tissue infection | 4 (0.7%) |
| Healing failure | 3 (0.5%) |
| Adhesive capsulitis | 3 (0.5%) |
| Transverse skin thickening | 2 (0.3%) |
| Musculocutaneous nerve injury | 1 (0.2%) |
| Reoperation | |
| Revision of index procedure | 9 |
| Anatomic or reverse total shoulder arthroplasty | 3 |
| Hemiarthroplasty | 1 |
| Biceps tenodesis | 1 |
| Spine surgery for radicular pain | 1 |
The majority of complications and revisions were associated with concomitant procedures rather than isolated SSND (Table III). Similarly, multiple linear regression investigating the effect of concomitant RCR, labral repair, and biceps tenodesis/tenotomy on outcomes including RTS and persistent symptoms demonstrates statistically significant intercepts at 1.00 (0.98-1.02, P < .001) and 0.13 (confidence interval = 0.39-0.22, P = .007), respectively, indicating baseline rates of RTS at 100% and persistent symptom rates of 13% without concomitant procedures. While there were insignificant data to compare RTS rates with associated procedures in SSND performed at the SSN versus SGN, there were no significant trends noted in persistent symptoms for SSND performed at either the SSN (P = .848) or the SGN (P = .729).
Discussion
This expanded systematic review demonstrates that SSND is associated with statistically significant improvements in all PROM scores and that the vast majority of patients returned to sport or military duty with low rates of adverse events directly related to SSND. Additionally, a vast majority of patients present with preoperative EDT abnormalities prior to SSND; however, up to 30% will continue to have postoperative abnormalities despite improvements in PROMs. Collectively, this systematic review supports SSND as a safe and effective surgical treatment for suprascapular neuropathy with high rates of RTS and military duty, which is especially important given the higher rate of suprascapular neuropathy observed among these populations.9,48
Patient-reported outcome measures (PROMs)
In this study, all 6 measured PROMs improved significantly following SSND. While there is scant literature to confirm the minimal clinically important difference values specific to SSND, assessing the 25.4-point improvement in ASES following SSND as compared to the 15.4 (standard deviation = 5.7) point ASES threshold for other shoulder procedures indicates substantial clinical improvement. In comparing the substantial clinical benefit and patient acceptable symptom state thresholds defined for subacromial impingement, an 11-point improvement in DASH scores and a final VAS pain score of 3.0 or less indicates clinical benefit.49 Promisingly, improvements in PROMs observed in this study are consistent with existing literature, with Momaya et al and Memon et al both reporting significant improvements in VAS pain scores in addition to improvements in postoperative strength testing.36,37 In appropriately indicated patients, these results suggest that SSND can be expected to improve measures of patient pain and function postoperatively, although future research establishing minimal clinically important difference, substantial clinical benefit, and patient acceptable symptom state thresholds specific to SSND will offer value in understanding a targeted threshold for clinical improvements associated with this procedure.
Return to sport
Overhead athletes are at risk for various shoulder injuries45 and compose the predominant athletic population at risk for developing suprascapular neuropathy.29,43,48 While the reason for suprascapular neuropathy in this population is not fully understood, it has been theorized that the high incidence of labral tears generates paralabral cysts that lead to the development of suprascapular neuropathy.36 In this study, 98% of patients were able to RTS or military duty with 96% of those patients able to RTS or duty at their previous functional level. Similar findings have been reported in other large reviews, with a notably high (>85%) return to play.36,37 The high rate of RTS among this patient cohort supports the assertion that SSND offers benefits to the athlete population and does not appear to prevent return to activity. However, the functional improvements afforded by SSND appear to be limited to patients with suprascapular neuropathy, as multiple recent studies have shown that SSND offers no benefit as a routine adjunct to RCR.21,32,56 Subsequently, identifying patients with symptomatic suprascapular neuropathy or SSN/SGN compression becomes critical in indicating appropriate patients for SSND rather than including SSND in all RCR procedures by default.
Electrodiagnostic testing (EDT)
Based on the results of this present study, it is prudent that patients with physical examination and advanced imaging findings suggestive of suprascapular neuropathy undergo neurodiagnostic testing to aid in the diagnosis and establish a pretreatment baseline.48 As discussed, there are many potential causes for suprascapular neuropathy with labral tear-associated cysts and retracted rotator cuff tears being among the most common. In the present study, 93% of patients underwent preoperative EDT and 90% of patients with preoperative EDT had associated abnormal findings. In their direct comparison, Tsikouris et al found that high-level athletes with rotator cuff tears or glenoid labral cysts with abnormal preoperative suprascapular EDT had superior clinical outcomes when treated with combined arthroscopic repair/cyst decompression in combination with SSND as compared to the indexed arthroscopic procedure alone.52 Given that routine SSND for RCR appears to lack substantial benefits, achieving a preoperative suprascapular neuropathy diagnosis offers value in establishing which patients will benefit from SSND.21,32,56 Based on the findings of the present study, the authors believe that iatrogenic injury to the nerve and the associated complication profile during the procedure should only be risked if a preoperative suprascapular neuropathy is clinically diagnosed.
Importantly, however, not all patients with rotator cuff tears or paralabral cysts will have abnormal EDT findings of suprascapular neuropathy. Collin et al prospectively performed EDT on all their patients undergoing RCR and found only 2% showed abnormal EDT findings.11 Various other studies have reported higher prevalence rates; however, it is important to note these higher rates were more common in massive rotator cuff tears.7,12,27,53 Gerber et al21 performed a prospective, randomized control trial on combining SSND in RCR for patients without preoperative EDT abnormalities but ultimately terminated the study early as emerging findings explicitly showed no benefit for the adjunct nerve decompression in this setting. Ultimately, the high rate of successful PROM achievement and RTS in a population with 90% abnormal preoperative EDT described in this study suggests that SSND appears to have added benefits when indicated as a result of abnormal preoperative EDT findings.
Adverse events
In this review, approximately 12% of patients reported continued pain or discomfort in the postoperative setting, while 11% experienced complications and 3.3% required subsequent surgery. It is our opinion, based on the nature of included studies, that the rates of adverse events are undoubtedly overestimates given the high rate of concomitant procedures associated with SSND coupled with a common lack of differentiation between SSND-related adverse events from other procedural adverse events. This is reinforced by the significant variability among complication and reoperation rates between included studies. When limited to rates of persistent symptoms and RTS associated with RCR, labral repair, and biceps tenodesis/tenotomy rates, the statistically significant estimated rate of these persistent symptoms was 13% without evidence of statistically significant changes based on the 3 associated procedures, likely explaining the overall rates of adverse events in this article that appear higher than similar reviews.36,37 However, there was significant heterogeneity between the included studies that should be interpreted accordingly. Importantly, after accounting for continued pain or discomfort, the adverse events rates were notably similar.
Limitations
As is the nature of any systematic review, the conclusions drawn in the present study are limited by the evidence reported by articles eligible for inclusion. PROMs selected for inclusion varied significantly between studies and, other than VAS, were not reported widely enough to determine how concomitant procedures impact final PROM scores. Additionally, rates of adverse events included those specific to SSND as well as other concomitant procedures, thereby overestimating complication and reoperation rates from SSND directly. Additionally, this study did not attempt to compare open versus arthroscopic SSND and faced limitations in separately assessing outcomes after SSND at the SSN versus the SGN. Overall, there is a paucity of prospective comparative studies in the use of EDT and open verses arthroscopic management and the generalizability of this article may be limited in centers without the use of EDT or for surgeons with limited training in surgical techniques of SSND.
Conclusion
Suprascapular neuropathy treated with SSND significantly improves patient-reported outcomes and is noninferior to similar procedures without SSND. Appropriate clinical diagnosis of suprascapular neuropathy is required as opposed to a routine adjunct procedure with other arthroscopic shoulder surgery. Ultimately, SSND is associated with high rates of RTS and relatively low rates of adverse events; however, the risk of continued symptoms and electrodiagnostic test-related complications is an important point on preoperative counseling.
Disclaimers:
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest: Each author certifies that they have no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Footnotes
Institutional review board approval was not required for this systematic review.
The views expressed in this publication are those of the author(s) and do not reflect the official policy or position of William Beaumont Army Medical Center, Department of the Army, Defense Health Agency, or the US Government.
References
- 1.Abboud J.A., Silverberg D., Glaser D.L., Ramsey M.L., Williams G.R. Arthroscopy effectively treats ganglion cysts of the shoulder. Clin Orthop Relat Res. 2006;444:129–133. doi: 10.1097/01.blo.0000201155.44572.9b. [DOI] [PubMed] [Google Scholar]
- 2.Albritton M.J., Graham R.D., Richards R.S., Basamania C.J. An anatomic study of the effects on the suprascapular nerve due to retraction of the supraspinatus muscle after a rotator cuff tear. J Shoulder Elbow Surg. 2003;12:497–500. doi: 10.1016/s1058-2746(03)00182-4. [DOI] [PubMed] [Google Scholar]
- 3.Arriaza R., Ballesteros J., López-Vidriero E. Suprascapular neuropathy as a cause of swimmer's shoulder: results after arthroscopic treatment in 4 patients. Am J Sports Med. 2013;41:887–893. doi: 10.1177/0363546513477383. [DOI] [PubMed] [Google Scholar]
- 4.Bayramoğlu A., Demiryürek D., Tüccar E., Erbil M., Aldur M.M., Tetik O., et al. Variations in anatomy at the suprascapular notch possibly causing suprascapular nerve entrapment: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2003;11:393–398. doi: 10.1007/s00167-003-0378-3. [DOI] [PubMed] [Google Scholar]
- 5.Bilsel K., Erdil M., Elmadag M., Ozden V.E., Celik D., Tuncay I. The effect of infraspinatus hypotrophy and weakness on the arthroscopic treatment of spinoglenoid notch cyst associated with superior labrum anterior-to-posterior lesions. Knee Surg Sports Traumatol Arthrosc. 2014;22:2209–2215. doi: 10.1007/s00167-013-2469-0. [DOI] [PubMed] [Google Scholar]
- 6.Boykin R.E., Friedman D.J., Higgins L.D., Warner J.J. Suprascapular neuropathy. J Bone Joint Surg Am. 2010;92:2348–2364. doi: 10.2106/JBJS.I.01743. [DOI] [PubMed] [Google Scholar]
- 7.Boykin R.E., Friedman D.J., Zimmer Z.R., Oaklander A.L., Higgins L.D., Warner J.J. Suprascapular neuropathy in a shoulder referral practice. J Shoulder Elbow Surg. 2011;20:983–988. doi: 10.1016/j.jse.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 8.Cano-Martínez J.A., Nicolás-Serrano G., Villodres Corpás J., Bento-Gerard J. Arthroscopic release of proximal supra-scapular nerve entrapment: Medium-term results. Rev Esp Cir Ortop Traumatol (Engl Ed) 2021;65:91–98. doi: 10.1016/j.recot.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Challoumas D., Dimitrakakis G. Insights into the epidemiology, aetiology and associations of infraspinatus atrophy in overhead athletes: a systematic review. Sports BioMech. 2017;16:325–341. doi: 10.1080/14763141.2017.1306096. [DOI] [PubMed] [Google Scholar]
- 10.Chen A.L., Ong B.C., Rose D.J. Arthroscopic management of spinoglenoid cysts associated with SLAP lesions and suprascapular neuropathy. Arthroscopy. 2003;19:E15–E21. doi: 10.1016/s0749-8063(03)00381-5. [DOI] [PubMed] [Google Scholar]
- 11.Collin P., Treseder T., Lädermann A., Benkalfate T., Mourtada R., Courage O., et al. Neuropathy of the suprascapular nerve and massive rotator cuff tears: a prospective electromyographic study. J Shoulder Elbow Surg. 2014;23:28–34. doi: 10.1016/j.jse.2013.07.039. [DOI] [PubMed] [Google Scholar]
- 12.Costouros J.G., Porramatikul M., Lie D.T., Warner J.J. Reversal of suprascapular neuropathy following arthroscopic repair of massive supraspinatus and infraspinatus rotator cuff tears. Arthroscopy. 2007;23:1152–1161. doi: 10.1016/j.arthro.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 13.Davis F.B., Katsuura Y., Dorizas J.A. A retrospective review of 112 patients undergoing arthroscopic suprascapular nerve decompression. J Orthop. 2020;19:31–35. doi: 10.1016/j.jor.2019.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dramis A., Pimpalnerkar A. Suprascapular neuropathy in volleyball players. Acta Orthop Belg. 2005;71:269–272. [PubMed] [Google Scholar]
- 15.Edelson J.G. Bony bridges and other variations of the suprascapular notch. J Bone Joint Surg Br. 1995;77:505–506. [PubMed] [Google Scholar]
- 16.Fabre T., Piton C., Leclouerec G., Gervais-Delion F., Durandeau A. Entrapment of the suprascapular nerve. J Bone Joint Surg Br. 1999;81:414–419. doi: 10.1302/0301-620x.81b3.9113. [DOI] [PubMed] [Google Scholar]
- 17.Feinberg J.H., Mehta P., Gulotta L.V., Allen A.A., Altchek D.W., Cordasco F.A., et al. Electrodiagnostic evidence of suprascapular nerve recovery after decompression. Muscle Nerve. 2019;59:247–249. doi: 10.1002/mus.26354. [DOI] [PubMed] [Google Scholar]
- 18.Ferretti A., De Carli A., Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch. The natural history of infraspinatus atrophy in volleyball players. Am J Sports Med. 1998;26:759–763. doi: 10.1177/03635465980260060401. [DOI] [PubMed] [Google Scholar]
- 19.Freehill M.T., Shi L.L., Tompson J.D., Warner J.J. Suprascapular neuropathy: diagnosis and management. Phys Sportsmed. 2012;40:72–83. doi: 10.3810/psm.2012.02.1953. [DOI] [PubMed] [Google Scholar]
- 20.Garcia J.C., Júnior, Paccola A.M., Tonoli C., Zabeu J.L., Garcia J.P. Arthroscopic release of the suprascapular nerve: surgical technique and evaluation of clinical cases. Rev Bras Ortop. 2011;46:403–407. doi: 10.1016/S2255-4971(15)30252-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gerber C., Meyer D.C., Wieser K., Sutter R., Schubert M., Kriechling P. Suprascapular nerve decompression in addition to rotator cuff repair: a prospective, randomized observational trial. J Shoulder Elbow Surg. 2020;29:1633–1641. doi: 10.1016/j.jse.2020.03.051. [DOI] [PubMed] [Google Scholar]
- 22.Hama H., Ueba Y., Morinaga T., Suzuki K., Kuroki H., Yamamuro T. A new strategy for treatment of suprascapular entrapment neuropathy in athletes: shaving of the base of the scapular spine. J Shoulder Elbow Surg. 1992;1:253–260. doi: 10.1016/S1058-2746(09)80067-0. [DOI] [PubMed] [Google Scholar]
- 23.Hashiguchi H., Iwashita S., Ohkubo A., Takai S. SLAP repair with arthroscopic decompression of spinoglenoid cyst. SICOT J. 2016;2:1. doi: 10.1051/sicotj/2015036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katsuura Y., Yao K., Chang E., Kadrie T.A., Dorizas J.A. Shoulder double crush syndrome: a retrospective study of patients with concomitant suprascapular neuropathy and cervical radiculopathy. Clin Med Insights Arthritis Musculoskelet Disord. 2020;13 doi: 10.1177/1179544120921854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim S.J., Choi Y.R., Jung M., Park J.Y., Chun Y.M. Outcomes of arthroscopic decompression of spinoglenoid cysts through a subacromial approach. Arthroscopy. 2017;33:62–67. doi: 10.1016/j.arthro.2016.05.034. [DOI] [PubMed] [Google Scholar]
- 26.Kim D.S., Park H.K., Park J.H., Yoon W.S. Ganglion cyst of the spinoglenoid notch: comparison between SLAP repair alone and SLAP repair with cyst decompression. J Shoulder Elbow Surg. 2012;21:1456–1463. doi: 10.1016/j.jse.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Lafosse L., Piper K., Lanz U. Arthroscopic suprascapular nerve release: indications and technique. J Shoulder Elbow Surg. 2011;20:S9–S13. doi: 10.1016/j.jse.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Lafosse L., Tomasi A., Corbett S., Baier G., Willems K., Gobezie R. Arthroscopic release of suprascapular nerve entrapment at the suprascapular notch: technique and preliminary results. Arthroscopy. 2007;23:34–42. doi: 10.1016/j.arthro.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Lajtai G., Pfirrmann C.W., Aitzetmüller G., Pirkl C., Gerber C., Jost B. The shoulders of professional beach volleyball players: high prevalence of infraspinatus muscle atrophy. Am J Sports Med. 2009;37:1375–1383. doi: 10.1177/0363546509333850. [DOI] [PubMed] [Google Scholar]
- 30.Leclere L.E., Shi L.L., Lin A., Yannopoulos P., Higgins L.D., Warner J.J. Complete Fatty infiltration of intact rotator cuffs caused by suprascapular neuropathy. Arthroscopy. 2014;30:639–644. doi: 10.1016/j.arthro.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 31.Lichtenberg S., Magosch P., Habermeyer P. Compression of the suprascapular nerve by a ganglion cyst of the spinoglenoid notch: the arthroscopic solution. Knee Surg Sports Traumatol Arthrosc. 2004;12:72–79. doi: 10.1007/s00167-003-0443-y. [DOI] [PubMed] [Google Scholar]
- 32.Ma H.H., Wu W.T., Tsai I.C., Chang K.V. Does suprascapular nerve release provide additional benefits for rotator cuff repair: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2022;31:2421–2430. doi: 10.1016/j.jse.2022.05.015. [DOI] [PubMed] [Google Scholar]
- 33.Mall N.A., Hammond J.E., Lenart B.A., Enriquez D.J., Twigg S.L., Nicholson G.P. Suprascapular nerve entrapment isolated to the spinoglenoid notch: surgical technique and results of open decompression. J Shoulder Elbow Surg. 2013;22:e1–e8. doi: 10.1016/j.jse.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Mallon W.J., Wilson R.J., Basamania C.J. The association of suprascapular neuropathy with massive rotator cuff tears: a preliminary report. J Shoulder Elbow Surg. 2006;15:395–398. doi: 10.1016/j.jse.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 35.Martin S.D., Warren R.F., Martin T.L., Kennedy K., O'Brien S.J., Wickiewicz T.L. Suprascapular neuropathy. Results of non-operative treatment. J Bone Joint Surg Am. 1997;79:1159–1165. doi: 10.2106/00004623-199708000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Memon M., Kay J., Ginsberg L., Simunovic N., Bak K., Lapner P., et al. Arthroscopic management of suprascapular neuropathy of the shoulder improves pain and functional outcomes with minimal complication rates. Knee Surg Sports Traumatol Arthrosc. 2018;26:240–266. doi: 10.1007/s00167-017-4694-4. [DOI] [PubMed] [Google Scholar]
- 37.Momaya A.M., Kwapisz A., Choate W.S., Kissenberth M.J., Tolan S.J., Lonergan K.T., et al. Clinical outcomes of suprascapular nerve decompression: a systematic review. J Shoulder Elbow Surg. 2018;27:172–180. doi: 10.1016/j.jse.2017.09.025. [DOI] [PubMed] [Google Scholar]
- 38.Nolte P.C., Woolson T.E., Elrick B.P., Tross A.K., Horan M.P., Godin J.A., et al. Clinical outcomes of arthroscopic suprascapular nerve decompression for suprascapular neuropathy. Arthroscopy. 2021;37:499–507. doi: 10.1016/j.arthro.2020.10.020. [DOI] [PubMed] [Google Scholar]
- 39.Perry N.P.J., Wolfe J.A., Nguyen-Ta K., Christensen D., McDonald L.S., Dickens J.F., et al. Biceps tenodesis and intra-articular decompression for treatment of superior labral tear from anterior to posterior and associated paralabral cyst in active duty military. Mil Med. 2018;183:e194–e200. doi: 10.1093/milmed/usx019. [DOI] [PubMed] [Google Scholar]
- 40.Pillai G., Baynes J.R., Gladstone J., Flatow E.L. Greater strength increase with cyst decompression and SLAP repair than SLAP repair alone. Clin Orthop Relat Res. 2011;469:1056–1060. doi: 10.1007/s11999-010-1661-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ringel S.P., Treihaft M., Carry M., Fisher R., Jacobs P. Suprascapular neuropathy in pitchers. Am J Sports Med. 1990;18:80–86. doi: 10.1177/036354659001800113. [DOI] [PubMed] [Google Scholar]
- 42.Sachinis N.P., Papagiannopoulos S., Sarris I., Papadopoulos P. Outcomes of arthroscopic nerve release in patients treated for large or massive rotator cuff tears and associated suprascapular neuropathy: a prospective, randomized, double-blinded clinical trial. Am J Sports Med. 2021;49:2301–2308. doi: 10.1177/03635465211021834. [DOI] [PubMed] [Google Scholar]
- 43.Sandow M.J., Ilic J. Suprascapular nerve rotator cuff compression syndrome in volleyball players. J Shoulder Elbow Surg. 1998;7:516–521. doi: 10.1016/s1058-2746(98)90205-1. [DOI] [PubMed] [Google Scholar]
- 44.Savoie F.H., Zunkiewicz M., Field L.D., Replogle W.H., O'Brien M.J. A comparison of functional outcomes in patients undergoing revision arthroscopic repair of massive rotator cuff tears with and without arthroscopic suprascapular nerve release. Open Access J Sports Med. 2016;7:129–134. doi: 10.2147/OAJSM.S113020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Scanaliato J.P., Wells M.E., Dunn J.C., Garcia E.J. Overview of sport-specific injuries. Sports Med Arthrosc Rev. 2021;29:185–190. doi: 10.1097/JSA.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 46.Shah A.A., Butler R.B., Sung S.Y., Wells J.H., Higgins L.D., Warner J.J. Clinical outcomes of suprascapular nerve decompression. J Shoulder Elbow Surg. 2011;20:975–982. doi: 10.1016/j.jse.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 47.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 48.Strauss E.J., Kingery M.T., Klein D., Manjunath A.K. the evaluation and management of suprascapular neuropathy. J Am Acad Orthop Surg. 2020;28:617–627. doi: 10.5435/JAAOS-D-19-00526. [DOI] [PubMed] [Google Scholar]
- 49.Su F., Allahabadi S., Bongbong D.N., Feeley B.T., Lansdown D.A. Minimal clinically important difference, substantial clinical benefit, and patient acceptable symptom state of outcome measures relating to shoulder pathology and surgery: a systematic review. Curr Rev Musculoskelet Med. 2021;14:27–46. doi: 10.1007/s12178-020-09684-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thompson W.A., Kopell H.P. Peripheral entrapment neuropathies of the upper extremity. N Engl J Med. 1959;260:1261–1265. doi: 10.1056/NEJM195906182602503. [DOI] [PubMed] [Google Scholar]
- 51.Ticker J.B., Djurasovic M., Strauch R.J., April E.W., Pollock R.G., Flatow E.L., et al. The incidence of ganglion cysts and other variations in anatomy along the course of the suprascapular nerve. J Shoulder Elbow Surg. 1998;7:472–478. doi: 10.1016/s1058-2746(98)90197-5. [DOI] [PubMed] [Google Scholar]
- 52.Tsikouris G.D., Bolia I.K., Vlaserou P., Odantzis N., Angelis K., Psychogios V. Shoulder arthroscopy with versus without suprascapular nerve release: clinical outcomes and return to sport rate in elite overhead athletes. Arthroscopy. 2018;34:2552–2557. doi: 10.1016/j.arthro.2018.03.046. [DOI] [PubMed] [Google Scholar]
- 53.Vad V.B., Southern D., Warren R.F., Altchek D.W., Dines D. Prevalence of peripheral neurologic injuries in rotator cuff tears with atrophy. J Shoulder Elbow Surg. 2003;12:333–336. doi: 10.1016/s1058-2746(03)00040-5. [DOI] [PubMed] [Google Scholar]
- 54.Westerheide K.J., Dopirak R.M., Karzel R.P., Snyder S.J. Suprascapular nerve palsy secondary to spinoglenoid cysts: results of arthroscopic treatment. Arthroscopy. 2006;22:721–727. doi: 10.1016/j.arthro.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 55.Yamakado K. Arthroscopic rotator cuff repair with or without suprascapular nerve decompression in posterosuperior massive rotator cuff tears. Int Orthop. 2019;43:2367–2373. doi: 10.1007/s00264-019-04356-4. [DOI] [PubMed] [Google Scholar]
- 56.Yang L.M.H., Kuo L.T., Hsu W.H., Yu P.A., Chen C.L., Tsai Y.H. Suprascapular nerve release does not provide additional benefits in arthroscopic rotator cuff repair surgery: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2023;31:1873–1882. doi: 10.1007/s00167-022-07066-4. [DOI] [PubMed] [Google Scholar]
- 57.Yang P., Wang C., Zhang D., Zhang Y., Yu T., Qi C. Comparison of clinical outcome of decompression of suprascapular nerve at spinoglenoid notch for patients with posterosuperior massive rotator cuff tears and suprascapular neuropathy. BMC Musculoskelet Disord. 2021;22:202. doi: 10.1186/s12891-021-04075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]