Summary
In 2016, China introduced universal antiretroviral therapy (ART) for all HIV-infected individuals regardless of CD4 cell count. However, the natural history and rate of CD4 count decline among heterosexually-infected individuals remain uncharacterized. Analyzing national surveillance data can address this gap and shed light on the pathogenesis of HIV in this population. We used a linear mixed-effects model to assess CD4 trajectory over time before ART initiation and estimated the median time from HIV seroconversion to reaching CD4 thresholds of < 500, < 350, and < 200 cell/mm3. From the Chinese HIV/AIDS Comprehensive Response Information Management System, 59,085 eligible individuals were identified, with 113 having data to estimate the date of HIV seroconversion. The linear mixed-effects models estimated an intercept of 23.64 (95% confidence interval [CI]: 22.41 to 24.87) and a slope of -1.32 (95% CI: -1.34 to -1.30) for males, and an intercept of 22.70 (95% CI: 21.00 to 24.40) and a slope of -1.29 (95% CI: -1.31 to -1.27) for females. The estimated median times from HIV seroconversion to reaching CD4 count thresholds of < 500, < 350, < 200 cells/mm3 were 0.97, 3.74, and 7.20 years for males, and 0.26, 3.09, and 6.48 years for females, respectively. Males consistently took longer to reach these CD4 count thresholds compared to females of the same age group. Older individuals (≥ 40 years) reached CD4 thresholds faster than younger individuals (15-29 years), indicating more rapid disease progression in older people living with HIV.
Keywords: HIV/AIDS, disease progression, CD4+ T cell count, linear mixed-effects model
Introduction
HIV remains a major public health issue globally and in China. By the end of 2019, approximately 37.9 million people were living with HIV (PLHIV) worldwide (1). In China, an estimated 1.25 million people were living with HIV in 2018, with 73.1% infected through heterosexual contact (2,3). Effective clinical and public health management rely on accurate estimates of new HIV infections and their distribution by factors such as age, sex, and transmission mode. Understanding the natural history of HIV/AIDS and its disease progression is essential for this purpose (4).
The most renowned study on the natural history of HIV, conducted by Fauci and colleagues in 1996, showed that the rate of CD4 level decline decreases over time before antiretroviral therapy (ART) initiation based on clinical assessments and laboratory measurements of CD4 counts and virus loads (5). Similar studies (6-8) have been conducted in low and middle-income regions, as well as in Europe and the United States, involving cohorts of individuals with HIV not on ART (9-11). However, no such studies have been conducted in China (12).
In 2015, World Health Organization (WHO) recommended ART for all PLHIV regardless of CD4 level. China adopted this policy in the national treatment guideline in June 2016 (13). Understanding the natural history of HIV infection and disease progression in China has become challenging since the implementation of the "treat-all" policy.
CD4 cell count is a crucial biomarker for studying HIV disease progression and prognosis (14,15). The rate of CD4 decline since infection can be used in statistical models to estimate HIV incidence (5). Two back-calculation methods have been developed for estimating the rate of decline of CD4 count: a multi-state modelling method and a CD4 depletion modelling method. The multi-state model categorizes HIV infections by CD4 level (16,17), while the CD4 depletion model uses longitudinal data of individually repeated measurements of CD4 count before ART initiation in a linear mixed-effects model (4,7,18).
Advantages of the CD4 depletion modelling method include: i) handling correlation between CD4 measurements without assuming independence; ii) not requiring complete historic data on HIV diagnoses, which is useful when there are fewer CD4 counts available in the early years of a study (19); and (3) back-calculating seroconversion time for each individual, describing the distribution of new infections over a calendar year. These advantages enable the estimation of new HIV infections in China and the time from seroconversion to various CD4 cell count thresholds.
To our knowledge, and based on a systematic literature search in PubMed, Embase, Web of Science, and Chinese database, no published studies have addressed the natural history and disease progression indicated by the rate of decline in CD4 cell count among heterosexually infected HIV patients in China. Using data from the Chinese HIV/AIDS Comprehensive Response Information Management System (CRIMS), we conducted an analysis of heterosexually-infected patients and applied a linear mixed-effects model (adapted from the CD4 depletion modelling method) to estimate the rate of CD4 decline before ART initiation and the time from HIV seroconversion to CD4 cell count thresholds of < 200, < 350, < 500 cell/mm3.
Patients and Methods
Data source and study population
HIV has been a notifiable infectious disease in China since 1985. Established in 2005, CRIMS is an integrated internet-based system for real-time collection and reporting of newly diagnosed HIV/AIDS cases in China. Local physicians and health professionals report newly diagnosed HIV/AIDS cases to CRIMS using a uniform case reporting form (CRF) that includes personal information, such as date of birth, sex, residence, occupation, date of diagnosis, and testing results. All cases are validated by local clinicians and uploaded to China CDC for analysis and monitoring.
Eligible subjects included all HIV cases reported to CRIMS who met the following criteria: i) diagnosed with HIV between January 2006 and May 2019 (as the reporting quality in CRIMS improved starting in January 2006; ii) aged 15 years or older at the time of diagnosis; iii) self-reported infection through heterosexual contact; and iv) had at least two CD4 measurements before ART initiation. Exclusion criteria included incomplete records and non-citizens of China.
Statistical Methods
CD4 counts are periodically measured in PLHIV in China. We used these periodic assessments to construct an analytic dataset with CD4 counts over time for each subject. A linear mixed-effects model with random slope and/or random intercept was used to fit variations within and between individuals' CD4 measurements (20).
The study included three key variables: i) seroconversion date, estimated as the midpoint between last negative HIV test date and the first positive test date within a three-year interval; ii) t1, the interval between the HIV seroconversion date and each CD4 test date, used as the independent variable in the initial regression sqrt(CD4) = a + b•t1; and iii) t2, the intervals between the first CD4 test date and subsequent CD4 test dates, used as the independent variable in the second regression sqrt(CD4) = a'+ b'•t'2.
The model fit the square root of CD4 over time:  (5,19), where the variable t denotes time from date of infection to CD4 test date. We first estimated the intercept (ai), the average square root of CD4 count at the date of seroconversion, and the slope (bi), the rate of change in the square root of CD4 count over time. In the initial regression, sqrt(CD4) = a + b•t1, a was treated as a fixed intercept (assuming all individuals had the same CD4 count at time of seroconversion), and b as either fixed or random. Fixed b values were expected to be close to the mean of random b and fixed b'. The fixed b' values were estimated using data from all individuals in the second regression, sqrt(CD4) = a'+ b'•t'2. In this regression, b' was treated as a fixed slope (assuming all individuals had the same depletion rate), and a' as a random intercept (each person had a different value of CD4 count on the first CD4 test date). Assuming linearity in the CD4 depletion model during the study period, b and b' should be statistically equivalent. However, a and a' are different (with a > a').
(5,19), where the variable t denotes time from date of infection to CD4 test date. We first estimated the intercept (ai), the average square root of CD4 count at the date of seroconversion, and the slope (bi), the rate of change in the square root of CD4 count over time. In the initial regression, sqrt(CD4) = a + b•t1, a was treated as a fixed intercept (assuming all individuals had the same CD4 count at time of seroconversion), and b as either fixed or random. Fixed b values were expected to be close to the mean of random b and fixed b'. The fixed b' values were estimated using data from all individuals in the second regression, sqrt(CD4) = a'+ b'•t'2. In this regression, b' was treated as a fixed slope (assuming all individuals had the same depletion rate), and a' as a random intercept (each person had a different value of CD4 count on the first CD4 test date). Assuming linearity in the CD4 depletion model during the study period, b and b' should be statistically equivalent. However, a and a' are different (with a > a').
We used the model to estimate the time from seroconversion to reaching CD4 cell count thresholds of < 200, < 350, < 500 cell/mm3 to assess disease progression among men who have sex with women (MSW) and women who have sex with men (WSM).
Analyses were performed using SAS 9.4 (Statistical Analysis Software 9.4, SAS Institute Inc, Cary, North Carolina, USA). All tests were two-tailed with p values of 0.05 or less considered statistically significant.
Ethical review
The study was approved by the Ethics Committee of the National Centers for STD/AIDS Prevention and Control, China CDC (Ethical approval number: X190311565).
Results and Discussion
Our analytic dataset included 59,085 eligible cases. Of these, 113 cases had data to estimate the date of seroconversion, defined by a negative HIV test followed by a positive HIV test within three years. Table 1 summarizes the characteristics of the eligible cases used for fitting the initial and second regression models. The median of first CD4 counts was 489 cells/ mm3 (interquartile range [IQR]: 372-620 cell/mm3), with 48% of cases having an initial CD4 count ≥ 500 cells/mm3.
Table 1. Characteristics of 59 085 HIV/AIDS cases included in this study.
| Variable | n | (%) |
|---|---|---|
| Gender | ||
| Male | 34 337 | 58.11 |
| Female | 24 748 | 41.89 |
| Age group* | ||
| 15-29 | 19 984 | 33.83 |
| 30-39 | 16 499 | 27.93 |
| ≥ 40 | 22 594 | 38.25 |
| Education | ||
| Primary/illiterate | 19 245 | 32.57 |
| Junior high | 25 560 | 43.26 |
| Senior high and above | 14 280 | 24.17 |
| Ethnic group | ||
| Han | 43 506 | 73.63 |
| Others | 15 579 | 26.37 |
| First CD4 cell count (cells/mm3) | ||
| < 200 | 4 261 | 7.21 |
| 200-349 | 7 749 | 13.12 |
| 350-499 | 18 778 | 31.78 |
| ≥ 500 | 28 297 | 47.89 |
| Total | 59 085 | 100.00 |
Note: *There were 8 cases with missing information on age.
For CD4 cell count declines without ART, Table 2 presents the intercept and slope estimates from the linear mixed-effects CD4 depletion model by age and gender. For males, the rate of decline in the square root of CD4 count (slope) ranged from -1.21 (95% CI: -1.24 to -1.18) in the youngest group (15-29 years) to -1.48 (95% CI: -1.51 to -1.44) in the oldest group (≥ 40 years). For females, the rate of decline ranged from -1.22 (95% CI: -1.25 to -1.19) in the youngest group to -1.46 (95% CI: -1.50 to -1.41) in the oldest group. The intercepts, representing the square root of the model-estimated CD4 cell count at the time of seroconversion, varied slightly, with the lowest intercept observed in the 30-39 age group for both males and females. Intercepts for females were consistently lower than those for males. The intercept for males in the 15-29 and ≥ 40 age groups were 24.42 (95% CI: 22.64 to 26.20) and 24.04 (95% CI: 21.28 to 26.80), respectively. For females, the intercepts were 23.80 (95% CI: 21.49 to 26.12) and 22.62 (95% CI: 20.36 to 24.87), respectively. Overall, the average intercept and slope were 23.64 (22.41 to 24.87) and -1.32 (-1.34 to -1.30) for males, and 22.70 (21.00 to 24.40) and -1.29 (-1.31 to -1.27) for females.
Table 2. Intercept and slope estimates from liner mixed-effects CD4 depletion model, by age and gender.
| Gender | Age group | Cases for intercept estimates | Intercept | 95% CI | p value | Cases for slope estimates | Slope | 95% CI | p value |
|---|---|---|---|---|---|---|---|---|---|
| Male | 15-29y | 22 | 24.42 | 22.64 - 26.20 | < 0.001 | 9656 | -1.21 | -1.24 - -1.18 | < 0.001 |
| 30-39y | 28 | 23.17 | 21.25 - 25.08 | < 0.001 | 10005 | -1.27 | -1.30 - -1.24 | < 0.001 | |
| ≥ 40y | 26 | 24.04 | 21.28 - 26.80 | < 0.001 | 14675 | -1.48 | -1.51 - -1.44 | < 0.001 | |
| subtotal | 76 | 23.64 | 22.41 - 24.87 | < 0.001 | 34336 | -1.3 | -1.34 - -1.30 | < 0.001 | |
| Female | 15-29y | 10 | 23.80 | 21.49 - 26.12 | < 0.001 | 10328 | -1.22 | -1.25 - -1.19 | < 0.001 |
| 30-39y | 9 | 22.55 | 17.73 - 27.37 | < 0.001 | 6494 | -1.27 | -1.31 - -1.23 | < 0.001 | |
| ≥ 40y | 18 | 22.62 | 20.36 - 24.87 | < 0.001 | 7919 | -1.46 | -1.50 - -1.41 | < 0.001 | |
| subtotal | 37 | 22.70 | 21.00 - 24.40 | < 0.001 | 24741 | -1.29 | -1.31 - -1.27 | < 0.001 |
A monotonic decline in CD4 count over time since seroconversion was observed, with steeper declines in the earlier years post-infection for both males and females across all age groups (Figure 1). Among males, the CD4 count trajectories of the 30-39 and ≥ 40 age groups crossed after four years of infection, indicating greater CD4 depletion in later years among older males (≥ 40 years). The 15-29 year group consistently exhibited the highest CD4 cell count over time since seroconversion for both males and females.
Figure 1.
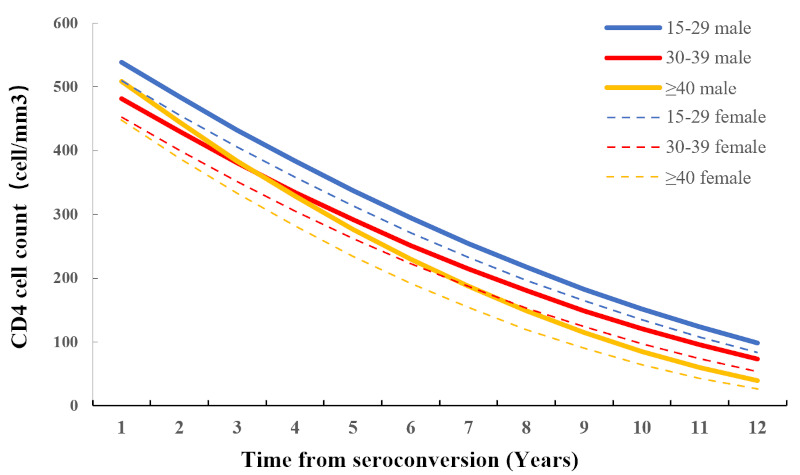
CD4 cell count decline over time since HIV seroconversion by age and gender based on the linear mixed-effects CD4 depletion model.
To our knowledge, this study represents the first national-level exploration of HIV disease progression among heterosexually infected individuals in China. We estimated the date of HIV seroconversion using national surveillance data and applied a mixed-effects CD4 depletion model to estimate the time from seroconversion to reaching three CD4 count thresholds.
Compared to Lodi et al. (9), our estimated times from seroconversion to reaching CD4 thresholds of < 500, < 350, and < 200 cells/mm3 were shorter by approximately 1, 4, and 8 years, respectively. Although the reasons for these differences are unclear, they may be attributable to variations in race/ethnicity, HIV subtype, baseline disease condition, and non-ART treatment (11,15).
The linear mixed-effects model in this study effectively handles random effects between multilevel variables and is widely used in longitudinal data analyses involving repeated CD4 measurements (19,21). Our model demonstrated a negative relationship between CD4 count and time since infection, with a greater rate of decline among older adults. These findings align with results from studies conducted in the United States (9), Brazil (10), and Europe (15).
Table 3 shows estimated time intervals from HIV seroconversion to reaching CD4 cell count thresholds of < 500, <350 and < 200 cells/mm3 by age (Year) and gender. Notably, females tend to reach these thresholds sooner than males, while the youngest age group (15-29 years) reached thresholds the slowest, highlighting faster disease progression in females and slowest progression in the youngest age group. Specifically, males took 6-10 months longer to reach the CD4 thresholds compared to females of the same age. Median times from HIV infection to reaching CD4 thresholds of < 500, < 350, and < 200 cells/mm³ were 0.97, 3.74, and 7.20 years for males, and0.26, 3.09, and 6.48 years for females. These findings contrast with a previous study showing longer times for women to reaching CD4 cell counts of < 500, < 350, and < 200 cells/mm³ than men, despite a similar pace of CD4 decline (11). CD4 stands as a pivotal biomarker for monitoring HIV disease progression, and researchers generally refer to median time after HIV seroconversion as an indicator of disease progression (22). Our results reveal shorter median times from seroconversion to the three CD4 cell count thresholds for women than for women. The disparity might potentially be attributed to varying initial CD4 levels between genders. Lodi and colleagues proposed that men experience a steeper CD4 decline than women after seroconversion. However, our analysis found little difference in CD4 decline rate by gender, which was not influenced by regional or ethnic stratification. A Singapore cohort study emphasized a significant impact of the infecting subtype, especially subtype CRF01_AE, on the rate of CD4 decline (14). Therefore, further exploration is needed to understand the relationship between HIV subtype and the rate of CD4 decline by gender.
Table 3. Median estimated time from seroconversion to CD4 cell count < 500, < 350, < 200 cell/mm3 by age.
| Variable | CD4 < 500 |
CD4 < 350 |
CD4 < 200 |
|||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| 15-29y | ||||||
| Median (95% CI) | 1.70 (0.23-3.25) | 1.18 (0.00-3.16) | 4.72 (3.17-6.35) | 4.17 (2.23-4.23) | 8.49 (6.85-10.22) | 7.92 (5.88-10.07) |
| 30-39y | ||||||
| Median (95% CI) | 0.64 (0.00-2.19) | 0.15 (0.00-4.07) | 3.51 (1.96-5.14) | 3.02 (0.00-7.04) | 7.11 (5.47-8.82) | 6.62 (2.74-10.75) |
| ≥ 40y | ||||||
| Median (95% CI) | 1.13 (0.00-3.08) | 0.18 (0.00-1.78) | 3.60 (1.70-5.62) | 2.68 (1.10-4.37) | 6.69 (4.73-8.79) | 5.81 (4.15-7.61) |
| Total | ||||||
| Median (95% CI) | 0.97 (0.04-1.93) | 0.26 (0.00-1.61) | 3.74 (2.76-4.74) | 3.09 (1.75-4.48) | 7.20 (6.17-8.25) | 6.48 (5.12-7.89) |
Our analysis revealed that the rate of CD4 decline was faster among older individuals and that females experienced faster disease progression than males. Among heterosexually infected individuals, females had faster disease progression, with an estimated time from seroconversion to reaching CD4 thresholds six to ten months sooner than males. The initial CD4 cell counts at HIV seroconversion were highest in the 15- 29 age group, with the rate of CD4 count decline increasing with age.
Since China implemented the "treat-all" policy in 2016, studying the natural history and disease progression of PLHIV has become more challenging. Using the national surveillance database and a linear mixed-effects model based on CD4 depletion modelling methods, we were able to explore HIV disease progression at the national level. The estimated rate of CD4 decline can inform back-calculation of the distribution of years since infection, aiding estimation of new infections in China.
Our study has several limitations. First, the estimation for seroconversion date as the midpoint between the last negative HIV test date and first positive HIV test date within a three-year interval may compromise accuracy and precision. Additionally, the small number of cases with a negative HIV test within three years prior to a positive test could impact the precision and generalizability of the intercept estimates. However, the slope estimates, based on all 59 085 eligible patients, mitigate these concerns. The lack of information on HIV subtype and other disease prognostic factors also limits our ability to address patient heterogeneity.
In conclusion, the rate of CD4 decline was faster among older ages and females in China, with progression to CD4 thresholds occurring faster in women and older age groups (≥ 40 years) than men and younger age group (15-29 years). Further studies should utilize the modeled CD4 decline rate to estimate new infections who acquired HIV through heterosexual contact, which can help decision-makers evaluate the effectiveness of HIV prevention and control measures in China.
Acknowledgements
We gratefully thank Dr. Lance Rodewald of National Immunization Program, Chinese Center for Disease Control and Prevention (China CDC) for his careful review of this manuscript.
Funding
This work was supported by the National Science and Technology Major Projects of China (2017ZX10201101-002-005).
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. UNAIDS. Access the UNAIDS data tables with the latest HIV numbers. http://www.unaids.org/en/resources/documents/2018/unaids-data-2018 (accessed April 3, 2024).
- 2. Lv F, Chen FF. National HIV/AIDS epidemic estimated and interpretation in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2019:40:1191-1196. (in Chinese) [DOI] [PubMed] [Google Scholar]
- 3. China National Health Commission. New progress in AIDS prevention and control in China in 2019. http://www.nhc.gov.cn/jkj/s3586/201911/c2388ce70bdd404ea6dfcd886591784d.shtml (accessed April 3, 2024). (in Chinese) .
- 4. Van der Paal L, Shafer LA, Todd J, Mayanja BN, Whitworth JA, Grosskurth H. HIV-1 disease progression and mortality before the introduction of highly active antiretroviral therapy in rural Uganda. AIDS. 2007; 21:S21-S29. [DOI] [PubMed] [Google Scholar]
- 5. Fauci AS, Pantaleo G, Stanley S, Weissman D. Immunopathogenic mechanisms of HIV infection. Annals of internal medicine. 1996; 124:654-663. [DOI] [PubMed] [Google Scholar]
- 6. Easterbrook PJ, Smith M, Mullen J, O'Shea S, Chrystie I, de Ruiter A, Tatt ID, Geretti AM, Zuckerman M. Impact of HIV-1 viral subtype on disease progression and response to antiretroviral therapy. J Int AIDS Soc. 2010; 13:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kiwanuka N, Robb M, Laeyendecker O, et al. HIV- 1 viral subtype differences in the rate of CD4+ T-cell decline among HIV seroincident antiretroviral naive persons in Rakai district, Uganda. J Acquir Immune Defic Syndr. 2010; 54:180-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pantazis N, Morrison C, Amornkul PN, Lewden C, Salata RA, Minga A, Chipato T, Jaffe H, Lakhi S, Karita E, Porter K, Meyer L, Touloumi G; CASCADE Collaboration in EuroCoord and ANRS 1220 Primo-CI Study Group. Differences in HIV natural history among African and non-African seroconverters in Europe and seroconverters in Sub-Saharan Africa. PLoS One. 2012; 7:e32369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lodi S, Phillips A, Touloumi G, Geskus R, Meyer L, Thiébaut R, Pantazis N, Amo JD, Johnson AM, Babiker A, Porter K; CASCADE Collaboration in EuroCoord. Time from human immunodeficiency virus seroconversion to reaching CD4+ cell count thresholds < 200, < 350, and < 500 Cells/mm3: assessment of need following changes in treatment guidelines. Clin Infect Dis. 2011; 53:817-825. [DOI] [PubMed] [Google Scholar]
- 10. Szwarcwald CL, Pascom ARP, Souza Júnior PRD. Estimation of HIV incidence and the number of people living with HIV/AIDS in Brazil, 2012. Journal of AIDS & Clinical Research. 2015; 6:3. [Google Scholar]
- 11. CASCADE Collaboration. Differences in CD4 cell counts at seroconversion and decline among 5739 HIV- 1-infected individuals with well-estimated dates of seroconversion. J Acquir Immune Defic Syndr. 2003; 34:76-83. [DOI] [PubMed] [Google Scholar]
- 12. Huang X, Lodi S, Fox Z, Li W, Phillips A, Porter K, Lutsar I, Kelleher A, Li N, Xu X, Wu H, Johnson AM; Beijing PRIMO cohort study; CASCADE Collaboration in EuroCoord. Rate of CD4 decline and HIV-RNA change following HIV seroconversion in men who have sex with men: a comparison between the Beijing PRIMO and CASCADE cohorts. J Acquir Immune Defic Syndr. 2013; 62:441-446. [DOI] [PubMed] [Google Scholar]
- 13. China National Health Commission. Notice on adjustment of free antiretroviral therapy guideline for HIV treatment. http://www.nhc.gov.cn/yzygj/s3593/201606/0b0fa78e10dc41328e842b1bf9cd433e.shtml (accessed April 3, 2024). (in Chinese) .
- 14. Ng OT, Lin L, Laeyendecker O, Quinn TC, Sun YJ, Lee CC, Leo YS. Increased rate of CD4+ T-cell decline and faster time to antiretroviral therapy in HIV-1 subtype CRF01_AE infected seroconverters in Singapore. Plos One. 2011; 6:e15738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Touloumi G, Pantazis N, Pillay D, Paraskevis D, Chaix ML, Bucher HC, Kücherer C, Zangerle R, Kran AM, Porter K; CASCADE collaboration in EuroCoord. Impact of HIV-1 subtype on CD4 count at HIV seroconversion, rate of decline, and viral load set point in European seroconverter cohorts. Clin Infect Dis. 2013; 56:888-897. [DOI] [PubMed] [Google Scholar]
- 16. Sommen C, Alioum A, Commenges D. A multistate approach for estimating the incidence of human immunodeficiency virus by using HIV and AIDS French surveillance data. Stat Med. 2009; 28:1554-1568. [DOI] [PubMed] [Google Scholar]
- 17. Sweeting MJ, De Angelis D, Aalen OO. Bayesian back-calculation using a multi-state model with application to HIV. Stat Med. 2005; 24:3991-4007. [DOI] [PubMed] [Google Scholar]
- 18. Li Y, Han Y, Xie J, Gu L, Li W, Wang H, Lv W, Song X, Li Y, Routy JP, Ishida T, Iwamoto A, Li T; CACT0810 group. CRF01_AE subtype is associated with X4 tropism and fast HIV progression in Chinese patients infected through sexual transmission. AIDS. 2014; 28:521-530. [DOI] [PubMed] [Google Scholar]
- 19. Song R, Hall HI, Green TA, Szwarcwald CL, Pantazis N. Using CD4 data to estimate HIV incidence, prevalence, and percent of undiagnosed infections in the United States. J Acquir Immune Defic Syndr. 2017; 74:3-9. [DOI] [PubMed] [Google Scholar]
- 20. Singer D, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence (New York, 2003; online edn, Oxford Academic, 1 Sept. 2009). https://doi.org/10.1093/acprof:oso/9780195152968.001.0001 (accessed July 8, 2024).
- 21. Tilling K, Lawton M, Robertson N, Tremlett H, Zhu F, Harding K, Oger J, Ben-Shlomo Y. Modelling disease progression in relapsing-remitting onset multiple sclerosis using multilevel models applied to longitudinal data from two natural history cohorts and one treated cohort. Health Technol Assess. 2016; 20:1-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lewden C, Chene G, Morlat P, Raffi F, Dupon M, Dellamonica P, Pellegrin JL, Katlama C, Dabis F, Leport C; Agence Nationale de Recherches sur le Sida et les Hepatites Virales (ANRS) CO8 APROCO-COPILOTE Study Group; Agence Nationale de Recherches sur le Sida et les Hepatites Virales (ANRS) CO3 AQUITAINE Study Group. HIV-infected adults with a CD4 cell count greater than 500 cells/mm3 on long-term combination antiretroviral therapy reach same mortality rates as the general population. J Acquir Immune Defic Syndr. 2007; 46:72-77. [DOI] [PubMed] [Google Scholar]


