Abstract
Background
Cirrhosis comprises a significant health challenge in the Middle East and North African (MENA) region impacting healthcare systems and communities. This study sought to investigate trends in the burden of cirrhosis and other chronic liver disease, different etiologies, deaths, and the disability burden utilizing data from the Global Burden of Disease (GBD) database.
Methods
Analyzing epidemiological trends from 1990 to 2021 across 21 MENA countries, this research utilized data on age-standardized incidence rates (ASIR), age-standardized death rates, and age-standardized disability-adjusted life years (DALYs) to evaluate the burden of cirrhosis and other chronic liver disease. The study also examined national variations and sociodemographic relationships.
Results
The study identified a 114.9% increase in cirrhosis and other chronic liver disease incidence within the MENA region between 1990 and 2021, with 7,344,030 incident cases reported in 2021. The ASIR showed a steeper rise in females (9.6%) compared to males (7.0%). Etiology-specific analysis revealed an increase in the ASIR for MASLD related cirrhosis and other chronic liver disease by 22.2%, while those due to alcohol as well as hepatitis B and C decreased by 28.1%, 59.3%, and 30%, respectively. Despite the rising incidence, overall age-standardized death rates across all etiologies decreased by 54.3%, with DALYs showing a 51.4% decrease during the same period. Country-specific trends varied significantly, with Oman recording the highest annual ASIR increase (0.64%), and Qatar observing the most substantial annual reduction in age-standardized death rates (-2.88%).
Conclusion
The study highlights evolving trends in cirrhosis and other chronic liver disease within the MENA region, emphasizing the necessity for comprehensive, etiology, and gender-specific interventions. Despite an increasing incidence, the observed improvements in mortality rates and age-standardized disability burden indicate progress in public health efforts to mitigate cirrhosis’s impact. These findings point to the complex nature of cirrhosis outcomes and the urgent need for tailored strategies to manage its increasing burden effectively.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20445-5.
Keywords: Cirrhosis, MENA region, Global burden of Disease, Epidemiological trends, Age-standardized incidence rates
Introduction
Cirrhosis presents a significant global health challenge, with its impact being particularly pronounced within the Middle East and North Africa (MENA) region, where it stands as the leading cause of liver-related mortality [1–3]. This condition, resulting from various etiologies including viral hepatitis, alcohol use disorder, malignancy, and metabolic factors, contributes to over two million deaths annually, accounting for around 4% of total global mortality [1–3]. Cirrhosis places a heavy burden on healthcare systems, contributing significantly to global morbidity, mortality, and Disability-Adjusted Life Years (DALYs) [4, 5]. Despite the global recognition of cirrhosis as a major public health issue, its specific consequences within the MENA region necessitate a dedicated investigation to fully understand and address its impact.
Liver injury triggers a healing process characterized by fibrosis, preserving the liver’s function and structural organization. However, with repeated injury, fibrosis becomes more extensive, disrupting the liver’s architecture and leading to functional loss and the development of cirrhosis. As cirrhosis develops, increased pressure in the portal vein (portal hypertension) and the liver’s impaired ability to synthesize proteins and clear toxins contribute to further complications [6]. In developed countries, alcohol use and metabolic dysfunction-associated steatotic liver disease (MASLD) have emerged as the leading causes of cirrhosis, while viral hepatitis, especially hepatitis B, continues to be the most common cause in developing regions and Asia [7]. Compensated cirrhosis, where the liver’s function remains relatively intact, has a prognosis similar to that of healthy individuals, with a decompensation rate of 10% in the first year of diagnosis [8]. Decompensated cirrhosis is associated with ascites, gastrointestinal bleeding due to portal hypertension, and hepatic encephalopathy. Spontaneous bacterial peritonitis may arise as a complication of ascites, while hepatocellular carcinoma can also occur as a serious complication of cirrhosis [9, 10].
From a public health perspective, emerging research in the literature has indicated a global increase in both the incidence and prevalence of cirrhosis [11]. Notably, there has been a worrying rise in cirrhosis rates attributed to metabolic dysfunction-associated steatohepatitis (MASH) [4]. The burden of cirrhosis displays regional variances, with Eastern Europe witnessing a marked increase in age-standardized death rates and DALYs due to cirrhosis, highlighting the significant health impact in that area [12]. In contrast, Egypt exhibits one of the highest age-standardized mortality rates for cirrhosis, accounting for one-fifth of all deaths among males aged 45 to 54 [1, 13]. Additionally, a gender disparity exists in the disease’s impact, with men experiencing higher DALYs (783.3 per 100,000) compared to women (344.0 per 100,000) in 2019 [1]. Despite these findings, data on morbidity and mortality trends in the MENA region, particularly in North Africa, remain limited [14]. A systematic review covering a small population of 10,000 cases from the region over two decades further emphasizes the data scarcity [15].
With this gap in the literature in mind, this study sets out to conduct a thorough analysis of the burden of cirrhosis and other chronic liver disease within the MENA region, leveraging the rich data available in the Global Burden of Disease (GBD) dataset [16]. By examining the dataset, which spans the years 1990 to 2021, we aim to explore the incidence, mortality, and DALYs associated with these conditions to provide insights into their epidemiological trends and changing dynamics. Understanding these trends and disparities is vital for developing targeted interventions and healthcare strategies to mitigate the public health impact. By focusing on a population that is often underrepresented, this study aspires to inform regional public health policies and guide interventions to reduce the burden of cirrhosis and other chronic liver diseases.
Methods
Data source
The GBD study is a comprehensive regional and global database evaluating mortality and disability from major diseases, injuries, and risk factors [17]. The study is conducted by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington in Seattle. The GBD 2021 study compiled data from a range of sources, including censuses, household surveys, disease registries, health service utilization data, and vital statistics records. This robust dataset includes multiple health measures, such as deaths, incidence, prevalence, years of life lost (YLLs), years lived with disability (YLDs), and DALYs, covering 371 diseases and injuries across 88 risk factors [18]. It offers insights for both sexes across 204 countries and territories, allowing comparisons from 1990 to 2021, thereby facilitating comprehensive analyses over time [19].
The GBD study categorized cirrhosis into compensated and decompensated types, using ICD-10 codes B18 and K70–77. Chronic viral hepatitis B and C were classified under B18.0–B18.2, while B18.8 and 18.9 were mapped to other chronic viral causes. Alcohol-related liver disease was associated with K70. MASLD, represented by K75.81 and K76.0, reflects non-alcoholic metabolic liver disease, including both its steatotic and steatohepatitic forms. The “cirrhosis due to other causes” category included autoimmune hepatitis (K75.4), toxic liver diseases, and other unspecified liver conditions under the K76 series. Acute hepatitis codes and those for diabetes were excluded. Deaths from hepatocellular carcinoma were also excluded due to their distinct cause definition and management implications compared to cirrhosis [20].
Measures
We report trends based on incidence, mortality, and DALYs for liver cirrhosis and other chronic liver disease from 1990 to 2021 from the Global Health Data Exchange (GHDx) query tool across all age groups [21]. The study identified five primary etiologies for liver cirrhosis: hepatitis B, hepatitis C, alcohol use, MASLD, and other chronic liver disease such as autoimmune hepatitis, toxic liver diseases, other inflammatory liver diseases, unspecified chronic hepatitis, and other diseases of the liver. Incident cases and deaths were identified based on ICD-10 codes. While the GBD study uses the term Non-Alcoholic Fatty Liver Disease (NAFLD), we follow the updated terminology from the June 2023 multi-society consensus, referring to these conditions as MASLD and MASH.
Incidence was defined as the number of new cases within a specified time frame, presented as total raw counts and age-standardized incidence rates per 100,000 individuals. Mortality rates were estimates derived from vital registration data and household surveys, reported as total raw counts and age-standardized death rates per 100,000 individuals. DALYs were defined as the combined measure of years lived with a disability and years of life lost, reported as total raw counts and age-standardized rates per 100,000 individuals.
Geographical location
We used the GBD dataset categorization of MENA countries, which included the following 21 countries: Afghanistan, Algeria, Bahrain, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Saudi Arabia, Sudan, Syria, Tunisia, Turkey, United Arab Emirates, Yemen.
Risk factors
The inclusion of risk factors in our analysis was guided by the GBD 2021 study. We incorporated all risk factors reported for liver cirrhosis, specifically highlighting alcohol and drug use. However, it is noteworthy that the GBD study provided detailed risk factors for conditions like hepatitis and alcohol-induced liver disease but did not include risk factor data for MASLD.
Statistical analysis
The GBD study utilizes methodologies like the Cause of Death Ensemble model (CODEm), spatiotemporal Gaussian process regression (ST-GPR), to process initial datasets. We accessed the refined data through the GBD platform to conduct further analysis.
Our investigation focused on reporting incident cases, DALYs, deaths, and age-standardized rates for incidence, DALYs, and deaths related to cirrhosis and other chronic liver disease, all with accompanying 95% uncertainty intervals (UIs). We calculated the annual proportion of incident cases and deaths by etiology, location, and year. The percentage changes in these metrics from 1990 to 2021 were computed as:
 |
Additionally, we calculated the Estimated Annual Percentage Changes (EAPCs) in the age-standardized incidence rate (ASIR), age-standardized DALY rate, and age-standardized death rate, including 95% confidence intervals (CIs), using a regression line fitted to the natural logarithm of the rates against calendar years; for example:
 |
where y = ln(ASR), and x = calendar year. The EAPC was calculated as:
 |
The Socio-demographic Index (SDI) is a composite measure of development status that was used and correlates with health outcomes. It is calculated as the geometric mean of indices of income, education, and fertility rate. The SDI values range from 0 (minimum) to 1 (maximum), and data for all countries in 2021 were sourced from the GHDx.
Trends were classified as upward or downward based on the EAPC and their 95% CI. Correlations between EAPC values in ASDR with SDI values in 2021 were evaluated using Pearson correlation analyses. All analyses as well as graphical illustrations were conducted using R programming version 4.3.3. A P-value of < 0.05 was considered statistically significant.
Results
Trends in the incidence cirrhosis and other chronic liver disease
The total incidence of cirrhosis and other chronic liver disease exhibited significant changes from 1990 to 2021, as shown in Table 1. For both genders combined, the total number of incident cases escalated from 3,417,410 (3,137,082 − 3,705,270) in 1990 to 7,344,030 (6,824,597–7,868,809) in 2021, marking a substantial increase of 114.9%. This rise was slightly more pronounced in females, with an increase of 116.7% (from 1,539,991 (1,419,640–1,665,926) to 3,336,640 (3,085,674–3,590,052)), compared to males, who saw an increase of 113.5% (from 1,877,419 (1,722,031 − 2,037,897) to 4,007,389 (3,720,851–4,275,157)).
Table 1.
Raw incident case counts and age-standardized incidence rates of liver cirrhosis and other chronic liver diseases, 1990 vs. 2021
| Cause | Gender | Raw number of Incident cases among all age groups | Age-standardized Incidence Rate per 100,000 individuals | ||||
|---|---|---|---|---|---|---|---|
| Value in 1990 (Lower – Upper) | Value in 2021 (Lower – Upper) | % Change | Value in 1990 (Lower – Upper) | Value in 2021 (Lower – Upper) | % Change | ||
| Cirrhosis and other chronic liver diseases | Male | 1,877,419 (1722031–2037897) | 4,007,389 (3720851–4275157) | 113.50% | 1138.5 (1063.43–1217.35) | 1218.3 (1139.64–1291.52) | 7.00% |
| Female | 1,539,991 (1419640–1665926) | 3,336,640 (3085674–3590052) | 116.70% | 1010.8 (938.65–1088.16) | 1108.1 (1030.99–1183.88) | 9.60% | |
| Both | 3,417,410 (3137082–3705270) | 7,344,030 (6824597–7868809) | 114.90% | 1076.1 (1002.1–1152.94) | 1165.3 (1088.8–1238.07) | 8.30% | |
| Chronic hepatitis B including cirrhosis | Male | 246,075 (207949–288586) | 165,957 (148730–181284) | -32.60% | 122.6 (106.77–139.46) | 51 (45.81–55.61) | -58.40% |
| Female | 174,911 (141947–212840) | 105,594 (92019–117148) | -39.60% | 89.7 (75.16–105.2) | 35.1 (30.66–38.84) | -60.90% | |
| Both | 420,985 (351271–501263) | 271,550 (241047–297226) | -35.50% | 106.5 (91.77–122.85) | 43.3 (38.45–47.39) | -59.30% | |
| Chronic hepatitis C including cirrhosis | Male | 168,901 (141607–201136) | 224,114 (178241–270935) | 32.70% | 107.5 (90.09–126.56) | 73.6 (59.3–88.88) | -31.50% |
| Female | 181,217 (149895–215283) | 236,972 (187892–289572) | 30.80% | 115.1 (95.36–136.55) | 82.3 (66.16–99.29) | -28.50% | |
| Both | 350,118 (290991–416297) | 461,086 (369907–559148) | 31.70% | 111.2 (92.89–130.79) | 77.8 (62.72–93.88) | -30.00% | |
| Cirrhosis due to alcohol | Male | 2000 (1326–2816) | 4059 (2674–5620) | 103.00% | 2.4 (1.61–3.41) | 1.8 (1.16–2.46) | -27.60% |
| Female | 613 (387–894) | 1179 (749–1701) | 92.30% | 0.8 (0.51–1.15) | 0.5 (0.35–0.78) | -31.50% | |
| Both | 2613 (1718–3690) | 5238 (3420–7361) | 100.50% | 1.6 (1.06–2.28) | 1.2 (0.76–1.63) | -28.10% | |
| Metabolic associated steatosis liver disease including cirrhosis | Male | 1,451,588 (1316998–1598681) | 3,600,723 (3328807–3859632) | 148.10% | 899.9 (828.82–974.42) | 1087.1 (1011.59–1159.16) | 20.80% |
| Female | 1,169,496 (1062394–1289000) | 2,975,364 (2735673–3221712) | 154.40% | 794.9 (725.15–863.78) | 982.9 (907.77–1055.7) | 23.60% | |
| Both | 2,621,084 (2381850–2884895) | 6,576,087 (6064679–7077142) | 150.90% | 848.6 (777.7–920.25) | 1037 (962.4–1109.01) | 22.20% | |
| Cirrhosis due to other causes | Male | 8856 (7435–10450) | 12,536 (10365–15214) | 41.60% | 6 (4.87–7.59) | 4.8 (3.92–6.04) | -20.20% |
| Female | 13,755 (11858–15787) | 17,532 (14436–20588) | 27.50% | 10.3 (8.29–12.75) | 7.3 (5.87–8.92) | -28.90% | |
| Both | 22,610 (19383–26188) | 30,069 (24934–36276) | 33.00% | 8.2 (6.64–10.31) | 6 (4.94–7.49) | -25.80% | |
Focusing on the age-standardized incidence rate (ASIR), there was an overall increase of 8.3%, going from 1076.1 (1002.1–1152.94) per 100,000 individuals in 1990 to 1165.3 (1088.8–1238.07) per 100,000 individuals in 2021, with an EAPC of 0.32% (95% CI: 0.29–0.35), as shown in supplementary Table 1. This increase was higher in females, with a 9.6% rise (from 1010.8 (938.65–1088.16) to 1108.1 (1030.99–1183.88) per 100,000 individuals), than in males, with a 7.0% rise (from 1138.5 (1063.43–1217.35) to 1218.3 (1139.64–1291.52) per 100,000 individuals).
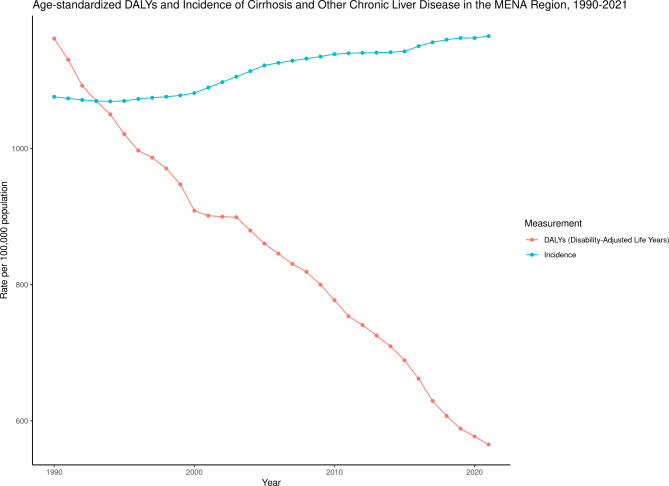
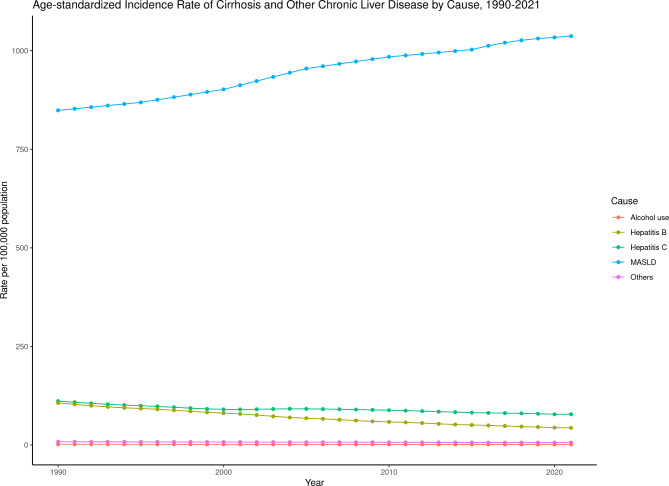
Figure 1 shows the trends in ASIR of different etiologies of cirrhosis and other chronic liver diseases. In the case of cirrhosis and other chronic liver disease due to alcohol use, the overall ASIR decreased by 28.1%. For cirrhosis and other chronic liver disease due to hepatitis B, the ASIR saw a significant overall decrease of 59.3%. The ASIR due to hepatitis C decreased by 30.0%. In contrast, ASIR due to MASLD witnessed an overall increase of 22.2%. Finally, for cirrhosis and other chronic liver disease due to other causes, the ASIR saw a decrease of 25.8%. Figure 2 shows the incidence rates of cirrhosis and other chronic liver diseases, highlighting distinct patterns when stratified by cause, gender, and age. In 2021, MASLD had the highest incidence across most age groups, peaking in young adults. Although its rates generally decline with age, fluctuations are observed in older groups. Chronic hepatitis B shows higher rates in middle-aged adults, while hepatitis C rises with age, peaking in older populations. Alcohol-related cirrhosis steadily increases with age, with minimal presence in younger individuals. Cirrhosis from other causes also shows an age-related increase, with higher rates in older females compared to males.
Fig. 1.
Age-standardized incidence and DALY rates attributable to cirrhosis and other chronic liver disease from 1990 to 2021
Fig. 2.
Age-standardized incidence of cirrhosis and other chronic liver disease by cause from 1990 to 2021
Trends in deaths of cirrhosis and other chronic liver disease
The total deaths attributed to cirrhosis and other chronic liver disease observed a notable increase from 1990 to 2021, rising from 76,869 (68,591 − 88,469) to 99,628 (86,818 − 116,009), an overall increase of 29.6% (Table 2). This trend was significantly more pronounced in males, who experienced a 44.2% increase (from 41,201 (35,683 − 47,814) to 59,394 (50,489 − 69,942)), compared to a 12.8% increase in females (from 35,668 (30,531 − 41,899) to 40,234 (34,329 − 46,838)).
Table 2.
Raw death counts and age-standardized death rates of liver cirrhosis and other chronic liver diseases, 1990 vs. 2021
| Cause | Gender | Raw number of Deaths among all age groups | Age-standardized Deaths Rate per 100,000 individuals | ||||
|---|---|---|---|---|---|---|---|
| Value in 1990 (Lower – Upper) | Value in 2021 (Lower – Upper) | % Change | Value in 1990 (Lower – Upper) | Value in 2021 (Lower – Upper) | % Change | ||
| Cirrhosis and other chronic liver diseases | Male | 41,201 (35683–47814) | 59,394 (50489–69942) | 44.20% | 51.65 (44.62–60.89) | 26.82 (22.96–31.45) | -48.10% |
| Female | 35,668 (30531–41899) | 40,234 (34329–46838) | 12.80% | 49.5 (41.14–59.35) | 19.48 (16.75–22.50) | -60.60% | |
| Both | 76,869 (68591–88469) | 99,628 (86818–116009) | 29.60% | 50.81 (44.25–59.40) | 23.23 (20.32–26.82) | -54.30% | |
| Chronic hepatitis B including cirrhosis | Male | 15,741 (12162–19441) | 21,068 (16137–27412) | 33.80% | 20.22 (15.66–25.33) | 9.54 (7.34–12.44) | -52.80% |
| Female | 11,002 (7965–14741) | 11,275 (8169–14963) | 2.50% | 15.69 (11.19–21.67) | 5.44 (3.96–7.21) | -65.30% | |
| Both | 26,744 (20582–33766) | 32,342 (24451–41807) | 20.90% | 18.01 (13.86–23.31) | 7.51 (5.70–9.91) | -58.30% | |
| Chronic hepatitis C including cirrhosis | Male | 17,779 (14265–22403) | 26,409 (20644–32945) | 48.50% | 23.06 (18.03–29.08) | 11.83 (9.26–14.62) | -48.70% |
| Female | 14,739 (11490–18850) | 16,187 (12645–20009) | 9.80% | 21.33 (16.15–27.59) | 7.78 (6.12–9.55) | -63.50% | |
| Both | 32,519 (25990–40756) | 42,596 (33773–52747) | 31.00% | 22.29 (17.69–28.09) | 9.84 (7.77–12.07) | -55.80% | |
| Cirrhosis due to alcohol | Male | 1851 (1189–2821) | 2973 (1954–4283) | 60.70% | 2.32 (1.51–3.51) | 1.33 (0.86–1.89) | -42.70% |
| Female | 647 (398–1020) | 811 (510–1171) | 25.30% | 0.9 (0.57–1.41) | 0.39 (0.24–0.57) | -56.70% | |
| Both | 2498 (1605–3826) | 3784 (2484–5416) | 51.50% | 1.61 (1.04–2.42) | 0.87 (0.56–1.24) | -46.00% | |
| Metabolic associated steatosis liver disease including cirrhosis | Male | 1180 (774–1773) | 3710 (2470–5424) | 214.40% | 1.64 (1.03–2.46) | 1.79 (1.19–2.61) | 9.10% |
| Female | 1802 (1138–2848) | 4327 (2842–6306) | 140.20% | 2.74 (1.69–4.41) | 2.22 (1.44–3.25) | -19.00% | |
| Both | 2982 (1916–4571) | 8037 (5430–11688) | 169.50% | 2.21 (1.39–3.50) | 2.01 (1.35–2.93) | -9.00% | |
| Cirrhosis due to other causes | Male | 4649 (3595–5898) | 5234 (3958–7119) | 12.60% | 4.41 (3.21–6.29) | 2.33 (1.71–3.24) | -47.10% |
| Female | 7477 (5676–9837) | 7634 (5783–10192) | 2.10% | 8.84 (6.09–12.68) | 3.66 (2.75–4.95) | -58.60% | |
| Both | 12,126 (9557–15361) | 12,869 (9935–17033) | 6.10% | 6.69 (4.83–9.46) | 3.00 (2.31–4.13) | -55.20% | |
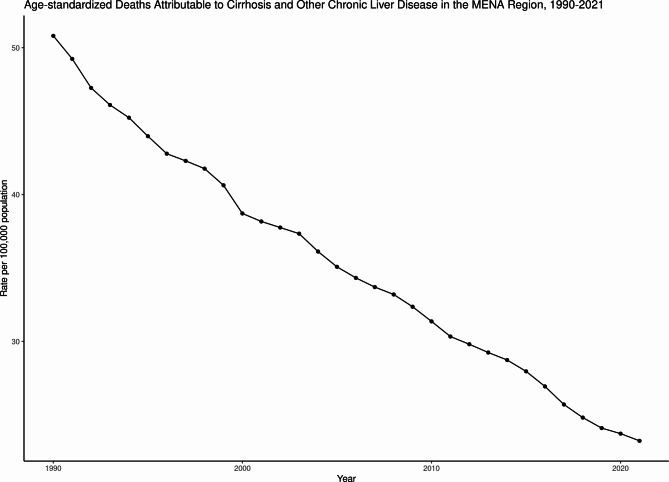
Regarding the age-standardized death rate, there was a notable decrease over this period, with an annual decrease of 2.40% (95% CI: 2.34–2.46). The overall age-standardized death rate for cirrhosis and other chronic liver disease fell by 54.3%, from 50.81 (44.25–59.40) to 23.23 (20.32–26.82) per 100,000 people, as shown in Fig. 3. This pattern of decrease was consistent across both genders, with a more significant decrease in females (60.6% reduction from 49.5 (41.14–59.35) to 19.48 (16.75–22.50)) compared to males (48.1% reduction from 51.65 (44.62–60.89) to 26.82 (22.96–31.45)), as shown in Table 2.
Fig. 3.
Incidence Rate of cirrhosis and other chronic liver disease by cause in 2021 across different age groups, males vs. females
Specifically, cirrhosis and other chronic liver disease due to alcohol use saw a 46.0% decrease in the age-standardized death rate (from 1.61 (1.04–2.42) to 0.87 (0.56–1.24)), with similar trends observed for hepatitis B (58.3% decrease from 18.01 (13.86–23.31) to 7.51 (5.70–9.91)), hepatitis C (55.8% decrease from 22.29 (17.69–28.09) to 9.84 (7.77–12.07)), MASLD (9.0% decrease from 2.21 (1.39–3.50) to 2.01 (1.35–2.93)), and other causes (55.2% decrease from 6.69 (4.83–9.46) to 3.00 (2.31–4.13)). Each of these categories showed a more significant rate of decrease in females, aligning with the overall trend.
Trends in DALYs of cirrhosis and other chronic liver disease
There was a notable change in the total DALYs for cirrhosis and other chronic liver disease across various categories from 1990 to 2021, as shown in Table 3. For instance, the total DALYs in both genders changed from 2,259,566 (2,028,320–2,517,966) in 1990 to 2,793,003 (2,407,973–3,266,285) in 2021, marking a 23.6% increase. The increase was more pronounced in males, who experienced a 33.8% surge (from 1,279,776 (1,098,333–1,452,111) to 1,712,187 (1,465,227–2,019,863)), compared to females, with a 10.3% rise (from 979,791 (852,658–1,117,548) to 1,080,815 (913,536–1,269,358)).
Table 3.
Raw DALY counts and age-standardized DALY rates of liver cirrhosis and other chronic liver diseases, 1990 vs. 2021
| Cause | Gender | Raw number of DALYs among all age groups | Age-standardized DALYs Rate per 100,000 individuals | ||||
|---|---|---|---|---|---|---|---|
| Value in 1990 (Lower – Upper) | Value in 2021 (Lower – Upper) | % Change | Value in 1990 (Lower – Upper) | Value in 2021 (Lower – Upper) | % Change | ||
| Cirrhosis and other chronic liver diseases | Male | 1,279,776 (1098333–1452111) | 1,712,187 (1465227–2019863) | 33.80% | 1262.6 (1092.55–1459.53) | 667.8 (571.11–786.24) | -47.10% |
| Female | 979,791 (852658–1117548) | 1,080,815 (913536–1269358) | 10.30% | 1050.4 (904.47–1220.91) | 456.0 (389.52–533.35) | -56.60% | |
| Both | 2,259,566 (2028320–2517966) | 2,793,003 (2407973–3266285) | 23.60% | 1161.8 (1040.45–1326.38) | 565.1 (490.32–658.07) | -51.40% | |
| Chronic hepatitis B including cirrhosis | Male | 451,493 (347678–553341) | 586,652 (443339–759763) | 29.90% | 480.2 (374.61–592.96) | 231.6 (177.10–296.23) | -51.80% |
| Female | 268,394 (202121–345046) | 288,052 (212326–378127) | 7.30% | 321.9 (237.75–425.64) | 123.3 (90.90–162.15) | -61.70% | |
| Both | 719,887 (572352–893447) | 874,703 (657842–1138729) | 21.50% | 403.1 (317.14–501.22) | 178.7 (135.89–230.42) | -55.70% | |
| Chronic hepatitis C including cirrhosis | Male | 506,453 (406512–629847) | 747,589 (587724–942251) | 47.60% | 542.7 (438.61–676.81) | 291.7 (230.38–364.40) | -46.30% |
| Female | 352,472 (281059–441362) | 416,444 (311810–515753) | 18.10% | 427.6 (336.03–542.61) | 177.6 (136.93–219.34) | -58.50% | |
| Both | 858,925 (699454–1068493) | 1,164,034 (911163–1445364) | 35.50% | 487.5 (394.05–606.41) | 236.2 (186.20–293.56) | -51.50% | |
| Cirrhosis due to alcohol | Male | 51,506 (33231–76916) | 82,229 (53498–117920) | 59.60% | 56.2 (36.36–84.28) | 32.5 (21.40–46.60) | -42.20% |
| Female | 15,617 (9371–24454) | 20,258 (12544–29232) | 29.70% | 19.0 (11.63–29.49) | 8.8 (5.53–12.60) | -53.80% | |
| Both | 67,123 (43802–99779) | 102,487 (67122–146556) | 52.70% | 37.9 (24.61–58.15) | 20.9 (13.73–29.57) | -44.90% | |
| Metabolic associated steatosis liver disease including cirrhosis | Male | 30,974 (20567–45886) | 96,110 (64831–140684) | 210.30% | 35.3 (23.33–52.82) | 39.7 (26.57–57.81) | 12.20% |
| Female | 39,822 (26542–58792) | 100,308 (67460–144720) | 151.90% | 51.0 (33.13–78.20) | 45.2 (30.23–65.12) | -11.40% | |
| Both | 70,795 (47287–102440) | 196,418 (132816–288480) | 177.40% | 43.4 (28.35–65.28) | 42.5 (28.54–61.59) | -1.90% | |
| Cirrhosis due to other causes | Male | 239,349 (187896–291427) | 199,607 (156820–253217) | -16.60% | 148.1 (115.63–187.38) | 72.4 (56.20–92.78) | -51.10% |
| Female | 303,486 (246613–365256) | 255,753 (204311–320180) | -15.70% | 230.9 (179.01–292.25) | 101.2 (79.96–129.07) | -56.20% | |
| Both | 542,836 (454086–638264) | 455,360 (363443–564791) | -16.10% | 189.8 (152.47–235.26) | 86.7 (68.87–108.69) | -54.30% | |
The age-standardized DALY rate per 100,000 individuals saw significant decreases in both genders. In males, this rate decreased from 1,262.6 (1,092.55–1,459.53) to 667.8 (571.11–786.24), a reduction of 47.1%. In females, the decrease was from 1,050.4 (904.47–1,220.91) to 456.0 (389.52–533.35), translating to a 56.6% reduction. Overall, there was a 51.4% decrease from 1,161.8 (1,040.45–1,326.38) to 565.1 (490.32–658.07), with an annual decrease of 1.56% (95% CI: 1.51–1.62), as shown in Fig. 4.
Fig. 4.
Age-standardized deaths contributable to cirrhosis and other chronic liver disease from 1990 to 2021
Looking specifically at cirrhosis and other chronic liver disease due to alcohol use, the age-standardized DALY rate in males decreased by 42.2% (from 56.2 (36.36–84.28) to 32.5 (21.40–46.60)), and in females, it dropped by 53.8% (from 19.0 (11.63–29.49) to 8.8 (5.53–12.60)). For hepatitis B-related liver disease, there was a 51.8% decrease in males (from 480.2 (374.61–592.96) to 231.6 (177.10–296.23)) and 61.7% decrease in females (from 321.9 (237.75–425.64) to 123.3 (90.90–162.15)). Hepatitis C-related cirrhosis and other chronic liver disease saw a 46.3% decrease in males (from 542.7 (438.61–676.81) to 291.7 (230.38–364.40)) and a 58.5% decrease in females (from 427.6 (336.03–542.61) to 177.6 (136.93–219.34)).
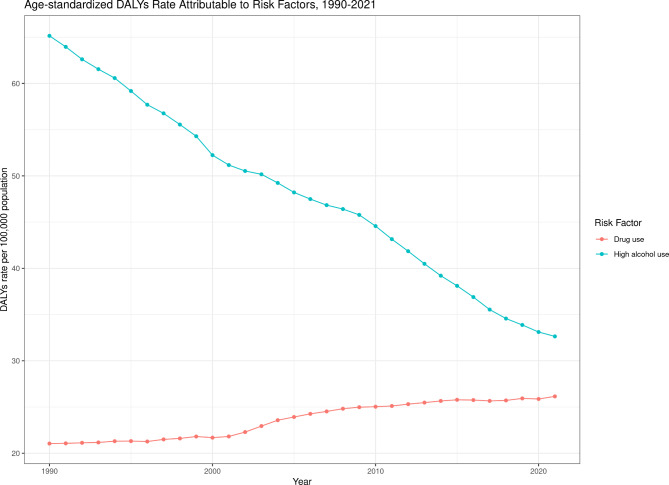
For MASLD, there was an increase of 12.2% in males (from 35.3 (23.33–52.82) to 39.7 (26.57–57.81)), while in females, the rate decreased by 11.4% (from 51.0 (33.13–78.20) to 45.2 (30.23–65.12)). Cirrhosis due to other causes saw a 51.1% decrease in males (from 148.1 (115.63–187.38) to 72.4 (56.20–92.78)) and a 56.2% decrease in females (from 230.9 (179.01–292.25) to 101.2 (79.96–129.07)). The age standardized DALYs rate attributable to cirrhosis and other chronic liver disease due to alcohol use as a risk factor had a marked decrease from 1990 to 2021, indicating a significant reduction in the health burden from alcohol over the past three decades as shown in Fig. 5. Conversely, the DALYs rate associated with drug use as a risk factor had a gradual increase during the same period, notably after the early 2000s.
Fig. 5.
Age-standardized DALY rates attributable to risk factors from 1990–2021
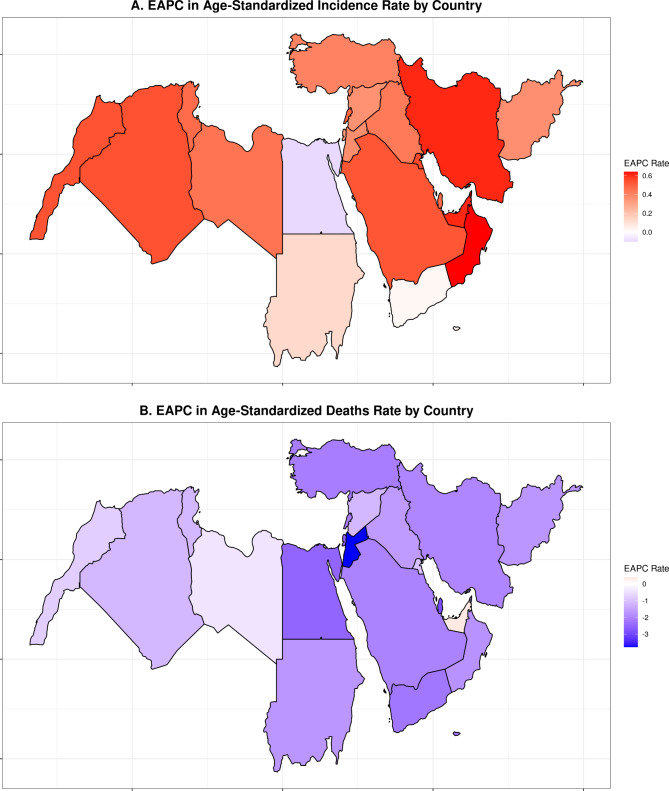
EASR in ASIR and age-standardized DALYs rate by country
For the age-standardized incidence rate, Oman demonstrated the greatest increase at 0.64% (95% CI: 0.62–0.66). Conversely, Egypt was the only country to show a small annual decrease in incidence rates at -0.10% (95% CI: -0.15 – -0.05), as shown in Fig. 6A.
Fig. 6.
Estimated annual percentage change in age-standardized incidence rate (A) and age-standardized DALY rate (B) by country from 1990 to 2021
Regarding the annual change in the age-standardized death rate, the annual change indicated a general decline in mortality rates across the region. Bahrain experienced the most significant annual reduction in the age-standardized death rate at -2.84% (95% CI: -3.32 – -2.35). In contrast, United Arab Emirates stood out as the only country to exhibit an annual increase, albeit slight, at 0.41% (95% CI: -0.16–0.99), as shown in Fig. 6B.
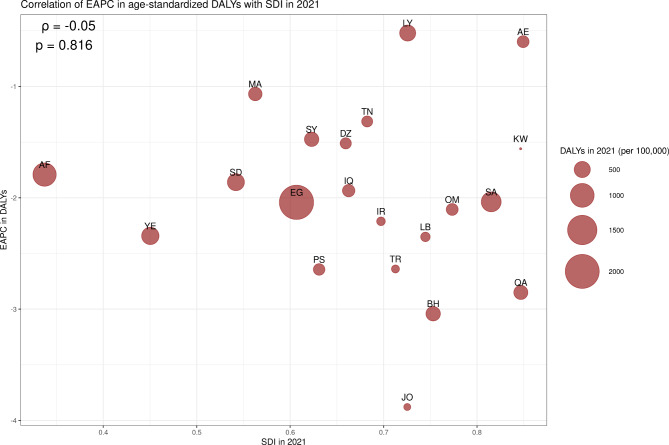
Analysis of the annual change in the age-standardized DALY rate, in relation to the SDI in 2021, revealed no significant correlation (p-value = 0.816). The most substantial annual decrease in the age-standardized DALY rate was observed in Jordan at -3.88% (95% CI: -4.30 – -3.45), while Libya had the smallest decrease at -0.52% (95% CI: -0.90 – -0.14), as shown in Fig. 7.
Fig. 7.
Correlation of estimated annual percentage change in age-standardized incidence rate with the countries’ sociodemographic index in 2021
Discussion
In this study, we assessed the burden of cirrhosis and other chronic liver disease within the MENA region from 1990 to 2021 by analyzing data from the GBD dataset. Our analysis reveals a pressing need for national healthcare policymakers to confront the escalating incidence rates by developing and implementing targeted interventions. To the best of our knowledge, this is the first study to utilize the 2021 iteration of the GBD dataset to quantify the burden of cirrhosis and other chronic liver disease in the MENA region. Overall, our findings indicate a marked increase in incidence, escalating from 3,417,410 cases in 1990 to 7,344,030 in 2021, which translates to a 114.9% increase alongside a 8.3% rise in the ASIR from 1076.1 to 1165.3 per 100,000 individuals. This increase was primarily driven by the sharp rise in MASLD, which saw a 150.9% increase in incident cases and a 22.2% rise in ASIR. In contrast, other causes, including chronic hepatitis B and C, as well as alcohol-related cirrhosis, showed declining trends in ASIR. These trends of incidence were observed in both males and females across most etiologies. Interestingly, despite the growing incidence of cirrhosis and other chronic liver disease, there was a discernible decrease in overall disease burden, as evidenced by a reduction in the age-standardized death rates from 50.8 to 23.2 per 100,000 individuals and the age-standardized DALYs rate from 1161.8 to 565.1 per 100,000 individuals. Qatar showcased the most notable annual decline in age-standardized death rates at -2.88%, while Oman exhibited the highest annual increase in ASIR at 0.64%. This paradoxical trend of increasing incidence yet declining mortality and morbidity rates mirrors global patterns, emphasizing the public health challenges and opportunities for advancement within the MENA region.
In observing trends of increasing total raw death counts alongside declining age-standardized death and DALY rates, our findings echo the dual narrative of global health progress against cirrhosis mortality and the persistent challenge it represents, especially in the MENA region. More specifically, this mirrors the pattern described by Mokdad et al. in their analysis of GBD 2010 data across 187 countries from 1980 to 2010, noting an increase in mortality despite a decrease in age-standardized death rates similar to our study’s findings [13]. The rise in the total number of deaths attributed to cirrhosis in our study period likely results from demographic shifts, including population growth and aging [20]. Another comprehensive study spanning 195 countries from 1990 to 2017 found a global decrease in cirrhosis age-standardized death and DALY rates, aligning with our observations [20]. It also noted lower death and DALY rates in regions with higher SDI, such as Pacific Asia and North America, underscoring a global escalation in the cirrhosis burden due to increased deaths, DALYs, and age-standardized prevalence of cirrhosis. Despite a notable decrease in age-standardized death rates in the MENA region, mortality rates remain significantly higher than the global, with Egypt presenting the highest age-standardized death rate despite a 22.4% reduction from 1990 to 2017 [20]. These findings underscore the intricate relationship between demographic factors, healthcare interventions, and the cirrhosis burden.
Furthermore, the rising incidence of non-HCV related liver disease, particularly MASLD, highlights a critical and growing challenge within the MENA region’s healthcare infrastructure. Despite the initiation of public health programs aimed at various cirrhosis causes, MASLD emerges as a significant, yet largely unaddressed, contributor to the regional disease burden, with ASIR rates marking the largest increase in our analysis [22]. This observation is consistent with findings by Wang et al., [19] who reported a global uptick in MASLD ASIR, specifying an EAPC of 0.1. Their study notably highlights the MENA region—and Egypt in particular—as a hotspot for MASLD incidence and mortality, identifying the highest mortality rates in middle-SDI countries and the lowest in high-SDI settings, with a negative correlation observed between SDI and death rates (r = − 0.403, p < 0.001).19 This emerging trend of MASLD not only accentuates the pressing need for targeted healthcare strategies but also calls for a deeper investigation into how cirrhosis morbidity intersects with socioeconomic determinants. Such an analysis is crucial for comprehensively addressing the intricate demands of healthcare enhancement in the MENA region.
Our investigation into the correlation between cirrhosis and other chronic liver disease morbidity and socioeconomic factors within the MENA region has yielded unexpected results, diverging from established literature that show a strong link between socioeconomic status and liver disease burden. Historically, studies have demonstrated that low socioeconomic status is associated with an increased risk of various liver diseases, including cirrhosis, primary liver cancer, and nonalcoholic liver disease [23–26]. Such populations are often more susceptible to reaching advanced stages of liver disease and bear a disproportionate burden of liver cancer [27]. This correlation is well-documented across different global contexts, from Europe to Asia [23, 25, 28], suggesting a universal trend where socioeconomically disadvantaged groups face heightened risks and poorer health outcomes related to liver disease. The absence of a significant correlation in our findings may indicate unique regional dynamics within the MENA context or perhaps reflect variances in data collection, socioeconomic measures, or the multifaceted nature of healthcare access and quality across these countries. It raises critical questions about the interplay between socioeconomic factors and health outcomes in the region, suggesting that other determinants, such as healthcare policies, public health initiatives, or even genetic predispositions, may play a more significant role in influencing cirrhosis morbidity in the MENA region than previously thought. Furthermore, this relationship can be discussed in the special context of the MENA region, an area that has been subject to political turmoil, armed conflict, and migration [29, 30]. Overall, this discrepancy shows the need for a deeper investigation into how socioeconomic disparities contribute to the incidence and progression of liver diseases in MENA, including factors such as alcohol consumption patterns, which have been identified elsewhere as being influenced by socioeconomic status. This nuanced understanding is essential for developing targeted interventions that address not only the clinical aspects of liver disease but also the socioeconomic dimensions that exacerbate health disparities.
Public health implications
Effective prevention and early detection are pivotal in the management of chronic liver diseases (CLD), necessitating robust screening protocols. In the United States, evolving hepatitis C screening recommendations now advocate for universal, one-time screening of all individuals over 18 years old and all pregnant persons, contingent on a prevalence greater than 0.1%. This approach is underpinned by the cost-effectiveness of screening and the advent of direct-acting antiviral (DAA) agents for hepatitis C treatment [31]. Similarly, screening for MASLD in primary care settings targets individuals with metabolic risk factors and/or type II diabetes mellitus, reflecting a proactive stance towards early identification and management [32]. However, the MENA region exhibits a notable scarcity in screening recommendations and implementation for at-risk populations, highlighting a critical gap in CLD prevention strategies. Bridging this gap requires leveraging the successes and lessons learned from the US and other regions to tailor and implement effective screening protocols within MENA, accommodating the unique healthcare infrastructure and population health needs of the region.
While liver biopsy remains the definitive standard for cirrhosis diagnosis, its invasive nature limits its utility, particularly for ongoing disease monitoring. The emergence of non-invasive testing (NITs) has revolutionized the diagnosis and management of CLD both in the United States and globally [33]. In Lebanon, a retrospective study of 620 patients using FibroScan identified MASLD as the leading cause of liver disease [34]. While non-invasive testing (NIT) methods, such as the Fibrosis-4 (FIB-4) index and aspartate aminotransferase to platelet ratio index (APRI), are generally accessible, affordable, and straightforward to perform, access to more advanced diagnostics like transient elastography and specialized fibrosis seromarkers may remain limited. Although healthcare systems in affluent countries such as the UAE and Saudi Arabia typically provide broad insurance coverage, variability in healthcare delivery and infrastructure can still affect the consistent availability of these diagnostics, showing the need for improved access strategies [35]. These challenges underscore the urgent need to enhance diagnostic procedures for MASLD and MASH within the region. This imperative to improve diagnostics dovetails with the region’s pressing demand for liver transplantation (LT), further illustrating the interconnected challenges of managing CLD in the MENA and the critical role of advancing diagnostic and treatment capacities to address these needs comprehensively [36].
Moreover, the demand for LT in the MENA region is acute, with the need estimated at over 50 per million population, significantly exceeding the capacity of LT centers [37]. Since the introduction of deceased donor (DDs) transplantation in 1986 [38], the landscape of LT in the MENA has evolved. However, with the exception of Iran, living donors (LDs) predominate, even where DD donation is legally permitted. This reliance on LDs, compounded by a scarcity of DDs, financial burdens borne out-of-pocket, and insufficient social support, exacerbates the challenges of meeting the LT demand in the region [39].
Addressing these challenges involves strengthening screening programs, expanding access to NITs, and enhancing LT infrastructure. Integrating hepatitis and metabolic risk screening into primary care could support earlier detection, particularly if accompanied by targeted public awareness initiatives. Financial barriers to diagnostics might be reduced through subsidies or partnerships with private insurers, improving accessibility. Regional collaboration on transplant networks may also offer a way to alleviate donor shortages by pooling expertise and resources. While the successes of DD LT programs in Iran provide useful frameworks, solutions will need to be adapted to the specific healthcare systems and challenges within each country. Thoughtfully pursuing these strategies holds promise for mitigating the burden of cirrhosis and other chronic liver disease and improving long-term outcomes across the region.
Strengths and limitations
This study represents a significant advancement in understanding the burden of cirrhosis and other chronic liver disease in the MENA region, primarily by being the first to apply the 2021 iteration GBD dataset for a comprehensive analysis spanning nearly three decades. Its strengths lie in offering a detailed exploration of cirrhosis and other chronic liver disease incidence, death, and DALY trends, differentiated by etiology, thereby shedding light on the primary drivers of the disease within a very understudied region in public health research. Additionally, by comparing the MENA data with global trends, the study places the regional findings in a broader context, emphasizing unique challenges and the critical need for targeted healthcare interventions. The inclusion of both mortality and morbidity trends offers a holistic view of the disease’s impact, crucial for assessing healthcare outcomes and the effectiveness of existing strategies.
However, the study’s reliance on secondary GBD data introduces potential limitations related to the accuracy and completeness of the dataset, which could influence the findings. The regional focus, while valuable, might obscure country-specific nuances and variations in the burden across the MENA region due to diverse healthcare infrastructures and policies. Additionally, the study’s observation of an unexpected lack of significant correlation between cirrhosis and other chronic liver disease morbidity and socioeconomic factors suggests possible data gaps or complexities in the interplay between disease incidence and socioeconomic determinants. These limitations highlight the need for cautious interpretation of the findings and suggest areas for further research, particularly in refining disease management strategies and enhancing healthcare policy effectiveness within the MENA region.
Our study utilizes the standard definitions established by the GBD to align with global research efforts and facilitate cross-study comparisons. However, a key limitation lies in the broad categorization of “cirrhosis and other chronic liver diseases,” which includes various liver conditions that may not have progressed to cirrhosis, potentially overestimating the burden. Furthermore, autoimmune, cryptogenic, and parasitic causes of liver disease, such as schistosomiasis, are grouped under generalized categories like “other causes.” This aggregation limits the ability to isolate the contributions of these specific etiologies, particularly in regions where parasitic infections are endemic, such as Egypt. These limitations highlight challenges in capturing the true burden and epidemiological patterns of liver disease across different geographic and clinical contexts.
Future research
The findings from this study highlight the pressing need for extensive research to uncover the root causes of cirrhosis and other chronic liver disease across the MENA region, evaluate the impact of existing healthcare measures, and investigate pioneering treatments. The increasing incidence of cirrhosis and other chronic liver disease fueled notably by MASLD, alongside the substantial pressure it places on healthcare infrastructures, mandates a concentrated research effort on modifiable risk factors and disease progression mechanisms. Such insights would facilitate the crafting of precise prevention methodologies capable of either mitigating or reversing the escalating trend of chronic liver disease.
Furthermore, the demand for longitudinal research is paramount to generate robust data concerning the long-term prognosis for cirrhosis patients within the MENA area. These studies are vital for the assessment of intervention efficacy in real-world settings, including the impact of vaccination drives, initiatives aimed at curtailing alcohol use, and the application of direct-acting antiviral agents for hepatitis C treatment. Analysis focusing on the cost-effectiveness of these strategies will provide invaluable guidance for health policymakers in optimizing resource distribution.
In addition, developing novel treatment strategies that align with the unique demographic, genetic, and environmental characteristics of the MENA population is essential. This includes exploring the role of precision medicine in cirrhosis management and assessing the effectiveness of emerging therapeutic compounds. A promising research avenue involves enhancing non-invasive diagnostic techniques, which are pivotal for early detection and effective management of cirrhosis. By refining these methods, the dependence on liver biopsies could be reduced, leading to improved patient care and outcomes.
Finally, while we calculated incidence and other metrics by country, we did not explore the specific reasons behind the observed trends at the national level. Drawing meaningful conclusions about the drivers of these variations is beyond the scope of this regional-level analysis. We believe that country-specific data would provide more nuanced insights and enable a better understanding of these patterns. Future research focused on individual countries is needed to identify the underlying factors contributing to these trends and inform tailored public health strategies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the GBD collaborators for the data used in this study.
Author contributions
(A=Study Design, B=Data collection, C=Statistical analysis, D=Data interpretation, E=Manuscript preparation, F=Literature search, G=Manuscript review)Omar Al Ta’ani: ABCDEFGWesam Aleyadeh: ADEFGYazan Al-Ajlouni: ADEFGLynna Alnimer: DEFGAbdellatif Ismail: DEFGBashar Natour: EFGBasile Njei: ADEFG.
Funding
No funding was obtained for this manuscript.
Data availability
The data supporting this study’s findings come from the GBD study, available on the Institute for Health Metrics and Evaluation website. The GBD offers comprehensive health data worldwide, including mortality, morbidity, and risk factor estimates for various diseases and conditions.The dataset can be accessed by visiting the IHME GBD Data Tool at https://vizhub.healthdata.org/gbd-compare/#. This interactive tool allows for the exploration of health trends at global, regional, and country levels. The dataset is openly accessible under IHME’s terms, supporting its use for research and policy analysis.
Declarations
Ethics approval and consent to participate
Given that we utilized publicly accessible data, no IRB or individual consent was needed.
Consent for publication
Given that we utilize publicly accessible data, individual consent for publication is not required.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Devarbhavi H, Asrani SK, Arab JP, Nartey YA, Pose E, Kamath PS. Global burden of liver disease: 2023 update. J Hepatol. 2023;79(2):516–37. [DOI] [PubMed] [Google Scholar]
- 2.Sheena BS, Hiebert L, Han H, Ippolito H, Abbasi-Kangevari M, Abbasi-Kangevari Z, et al. Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7(9):796–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harikrishnan S, Jeemon P, Mini G, Thankappan K, Sylaja P. GBD 2017 causes of death collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. 2018. [DOI] [PMC free article] [PubMed]
- 4.Zhai M, Long J, Liu S, Liu C, Li L, Yang L, et al. The burden of liver cirrhosis and underlying etiologies: results from the global burden of disease study 2017. Aging. 2021;13(1):279–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collaborators GBDMD. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371(9615):838–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleming KM, Aithal GP, Card TR, West J. The rate of decompensation and clinical progression of disease in people with cirrhosis: a cohort study. Aliment Pharmacol Ther. 2010;32(11–12):1343–50. [DOI] [PubMed] [Google Scholar]
- 9.Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with Acute Decompensation of cirrhosis. Gastroenterology. 2013;144(7):1426–e379. [DOI] [PubMed] [Google Scholar]
- 10.Al Ta’aniO, Al-Ajlouni Y, Jagdish B, Khataniar H, Aleyadeh W, Al-Bitar F, Singh T. Examining the evolving landscape of liver cancer burden in the United States from 1990 to 2019. BMC Cancer. 2024;24(1):1098. 10.1186/s12885-024-12869-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao S, Xie W, Zhang Y, Lei L, Pan Y. Changing epidemiology of cirrhosis from 2010 to 2019: results from the global Burden Disease study 2019. Ann Med. 2023;55(2):2252326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang X, Zhang X, Liu M, Zhu L, He Z. Global, regional, and national burden of cirrhosis and other chronic liver diseases due to alcohol use, 1990–2019: a systematic analysis for the Global Burden of Disease study 2019. BMC Gastroenterol. 2022;22(1):484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–71. [DOI] [PubMed] [Google Scholar]
- 15.Alberts CJ, Clifford GM, Georges D, Negro F, Lesi OA, Hutin YJF, et al. Worldwide prevalence of hepatitis B virus and hepatitis C virus among patients with cirrhosis at country, region, and global levels: a systematic review. Lancet Gastroenterol Hepatol. 2022;7(8):724–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roth G. Global burden of disease collaborative network. global burden of disease study 2017 (GBD 2017) results. Seattle, United States: Institute for health metrics and evaluation (IHME), 2018. Lancet. 2018;392:1736-88.
- 17.Al Ta'ani O, Al-Ajlouni YA, Aleyadeh W, Al-Bitar F, Alsakarneh S, Saadeh A, et al. The impact of overweight and obesity on health outcomes in the United States from 1990 to 2021. Diabetes Obes Metab. 2024;26(11):5455–5465. 10.1111/dom.15924 [DOI] [PubMed]
- 18.GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of Disease Study 2021. Lancet. 2024;402(10421):1324–45. 10.1016/S0140-6736(24)00757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang H, Abbas KM, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F, et al. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1160–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sepanlou SG, Safiri S, Bisignano C, Ikuta KS, Merat S, Saberifiroozi M, et al. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Global Burden of Disease Collaborative Network. Global burden of Disease Study 2021 (GBD 2021). Seattle, United States: Institute for Health Metrics and Evaluation (IHME); 2024. [Google Scholar]
- 22.Elsharkawy A, El-Raziky M, El-Akel W, El-Saeed K, Eletreby R, Hassany M, et al. Planning and prioritizing direct-acting antivirals treatment for HCV patients in countries with limited resources: lessons from the Egyptian experience. J Hepatol. 2018;68(4):691–8. [DOI] [PubMed] [Google Scholar]
- 23.Blachier M, Leleu H, Peck-Radosavljevic M, Valla DC, Roudot-Thoraval F. The burden of liver disease in Europe: a review of available epidemiological data. J Hepatol. 2013;58(3):593–608. 10.1016/j.jhep.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health. 2015;15:400. 10.1186/s12889-015-1720-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Askgaard G, Fleming KM, Crooks CJ, Kraglund F, Jensen CB, West J, et al. Socioeconomic inequalities in the incidence of alcohol-related liver disease: a nationwide Danish study. Lancet Reg Health Eur. 2021;8:100172. 10.1016/j.lanepe.2021.100172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Talens M, Tumas N, Lazarus JV, Benach J, Pericàs JM. What do we know about inequalities in NAFLD distribution and outcomes? A scoping review. J Clin Med. 2021;10(21):5019. 10.3390/jcm10215019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ma J, Siegel RL, Islami F, Jemal A. Temporal trends in liver cancer mortality by educational attainment in the United States, 2000–2015. Cancer. 2019;125(12):2089–98. 10.1002/cncr.31932. [DOI] [PubMed] [Google Scholar]
- 28.Jayaraman T, Lee YY, Chan WK, Mahadeva S. Epidemiological differences of common liver conditions between Asia and the West. JGH Open. 2020;4(3):332–9. 10.1002/jgh3.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mokdad AH, Jaber S, Aziz MIA, AlBuhairan F, AlGhaithi A, AlHamad NM, et al. The state of health in the arab world, 1990–2010: an analysis of the burden of diseases, injuries, and risk factors. Lancet. 2014;383(9914):309–20. [DOI] [PubMed] [Google Scholar]
- 30.Al-Ajlouni YA, Al Ta’ani O, Mushasha R, Lee JL, Capoor J, Kapadia MR, et al. The burden of musculoskeletal disorders in the Middle East and North Africa (MENA) region: a longitudinal analysis from the global burden of disease dataset 1990–2019. BMC Musculoskelet Disord. 2023;24(1):439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C screening among adults - United States, 2020. MMWR Recomm Rep. 2020;69(2):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pandyarajan V, Gish RG, Alkhouri N, Noureddin M. Screening for nonalcoholic fatty liver disease in the primary care clinic. Gastroenterol Hepatol. 2019;15(7):357. [PMC free article] [PubMed] [Google Scholar]
- 33.Younossi ZM, Noureddin M, Bernstein D, Kwo P, Russo M, Shiffman ML, et al. Role of Noninvasive tests in Clinical Gastroenterology practices to identify patients with nonalcoholic steatohepatitis at high risk of adverse outcomes: Expert Panel recommendations. Am J Gastroenterol. 2020;116(2):254–62. [DOI] [PubMed] [Google Scholar]
- 34.Sawaf B, Ali AH, Jaafar RF, Kanso M, Mukherji D, Khalife MJ, et al. Spectrum of liver diseases in patients referred for Fibroscan: a single center experience in the Middle East. Ann Med Surg (Lond). 2020;57:166–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sanai F, Alkhatry M, Alzanbagi A, Kumar S. Hepatitis B virus infection in Saudi Arabia and the UAE: public health challenges and their remedial measures. J Infect Public Health. 2023;16(9):1410–7. 10.1016/j.jiph.2023.07.008. [DOI] [PubMed] [Google Scholar]
- 36.Hashem A, Shastri Y, Al Otaibi M, Buchel E, Saleh H, Ahmad R, et al. Expert Opinion on the management of non-alcoholic fatty liver Disease (NAFLD) in the Middle East with a focus on the Use of Silymarin. Gastroenterol Insights. 2021;12(2):155–65. [Google Scholar]
- 37.Al Sebayel M, Abaalkhail F, Al Abbad S, AlBahili H, Elsiesy H, Aleid M, et al. Liver transplantation in the Kingdom of Saudi Arabia. Liver Transpl. 2017;23(10):1312–7. [DOI] [PubMed] [Google Scholar]
- 38.Hosseini SAM, Nikeghbalian S, Salahi H, Kazemi K, Shemsaeifar A, Bahador A et al. Evolution of liver transplantation program in Shiraz, Iran. Hepat Monthly. 2017;17(11).
- 39.Lankarani B, Malek Hosseini K. The Situation of Liver Transplantation Programs in Iran. Middle East J Dig Dis. 2018;10(3):194–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting this study’s findings come from the GBD study, available on the Institute for Health Metrics and Evaluation website. The GBD offers comprehensive health data worldwide, including mortality, morbidity, and risk factor estimates for various diseases and conditions.The dataset can be accessed by visiting the IHME GBD Data Tool at https://vizhub.healthdata.org/gbd-compare/#. This interactive tool allows for the exploration of health trends at global, regional, and country levels. The dataset is openly accessible under IHME’s terms, supporting its use for research and policy analysis.