Abstract
Background
Encouraging compliance with recommended levels of exercise for older adults is a public health challenge. A minimal-resource solution is telephone coaching.
Objectives
Primary aim: to compare timed up and go (TUG) performance 6 months after beginning a home exercise program between a group of older individuals who received additional telephone coaching, and a control group performing the home exercise program alone. Secondary aims: to compare functional and fall-related outcomes between groups at 6 and 12 months.
Methods
Multicentre, assessor-blinded, randomised, controlled, open label, prospective study. Inclusion criteria included age ≥ 65 years, ≥ 1 fall in the past year, and discharged home from hospital rehabilitation or outpatient physiotherapy. All participants received a home exercise booklet and were asked to perform a set of exercises as often as possible (daily). The coaching group additionally received a monthly telephone call (total 5 calls) from their previous physiotherapist. Primary outcome was TUG performance at 6 months. Outcomes were measured at inclusion, and at 6 and 12 months. The primary outcome was analysed using a linear mixed model adjusted for the baseline value.
Results
In total, 99 individuals were included (coaching group n = 50, control group, n = 49; mean [SD] age 83.1 [5.8] years and 77% women). TUG performance did not differ between groups at 6 months (adjusted difference 1.37, SE 1.32, 95% CI 1.26 to 4.01, p = 0.30). Secondary outcomes did not differ between groups at 6 or 12 months except compliance to the exercise program was higher in the coaching than the control group at 6 months (adjusted difference 1.0, SE 0.5, 95% CI 0.02 to 2.0, p = 0.05).
Conclusions
The lack of difference between the groups in the time taken to complete the TUG at 6 months suggests that the monthly telephone coaching sessions did not improve the effectiveness of a home exercise programme in elderly people who had suffered at least one fall. The trial was registered on ClinicalTrials.gov (NCT02828826; 11th of july 2016, last modification 16th of September 2024).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-05488-y.
Keywords: Older adults, Exercise, Telephone coaching, Compliance, Falls
Introduction
Falls experienced by older adults are a major public health issue. In France, over 2 million people aged > 65 years fall each year [1]. A study on health behaviours reported that 19.5% of individuals aged 55 to 85 years reported limiting their movements to avoid falling again [2]. Recurrences are frequent, with a prevalence ranging from 10 to 25% depending on age, comorbidities, and institutionalization [3].
Recent recommendations state that older adults at low fall risk should aim to participate in 150–300 min per week of intermediate-intensity physical activity or 75–150 min per week of vigorous-intensity physical activity, those at a medium risk should participate in supervised programs and those at high fall risk should undergo multidomain interventions [4]. However, such programs are not yet available throughout France. In France, older adults who are hospitalised and found to have impaired balance and gait usually undergo rehabilitation. At discharge, they may be prescribed further rehabilitation. Those considered to have recovered sufficient capacity may not receive such a prescription. These individuals are at risk of losing their recent improvements if they do not strive to maintain them. Equally, individuals who partake in a period of outpatient rehabilitation to improve their balance and gait capacity may lose the benefits after discharge. Without maintenance exercises, physical performance declines after a few weeks, depending on the individuals’ ages and the duration of training [5–8]. Maintaining the benefits of rehabilitation after discharge from inpatient or outpatient physiotherapy is therefore essential to prevent decline and reduce the fall risk.
Home exercises programs, such as the Otago Exercise Program [9], have been developed to improve functional capacity in older adults and reduce the fall risk. However, long-term compliance to these programs is an issue. The first study of the Otago Exercise Program found that at one year, only 42% (48 of 114) of those in the exercise group were still completing the programme ≥ 3 times a week [9]. Mean compliance to the balance and strength retraining component of another program was only 63% [10], and for another program only half of participants reported performing exercises for at least 75% of the intervention period [11]. Even compliance to supervised programs may be low. In a weekly program involving balance and strength training, mean attendance was only once every 2 weeks [12].
Encouraging compliance to the recommended levels of exercise is thus a public health challenge. One solution that uses minimal resources is telephone coaching. Telephone coaching involves regular telephone calls by a professional to an individual at home with the aim of supporting them in their care program. Telephone coaching appears to be effective for different conditions, including compliance to a dietary plan [13], smoking cessation [14], and patient follow-up after discharge from hospitalization [15]. In the rehabilitation field, a study on the impact of telephone follow-up in people with osteoarthritis demonstrated improvements in physical performance [16].
The main aim of the study was to compare physical performance at 6 months in a group of elderly patients who had suffered a fall and had returned home receiving telephone coaching from a physiotherapist and a control group without this telephone coaching. The secondary aims were (1) to evaluate and compare between the 2 groups at 12 months the effect of telephone coaching on physical performance and (2) to evaluate and compare between the 2 groups at 6 and 12 months (a) the number of falls, (b) fear of falling, (c) autonomy, (d) lower limb performance, (e) one leg balance, (f) walking speed, (g) number of repeat hospitalisations for falls, (h) number of physiotherapy sessions and (i) the number of exercises performed per week from the program provided.
We hypothesized that monthly telephone coaching by a physiotherapist in addition to the provision of an exercise booklet would improve outcomes relative to the group that only received the exercise booklet.
Methods
Design
We conducted a multicentre, randomised, controlled, open label, prospective study between October 2016 and August 2022.
Participants were recruited among those being discharged home from hospital or being discharged from outpatient physiotherapy and living at home. Individuals who had undergone physiotherapy to improve gait and balance were potentially eligible. Participating outpatient clinics were recruited via the Primary Care Research Network of Nantes, other physiotherapy networks, at conferences and by word of mouth between physiotherapists.
The participating physiotherapist at each centre performed the inclusion and randomisation. Randomisation was centralised and performed using a secure, computer-generated, interactive, web-response system (ENNOV CLINICAL software) available at each study centre. Randomisation was stratified on study centre with a 1 : 1 ratio and performed with fixed blocks.
Participants
Inclusion criteria were people aged ≥ 65 years, ≥ 1 fall in the past year, being discharged home from hospital rehabilitation with no prescription for further physiotherapy or being discharged from outpatient physiotherapy and living at home, ≥ 24/30 points on Mini Mental Status evaluation, able to stand up from a chair and walk ≥ 6 m with no human assistance and having provided written informed consent.
We did not include people who were under guardianship, had a progressive or degenerative pathology that could affect gait, were unable to use a telephone, had a visual impairment preventing reading of the exercise program, who refused to participate, who did not want to stop outpatient physiotherapy for the study duration, or who were included in another interventional research protocol Table 1 shows the locations where participants were included.
Table 1.
Inclusion center
| Center | In/outpatient |
Coaching N = 50 |
Control N = 49 |
Total N = 99 |
| Hospital center Cholet | inpatient | 15 (30.0%) | 14 (28.6%) | 29 (29.3%) |
| Hospital center La Rochelle | inpatient | 0 (0.00%) | 1 (2.0%) | 1 (1.0%) |
| Hospital center La Roche sur Yon | inpatient | 0 (0.00%) | 1 (2.0%) | 1 (1.0%) |
| Nantes | outpatient | 1 (2.0%) | 2 (4.1%) | 3 (3.0%) |
| Hospital center Montaigu | inpatient | 2 (4.0%) | 2 (4.1%) | 4 (4.0%) |
| Hospital center Nantes | inpatient | 21 (42.0%) | 20 (40.8%) | 41 (41.4%) |
| Pontchâteau | intpatient | 1 (2.0%) | 0 (0.00%) | 1 (1.0%) |
| Puy-en-Velay | outpatient | 2 (4.0%) | 2 (4.1%) | 4 (4.0%) |
| Hospital center Saint-Nazaire | inpatient | 5 (10.0%) | 5 (10.2%) | 10 (10.1%) |
| Saint Gervais | outpatient | 3 (6.0%) | 2 (4.1%) | 5 (5.1%) |
| Outpatient inclusion |
Coaching N = 50 |
Control N = 49 |
Total N = 99 |
|
| NON | 44 (88.0%) | 43 (87.8%) | 87 (87.9%) | |
| OUI | 6 (12.0%) | 6 (12.2%) | 12 (12.1%) |
Intervention
Participants were asked to stop their usual physiotherapy, if they had any, during the study period.
All participants received an exercise booklet from their hospital or outpatient physiotherapist who explained the booklet to them and checked they could do all the exercises correctly and safely.
The exercise booklet had been developed previously by the first author (GR) who had been using it in his practice for 2 years. It was 24 pages long and began with information about gait and balance and the effects of aging, how to get up off the floor and what to do in case of a severe fall, recommendations in terms of footwear, and information about why exercising is important. The main part described the exercises, with illustrations for each (Additional file 2). The exercises were organised into 3 categories according to their purpose: flexibility, transfers and strengthening, and balance and gait. To ensure safety, all the exercises were organised around a chair. Some were performed sitting in the chair and others standing holding the chair or walking around the chair. Participants were instructed to perform at least one exercise from each category as often as possible (daily) for the whole duration of the study (12 months).
More specifically, each intervention lasts about 20 min (semi-directive and motivational interview, questions about general condition, events that have occurred events since the last call, a report on the interview practice, the number of falls, a remote self-evaluation (unipodal balance, FTSST, fear of falling). 5 telephone calls were planned as part of this study, at a rate of one call per month.
Control group
Participants in the control group received no further follow-up other than the assessments at M6 and M12. Exercise booklets were given to facilitate reader comprehension.
Intervention group
Participants in the coaching group received a monthly telephone call from their hospital or outpatient physiotherapist (total of 5 telephone calls). Calls lasted approximately 20 min and included a semi-directed motivational interview, questions about general state of health, events since the last call, exercises the person had undertaken, the number of falls, a remote self-assessment of some follow-up criteria (one leg balance, FTSST and fear of falling). Using this information, the physiotherapist encouraged the person to continue to practise the exercises as regularly as possible, or to increase the number and/or frequency of exercises performed depending on the self-assessment results.
Endpoints
The primary endpoint was the between group difference in Timed Up and Go (TUG) test performance time 6 months after discharge from the rehabilitation department.
The secondary endpoints were between group difference in:
TUG test performance time at 12 months.
At 6 and 12 months:
Number of falls.
Fear of falls rating on a VAS.
Instrumental Activities of Daily Living (IADL) score.
Five Times Sit to Stand Test (FTSST) score.
One leg balance time.
Speed on the 4 m timed walk.
Number of hospital admissions for falls.
Requirement of outpatient physiotherapy for rehabilitation.
Self-reported number of exercise sessions performed.
Assessments
The following demographic and clinical data were noted by interviewing the participant: age, sex, the presence of an informal carer at home, type of residence (home or non-medicalised residential care facility) body mass index, and mini mental state score.
Participants underwent 3 assessments: before discharge from hospital or from outpatient physiotherapy (M0), 6 months post discharge (M6) and 12 months post discharge (M12).
The assessments at M6 and M12 were carried out during a visit to the investigator site.
Assessments were performed by a trained clinical research technician who was blinded to group allocation. Data relating to hospital admission for falls and attendance of outpatient physiotherapy were sought from the individual or their general practitioner if the participant reported having consulted during the study period.
Timed up-and-go test
The TUG test measures gait capacity and balance. Participants were asked to stand up from a standard chair with armrests, to walk 3 m to a line marked on the floor, turn around, return and sit down in the chair. Participants wore their usual shoes and used their usual gait aids. Performance time was measured using a stopwatch. A practice run was allowed and then 1 trial was timed.
The TUG test is reliable and has excellent interrater agreement [17]. It has good diagnostic validity with a sensitivity and specificity of 87% for the prediction of falls [18].
Occurrence of falls
Participants were asked to record any falls on the appropriate date in their exercise log-book. A fall was defined as “the fact of finding oneself involuntarily on the ground or in a position lower than one’s starting position” [3, 19].
Fear of falling
Participants were asked to rate their fear of falling on a visual analogue scale (VAS) ranging from 0/10 “no fear of falling” to 10/10 “extreme fear of falling”.
Instrumental activities of daily living [20]
The Instrumental Activities of Daily Living (IADL) [20] assesses a patient’s level of dependence to perform activities of daily living. It consists of a scale evaluating 8 activities that the individual must be able to perform to remain at home: using the telephone, shopping, food preparation, housekeeping, laundry, mode of transportation, responsibility for own medications, and ability to handle finances. The score ranges from 0 to 8 points.
Five times sit to stand test [21]
The FTSST test is a functional test of lower limb strength and balance. The time taken to rise as fast as possible 5 times in a row from a standard chair without pushing on the armrests is measured.
One leg balance test [22]
This test is a timed assessment of postural maintenance of static single-limb postural balance Participants were asked to stand on the foot of their choice for as long as possible. Performance was timed using a stopwatch. Three trials were performed and the best result was used in the analysis.
Balance on one leg appears to be a significant predictor of falls with injuries (relative risk: 2.13; 95% CI: 1.04, 4.34; P =. 03) [22].
Gait speed
The assessment of gait speed is an objective measure of the functional mobility of an older person. Gait speed was assessed over 4 m [23, 24]. Participants walked at their own, comfortable pace. Performance time was measured using a stopwatch that began when the participant initiated the first step and ended when they crossed the 4 m mark. Two trials were recorded and the fastest was used in the analysis. This test has excellent reliability [25]. A walking speed of less than 1 m/Sect. (4 s for 4 m) is an indicator of frailty [26].
Hospital admission for a fall
Any hospital admissions for a fall were collected by asking the participant or by consulting their medical records.
Outpatient physiotherapy
Any outpatient physiotherapy prescriptions to improve gait and/or balance made by the participant’s general practitioner during the study period were collected by asking the participant or by consulting their medical records.
Number of exercise sessions per week
Participants were provided with a log-book in which they were asked to mark the days on which they performed a complete exercise session (at least 1 exercise from each category = 3 exercises).
Training of participating physiotherapists
The first author (GR) trained all participating physiotherapists either during a ½ day onsite session or during a 2.5 h video-conference session for those who could not attend because of the distance involved. The project manager was also present to discuss the legal and financial aspects of the project. Participating physiotherapists also received a telephone coaching guide booklet (Additional file 1).
Statistical analysis
Sample size
A descriptive pilot study of 25 individuals undergoing physiotherapy associated with follow-up telephone coaching conducted in our department (unpublished) showed that mean (SD) TUG performance time decreased (i.e., improved) from 15.1 (4.5) s to 11.8 (2.6) s at 6 months. Considering an alpha risk of 5%, a power of 80%, and an SD of 4.5s, a sample size of 162 individuals was necessary to detect a difference of 2s on the TUG between groups. Accounting for a 10% rate of missing values (withdrawal of consent, loss to follow-up etc.), a total of 180 patients were to be randomized, with 90 patients per group.
Baseline description
Descriptive analysis of all variables was performed for the whole sample and for each group, and data are presented as numbers and percentages for qualitative variables and minimum, maximum, mean, standard deviation and quartiles for quantitative variables.
Sample and missing data
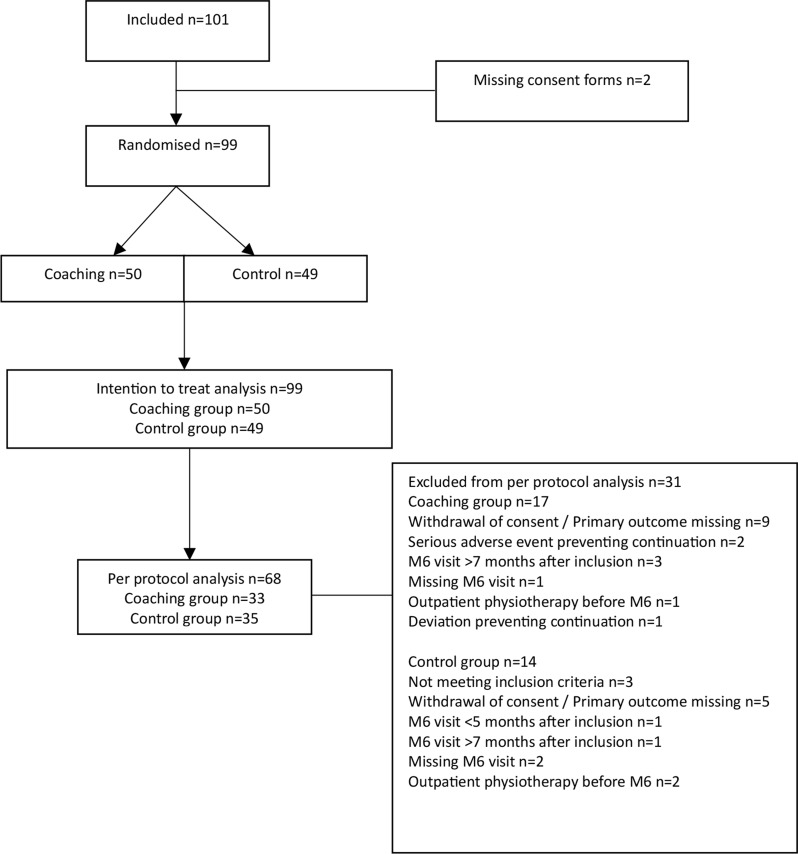
Analyses were performed according to the intention to treat principle on all randomized individuals. A sensitivity analysis was also performed on the per protocol population on the primary endpoint. The Fig. 1 shows the participants excluded from the per protocol analysis.
Fig. 1.
Flow chart of inclusions in the intention to treat and per protocol analyses
For the primary endpoint, missing data were imputed with multiple imputation (predictive mean matching). No imputation was done on secondary endpoints.
Analysis of primary endpoint: mean TUG performance time at 6 months was compared between the 2 groups using a linear mixed model with the TUG time at D0, the group, the visit and the interaction between group and visit as fixed factors and with patients and centers as random factors. Model without centers effect was presented on appendix with goodness of fit for the 2 models (BIC).
Secondary endpoint analyses involved comparing endpoints between the 2 groups using either linear mixed models or generalized linear models with random effects. In theses models, participants were considered as random effect to taking into account repeated measured at M6 and M12 and the randomisation stratification on centers. For quantitative variables, these models were adjusted for baseline values.
Results
Participants
Ten centres (7 hospitals and 3outpatient physiotherapy clinics) participated in the study. In total, 101 individuals were included. Two consent forms were missing, therefore and 99 participants were randomly allocated to the coaching or the control group. Mean (SD) age was 83.1 (5.8) years (range 65 to 98 years) and 77% were women (Table 2).
Table 2.
Outcomes and results of between-group analyses at each time point
| Test | Time point | Coaching n = 50 |
Missing data | Control n = 49 |
Missing data | Adjusted difference / OR | SE | 95% CI | p-value |
|---|---|---|---|---|---|---|---|---|---|
| TUG (sec) | M0 | 14.7 (7.6) | 1 | 14.4 (12.3) | 3 | ||||
| M6 | 14.8 (6.4) | 13 | 12.9 (5.0) | 10 | 1.37 | 1.32 | -1.26 to 4.01 | 0.30 | |
| M12 | 14.9 (8.3) | 15 | 13.6 (7.0) | 15 | 1.72 | 1.33 | —-0.96 to 4.40 | 0.20 | |
| ≥ 1 fall YES | M6 | 11 (23.9%) | 4 | 9 (20.9%) | 6 | 1.19 | 0.43 to 3.25 | 0.73 | |
| M12 | 6 (12.2%) | 1 | 9 (20.0%) | 4 | 0.56 | 0.18 to 1.73 | 0.31 | ||
| Fear of falling | M0 | 3.8 (2.3) | 1 | 2.7 (2.0) | 3 | ||||
| M6 | 3.7 (2.3) | 13 | 3.4 (2.6) | 10 | -0.56 | 0.54 | -1.64 to 0.53 | 0.31 | |
| M12 | 3.7 (2.5) | 15 | 3.8 (2.8) | 13 | -0.69 | 0.55 | -1.80 to 0.41 | 0.22 | |
| IADL score | M0 | 6.9 (1.4) | 1 | 7.3 (1.1) | 3 | ||||
| M6 | 6.8 (1.4) | 13 | 7.1 (1.3) | 9 | -0.09 | 0.27 | -0.63 to 0.44 | 0.73 | |
| M12 | 6.6 (1.8) | 15 | 7.1 (1.5) | 13 | -0.28 | 0.28 | -0.83 to 0.28 | 0.32 | |
| One leg balance time (sec) | M0 | 7.9 (10.8) | 2 | 7.4 (7.5) | 3 | ||||
| M6 | 7.9 (10.9) | 16 | 9.0 (7.2) | 11 | -1.31 | 2.44 | -6.21 to 3.58 | 0.59 | |
| M12 | 7.6 (11.2) | 18 | 12.5 (16.7 | 16 | -5.72 | 2.56 | -10.85 to -0.60 | 0.03 | |
| Five Times Sit To Stand time* (sec) | M0 | 16.2 (10.0) | 11 | 13.7 (5.6) | 7 | ||||
| M6 | 15.3 (4.2) | 20 | 15.0 (5.3) | 12 | -0.17 | 1.16 | -2.51 to 2.16 | 0.88 | |
| M12 | 16.9 (5.8) | 19 | 14.4 (4.2) | 16 | 1.87 | 1.20 | -0.54 to 4.28 | 0.13 | |
| Gait speed (m/s) | M0 | 1.4 (0.7) | 1 | 1.2 (0.3) | 3 | ||||
| M6 | 1.5 (0.9) | 13 | 1.3 (0.6) | 10 | 0.08 | 0.14 | -0.20 to 0.36 | 0.56 | |
| M12 | 1.5 (0.7) | 15 | 1.3 (0.6) | 15 | 0.04 | 0.15 | -0.25 to 0.33 | 0.80 | |
| ≥ 1 admission for fall YES | M6 | 2 (4.3%) | 4 | 2 (4.9%) | 8 | 0.89 | 0.11 to 6.95 | 0.91 | |
| M12 | 1 (2.2%) | 4 | 2 (4.9%) | 8 | 0.43 | 0.04 to 5.29 | 0.51 | ||
| Need for outpatient physio YES | M6 | 9 (23.1%) | 11 | 11 (27.5%) | 9 | 0.79 | 0.28 to 2.26 | 0.66 | |
| M12 | 11 (31.4%) | 15 | 14 (38.9%) | 13 | 0.72 | 0.26 to 1.98 | 0.52 | ||
| NO. exercises performed per week | M6 | 3.8 (2.1) | 13 | 2.7 (2.0) | 9 | 1.0 | 0.5 | 0.02 to 2.0 | 0.05 |
| M12 | 2.5 (2.3) | 16 | 2.5 (2.4) | 14 | -0.01 | 0.5 | -1.1to 1.0 | 0.99 |
Data are mean (Standard Deviation) or n (%)
* Some participants used the armrests to stand during the FTSST
** Adjusted difference for quantitative variable / Odd Ratio (OR) for qualitative variable
For quantitative variables, data are difference and SE (linear mixed model, adjusted on baseline value and with center as random effect), for qualitative variables, data are OR (generalised linear mixed models with center as random factor)
Primary outcome (Table 3)
Table 3.
Participant demographics
| COACHING N = 50 |
CONTROL N = 49 |
Total N = 99 |
||
|---|---|---|---|---|
| Age (year) | Missing | 1 | 2 | 3* |
| Mean (SD) | 82.8 (6.9) | 83.4 (4.4) | 83.1 (5.8) | |
| Sex | Missing | 1 | 2 | 3 |
| Male | 13 (26.5%) | 9 (19.1%) | 22 (22.9%) | |
| Female | 36 (73.5%) | 38 (80.9%) | 74 (77.1%) | |
| Informal carer at home | Missing | 1 | 2 | 3 |
| Yes | 18 (36.7%) | 12 (25.5%) | 30 (31.3%) | |
| Type of residence | Missing | 1 | 2 | 3 |
| Home | 47 (95.9%) | 46 (97.9%) | 93 (96.9%) | |
| Residential care | 2 (4.1%) | 1 (2.1%) | 3 (3.1%) | |
| Body mass index (Kg /m²) | Missing | 1 | 2 | 3 |
| Mean (SD) | 24.8 (3.8) | 25.1 (4.1) | 25.0 (3.9) | |
| Mini mental state score | Missing | 1 | 2 | 3 |
| Mean (SD) | 27.5 (1.9) | 27.0 (1.7) | 27.3 (1.8) | |
* These 3 participants withdrew consent and opposed the use of their data
Change in TUG performance time did not differ between groups at M6.
Per protocol analysis was also performed for the primary outcome. The conclusion of this analysis was the same as that of the ITT analysis for the TUG time at M6, i.e., no between-group difference (difference 1.20, SE 1.40, 95% CI -1.61 to 4.01, p = 0. 0.39).
Secondary outcomes (Table 3)
No significant differences were found between the groups for any of the secondary outcomes except at M6 for the number of exercises performed per week which was significantly higher in the coaching than the control group, and a statistically significantly better balance at 12 months in the control group compared with the coaching group.
In total 24% of participants in the coaching group and 21% of participants in the control group reported 1 or more falls between M0 and M6; 12% of the coaching group and 20% of the control group reported 1 or more falls between M6 and M12. In total, 4% of participants in the coaching and 5% in the control group required hospitalisations before M6, and 2% in the coaching group and 5% in the control group required hospitalisations between M6 and M12. One fall occurred while performing the exercises; the 85-year-old participant sustained a femoral trochanter fracture.
Harms
Two serious adverse event preventing continuation occurred during the trial: one patient developed cancer preventing continuation of the protocol, and the other died of multivisceral failure.
Discussion
Summary of results
This study of the effects of telephone coaching provided to support a home exercise program on TUG performance did not find a greater effect of coaching than of the provision of a home exercise booklet alone, in contrast with our hypothesis. None of the secondary outcomes were enhanced by the coaching, except for number of exercise sessions per week, which was stronger in the group that received the coaching than the group that did not.
Lack of an effect of telephone coaching on outcomes
Few studies have specifically evaluated the additional benefits of telephone coaching supporting a home exercise program in older adults experiencing falls. One study evaluated the impact of telephone coaching in addition to a home exercise program for people with knee osteoarthritis. Both groups received 5 × 30 min sessions of face-to-face physiotherapy over 6 months and participants in the coaching group additionally received 6–12 telephone coaching sessions during the same period. However, similarly to our study, functional outcomes did not differ between groups [27], although both groups in that study improved. In both that study and the present study, the lack of a between-group difference in any of the functional outcomes occurred despite greater compliance to the exercise program by the coaching group − 14% more over 6 months in Bennel et al.‘s study and an extra session per week in our study. A study of people discharged home after a stroke who received either standard care (including rehabilitation) or standard care with an additional individualised coaching program involving exercise and activity, which was considerably more intense than the home exercise and telephone coaching proposed in the present study, also found no impact of coaching on functional outcomes, despite a reasonable level of compliance [28]. Although these studies were performed in people with dissimilar pathologies and using diverse types of outcome measures, these results suggest that substantial differences in compliance may be necessary to alter functional outcomes. Further studies should address the question of how to induce such a substantial difference using telephone coaching.
Effect of coaching on number of exercise sessions per week
Although the coaching did not improve any performance related outcomes relative to the control group in the present study, it did improve compliance to the exercise program. The coaching group performed on average 1 more exercise session per week (3.8 sessions) than the control group (2.7 sessions) during the first 6 months post discharge. Once the coaching was stopped, the weekly number of sessions reduced by around 1 session in the coaching group, further supporting the beneficial effect of the coaching on compliance. According to the literature, telephone coaching facilitates behaviour change [16] and improves compliance to home exercise programs. However, this effect is stronger if there is some face-to-face contact with the telephone coach as this facilitates relationship building [29, 30]. In the present study, the telephone coach was the participant’s previous physiotherapist, therefore a relationship had already been established.
Between 6 and 12 months, both groups performed a similar weekly number of sessions (2.5 sessions). The relatively good compliance of the control group could explain the lack of difference in outcomes between the groups, a between-group difference of only 1 session per week during the first 6 months of the study may have been insufficient to induce a difference in the performance outcomes.
The relatively good compliance of the control group over the year of follow-up may have been motivated by the knowledge of their participation in a research protocol and the fact they knew they were to undergo follow-up assessments for the study at 6 and 12 months. Another explanation may be that the simplicity of the program (only 4 exercises per day) promoted compliance, facilitating integration of the program into the participants’ lifestyles. In a study involving a more intensive exercise program, only around 20% of participants performed the recommended 3 sessions per week [31].
Lack of a functional decline in both groups
The purpose of the home exercise program was to maintain the effects of the in- or outpatient physiotherapy programs the participants had previously undertaken. Decline in performance is common, both with natural aging and after cessation of an exercise program. Many studies have shown a decline in strength, gait and balance performance in older, non-falling adults after cessation of exercise program [5–8]. Although we did not analyse within-group changes, the changes that occurred in TUG performance time were likely smaller than the minimum clinically important difference (MCID) [32, 33]. The MCID for the TUG test varies from around 1.6s to 15s according to the method used to determine its value and the pathology studied [32–34]. Since performance time did not increase by more than 1.6s in either group, we consider that no decline occurred. Therefore, the lack of decline in both groups after discharge from in- or outpatient physiotherapy suggests that the benefits of the rehabilitation were maintained. This is particularly important since decline after cessation of training occurs more quickly in older-older adults (aged 74–86 years, similar to those in the present study) than in younger-older adults (aged 60–73 years) [7]. Furthermore, the participants in the present study were fallers, unlike those included in other studies of decline [5–8], decline could therefore be expected to be more rapid in the present study, which was not the case.
Other studies have shown improvements with home exercise programs. One example is the Otago exercise program [35]. This program involves a more intensive home exercise program than the one tested here. It includes performing a range of exercises at home at least 3 times per week, supported by therapist home visits and telephone calls. It has been found to improve functional performance, strength and reduction fall risk, although this effect may depend on the sample [31]. In the present study, TUG performance did not improve, however it appears to have been maintained, which was the intended purpose of the program since it was provided after a bout of in- or out-patient rehabilitation. This finding suggests that performing a low-grade exercise program twice per week may be sufficient to maintain performance levels after discharge from a rehabilitation program. This result needs to be confirmed by studies specifically dedicated to this hypothesis.
Strengths and limitations
This study is among the first to evaluate the effectiveness of telephone coaching supporting a home exercise program in older adults who fall. The coaching was provided for 6 months and the follow-up lasted 12 months, providing a long-term assessment of the outcomes.
The main limitations of the study were the relatively large amount of missing data and the fact the planned sample size was not reached. The lack of motivation of some staff in one of the centres resulted in a surprising, large number of consent withdrawals (Fig. 1). This was because the Covid 19 pandemic complicated recruitment. Furthermore, changes in hospital discharge policy occurred during the time of the study, meaning that patients were discharged from hospital at lower functional levels and with a prescription for follow-up outpatient physiotherapy, an exclusion criterion for study participation.
The coaching was provided once per month to ensure the feasibility of the study; however, we believe that once per week coaching would be more appropriate and more effective.
Conclusions
Although the participants in the coaching group performed significantly more exercises than those in the control group during the first 6 months of the study, there was no between-group difference in TUG performance time at 6 months suggesting that monthly telephone coaching sessions did not enhance the effectiveness of a home exercise program in older adults who had sustained at least 1 fall. The exercise program was relatively simple and was performed only 2 to 3 times per week, however TUG performance did not appear to decline in either group over the 12-month follow-up. Future studies should investigate the intensity and content of telephone coaching programs necessary to enhance functional and fall-related outcomes in older adults.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Appendix 1 CONSORT checklist
Supplementary Material 2: Appendix 2 Coaching guide booklet
Acknowledgements
We thank Johanna Robertson, PT, PhD for writing assistance.
Abbreviations
- FTSST
Five Times Sit to Stand Test
- IADL
Instrumental Activities of Daily Living
- IANA
International Academy on Nutrition and Aging
- MCID
Minimum clinically important difference
- TUG
Timed up and go
- VAS
Visual analogue scale
Author contributions
conception or design of the work; GR, JF, CV, CCC. The acquisition, analysis, or interpretation of data; GR, JF, CV, TR•. The creation of new software used in the work; none. Have drafted the work or substantively revised it GR, JF, CV, CCC, TR.
Funding
This study was supported by a grant from the French Ministry of Health (PHRIP, 2015, n° 15–0030).
Data availability
Data relating to this study are available on reasoned request from the paramedical care research coordination unit at Nantes University Hospital: RECHERCHE-PARAMEDICALE@chu-nantes.fr.
Declarations
Ethics approval and consent to participate
The trial was granted ethical approval by the ethics committee “Comité de protection des personnes Ouest IV”, reports to French health ministry, 3rd of May, 2016, ref 22/16 and all participants provided written informed consent for participation. The trial was registered on www.ClinicalTrials.gov (NCT02828826; 11th of july 2016, last modification 16th of September 2024). The study is reported according to the CONSORT guidelines (Appendix 1).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
We have no Conflict of Interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.French health insurance. Fréquence et causes des chutes. 2024. https://www.ameli.fr/assure/sante/themes/chutes-troubles-marche/frequence-et-causes-des-chutes. Accessed 23 Jul 2024.
- 2.Santé Publique France. Les comportements de santé des 55–85 ans. Analyses du Baromètre santé 2010. 2022. https://www.santepubliquefrance.fr/import/les-comportements-de-sante-des-55-85-ans.-analyses-du-barometre-sante-2010. Accessed 23 Jul 2024.
- 3.Haute Autorité de Santé. Évaluation et prise en charge des personnes âgées faisant des chutes répétées. Haute Autorité de Santé. 2009. https://www.has-sante.fr/jcms/c_793371/fr/evaluation-et-prise-en-charge-des-personnes-agees-faisant-des-chutes-repetees. Accessed 23 Jul 2024.
- 4.Montero-Odasso M, van der Velde N, Martin FC, Petrovic M, Tan MP, Ryg J, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. 2022;51:afac205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carvalho MJ, Marques E, Mota J. Training and Detraining effects on Functional Fitness after a Multicomponent Training in Older Women. Gerontology. 2008;55:41–8. [DOI] [PubMed] [Google Scholar]
- 6.Leitão L, Pereira A, Mazini M, Venturini G, Campos Y, Vieira J, et al. Effects of three months of Detraining on the Health Profile of Older Women after a Multicomponent Exercise Program. Int J Environ Res Public Health. 2019;16:3881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toraman NF, Ayceman N. Effects of six weeks of detraining on retention of functional fitness of old people after nine weeks of multicomponent training. Br J Sports Med. 2005;39:565–8. discussion 568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Correa CS, Cunha G, Marques N, Oliveira-Reischak Ã, Pinto R. Effects of strength training, detraining and retraining in muscle strength, hypertrophy and functional tasks in older female adults. Clin Physiol Funct Imaging. 2016;36:306–10. [DOI] [PubMed] [Google Scholar]
- 9.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu-Ambrose T, Davis JC, Best JR, Dian L, Madden K, Cook W, et al. Effect of a home-based Exercise Program on subsequent falls among Community-Dwelling High-Risk older adults after a fall: a Randomized Clinical Trial. JAMA. 2019;321:2092–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mansson L, Lundin-Olsson L, Skelton DA, Janols R, Lindgren H, Rosendahl E, et al. Older adults’ preferences for, adherence to and experiences of two self-management falls prevention home exercise programmes: a comparison between a digital programme and a paper booklet. BMC Geriatr. 2020;20:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aartolahti E, Lönnroos E, Hartikainen S, Häkkinen A. Long-term strength and balance training in prevention of decline in muscle strength and mobility in older adults. Aging Clin Exp Res. 2020;32:59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Desroches S, Lapointe A, Ratté S, Gravel K, Légaré F, Turcotte S. Interventions to enhance adherence to dietary advice for preventing and managing chronic diseases in adults. Cochrane Database Syst Rev. 2013;:CD008722. [DOI] [PMC free article] [PubMed]
- 14.Matkin W, Ordóñez-Mena JM, Hartmann-Boyce J. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2019;5:CD002850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;2006:CD004510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Desai PM, Hughes SL, Peters KE, Mermelstein RJ. Impact of telephone reinforcement and negotiated contracts on behavioral predictors of exercise maintenance in older adults with osteoarthritis. Am J Health Behav. 2014;38:465–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin M-R, Hwang H-F, Hu M-H, Wu H-DI, Wang Y-W, Huang F-C. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc. 2004;52:1343–8. [DOI] [PubMed] [Google Scholar]
- 18.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed Up & Go Test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 19.Word Health Organisation. Chutes. 2021. https://www.who.int/fr/news-room/fact-sheets/detail/falls. Accessed 23 Jul 2024.
- 20.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 21.Buatois S, Miljkovic D, Manckoundia P, Gueguen R, Miget P, Vançon G, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc. 2008;56:1575–7. [DOI] [PubMed] [Google Scholar]
- 22.Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45:735–8. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg A, Schepens S. Measurement error and minimum detectable change in 4-meter gait speed in older adults. Aging Clin Exp Res. 2011;23:406–12. [DOI] [PubMed] [Google Scholar]
- 24.van Abellan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881–9. [DOI] [PubMed] [Google Scholar]
- 25.Peters DM, Fritz SL, Krotish DE. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. 2013;36:24–30. [DOI] [PubMed] [Google Scholar]
- 26.Cesari M, Kritchevsky SB, Penninx BWHJ, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic value of usual gait speed in well-functioning older people–results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–80. [DOI] [PubMed] [Google Scholar]
- 27.Bennell KL, Campbell PK, Egerton T, Metcalf B, Kasza J, Forbes A, et al. Telephone coaching to enhance a home-based physical activity program for knee osteoarthritis: a Randomized Clinical Trial. Arthritis Care Res (Hoboken). 2017;69:84–94. [DOI] [PubMed] [Google Scholar]
- 28.Askim T, Langhammer B, Ihle-Hansen H, Gunnes M, Lydersen S, Indredavik B, et al. Efficacy and safety of Individualized Coaching after Stroke: the LAST study (life after stroke): a pragmatic randomized controlled trial. Stroke. 2018;49:426–32. [DOI] [PubMed] [Google Scholar]
- 29.Hinman RS, Delany CM, Campbell PK, Gale J, Bennell KL. Physical therapists, Telephone coaches, and patients with knee osteoarthritis: qualitative study about working together to promote Exercise Adherence. Phys Ther. 2016;96:479–93. [DOI] [PubMed] [Google Scholar]
- 30.Yan T, Wilber KH, Simmons WJ. Motivating high-risk older adults to exercise: does coaching matter? Home Health Care Serv Q. 2011;30:84–95. [DOI] [PubMed] [Google Scholar]
- 31.Tuvemo Johnson S, Anens E, Johansson A-C, Hellström K. The Otago Exercise Program with or without motivational interviewing for Community-Dwelling older adults: a 12-Month Follow-Up of a Randomized, Controlled Trial. J Appl Gerontol. 2021;40:289–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kool N, Kool J, Bachmann S. Duration of rehabilitation therapy to achieve a minimal clinically important difference in mobility, walking endurance and patient-reported physical health: an observational study. J Rehabil Med. 2023;55:jrm12322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wright AA, Cook CE, Baxter GD, Dockerty JD, Abbott JH. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J Orthop Sports Phys Ther. 2011;41:319–27. [DOI] [PubMed] [Google Scholar]
- 34.Braun T, Thiel C, Schulz R-J, Grüneberg C. Responsiveness and interpretability of commonly used outcome assessments of mobility capacity in older hospital patients with cognitive spectrum disorders. Health Qual Life Outcomes. 2021;19:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang Y, Wang K, Liu H, Qu J, Wang Y, Chen P, et al. The impact of Otago exercise programme on the prevention of falls in older adult: a systematic review. Front Public Health. 2022;10:953593. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Appendix 1 CONSORT checklist
Supplementary Material 2: Appendix 2 Coaching guide booklet
Data Availability Statement
Data relating to this study are available on reasoned request from the paramedical care research coordination unit at Nantes University Hospital: RECHERCHE-PARAMEDICALE@chu-nantes.fr.