Abstract
Background
Hypertension is one of the main factors contributing to the global burden of non-communicable diseases. Previous research has revealed that stress, bad lifestyle choices and a lack of knowledge about the disease are the main causes of hypertension that can be controlled. The key cause behind the prevalence of the condition is the lack of medication adherence by patients. This study aims to evaluate medication adherence in patients with hypertension through the Morisky Medication Adherence Scale (MMAS) and to observe any adverse drug reaction leading to non-adherence of medications.
Methods
A descriptive, cross-sectional study was conducted on 124 patients who attended the outpatient department of medicine. The descriptive tools were MMAS and causality scales for adverse drug reactions.
Result
The mean MMAS score was 5.20±1.29. Amongst the demographic profile, age, sex, comorbidities and duration of disease were significantly associated with decreased mean MMAS scores. Forty-two patients experienced drug reactions and only four patients were adherent to their medications.
Conclusion
Our study suggests that patients were poorly adherent to their medications. Effective interventions should be considered to improve adherence in patients. Monitoring for adverse drug reactions can lead to improved patient outcomes, whilst interventions to improve adherence can lead to better blood pressure control and reduced risk of cardiovascular events.
Keywords: adverse drug reaction, hypertension, medication adherence, MMAS-8
Introduction
In India, at least one in four adults has hypertension yet only 12% of them have their blood pressure under control.1 One of the main factors contributing to the global burden of non-communicable diseases is hypertension, with regional and racial variations in the prevalence of hypertension that may be caused by both environmental and hereditary factors. Hypertension is a chronic medical condition in which the blood vessels have persistently raised pressure2,3 and is responsible for an estimated 1.6 fatalities each year in India, with 24% of deaths due to coronary heart disease and 57% due to stroke.4,5 According to recent estimates in India, the frequency of deaths is greater in urban regions as compared to rural areas (33.8% versus 27.6%; p=0.05) and the overall death rate is 29.8% (95% CI 26.7–33).6 According to the 2018 Indian Council of Medical Research data, 10.8% of all deaths in India are attributed to hypertension, with many of those who pass away being unaware of their condition.3 In India, the prevalence of adult-onset hypertension has dramatically increased over the past three decades, with urban prevalence at 33% and rural prevalence at 25%.7
The cause of hypertension is often not known. In many cases, it may be due to accompanying comorbid conditions. Primary causes include age (>65 years), obesity, insulin intake, high salt diet, excessive salt intake, sedentary lifestyle and smoking. Secondary causes include cardiovascular diseases, chronic kidney disease, diabetes, pheochromocytoma, pregnancy, sleep apnoea and hyperthyroidism. Previous research has revealed that stress and lack of knowledge about the disease have also contributed to the causes of hypertension that can be controlled. However, the crucial cause behind the prevalence of hypertension is the lack of adherence of the patient to their medicine.8
Medication adherence is described by the World Health Organization as the degree to which a person’s behaviour corresponds with the agreed recommendations from a health care provider.7 Poor adherence to hypertension regimens can have major health repercussions, possibly leading to ischaemic heart disease, myocardial infarction, stroke and other types of heart disease.8 The consequences of non-adherence to hypertensive medication range from end-organ damage associated with hypertension, such as microalbuminuria, stroke and heart failure as well as treatment failure, reduced functional abilities, a lower quality of life and additional medical/surgical procedures.
Compared to advanced economies, non-adherence rates are higher in developing nations. Studies conducted in the northern zone of India have found that the percentage of patients with hypertension who do not adhere to their medications as prescribed ranges from 19% to 96%.9,10 The varying rates may be due to multiple factors that affect adherence. The possible reasons for non-adherence in India may be patient-related fear, mistrust, financial problems, recall problems, access concerns, difficulty in remembering to take medicines or doctor-related lack of communication with patients and healthcare system issues. Indeed, 78% of patients reported that is difficult to pay for medication and 54% indicated that it is difficult to get refill on time.11,12
A study conducted in West India reported that 76.5% of patients with hypertension were non-adherent to their medication.13 A study by Misra et al.14 stated that adherence was improved by 18.9% by pill count method and by 27.4% using a reminder system. Not taking the right dose or abandoning treatment altogether can lead to disease progression, cardiovascular risk, mortality and prolonged hospitalization.15
As the benefits of the treatment cannot be completely appreciated unless blood pressure is effectively controlled, ensuring adherence is as crucial as the diagnosis itself. Understanding the causes of poor adherence can aid in preventing problems, developing and focusing interventions to improve adherence in the hypertensive population. Therefore, this study was conducted to examine the factors related with non-adherence to medications and to identify side-effects due to the scarcity of data about it in our region.
Methods
Study design and setting
This was an institution-based cross-sectional study conducted over 3 months. The study was conducted in accordance with the ethical standards of the Teerthanker Mahaveer Medical College and Research Centre. The size of the study population to be recruited into the research was calculated using the formula n=z2α/2P (100−P)/E2, where Zα/2 is standard normal variate, P is prevalence rate and E is allowable error. Hence, Zα/2 was taken as 1.96 at 95% CI, P (according to a previous study8) as 29.8% and E as 10%. Therefore, the minimum sample size was calculated to be ~80. A total of 124 patients were recruited for the study.
Inclusion and exclusion criteria
Inclusion criteria
All patients of either sex, aged 18 years or above, diagnosed with hypertension and on antihypertensive medication for more than 6 months were included in the study. Informed consent was taken from patients before inclusion.
Exclusion criteria
Pregnant and lactating women were excluded from the study. Patients who refused to participate in the study were also excluded.
Dependent variable
The data were collected through interview method. The dependent variable was adherence to prescribed antihypertensive medications. Adherence was assessed using the eight-item Morisky Medication Adherence Scale (MMAS-8),9 where total scores of <6 indicated low adherence, 6–8 indicated medium adherence, and >8 indicated high adherence.16
Independent variables
Sociodemographic factors were age, sex, marital status, religion, ethnicity and level of education. Personal factors were comorbidities, knowledge about the disease and duration of hypertension. The data were collected using a pre-formed questionnaire approved by the ethical committee of the Teerthanker Mahaveer Medical College and Research Centre.
Pharmacovigilance monitoring
Adverse drug reactions (ADRs) were assessed through interview at the time of recruitment. Information on ADRs was analyzed using ADR reporting form provided by IPC version 1.4.17 ADRs were analyzed using the WHO causality assessment scale.18
Data analysis
The respondents’ demographic traits were depicted using descriptive statistics. The continuous variables were expressed as mean standard deviation and categorical variables were measured as percentages. To identify the type of data distribution, the Kolmogorov–Smirnov test was used. Whilst Spearman’s rank correlation coefficient was used to assess the relationship between the study variables, inferential statistics (Mann–Whitney U test and Kruskal–Wallis test) were used to evaluate the difference. For the Mann–Whitney U test and Kruskal–Wallis test, a p value of 0.05 was considered significant. The data were entered in Microsoft Excel 2016 and then exported into SPSS VERSION 21.
Ethical considerations
Consent for the protocol was given by the Constitutional Review Committee. The study was approved by Institutional Ethical Committee (Teerthanker Mahaveer Medical College and Research Centre).
Results
Demographic characteristics
A total of 124 patients were recruited in the study (Table 1). The Kolmogorov–Smirnov test revealed non-normal distribution of the data. Mean age of the study participants was 54.07±10.76 years. The sex distribution revealed that 52 (58.1%) women were non-adherent. Participants above 60 years were less adherent (3.11±1.53). Adherence (4.97±1.23) was less in employed individuals as compared to unemployed participants. Patients with comorbid diseases, like diabetes (n=62), cardiovascular diseases (n=38) and cerebrovascular diseases (n=24) were moderately adherent to their medications. Participants in a high-income group (>US$7000 per year) showed low adherence. Literacy did not affect the adherence level as both educated and uneducated patients were moderately adherent (5.06±1.77). Middle socioeconomic class participants were highly adherent. Duration of the disease did not affect adherence level of the medications.
Table 1.
Sociodemographic profile of patients and MMAS-8 score.
| Description | N (%) | MMAS score | p value |
|---|---|---|---|
| Age* (54.07±10.76), years |
0.003 |
||
| 18–39 years | 11 (8.9) | 5.27±0.904 | |
| 40–59 years | 76 (61.3) | 5.24±1.25 | |
| ≥60 years | 37 (29.8) | 3.11±1.53 | |
| Sex ** |
0.005 |
||
| Male | 52 (41.9) | 5.11±1.18 | |
| Female | 72 (58.1) | 3.26±1.37 | |
| Marital status ** |
0.489 |
||
| Married | 120 (96.8) | 5.20±1.3 | |
| Unmarried | 4 (3.2) | 5±0.82 | |
| Residence ** |
0.560 |
||
| Rural | 65 (52.4) | 5.2±1.27 | |
| Urban | 59 (47.6) | 5.15±1.32 | |
| Occupation * |
0.391 |
||
| Housewife | 56 (45.2) | 5.3±1.44 | |
| Employed | 36 (29) | 4.97±1.23 | |
| Unemployed | 18 (14.5) | 5.44±1.04 | |
| Retired | 14 (11.3) | 5.07±1.14 | |
| Comorbidities * |
0.009 |
||
| Diabetes | 62 (50) | 5.38±1.27 | |
| Patients with heart disease | 38 (30.6) | 5.07±1.36 | |
| Patient with cerebrovascular disease | 24 (19.4) | 4.91±1.21 | |
| Income * |
0.104 |
||
| <US$2000/year | 17 (13.7) | 5.58±1.8 | |
| US$2000–US$7000$/year | 99 (79.8) | 5.16±1.2 | |
| >US$7000/year | 8 (6.5) | 4.87±0.99 | |
| Literacy * |
0.894 |
||
| Illiterate | 29 (23.4) | 5.06±1.77 | |
| Primary | 30 (24.21) | 5.26±1.14 | |
| Secondary | 15 (12.1) | 5.06±1.38 | |
| Graduate | 50 (40.3) | 5.28±1.03 | |
| Socioeconomic class * | 0.283 | ||
| Poor | 18 (14.5) | 5.5±1.82 | |
| Lower class | 96 (77.4) | 5.13±1.21 | |
| Lower middle class | 10 (8.1) | 6.3±0.94 | |
| Duration* of disease | 0.001 | ||
| <5 year | 36 (29) | 6.97±1.5 | |
| 5–10 year | 66 (53.21) | 5.25±1.18 | |
| >10 year | 22 (17.7) | 5.4±1.25 | |
Kruskal–Wallis test;
Mann–Whitney p<0.05.
MMAS-8
The mean MMAS-8 score was 5.20±1.29. The median was 6 and mode was 6. MMAS-8 score was assessed using eight questions. Each question was assessed according to positive attitude (medication compliance) and a negative attitude (medication non-compliance). A score of 1 was given for negative attitude and 0 for positive attitude. Figure 1 shows the frequency of positive and negative attitude. The majority (66.1%) of participants regularly forgot to take their high blood pressure medication. Only 29% of the patients missed taking their medications for reasons other than forgetting. Overall, 89 (71.8%) patients never stopped taking medication without telling the doctor and 76 (61.3%) patients forgot to take medications along with them when travelling or leaving home. About 98% of patients took medications a day before the visiting the doctor. Only 38% patients did not take medicine if they felt that their blood pressure was under control. Thirty-four patients felt hassled about sticking to their blood pressure treatment plan. Only 18.5% of patients sometimes had difficulty remembering to take their blood pressure medication. The prevalence of negative responses to MMAS-8 components in terms of non-adherence was greater in women. MMAS-8 components 5 and 8 were significantly associated with sex (Table 2). Women (48.4%) more often forget to take their medications than men, whereas men (13.7%) had difficulty in taking all medications.
Figure 1.
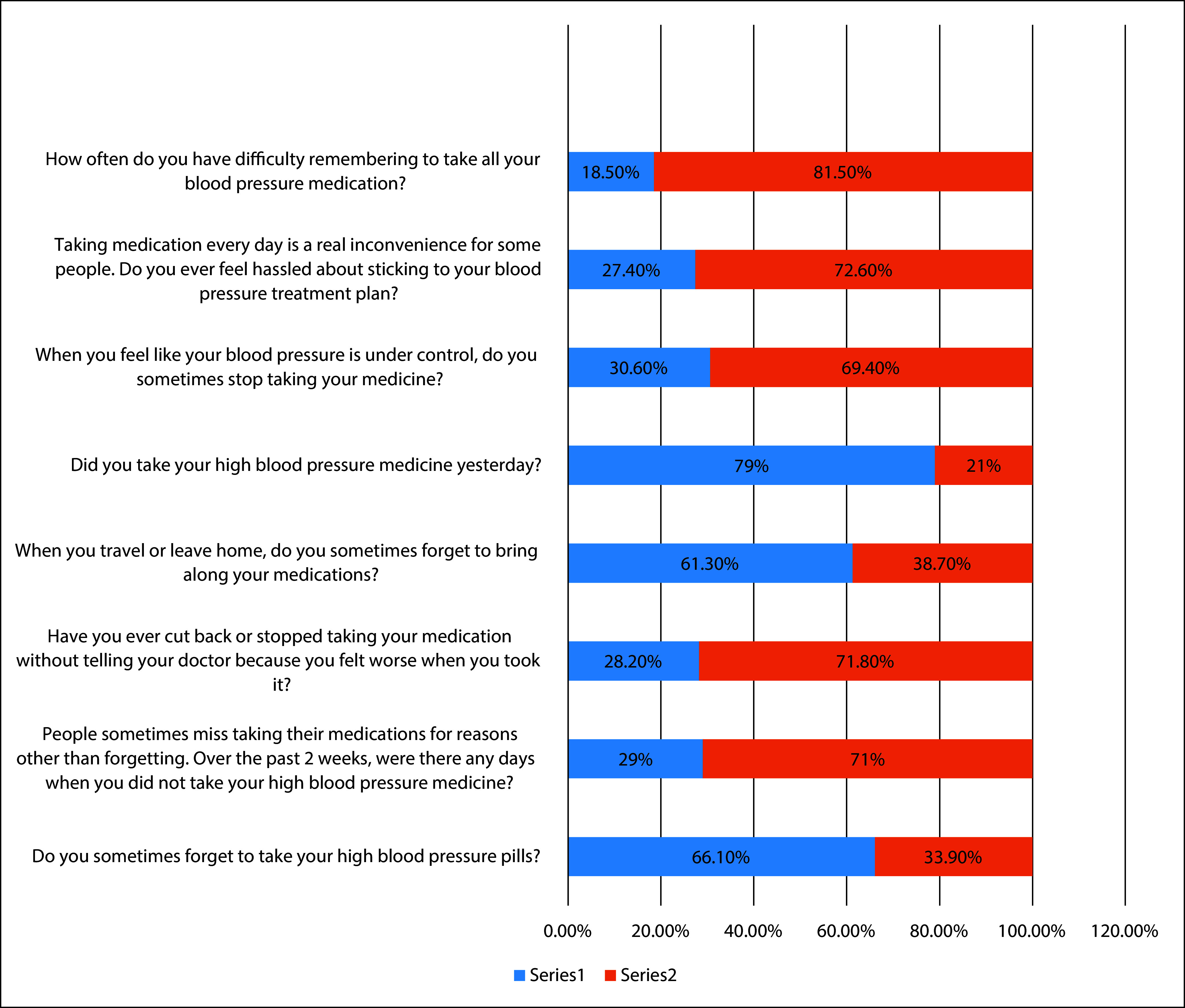
Frequency of responses of MMAS questions. Series 1 (depicted in blue) negative attitude and series 2 (depicted in orange) positive attitude.
Table 2.
Association of gender with MMAS-8 components (*p<0.05).
| MMAS-8 components | Yes | Male (yes) | Female (Yes) | χ2 value | p value |
|---|---|---|---|---|---|
| Component 5: Did you take your high blood pressure medicine yesterday? | 98 (79%) | 38 (30.6%) | 60 (48.4%) | 1.91 | 0.003* |
| Component 8: How often do you have difficulty remembering to take all your blood pressure medication? | 23 (18.5%) | 12.9 (13.7%) | 7 (5.6%) | 1.534 | 0.002* |
χ2 test,
p<0.05.
Pharmacological class of drug used
The majority (107) of patients were using angiotensin receptor blockers (ARBs). Eight (6.5%) patients were using a calcium channel blocker. Diuretics were used by five (4%) patients. Only four (3.2%) patients were on polytherapy (a combination of ARBs, calcium channel blocker and diuretics).
ADRs
Out of 124 patients, 42 (33%) experienced an ADR. Amongst 124 patients, 121 patients received ARBs. Thirty-five patients experienced ADR such as dizziness (31.43%), angioedema (51.14%), nausea (20%) or weakness (20%) due to ARBs. Ten patients experienced ADRs due to calcium channel blockers such as pedal oedema (20%) and tremors (30%). Only four patients experienced ADRs due to diuretics, including muscle cramps (28.57%) and headache (28.57%). The prevalence of ADR and causality assessment as per WHO-UMC scale is shown in Table 3.
Table 3.
Frequency of adverse drug reactions and WHO causality assessment.
| Drugs | Adverse drug events | Total no of patients with adverse drug events/no. of patients receiving drugs | % Adverse drug events | Causality assessment |
|---|---|---|---|---|
| Angiotensin receptor blockers | Dizzziness (11) | 35/121 | 28.92 | Probable |
| Angioedema (20) | Probable | |||
| Nausea (7) | Possible | |||
| Weakness (7) | Unlikely | |||
| Calcium channel blocker | Pedal oedema (2) | 3/10 | 30 | Probable |
| Tremors (3) | Possible | |||
| Diuretic | Muscle cramps (2) | 4/7 | 57.14 | Unlikely |
| Headache (2) | Probable |
Adherence
Only four patients were highly adherent to the medications and 120 patients were non-adherent (56 were moderately adherent and 64 had low adherence). The mean MMAS-8 score for low adherence was 4.01±1.07 and that for moderate adherence was 6.03±0.18. Descriptive analysis of adherence level is shown in Figure 2.
Figure 2.
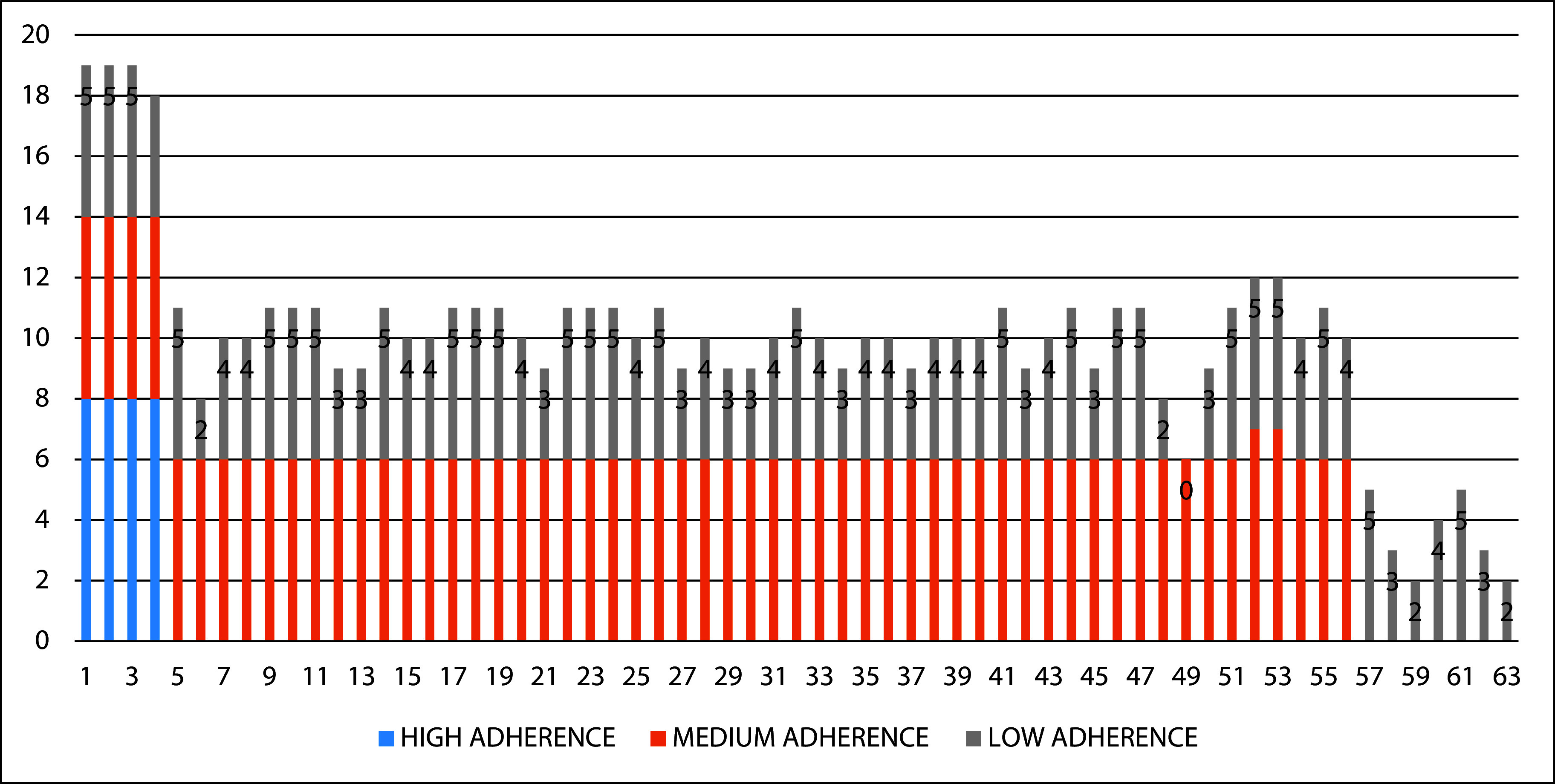
Descriptive analysis according to adherence.
Discussion
Hypertension is one of the most common non-communicable diseases. Increased drug compliance for chronic illness can considerably reduce hospital admission, enhance the quality of life and lower healthcare expenses. The overall medication adherence was very low in this study. About 75% of patients were non-adherent to the medications. Our results were contrary to those of Ramli et al.,19 Boratas et al.20 and Patel et al.21 where the majority (>50%) of the recruited participants were adherent to their medications. In our study, the poor medication adherence rate was 38.71% and medium adherence level was 58.61%. Similar findings were obtained by Alsolami et al.22 and Maciel et al.23 In our study, men were more adherent to the hypertensive medication, in contradiction to the studies by Tibebu et al.,24 Mebrahtu et al.25 and Mekonnen et al.26 where women were more adherent. This can be due to women being less vigilant concerning their care of health. In our study, patients older than 60 years were less adherent to their medications. Similar findings were seen in studies conducted in Ethopia26 and Korea.27
The decreased medication adherence amongst patients with hypertension highlights the role of importance of education and various sociodemographic factors like gender, education and income. The potential reasons for low adherence may be social and cultural barriers specific to the population under study. Stigma is a common reason for non-adherence. The fear of stigmatization can be so intense that patients prefer not to take their medications if there is a possibility that someone might be watching. Additionally, lack of support from family members can have a substantial effect on adherence.23 Good access to the healthcare system and enough time for discussion of illness are necessary to ensure patient adherence.24 Support from healthcare providers and freely accessible care appear to increase adherence.22 Financial stability is another factor that may contribute to adherence because family needs and food are much more important than medication costs.25 Lack of understanding of medical insurance is another factor that leads to non-adherence in low- and middle-income countries.25
Patients at the extremes of age frequently have various comorbid conditions and poor memory and as a result engage in non-adherence to treatment. Patients taking hypertensive drugs for less than 5 years exhibited higher adherence than patients taking them for more than 5 years (Table 1). The majority (86.3%) of the patients were on monotherapy for hypertension. ARBs were the most commonly drug used. According to available studies,28 monotherapy is frequently used to treat hypertension. In fact, 76% of patients with hypertension were receiving monotherapy. According to studies conducted by Gupta et al.29 and Williams et al.,30 the pharmacological class of drug employed may change according to patient demographics, comorbidities and doctor preference. ARBs are suggested as a first-line therapy choice for hypertension due to their effectiveness in lowering blood pressure and preventing cardiovascular events.
Improving medication adherence to antihypertensive therapy in patients with hypertension can lead to better blood pressure control and a reduced risk of cardiovascular events. There are several strategies that healthcare providers can use to promote adherence to medication regimens in patients with hypertension, including patient education, simplification of medication regimens and use of reminder systems.31,32 Healthcare providers can also supply patients with written materials or online resources to reinforce these messages.33,34
A multifaceted intervention by Nieuwlaat et al.35 that included patient education, medication reminders and pharmacist-led reminders led to improved adherence and blood pressure control in patients with hypertension. Simplification of medication32 regimens includes reducing the number of medications that patients are taking, simplifying dosing schedules and using combination medications that contain multiple antihypertensive agents. It can also reduce the complexity of treatment and make it easier for patients to adhere to their prescribed medication regimen. Reminder systems are another effective strategy for improving medication adherence in patients with hypertension. This can include using pill boxes or medication organizers, setting alarms or reminders on mobile devices or electronic devices, or using tele-monitoring systems that remind patients to take their medications and provide feedback on adherence.36,37 Health literacy is an important factor that can impact medication in patients with hypertension. Patients with low literacy may have difficulty in medication instructions or recognizing the importance of taking their medications as prescribed. Healthcare providers can use plain language when communicating with patients, use visual aids or demonstrations to reinforce instructions, and provide written materials that are easy to understand.38,39 Two crucial components of antihypertensive medication – pharmacovigilance and adherence –have received substantial research in medical field.40
ADRs associated with antihypertensive drugs can range from mild symptoms, such as dizziness and fatigue, to more serious complications such as hypotension, electrolyte imbalances and renal failure. Monitoring for ADRs is especially important in patients who are taking multiple medications or who have comorbidities that increase their risk of adverse effects. About 33% of patients experienced ADRs in our study. Similar results were seen in the study done by Husain et al.41 and Palikhey et al.42 Calcium channel blockers were the cause of the ADR of oedema in agreement with previous studies. Amlodipine most likely raises hydrostatic pressure in the lower extremities, which causes pedal oedema, as a result of precapillary dilation and post capillary constrictions.34 Diuretics are known to induce fluid or electrolyte imbalances, which could be the reason for the typical side-effects such as light-headedness and muscle cramps.35 Most of the ADRs in our study were possible (49.15%) followed by probable (35.59%) and then unlikely (15.25%), consistent with studies by Palikhey et al.,42 Husain et al.41 and Mishra et al.43
Unpleasant side-effects caused by drugs have a significant impact of medication adherence and quality of life. Patients that experience ADRs are non-adherent, leading to physical harm, mental stress and prolonged hospital visits. The effectiveness of pharmacovigilance monitoring in patients receiving antihypertensive therapy has been assessed in number of studies. For instance, Husain et al.41 found that monitoring for ADR in elderly patients with hypertension led to a reduction in hospitalization. Pharmacovigilance monitoring and adherence interventions have shown promising results improving patient outcomes in antihypertensive therapy.44 Studies have concluded that interventions comprising pharmacist-led medication reconciliation, patient counseling, collaborative care involving pharmacists and doctors, and automated voice messages improved patient adherence by 15%.45
There are also challenges associated with these strategies that need to be addressed. One major challenge is patient non-compliance, which can be intentional or unintentional. Intentional non-compliance can be due to a variety of factors, including concerns about medication side-effects, lack of trust in healthcare providers and financial constraints. Unintentional non-compliance can be due to forgetfulness, difficulty in understanding medication instructions or lack of social support. Despite these challenges, there is growing recognition of the importance of adherence and pharmacovigilance monitoring in antihypertensive therapy.
Conclusion
Research confirms the existence of non-adherence to medication as a problem amongst patients with hypertension in India. The low adherence is significantly associated with sex, comorbidities and duration of disease. The medications were associated with unpleasant side-effects that may also have led to low adherence. All the ADRs mentioned in the study are treatable and can be managed if proper education is provided to the patients.
Improving medication adherence in patients with hypertension is an important component of antihypertensive therapy that can lead to better patient outcomes. However, there are also challenges associated with these strategies such as patient non-compliance and difficulty in identifying ADRs. The present study suggests that further research is needed to implement health education programmes and increase awareness, with interventions being required to improve outcomes of patients with chronic diseases like hypertension.
Limitations
The study was conducted for a very short time and so the sample size was very small.
Acknowledgements
The authors would like to acknowledge medicine department for allowing them to conduct the study.
Footnotes
Disclosure and potential conflicts of interest: The authors declare that they have no conflicts of interest relevant to this manuscript. All other authors declare no conflict of interest. The International Committee of Medical Journal Editors (ICMJE) Potential Conflicts of Interests form for the authors is available for download at: https://www.drugsincontext.com/wp-content/uploads/2024/09/dic.2024-5-2-COI.pdf
Funding declaration: There was no funding associated with the preparation of this article.
Correct attribution: Copyright © 2024 Agrawal P, Patrick S, Thomas M, Gupta D, Singh Matreja P, Singh P, Zafar S. https://doi.org/10.7573/dic.2024-5-2. Published by Drugs in Context under Creative Commons License Deed CC BY NC ND 4.0.
Provenance: Submitted, fee waiver; externally peer reviewed.
Drugs in Context is published by BioExcel Publishing Ltd. Registered office: 6 Green Lane Business Park, 238 Green Lane, New Eltham, London, SE9 3TL, UK.
BioExcel Publishing Limited is registered in England Number 10038393. VAT GB 252 7720 07.
For all manuscript and submissions enquiries, contact the Editorial office editorial@drugsincontext.com
For all permissions, rights, and reprints, contact David Hughes david.hughes@bioexcelpublishing.com
Contributions: Conceptualization: SP and PM were involved in formulation or evolution of overarching research goals and aims. Methodology: all authors were involved. Software: PA. Validation: all authors were involved. Formal analysis: all authors were involved. Investigation: SZ and PA. Resources: All authors were involved in study material. Project administration: PM and PS were involved with management and co-ordination responsibility for the research activity planning and execution. Funding acquisition: all authors were involved. Visualization: DG and PS were involved in the preparation, creation and/or presentation of the published work, specifically visualization/data presentation. Writing of original draft: all authors were involved with preparation, creation and/or presentation of the published work, specifically writing the initial draft. Writing, review and editing: all authors were involved in the preparation, creation and/or presentation of the published work by those from the original research group, specifically critical review, commentary or revision, including pre- or post-publication stages. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
References
- 1.Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Diabetes and hypertension in India: a nationally representative study of 1.3 million adults. JAMA Intern Med. 2018;178(3):363–372. doi: 10.1001/jamainternmed.2017.8094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vijna, Mishra CP. Prevalence and predictors of hypertension: evidence from a study of rural India. J Family Med Prim Care. 2022;11(3):1047–1054. doi: 10.4103/jfmpc.jfmpc_967_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kotwal A, Joseph P. Conquering the silent killer: hypertension prevention and management in India. Indian J Community Med. 2023;48(1):1–3. doi: 10.4103/ijcm.ijcm_1000_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R, Yusuf S. Towards better hypertension management in India. Indian J Med Res. 2014;139(5):657–660. [PMC free article] [PubMed] [Google Scholar]
- 5.King-Shier KM, Dhaliwal KK, Puri R, LeBlanc P, Johal J. South Asians’ experience of managing hypertension: a grounded theory study. Patient Prefer Adherence. 2019;13:321–329. doi: 10.2147/PPA.S196224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anchala R, Kannuri NK, Pant H, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–314. doi: 10.4065/mcp.2010.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26(3):155–159. doi: 10.5001/omj.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herttua K, Tabák AG, Martikainen P, Vahtera J, Kivimäki M. Adherence to antihypertensive therapy prior to the first presentation of stroke in hypertensive adults: population-based study. Eur Heart J. 2013;34:2933–2939. doi: 10.1093/eurheartj/eht219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Q, Chang A, Ritchey MD, Loustalot F. Antihypertensive medication adherence and risk of cardiovascular disease among older adults: a population-based cohort study. J Am Heart Assoc. 2017;6:e006056. doi: 10.1161/JAHA.117.006056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhandari S, Sarma PS, Thankappan KR. Adherence to antihypertensive treatment and its determinants among urban slum dwellers in Kolkata, India. Asia Pac J Public Health. 2015;27:NP74–NP84. doi: 10.1177/1010539511423568. [DOI] [PubMed] [Google Scholar]
- 12.Chadha SL, Radhakrishnan S, Ramachandran K, Kaul U, Gopinath N. Prevalence, awareness and treatment status of hypertension in urban population of Delhi. Indian J Med Res. 1990;92:233–240. [PubMed] [Google Scholar]
- 13.Nagarkar AM, Gadhave SA, Sharma I, Choure A, Morisky D. Factors influencing medication adherence among hypertensive patients in a tertiary care hospital, Pune, Maharashtra. Natl J Community Med. 2013;4:559–563. [Google Scholar]
- 14.Misra P, Salve HR, Srivastava R, Kant S, Krishnan A. Adherence to treatment among hypertensive individuals in a rural population of North India. Indian J Community Health. 2017;29(2):176–181. doi: 10.47203/IJCH.2017.v29i02.009. [DOI] [Google Scholar]
- 15.Hamrahian SM, Maarouf OH, Fülöp T. A critical review of medication adherence in hypertension: barriers and facilitators clinicians should consider. Patient Prefer Adherence. 2022;16:2749–2757. doi: 10.2147/PPA.S368784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uchmanowicz B, Jankowska EA, Uchmanowicz I, Morisky DE. Self-reported medication adherence measured with Morisky Medication Adherence Scales and its determinants in hypertensive patients aged ≥60 years: a systematic review and meta-analysis. Front Pharmacol. 2019;10:168. doi: 10.3389/fphar.2019.00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Performance Report of Pharmacovigilance Programme of India, 2017–18. Ghaziabad: Indian Pharmacopoeia Commission; 2018. [Accessed September 14, 2024]. pp. 24–42. https://www.ipc.gov.in/PvPI/pub/Annual%20Performace%20Report%202017-18.pdf . [Google Scholar]
- 18.Zaki SA. Adverse drug reaction and causality assessment scales. Lung India. 2011;28(2):152–153. doi: 10.4103/0970-2113.80343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence. 2012;6:613–622. doi: 10.2147/PPA.S34704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boratas S, Kilic HF. Evaluation of medication adherence in hypertensive patients and influential factors. Pak J Med Sci. 2018;34(4):959–963. doi: 10.12669/pjms.344.14994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Ann Pharmacother. 2002;36(1):40–45. doi: 10.1345/aph.1A046. [DOI] [PubMed] [Google Scholar]
- 22.Alsolami F, Correa-Velez I, Hou XY. Factors affecting antihypertensive medications adherence among hypertensive patients in Saudi Arabia. Am J Med Sci. 2015;5(4):181–189. [Google Scholar]
- 23.Maciel APF, Pimenta HB, Caldeira AP. Quality of life and medication adherence in hypertensive patients. Acta Paul Enferm. 2016;29:542–548. doi: 10.1590/1982-0194201600075. [DOI] [Google Scholar]
- 24.Tibebu A, Mengistu D, Bulto LN. Adherence to prescribed antihypertensive medications and associated factors for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Int J Health Sci. 2017;11(4):47–52. [PMC free article] [PubMed] [Google Scholar]
- 25.Mebrahtu G, Moleki M, Okoth Achila O, Seyoum Y, Adnoy ET, Ovberedjo M. Antihypertensive medication adherence and associated factors: a cross-sectional analysis of patients attending a national referral hospital in Asmara, Eritrea. Patient Prefer Adherence. 2021;15:2619–2632. doi: 10.2147/PPA.S319987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mekonnen HS, Gebrie MH, Eyasu KH, Gelagay AA. Drug adherence for antihypertensive medications and its determinants among adult hypertensive patients attending in chronic clinics of referral hospitals in Northwest Ethiopia. BMC Pharmacol Toxicol. 2017;18(1):27. doi: 10.1186/s40360-017-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee H, Yano Y, Cho SMJ, et al. Adherence to antihypertensive medication and incident cardiovascular events in young adults with hypertension. Hypertension. 2021;77(4):1341–1349. doi: 10.1161/HYPERTENSIONAHA.120.16784. [DOI] [PubMed] [Google Scholar]
- 28.Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120(8):713–719. doi: 10.1016/j.amjmed.2006.08.033. [DOI] [PubMed] [Google Scholar]
- 29.Gupta P, Patel P, Štrauch B, et al. Risk factors for nonadherence to antihypertensive treatment. Hypertension. 2017;69(6):1113–1120. doi: 10.1161/HYPERTENSIONAHA.116.08729. [DOI] [PubMed] [Google Scholar]
- 30.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041. doi: 10.1093/eurheartj/ehy339. . Erratum in: Eur Heart J 2019; 40(5)475. [DOI] [PubMed] [Google Scholar]
- 31.Saleem F, Hassali MA, Shafie AA, Atif M. Drug attitude and adherence: a qualitative insight of patients with hypertension. J Young Pharm. 2012;4:101. doi: 10.4103/0975-1483.96624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Geffen EC, Hermsen JH, Heerdink ER, Egberts AC, Verbeek-Heida PM, van Hulten R. The decision to continue or discontinue treatment: experiences and beliefs of users of selective serotonin-reuptake inhibitors in the initial months – a qualitative study. Res Soc Adm Pharm. 2011;7:134–150. doi: 10.1016/j.sapharm.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Cross AJ, Elliott RA, Petrie K, Kuruvilla L, George J. Interventions for improving medication-taking ability and adherence in older adults prescribed multiple medications. Cochrane Database Syst Rev. 2020;5(5):CD012419. doi: 10.1002/14651858.CD012419.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kini V, Ho PM. Interventions to improve medication adherence: a review. JAMA. 2018;320(23):2461–2473. doi: 10.1001/jama.2018.19271. [DOI] [PubMed] [Google Scholar]
- 35.Nieuwlaat R, Wilczynski N, Navarro T, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;2014(11):CD000011. doi: 10.1002/14651858.CD000011.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elnaem MH, Irwan NA, Abubakar U, Sulaiman SAS, Elrggal ME, Cheema E. Impact of medication regimen simplification on medication adherence and clinical outcomes in patients with long-term medical conditions. Patient Prefer Adherence. 2020;14:2135–2145. doi: 10.2147/PPA.S268499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wan LH, Zhang XP, You LM, Ruan HF, Chen SX. The efficacy of a comprehensive reminder system to improve health behaviors and blood pressure control in hypertensive ischemic stroke patients: a randomized controlled trial. J Cardiovasc Nurs. 2018;33(6):509–517. doi: 10.1097/JCN.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 38.Patel S, Jacobus-Kantor L, Marshall L, et al. Mobilizing your medications: an automated medication reminder application for mobile phones and hypertension medication adherence in a high-risk urban population. J Diabetes Sci Technol. 2013;7(3):630–639. doi: 10.1177/193229681300700307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guo A, Jin H, Mao J, et al. Impact of health literacy and social support on medication adherence in patients with hypertension: a cross-sectional community-based study. BMC Cardiovasc Disord. 2023;23(1):93. doi: 10.1186/s12872-023-03117-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schönfeld MS, Pfisterer-Heise S, Bergelt C. Self-reported health literacy and medication adherence in older adults: a systematic review. BMJ Open. 2021;11(12):e056307. doi: 10.1136/bmjopen-2021-056307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Husain A, Aqil M, Alam M, Khan M, Kapur P, Pillai K. A pharmacovigilance study of antihypertensive medicines at a South Delhi Hospital. Indian J Pharm Sci. 2009;71:338–341. doi: 10.4103/0250-474X.56018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palikhey A, Chaudhary R, Shrestha L, et al. Prevalence of adverse drug reactions of anti-hypertensive drugs in a tertiary care hospital, Bhairahawa, Nepal. J Coll Med Sci Nepal. 2022;18(4):415–421. [Google Scholar]
- 43.Mishra S, Syed Ahmad SS, Nigam N, et al. Adverse drug reaction monitoring among hypertensive patients of tertiary care center of north India related to antihypertensive drugs. Asian J Pharm Clin Res. 2021;14(3):157–160. doi: 10.22159/ajpcr.2021.v14i3.40496. [DOI] [Google Scholar]
- 44.Yadav L, Dutta S, Sharma J, Rai RK, Matreja PS, Pahwa I. A pharmacovigilance study to analyze the adverse drug reactions in patients treated with antihypertensive drug in tertiary care teaching hospitals. J Popul Therapeut Clin Pharmacol. 2024;31(4):1225–1233. doi: 10.53555/jptcp.v31i4.5741. [DOI] [Google Scholar]
- 45.Ho PM, Lambert-Kerzner A, Carey EP, et al. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med. 2014;174(2):186–193. doi: 10.1001/jamainternmed.2013.12944. [DOI] [PubMed] [Google Scholar]

