Abstract
Background
The International Classification of Headache Disorders (ICHD-3) uses moderate or severe pain intensity in the diagnostic criterion for migraine. However, few studies have analyzed pain rating on a visual analog scale to identify the numerical intensity that correlates with migraine.
Objective
To evaluate the impact of daily self-rated headache pain among patients with either episodic or chronic migraine. This study specifically aims to evaluate the probability of patients labeling their head pain as a headache vs. migraine based on the pain level reported.
Methods
A retrospective chart review was conducted on patients with a clinical diagnosis of migraine from July 1, 2014, to July 1, 2019.
Results
Data of 114 subjects (57 episodic migraine and 57 chronic migraine) were used for analysis. Patients with episodic migraine on average rated a migraine more severe than a headache (4.1 vs. 6.4; p < 0.001). Patients with chronic migraine on average also rated migraine more severe than a headache (4.3 vs. 6.8; p = 0.0054). Chronic migraine patients transitioned from calling head pain a headache to a migraine significantly later than episodic migraine patients (4.5 vs. 6.8; p < 0.05).
Conclusion
A migraine is perceived as having higher pain intensity than a headache in patients with both episodic and chronic migraine. On average, patients with chronic migraine had a higher pain rating at which they report head pain to be considered a migraine.
Keywords: Chronic migraine, Episodic migraine, Headache, Visual analog scale, Pain relief
Background
Migraine is a common neurological complaint affecting an estimated 14.0% of the global population [1]. Additionally, migraine is the second highest cause of years lived with disability globally [2]. When classifying head pain as migraine, neurologists and headache specialists have largely focused on objective measurements from the International Classification of Headache Disorders (ICHD-3) [3]. The ICHD-3 classifies head pain as migraine when it is recurrent, lasting 4 h to 72 h, unilaterally located, having a pulsating quality, moderate to severe intensity, aggravated by routine physical activity, and associated with nausea and/or photophobia and phonophobia. Although the ICHD-3 uses moderate or severe intensity as an indicator for migraine diagnosis, few studies have analyzed this on a subjective pain scale. Eleven-point pain scales, such as the Visual Analogue Scale (VAS), have been found to positively impact patient care by focusing on patient pain perception and eliminating physician bias, allowing for better treatment regimens [4]. This has been recognized by the neurological community which uses the headache diary as the gold standard for assessing chronic migraine burden [5]. The headache diary is a prospective, and patient subjective, measurement of pain using an eleven-point pain scale to assess daily head pain. By having patients identify their pain daily the headache diary eliminates patient recall bias allowing for an accurate assessment of head pain burden [5].
This study uses a daily headache diary, which in addition to rating head pain, asks patients to categorize their head pain as either a headache or migraine. According to the ICHD-3, all head pain experienced by migraine sufferers is classified as migraine following a migraine diagnosis. However, the authors wanted to determine the pain intensity that patients considered their head pain to be a migraine rather than a headache subjectively. By having patients categorize their head pain as either headache or migraine, it was hypothesized that a patient’ s perception of a migraine could be predicted by the reported pain level alone.
Additionally, the use of abortive therapy for head pain was analyzed. Previous literature recommends using abortive therapy as early as possible during a migraine [6]. Patients commonly use over the counter medications such as aspirin, NSAIDs, and acetaminophen for mild to moderate headaches despite neurologists counseling against stepwise treatment. However, severe migraines are more likely to be treated with triptans, antiemetics, dexamethasone, ergotamines, isometheptene compounds or lidocaine if no improvement [6]. We compared pain ratings and head pain categorization with the use of head pain abortive therapy to find whether severity and patient head pain categorization influenced the use of abortive therapy during a migraine attack. Demographic, comorbidity, and current treatment information was also collected and analyzed to find correlations between pain severity and previously determined migraine risk factors or treatments.
Methods
Study participants
A total of 114 female and male participants (mean age 42.12 episodic and 48.09 chronic) were enrolled in this retrospective chart review. Data was collected from patient charts located in the SRS electronic medical record (EMR) system. All participants were under the care of the same board-certified headache specialist from July 2014 to July 2019. Patients between 18 and 85 years of age were included. All participants were diagnosed with either Migraine, Unspecified, not Intractable, without Status Migrainosus (International Classification of Disease, Tenth Revison (ICD-10) code G43.909) or Chronic migraine without aura, intractable, without status migrainosus (ICD-10 code G43.719). No patients diagnosed with aura were included in the data set to eliminate any biased aura symptoms, as many patients and providers perceive aura as a telling sign of migraine irrespective of severity [2].
Data collection
All participants in the study were categorized as either chronic or episodic migraine sufferers based on the number of migraines per month at time of headache diary data collection, irrespective of initial diagnosis. According to the current ICHD-3 guidelines, chronic migraine sufferers have over 15 days of head pain a month, whereas episodic migraine sufferers have less than 15 days of head pain a month. Categorization of participants may differ from initial diagnosis due to current treatment regimen with prophylactic treatment at time of data collection.
Patients included in the sample completed at least one month of head pain ratings in a prospective, non-electronic, daily headache diary. Each headache diary spanned the course of one calendar month (between 28 and 31 days). One month of headache diary data per participant was included in the final analysis. The migraine calendar month chosen from each participant for analysis was the final complete month of data collected. Headache diary data was excluded from the trial if it spanned less than one calendar month. For the daily headache diary, patients were instructed to rate their maximum head pain on an eleven-point pain scale VAS (0–10) over the previous 24 h. Patients were then instructed to categorize their head pain as either a headache or migraine based on their own perception of head pain intensity and symptoms. Patients were also instructed to indicate whether abortive therapy was used, if any, in the treatment of the pain. Demographic, comorbidity, and current treatment data were collected as dichotomous data. This data was collected from the EMR progress note that most recently listed each demographic prior to the first headache calendar month being completed. Demographic data included height, weight, age, and BMI. Comorbidity data included hypertension, hyperlipidemia, cerebrovascular disease, anxiety, and depression. Current treatment data included abortive and prophylactic therapy.
Forty-one patients were excluded from the study. Patients who listed all head pain as exclusively headache or migraine without distinction were excluded with the assumption that there was a lack of understanding of headache calendar instruction. Daily headache diaries completed outside of the July 2014 to July 2019 time frame were excluded. All data completed in less than one full month was excluded to allow for better identification of episodic vs. chronic migraine sufferers at time of the daily headache diary.
Statistical analysis
For the average headache or migraine rating for chronic/episodic conditions a MEANS Procedure was used via the SAS System. This was then followed by a t-TEST Procedure via the SAS System where average headache was directly evaluated against average migraine for episodic/chronic conditions.
For the comparison of headache ratings between episodic and chronic conditions and for the comparison of migraine ratings between episodic and chronic conditions, a t-TEST Procedure via the SAS System was used.
For the comparison of migraine ratings between episodic and chronic conditions a t-TEST Procedure via the SAS System was used.
For when episodic/chronic transition from calling head pain a headache to a migraine, a MEANS Procedure was used via the SAS System. This was then followed by a t-TEST Procedure via the SAS System to compare the transition between both groups.
For the demographics in the chronic/episodic conditions, a FREQ Procedure including a chi-square test via the SAS System was used each time.
For the medication therapy results a FREQ procedure including a chi-square test via the SAS System was used to compare the groups. Additionally, a t-TEST Procedure via the SAS System was used to compare the means of each group.
Results
Data of 114 subjects (57 episodic migraine patients and 57 chronic migraine patients) were used for analysis.
Demographics and comorbidities
Demographics and comorbidities (Table 1 and Table 2) are listed below for each group. Among those with episodic migraines, the mean migraine rating among females was 6.4 while males were 6.5, This was not statistically significant (p = 0.915). Furthermore, the mean headache rating among females was 4.1 while males was 3.8 and this was also not statistically significant (p = 0.681). Among those with chronic migraines, the mean migraine rating among females was 6.9 and 4.8 for males. This association was statistically significant (p = 0.004). However, the mean headache rating among females was 4.4 while males were 2.6 and this association was not statistically significant (p = 0.083).
Table 1.
Demographics and comorbidities for patients diagnosed with episodic migraines
| Demographic | Number of patients |
|---|---|
| female | 53 |
| Male | 4 |
| Age | 47.32 |
| Hypertension | 12 |
| Hyperlipidemia | 9 |
| Cerebrovascular disease | 6 |
| Anxiety | 25 |
| Depression | 20 |
Table 2.
Demographics and comorbidities for patients diagnosed with chronic migraines
| Demographic | Number of patients |
|---|---|
| female | 54 |
| Male | 3 |
| Age | 49.05 |
| Hypertension | 6 |
| Hyperlipidemia | 7 |
| Cerebrovascular disease | 2 |
| Anxiety | 22 |
| Depression | 20 |
Pain severity rating
Among study participants with episodic migraine, the average headache rating was 4.1 and the average migraine rating was 6.4. This association was statistically significant (p < 0.001). Among study participants with chronic migraines, the average headache rating was 4.3 and the average migraine rating was 6.8. This association was statistically significant (p = 0.0054).
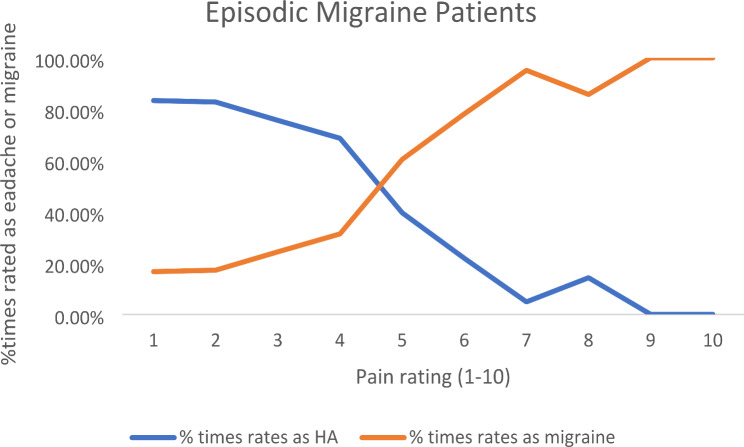
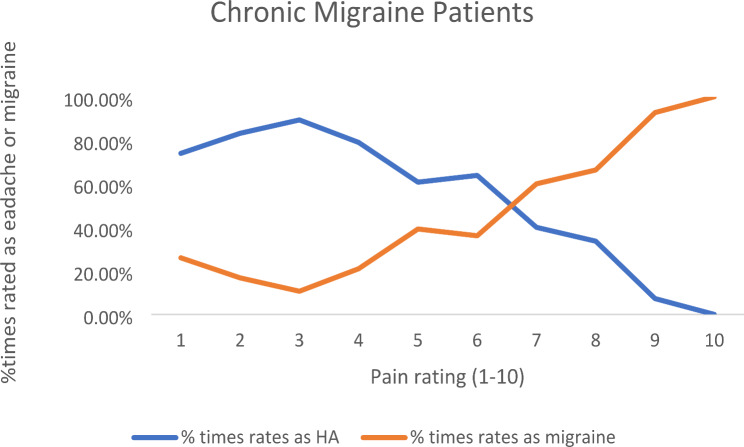
On a VAS pain scale from 0 to 10, episodic patients change from calling a headache to a migraine at 4.5. while chronic patients change from calling a headache to a migraine at 6.8 This was statistically significant (p < 0.05). (See Graph 1 and 2)
Graph 1.
Percent of head pain episodes rated as headache vs. migraine on VAS pain scale from 0 to 10. Episodic migraine patients change from calling a headache to a migraine at 4.5
Graph 2.
Percent of head pain episodes rated as headache vs. migraine on VAS pain scale from 0 to 10. Chronic migraine patients change from calling a headache to a migraine at 6.8
Abortive therapy
The mean number of times using abortive medication per migraine among those with chronic migraines was 6.15 and among those with episodic migraines was 0.80 (p < 0.001). The mean of number of times using abortive medication per headache among those with chronic migraines was 5.44 and among those with episodic migraines was 0.54 (p < 0.001).
Discussion
The complexity of pain beliefs arises from the subjectivity of pain where the belief of what the pain means for the patient may differ with scientific understanding. Thus, self-recorded ratings of headache category and severity in a headache calendar or diary are widely recommended for patients with a clinical diagnosis of migraine headaches. These calendars can help patients identify patterns and triggers of their headaches, as well as assist clinicians in proper diagnosis of headache category, such as episodic or chronic type. The subjective information that patients provide clinicians as well as having a proper diagnosis for headache type is important for creating the proper treatment plan for each patient [5, 7].
Pain burden can be measured using a headache calendar to aid physicians in assessing migraine experience. In the current study, both episodic and chronic migraine patients consider a migraine to be more severe than a headache. Condello et al. [8] used a questionnaire to conclude that both episodic and chronic migraine patients have similar personal beliefs regarding their subjective experience of migraine pain. This emphasizes the similarity of pain perception amongst both groups and is consistent with the current study. Similarly, previous studies support the finding that migraines are rated as more intense than other types of headaches. A review from Stewart et al. [9] found that patients from population-based studies report migraines to be more disabling, painful, and longer in duration than headaches.
This is one of the first studies, to our knowledge, that addresses when migraine sufferers transition from calling head pain a headache to a migraine. It was found that on the pain rating scale, chronic migraine patients stop calling head pain a headache and begin calling it a migraine when it is significantly more intense than episodic migraine patients. It is hypothesized that this may be due to a prolonged tolerance effect following long-term chronic pain. Researchers have found that continuous exposure to painful stimuli may lead to an increase pain tolerance through conditioning and adaptation [10, 11]. Future studies should evaluate this potential prolonged tolerance effect in chronic migraine patients compared to episodic migraine sufferers.
Migraine prevention and abortive treatment are critical in the management of patient’s pain experience. Abortive treatment for chronic migraines can help decrease attack intensity to improve quality of life. In the current study, abortive medications are more likely to be used when head pain is considered a migraine by patients with both episodic and chronic migraines. This is consistent with either an increase in pain intensity and disability associated with migraines compared to headaches [12], or an association patients make by attributing the use of abortive therapy with migraine. Sun-Edelstein et. Al.’s review on the pharmacological treatment of chronic migraine emphasizes the goal of acute abortive treatment resulting in headache freedom within 2 h. The current study found that abortive medication for headaches and migraines is more likely to be used with chronic migraine patients than episodic migraine patients. It is hypothesized that abortive medication is of utmost importance for chronic migraine sufferers to decrease the higher pain intensity levels and maintain quality of life. Magnusson et al. [13] utilized headache diaries and a pain inventory to conclude that headache intensity is the major correlate to headache-related disability, with increased levels of pain intensity leading to increased levels of disability. Thus, future studies should address the higher utilization of abortive medication for chronic migraine patients, where it is most likely used to decrease these higher levels of disability.
Finally, the design of the current study leads to some limitations. As a retrospective chart review, there may be selection bias, information bias, missing data, patient recall bias, and generalization bias. It is important to consider that the VAS analog scale is only one patient-reported outcome measure (PROM) and therefore is subject to limitations surrounding patients’ understanding of this 10-point measure [14]. Additionally, most of the subjects included in both groups were female. Females are more likely to suffer from migraine pain due to the role of estrogens in neuroexcitability in the brain, so the distribution in the study is consistent with previous literature [15]. However, this potentially leads to confounding factors within the current study. Future studies should evaluate gender differences in subjectivity amongst migraine pain and how these correlate with abortive therapy use. The current study also includes data from only one migraine clinic, which may limit the generalizability of its findings. Future studies should evaluate patient pain perceptions across diverse populations to determine if perceptions vary between groups.
Conclusion
Patients on average rate a migraine to be more severe than a headache, consistent with migraine severity as moderate or severe. A higher VAS pain score is reported as a migraine in chronic migraine patients suggesting a shift in pain tolerance. Additional prospective clinical trials are recommended moving forward to aid in quantifying the pain burden of migraine on patients.
Acknowledgements
Janet Simon, PhD from Ohio University, Athens, Ohio for assistance with data analysis.
Abbreviations
- EMR
Electronic medical record
- ICD-10
International Classification of Disease, Tenth Revison
- ICHD-3
International Classification of Headache Disorders
- PROM
Patient Reported Outcome Measure
- VAS
Visual Analogue Scale
Author contributions
H.L. and M.T. contributed in design of the work. E.T., E.P. contributed in data acquisition. E.T., E.P., and M.T. contributed in drafting the manuscript and preparing all figures. P.M., M.T. contributed in substantive revision of the final manuscript. M.T. contributed as the principal investigator. All authors reviewed the manuscript.
Funding
None to disclose.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Mount Carmel Institutional Review Board.
Mount Carmel Corporate Services Center 6150 East Broad Street Columbus, Ohio 43213.
Email: irb@mchs.com Consent: Approval for a Chart Review with consent waived for the use of protected health information was obtained.
Competing interests
Martin Taylor, DO, PhD is a consultant speaker and participates in research support for Abbvie. He is a consultant for Revance. He also participates in research support for Ipsen.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stovner LJ, Hagen K, Linde M, et al. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23:34. 10.1186/s10194-022-01402-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steiner TJ, Husøy A, Stovner LJ. GBD2021: headache disorders and global lost health – a focus on children, and a view forward. J Headache Pain. 2024;25:91. 10.1186/s10194-024-01795-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. 10.1177/0333102413485658 [DOI] [PubMed]
- 4.Cakir U, Cete Y, Yigit O, Bozdemir MN. Improvement in physician pain perception with using pain scales. Eur J Trauma Emerg Surg. 2018;44(6):909–15. 10.1007/s00068-017-0882-7 [DOI] [PubMed] [Google Scholar]
- 5.Nappi G, Jensen R, Nappi R, Sances G, Torelli P, Olesen J. Diaries and calendars for migraine. Rev Cephalalgia. 2006;26(8):905–16. 10.1111/j.1468-2982.2006.01155.x [DOI] [PubMed] [Google Scholar]
- 6.Jenkins B. Migraine management. Aust Prescr. 2020;43(5):148–51. 10.18773/austprescr.2020.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Torres-Ferrus M, Gallardo VJ, Alpuente A, Pozo-Rosich P. Influence of headache pain intensity and frequency on migraine-related disability in chronic migraine patients treated with OnabotulinumtoxinA. J Headache Pain. 2020;21(1). 10.1186/s10194-020-01157-8 [DOI] [PMC free article] [PubMed]
- 8.Condello C, Piano V, Dadam D, Pinessi L, Lanteri-Minet M. Pain beliefs and perceptions inventory: a cross-sectional study in chronic and episodic migraine. Headache. 2015;55(1):136–48. [DOI] [PubMed] [Google Scholar]
- 9.Stewart WF, Shechter A, Lipton RB. Migraine heterogeneity. Disability, pain intensity, and attack frequency and duration. Neurology. 1994;44(6 Suppl 4):S24–39. [PubMed] [Google Scholar]
- 10.Williams DA, Thorn BE. An empirical assessment of pain beliefs. Pain. 1989;36(3):351–8. 10.1016/0304-3959(89)90095-X [DOI] [PubMed] [Google Scholar]
- 11.Heinricher MM. Pain modulation and the transition from acute to chronic pain. In: Ma C, Huang Y, editors. Translational research in pain and itch. Advances in Experimental Medicine and Biology. Volume 904. Dordrecht: Springer; 2016. [DOI] [PubMed] [Google Scholar]
- 12.Sun-Edelstein C, Rapoport AM. Update on the pharmacological treatment of chronic migraine. Curr Pain Headache Rep. 2016;20:6. [DOI] [PubMed] [Google Scholar]
- 13.Magnusson JE, Becker WJ. Migraine frequency and intensity: relationship with disability and psychological factors. Headache. 2003;43(10):1049–59. 10.1046/j.1526-4610.2003.03206.x [DOI] [PubMed] [Google Scholar]
- 14.Waliszewska-Prosół M, Montisano DA, Antolak M, et al. The impact of primary headaches on disability outcomes: a literature review and meta-analysis to inform future iterations of the global burden of disease study. J Headache Pain. 2024;25:27. 10.1186/s10194-024-01735-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossi MF, Tumminello A, Marconi M, Gualano MR, Santoro PE, Malorni W, Moscato U. Sex and gender differences in migraines: a narrative review. Neurol Sci. 2022;43(9):5729–34. 10.1007/s10072-022-06178-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.