Abstract
BACKGROUND
As a less invasive technique, peroral endoscopic myotomy (POEM) has recently been widely accepted for treating achalasia with an excellent safety profile, durability, and efficacy in adults. In pediatric and geriatric patients, the treatment is more difficult.
AIM
To discuss the clinical outcomes of POEM in pediatric and geriatric patients with achalasia.
METHODS
We conducted a comprehensive search of PubMed, Embase and Cochrane Library databases from inception to July 2024. The primary outcomes were technical and clinical success. Secondary outcomes of interest included adverse events and gastroesophageal reflux disease (GERD). The pooled event rates were calculated by comprehensive meta-analysis software.
RESULTS
A total of 32 studies with 547 pediatric patients and 810 geriatric patients were included in this study. The pooled event rates of technical success, clinical success, GERD and adverse events of POEM for treating achalasia in pediatric patients were 97.1% [95% confidence interval (CI): 95.0%-98.3%; I² = 0%; P < 0.000], 93.2% (95%CI: 90.5%-95.2%; I² = 0%; P < 0.000), 22.3% (95%CI: 18.4%-26.7%; I² = 43.874%; P < 0.000) and 20.4% (95%CI: 16.6%-24.8%; I² = 67.217%; P < 0.000), respectively. Furthermore, in geriatric patients, the pooled event rates were 97.7% (95%CI: 95.8%-98.7%; I² = 15.200%; P < 0.000), 93.2% (95%CI: 90.3%-95.2%; I² = 0%; P < 0.000), 23.9% (95%CI: 19.4%-29.1%; I² = 75.697%; P < 0.000) and 10.8% (95%CI: 8.3%-14.0%; I² = 62.938%; P < 0.000], respectively.
CONCLUSION
Our findings demonstrated that POEM was an effective and safe technique for pediatric and geriatric patients with achalasia.
Keywords: Achalasia, Peroral endoscopic myotomy, Pediatric, Geriatric, Meta-analysis
Core Tip: Peroral endoscopic myotomy (POEM), a minimally invasive procedure, has gained substantial acceptance as a treatment for achalasia due to its excellent safety profile, durability, and efficacy in adults. We conducted this systematic review and meta-analysis to summarize the durability, safety, and efficacy of POEM for treating achalasia in pediatric and geriatric patients. Our results indicated that POEM was an effective and safe technique for pediatric and geriatric patients with achalasia.
INTRODUCTION
Achalasia is a moderately uncommon esophageal smooth muscle motility disorder characterized by the absence or spastic contractions of the esophageal body and the loss of deglutition-induced relaxation of the lower esophageal sphincter (LES)[1]. Typically, dysphagia is experienced by the patient. Regurgitation of undigested food, heartburn, respiratory symptoms, chest pain, and weight loss are other clinical symptoms of achalasia[2]. The estimated annual incidence rate of achalasia is between 0.03 and 1.63 per 100000 people, and the annual prevalence of achalasia is reported to range from 1.8 to 12.6 per 100000 people[3]. Achalasia can occur at all ages and equally in men and women, with no racial predilection[3], but it is an exceedingly rare illness in the pediatric population, with an estimated prevalence between 0.02 and 0.31 per 100000 children, approximately 10 times lower than that in adults[4-6]. The prevalence increases with age, with a peak in the seventh decade of life[7].
Botulinum toxin injection, laparoscopic Heller myotomy (LHM) and pneumatic dilation (PD) are available therapeutic approaches for achalasia[8-11]. In the past decade, a novel technique called peroral endoscopic myotomy (POEM) was created to combine an endoscopic approach with the principles of natural orifice transluminal endoscopic surgery to perform myotomy for achalasia. The American College of Gastroenterology clinical guidelines indicate that POEM and LHM result in comparable symptomatic improvements in patients with achalasia[3]. A systematic review and meta-analysis compared the results between 1958 patients after POEM and 5834 patients after LHM, and reported that the predicted probability of improvement in dysphagia was 93.5% for POEM and 91.0% for LHM at 12 months, and 92.7% for POEM and 90.0% for LHM at 24 months[12].
Briefly, the POEM procedure requires submucosal injection with indigo carmine dye, mucosal incision, submucosal dissection, myotomy and closure of the mucosal incision[3]. The POEM procedure in special populations is similar to that in general patients, with only minor modifications. However, the length of the pediatric esophagus is short, and the esophageal wall in children is relatively thin, which undoubtedly increases the difficulty of the operation[13]. In addition, geriatric patients tend to have more comorbidities, and thus have a higher risk during surgery and anesthesia[14,15].
Therefore, we aimed to conduct this systematic review and meta-analysis to summarize the durability, safety and efficacy of POEM in pediatric and geriatric patients with achalasia.
MATERIALS AND METHODS
This systematic review and meta-analysis strictly conformed to the preferred reporting items for systematic reviews and meta-analyses statement[16]. Our study did not require ethical approval or written consent.
Search strategy
A systematic literature search was conducted via the PubMed, Embase and Cochrane Library databases from inception to July 2024, with studies limited to those written in the English language. The key words included “peroral endoscopic myotomy”, “per-oral endoscopic myotomy”, “POEM”, “achalasia” and all possible combinations (Supplementary Table 1). To ensure a thorough search of the literature, the words “pediatric” and “geriatric” were not used. In addition to searching the literature using keywords, the inclusion of articles following a meticulous review of references was pursued to identify those that satisfied the specified criteria for inclusion.
Study selection
Two authors screened the titles and abstracts of all articles separately, in accordance with the exclusion and inclusion criteria. Next, the full texts of relevant articles were reviewed after screening. Any disagreements between reviewers in the search process were resolved by discussion with a third reviewer. The inclusion criteria were as follows: (1) Population: Patients diagnosed with achalasia and aged ≤ 18 years (pediatric) or ≥ 60 years (geriatric); (2) Treatment: POEM; and (3) Outcomes: Technical and clinical success, adverse events and gastroesophageal reflux disease (GERD). Exclusion criteria were as follows: (1) Case reports with < 5 patients, reviews, and animal experiments; (2) Studies that did not provide enough data; and (3) Studies not published in the English language.
Data extraction and definition
Data regarding the characteristics of the selected studies (first author, year of publication, country, study type, study interval, number of patients, gender and age), pre- and postoperative data of the patients (duration of symptoms, myotomy length, operation time, length of hospital stay and follow-up time), and clinical outcomes (technical success and clinical success rates, adverse events and GERD rates) were independently extracted by two authors using a prepared standardized form. The definition of technical success was completion of the entire POEM procedure. Clinical success was regarded as an Eckardt score ≤ 3 during the follow-up period after POEM. The severity of adverse events was graded on the basis of the American Society for Gastrointestinal Endoscopy (ASGE) lexicon[17]. GERD included symptomatic reflux and reflux esophagitis.
Quality assessment of the studies
Two reviewers independently conducted a quality assessment using the National Institutes of Health (NIH) quality assessment tool, which is applicable for pre-post studies with no control group[18].
Statistical analysis
Statistical analysis was performed using comprehensive meta-analysis software version 3.0 (Biostat, Englewood, NJ, United States). The outcomes are presented as pooled event rates and 95% confidence interval (CI), and the significance degree P was set at < 0.05. Heterogeneity among the studies was assessed using the I² statistic. Significant heterogeneity was considered, if the I² value was ≥ 50%, and a random-effect model was used. A funnel plot was used to evaluate publication bias.
RESULTS
Eligible studies
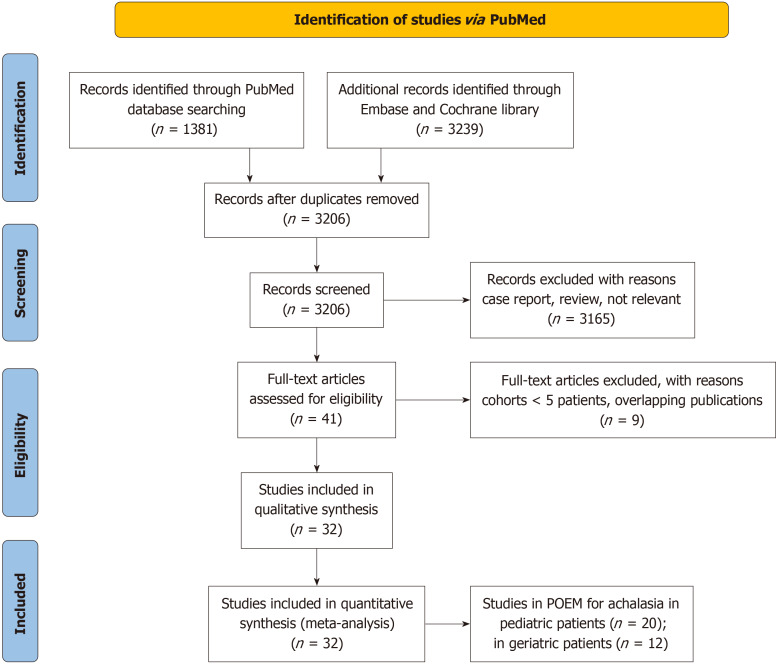
A total of 4620 articles was identified in the initial search, and 3206 studies remained after the removal of duplicates. On the basis of the inclusion and exclusion criteria, 41 articles were eligible after the titles and abstracts were reviewed. Nine studies were excluded as the cohorts included fewer than five patients or due to overlapping publications. Ultimately, 32 articles were included in this review (pediatric patients, n = 20[19-38]; geriatric patients, n = 12[13,39-49]) (Figure 1).
Figure 1.
Flow diagram showing study selection. POEM: Peroral endoscopic myotomy.
According to the NIH quality assessment tool, 13 studies were of good quality, eight studies showed fair quality, and one study exhibited poor quality (Supplementary Table 2 and Supplementary Table 3). The reasons why the study was rated as poor quality were as follows: The eligibility criteria and study population were not clearly described; Only five pediatric patients who underwent POEM were enrolled in this study; The definition of outcomes was not clearly described; Blinding or masking means were used for the outcome evaluations; P values were not reported. Due to the lack of information in articles published in conference abstracts, no quality assessment was conducted.
Role of POEM for achalasia in pediatric patients
Baseline characteristics: Table 1 shows the baseline characteristics of the original studies of POEM for treating achalasia in pediatric patients[19-38]. Twenty articles involving 547 pediatric patients investigated the efficacy and safety of POEM, including 5 prospective studies and 15 retrospective studies. Among these articles, seven studies were conducted in China, four in the United States, two in Japan, two in Italy, two in India, one in France, one in Israel and one in Chile. These studies were performed between 2007 and 2021. The age of the patients in these studies ranged from 0.9 to 18 years, and 55.4% of the patients were male. The duration of symptoms ranged from 12 to 26.4 months. The mean myotomy length and operation time was mentioned in 18 and 17 studies, which ranged from 6.5 to 14 cm and 30 to 142 minutes, respectively. Furthermore, the length of hospital stay and follow-up time ranged from 1 to 9 days and from 6 to 85.75 months, respectively.
Table 1.
Baseline characteristics of the studies on peroral endoscopic myotomy for achalasia in pediatric patients
|
Ref.
|
Country
|
Study type
|
Study interval
|
Patients (n)
|
Gender (M:F)
|
Age (yr)
|
Duration of symptoms (month)
|
Myotomy length (cm)
|
Operation time (min)
|
Hospital stay (day)
|
Follow-up (month)
|
Method of GERD diagnosis
|
| Li et al[19], 2015 | China | Prospective | October 2011 to March 2014 | 9 | 4:5 | 14.1 (10-17) | 26.4 (6-60) | 8.3 | 56.7 | - | 16.3 (3-30) | Esophageal manometry, barium esophagram and EGD |
| Chen et al[20], 2015 | China | Prospective | August 2010 to July 2012 | 27 | 11:16 | 13.8 (6-17) | 20.4 (6-36) | 9.6 (7-11) | 39.4 (21-90) | 3.2 (1-7) | 24.6 (15-38) | EGD |
| Caldaro et al[21], 2015 | Italy | Retrospective | 2009 to 2014 | 9 | 3:6 | 12.2 ± 3.8 | - | 11 ± 2 | 62 ± 12.7 | 4.1 (2-7) | 12.7 (5-28) | pH-monitoring and EGD |
| Tang et al[22], 2015 | China | Retrospective | July 2012 to August 2014 | 5 | 3:2 | 15 | 12 (3-15) | 8 (6-11) | 50 (40-90) | 7 (5-13) | 18 (12-23) | EGD, mano-metry |
| Tan et al[23], 2016 | China | Retrospective | January 2007 to June 2015 | 12 | 6:6 | 13.7 ± 2.6 | 23.6 ± 16.8 | - | - | - | 36 | EGD, esophageal manometry |
| Stavropoulos et al[24], 2017 | United States | Retrospective1 | 2013 to 2016 | 10 | 7:3 | 14.7 (10-17) | 21 (3-84) | 11.4 ± 5.98 | 55 (33-111) | 1.2 (1-2) | 15 (1-30) | - |
| Zangen et al[25], 2017 | Israel | Retrospective1 | - | 5 | 2:3 | 15.4 (10- 18) | - | 11.2 (10-14) | 62 (43-73) | - | 6 | HRM |
| Kethman et al[26], 2018 | United States | Prospective | 2014 to 2016 | 10 | 8:2 | 13.4 ± 3.3 | - | 7 (4-9) | 142 (60-259) | - | - | - |
| Miao et al[27], 2018 | China | Prospective | October 2014 to October 2016 | 21 | 9:12 | 5.5 (0.9-18) | 18 (3.6-30) | 9 (6-11) | 40 (30-55) | 9 (7-12) | 13.2 (3-24) | 99mTc DTPA scintigraphic examinations, gastroscopy and esophageal manometry |
| Korrapati et al[28], 2018 | India | Retrospective1 | - | 15 | 10:5 | 15 (3-18) | 21.9 (6-54) | 8 (6-11) | 85.3 ± 31 | 4.4 ± 2.5 | 19.8 (1.5-51) | EGD |
| Nishimoto et al[29], 2018 | Japan | Retrospective1 | May 2015 to November 2017 | 13 | - | 15 (10-18) | - | - | - | - | 18.3 (0-30) | - |
| Mangiola et al[30], 2018 | Italy | Retrospective1 | January 2012 to June 2017 | 26 | 12:14 | 10.9 (2-17) | 18.2 ± 14.9 | 10 ± 2.6 | 56.2 ± 12.6 | 3.7 ± 1.7 | 30.2 ± 15.4 | Manometry, 24 h pH-monitoring, and EGD |
| Yamashita et al[31], 2018 | Japan | Retrospective1 | September 2011 to June 2017 | 7 | - | 15.0 (9-18) | 30.7 (1-84) | 14 (7-24) | - | - | 39.6 (18-54) | - |
| Choné et al[32], 2019 | France | Retrospective | January 2012 to August 2018 | 117 | 69:48 | 14.2 (3.7) | 21.3 (21.2) | 8.3 (3-21) | 72.5 (16-240) | 3.9 (1-14) | 18 (3.3-53.7) | - |
| Nabi et al[33], 2019 | India | Retrospective | September 2013 to Jan 2018 | 44 | 22:21 | 14.58 ± 3.41 | 24 (2-96) | 10.09 (5-15) | 65.46 (18-240) | 3 (2-4) | 18 (1-53.1) | Symptoms, EGD and 24-h pH-impedance |
| Liu et al[34], 2019 | China | Retrospective | August 2010 to August 2017 | 130 | 82:48 | - | 12 (0-13) | 7.2 ± 1.4 | 30 (15-255) | 3 (1-21) | 40 (4-88) | Barium swallow, EGD and HRM |
| Saez et al[35], 2020 | Chile | Retrospective | March 2017 to November 2019 | 5 | 4:1 | 11 (5-15) | - | 9.8 (9-11) | 70 (50-120) | 2 (1-3) | 20.5 (4 -37) | EGD and HRM |
| Wood et al[36], 2020 | United States | Prospective | 2014 to 2019. | 21 | 14:7 | 13 (2-17) | - | 7 ± 1.1 | 92 ± 52 | 1 ± 0.5 | 12 | - |
| Peng et al[37], 2022 | China | Retrospective | October 2011 to November 2016 | 24 | 14:10 | 14.42 ± 2.65 | 14.5 (3-84) | 9 (5-10) | 58.67 ± 19.10 | 6.42 ± 2.15 | 85.75 ± 25.91 | Gerd Q score and EGD |
| Petrosyan et al[38], 2022 | United States | Retrospective | July 2015 to September 2021 | 37 | 23:14 | 11.6 ± 4.5 | - | 6.5 ± 0.93 | 138.1 ± 62.2 | 2.4 ± 0.9 | 22.6 ± 20 | - |
Published conference abstracts.
M: Male; F: Female; POEM: Peroral endoscopic myotomy; pH: Potential of hydrogen; EGD: Esophagogastroduodenoscopy; HRM: High resolution esophageal manometry; 99mTc DTPA: Diethylenetriaminepentaacetic acid.
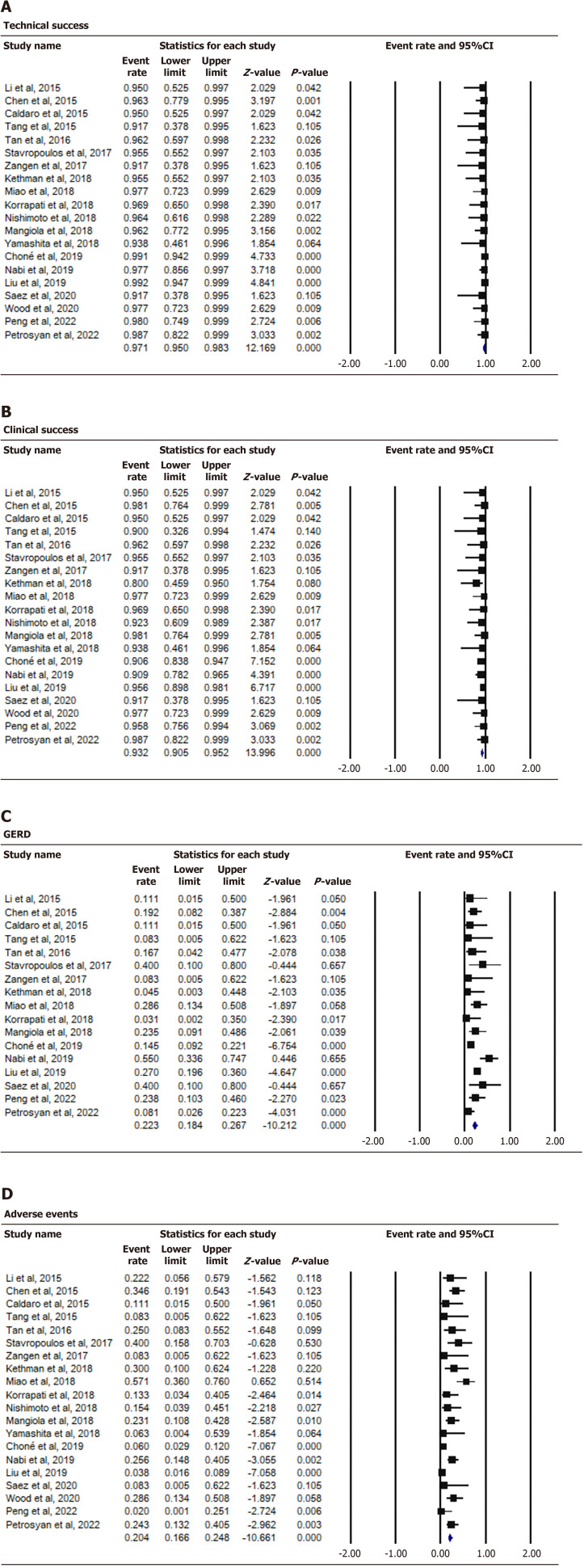
Clinical outcomes: In total, 20 studies (Table 2) reported the technical success and clinical success rates of POEM for achalasia in pediatric patients; The pooled rates were 97.1% (95%CI: 95.0%-98.3%; I² = 0%; P < 0.000) and 93.2% (95%CI: 90.5%-95.2%, I² = 0%; P < 0.000], respectively (Figure 2A and B). On the other hand, the pooled rates of GERD and adverse events were 22.3% (95%CI: 18.4%-26.7%; I² = 43.874%; P < 0.000) and 20.4% (95%CI: 16.6%-24.8%; I² = 67.217%; P < 0.000), respectively (Figure 2C and D). It must be noted that the definition of adverse events in each study was inconsistent, with some authors defining adverse events as those requiring intervention or major adverse events[33,34], whereas others defined gas-related complications without clinical symptoms as adverse events[19,23,27].
Table 2.
Clinical outcomes of the studies on peroral endoscopic myotomy for achalasia in pediatric patients, n (%)
|
Ref.
|
Technical success
|
Clinical success
|
GERD
|
Adverse events
|
| Li et al[19], 2015 | 9/9 (100) | 9/9 (100) | 1/9 (11.1) | 2/9 (11.1) |
| Chen et al[20], 2015 | 26/27 (96.3) | 26/26 (100) | 5/26 (19.2) | 9/26 (34.6) (Cumulative adverse events on CT scan: 53) |
| Caldaro et al[21], 2015 | 9/9 (100) | 9/9 (100) | 1/9 (11.1) | 1/9 (11.1) |
| Tang et al[22], 2015 | 5/5 (100) | 4/4 (100) | 0 (0) | 0 (0) |
| Tan et al[23], 2016 | 12/12 (100) | 12/12 (100) | 2/12 (16.7) | 3/12 (8.3) |
| Stavropoulos et al[24], 2017 | 10/10 (100) | 10/10 (100) | 2/5 (40) | 4/10 (40) |
| Zangen et al[25], 2017 | 5/5 (100) | 5/5 (100) | 0 (0) | 0 (0) |
| Kethman et al[26], 2018 | 10/10 (100) | 8/10 (80) | 0 (0) | 3/10 (30) |
| Miao et al[27], 2018 | 21/21 (100) | 21/21 (100) | 6/21 (28.6) | 12/21 (57.1) |
| Korrapati et al[28], 2018 | 15/15 (100) | 15/15 (100) | 0 (0) | 2/15 (13.3) |
| Nishimoto et al[29], 2018 | 13/13 (100) | 12/13 (92.3) | - | 2/13 (15.4) |
| Mangiola et al[30], 2018 | 25/26 (96.2) | 26/26 (100) | 4/17 (23.5) | 6/26 (23.1) |
| Yamashita et al[31], 2018 | 7/7 (100) | 7/7 (100) | - | 0 (0) |
| Choné et al[32], 2019 | 116/117 (99.1) | 106/117 (90.6) | 17/117 (21.4) | 7/117 (8.5) |
| Nabi et al[33], 2019 | 43/44 (97.7) | 40/44 (90.9) | 11/20 (55) | 11/43 (25.6) |
| Liu et al[34], 2019 | 129/130 (99.2) | 108/113 (95.6) | 30/111 (27.0) | 5/130 (3.8) |
| Saez et al[35], 2020 | 5/5 (100) | 5/5 (100) | 2/5 (40) | 0 (0) |
| Wood et al[36], 2020 | 21/21 (100) | 21/21 (100) | - | 6/21 (28.6) |
| Peng et al[37], 2022 | 24/24 (100) | 23/24 (95.8) | 5/21 (23.8) | 0 (0) |
| Petrosyan et al[38], 2022 | 37/37 (100) | 37/37 (100) | 3/37 (8.1) | 9/37 (24.3) |
GERD: Gastroesophageal reflux disease; CT: Computed tomography.
Figure 2.
Forest plot of peroral endoscopic myotomy for achalasia in pediatric patients. A: Technical success; B: Clinical success; C: Gastroesophageal reflux disease; D: Adverse events. GERD: Gastroesophageal reflux disease.
Role of POEM for achalasia in geriatric patients
Baseline characteristics: There were eight original studies and four conference abstracts on the efficacy and safety of POEM in geriatric patients, and the results are shown in Table 3[13,39-49]. Among these articles, four studies were conducted in Japan, three in the United States, three in China, one in Italy, and one in the Netherlands. All studies were retrospective cohort studies, and were conducted from September 2008 to May 2021. A total of 810 geriatric patients aged 67.9 to 84 years (aged ≥ 80 years in one study) were included in this study, and 50% of the patients were male. The duration of symptoms, reported in nine studies, ranged from 4.4 to 30 years. Myotomy length was mentioned in 10 studies, which ranged from 10 to 14.5 cm. In addition, the operation duration of POEM, reported in 8 studies, ranged from 46.87 to 138.3 minutes. Moreover, the duration of hospital stay and the follow-up time ranged from 1 to 9.8 years and from 2 to 41 months, respectively.
Table 3.
Baseline characteristics of the studies on peroral endoscopic myotomy for achalasia in geriatric patients
|
Ref.
|
Country
|
Study type
|
Study interval
|
Patients (n)
|
Gender (M:F)
|
Age (yr)
|
Duration of symptoms (month)
|
Myotomy length (cm)
|
Operation time (min)
|
Hospital stay (day)
|
Follow-up (month)
|
Method of GERD diagnosis
|
| Wang et al[39], 2016 | China | Retrospective | January 2010 to December 2015 | 21 | 12:9 | 67.9 ± 4.3 | 13.9 ± 11.7 | - | - | - | 21.8 | EGD, esophageal manometry and barium esophagram |
| Chen et al[13], 2018 | United States | Retrospective | January 2010 to January 2016 | 76 | 40:36 | 84 ± 3.2 | 24.0 (17.8-30.3) | 10.0 ± 4.0 | 103.7 ± 47.9 | 3 | 8.5 (IQR: 2.2-18.2) | - |
| Landi et al[40], 2018 | Italy | Retrospective1 | May 2011 to April 2017 | 88 | 39:49 | 72.2 ± 4.7 | - | 12.3 ± 3 | - | - | 24 | - |
| Liu et al[41], 2019 | China | Retrospective | August 2010 to December 2017 | 139 | 65:74 | 70.22 ± 5.68 | 8 (IQR: 2-20) | 10.57 ± 1.81 | 50 (IQR: 36-76) | 3 (IQR: 2-4) | 41 (IQR: 26-60) | Barium swallow, EGD and HRM |
| Klair et al[42], 2019 | United States | Retrospective1 | December 2014 to October 2018 | 62 | 36:26 | 72.3 ± 5.7 | - | 13.8 | - | 1.9 | - | - |
| Abe et al[43], 2020 | Japan | Retrospective | April 2015 to March 2019 | 28 | 12:16 | ≥ 80 | 5.5 (0.25-59) | 14.5 (4-26) | 60.5 (36-124) | 9.8 (4-51) | - | EGD and HRM |
| Sanaka et al[44], 2020 | United States | Retrospective | April 2014 to May 2019 | 55 | 31:24 | 74 (70-79) | 30 (12-60) | 10 (IQR: 8-10) | 90 (IQR: 7.5-110) | 1 (IQR: 1-2) | 2.4 (IQR: 2.2-2.7) | HRM, timed barium esophagram and 24-h esophageal pH study |
| Angeli Abad et al[45], 2020 | Netherlands | Retrospective1 | September 2008 to June 2019 | 66 | 28:38 | 83 (80-92) | 10.5 (0.2-62.4) | - | - | 7 ± 4.1 | 12 | - |
| Okada et al[46], 2021 | Japan | Retrospective | September 2011 to March 2020 | 100 | 40:60 | 74.2 (65-93) | 10.3 ± 13.6 | 12.5 (3-25) | 138.3 (50-460) | - | 36 | - |
| Nakamura et al[47], 2021 | Japan | Retrospective | August 2014 to May 2021 | 11 | 7:4 | 81 (75-87) | 5 (2-40) | 13 (8-19) | 109 (62-144) | - | 36 | EGD, esophagography and HRM |
| Ujiie et al[48], 2021 | Japan | Retrospective | January 2015 to December 2019 | 18 | 12:6 | 78 (75-86) | 4.4 (0.05-50.2) | 10 (5-16) | 104 (45-165) | - | 2 | IRP, HRM and EGD |
| Zhao et al[49], 2022 | China | Retrospective1 | November 2010 to September 2019 | 146 | - | - | - | 7.09 ± 2.49 | 46.87 ± 19.29 | - | - | GerdQ score |
Published conference abstracts.
M: Male; F: Female; EGD: Esophagogastroduodenoscopy; HRM: High resolution esophageal manometry; IRP: Integrated relaxation pressure; IQR: Interquartile range; pH: Potential of hydrogen.
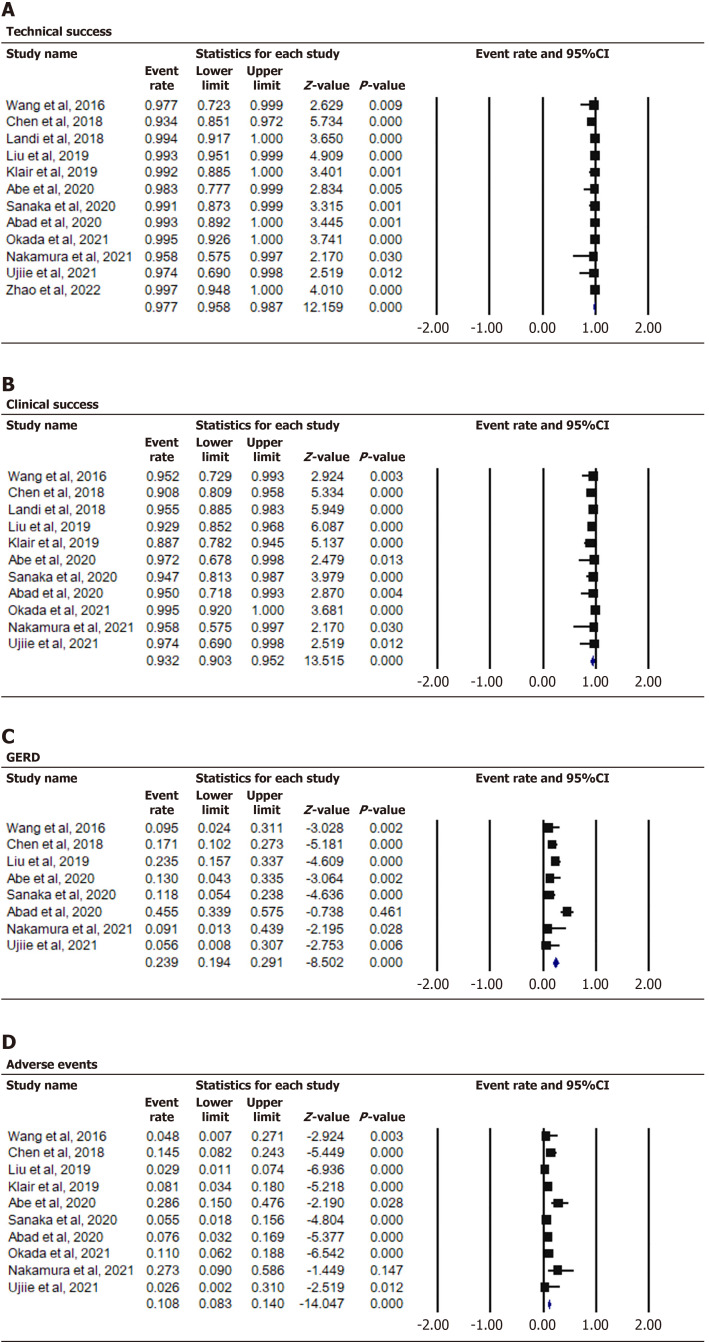
Clinical outcomes: Overall, the 12 studies (Table 4) had pooled rates of technical success, clinical success, GERD and adverse events of 97.7% (95%CI: 95.8%-98.7%; I² = 15.200%; P < 0.000), 93.2% (95%CI: 90.3%-95.2%; I² = 0%, P < 0.000), 23.9% (95%CI: 19.4%-29.1%; I² = 75.697%; P < 0.000), and 10.8% (95%CI: 8.3%-14.0%; I² = 62.938%; P < 0.000), respectively (Figure 3).
Table 4.
Results of the studies on peroral endoscopic myotomy for achalasia in geriatric patients, n (%)
|
Ref.
|
Technical success
|
Clinical success
|
GERD
|
Adverse events
|
| Wang et al[39], 2016 | 21/21 (100) | 20/21 (95.2) | 2/21 (9.5) | 1/21 (4.8) |
| Chen et al[13], 2018 | 71/76 (93.4) | 59/65 (90.8) | 13/76 (16.1) | 11/76 (14.5) |
| Landi et al[40], 2018 | 88/88 (100) | 84/88 (95.4) | - | - |
| Liu et al[41], 2019 | 138/139 (99.3) | 79/85 (92.9) | 20/85 (23.53) | 4/139 (2.88) |
| Klair et al[42], 2019 | 62/62 (100) | 55/62 (88.7) | - | 5/62 (8.1) |
| Abe et al[43], 2020 | 28/28 (100) | 17/17 (100) | 3/23 (13.0) | 8/28 (28.6) |
| Sanaka et al[44], 2020 | 55/55 (100) | 36/38 (94.7) | 6/51(11.8) | 3/55 (5.5) |
| Angeli Abad et al[45], 2020 | 66/66 (100) | 19/20 (95.0) | - | 5/66 (7.6) |
| Okada et al[46], 2021 | 100/100 (100) | 92/92 (100) | - | 11/100 (11) |
| Nakamura et al[47], 2021 | 11/11 (100) | 11/11 (100) | 1/11 (9) | 3/11 (27.3) |
| Ujiie et al[48], 2021 | 18/18 (100) | 18/18 (100) | 1/18 (5.6) | 0 (0) |
| Zhao et al[49], 2022 | 146/146 (100) | (96.33) | (15.60) | - |
GERD: Gastroesophageal reflux disease.
Figure 3.
Forest plot of peroral endoscopic myotomy for achalasia in geriatric patients. A: Technical success; B: Clinical success; C: Gastroesophageal reflux disease; D: Adverse events. GERD: Gastroesophageal reflux disease.
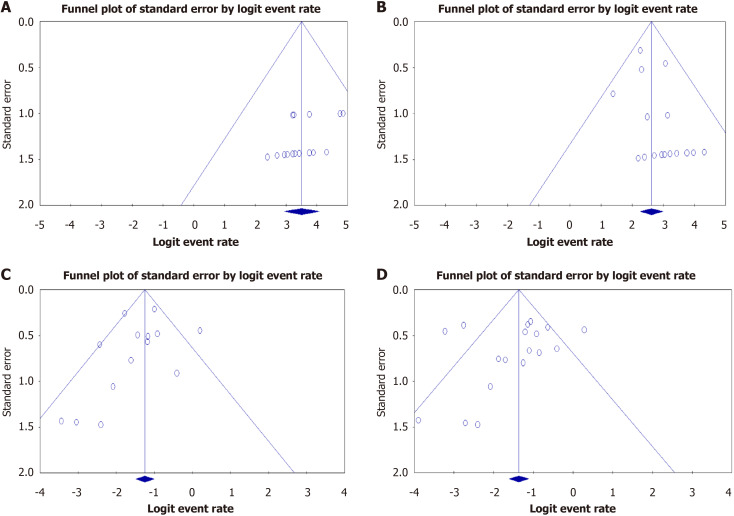
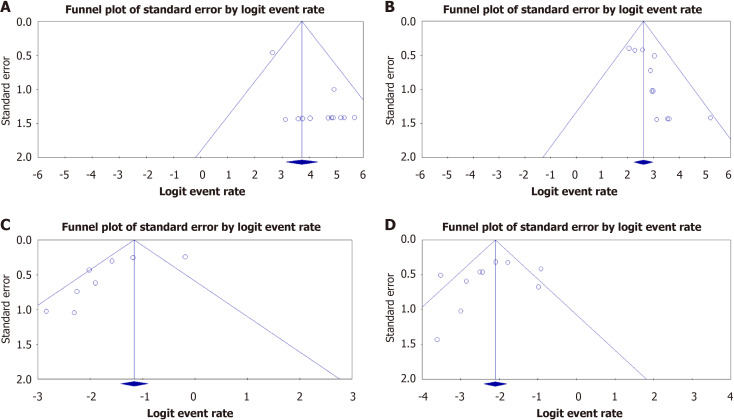
Publication Bias: Most of the funnel plots were relatively symmetric, suggesting that publication bias was not significant (Figure 4, Figure 5A and B). However, funnel plots regarding GERD and adverse events in geriatric patients displayed substantial asymmetry (Figure 5C and D).
Figure 4.
Assessment of publication bias in pediatric patients. A: Technical success; B: Clinical success; C: Gastroesophageal reflux disease; D: Adverse events.
Figure 5.
Assessment of publication bias in geriatric patients. A: Technical success; B: Clinical success; C: Gastroesophageal reflux disease; D: Adverse events.
DISCUSSION
Achalasia is a relatively uncommon disorder of the esophageal smooth muscle, and the annual incidence and prevalence increases with age, but it can affect all ages[1]. Due to the short length and weak wall of the esophagus in pediatric patients, and esophagus modifications contributing to a corkscrew esophagus, increased comorbidities and poor treatment tolerance in geriatric patients[43,49-52], the difficulty of surgery and the incidence of postoperative adverse events in these populations are increased.
Currently, the purpose of all treatment methods for achalasia is to reduce the hypertonicity of the LES to attain the goals of reducing symptoms, improving esophageal emptying, and avoiding further dilation of the esophagus[3]. Pharmacologic, botulinum toxin injection, PD, POEM, and LHM are currently available therapeutic approaches. Specifically, pharmacologic therapy is the least effective treatment for achalasia, resulting in a short-term reduction in LES pressure in 13%-65% of patients and symptom relief in 0%-87% of patients[8]. The effect of botulinum toxin is limited as it is not long-lasting and requires repeated therapy[9]. PD is an effective choice for patients with achalasia, and reports suggest that 50%-93% of patients might achieve symptom relief[1]. However, a recent meta-analysis demonstrated that the long-term efficacy of PD was inferior to that of POEM[10]. LHM is generally regarded as the gold standard because it can provide long-lasting symptom relief; however, for geriatric patients and patients with multiple comorbidities, it is not appropriate as it is an invasive procedure and can result in operative complications[11-13].
The minimally invasive technique POEM was first described by Inoue et al[15]. This technique is used for treating achalasia in adults, and is becoming increasingly available in pediatric and geriatric patients. The clinical guidelines established by the ASGE in the Preservation and Incorporation of Valuable Endoscopic Innovations (PIVI) paper[3] showed that POEM for achalasia treatment is considered a viable therapeutic modality and should fulfil the following criteria: (1) ≥ 80% efficacy at 12 months after the procedure (Eckardt score ≤ 3 with a dysphagia component of ≤ 2); and (2) Serious adverse event rate ≤ 6% and mortality rate ≤ 0.1% within 30 days after the procedure.
Previous investigations have demonstrated that POEM can provide short-term benefits in pediatric patients, with a median follow-up period of approximately 13.2 to 40 months. Given that children have a longer life expectancy, the long-term therapeutic outcomes for this patient group are especially significant[37]. The largest series of POEM for children with achalasia was conducted in China by Liu et al[34] published in 2019. The authors retrospectively evaluated a total of 130 pediatric patients. The technical success rate for POEM in these patients was 99.2%, and the clinical success rates at 1, 3, and 5 years were 98.2%, 96.5%, and 95.6%, respectively. In our study, the pooled technical and clinical success rates for pediatric patients were 97.1% (95%CI: 95.0%-98.3%; I² = 0%; P < 0.000) and 93.2% (95%CI: 90.5%-95.2%; I² = 0%, P < 0.000), and the follow-up time ranged from 6 to 85.75 months. These findings build on the outcomes of earlier research and offer further support that POEM is a highly effective therapeutic approach for childhood achalasia.
Most cases of achalasia occur in individuals between the ages of 30 and 50 years, although it is not uncommon for older adults to be diagnosed with the condition. The risk of aspiration pneumonia, a potentially lethal complication of regurgitation in achalasia, is particularly high in the elderly, highlighting the significance of exploring effective clinical interventions for this patient population[46]. To date, many studies have reported the results of POEM in elderly patients[39-49]. Zhong et al[52] published a meta-analysis that included seven studies involving 469 geriatric patients. They reported that the pooled technical success rate was 98.1%, and the pooled clinical success rate was 92.5%. We conducted a more comprehensive study and found that the pooled technical and clinical success rates for geriatric patients were 97.7% (95%CI: 95.8%-98.7%; I² = 15.200%; P < 0.000) and 93.2% (95%CI: 90.3%-95.2%; I² = 0%, P < 0.000), respectively.
POEM can potentially enhance the quality of life in pediatric patients as they mature. Nevertheless, it is important to be aware of the potential adverse events following POEM, which may include GERD, pneumoperitoneum, pneumothorax, pneumonitis, mucosal injury, subcutaneous emphysema and mediastinal emphysema[53]. Our study revealed that the pooled adverse event rate following POEM in pediatric achalasia was 20.4% (95%CI: 16.6%-24.8%; I² = 67.217%; P < 0.000), and the pooled GERD rate was 22.3% (95%CI: 18.4%-26.7%; I² = 43.874%; P < 0.000). Chen et al[20] reported cumulative adverse events of 53 on the basis of computed tomography scans, which were related to gas. They revealed that this high incidence was due to air for insufflation in 20 patients (76.9%). They also demonstrated that air insufflation had a higher rate of postoperative gas-related adverse events than carbon dioxide insufflation [84.6% (11/13) vs 16.7% (1/6)][22]. In addition, Lee et al[54] included 12 studies involving 146 pediatric patients who underwent POEM. The authors found that at least 93% of the children experienced an improvement in achalasia symptoms after POEM, with a limited number of patients reporting minor adverse effects that could be controlled conservatively. Recently, Zhong et al[55] published an updated meta-analysis involving a total of 11 studies with 389 children. The pooled major adverse event rate was reported to be 12.8%, while the pooled GERD rate was 17.8%. Two meta-analyses suggested that POEM was effective and safe for treating achalasia in pediatric patients[54,55].
In geriatric patients, the pooled adverse events and GERD rates following POEM for achalasia were 10.8% (95%CI: 8.3%-14.0%; I² = 62.938%; P < 0.000) and 23.9% (95%CI: 19.4%-29.1%; I² = 75.697%; P < 0.000], respectively. Furthermore, Zhong et al[55] published a meta-analysis including 7 studies involving 469 geriatric patients, and the major adverse event rate was 9.0%, and the clinical reflux rate was 17.4%. In total, almost all these studies indicated that POEM is a safe and effective treatment for geriatric patients with esophageal achalasia[56].
There were several limitations in our analyses. First, the results of the NIH quality assessment revealed that one of our included studies was of poor quality, which may have reduced the evidence quality in our article. In addition, our study lacked several characteristic indicators, including achalasia type, American Society of Anesthesiology physical status classification system score, type of myotomy, pre- and postoperative Eckardt score, and LES pressure; thus, the analysis was not comprehensive. In addition, the study examining GERD and adverse events in geriatric patients exhibited publication bias; therefore, future investigations should include subgroup analyses to determine the underlying reasons for this. Furthermore, as the symptoms of GERD are very similar to those of achalasia, possible confusion could have occurred during interpretation of the results. A large proportion of cases with long-term follow-up could not be objectively evaluated for GERD, and the possibility of selection bias could not be completely ruled out. Both may have led to a higher pooled rate of GERD. Lastly, almost all of the studies were small sample, nonrandomized and observational studies, which may have been subject to a range of biases.
CONCLUSION
Currently, on the basis of the available published evidence, POEM has been shown to be an effective and safe therapy for achalasia in both pediatric and geriatric patients. Nevertheless, there is a need for additional high-quality randomized controlled trials to establish the optimal treatment approach for achalasia within these specific populations.
Footnotes
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade D, Grade D, Grade D
Novelty: Grade B, Grade C, Grade D, Grade D
Creativity or Innovation: Grade B, Grade C, Grade D, Grade D
Scientific Significance: Grade A, Grade C, Grade C, Grade D
P-Reviewer: Jankovic J; Tawheed A; Wang Y S-Editor: Fan M L-Editor: Webster JR P-Editor: Zhao YQ
Contributor Information
Xin-Xin Pu, Department of Gastroenterology, Dechang People’s Hospital of Sichuan Province, Liangshan 615500, Sichuan Province, China; Department of Gastroenterology, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China.
Shu Huang, Department of Gastroenterology, Lianshui People’s Hospital of Kangda College Affiliated to Nanjing Medical University, Huaian 223499, Jiangsu Province, China.
Chun-Yu Zhong, Department of Ultrasound, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China.
Xia Wang, Department of Gastroenterology, Dechang People’s Hospital of Sichuan Province, Liangshan 615500, Sichuan Province, China.
Su-Fen Fu, Department of Gastroenterology, Dechang People’s Hospital of Sichuan Province, Liangshan 615500, Sichuan Province, China.
Ying-Qin Lv, Department of Gastroenterology, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China.
Kang Zou, Department of Gastroenterology, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China.
Mu-Han Lü, Department of Gastroenterology, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China.
Yan Peng, Department of Gastroenterology, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China.
Xiao-Wei Tang, Department of Gastroenterology, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China. solitude5834@hotmail.com.
References
- 1.Savarino E, Bhatia S, Roman S, Sifrim D, Tack J, Thompson SK, Gyawali CP. Achalasia. Nat Rev Dis Primers. 2022;8:28. doi: 10.1038/s41572-022-00356-8. [DOI] [PubMed] [Google Scholar]
- 2.Zaninotto G, Bennett C, Boeckxstaens G, Costantini M, Ferguson MK, Pandolfino JE, Patti MG, Ribeiro U Jr, Richter J, Swanstrom L, Tack J, Triadafilopoulos G, Markar SR, Salvador R, Faccio L, Andreollo NA, Cecconello I, Costamagna G, da Rocha JRM, Hungness ES, Fisichella PM, Fuchs KH, Gockel I, Gurski R, Gyawali CP, Herbella FAM, Holloway RH, Hongo M, Jobe BA, Kahrilas PJ, Katzka DA, Dua KS, Liu D, Moonen A, Nasi A, Pasricha PJ, Penagini R, Perretta S, Sallum RAA, Sarnelli G, Savarino E, Schlottmann F, Sifrim D, Soper N, Tatum RP, Vaezi MF, van Herwaarden-Lindeboom M, Vanuytsel T, Vela MF, Watson DI, Zerbib F, Gittens S, Pontillo C, Vermigli S, Inama D, Low DE. The 2018 ISDE achalasia guidelines. Dis Esophagus. 2018;31 doi: 10.1093/dote/doy071. [DOI] [PubMed] [Google Scholar]
- 3.Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2020;115:1393–1411. doi: 10.14309/ajg.0000000000000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marlais M, Fishman JR, Fell JM, Haddad MJ, Rawat DJ. UK incidence of achalasia: an 11-year national epidemiological study. Arch Dis Child. 2011;96:192–194. doi: 10.1136/adc.2009.171975. [DOI] [PubMed] [Google Scholar]
- 5.Mayberry JF, Mayell MJ. Epidemiological study of achalasia in children. Gut. 1988;29:90–93. doi: 10.1136/gut.29.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sato H, Yokomichi H, Takahashi K, Tominaga K, Mizusawa T, Kimura N, Kawata Y, Terai S. Epidemiological analysis of achalasia in Japan using a large-scale claims database. J Gastroenterol. 2019;54:621–627. doi: 10.1007/s00535-018-01544-8. [DOI] [PubMed] [Google Scholar]
- 7.Li CJ, Tan YY, Wang XH, Liu DL. Peroral endoscopic myotomy for achalasia in patients aged ≥ 65 years. World J Gastroenterol. 2015;21:9175–9181. doi: 10.3748/wjg.v21.i30.9175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaezi MF, Richter JE. Current therapies for achalasia: comparison and efficacy. J Clin Gastroenterol. 1998;27:21–35. doi: 10.1097/00004836-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F, Ciovica R. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg. 2009;249:45–57. doi: 10.1097/SLA.0b013e31818e43ab. [DOI] [PubMed] [Google Scholar]
- 10.Zhong C, Tan S, Huang S, Lü M, Peng Y, Fu X, Tang X. Peroral endoscopic myotomy versus pneumatic dilation for achalasia: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2020;32:1413–1421. doi: 10.1097/MEG.0000000000001800. [DOI] [PubMed] [Google Scholar]
- 11.Evensen H, Kristensen V, Larssen L, Sandstad O, Hauge T, Medhus AW. Outcome of peroral endoscopic myotomy (POEM) in treatment-naive patients. A systematic review. Scand J Gastroenterol. 2019;54:1–7. doi: 10.1080/00365521.2018.1549271. [DOI] [PubMed] [Google Scholar]
- 12.Schlottmann F, Luckett DJ, Fine J, Shaheen NJ, Patti MG. Laparoscopic Heller Myotomy Versus Peroral Endoscopic Myotomy (POEM) for Achalasia: A Systematic Review and Meta-analysis. Ann Surg. 2018;267:451–460. doi: 10.1097/SLA.0000000000002311. [DOI] [PubMed] [Google Scholar]
- 13.Chen YI, Inoue H, Ujiki M, Draganov PV, Colavita P, Mion F, Romanelli J, Chiu P, Balassone V, Patel L, Abbas A, Yang D, Dunst C, Pioche M, Roman S, Rivory J, Ponchon T, Desilets D, Maselli R, Onimaru M, Nakamura J, Hata Y, Hajiyeva G, Ismail A, Ngamruengphong S, Bukhari M, Chavez YH, Kumbhari V, Repici A, Khashab MA. An international multicenter study evaluating the clinical efficacy and safety of per-oral endoscopic myotomy in octogenarians. Gastrointest Endosc. 2018;87:956–961. doi: 10.1016/j.gie.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Finlayson EV, Birkmeyer JD. Operative mortality with elective surgery in older adults. Eff Clin Pract. 2001;4:172–177. [PubMed] [Google Scholar]
- 15.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454. doi: 10.1016/j.gie.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 18.NIH Quality Assessment Tool for Before-After Studies with No Control Group. [cited 10 September 2024]. Available from: http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/
- 19.Li C, Tan Y, Wang X, Liu D. Peroral endoscopic myotomy for treatment of achalasia in children and adolescents. J Pediatr Surg. 2015;50:201–205. doi: 10.1016/j.jpedsurg.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 20.Chen WF, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, Zhong YS, Ma LL, Qin WZ, Hu JW, Cai MY, He MJ, Cui Z. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. 2015;81:91–100. doi: 10.1016/j.gie.2014.06.035. [DOI] [PubMed] [Google Scholar]
- 21.Caldaro T, Familiari P, Romeo EF, Gigante G, Marchese M, Contini AC, Federici di Abriola G, Cucchiara S, De Angelis P, Torroni F, Dall'Oglio L, Costamagna G. Treatment of esophageal achalasia in children: Today and tomorrow. J Pediatr Surg. 2015;50:726–730. doi: 10.1016/j.jpedsurg.2015.02.047. [DOI] [PubMed] [Google Scholar]
- 22.Tang X, Gong W, Deng Z, Zhou J, Ren Y, Zhang Q, Chen Z, Jiang B. Usefulness of peroral endoscopic myotomy for treating achalasia in children: experience from a single center. Pediatr Surg Int. 2015;31:633–638. doi: 10.1007/s00383-015-3717-9. [DOI] [PubMed] [Google Scholar]
- 23.Tan Y, Zhu H, Li C, Chu Y, Huo J, Liu D. Comparison of peroral endoscopic myotomy and endoscopic balloon dilation for primary treatment of pediatric achalasia. J Pediatr Surg. 2016;51:1613–1618. doi: 10.1016/j.jpedsurg.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 24.Stavropoulos SN, Sosulski AB, Modayil RJ, Gurram KC, Brathwaite CE, Coren CV, Boinpally H, Grendell JH. Sa2075 Use of Peroral Endoscopic Myotomy (POEM) in Pediatric Patients as a Primary or Rescue Therapy for Achalasia. Gastrointest Endosc. 2017;85:AB285–AB286. [Google Scholar]
- 25.Abstract Supplement for NeuroGASTRO 2017 Congress, 24-26 August 2017, Cork, Ireland . Neurogastroenterol Motil 2017; 29 Suppl 2: 3-140. [DOI] [PubMed] [Google Scholar]
- 26.Kethman WC, Thorson CM, Sinclair TJ, Berquist WE, Chao SD, Wall JK. Initial experience with peroral endoscopic myotomy for treatment of achalasia in children. J Pediatr Surg. 2018;53:1532–1536. doi: 10.1016/j.jpedsurg.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 27.Miao S, Wu J, Lu J, Wang Y, Tang Z, Zhou Y, Huang Z, Ying H, Zhou P. Peroral Endoscopic Myotomy in Children With Achalasia: A Relatively Long-term Single-center Study. J Pediatr Gastroenterol Nutr. 2018;66:257–262. doi: 10.1097/MPG.0000000000001675. [DOI] [PubMed] [Google Scholar]
- 28.Korrapati SK, Nemade P, Mahadik M, Biradar V, Pujari R, Bapaye J, Bapaye A. APDW 2018 E‐poster Presentations. J Gastroen Hepatol. 2018;33:54–221. [Google Scholar]
- 29.Nishimoto M, Shimamura Y, Abad MRAZ, Tokunaga R, Mochizuki Y, Nishikawa Y, Ueno A, Fukuda H, Sumi K, Ikeda H, Onimaru M, Goda K, Ito H, Inoue H. APDW 2018 E‐poster Exhibitions – Pediatric. J Gastroen Hepatol. 2018;33:546–548. [Google Scholar]
- 30.Mangiola F, Familiari P, Landi R, Calì A, D'aversa F, Bove V, Boskoski I, Tringali A, Perri V, Costamagna G. Tu1149 Peroral Endoscopic Myotomy for The Treatment of Achalasia In Children: Experience of A Single Center With Long Term Follow-Up. Gastrointest Endosc. 2018;87:AB542. [Google Scholar]
- 31.Ebrahim M, Schiodt FV, Willemoe GL, Dahl EE, Christensen E, Rashid S, Holm O, Zander M, Heitmann M, Hansen MB. UEG Week 2018 Poster Presentations. UEG J. 2018;6 [Google Scholar]
- 32.Choné A, Familiari P, von Rahden B, Desai P, Inoue H, Shimamura Y, Eleftheriadis N, Yamashita K, Khashab MA, Shiwaku H, Seewald S, Draganov PV, Alvarez LBM, Chaussade S, Tantau M, Abraham M, Marks J, Arevalo G, Albéniz E, Mion F, Roman S, Rivory J, Dubois R, Lachaux A, Benech N, Subtil F, Ponchon T, Barret M, Pioche M. Multicenter Evaluation of Clinical Efficacy and Safety of Per-oral Endoscopic Myotomy in Children. J Pediatr Gastroenterol Nutr. 2019;69:523–527. doi: 10.1097/MPG.0000000000002432. [DOI] [PubMed] [Google Scholar]
- 33.Nabi Z, Ramchandani M, Chavan R, Darisetty S, Kalapala R, Shava U, Tandan M, Kotla R, Reddy DN. Outcome of peroral endoscopic myotomy in children with achalasia. Surg Endosc. 2019;33:3656–3664. doi: 10.1007/s00464-018-06654-1. [DOI] [PubMed] [Google Scholar]
- 34.Liu Z, Wang Y, Fang Y, Huang Y, Yang H, Ren X, Xu M, Chen S, Chen W, Zhong Y, Zhang Y, Qin W, Hu J, Cai M, Yao L, Li Q, Zhou P. Short-term safety and efficacy of peroral endoscopic myotomy for the treatment of achalasia in children. J Gastroenterol. 2020;55:159–168. doi: 10.1007/s00535-019-01607-4. [DOI] [PubMed] [Google Scholar]
- 35.Saez J, Mejia R, Pattillo JC, Vuletin F, Monrroy H, Jaime F, Sharp A. Per oral endoscopic myotomy (POEM) in pediatric patients with esophageal achalasia: First Latin-American experience. J Pediatr Surg. 2021;56:706–710. doi: 10.1016/j.jpedsurg.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 36.Wood LS, Chandler JM, Portelli KE, Taylor JS, Kethman WC, Wall JK. Treating children with achalasia using per-oral endoscopic myotomy (POEM): Twenty-one cases in review. J Pediatr Surg. 2020;55:1006–1012. doi: 10.1016/j.jpedsurg.2020.02.028. [DOI] [PubMed] [Google Scholar]
- 37.Peng D, Tan Y, Li C, Lv L, Zhu H, Liang C, Li R, Liu D. Peroral Endoscopic Myotomy for Pediatric Achalasia: A Retrospective Analysis of 21 Cases With a Minimum Follow-Up of 5 Years. Front Pediatr. 2022;10:845103. doi: 10.3389/fped.2022.845103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petrosyan M, Mostammand S, Shah AA, Darbari A, Kane TD. Per Oral Endoscopic Myotomy (POEM) for pediatric achalasia: Institutional experience and outcomes. J Pediatr Surg. 2022;57:728–735. doi: 10.1016/j.jpedsurg.2022.02.017. [DOI] [PubMed] [Google Scholar]
- 39.Wang X, Tan Y, Lv L, Zhu H, Chu Y, Li C, Liu D. Peroral endoscopic myotomy versus pneumatic dilation for achalasia in patients aged ≥ 65 years. Rev Esp Enferm Dig. 2016;108:637–641. doi: 10.17235/reed.2016.4488/2016. [DOI] [PubMed] [Google Scholar]
- 40.Landi R, Familiari P, Mangiola F, Calì A, D'aversa F, Bove V, Boskoski I, Tringali A, Perri V, Costamagna G. Tu1154 Peroral Endoscopic Myotomy for The Treatment of Esophageal Motility Disorders: Baseline Characteristics And Procedural Outcomes In Young And Elderly Patients. Gastrointest Endosc. 2018;87:AB544–AB545. [Google Scholar]
- 41.Liu XY, Cheng J, Chen WF, Xu MD, Liu ZQ, Wang Y, Chen SY, Zhong YS, Zhang YQ, Qin WZ, Hu JW, Cai MY, Yao LQ, Li QL, Zhou PH. Effect of peroral endoscopic myotomy in geriatric patients: a propensity score matching study. Surg Endosc. 2020;34:2911–2917. doi: 10.1007/s00464-019-07070-9. [DOI] [PubMed] [Google Scholar]
- 42.Klair JS, Hasan Y, Masadeh M, Gerke H, Murali A, Parekh K, Keech J, Nau P, El Abiad R. 379 Safety and Efficacy of Peroral Endoscopic Myotomy (POEM) in Patients ≥ 65 Years at a Single Academic Tertiary Care Center. Am J Gastroenterol. 2019;114:S221–S221. [Google Scholar]
- 43.Abe H, Tanaka S, Kawara F, Toyonaga T, Ariyoshi R, Sakaguchi H, Sako T, Ikezawa N, Kodama Y. Comparison of the safety and efficacy of peroral endoscopic myotomy between octogenarians and non-octogenarians. Dig Endosc. 2021;33:110–117. doi: 10.1111/den.13686. [DOI] [PubMed] [Google Scholar]
- 44.Sanaka MR, Chadalavada P, Alomari M, Tang A, Parikh M, Garg R, Gupta N, Thota P, Gabbard S, Murthy S, Raja S. Peroral endoscopic myotomy is a safe and effective treatment modality for geriatric patients with achalasia. Esophagus. 2020;17:484–491. doi: 10.1007/s10388-020-00746-5. [DOI] [PubMed] [Google Scholar]
- 45.Angeli Abad MR, Inoue H, Fujiyoshi Y, Nishikawa Y, Sakaguchi T, Shimamura Y, Sumi K, Kimura R, Izawa S, Ikeda H, Onimaru M. Sa1268 Clinical Outcomes of Peroral Endoscopic Myotomy In Octo- and Nonagenarian Achalasia Patients: A Large Single-Center Experience. Gastrointest Endosc. 2020;91:AB141. [Google Scholar]
- 46.Okada H, Shiwaku H, Ohmiya T, Shiwaku A, Hasegawa S. Efficacy and safety of peroral endoscopic myotomy in 100 older patients. Esophagus. 2022;19:324–331. doi: 10.1007/s10388-021-00881-7. [DOI] [PubMed] [Google Scholar]
- 47.Nakamura J, Hikichi T, Hashimoto M, Takasumi M, Kato T, Kobashi R, Yanagita T, Suzuki R, Sugimoto M, Sato Y, Irie H, Takagi T, Kobayakawa M, Ohira H. Efficacy and Safety of Peroral Endoscopic Myotomy for Esophageal Achalasia and Achalasia-Related Diseases in Patients Aged 75 Years and Over. Healthcare (Basel) 2021;9 doi: 10.3390/healthcare9121668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ujiie N, Sato C, Taniyama Y, Koseki K, Takaya K, Okamoto H, Fukutomi T, Unno M, Kamei T. Characteristics of esophageal achalasia in geriatric patients over 75 years of age and outcomes after peroral endoscopic myotomy. Geriatr Gerontol Int. 2021;21:788–793. doi: 10.1111/ggi.14235. [DOI] [PubMed] [Google Scholar]
- 49.Zhao X, Chai N, Wu Q, Du R, Ye L, Li X, Linghu E. E-Poster Area: Blue Ribbon Posters. Dig Endosc. 2022;34:64–213. [Google Scholar]
- 50.Bartenstein P, Schober O. [In vivo imaging of benzodiazepine receptors of the central type] Wien Klin Wochenschr. 1991;103:647–648. [PubMed] [Google Scholar]
- 51.Snyder CW, Burton RC, Brown LE, Kakade MS, Finan KR, Hawn MT. Multiple preoperative endoscopic interventions are associated with worse outcomes after laparoscopic Heller myotomy for achalasia. J Gastrointest Surg. 2009;13:2095–2103. doi: 10.1007/s11605-009-1049-6. [DOI] [PubMed] [Google Scholar]
- 52.Zhong C, Huang S, Xia H, Tan S, Lü M, Peng Y, Tang X. Role of Peroral Endoscopic Myotomy in Geriatric Patients with Achalasia: A Systematic Review and Meta-Analysis. Dig Dis. 2022;40:106–114. doi: 10.1159/000516024. [DOI] [PubMed] [Google Scholar]
- 53.Luvsandagva B, Adyasuren B, Bagachoimbol B, Luuzanbadam G, Bai T, Jalbuu N, Duger D, Hou X. Efficacy and safety of peroral endoscopic myotomy for pediatric achalasia: A nationwide study. Medicine (Baltimore) 2024;103:e38970. doi: 10.1097/MD.0000000000038970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee Y, Brar K, Doumouras AG, Hong D. Peroral endoscopic myotomy (POEM) for the treatment of pediatric achalasia: a systematic review and meta-analysis. Surg Endosc. 2019;33:1710–1720. doi: 10.1007/s00464-019-06701-5. [DOI] [PubMed] [Google Scholar]
- 55.Zhong C, Tan S, Huang S, Peng Y, Lü M, Tang X. Clinical outcomes of peroral endoscopic myotomy for achalasia in children: a systematic review and meta-analysis. Dis Esophagus. 2021;34 doi: 10.1093/dote/doaa112. [DOI] [PubMed] [Google Scholar]
- 56.Peng D, Tan Y, Chen X, Lv L, Zhu H, Li R, Liu D. Prognostic factors analysis of symptoms recurrence after peroral endoscopic myotomy for the treatment of achalasia in older adults. J Gastrointest Surg. 2024;28:1349–1351. doi: 10.1016/j.gassur.2024.05.023. [DOI] [PubMed] [Google Scholar]