Abstract
BACKGROUND
Cancer presents a significant public health challenge in China, necessitating broad collaboration across society. The Chinese government has articulated a goal to increase the overall five-year survival rate for cancer by 15% by 2030. Achieving this objective requires not only advances in medical technology, but also an improvement in the dissemination of knowledge pertaining to cancer prevention and treatment.
AIM
To provide a comprehensive understanding of the status of cancer prevention and level of popularization in China in 2023.
METHODS
From January 2023 to May 2023, online questionnaires were distributed to 3000 participants, including medical personnel, patients with cancer, their families, and the general public. There were 2711 valid responses, covering the entire nation.
RESULTS
A total of 1020 medical personnel and 1691 patients with cancer, their family members, and the general public participated in the survey. Among medical personnel, 93.2% had popularized cancer health. Commonly addressed topics included cancer prevention (85.9%) and cancer screening (77.8%). Primary challenges included time constraints (73.9%), insufficient personnel and material support (66.7%), and uncertainty as to where to begin (49.3%). Among patients with cancer, their family members, and the general public, 93.4% reported reading or watching cancer science popularization materials and 56.9% expressed a desire for deeper understanding. The most sought-after topics in cancer science popularization included cancer screening (80.2%) and cancer prevention (75.8%). The greatest challenge encountered in accessing cancer health popularization was an abundance of misinformation (67.5%).
CONCLUSION
Most clinical doctors, patients, family, and the general public wish to participate in cancer education. However, improvement in the quality of content in cancer prevention and treatment education is required.
Keywords: Cancer health popularization, Patient education, Science popularization, Cancer prevention
Core Tip: Cancer poses a significant threat to the health and lives of the Chinese population. Therefore, enhancing public awareness of cancer health is of paramount importance. Prior to this study, there has been no investigation of the status of cancer health education in China. Through the distribution of random questionnaires across 31 provinces in China, 1020 healthcare professionals and 1691 patients with cancer, their family members, and the general public participated. Most participants expressed a strong willingness to participate in cancer health education. Therefore, improvement in the quality of cancer health education is required.
INTRODUCTION
The global incidence of cancer has been on the rise in recent years[1,2]. And in China, According to data released by the National Cancer Center of China, in 2022, there were 4.82 million new cases of malignant tumors in China, with a total of 2.57 million deaths due to cancer, accounting for a significant proportion of total deaths[3]. From 2000 to 2018, the standardized incidence rate of all cancers in China increased by an average of 1.4% per year. Cancer remains a major public health concern in China. Prior studies focused on the Chinese population identified 23 types of risk factors for cancer, classified into five major categories[4]. Primary risk factors include active smoking, alcohol consumption and low fruit and vegetable intake[5,6]. Faced with the formidable challenge of cancer prevention and control and the clear identification of risk factors for cancer, the timely implementation of proactive primary cancer prevention strategies could effectively reduce the disease burden of cancer in China.
The role of health education, through its popularization as a primary prevention strategy for cancer, cannot be overlooked[7-9]. With continuous development of Internet technology, health information has become more accessible to the public[10]. Among the respondents in China, health popularization was the most frequently searched type of online health information[11]. Simultaneously, healthcare professionals are increasingly recognizing the importance of health popularization and to have the ability to communicate scientific knowledge to the general population[12]. However, the proliferation of misinformation has also led to the spread of false information on health popularization[13]. Instances, such as previous anti-vaccine movements have presented new challenges and risks to health popularization efforts[14-16].
Understanding the status of cancer health popularization in a specific region or country, along with identifying challenges and difficulties, is crucial for formulating effective health popularization policies[17,18]. To our knowledge, no survey reports have specifically addressed the status of cancer popularization in China. Therefore, we conducted a survey and analysis of the status of cancer health popularization, targeting medical personnel, patients with cancer, their families, and the general public.
MATERIALS AND METHODS
Participants
From January 2023 to May 2023, online questionnaires were distributed via the Medlive platform (https://www.medlive. cn/) to a total of 3000 participants, including medical personnel, cancer patients, their families, and the general public, in China. We subsequently received 2711 valid responses, covering 31 provinces of the country.
Study design
The cancer health popularization survey and analysis conducted in this study used a randomized questionnaire survey conducted anonymously. The questionnaire included single-choice, multiple-choice, numeric fill-in-the-blank, and text fill-in-the-blank questions. In designing the survey questionnaire, a draft questionnaire was sent to relevant industry experts and clinical specialists affiliated with the Chinese Anti-Cancer Association, for feedback. The questionnaire content was reviewed, supplemented, and finalized based on the input.
The survey questionnaire for medical personnel included the following: Sex, age, professional title, hospital level, region and city of residence, participation in cancer health popularization activities, common forms and frequency of cancer health popularization activities, time allocated to cancer health popularization activities per week, perspectives on cancer health popularization, difficulties encountered in conducting cancer health popularization activities, and areas of interest in receiving health popularization training.
The survey questionnaire for patients, family members, and the general public included the following: Sex, age, education level, region and city of residence, attitude towards cancer health popularization, demand for cancer health popularization content, common forms and frequency of accessing cancer health popularization knowledge, common sources and timing of accessing cancer health popularization knowledge, credibility of current cancer health popularization knowledge, and difficulties encountered in accessing cancer health popularization knowledge.
Data interpretation
Single-choice questions (%): Percentage of respondents selecting each option for the question, with the sum of the percentages for each option totaling 100%.
Multiple-choice questions (%): Percentage of respondents selecting each option for the question, with the sum of percentages for each option exceeding 100%.
Numeric fill-in-the-blank questions: Arithmetic mean.
Text fill-in-the-blank questions: Encoding by induction method followed by statistical processing.
Statistical analysis
Frequencies and frequency rates were used to represent count or ordinal data. The collected survey questionnaires underwent data cleaning, incomplete questionnaires were removed, and data logic issues and doubtful data were reviewed. Once the data cleaning process was complete, IBM SPSS Statistics 21 was used for statistical analysis.
RESULTS
Outcomes for medical personnel
Characteristics: There were 1020 medical personnel and 65.1% were male and 34.9% were female. The 31-40 years age group had the highest proportion (46.7 %). Most medical personnel were affiliated with third-level Grade A hospitals (69.4%). Directors accounted for 16.8%, vice-directors 39.2%, attending physicians 41.7%, and residents 2.4%. The oncology department was the predominant department among the respondents (37.4 %). They were primarily located in the East China region (40.9%). Third-tier cities accounted for the majority (38.0%) of the city distribution (Table 1).
Table 1.
Characteristics of 1020 medical personnel
|
Variable
|
n
|
Percentage (%)
|
| Gender | ||
| Male | 664 | 65.1 |
| Female | 356 | 34.9 |
| Age (year) | ||
| 21-30 | 29 | 2.8 |
| 31-40 | 476 | 46.7 |
| 41-50 | 378 | 37.1 |
| 51-60 | 123 | 12.1 |
| 61-70 | 13 | 1.2 |
| Over 70 | 1 | 0.1 |
| Professional title | ||
| Directors | 171 | 16.8 |
| Vice directors | 400 | 39.2 |
| Attending | 425 | 41.7 |
| Residents | 24 | 2.4 |
| Hospital level | ||
| Third-level Grade-A | 708 | 69.4 |
| Third-level | 181 | 17.7 |
| Second-level | 128 | 12.5 |
| First-level | 24 | 2.4 |
| Regions | ||
| Northeast | 70 | 6.9 |
| North | 201 | 19.7 |
| East | 417 | 40.9 |
| South | 68 | 6.7 |
| Central | 166 | 16.3 |
| Northwest | 54 | 5.3 |
| Southwest | 44 | 4.3 |
| Cities | ||
| First-tier | 131 | 12.8 |
| Second-tier | 288 | 28.2 |
| Third-tier | 388 | 38.0 |
| Towns | 213 | 20.4 |
| Villages | 5 | 0.5 |
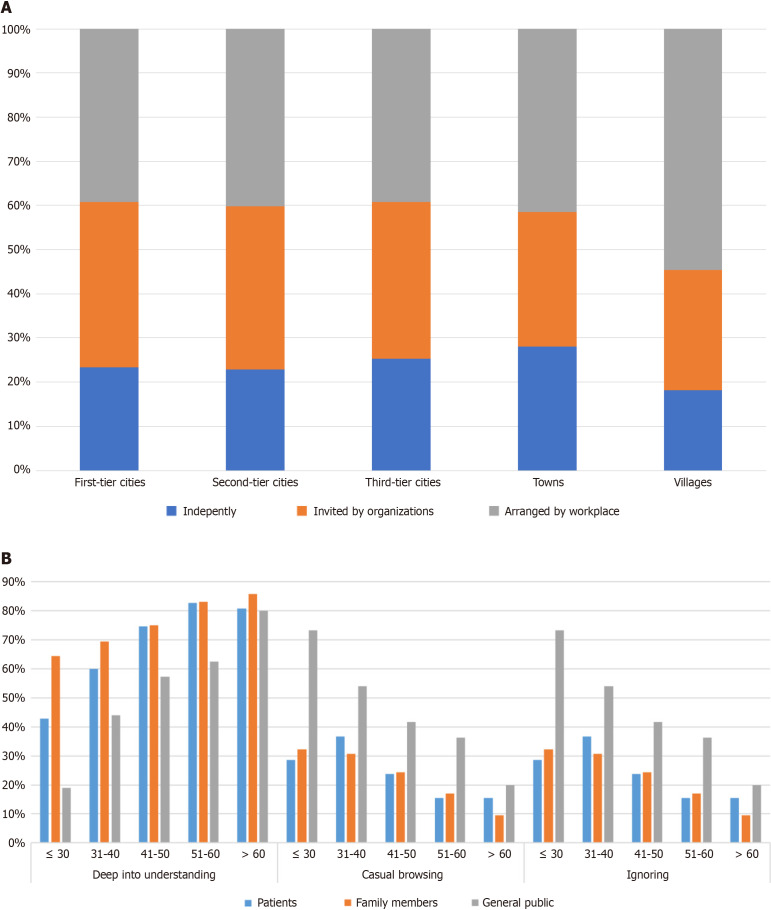
Organizational forms of cancer health popularization: The most common organizational form of cancer health popularization activities conducted by medical personnel was assigned and arranged by their workplace (73.9%). This was followed by invitations by media organizations, social institutions, and academic groups (64.7%). Additionally, 46.0% of the respondents independently organized these activities. In first-tier and second-tier cities, there were more opportunities for medical personnel to be invited by media organizations, social institutions, and academic groups, for health popularization activities, whereas doctors in towns and villages had fewer such opportunities and mostly organized activities independently (Figure 1A). On average, medical personnel spend approximately four hours per week on cancer health popularization activities.
Figure 1.
Cancer health education: organizational forms and public attitudes. A: The main organizational forms of cancer health popularization activities conducted by medical personnel in different regions; B: The attitude of the general public towards tumor popular science tends to change with increasing age.
Perspectives of cancer health popularization: Medical personnel primarily conduct cancer health popularization for patients (87.4%) and their family members (89.8%), followed by the general public (70.8%). Their efforts focused on cancer prevention (85.9%), cancer screening (77.8%), cancer treatment and related adverse reactions (74.1%), cancer diagnosis (69.5%), cancer rehabilitation follow-up (66.2%), and lifestyle management of patients with cancer (62.3%; Table 2).
Table 2.
Main perspectives of cancer health popularization
|
Variable
|
n
|
Percentage (%)
|
| Cancer prevention | 817 | 85.9 |
| Cancer screening | 740 | 77.8 |
| Cancer treatment and related adverse reactions | 705 | 74.1 |
| Cancer diagnosis | 661 | 69.5 |
| Cancer rehabilitation | 630 | 66.2 |
| Cancer patient lifestyle management | 592 | 62.3 |
| Psychological counseling: Depression, anxiety, etc. | 379 | 39.9 |
Forms and frequency of cancer health popularization activities: Seven hundred and twenty-six (76.3%) respondents selected for "Popular Science Lectures", with the majority attending one to three times per month. Seven hundred and twenty-one (75.8%) respondents selected "Text and Image Popularization", involving writing popular science articles and publishing them on public platforms, with 621 (65.3%) respondents selecting "Short Video Popularization", mainly creating and publishing short science videos on video platforms, with most individuals doing so one to three times every two to three years or one to three times per year. Four hundred and eighty-five (51.0%) respondents selected "Q&A Style Popularization", providing question-and-answer services on internet medical health service platforms, primarily one to three times per month. Overall, 401 (42.2%) respondents selected "Comic Popularization", participating in the production of popular science comics and publishing them on public platforms, mostly one to three times per year or every two to three years. 315 (33.1%) respondents selected "Live Streaming Popularization", conducting science popularization in a live streaming format on video platforms, mostly one to three times per year or every two to three years. 309 (32.5%) respondents selected "Writing Popular Science Books/Manuals", mostly every two to three years. See Table 3.
Table 3.
Main forms of cancer health popularization activities.
|
Variable
|
n
|
Percentage (%)
|
| Text and image popularization | 721 | 75.8 |
| Comic popularization | 401 | 42.2 |
| Popular science lectures | 726 | 76.3 |
| Short video popularization | 621 | 65.3 |
| Live streaming popularization | 315 | 33.1 |
| Q&A style popularization | 485 | 51.0 |
| Writing popular science books/manuals | 309 | 32.5 |
Difficulties encountered in conducting cancer health popularization activities: The main challenges to overcome in performing cancer prevention and control popularization activities include busy schedules and lack of time, as cited by the majority of respondents (73.9%). Insufficient support in terms of manpower and resources made it difficult to organize activities (66.7%). Some respondents expressed a lack of direction and uncertainty regarding where to begin (49.3%), whereas others had limited dissemination channels to engage more patients and the general public (47.8%). Inadequate written expression skills, uncertainty regarding presentation methods (42.0%) and deficiencies in verbal communication skills (39.1%) were also noted (Supplementary Table 1).
Outcomes for patients, family members, and the general public
Characteristics: There were 1691 respondents, including 943 males (55.8%) and 748 females (44.2%). The majority fell within the 41-50 age range (32.1%), followed by the 31-40 age range (31.5%). In terms of educational background, 873 respondents (51.6%) held bachelor’s degrees.
Geographically, the distribution was 514 respondents (30.4%) from the East China region and 506 respondents (29.9%) from the North China region. In terms of urban distribution, excluding rural areas, the distribution was relatively uniform with 390 respondents (23.1%) from first-tier cities, 420 (24.8%) from second-tier cities, 458 (27.1%) from third-tier cities, 352 (20.8%) from towns, and 70 (4.1%) from villages (Table 4).
Table 4.
Characteristics of 1691 patients, family members, and the general public
| Variable |
Sum
|
Patients
|
Family members
|
General public
|
||||
|
n
|
Percentage (%)
|
n
|
Percentage (%)
|
n
|
Percentage (%)
|
n
|
Percentage (%)
|
|
| Gender | ||||||||
| Male | 943 | 55.8 | 76 | 42.7 | 246 | 55.3 | 621 | 58.1 |
| Female | 748 | 44.2 | 102 | 57.3 | 199 | 44.7 | 447 | 41.9 |
| Age | ||||||||
| Below 20 | 5 | 0.3 | 1 | 0.6 | 0 | 0.0 | 4 | 0.4 |
| 21-30 | 227 | 13.4 | 7 | 3.9 | 29 | 6.5 | 191 | 17.9 |
| 31-40 | 533 | 31.5 | 30 | 16.9 | 134 | 30.1 | 369 | 34.5 |
| 41-50 | 543 | 32.1 | 59 | 33.1 | 167 | 37.5 | 317 | 29.7 |
| 51-60 | 318 | 18.8 | 53 | 29.8 | 93 | 21.0 | 172 | 16.1 |
| 61-70 | 52 | 3.1 | 20 | 11.2 | 20 | 4.5 | 12 | 1.1 |
| Over 70 | 13 | 0.8 | 8 | 4.5 | 2 | 0.4 | 3 | 0.3 |
| Educational background | ||||||||
| Doctor | 133 | 7.8 | 4 | 2.2 | 34 | 7.6 | 95 | 8.9 |
| Master | 405 | 24.0 | 16 | 9.0 | 85 | 19.1 | 304 | 28.4 |
| Bachelor | 873 | 51.6 | 58 | 32.6 | 222 | 50.0 | 593 | 55.5 |
| Associate | 164 | 9.7 | 41 | 23.0 | 61 | 13.7 | 62 | 5.8 |
| Vocational school | 33 | 2.0 | 15 | 8.5 | 14 | 3.1 | 4 | 0.4 |
| High school | 49 | 2.9 | 26 | 14.6 | 18 | 4.0 | 5 | 0.5 |
| Junior high school or below | 34 | 2.0 | 18 | 10.1 | 11 | 2.5 | 5 | 0.5 |
| Regions | ||||||||
| East | 514 | 30.4 | 62 | 34.8 | 129 | 29.0 | 323 | 30.3 |
| North | 506 | 29.9 | 34 | 19.1 | 135 | 30.3 | 337 | 31.6 |
| Central | 242 | 14.3 | 28 | 15.7 | 63 | 14.2 | 151 | 14.1 |
| South | 137 | 8.1 | 25 | 14.0 | 32 | 7.2 | 80 | 7.5 |
| Southwest | 107 | 6.3 | 11 | 6.2 | 24 | 5.4 | 72 | 6.7 |
| Northeast | 104 | 6.2 | 14 | 7.9 | 41 | 9.2 | 49 | 4.6 |
| Northwest | 81 | 4.8 | 4 | 2.3 | 21 | 4.7 | 56 | 5.2 |
| Cities | ||||||||
| First-tier | 390 | 23.1 | 35 | 19.7 | 93 | 20.9 | 262 | 24.5 |
| Second-tier | 420 | 24.8 | 31 | 17.4 | 111 | 24.9 | 278 | 26.1 |
| Third-tier | 458 | 27.1 | 44 | 24.7 | 118 | 26.5 | 296 | 27.7 |
| Towns | 352 | 20.8 | 47 | 26.4 | 100 | 22.5 | 205 | 19.2 |
| Villages | 70 | 4.1 | 20 | 11.2 | 23 | 5.2 | 27 | 2.5 |
Attitude towards cancer health popularization: Of the respondents, 93.7% had acquired or studied tumor-related popular science knowledge. 962 respondents (56.9%) expressed a desire for in-depth understanding upon encountering tumor-related popular science content, with patients with tumors and their families showing a stronger inclination towards deepening their understanding, while the general public tended to casually browse (50.6%). Additionally, most of the respondents (81.3%) actively sought tumor-related knowledge. With increasing age, respondents were more inclined to delve deeper into popular tumor science content, while the general public, particularly the younger demographic, demonstrated lower interest in popular tumor science, leaning towards casual browsing or outright neglect (Figure 1B).
Demand for cancer health popularization content: The respondents expressed a desire to acquire popular science content of multiple aspects related to tumors, including tumor screening (80.2%), tumor prevention (75.8%), tumor treatment methods (65.7%), tumor diagnosis and examination methods (62.3%), tumor symptoms (61.8%), daily life precautions and misconceptions (58.5%), prevention of tumor recurrence (56.3%), coping with adverse reactions to tumor treatment (53.6%), and psychological guidance (47.2%; Table 5).
Table 5.
Main demands for cancer health popularization content
|
Variable
|
n
|
Percentage (%)
|
| Tumor screening | 1326 | 80.2 |
| Tumor prevention | 1253 | 75.8 |
| Tumor treatment methods | 1086 | 65.7 |
| Tumor diagnosis and examination methods | 1030 | 62.3 |
| Tumor symptoms | 1022 | 61.8 |
| Daily life precautions and misconceptions | 968 | 58.5 |
| Prevention of tumor recurrence | 932 | 56.3 |
| Management of adverse reactions | 886 | 53.6 |
| Psychological guidance: Depression, anxiety, etc. | 780 | 47.2 |
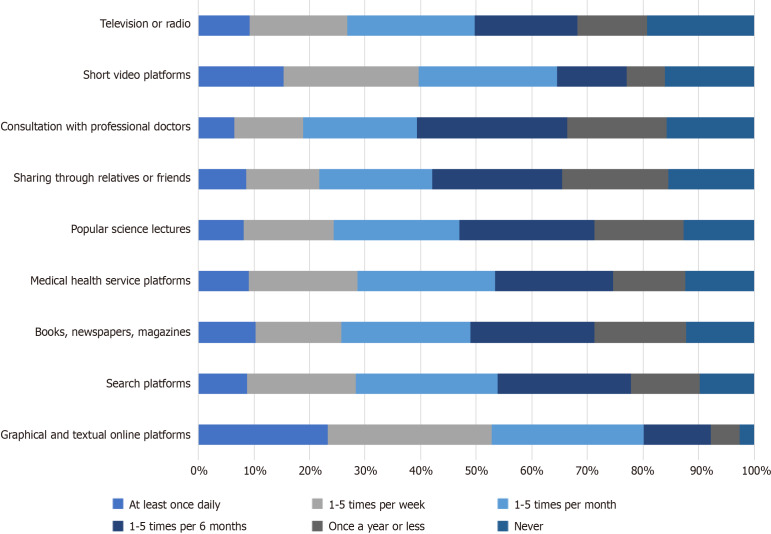
Common forms and frequency of accessing cancer health popularization knowledge: One thousand three hundred and thirty-nine (97.4%) respondents selected "graphical and textual online platforms”, with frequencies primarily ranging from one to five times per week (29.4%) and at least once daily (23.3%). One thousand two hundred and forty (90.2%) respondents selected "search platforms for retrieval", with a frequency primarily ranging from one to five times per month (25.5%). One thousand two hundred and seven (87.8%) respondents selected "books (physical/e-books), newspapers, magazines, etc.", with a frequency primarily ranging from one to five times per month (23.2%). One thousand two hundred and four (87.6%) respondents selected "viewing relevant popular science on internet medical health service platforms", with a frequency primarily ranging from one to five times per month (24.7%). One thousand two hundred and one (87.3%) respondents selected "popular science lectures", with a frequency primarily ranging from one to five times per half year (24.2%). One thousand one hundred and sixty three (84.6%) respondents selected "sharing through relatives or friends with experience of tumor illness", with a frequency primarily ranging from one to five times per half year (23.3%). One thousand one hundred and fifty-eight (84.2%) respondents selected "direct consultation with professional doctors", with a frequency primarily ranging from one to five times per half year (27.1%). One thousand one hundred and fifty-four (83.9%) respondents selected "short video platforms", with a frequency primarily ranging from one to five times per month (25.0%). One thousand one hundred and eleven (80.8%) respondents (80.8%) selected "television, radio", with a frequency primarily ranging from one to five times per month (22.9%; Figure 2).
Figure 2.
Common forms and frequencies of public access to cancer health popularization knowledge.
Difficulties encountered in accessing cancer health popularization knowledge
Studies reported that difficulties in acquiring knowledge about cancer prevention and treatment include an overabundance of false information, making it difficult to discern authenticity (67.5%), excessive complexity of theoretical knowledge that lacks practical relevance (57.9%), lack of engagement and excessive professionalism, making it challenging for the general public to understand (45.5%), and uncertainty about where to access reliable information (22.1%). These challenges underscore the importance of providing accurate, practical, and engaging information on cancer prevention and treatment to effectively educate the public[19] (Supplementary Table 2).
DISCUSSION
Cancer represents a significant global public health challenge, necessitating broad collaboration across various sectors of society. The "Healthy China 2030" plan explicitly outlines one of its goals as increasing the overall five-year survival rate for cancer by 15% by the year 2030[20]. To accomplish this formidable task, not only to rely on overall economic and technological advances, but also to intensify efforts to disseminate knowledge regarding tumor prevention and treatment and more broadly and promote the concept of "prevention first" in cancer control[21]. This will enhance cancer prevention awareness among the general population and contribute to the realization of the strategic goals of Healthy China.
According to the survey results, 93.2% of doctors were engaged in cancer prevention and treatment health education. However, the majority were assigned by their employers, followed by invitations from media organizations, social institutions, and academic groups, particularly those from developed regions (first-tier, second-tier, and third-tier cities). This indicates that clinicians should take more initiative in cancer-related health education. More professionals should be encouraged to participate in grassroots health education, particularly by igniting the enthusiasm of grassroots doctors for cancer-related health education[22,23]. By implementing incentive measures through government authorities, the enthusiasm of healthcare professionals to engage in popular science education can be stimulated. Policies should be enacted to support the expansion of the cancer health education workforce, with particular emphasis on fostering cancer education specialists in rural and grassroots areas.
In the current landscape of health education, artificial intelligence (AI) technology is playing an increasingly important role[24,25]. Previous studies have shown that ChatGPT's responses perform comparably to those of professional doctors in some areas and can even provide dietary advice[26,27]. Healthcare professionals should actively pursue learning the latest content creation techniques and leverage AI technology to efficiently produce cancer health education materials. While creating accessible and relatable educational content for the general public, attention must also be paid to ensuring the scientific accuracy and reliability of AI-generated materials[28].
For patients, their families, and the general public, 93.4% of the survey respondents have read or watched educational materials related to cancer diagnosis and treatment. More than half (57.0%) of the respondents expressed a desire to delve deeper into cancer-related educational content, and the majority (81.3%) actively sought knowledge on cancer-related topics. This indicates a growing demand for cancer prevention and treatment education among the general population and presents opportunities for cancer education initiatives[29,30]. Healthcare professionals should proactively adapt to the public’s health needs, conducting targeted educational outreach and actively participating in organized health literacy training programs to enhance their ability to communicate effectively with the general public.
With the flourishing development of new media technologies and handheld mobile devices, the general public has primarily gained knowledge on cancer prevention and treatment through graphic and text-based online platforms, search engines, and short video platforms[31,32]. Traditional forms such as television/radio, educational lectures, and books/newspapers/magazines also serve as important channels for acquiring knowledge regarding cancer prevention and treatment, although their frequency of use is lower. Patients with cancer not only trust healthcare professionals, but also place greater trust in fellow patients with similar experiences when it comes to disseminating knowledge regarding cancer prevention and treatment[33,34]. Therefore, it is essential to encourage patients to share their authentic experiences, which can help increase the public understanding of the disease, alleviate panic, and correct misconceptions[35].
The quality of cancer prevention and treatment education requires further improvement. The main challenges faced by the public in accessing knowledge in this area include the prevalence of false information and pseudoscience, overwhelming complexity of theoretical knowledge, and a lack of engagement[36]. Currently, text-based and lecture formats remain the primary forms of disseminating cancer prevention and treatment education, while new media, such as short videos and comics, serve as powerful tools for publicizing cancer prevention and treatment. Moreover, patients with cancer and their families showed a high interest in interactive Q&A educational content. To make education more accessible and practical, it is crucial to ensure that the content is both professionally authoritative and easily understandable, catering to a wide audience, while maintaining accuracy[37]. Healthcare professionals should diversify the formats of health education by incorporating new media technologies. In addition to lectures, they should actively use platforms like short videos and comics to promote health knowledge, enhancing interactivity with the general public.
CONCLUSION
Most medical personnel, patients, family members, and the general public expressed a strong willingness to participate in cancer education. However, there is a mismatch between the output and demand between these groups. There is a need for further improvement in the quality of cancer prevention and treatment education content.
ACKNOWLEDGEMENTS
Thanks to the Medlive platform (https://www.medlive.cn/) for their assistance in distributing and collecting the questionnaires for this study.
Footnotes
Institutional review board statement: This study was approved by Institutional Review Board of the Cancer Hospital of the Chinese Academy of Medical Sciences.
Informed consent statement: Informed consent was obtained from all the participants prior to the enrollment of this study.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Mahendar A S-Editor: Lin C L-Editor: A P-Editor: Zhao YQ
Contributor Information
Hai-Tao Hu, Department of Pancreatic and Gastric Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China.
Yu-Juan Jiang, Department of Pancreatic and Gastric Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China.
Xin-Xin Shao, Department of Pancreatic and Gastric Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China.
Yi-Ming Lu, Department of Pancreatic and Gastric Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China.
Yan-Tao Tian, Department of Pancreatic and Gastric Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China.
Quan Xu, Department of Pancreatic and Gastric Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China. 64804070@qq.com.
Data sharing statement
The data used to support the findings of this study are available from the corresponding author upon request.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229–263. doi: 10.3322/caac.21834. [DOI] [PubMed] [Google Scholar]
- 3.Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, Li L, Wei W, He J. Cancer incidence and mortality in China, 2022. J Natl Cancer Cent. 2024;4:47–53. doi: 10.1016/j.jncc.2024.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen W, Xia C, Zheng R, Zhou M, Lin C, Zeng H, Zhang S, Wang L, Yang Z, Sun K, Li H, Brown MD, Islami F, Bray F, Jemal A, He J. Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health. 2019;7:e257–e269. doi: 10.1016/S2214-109X(18)30488-1. [DOI] [PubMed] [Google Scholar]
- 5.Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M Comparative Risk Assessment collaborating group (Cancers) Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet. 2005;366:1784–1793. doi: 10.1016/S0140-6736(05)67725-2. [DOI] [PubMed] [Google Scholar]
- 6.Liu T, Liu CA, Zhang QS, Zhang Q, Wang YM, Song MM, Lin SQ, Deng L, Wu SL, Shi HP. Early-onset and later-onset cancer: trends, risk factors, and prevention in Northern China. Sci China Life Sci. 2024;67:1928–1940. doi: 10.1007/s11427-023-2523-5. [DOI] [PubMed] [Google Scholar]
- 7.Den Broeder L, Devilee J, Van Oers H, Schuit AJ, Wagemakers A. Citizen Science for public health. Health Promot Int. 2018;33:505–514. doi: 10.1093/heapro/daw086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siddiqi SM, Uscher-Pines L, Leinhos M, Dekker D, Chari R. Public Health Readiness for Citizen Science: Health Department Experiences. J Public Health Manag Pract. 2023;29:464–472. doi: 10.1097/PHH.0000000000001658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonney R, Phillips TB, Ballard HL, Enck JW. Can citizen science enhance public understanding of science? Public Underst Sci. 2016;25:2–16. doi: 10.1177/0963662515607406. [DOI] [PubMed] [Google Scholar]
- 10.Hesse BW, Kwasnicka D, Ahern DK. Emerging digital technologies in cancer treatment, prevention, and control. Transl Behav Med. 2021;11:2009–2017. doi: 10.1093/tbm/ibab033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shen J, Xu L, Wang J, Zong M. Investigation and analysis of public demands on health science popularization: A cross-sectional study. Asian J Surg. 2022;45:1900–1901. doi: 10.1016/j.asjsur.2022.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Campbell IH, Rudan I. Helping global health topics go viral online. J Glob Health. 2020;8:010101. doi: 10.7189/jogh.10-010101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waldrop MM. News Feature: The genuine problem of fake news. Proc Natl Acad Sci U S A. 2017;114:12631–12634. doi: 10.1073/pnas.1719005114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wawrzuta D, Jaworski M, Gotlib J, Panczyk M. Characteristics of Antivaccine Messages on Social Media: Systematic Review. J Med Internet Res. 2021;23:e24564. doi: 10.2196/24564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dubé È, Ward JK, Verger P, MacDonald NE. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu Rev Public Health. 2021;42:175–191. doi: 10.1146/annurev-publhealth-090419-102240. [DOI] [PubMed] [Google Scholar]
- 16.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16:2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ritchie D, Mallafré-Larrosa M, Ferro G, Schüz J, Espina C. Evaluation of the impact of the European Code against Cancer on awareness and attitudes towards cancer prevention at the population and health promoters' levels. Cancer Epidemiol. 2021;71:101898. doi: 10.1016/j.canep.2021.101898. [DOI] [PubMed] [Google Scholar]
- 18.Karasiewicz M, Chawłowska E, Lipiak A, Wiȩckowska B. How to Improve Cancer Prevention Knowledge? A Way to Identify Gaps and Tackle the Limited Availability of Health Education Services in Primary Health Care Using the European Code Against Cancer. Front Public Health. 2022;10:878703. doi: 10.3389/fpubh.2022.878703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gage-Bouchard EA, LaValley S, Warunek M, Beaupin LK, Mollica M. Is Cancer Information Exchanged on Social Media Scientifically Accurate? J Cancer Educ. 2018;33:1328–1332. doi: 10.1007/s13187-017-1254-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen P, Li F, Harmer P. Healthy China 2030: moving from blueprint to action with a new focus on public health. Lancet Public Health. 2019;4:e447. doi: 10.1016/S2468-2667(19)30160-4. [DOI] [PubMed] [Google Scholar]
- 21.Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020-2070. Nat Rev Clin Oncol. 2021;18:663–672. doi: 10.1038/s41571-021-00514-z. [DOI] [PubMed] [Google Scholar]
- 22.Bailey MB, Shiau R, Zola J, Fernyak SE, Fang T, So SK, Chang ET. San Francisco hep B free: a grassroots community coalition to prevent hepatitis B and liver cancer. J Community Health. 2011;36:538–551. doi: 10.1007/s10900-010-9339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sangwan RK, Huda RK, Panigrahi A, Toteja GS, Sharma AK, Thakor M, Kumar P. Strengthening breast cancer screening program through health education of women and capacity building of primary healthcare providers. Front Public Health. 2023;11:1276853. doi: 10.3389/fpubh.2023.1276853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu Y, Min H, Li M, Shi Y, Ma A, Han Y, Gan Y, Guo X, Sun X. Effect of Artificial Intelligence-based Health Education Accurately Linking System (AI-HEALS) for Type 2 diabetes self-management: protocol for a mixed-methods study. BMC Public Health. 2023;23:1325. doi: 10.1186/s12889-023-16066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aggarwal A, Tam CC, Wu D, Li X, Qiao S. Artificial Intelligence-Based Chatbots for Promoting Health Behavioral Changes: Systematic Review. J Med Internet Res. 2023;25:e40789. doi: 10.2196/40789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ponzo V, Goitre I, Favaro E, Merlo FD, Mancino MV, Riso S, Bo S. Is ChatGPT an Effective Tool for Providing Dietary Advice? Nutrients. 2024;16 doi: 10.3390/nu16040469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peng W, Feng Y, Yao C, Zhang S, Zhuo H, Qiu T, Zhang Y, Tang J, Gu Y, Sun Y. Evaluating AI in medicine: a comparative analysis of expert and ChatGPT responses to colorectal cancer questions. Sci Rep. 2024;14:2840. doi: 10.1038/s41598-024-52853-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kanjee Z, Crowe B, Rodman A. Accuracy of a Generative Artificial Intelligence Model in a Complex Diagnostic Challenge. JAMA. 2023;330:78–80. doi: 10.1001/jama.2023.8288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Atiyyat N, Ibraheemi AA, Rababa M, Othman WM, Khait AA, Jaradat DAS. Public Awareness of Palliative Care: A Nationally Representative Sample of Jordanian Adults. J Pain Symptom Manage. 2024;68:123–131. doi: 10.1016/j.jpainsymman.2024.04.016. [DOI] [PubMed] [Google Scholar]
- 30.Kreps GL, Sparks L. Meeting the health literacy needs of immigrant populations. Patient Educ Couns. 2008;71:328–332. doi: 10.1016/j.pec.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 31.Azizoddin DR, Adam R, Kessler D, Wright AA, Kematick B, Sullivan C, Zhang H, Hassett MJ, Cooley ME, Ehrlich O, Enzinger AC. Leveraging mobile health technology and research methodology to optimize patient education and self-management support for advanced cancer pain. Support Care Cancer. 2021;29:5741–5751. doi: 10.1007/s00520-021-06146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao Q, Qiu X, Liu W, Nian Z, Chen T, Chen J, Xie R, Yang L. Application of a WeChat Mini Program to provide pharmaceutical care for cancer pain patients: A randomized controlled trial. Digit Health. 2024;10:20552076241255654. doi: 10.1177/20552076241255654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu Q, Jin Z, Wang P. The Relationship Between the Physician-Patient Relationship, Physician Empathy, and Patient Trust. J Gen Intern Med. 2022;37:1388–1393. doi: 10.1007/s11606-021-07008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo Y, Liu Y, Chen H, Zhang X, Luo R, Zhu Y, Feng Z, Sun Y, Wang S. How about trust in physician-patient relationship? A concept analysis of physicians' perspectives. Patient Educ Couns. 2023;112:107709. doi: 10.1016/j.pec.2023.107709. [DOI] [PubMed] [Google Scholar]
- 35.Scharrer L, Rupieper Y, Stadtler M, Bromme R. When science becomes too easy: Science popularization inclines laypeople to underrate their dependence on experts. Public Underst Sci. 2017;26:1003–1018. doi: 10.1177/0963662516680311. [DOI] [PubMed] [Google Scholar]
- 36.Paul PV. Fake News, Alternative Facts, Post-Truths, Misinformation, Misinterpretation-and Other Challenges Associated With Knowledge Generation. Am Ann Deaf. 2017;162:3–7. doi: 10.1353/aad.2017.0010. [DOI] [PubMed] [Google Scholar]
- 37.Stilgoe J, Lock SJ, Wilsdon J. Why should we promote public engagement with science? Public Underst Sci. 2014;23:4–15. doi: 10.1177/0963662513518154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.