Abstract
Pathology of the long head of the biceps tendon is commonly associated with massive rotator cuff tears (MRCTs), which account for roughly one third of all rotator cuff tears. Treatment options for this condition include tenotomy, tenodesis, augmentation, and the use of the tendon as a graft for partial superior capsule reconstruction. Augmentation and superior capsular reconstruction are evolving techniques in the management of MRCTs. However, similar to the lack of consensus on the treatment of MRCTs, there are no clear guidelines for the management of concurrent biceps tendon pathology.
Keywords: Biceps tendon, Long head, Massive, Rotator cuff, Augmentation, Patch, Reconstruction
Massive rotator cuff tears (MRCTs) represent a significant portion of rotator cuff tears, accounting for 20%-40% of all tears.10,51 In the setting of MRCTs, the long head of the biceps tendon (LHBT) is often affected, causing anterior shoulder pain and dysfunction as a result of tendonitis, partial tearing, or subluxation.1,21 Comprehending these pathologies can offer valuable insights and direction towards determining the optimal course of treatment.
There is a wide variety of treatment options for LHBT pathology in the setting of MRCTs. These include tenotomy, tenodesis, rotator cuff repair (RCR) augmentation, and as partial superior capsule reconstruction (BiSCR). Determining the appropriate course of treatment is patient specific and must factor in age, comorbidities, activity level, degree of biceps tendon pathology, and rotator cuff tissue quality such as tear size, pattern and fatty infiltration.45
The purpose of this article is to provide a comprehensive review of the anatomy and biomechanics of the LHBT, as well as the surgical options and outcomes for LHBT pathology in the context of MRCTs.
Anatomy
The biceps brachii muscle is comprised of a short head and a long head.48 The short head arises from the anterolateral aspect of the coracoid process as part of the conjoined tendon. The long head originates from the supraglenoid tubercle of the scapula.11,17 The LHBT has an intra-articular portion that passes over the humeral head before exiting the glenohumeral joint in the bicipital groove.11,17 The tendon measures around 5-6 mm in diameter and 9 cm in length, but its size may vary between individuals.18 Typically, the intra-articular portion is wide and flat, while the extra-articular portion is rounder and thinner.54
There are variations in vascular supply and sensory innervation along the length of the tendon. The proximal portion of the long head is richly vascularized with the anterior circumflex humeral artery being the main blood supply.18 In contrast, the distal portion is fibrocartilaginous and avascular which in turn facilitates its sliding motion within the groove. Sensory innervation follows a similar pattern, with rich sensory and sympathetic supply concentrated at the biceps tendon anchor proximally that then becomes less intense at the distal musculotendinous junction.4 This observation may explain why proximal LHBT pathology can be very symptomatic.
During arm movements, the LHBT is stabilized by the bicipital groove and the biceps pulley.41 The biceps pulley is a ligamentous structure that acts as a sling to stabilize the LHBT as it exits the joint.41 It is composed of two structures, namely the superior glenohumeral ligament (SGHL) and coracohumeral ligament (CHL).16 The transverse humeral ligament is a broad fibrous band located between the greater and lesser tuberosities of the humerus.49 Although it was traditionally thought to help retain the LHBT within the bicipital groove, its role as a stabilizer has been recently questioned by several authors.13,50 As the LHBT travels through the glenohumeral joint, it runs alongside the upper part of the subscapularis (SSC) muscle. Biceps subluxation can result from injury to the SGHL, CHL, and/or the associated SSC fibers.50
In the context of MRCTs, particularly involving partial anterosuperior SSC tendon tears, a distinctive 'comma' shape is appreciated as the SSC tendon retracts medially, revealing the SGHL and CHL.15, 16, 17 Termed the 'comma sign,' this hallmark aids in identifying the SSC's superolateral border. Research has highlighted the capsule's role in this configuration, thickening the rotator interval to connect the articular SSC and bursal SS tendons.15,17 This capsule-based structure envelops the bicipital groove, merging with the SGHL and CHL, reinforcing the SSC tendon's fibrous framework.
Biomechanics
The LHBT is regarded as a dynamic stabilizer of the glenohumeral joint. Although the precise contribution of the LHBT to humeral head stability remains a topic of debate, several studies have corroborated the importance of the LHBT in joint stability. Complete disruption of the LHBT has been shown to contribute to superior humeral head migration, and thus reduction of the acromiohumeral interval (AHI).44 In a clinical study conducted by Ratte et al,46 patients with a normal LHBT exhibited a narrowed AHI in 33.4% of cases compared to 100% of patients with a pathological LHBT (P = .05). In a cadaveric study by Han et al,24 BiSCR was shown to reduce superior humeral head translation and subacromial contact pressures at 0° and 60° of glenohumeral abduction. These findings suggest that an intact LHBT plays a role in maintaining a centered humeral head.
While some experts advocate preserving the LHBT in rotator cuff tears to act as a humeral head depressor, the biceps is not a primary stabilizer of the glenohumeral joint as the retentive effect is negligible when the coracoacromial arch is maintained.40 Thus, the long head of the biceps may contribute to shoulder stability, but its absence or a tenotomy alone may not cause significant instability. It is important to note that the glenohumeral joint is a complex structure, and stability is influenced by multiple factors, including the integrity of other structures like the rotator cuff muscles and joint capsule.
Surgical treatment options
In the management of MRCTs, two common approaches for dealing with the LHBT are biceps tenotomy or tenodesis.22 More recently, there have been emerging techniques that integrate the biceps into MRCT repair constructs.
Tenotomy and tenodesis
Biceps tenotomy is a simpler procedure that involves complete cutting or division of the LHBT (Fig. 1).22 The tendon is completely detached from its origin and allowed to retract into the arm away from the shoulder joint. Biceps tenotomy is considered when preserving the tendon is not a priority or when it is significantly degenerated or damaged. However, a cosmetic deformity known as a “Popeye deformity,” characterized by a visible bulge in the upper arm due to the retracted biceps muscle, is frequently postoperatively. Conversely, biceps tenodesis is a surgical procedure that involves detaching the LHBT from its origin and reattaching the tendon to a stable location on the humerus during RCR (Fig. 2).23 The goal is to stabilize the biceps tendon, and maintain cosmesis and perhaps function.
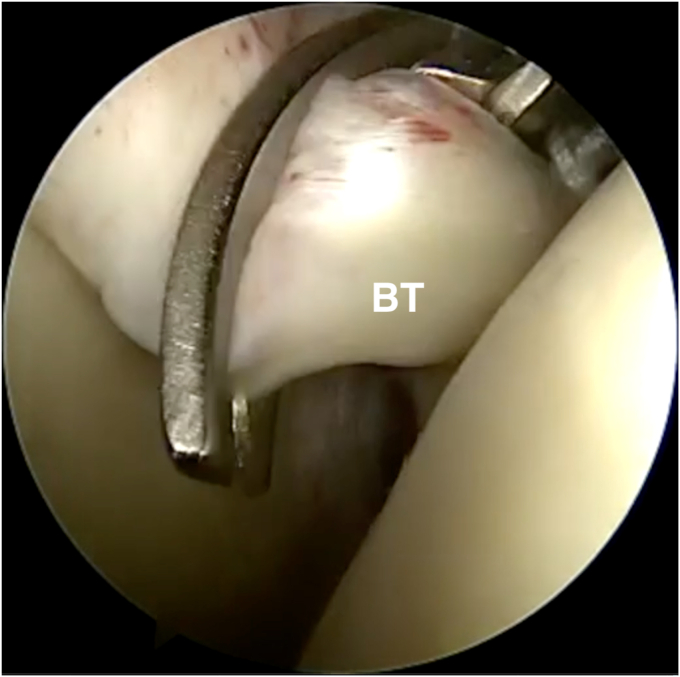
Figure 1.
Arthroscopic view of a right shoulder through a 70° arthroscope via the posterior portal in a patient in the lateral decubitus position showing tenotomy of the long head of biceps tendon using a scissor. BT, biceps tendon.
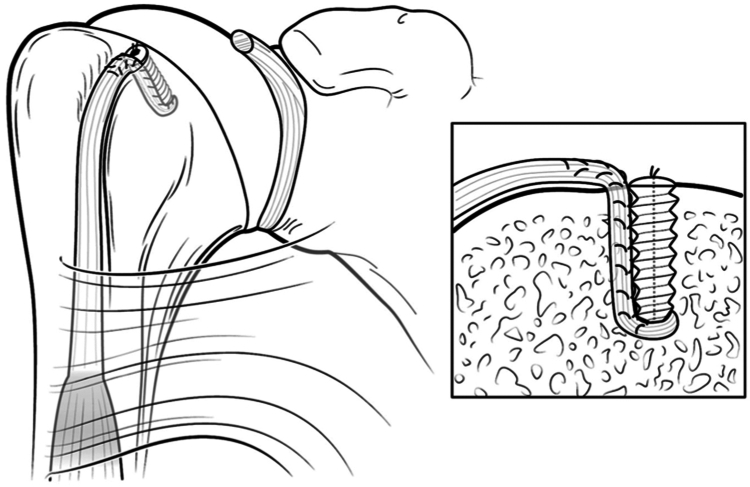
Figure 2.
Schematic of a biceps tenodesis high in the bicipital groove performed using an inlay technique. The interference screw and the biceps tendon, which is whipstiched past the length of the screw, are placed inside the bone socket as shown in the enlarged figure on the right. Obtained with permission from: Haidamous G, Noyes MP, Denard PJ. Arthroscopic Biceps Tenodesis Outcomes: A Comparison of Inlay and Onlay Techniques. Am J Sports Med. 2020 Oct;48(12):3051-3056. https://doi.org/10.1177/0363546520952357.
The clinical observation that LHBT spontaneous rupture could alleviate pain in MRCTs led Walch et al52 to introduce arthroscopic tenotomy in a series of 307 patients as a simple, palliative, and reproducible measure. However, their study included 38% of patients with preoperative shoulder osteoarthritis, raising questions about the extent to which tenotomy addressed rotator cuff pain, arthritis pain or both. Furthermore, patients with MRCTs and a high grade of fatty infiltration presented worse postoperative outcomes, indicating that fatty infiltration of the rotator cuff negatively influences the results of arthroscopic biceps tenotomy, similar to its effect on RCR. It is important to note that while the authors did not speculate on the mechanisms, they reported that the procedure was effective for a selected group of MRCTs.52 Isolated biceps tenotomy is considered for older patients with MRCTs seeking pain relief without requiring postoperative rehabilitation.7,40,43,52 Conversely, biceps tenodesis is undertaken among young, moderately active patients or in those concerned about the potential cosmetic deformity associated with tenotomy.22
Postoperatively, both biceps tenotomy and tenodesis have been found to significantly reduce pain and improve function.15,22 Zhang et al56 conducted a randomized control trial comparing clinical outcomes in patients at least 55 year old undergoing tenotomy (n = 77) or tenodesis (n = 74) with concomitant arthroscopic RCR. They found no significant differences in terms of Constant Scores (CS), forearm supination and elbow flexion strength, Popeye deformity, Visual Analog Scale (VAS) for pain, and satisfaction when comparing both procedures at an average 24-month follow-up. However, they reported a shorter surgical time (40.4 ± 4.0 vs. 50.4 ± 5.9 min; P < .001) and faster pain relief in the tenotomy group at the 2-week postoperative mark (VAS, 3.1 ± 1.8 vs. 4.8 ± 1.9; P < .001). Alternatively, Belay et al6 descriptively reported in their randomized controlled trial of 34 patients (tenotomy, n = 20; tenodesis, n = 14) a lower VAS pain score at 3 months (2.6 ± 2.1 vs. 4.5 ± 2.2). These findings may reflect that tenotomy is less challenging and provides faster pain relief despite being historically linked to a higher incidence of cosmetic deformity than tenodesis.
Although the most commonly reported complication with tenotomy is the Popeye deformity, with an incidence as high as 70%, other setbacks include loss of the LHBT ability to stabilize the humeral head and sudden onset cramping pain.7 Conversely, tenodesis involves tendon-to-tendon suturing leading to neutralization of opposite traction forces, thus reducing the risk of cosmetic deformity and superior humeral head translation.33 Despite these advantages, some complications, such as bicipital groove pain and stiffness, are more prevalent with tenodesis.34 Taking care not to over-tense the LHBT can help prevent bicipital groove pain.33 In this regard, tenodesis requires longer operative time and postoperative rehabilitation compared to tenotomy in the isolated setting.11,36 Tenodesis can be performed at different anatomical sites along the LHBT, requiring either an arthroscopic or open approach.35 Proximally, an all-arthroscopic technique can be utilized, while distally, an open approach is necessary.35 Proximal fixation includes Zone 1 (within the bicipital groove or integrated into the RCR) and Zone 2, at the suprapectoral region.35,36 Distal fixation is achieved through an open approach at the subpectoral level of the tendon.37 Arthroscopic tenodesis is often preferred, particularly when additional arthroscopic shoulder procedures are performed. Open tenodesis may be more suitable for cases where biceps pathology is too distal to be addressed arthroscopically, such as tendon lesions at or beyond the proximal edge of the pectoralis major, or for persistent pain following a previous biceps tenotomy or proximal tenodesis.25 Despite the lack of clinically significant differences between these two techniques, in the context of an arthroscopic repair of MRCT,1,20,23,53,55 a biceps tenodesis can be accomplished more efficiently with an arthroscopic approach rather than by performing a separate incision for distal fixation.
Augmentation
Biceps augmentation involves incorporating the LHBT into the RCR construct. The rationale behind this technique is to utilize LHBT’s biological profile to augment the repair and enhance the construct’s biomechanical properties. Colbath et al14 studied the ability of endogenous tenocytes derived from the LHBT scaffold to promote tenogenic differentiation of human adipose-derived mesenchymal stromal cells (ADMSCs). Tenocytes derived from the LHBT scaffold secreted growth factors that initiated ADMSC differentiation to an immature tenocyte-like phenotype. This immature phenotype demonstrated higher healing potential as shown by an 8.7× increase in scleraxis and a 3.6× in collagen type III messenger RNA expression compared to undifferentiated ADMSCs.
LHBT augmentation has gained popularity in recent years.42 Initially, biceps tenotomy or tenodesis was performed concomitantly with RCR. However, as the biological benefits have surfaced, more surgeons have integrated the LHBT to their repair constructs.8,52 In MRCTs, the LHBT can serve as an augmentation patch (Fig. 3) or can be sutured directly to the rotator cuff defect (Fig. 4). Early reports of biceps augmentation were described by Neviaser42 in 1971, where the LHBT tendon was cut proximally adjacent to the supraglenoid tuberosity and distally at the upper level of the bicipital groove. Subsequently, the intraarticular tendon segment was longitudinally sectioned to provide sufficient width to cover the humeral head, effectively using the LHBT as a patch. In another technique for biceps augmentation in MRCTs Ji et al27 left the LHBT's proximal insertion intact, and the tendon was incorporated into the defect area to provide additional resistance to suture cut out and enhance humeral head stability. Additional advantages include avoiding the potential risks associated with autograft and allografts, such as donor site morbidity and immune reactions, and increased cost.3 Despite the benefits of biceps augmentation, the biceps is not always present in the setting of a MRCT. Additionally, the potential as a graft source may be limited by tendon quality.42
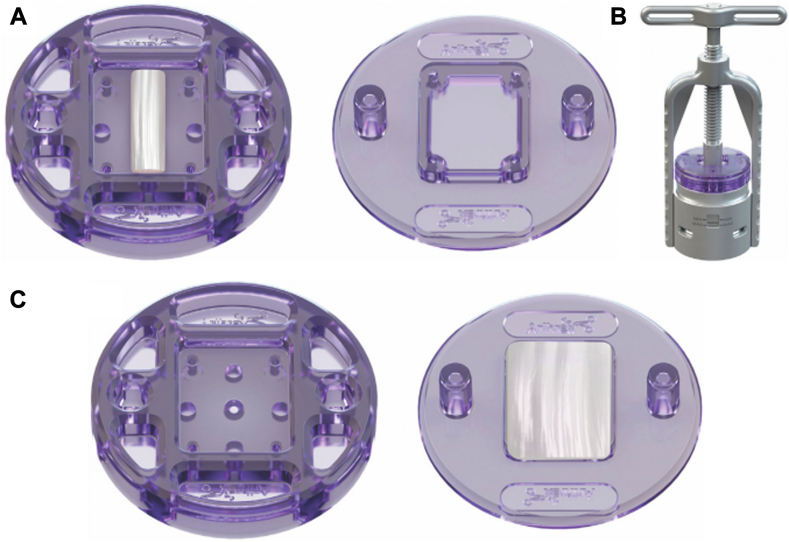
Figure 3.
Illustration of the LHBT preparation. (A) A 27 mm long segment of the LHBT is centered in the compression tray (Biceps Compression Tray; Arthrex Inc.). (B) The trays are placed into the device while holding compression between the minimum and maximum values (Modular Glenoid System; Arthrex Inc.). (C) Compressed biceps patch. LHBT, long head of the biceps tendon. Obtained with permission from: Denard PJ, Ardebol J, Pasqualini I, Horinek JL, Dines J, Tokish JM. Compressed autograft biceps tendon augmentation of subscapularis repair following shoulder arthroplasty. JSES Rev Rep Tech. 2022 Aug 24;2(4):535-538. https://doi.org/10.1016/j.xrrt.2022.08.002.
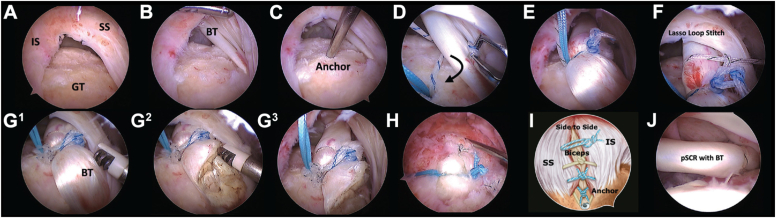
Figure 4.
Arthroscopic steps: (A-C) GT preparation and anchor placement. (D-F) LHBT tenodesis. (G1-G3) LHBT tenotomy. (H and I) Rotator cuff repair including LHBT. (J) Intra-articular view of SCR. BT, biceps tendon; GT, greater tuberosity; IS, infraspinatus; SCR, superior capsular reconstruction; SS, supraspinatus; LHBT, long head of the biceps tendon. Obtained with permission from: Llinás PJ, Bailie DS, Sanchez DA, Chica J, Londono JF, Herrera GA. Partial Superior Capsular Reconstruction to Augment Arthroscopic Repair of Massive Rotator Cuff Tears Using Autogenous Biceps Tendon: Effect on Retear Rate. Am J Sports Med. 2022 Sep;50(11):3064-3072. https://doi.org/10.1177/03635465221112659.
Studies have demonstrated that RCR with biceps augmentation generally leads to improvements in muscle strength and functional outcomes.3,13 Rhee et al47 reported significant improvement in functional outcomes in 31 cases undergoing open and arthroscopic RCR with LHBT augmentation in terms of VAS (Δ 1.75; P < .001), University of California Los Angeles score (Δ 18.6; P < .001), CS (Δ 33.4; P < .001), and Simple Shoulder Test (Δ 6; P < .001). Patients improved significantly in FF (Δ 36°; P < .001), external rotation (Δ 9°; P = .046), and abduction (Δ 34°; P < .001), but not in internal rotation (L1 to T10; P = .09). Complete healing was achieved in 64.3% of cases as determined using postoperative magnetic resonance images at the 32-month follow-up. Similarly, Jeong et al40 reported significant improvement in VAS, Simple Shoulder Test, CS, and range of motion (except external rotation) in their retrospective case series of 107 patients. At the 3-year follow-up, radiographs and magnetic resonance image showed a significant increase in the AHI (8.6-9.3 mm; P < .05) and a 79% healing rate, respectively. In a comparative study, Llinás et al46 compared clinical outcomes after arthroscopic RCR (n = 50 patients) to arthroscopic RCR with LHBT augmentation (n = 56). They showed significantly greater postoperative clinical improvement (American Shoulder and Elbow Surgeons score [ASES] 77 vs. 71, P < .01; VAS 1.6 vs. 2.1, P < .01) and healing (86% vs. 54%; P < .01) evaluated by ultrasound in the augmentation group at the 2-year follow-up.
While biceps augmentation offers potential benefits, there are considerations to be aware of. One important consideration is the increased complexity of the procedure, which may require additional surgical skills and expertise. Furthermore, the long-term effects and durability of biceps augmentation are still being studied, and further research is needed to fully understand its impact on long-term outcomes.
Superior capsular reconstruction
Superior capsule reconstruction was initially introduced by Mihata et al38 for patients with irreparable MRCTs using fascia lata autograft. However, to avoid donor site morbidity, Chillemi et al12 suggested using the LHBT. In their technique, the biceps tendon was tenotomized distally, and anchors were positioned anteriorly and posteriorly for lateral row fixation, thus providing a partial reconstruction of the superior capsule. BiSCR is suitable for MRCTs in young patients without arthritis, with fatty infiltration grade 3 or higher, and grade 4 retraction of the SS or infraspinatus tendons.5 However, like augmentation, BiSCR required sufficient tendon quality.2,9,30,39
Multiple studies have shown promising clinical outcomes with BiSCR.28, 29, 30 In their retrospective review, Barth et al49 found significant improvement in VAS (Δ 3.8; P < .001) and ASES (Δ 35; P < .001) in the BiSCR cohort of 24 patients. When comparing BiSCR to double-row (DR) repair or transosseous (TOE) repair plus patch, they found significantly higher postoperative strength (BiSCR 6.4 vs. TOE 4.7 vs. DR 4.0 kg; P = .006) and healing in the BiSCR cohort (BiSCR 92% vs. DR 61% vs. TOE 57%). In a retrospective review of 26 patients comparing superior capsule reconstruction with fascia lata to BiSCR, Kocaoglu et al31 reported that both groups improved comparably and significantly in ASES and VAS, with similar retear rates (21% vs. 17%; P > .05). They concluded LHBT use may offer similar improvement without the need for graft harvesting. Regardless of these positive outcomes, studies have consistently highlighted the importance of not over tensioning the LHBT at the proximal stump since it may generate persistent pain and compromise muscle strength for up to six months postoperatively.26,39 The tension on the proximal stump is influenced by suture placement and arm position, and when performed correctly, the procedure provides an effective downward vector that minimizes superior head migration.2,19 Nevertheless, autografts have fewer complications and revisions compared to allografts or xenografts.32
Conclusion
Having a comprehensive understanding of the available techniques for managing the LHBT during arthroscopic RCR of MRCTs is essential. Tenotomy is generally considered for older, less active patients, whereas tenodesis may be preferred for patients who desire a better cosmetic outcome and for those with higher activity levels requiring repetitive and forceful elbow flexion and forearm supination. In cases with repairable MRCTs and an intact LHBT, augmentation may be considered, while BiSCR presents as an option in irreparable tears. When present as a graft source, the LHBT represents a cost-effective choice with lower graft site morbidity compared to allografts. Nevertheless, both procedures require careful consideration of contraindications and surgical skill. In appropriately chosen patients, all available treatment options have demonstrated enhanced functional and healing outcomes.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: Dr. Denard has received consulting fees from Arthrex, Pacira Pharmaceuticals Incorporated; nonconsulting fees from Arthrex; royalties from Arthrex; education payments from Steelhead Surgical. Dr. Noble has received education payments from Rock Medical Orthopedics. Dr. Galasso has received education payments from Pinnacle, Arthrex; hospitality payments from Stryker. Dr. Menendez has received education payments has received Arthrex, Medwest Associates, Steelhead Surgical; hospitality payments from Stryker, Encore Medical, Medical Device Business Services. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this study.
References
- 1.Abraham V.T., Tan B.H.M., Kumar V.P. Systematic review of biceps tenodesis: arthroscopic versus open. Arthroscopy. 2016;32:365–371. doi: 10.1016/j.arthro.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 2.Adrian S.C., Field L.D. Biceps transposition for biological superior capsular reconstruction. Arthrosc Tech. 2020;9:e841–e846. doi: 10.1016/j.eats.2020.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aicale R., Poeta N., Savarese E., Bernardini G., Oliva F., Maffulli N. The use of long head biceps tendon autograft for massive rotator cuff tears: a PRISMA compliant systematic review. Br Med Bull. 2022;144:76–89. doi: 10.1093/bmb/ldac021. [DOI] [PubMed] [Google Scholar]
- 4.Alpantaki K. Sympathetic and sensory neural elements in the tendon of the long head of the biceps. J Bone Joint Surg Am. 2005;87:1580. doi: 10.2106/JBJS.D.02840. [DOI] [PubMed] [Google Scholar]
- 5.Barth J., Olmos M.I., Swan J., Barthelemy R., Delsol P., Boutsiadis A. Superior capsular reconstruction with the long head of the biceps autograft prevents infraspinatus retear in massive posterosuperior retracted rotator cuff tears. Am J Sports Med. 2020;48:1430–1438. doi: 10.1177/0363546520912220. [DOI] [PubMed] [Google Scholar]
- 6.Belay E.S., Wittstein J.R., Garrigues G.E., Lassiter T.E., Scribani M., Goldner R.D., et al. Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2019;27:4032–4037. doi: 10.1007/s00167-019-05682-1. [DOI] [PubMed] [Google Scholar]
- 7.Boileau P., Baqué F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 8.Boileau P., Krishnan S.G., Coste J.S., Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;18:1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 9.Boutsiadis A., Chen S., Jiang C., Lenoir H., Delsol P., Barth J. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: “The Chinese Way”. Arthrosc Tech. 2017;6:e1559–e1566. doi: 10.1016/j.eats.2017.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burkhart S.S., Barth J.R.H., Richards D.P., Zlatkin M.B., Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23:347–354. doi: 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Carter A.M., Erickson S.M., Harmon K.G. Proximal biceps tendon rupture. Phys Sportsmed. 1999;27:95–101. doi: 10.3810/psm.1999.06.888. [DOI] [PubMed] [Google Scholar]
- 12.Chillemi C., Mantovani M., Gigante A. Superior capsular reconstruction of the shoulder: the ABC (Arthroscopic Biceps Chillemi) technique. Eur J Orthop Surg Traumatol. 2018;28:1215–1223. doi: 10.1007/s00590-018-2183-1. [DOI] [PubMed] [Google Scholar]
- 13.Cho N.S., Yi J.W., Rhee Y.G. Arthroscopic biceps augmentation for avoiding undue tension in repair of massive rotator cuff tears. Arthroscopy. 2009;25:183–191. doi: 10.1016/j.arthro.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Colbath G., Murray A., Siatkowski S., Pate T., Krussig M., Pill S., et al. Autograft long head biceps tendon can be used as a scaffold for biologically augmenting rotator cuff repairs. Arthroscopy. 2022;38:38–48. doi: 10.1016/j.arthro.2021.05.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuff D.J., Pupello D.R., Santoni B.G. Partial rotator cuff repair and biceps tenotomy for the treatment of patients with massive cuff tears and retained overhead elevation: midterm outcomes with a minimum 5 years of follow-up. J Shoulder Elbow Surg. 2016;25:1803–1809. doi: 10.1016/j.jse.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Dilisio M.F., Neyton L. Comma sign–directed repair of anterosuperior rotator cuff tears. Arthrosc Tech. 2014;3:e695–e698. doi: 10.1016/j.eats.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eakin C.L., Faber K.J., Hawkins R.J., Hovis D.W. Biceps tendon disorders in athletes. J Am Acad Orthop Surg. 1999;7:300–310. doi: 10.5435/00124635-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Elser F., Braun S., Dewing C.B., Giphart J.E., Millett P.J. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581–592. doi: 10.1016/j.arthro.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 19.El-shaar R., Soin S., Nicandri G., Maloney M., Voloshin I. Superior capsular reconstruction with a long head of the biceps tendon autograft: a cadaveric study. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118785365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forsythe B., Zuke W.A., Agarwalla A., Puzzitiello R.N., Garcia G.H., Cvetanovich G.L., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodeses produce similar outcomes: a randomized prospective analysis. Arthroscopy. 2020;36:23–32. doi: 10.1016/j.arthro.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Friedman D.J., Dunn J.C., Higgins L.D., Warner J.J.P. Proximal biceps tendon: injuries and management. Sports Med Arthrosc Rev. 2008;16:162–169. doi: 10.1097/JSA.0b013e318184f549. [DOI] [PubMed] [Google Scholar]
- 22.Gill T.J., McIrvin E., Mair S.D., Hawkins R.J. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg. 2001;10:247–249. doi: 10.1067/mse.2001.114259. [DOI] [PubMed] [Google Scholar]
- 23.Green J.M., Getelman M.H., Snyder S.J., Burns J.P. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii without the use of interference screws. Arthroscopy. 2017;33:19–25. doi: 10.1016/j.arthro.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Han F., Kong C.H., Hasan M.Y., Ramruttun A.K., Kumar V.P. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: a biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105:257–263. doi: 10.1016/j.otsr.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 25.Hartwell M.J., Terry M.A. The Management of Biceps Pathology. Springer International Publishing; Cham: 2021. Arthroscopic versus open tenodesis: which patients need which? pp. 189–198. [Google Scholar]
- 26.Hermanowicz K., Góralczyk A., Malinowski K., Jancewicz P., Domżalski M.E. Long head biceps tendon—natural patch for massive irreparable rotator cuff tears. Arthrosc Tech. 2018;7:e473–e478. doi: 10.1016/j.eats.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ji J.H., Shafi M., Jeong J.J., Park S.E. Arthroscopic repair of large and massive rotator cuff tears using the biceps-incorporating technique: mid-term clinical and anatomical results. Eur J Orthop Surg Traumatol. 2014;24:1367–1374. doi: 10.1007/s00590-013-1323-x. [DOI] [PubMed] [Google Scholar]
- 28.Kim Y.S., Lee H.J., Park I., Sung G.Y., Kim D.J., Kim J.H. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim D., Um J., Lee J., Kim J. Improved clinical and radiologic outcomes seen after superior capsule reconstruction using long head biceps tendon autograft. Arthroscopy. 2021;37:2756–2767. doi: 10.1016/j.arthro.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 30.Kitridis D., Yiannakopoulos C., Sinopidis C., Givissis P., Galanis N. Superior capsular reconstruction of the shoulder using the long head of the biceps tendon: a systematic review of surgical techniques and clinical outcomes. Medicina (Kaunas) 2021;57:1–12. doi: 10.3390/medicina57030229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kocaoglu B., Firatli G., Ulku T.K. Partial rotator cuff repair with superior capsular reconstruction using the biceps tendon is as effective as superior capsular reconstruction using a tensor fasciae latae autograft in the treatment of irreparable massive rotator cuff tears. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120922526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lädermann A., Denard P.J., Barth J., Bonnevialle N., Lejeune E., Bothorel H., et al. Superior capsular reconstruction for irreparable rotator cuff tears: autografts versus allografts. Orthop Traumatol Surg Res. 2021;107(8S) doi: 10.1016/j.otsr.2021.103059. [DOI] [PubMed] [Google Scholar]
- 33.Lafosse T., Kopel L., Beckers J., Lafosse L. The 360 double lasso loop for biceps tenodesis: tips and tricks. Arthrosc Tech. 2021;10:e1889–e1895. doi: 10.1016/j.eats.2021.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loftis C.M., Kruse K. Single medial-row anchor with biceps tenodesis in a transosseous double-row construct for massive rotator cuff tear. Arthrosc Tech. 2022;11:e1447–e1452. doi: 10.1016/j.eats.2022.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lutton D.M., Gruson K.I., Harrison A.K., Gladstone J.N., Flatow E.L. Where to tenodese the biceps: proximal or distal? Clin Orthop Relat Res. 2011;469:1050–1055. doi: 10.1007/s11999-010-1691-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazzocca A.D., Bicos J., Santangelo S., Romeo A.A., Arciero R.A. The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis. Arthroscopy. 2005;21:1296–1306. doi: 10.1016/j.arthro.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 37.Mazzocca A.D., Rios C.G., Romeo A.A., Arciero R.A. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;21:896.e1–896.e7. doi: 10.1016/j.arthro.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 38.Mihata T., Lee T.Q., Watanabe C., Fukunishi K., Ohue M., Tsujimura T., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 39.Milano G., Marchi G., Bertoni G., Vaisitti N., Galli S., Scaini A., et al. Augmented repair of large to massive delaminated rotator cuff tears with autologous long head of the biceps tendon graft: the arthroscopic “Cuff-Plus” technique. Arthrosc Tech. 2020;9:e1683–e1688. doi: 10.1016/j.eats.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mirzaee F., Aslani M.A., Zafarani Z., Aslani H. Treatment of massive irreparable rotator cuff tear with arthroscopic subacromial bursectomy, biceps tenotomy, and tuberoplasty. Arch Bone Jt Surg. 2019;7:263–268. [PMC free article] [PubMed] [Google Scholar]
- 41.Nakata W., Katou S., Fujita A., Nakata M., Lefor A.T., Sugimoto H. Biceps pulley: normal anatomy and associated lesions at MR arthrography. Radiographics. 2011;31:791–810. doi: 10.1148/rg.313105507. [DOI] [PubMed] [Google Scholar]
- 42.Neviaser J.S. Ruptures of the rotator cuff of the shoulder. Arch Surg. 1971;102:483. doi: 10.1001/archsurg.1971.01350050049015. [DOI] [PubMed] [Google Scholar]
- 43.Pander P., Sierevelt I.N., Pecasse G.A.B.M., van Noort A. Irreparable rotator cuff tears: long-term follow-up, five to ten years, of arthroscopic debridement and tenotomy of the long head of the biceps. Int Orthop. 2018;42:2633–2638. doi: 10.1007/s00264-018-3991-y. [DOI] [PubMed] [Google Scholar]
- 44.Park H.J., Lee S.Y., Choi Y.J., Park J.H., Kim E. Association between subacromial impingement and acromiohumeral distance on MRI. Iran J Radiol. 2018;15:e13811. doi: 10.5812/iranjradiol.13811. [DOI] [Google Scholar]
- 45.Pill S.G., Walch G., Hawkins R.J., Kissenberth M.J. The role of the biceps tendon in massive rotator cuff tears. Instr Course Lect. 2012;61:113–120. [PubMed] [Google Scholar]
- 46.Rattee J., Sims L., Leswick D.A., Obaid H. Correlation between superior humeral head migration and proximal long head of biceps tendon pathology in patients with and without rotator cuff tears using magnetic resonance imaging and radiography. JSES Int. 2022;6:809–814. doi: 10.1016/j.jseint.2022.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rhee Y.G., Nam S.C., Chan T.L., Jin W.Y., Vishvanathan T. Bridging the gap in immobile massive rotator cuff tears: augmentation using the tenotomized biceps. Am J Sports Med. 2008;36:1511–1518. doi: 10.1177/0363546508316020. [DOI] [PubMed] [Google Scholar]
- 48.Rosenthal J., Nguyen M.-L., Karas S., Gottschalk M., Daly C., Wagner E., et al. A comprehensive review of the normal, abnormal, and post-operative MRI appearance of the proximal biceps brachii. Skeletal Radiol. 2020;49:1333–1344. doi: 10.1007/s00256-020-03415-x. [DOI] [PubMed] [Google Scholar]
- 49.Snow B.J., Narvy S.J., Omid R., Atkinson R.D., Vangsness C.T. Anatomy and histology of the transverse humeral ligament. Orthopedics. 2013;36:e1295–e1298. doi: 10.3928/01477447-20130920-23. [DOI] [PubMed] [Google Scholar]
- 50.Varacallo M., Seaman T.J., Mair S.D. StatPearls. StatPearls Publishing; Treasure Island, FL: 2024. Biceps tendon dislocation and instability. [PubMed] [Google Scholar]
- 51.Virk M.S., Cole B.J. Proximal biceps tendon and rotator cuff tears. Clin Sports Med. 2016;35:153–161. doi: 10.1016/j.csm.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 52.Walch G., Edwards T.B., Boulahia A., Nové-Josserand L., Neyton L., Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 53.Werner B.C., Evans C.L., Holzgrefe R.E., Tuman J.M., Hart J.M., Carson E.W., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis. Am J Sports Med. 2014;42:2583–2590. doi: 10.1177/0363546514547226. [DOI] [PubMed] [Google Scholar]
- 54.Werner A., Mueller T., Boehm D., Gohlke F. The stabilizing sling for the long head of the biceps tendon in the rotator cuff interval. Am J Sports Med. 2000;28:28–31. doi: 10.1177/03635465000280011701. [DOI] [PubMed] [Google Scholar]
- 55.Yeung M., Shin J.J., Lesniak B.P., Lin A. Complications of arthroscopic versus open biceps tenodesis in the setting of arthroscopic rotator cuff repairs: an analysis of the American Board of Orthopaedic Surgery database. J Am Acad Orthop Surg. 2020;28:113–120. doi: 10.5435/JAAOS-D-19-00252. [DOI] [PubMed] [Google Scholar]
- 56.Zhang Q., Zhou J., Ge H., Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23:464–469. doi: 10.1007/s00167-013-2587-8. [DOI] [PubMed] [Google Scholar]