Version Changes
Revised. Amendments from Version 1
The main changes involved:
Rewriting of the abstract to describe more clearly the project evaluation rather than the Kuteteza project itself
Clarification of the study aims and objectives and rationale for the approach, at various points in the manuscript
Rewriting of the discussion to ensure the main points are clearly communicated and to improve the flow of the section
Project materials (posters and leaflets) supplied as supplementary materials. Changes to the wording and layout of tables 2 and 3 to improve clarity Gender disaggregated data added to table 2 and the results section Use of the word shielding has been explained and the word put in quotations throughout the text The section about the FGD and other study tool has been moved to the relevant section Clarification around the intervention co-development Other minor changes in wording and organisation as recommended by reviewers
Abstract
Background
The COVID-19 epidemic in Malawi involved almost 90,000 recorded cases and 2,638 deaths. In response to early concerns about vulnerable older people in rural areas, we developed ‘Kuteteza’: a COVID-19 mitigation response project. Clinicians, public health professionals, and researchers collaborated with government and district-level staff in two Southern Malawi districts. Interventions included supported ‘shielding’ of older people – minimising social mixing whilst having their daily needs supported. Additional mitigation strategies included provision of masks, handwashing stations, and soap. Government partnerships allowed additional support for vulnerable groups. We present the findings of a realist project evaluation, assessing the feasibility of this approach.
Methods
We collated anonymised descriptive data on Kuteteza procedures and conducted qualitative structured observations in villages involved in the initiative. We carried out three focus groups involving community members, frontline health staff, and volunteers in each setting. These provided deeper insights into experiences of the pandemic and impacts of the intervention, including suggested opportunities during future outbreaks.
Results
The project involved 25 villages across two districts, with 1,087 people over the age of 60 voluntarily participating in ‘shielding’. Supplies of food, water, and cooking fuel were mostly arranged within the family. In Kuteteza villages, the handwashing stations and soap were widely used, and there was awareness and some observance of COVID-19 prevention measures. The project, including the provision of supplies, was greatly appreciated by communities, but wider contextual constraints – namely widespread economic insecurity – presented persisting challenges. Suggestions for improvement largely concerned project enhancements and extensions.
Conclusions
Through effective stakeholder engagement and contribution to national response strategy, the Kuteteza project helped raise COVID-19 awareness and supported populations at a critical time in the pandemic. Kuteteza approaches were welcomed locally and may be incorporated in future epidemic responses. Supported ‘shielding’ should be paired with government-led measures to mitigate economic hardship.
Keywords: Malawi, COVID-19, Community, Engagement, Public Health
Plain Language Summary
During the COVID pandemic in Malawi, cases were seen first and most often in the cities. Serious concerns were raised about how the pandemic might affect more rural populations, with poorer access to healthcare, greater income insecurity, and higher numbers of older adults (aged over 60 years). In an effort to prevent the worst of the expected impacts for older adults living in the villages, we formed a partnership of health workers, researchers, and policymakers, setting up the 'Kuteteza' response project (meaning ‘to protect’ in the Chichewa language).
The project worked with community members in 25 villages, supporting communities to enable 'shielding' of older adults: minimising their social mixing whilst also providing items such as handwashing stations, masks, food parcels and regular supplies of soap. Volunteers and health workers engaged with residents, spreading evidence-based information about COVID and feeding back community insights. This paper describes the results of a project evaluation – reporting numbers of villages and people involved, observations from participating villages, and insights from community members in focus groups.
One of the mains strengths of the project was in how the team worked together and with communities themselves, making sure actions were in line with national and regional policy and guidance and that it could quickly adapt to evolving needs as the pandemic progressed. We recommend these approaches for future responsive health projects, and present the outcomes of our evaluation for learning and discussion.
Introduction
Malawi saw its first cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in April 2020 1 : these constituted a small wave in July–August 2020, which was then followed by larger waves in January–February 2021, July–August 2021, and December 2021–January 2022 2 . Case numbers were relatively high with over a thousand cases per day at the height of the second and fourth waves, and over 85 000 confirmed cases nationally by February 2022 2 . Epidemiological patterns of the disease were like those seen in the rest of the world, with case severity and mortality rates in increasing with age, and higher in males than females 3, 4 .
The main disease epicentres in Malawi were the urban cities of Blantyre and Lilongwe, which experienced the highest numbers of confirmed cases, hospitalisations, and deaths from COVID-19, particularly in the first three waves. Of the 61 846 confirmed cases by November 2021, approximately 50% were in the cities of Blantyre or Lilongwe, with 46% of the 2302 confirmed deaths in Malawi from COVID-19 also occurring in these two cities 5 .
Following initial importations to Malawi and the spread through largely urban events, which drove the first wave, there was relatively more transmission to rural areas across the country in the third and fourth waves 3, 6 . Concerns here lay in the often-severe barriers to healthcare access in these regions as well as in the much greater presence of older adults in these areas, with over 90% of Malawi’s elderly population residing in rural communities 7– 10 .
In Malawi, the government implemented a coordinated multisectoral approach to COVID-19 response through establishment of operational clusters that comprised of multidisciplinary experts and development partners 11 . The protection cluster was specifically mandated to prevent and address the impacts of the COVID-19 outbreak through coordination and support to advocate for inclusion of specific rights, needs and vulnerabilities of susceptible groups including older adults 12 . This cluster was led and coordinated at the central level by the Ministry of Gender and UNICEF, and its activities were implemented in collaboration with various social protection partners at national, district and community levels. The cluster activities included providing policy guidance, risk communication and community engagement, and social protection support ( e.g., cash transfers, food items, and protective equipment) 13 . Whilst the overall objectives of the cluster included addressing the needs of older adults as one of the vulnerable groups, no specific activities targeting older adults were indicated or budgeted for in the first national COVID-19 response plan.
Public health approaches to preventing the spread of COVID-19 must be multifaceted and context-aligned for maximum effectiveness. One proposed element of such a public health approach is ‘shielding’: limiting the contact between those at high risk of developing severe disease (such as older adults) and the general population to reduce the number of severe cases in the population, thereby also protecting health systems from undue pressure 14– 16 . This could be arranged in various ways, such as at individual household or neighbourhood level, with the key elements of the approach including provision of adequate facilities and maintenance of minimum living standards for shielded individuals and the separate isolation of any potentially affected individuals away from others as soon as possible 17, 18 .
There has been some evidence on the ‘shielding’ of certain vulnerable groups, particularly early in national COVID-19 epidemics 18– 20 , but no global consensus on its role in the pandemic response. Controversies surrounding the use of ‘shielding’ in high-income countries have occurred due to concerns around the exclusion of the most vulnerable, and serious consequences of increased spread in settings where large numbers of high-risk individuals are brought together 21 . It is therefore evident that any adoption of ‘shielding’ approaches must be carefully considered, locally contextualised, and must only be implemented in a fully participatory way with empowered community engagement throughout 22 .
Expert guidance on the subject from the Social Science in Humanitarian Action Platform (SSHAP) partnership 18 emphasises the need for situational adaptation to allow co-development of any such interventions, together with community members; the importance of informed choice, with the option to ‘shield’ being open to individuals and their families and households; and the need for cross-sectoral management throughout. They recommend that ‘shielding’ should be part of a wider response that ensures basic water, sanitation and hygiene (WASH) facilities, COVID-19 awareness and services, safeguarding, and data collection to allow the assessment of any benefits and potential risks 18 .
‘Kuteteza’ (meaning ‘to protect’ in vernacular Chichewa) was a project using community engagement and participation in villages across two districts of Southern Malawi, to combine ‘shielding’ approaches with wider COVID-awareness, and provision of WASH and basic facilities for those in most need. In building a coordinated response involving researchers, environmental, Public health, and government teams, and community members on the ground, we developed an engaged, multi-component approach to protecting those potentially most at risk in the population from the direct and indirect harms of COVID-19 in Malawi.
In this study, we evaluated the feasibility of the use of a mitigation response strategy that included supported ‘shielding’ - minimising social mixing whilst having daily needs supported by social networks - for older adults in rural Malawian communities in the context of the COVID-19 pandemic response. We present the findings of a realist evaluation of these approaches incorporating quantitative and qualitative components.
Methods
Setting and study population
The project engaged with stakeholders at three tiers: national, district, and community levels. Nationally, we collaborated with the Department of Disability and Elderly Affairs and engaged with the Ministry of Health, through various national committees involved in the COVID-19 response. At the district level we worked particularly in Blantyre and Mangochi districts, both in the Southern region of Malawi, engaging with existing District Health Organisations, contributing to regular fora and responding to expressed needs at this level. In view of the responsive nature of the project to the emerging pandemic, districts selected for inclusion were on the basis of existing research and organisational networks, to allow effective engagement with health systems and rapid project rollout.
Blantyre, the economic capital of Malawi, has a population of about 800,264 and a relatively high population density compared with other cities in the county. Mangochi district, also in southern Malawi, has a mostly rural economy driven by agriculture and tourism, with an adult population of around 516, 976 10 . At the community level, we worked in twenty villages across Blantyre, located in rural areas outside the city limits. Mangochi district, has a mostly rural economy driven by agriculture and tourism, with a population of around 610,239. Here, the intervention focused on five villages surrounding the district’s town centre. In both districts, community members worked with project volunteers to identify residents over the age of 60 who – with their consent – were then included for (voluntary) participation in the study.
COVID response project
The project involved three phases, described below.
Phase 1 - A cross-sectional mapping exercise of COVID-19 stakeholders at national and district levels. This helped us to understand the need for a COVID-19 response in rural areas, with particular attention to protecting those with a high risk of severe outcomes. Identification of key individual and institutional stakeholders also helped us to ensure the programme of activities was contextually relevant and coordinated within wider public health and COVID response work taking place in Malawi at the time.
Phase 2 - Co-development and implementation of the Kuteteza package, together with community representatives and health workers. The intervention involved mitigating population-level morbidity and mortality from COVID-19 disease in rural areas of Malawi through a programme of supported ‘shielding’ with the assistance of community health workers, known in Malawi as Health Surveillance Assistants (HSAs), and village volunteers.
The Kuteteza programme included the following activities:
Preparatory work, training local volunteers in community engagement approaches and COVID*19 information and building communication links in each district between researchers, HSAs and volunteers.
Awareness-raising involving spreading of basic, evidence-based COVID-19 information through posters and leaflets in public spaces.
Voluntary self-identification of older people in each village – defined as those aged over 60 years – wishing to participate in the programme.
Supported rearrangement of living spaces for these individuals and provision of basic necessities (food, water, etc.), to allow ‘shielding’ within a household area, minimising contact with the rest of the community. The two above steps were implemented across the whole study area following a local pilot in one village, with small adaptations as necessary prior to rollout.
Provision of handwashing stations (Veronica buckets) to all ‘shielding’ households and regular provision of soap for use at these stations.
Provision of face masks to public, for use in public transportation, health clinics, etc.
Liaison with government departments and national committees to target available emergency resources (food packages) to most vulnerable residents in participating villages.
Phase 3 – Evaluation of the interventions using both qualitative and quantitative approaches. Results of this evaluation are described in the current paper.
Evaluation study design
We utilised a case study approach to qualitative inquiry to help us understand experiences of the ‘shielding’ initiative, identify any challenges, strengths and potential areas for improvement. A prospective ecological evaluation of the implementation was used to collect information on the process and outcomes, including understandings around COVID-19 and community and individual-level actions aimed at COVID-19 risk reduction. Details of evaluation methods are provided below.
Data collection
Quantitative data
Team members compiled an anonymised listing of village residents aged over 60 years who participated in ‘shielding’. For each participant, we collected information on proposed ‘shielding’ arrangements and on arrangements for the provision of basic necessities (food, water, medicines, etc.) and alternative care for dependents, such as infants, where necessary.
Aggregated data on the total numbers of suspected and confirmed cases of COVID-19 among individuals entering the project were collected through HSAs. We also collated data on the number of community engagement activities conducted and quantities of items distributed to measure uptake of the strategy and other approved interventions ( e.g., use of masks) in the community.
Qualitative data
Assessment methods included structured observations in each district and village, and district level focus group discussions (FGDs), involving residents, community volunteers and health surveillance assistants. Participant recruitment began on 20 th September 2021 and data collection started later in the same week, on 24 th September.
Table 1 summarises the qualitative tools and areas of evaluation.
Table 1. Summary of qualitative data collection tools and their aimed areas of evaluation.
FGD, focus group discussion; HSA, Health Surveillance Assistant.
| Activity | Participants and details | Topic areas |
|---|---|---|
| Structured observations | Assessments carried out on walks around village,
incorporating key sites in the village and events – e.g. schools, places of worship |
COVID-19 risk reduction actions underway in village
environment: - Presence of Ministry of Health approved information and awareness materials - Availability of handwashing stations around the village - Mask wearing amongst residents and others. Following of additional COVID-19 prevention guidance |
| Village level focus groups
(Two in each district – four in total) |
Village residents – including older and
younger members of the community (12 participants per FGD) |
Communities’ perceptions around COVID-19 risks and
responses taken, considering influence of the Kuteteza project in shaping these Assessment of intervention approaches and implementation including strengths, challenges, and opportunities for improvement |
| District level focus groups
(One in each of the two districts) |
District HSA teams, health volunteers, and
village chiefs (9–12 participants per FGD) |
Assessment of intervention, approaches, and
implementation, including strengths, challenges, and opportunities for improvement |
The focus group discussion (FGD) guide, additional data collection tools, participant information sheets and consent forms can be found as Extended data 23 .
Ethical considerations
The original project was a piece of responsive public health work. ‘Shielding’ was implemented as part of the public health response to COVID-19, in close collaboration with the Ministry of Health and local health authorities. Participation in ‘shielding’ elements was voluntary, and no information was required from those who opted into ‘shielding’, other than access to anonymised population level data. In terms of the qualitative evaluation, focus group participants were required to provide written informed consent, which was collected by trained field workers, and all data and documents were kept under the custody of the principal investigator in a locked cabinet, located in a restricted-access area. A named safeguarding lead was in place throughout the project, with various avenues of contact for participants to report any concerns, and structures for appropriate referral of any such reports. The project was sponsored and approved by the local ethics committee (College of Medicine Research Ethics Committee; COMREC) in Blantyre, Malawi (P.01/21/3246) on 7 th July 2021.
Data analysis
Quantitative data
Data collected through dedicated, pre-tested, paper-based case report forms designed by the research team were entered onto an electronic database by dedicated data clerks. Descriptive analysis was conducted using R 24 . Categorical variables are expressed as totals and percentages, while continuous variables are expressed as means, and defined by 95% confidence interval and standard deviation.
Qualitative data
Focus groups were conducted in Chichewa and facilitated by Malawian research team members. All focus groups were audio recorded (with consent from participants) and subsequently transcribed and translated into English by research assistants prior to uploading onto NVIVO for analysis by three members of the research team 25 While researchers had institutional access to NVIVO, an free, open-source alternative - Taguette – is also available. Observation notes were also translated and entered onto NVIVO for analysis. Reflexive thematic analysis was used for analysing all the qualitative data as it is a well-described method and relatively easy for multiple researchers to work on together (with discussions of themes and codes as they developed) 26 . Its theoretical flexibility also made it suitable for the current evaluation, with multiple sub-questions under investigation and different data sets from the two data collection methods used. Researchers created initial codes, then brought these to a group discussion for development and refinement and co-development of key themes with reference to the original data.
All qualitative and quantitative data were anonymised to preserve participants’ confidentiality and held on secure systems with access limited to only the necessary subset of researchers.
Reflexivity statement
The reflexivity statement can be found as Extended data 23 .
Results
Quantitative findings
A total of 1,640 individuals across 20 villages in Blantyre and 5 villages in Mangochi identified themselves as being over the age of 60 ( Table 2). This included 1,138 individuals in Blantyre (69.4%) and 502 in Mangochi (30.6%). Of these, 1,087 – 746 in Blantyre (68.6%) and 341 in Mangochi (31.2%) – agreed to participate in ‘shielding’ ( Table 3).
Table 2. Summary of participants in Blantyre and Mangochi.
| BLANTYRE | MANGOCHI | |
|---|---|---|
| Total villages | 20 | 5 |
|
Total individuals
shielded |
746 | 341 |
|
Total individuals
with data available |
478 | 267 |
| Mean age | 75 (95% CI:
73.2–77.4, sd 8.8) |
72.3 (95% CI
71.2–73.4; sd 9.0) |
| Gender | Female 64.6%
Male 34.4% Unknown 1.0% |
Female 55.9%
Male 43.0% Unknown 1.1% |
Table 3. Summary of provision arrangements across Blantyre and Mangochi.
| WATER (n (%)) | FOOD (n(%)) | MEDICINES * (n(%)) | FIRE/FUEL (n(%)) | |||||
|---|---|---|---|---|---|---|---|---|
| Blantyre | Mangochi | Blantyre | Mangochi | Blantyre | Mangochi | Blantyre | Mangochi | |
| Adult family member | 157 (32.8) | 184 (68.9) | 158 (33.1) | 190 (71.2) | 39 (39.4) | 65 (94.2) | 153 (32.0) | 185 (69.3) |
| Adult non-family member | 0 | 1 (0.3) | 0 | 1 (0.03) | 3 (3.0) | 0 | 0 | 1 (0.3) |
| Child family member | 261 (54.6) | 16 (6.0) | 250 (52.3) | 19 (7.1) | 41 (41.4) | 3 (4.3) | 256 (53.6) | 16 (6.0) |
| Child non-family member | 0 | 1 (0.3) | 1 (0.2) | 1 (0.3 | 0 | 0 | 0 | 0 |
| Unknown | 60 (12.6) | 65 (24.3) | 69 (14.2) | 56 (21.0) | 16 (16.1) | 1 (1.4) | 69 (14.4) | 65 (24.3) |
* 99/478 in Blantyre and 69/267 in Mangochi known to need medicines
Individual-level data were available for 478 individuals (64.1%) from Blantyre and 267 (78.3%) from Mangochi. The majority of the participants were female in both districts (61.3% overall), although gender participation was slightly more balanced in Mangochi than in Blantyre ( Table 2). Of these, the mean participant age was 75 years in Blantyre and 72.3 in Mangochi. A total of 99 participants (20.7%) from Blantyre and 69 (25.8%) from Mangochi needed medication to treat chronic conditions ( Table 3), and 471 (98.5%) and 239 (89.5%) participants in Blantyre and Mangochi respectively, had dependents under their care ( Table 4).
Table 4. Summary of care arrangements for dependents of shielded individuals across Blantyre and Mangochi.
| DEPENDENTS (n (%)) | ||
|---|---|---|
| Blantyre | Mangochi | |
| Remain with shielded person | 355 (98.6) | 238 (94.8) |
| Made other arrangements | 5 (1.4) | 12 (4.7) |
360/478 in Blantyre and 251/267 in Mangochi had dependents
The uptake of ‘shielding’ varied by village, ranging between 32.8% and 100% across villages in Blantyre and between 45.7% and 98.8% in Mangochi villages ( Figure 1). Across both settings, supplies of food, water, and fuels such as charcoal or firewood for the cooking fire were mostly arranged within the family. Still, there were important differences between the districts in this area. While in Mangochi, water, food, and fuels were supplied by adult family members in approximately 70% of cases, and medicines in 94.2% of those who required them, in Blantyre most supplies were arranged by children in the family. In more than 50% of participant households in Blantyre, children had responsibility for supplying basic necessities to the ‘shielding’ individuals, including medicines.
Figure 1.
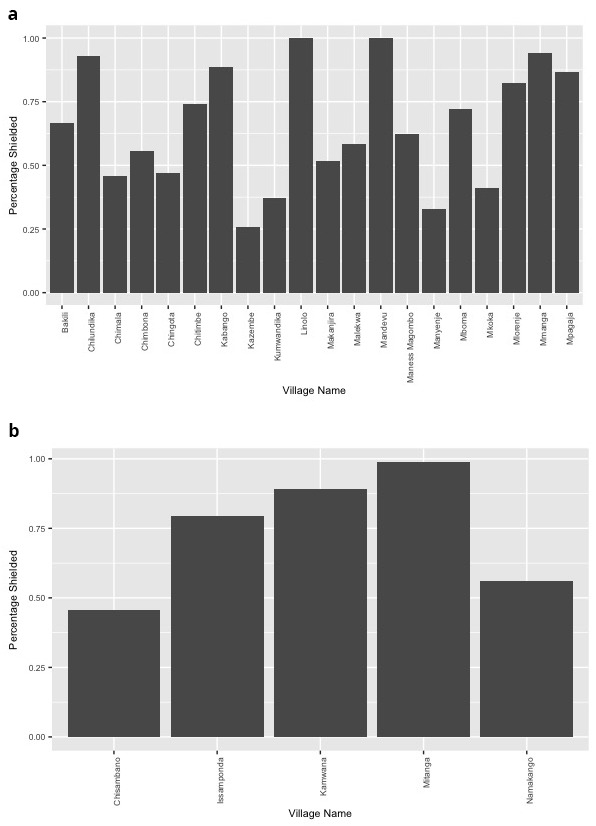
Percentage of eligible individuals that participated in ‘shielding’ during the COVID-19 pandemic across villages in Blantyre ( a) and Mangochi ( b).
Throughout the duration of the pilot, 120 individuals in the ‘shielding’ scheme presented with symptoms compatible with COVID-19 and were tested for the disease: 102 in Blantyre and 18 in Mangochi. Among these, 2 cases were confirmed in one village in Blantyre. Both cases resulted in death. There were a total of 28 deaths among those ‘shielding’ in Blantyre, including those caused by COVID-19, and 30 in Mangochi. As these data were collected in an aggregated form to protect the privacy of villagers, it was not possible for researchers to disaggregate these findings further.
Qualitative findings
Observations
Observations revealed that stations were available and in use at most households, although the regularly distributed soap bars were less ubiquitous. Questioning revealed that these tended to run out quickly as they were used in households for purposes other than handwashing ( e.g. laundry). Masks tended to be worn when traveling outside the village, to the health centre for instance, but were seen much less during day-to-day life within the village. An exception to this was in gatherings, where some adults wore masks. Gatherings were mainly outdoors, and a degree of ‘social distancing’ was also seen in some places such as schools. Handshakes (usually important in Malawian tradition) were replaced for many but not all, by fist/elbow bumps as a concession to COVID guidance. Researchers conducting observations did not find ‘COVID awareness’ materials (posters and leaflets provided by the project) on display in public areas in either of the districts, although volunteers were seen wearing branded T-shirts in both districts.
Focus groups
General perceptions of the project
When asked about the project in general there were positive responses from focus group members including residents, community leaders, and health volunteers in the villages where the project took place. Focus group participants expressed gratitude for the awareness spread by the project of COVID and prevention measures, but particularly for the resources – handwashing buckets, soap, and masks required for communities to protect themselves against COVID.
“The people understood the project … when they came and gave the elders those pails and soap it is when it showed that this project is helpful. So, it also encouraged other people including the elders… plus looking at the other things brought up like maize flour and relish, it gave encouragement that these people are taking care of the elders.”
Health volunteer, district level focus group, Mangochi
“P 10: We just want to thank you, thanks a lot. In the village we face a lot of challenges so don’t stop, continue, thank you.
P 3: We thank you because some people just speak but you have given us like masks, soap, buckets.
P 8: We thank this organization that you have listened to our problems and you will pass (on) the message
P 6: We thank you because nowadays even at the funeral when they see a bucket, they wash their hands unlike in the past.”
Local residents, village level focus group, Blantyre
Perceived benefits of the project
As indicated above, the elements of the project most positively commented upon were the addition of resources, over and above the awareness-raising and information components of the project. Focus group participants clearly explained how provision of these resources – soap, handwashing buckets, masks, and provision of food parcels for a subset of the most vulnerable through a government initiative – made it possible to enact the widely recommended COVID prevention measures.
“Even for us who are taking care of the elderly people, it is a great thing that you are giving us soap, it is hard to have soap in the village … it could have been difficult for us to also buy soap, the price of soap nowadays has gone up”
Resident carer for an older adult family member, village level focus group, Blantyre
“that time they started giving the food baskets it was helpful that the person will know when I eat this, I will do this”
Health volunteer, district level focus group, Blantyre
Suggested changes to the project
Alongside an appreciation for the various resources provided, there were frequent calls for more of these resources. Residents raised the issues of buckets breaking requiring replacement, and soap which was insufficient for all the purposes for which it was used.
This linked with a wider issue, again cited by many community members, volunteers, and staff, of a general scarcity of resources, which added complexity to the work of the project. A particular aspect of this, cited by many, was that of food security for older adults who were being encouraged to ‘shield’ in their homes.
“when you take soap and you give them, you find that the whole day she hasn’t eaten anything the whole day, and you say ‘here is the soap’”
Health volunteer, district level focus group, Blantyre
Many focus group participants proposed donations of food and other resources to support the ‘shielding’ older adults:
“the elders were saying … apart from the fact that you are giving us soap, pails, but food is also needed in this moment since we are not travelling”
Health volunteer, district level focus group, Mangochi
“Considering that some elders do not have guardians and they have maybe a small (vegetable garden) or a field, right. So maybe there could be a plan to give them fertiliser and seeds, since maybe it is hard to give them maize flour... so that they might eat in the future.”
Health volunteer, district level focus group, Mangochi
It was apparent from residents’ narratives how food insecurity prohibited some elderly individuals from ‘shielding’. In a context where insecurity was common, not all elderly residents had a named carer to consistently support their daily needs as intended in the project plans. In some cases, older people themselves had responsibility for their grandchildren, thus staying at home for protection against COVID presented additional problems. An older adult community member explained:
“…we are staying from morning without any food. With the money problem, you would search in the house and say, in the past I would keep money in here, maybe K20, and a school child is asking you ‘granny, give me K50 so I should buy freezes at school’, and you tell them, ‘where do I get it? I don’t have (money), I am just living without doing anything.’ … there are elders just staying, some do not have children, some lost their children, they don’t have anyone to assist them.”
Older adult community member, village level focus group, Mangochi
While the government partnership that enabled food packages to be delivered to some of the most vulnerable individuals was acknowledged, in reality many of the older adults involved in the project experienced economic scarcity and did not receive this support.
It was striking that this insecurity was not limited to older adults. Carers also brought up the need for food to support themselves in their work. One resident carer in Blantyre explained: “You have not eaten, then you will say am tired of caring for the patient because the body is weak.”
Volunteer recommendations
In focus groups, community volunteers, who were not paid for their time but received mobile phone credit to assist in their work, frequently requested more ‘benefits’ of various types, for their work on the project. Requested benefits included soap and buckets, as older adults received. One volunteer, in a village level focus group in Mangochi, stated: “I think the volunteers should also have buckets … they are supposed to lead by example”. Another, in Blantyre suggested, “like us volunteers, we distribute soap and we receive airtime … but we need also soap so that we can wash”. Other suggestions for benefits included mobile telephones to further aid communication and bicycles to fetch medicines or transport older adults to health centres, should this be necessary. Finally, there were suggestions of incentives such as refreshments during training sessions, and more high-profile venues for the sessions. As one focus group participant explained: “in Chichewa they say if you want the cow to give you more milk, you have to give enough food so that it can give good milk”.
The second category of recommendations from those involved in the running of the project was an extension to the scope of the project, in terms of participants, staff, and villages involved. Inclusion criteria were questioned by a few, who clearly valued the benefits afforded by the project so highly that issues of equity around which populations were involved were seen as very important. A member of a district level focus group explained: “There are 5 pilot villages. There are so many villages complaining that they also have grandparents who are just staying and struggling, they are also old they also need that same assistance.” Greater clarity around the selection process was a further recommendation from a few participants. This also applied to the selection of the subset of participants deemed particularly vulnerable, and to whom government food parcels was distributed.
“the distribution of that food: the list was shortlisted and some were left out but they were supposed to give to everyone or five kgs to each and everyone could be happy. The list was shortlisted and still other people are still complaining, so this could sorted: it’s better that they should be given 5kgs but everyone should be given, that’s all.”
Health volunteer, district level focus group, Blantyre
Further suggestions regarded the inclusion of those with certain chronic illnesses, and of additional volunteers, to cover wide geographical areas more easily.
Discussion
In this study, we aimed to evaluate the feasibility of a COVID-19 prevention and awareness initiative, engaging communities throughout, to optimise protection for those most vulnerable to the disease. The initiative included community engagement activities aimed at community health workers and village residents, the distribution of basic WASH items, namely, bucket-hand washing stations and regular soap supply, and the promotion of a voluntary ‘shielding’ strategy among those aged 60 and over to minimise exposure to the virus amongst those at greatest risk.
The initiative was widely taken up in both of the districts in which it was implemented, with more than half of residents in the majority of the villages opting into ‘shielding. This ‘shielding’ required arrangements to ensure basic needs were covered through a designated carer arranged by families and communities themselves: responsibilities which in a proportion of cases were taken on by children of the household.
Qualitative evaluation found the project to be well-received amongst community members, with a range of positive feedback. The project successfully foregrounded community participation and local partnerships in its approach. A key challenge was that of structural limitations inherent to the setting – largely related to financial scarcity – which at times made it difficult for participants and volunteers to fully engage with plans.
Economic challenges in these settings were foremost in the minds of participants. While individuals were grateful for the intervention and keen to be involved, food and fuel insecurity and related issues restricted their capacity to effectively shield. This scarcity was also reflected in the response to resources supplied: even soap provided for handwashing tended to run out quickly as it was used for a variety of household purposes, and participants commonly requested that the project extend to supply food or financial support.
Volunteers’ perspectives reflected these issues. Economic incentives (and the provision of material items) were often cited as recommendations for improving the work of volunteers engaged with the project, highlighting that volunteers were operating within the same settings and subject to the same environmental stressors as other community members.
The challenges brought by COVID in Malawi, on a background of extreme scarcity and already-stretched health systems, related in part to managing the COVID disease burden whilst also mitigating its indirect economic and social effects 11 . There is ample evidence of the COVID-related impacts on livelihoods and commodity prices, and subsequent food insecurity 27, 28 . Results of a national survey found that 82% of participants feared going hungry following COVID-related loss of income and price impacts 29 . Malawi also experienced worsening of various health and social outcomes due to COVID including mental health conditions, suicide, teenage pregnancy, and gender-based violence 30 . Participants of a qualitative study in Somalia felt the indirect economic and social outcomes to be the main impact of the pandemic 31 : a perspective echoed in participants’ responses in Malawi.
To mitigate the worst of the indirect effects of COVID, the Malawi government put in place an expanded programme of cash transfers and related financial safety nets, and a stringent national ‘lockdown’ was resisted 11, 30 . Whilst the financial measures did have a protective effect, a recent evaluation asserted that a scaling up of such measures was required to further protect at-risk populations in Malawi 28 .
Coetzee & Kagee use the theoretical domains framework to describe how ‘environmental context’ constrains individuals’ abilities to adhere to COVID prevention measures such as social isolation in low- and middle-income countries 32 . This also explains how immediate concerns such as finding food and income are prioritised above seemingly less important threats such as that of COVID. The medical anthropology literature even before COVID sheds further light on tensions between underlying structural limitations and individual medical concerns. In a landmark paper, Kalofonos powerfully exposes the challenges arising during the external provision of medical solutions (antiretroviral medications for HIV) in an environment characterised by food insecurity in Mozambique, highlighting the social risks of overlooking deeper inequities in health and wellbeing whilst exclusively tending to specific medical concerns. In terms of COVID specifically, Stoler and colleagues have revealed how water insecurity in 23 countries compromised COVID responses, accentuating existing inequalities.
The Kuteteza project – incorporating a team of Malawian and international colleagues and working in partnership with national and district level structures in Malawi – made efforts to take these wider contextual factors into account throughout its planning and implementation. Despite limited resources, provision of basic resources alongside health messaging was prioritised, and cooperation with the Malawi government allowed for food packages and additional resources to be targeted to optimise equitable distribution. In this context however, the available resources proved insufficient to cover the extent of the need within communities.
Singer and Rylko-Bauer, describing the direct and indirect impacts of COVID in terms of structural violence, highlight the need for global health approaches with an “orientation toward prevention and preparation”, which address wider health determinants 33 . Key to this is a move to real solidarity in the field of global health: attention to underlying inequities as well as ad hoc responses to emerging health issues. This is the global health challenge of our times.
To the authors’ knowledge, this is the first example of a community-led ‘shielding’ strategy arranged by and sustained within the community themselves 34 . However, our work revealed an unintended impact of the initiative. In Blantyre, care for the shielded older adult was delegated to a child family member in more than half of all cases, while in Mangochi child carers were in the minority. In both districts, minor dependents who were under the care of a shielded individual remained under their care out of necessity. The key difference was that in Blantyre, the economic capital of Malawi, low-skilled adults from rural villages often travel outside the village to find work, leaving children under the care of the older adult family members. In contrast, the economy of Mangochi, a rural setting, revolves around the lakeshore, making it more feasible for adults in the area to remain in their village 35 . This finding strongly emphasises the need to carefully consider a holistic approach when responding to public health emergencies, and anticipated the impact that such initiatives can have for dependent minors when they are left under the care of an individual who can become vulnerable in situations such as the COVID-19 pandemic.
Future pandemic preparedness plans would benefit from taking into consideration the impact of both the disease itself on the directly affected populations, and the vulnerability of those who might be left to bear the unintended consequences. Had the COVID-19 pandemic hit Malawi with the severity anticipated by early models, minors under the care of the older adult could have suffered from the loss of a main carer, while separated from parents who might not have been able to return if movement restrictions were in place 36, 37 . These complexities demonstrate the need for ongoing engagement with communities throughout all stages of pandemic preparedness planning and response to anticipate such unintended effects.
Strengths and limitations
The community-rooted nature of the project, with simple, clear messaging, and implementable recommendations (paired with the necessary resources) were a key strength of the Kuteteza project. These factors were positively reported on by participants and are and in keeping with calls in the literature for public engagement and achievable health advice to facilitate adherence 11, 32 .
The work faced two main limitations in regards of data collection. From the implementation perspective, and given the voluntary nature of ‘shielding’, it was not possible to evaluate how faithfully participants adhered to the recommendation of limiting their social mixing. While participants were grateful for the provision of buckets and soap, and adherence to their use was evidenced through observation, we could not confirm whether participants were indeed ‘shielding’.
While the number of individuals presenting with symptoms compatible with a SARS-COV2 diagnosis was low, and only two cases were confirmed among our target population, we cannot ascertain to what extent ‘shielding’ contributed to the low case load. Limitations in our data collection procedures also mean it is possible for cases to have been missed. In the project, cases were identified through records held by HSAs, who are trained in data collection procedures and trusted amongst community members 38 making case recording largely accurate, but national serological surveillance has revealed a SARS-COV2 circulation much greater than that reported 39 . Colleagues have reported that up 85% of participants recruited within a Malawian cohort with positive SARS-COV2 serology were asymptomatic 40 . This suggests – in line with serological studies and national data – that the number of symptomatic cases among shielded individuals in our intervention was likely to have been low, with total infections under-reported in our study 39, 41 . Higher than reported circulation of the virus would also advocate for the implementation of strategies to restrict exposure of susceptible, high-risk individuals in the event of the emergence of new SARS-COV2 variants, in conjunction with other medical and non-medical interventions.
Conclusions
In the event of health emergencies, involving communities and local health structures in initiatives that contribute to their protection can effectively raise awareness, ensure the spread of scientifically-sound information and advice, as well as ensuring that preventative measures are locally appropriate and feasible. However, the design of any community-led initiative needs to be carefully considered to ensure that protecting those vulnerable to the emerging threat does not result in unintended harms within communities. In this work we witnessed how selective lockdowns in rural communities in Malawi could have resulted in children being left with the burden of having to care for older adult relatives, for example.
Community health workers are trusted healthcare workers with often high levels of influence among those they serve and were instrumental in facilitating the implementation of this work. We would recommend their involvement in future community-based health preparedness and response plans, whilst noting that they may often face the same difficulties as those in their local communities and must also have their health, economic, and wider needs met as far as possible. Likewise, enhancing the use of community-based health interventions through the integration of community volunteers can also prove an invaluable tool in the prevention and early detection of health emergencies.
Finally, this project evidences the critical role of understanding local contexts in terms of pre-existing and continuing challenges experienced by communities through their daily lives. Health and development interventions – even those in emergency settings such as infectious disease outbreaks – would be strengthened by attention to, and action on, these factors.
Ethics and consent
The original project was a piece of responsive public health work. ‘shielding’ was implemented as part of the public health response to COVID-19, in close collaboration with the Ministry of Health and local health authorities. Participation in ‘shielding’ elements was voluntary, and no information was required from those who opted into ‘shielding’, other than access to anonymised population level data. In terms of the qualitative evaluation, focus group participants were required to provide written informed consent, which was collected by trained field workers, and all data and documents were kept under the custody of the principal investigator in a locked cabinet, located in a restricted-access area. A named safeguarding lead was in place throughout the project, with various avenues of contact for participants to report any concerns, and structures for appropriate referral of any such reports. The project was sponsored and approved by the local ethics committee (College of Medicine Research Ethics Committee; COMREC) in Blantyre, Malawi (P.01/21/3246) on 7 th July 2021.
Acknowledgements
With thanks to members of the original Kuteteza group – Moses Kumwenda, Elizabeth Corbett, Peter MacPherson, Ken Maleta, and Dianne J Terlouw – for their roles in shaping the first iterations of the project.
Funding Statement
This work was supported by the MLW Wellcome Trust Institutional Translational Partnership Award (WT-iTPA) Seed Grant Malawi-Liverpool Wellcome Trust Director’s Discretionary Fund [206545].
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 2; peer review: 3 approved]
Data availability
Underlying data
The quantitative and qualitative data supporting the conclusions of this article are not publicly available due to confidentiality concerns. Limited data may be made available on individual request via email to the corresponding author, with requests for additional data evaluated by the principal investigator on a case-by-case basis.
Extended data
Harvard Dataverse: 'Kuteteza' project - additional documents. https://doi.org/10.7910/DVN/AKVXEC 23
This project contains the following extended data:
Reflexivity statement
Focus group discussion guide
Additional data collection tools
Participant information sheets and consent forms
Information materials used in the project
Data are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
References
- 1. Safary E, Mtaita C: COVID – 19 Pandemic in Malawi. Afr J Health Sci. 2020;33(6). Reference Source [Google Scholar]
- 2. Worldometer: Malawi coronavirus cases. Worldometer,2022; [cited 2022 21st February]. Reference Source
- 3. Nyasulu JCY, Munthali RJ, Nyondo-Mipando AL, et al. : COVID-19 pandemic in Malawi: did public sociopolitical events gatherings contribute to its first-wave local transmission? Int J Infect Dis. 2021;106:269–75. 10.1016/j.ijid.2021.03.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Statistical Office: Malawi in figures. 2020 Edition. Lilongwe: Government of Malawi,2020. [Google Scholar]
- 5. Ministry of Health - MW: COVID-19 National Information Dashboard. Minstry of Health, Malawi,2021; [cited 2021 17th November]. Reference Source
- 6. Ministry of Health - MW: COVID-19 National Information Dashboard. Minstry of Health, Malawi,2022; [cited 2022 21st February]. Reference Source
- 7. Msokwa R: Improving access to health services in Malawi. South East Eur J Public Health. 2021;2. 10.11576/seejph-4383 [DOI] [Google Scholar]
- 8. Varela C, Young S, Mkandawire N, et al. : Transportation barriers to access health care for surgical conditions in Malawia cross sectional nationwide household survey. BMC Public Health. 2019;19(1): 264. 10.1186/s12889-019-6577-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ritter R: Access and barriers to health care services in rural Malawi. Bonn, Germany: University of Excellence Bonn,2021. Reference Source [Google Scholar]
- 10. National Statistical Office (NSO): 2018 Malawi Population and Housing Census. Malawi National Statistical Office (NSO),2018. Reference Source
- 11. Mzumara GW, Chawani M, Sakala M, et al. : The health policy response to COVID-19 in Malawi. BMJ Glob Health. 2021;6(5): e006035. 10.1136/bmjgh-2021-006035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Government of Malawi: National COVID-19 Preparedness and Response Strategy and Plan: July 2021 - June 2022. Lilongwe, 5th August,2021. Reference Source
- 13. UNICEF: UNICEF Malawi COVID-19 Situation Report 15 April. Lilongwe, Malawi: UNICEF, 15th April,2020. Reference Source
- 14. LSHTM Health in Humanitarian Crises Centre: COVID-19 response. London School of Hygiene & Tropical Medicine,2021; [cited 2021 17th November]. Reference Source
- 15. Schwalbe N, Lehtimaki S, Gutiérrez JP: COVID-19: rethinking risk. Lancet Glob Health. 2020;8(8):e974–e5. 10.1016/S2214-109X(20)30276-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dahab M, van Zandvoort K, Flasche S, et al. : COVID-19 control in low-income settings and displaced populations: what can realistically be done? Confl Health. 2020;14: 54. 10.1186/s13031-020-00296-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention: Operational Considerations for Humanitarian Settings. CDC,2020; [cited 2021 17th November]. Reference Source
- 18. Social Science in Humanitarian Action Platform: Considerations and principles for shielding people at high risk of severe outcomes from COVID-19 (April 2020). SSHAP,2020. Reference Source
- 19. Abdelmagid N, Ahmed SAE, Nurelhuda N, et al. : Acceptability and feasibility of strategies to shield the vulnerable during the COVID-19 outbreak: a qualitative study in six Sudanese communities. BMC Public Health. 2021;21(1): 1153. 10.1186/s12889-021-11187-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Zandvoort K, Jarvis CI, Pearson CAB, et al. : Response strategies for COVID-19 epidemics in African settings: a mathematical modelling study. BMC Med. 2020;18(1): 324. 10.1186/s12916-020-01789-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sridhar D, Rafiei Y: The problem with 'shielding' people from coronavirus? It's almost impossible. The Guardian. 29th May 2020; Sect. Opinion,2020. Reference Source
- 22. Gilmore B, Ndejjo R, Tchetchia A, et al. : Community engagement for COVID-19 prevention and control: a rapid evidence synthesis. BMJ Glob Health. 2020;5(10): e003188. 10.1136/bmjgh-2020-003188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Saleh S: 'Kuteteza' project - additional documents. DRAFT VERSION ed: Harvard Dataverse; [Dataset],2024. 10.7910/DVN/AKVXEC [DOI]
- 24. R Core Team: R: A Language and Environment for Statistical Computing. Vienna, Austria,2020. Reference Source
- 25. Ltd QIP: NVivo (released in March 2020).2020.
- 26. Braun V, Clarke V: Thematic Analysis Auckland. New Zealand: University of Auckland,2022; [cited 2022 19th May]. Reference Source [Google Scholar]
- 27. Dzimbiri MN, Mwanjawala P, Chilanga E, et al. : Perceived implications of COVID-19 policy measures on food insecurity among urban residents in Blantyre Malawi. BMC Public Health. 2022;22(1): 522. 10.1186/s12889-022-12922-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mnyanga M, Chirwa GC, Munthali S: Impact of Safety Nets on Household Coping Mechanisms for COVID-19 Pandemic in Malawi. Front Public Health. 2021;9: 806738. 10.3389/fpubh.2021.806738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lust E, Dulani B, Harris A, et al. : The First GLDIPOR Covid-19 Survey in Malawi. The Program on Governance and Local Development, University of Gothenburg,2020. [Google Scholar]
- 30. Chiumia IK, Mosiwa BA, Nkhonjera J, et al. : Emerging public health challenges during the COVID-19 pandemic in Malawi: a review. Public Health Chall. 2022;1(4):e40. 10.1002/puh2.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Braam DH, Srinivasan S, Church L, et al. : Lockdowns, lives and livelihoods: the impact of COVID-19 and public health responses to conflict affected populations - a remote qualitative study in Baidoa and Mogadishu, Somalia. Confl Health. 2021;15(1): 47. 10.1186/s13031-021-00382-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Coetzee BJ, Kagee A: Structural barriers to adhering to health behaviours in the context of the COVID-19 crisis: considerations for low- and middle-income countries. Glob Public Health. 2020;15(8):1093–102. 10.1080/17441692.2020.1779331 [DOI] [PubMed] [Google Scholar]
- 33. Singer MC, Rylko-Bauer B: The syndemics and structural violence of the COVID pandemic: anthropological insights on a crisis. Open Anthropol Res. 2021;1(1):7–32. 10.1515/opan-2020-0100 [DOI] [Google Scholar]
- 34. Owoyemi A, Okolie EA, Omitiran K, et al. : Importance of community-level interventions during the COVID-19 pandemic: lessons from Sub-Saharan Africa. Am J Trop Med Hyg. 2021;105(4):879–83. 10.4269/ajtmh.20-1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hyder A, Behrman JR: Female economic activity in Rural Malawi. J Dev Leadersh. 2014;3(1):1–10. [PMC free article] [PubMed] [Google Scholar]
- 36. Adams J, MacKenzie MJ, Amegah AK, et al. : The conundrum of low COVID-19 mortality burden in sub-Saharan Africa: myth or reality? Glob Health Sci Pract. 2021;9(3):433–43. 10.9745/GHSP-D-21-00172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Oleribe OO, Suliman AAA, Taylor-Robinson SD, et al. : Possible reasons why Sub-Saharan Africa experienced a less severe COVID-19 pandemic in 2020. J Multidiscip Healthc. 2021;14:3267–71. 10.2147/JMDH.S331847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ndambo MK, Munyaneza F, Aron M, et al. : The role of community health workers in influencing social connectedness using the household model: a qualitative case study from Malawi. Glob Health Action. 2022;15(1): 2090123. 10.1080/16549716.2022.2090123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mandolo J, Msefula J, Henrion MYR, et al. : SARS-CoV-2 exposure in Malawian blood donors: an analysis of seroprevalence and variant dynamics between January 2020 and July 2021. BMC Med. 2021;19(1): 303. 10.1186/s12916-021-02187-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Theu JA, Kabaghe AN, Bello G, et al. : SARS-CoV-2 prevalence in Malawi based on data from survey of communities and health workers in 5 high-burden districts, October 2020. Emerg Infect Dis. 2022;28(13):S76–S84. 10.3201/eid2813.212348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sachathep KKF, Tenthani L, Ogollah FM, et al. : Sars-cov-2 surveillance in 14 health facilities in Malawi. Top Antivir Med. 2021;29:245. Reference Source [Google Scholar]


