Abstract
Objective
This study aimed to investigate the risk factors affecting the presence of carotid plaque in asymptomatic adults.
Methods
Asymptomatic adults (age > 40 years, no symptoms of cardiovascular and cerebrovascular diseases) undergoing routine health examinations from physical examination department were included in this study. Carotid plaque was measured by Resona 7OB and Resona 8EXP color Doppler ultrasound and L9-3U and L4-5WU probes. The focal carotid intima–media thickness was greater than 1.1 mm, and the local protrusion of the artery wall into the artery lumen suggested the presence of carotid atherosclerotic plaque. According to their ultrasound results, 1077 asymptomatic adults were divided into a group with carotid plaque (477) and a group without carotid plaque (600).
Results
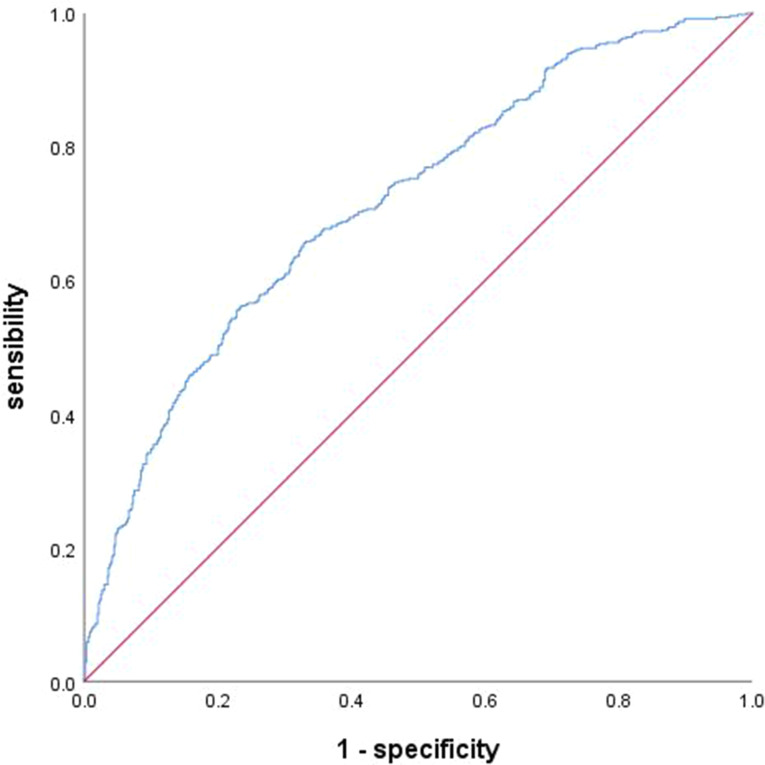
A total of 1077 asymptomatic adults were included in this study, of whom 44.3% had carotid plaque. The proportion of men with carotid plaque was 84.5%. Multifactorial logistic analysis suggested that age, fasting blood glucose (FBG), total cholesterol (TC), homocysteine (Hcy) and male gender were risk factors for carotid atherosclerosis. The predictive probability of these risk factor indicators derived from the multifactorial model was calculated using receiver operating characteristic (ROC) curves with SPSS 25.0 software. The calculated area under the receiver operating characteristic curve (AUC) was 0.715 (95% CI, 0.685–0.746).
Conclusion
Age, FBG, TC, Hcy and male gender are risk factors for carotid atherosclerosis in asymptomatic adults. Gender differences in carotid atherosclerosis deserve further attention.
Keywords: Carotid arteriosclerosis, Asymptomatic adults, Risk factors
Introduction
Ischaemic cardiovascular and cerebrovascular diseases (CCVDs), including coronary heart disease and stroke, rank first in incidence rate and mortality and bring great burden to global health care services [1, 2]. Atherosclerosis is an important pathophysiological process of ischaemic CCVDs. From the formation of atherosclerotic plaque to the occurrence of coronary heart disease, stroke and other clinical events, patients will experience a long-term development process, and clinical symptoms will change according to the shape and characteristics of potential plaque [3]. The incidence of stroke is higher in men than in women [4]. Men had higher-risk plaque features compared with women [5, 6]. The meta-analysis of the global burden of carotid atherosclerosis indicated that the age of onset was concentrated over 40 years old [7]. In the early stage of carotid atherosclerosis, intima–media thickening is the first manifestation, and atherosclerotic plaques then gradually form. On this basis, plaque haemorrhage, plaque rupture and fall off, mural thrombosis and secondary vascular stenosis, cause corresponding haemodynamic changes and lead to CCVDs. Carotid artery ultrasound is a first-line examination method for the screening and preliminary diagnosis of carotid artery diseases. It is also valuable in evaluating the echogenicity and surface characteristics of plaques [8, 9]. Early identification of asymptomatic adults with carotid plaque and active intervention are of great significance in reducing the risk of ischemic CCVDs. However, few studies focused on the early identification and risk factor analysis of carotid plaque in asymptomatic adults. Therefore, the present work aimed to explore the risk factors of carotid plaque in asymptomatic adults to provide information for preventing ischaemic CCVDs.
Data and methods
Research object
This study was approved by the hospital’s ethics committee. Data of 1077 asymptomatic adults(Asian populations) from May 2021 to June 2023 in the Physical Examination Department of Tangshan Gongren Hospital were collected. The inclusion criteria were as follows: (1) asymptomatic adults aged > 40 years with no symptoms of cardiovascular and cerebrovascular disease undergoing routine health examinations and (2) completed carotid ultrasound examination. The exclusion criteria were as follows: (1) malignant tumour; (2) connective tissue diseases; (3) diseases of the blood system (hereditary diseases of the blood system, acquired clonal disease, acquired immune diseases and clinical syndromes of the haematologic system); and (4) autoimmune diseases, osteoporosis, severe liver and kidney damage and mental disorders.
Carotid ultrasound
Carotid ultrasound was performed by an ultrasound specialist. All subjects were placed in a supine position with the lateral neck fully exposed and head tilted to the opposite side. The ultrasound specialist used Resona 7OB and Resona 8EXP color Doppler ultrasound and L9-3U and L4-5WU probes. The common carotid artery and its branches were detected successively, and the intimal thickness of the tube wall was observed. Carotid atherosclerotic plaque was defined as a focal carotid intima–media thickness greater than 1.1 mm with localised protrusion of the arterial wall into the arterial lumen [10].
Data collection
Baseline data included age, gender, systolic blood pressure (SBP), diastolic blood pressure, body mass index, fasting blood glucose (FBG), glycated haemoglobin, triglyceride (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL) and high-density lipoprotein cholesterol (HDL), homocysteine (Hcy), creatinine, urea nitrogen and uric acid. According to the ultrasound results, 1077 asymptomatic adults were divided into a group with carotid plaque (477) and a group without carotid plaque (600).
Statistical analysis
SPSS 25.0 statistical software was used for data analysis. For the comparison of baseline features, normal distribution test was performed firstly. The data did not conform to normal distribution. Continuous variables were represented by median and interquartile intervals, and non-parametric double independent sample tests were performed. X2 test was applied for categorical variables. Univariate analysis was performed firstly, followed by multivariate logistic stepwise regression analysis. With carotid plaque as the gold standard, the receiver operating characteristic (ROC) curve was drawn, the area under the receiver operating characteristic curve (AUC) was calculated and the Hosmer–Lemeshow (H–L) test was used to evaluate the fit degree of the model. All tests are two-sided, and P < 0.05 was considered statistically significant.
Results
Univariate analysis of asymptomatic adults with and without carotid plaque
A total of 1077 asymptomatic adults were included in this study, including 477 with carotid plaque (44.3%) and 600 without carotid plaque (55.7%). Among the 477 asymptomatic adults with carotid plaque, 403 were men (84.5%) and 74 were women (15.5%). Univariate analysis of data between the two groups revealed statistical differences for age, gender, Hcy, SBP and FBG (all P < 0.05) (Table 1).
Table 1.
Univariate analysis of asymptomatic adults with and without carotid plaque
| Risk factors | Asymptomatic adults with carotid plaque (n = 477) |
Asymptomatic adults without carotid plaque (n = 600) |
Z / X2 value | P value |
|---|---|---|---|---|
| Age (year), M(QR) | 57(10) | 52(10) | -10.143 | 0.000* |
| Gender, n(%) | 6.553 | 0.010* | ||
| Male | 403(84.5%) | 470(78.3%) | ||
| Female | 74(15.5%) | 130(21.7%) | ||
| SBP(mmHg), M(QR) | 134(21) | 134(22) | -2.932 | 0.003* |
| DBP(mmHg), M(QR) | 83(15) | 83(15) | -1.112 | 0.266 |
| BMI(Kg/m2), M(QR) | 25.95(4.21) | 25.95(3.58) | -0.495 | 0.621 |
| TG(mmol/L), M(QR) | 1.70(1.30) | 1.73(1.35) | -0.251 | 0.802 |
| TC(mmol/L), M(QR) | 5.25(1.79) | 5.15(1.32) | -0.856 | 0.392 |
| LDL(mmol/L), M(QR) | 3.19(1.26) | 3.12(0.99) | -0.441 | 0.659 |
| HDL(mmol/L), M(QR) | 1.22(0.42) | 1.23(0.44) | -0.428 | 0.669 |
| Hcy(umol/L), M(QR) | 13.30(4.70) | 12.20(3.98) | -5.020 | 0.000* |
| FBG(mmol/L), M(QR) | 5.83(1.80) | 5.43(1.01) | -6.847 | 0.000* |
| GHb(mmol/mol), M(QR) | 5.90(0.80) | 5.80(0.70) | -1.843 | 0.065 |
| Cr(µmol/L), M(QR) | 70.20(18.15) | 69.90(18.63) | -0.023 | 0.981 |
| Bun(µmol/L), M(QR) | 5.34(1.68) | 5.34(1.70) | -0.352 | 0.725 |
| UA(µmol/L), M(QR) | 378.00(130.50) | 380.00(126.00) | -0.159 | 0.874 |
Note *P < 0.05 Continuous variables do not satisfy the normal distribution test and are therefore represented by median and quartile range. M(QR), Median(Quartile Range); SBP: Systolic Blood Pressure; DBP, Diastolic Blood Pressure; BMI, Body Mass Index; TG, Triglycerides; TC, Total Cholesterol; LDL, Low Density Lipoprotein; HDL, High Density Lipoprotein; Hcy, Homocysteine; FBG, Fasting Blood Glucose; GHb, Glycosylated Hemoglobin; Cr, Creatinine; Bun, Blood Urea Nitrogen; UA, Uric Acid
Multivariate logistic regression analysis of carotid plaque in asymptomatic adults
TG, TC, LDL, HDL and variable with P < 0.05 such as age, gender, FBG, Hcy and SBP were included in the multivariate logistic analysis. The results suggested that age, FBG, TC, Hcy and male gender were all risk factors for carotid arteriosclerosis (Table 2).
Table 2.
Multivariate Logistic-analysis of the presence of carotid plaque in asymptomatic adults
| Risk factors | B | SB | Wald | Freedom | P value | OR value | 95% CI of OR value | |
|---|---|---|---|---|---|---|---|---|
| lower limit | upper limit | |||||||
| Age | 0.081 | 0.009 | 83.852 | 1 | 0.000* | 1.084 | 1.065 | 1.103 |
| FBG | 0.179 | 0.042 | 17.971 | 1 | 0.000* | 1.196 | 1.101 | 1.299 |
| TC | 0.142 | 0.057 | 6.179 | 1 | 0.013* | 1.153 | 1.031 | 1.290 |
| Gender | -0.489 | 0.185 | 6.978 | 1 | 0.008* | 0.613 | 0.426 | 0.881 |
| Hcy | 0.034 | 0.011 | 9.488 | 1 | 0.002* | 1.035 | 1.013 | 1.058 |
| Constant | -6.963 | 0.656 | 112.790 | 1 | 0.000 | 0.001 | ||
Note *P < 0.05 FBG, Fasting Blood Glucose; TC, Total Cholesterol; Hcy, Homocysteine; Assigned 0 for male and 1 for female
ROC curve and AUC value for predicting carotid plaque in asymptomatic adults
The prediction probability of the risk factor index for the multifactor model was determined by drawing the ROC curve with SPSS 25.0 software to calculate the AUC and the fitting degree of the prediction model. The AUC was 0.715 (95%CI 0.685–0.746), and the H–L test result was 12.104 (P = 0.147) with P > 0.05, suggesting a good model fit (Table 3; Fig. 1).
Table 3.
AUC value for predicting carotid plaque in asymptomatic adults
| AUC value for predicting carotid plaque | |
|---|---|
| AUC(95%CI) | Hosmer-Lemeshow test(P value) |
| 0.715(0.685–0.746) | 12.104(P = 0.147*) |
Note *P > 0.05
Fig. 1.
ROC curve for predicting carotid plaque in asymptomatic adults. AUC = 0.715
Discussion
Ischaemic CCVDs remain a global problem. The basic pathological change of CCVDs is atherosclerosis. Arterial stenosis caused by large plaques and rupture or bleeding of vulnerable plaques is the main pathological mechanism of atherosclerotic cardiovascular diseases, such as acute coronary syndrome and stroke [11]. Carotid ultrasound is a feasible, non-invasive and accurate method for detecting the early signs of atherosclerosis. Therefore, studying the risk factors of carotid plaque is necessary for the early detection of high-risk population and the development of active intervention measures to reduce the occurrence of ischaemic CCVDs to a certain extent.
Gender difference has a significant effect on the composition and progression of carotid plaque in the high-risk population of cardiovascular diseases and stroke. One study investigated the sex-specific risk factors of carotid intima–media thickness and plaque progression by following up on 7,908 people in a high-risk population of cardiovascular disease for about 2 years and found that carotid plaque intima–media thickness and risk factors for plaque progression differ by gender [12]. Another report found gender differences in carotid plaque composition and morphology in stroke people. Compared with women, men are more likely to have vulnerable components of carotid plaque, which can lead to a higher risk of stroke [13]. A meta-analysis [14] also confirmed that men have a larger carotid plaque size and a more vulnerable plaque composition than women. However, few studies have explored the effect of gender on the risk factors for carotid plaque in asymptomatic adults. Thus, further research is warranted. Our research found that gender difference plays an important role in carotid plaque in asymptomatic adults. Among the 1077 asymptomatic adults in this study, 204 were women and 74 had carotid plaque. Multivariate logistic regression analysis suggested that male gender was a risk factor for carotid arteriosclerosis. However, this finding can be attributed to the single-centre nature of this study and the small number of women attending routine health checkups.
The triglyceride-glucose (TyG) index is closely related to ischaemic CCVDs and can be calculated as ln[triglycerides (mg/dL)×fasting glucose (mg/dL)/2] [15]. An increased TyG index is associated with increased incidence and recurrence of stroke in the Chinese population [16, 17]. Accumulating evidence shows that the TyG index is a valuable predictor of cardiovascular diseases [18, 19] and may be a marker of carotid atherosclerosis [20]. However, our study did not find any correlation between TG and LDL and carotid atherosclerosis. This difference may be related to the single-centre nature of this research and the fact that asymptomatic adults who participated in routine medical examinations did not provide information on whether they received lipid-lowering therapy.
Elevated total Hcy levels are closely related to carotid atherosclerosis [21–23] and independently associated with increased plaque morphology and plaque area [24]. In an observational cohort study of 2919 Chinese participants, the risk for advanced carotid plaque increased with the Hcy levels (OR = 1.280). When stratified by gender, high Hcy levels in men were found to be significantly associated with advanced carotid plaque (OR = 1.410) [25]. In the present study, Hcy was also identified as an important risk factor for carotid plaque.
This study provides additional information for the prevention of ischaemic CCVDs in asymptomatic adults. However, it has some limitations. Firstly, the study participants were selected from asymptomatic adults admitted to a single centre, which may have contributed to selection bias. Secondly, only a few women participated in routine health checkups in the study population. In future studies, attention should be paid to the influence of gender.
Conclusion
Age, FBG, TC, Hcy and male gender were all risk factors for carotid arteriosclerosis. Gender differences in carotid atherosclerosis deserve further attention.
Acknowledgements
Not applicable.
Author contributions
CLL conceived and designed the study and helped to draft the manuscript. SGY and FYN were co-first authors and helped to write the manuscript. FM, WJH, CFF, CY, and LYD, ZBB performed the data collection and analyzed the data. All authors approved the final manuscript.
Funding
Not applicable.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to the privacy of the research subjects, but can be obtained from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Tangshan Gongren Hospital. Ethics number: [2023] Ethical Review Study No. (97). Ethics Committee Review Opinions: After review by the ethics committee, it was agreed to conduct the study. This study is a retrospective study. We retrospectively collected study subjects’ laboratory indicators such as blood glucose, blood lipids and carotid vascular ultrasound results.This study did not involve clinical trial research and there was no risk to the subjects. There is no written informed consent.
Clinical trial number
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guoyan Shi and Yani Fan Co-first author.
References
- 1.Benjamin EJ, Virani SS, Callaway CW, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 update: a Report from the American Heart Association. Circulation. 2018;137(12):e67–492. [DOI] [PubMed] [Google Scholar]
- 2.Jankovic N, Geelen A, Streppel MT, et al. WHO guidelines for a healthy diet and mortality from cardiovascular disease in European and American elderly: the CHANCES project. Am J Clin Nutr. 2015;102(4):745–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Relationship of atherosclerosis. In young men to serum lipoprotein cholesterol concentrations and smoking. A preliminary report from the Pathobiological determinants of atherosclerosis in Youth (PDAY) Research Group. JAMA. 1990;264(23):3018–24. [DOI] [PubMed] [Google Scholar]
- 4.Peters SAE, Carcel C, Millett ERC, et al. Sex differences in the association between major risk factors and the risk of stroke in the UK Biobank cohort study. Neurology. 2020;95(20):e2715–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ota H, Reeves MJ, Zhu DC, et al. Sex differences in patients with asymptomatic carotid atherosclerotic plaque: in vivo 3.0-T magnetic resonance study. Stroke. 2010;41(8):1630–5. [DOI] [PubMed] [Google Scholar]
- 6.Wentzel JJ, Bos D, White SJ, et al. Sex-related differences in coronary and carotid vessel geometry, plaque composition and shear stress obtained from imaging. Atherosclerosis. 2024;395:117616. [DOI] [PubMed] [Google Scholar]
- 7.Song P, Fang Z, Wang H, et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Glob Health. 2020;8(5):e721–9. [DOI] [PubMed] [Google Scholar]
- 8.Eckstein HH, Kühnl A, Dörfler A, et al. The diagnosis, treatment and follow-up of extracranial carotid stenosis. Dtsch Arztebl Int. 2013;110(27–28):468–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muraki M, Mikami T, Yoshimoto T, et al. New criteria for the sonographic diagnosis of a plaque ulcer in the extracranial carotid artery. AJR Am J Roentgenol. 2012;198(5):1161–6. [DOI] [PubMed] [Google Scholar]
- 10.Handa N, Matsumoto M, Maeda H, et al. Ultrasonic evaluation of early carotid atherosclerosis. Stroke. 1990;21:1567–72. [DOI] [PubMed] [Google Scholar]
- 11.Stary HC, Chandler AB, Dinsmore RE, et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis. Circulation. 1995;92:1355–74. [DOI] [PubMed] [Google Scholar]
- 12.Cheng Q, Zhou D, Wang J, et al. Sex-specific risk factors of carotid atherosclerosis progression in a high-risk population of cardiovascular disease. Clin Cardiol. 2023;46(1):22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Dam-Nolen DHK, van Egmond NCM, Dilba K, Nies K, et al. Sex differences in Plaque composition and morphology among symptomatic patients with mild-to-moderate carotid artery Stenosis. Stroke. 2022;53(2):370–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Dam-Nolen DHK, van Egmond NCM, Koudstaal PJ, et al. Sex differences in carotid atherosclerosis: a systematic review and Meta-Analysis. Stroke. 2023;54(2):315–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma X, Dong L, Shao Q, et al. Triglyceride glucose index for predicting cardiovascular outcomes after percutaneous coronary intervention in patients with type 2 diabetes mellitus and acute coronary syndrome. Cardiovasc Diabetol. 2020;19(1):31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao Y, Sun H, Zhang W, et al. Elevated triglyceride-glucose index predicts risk of incident ischaemic stroke: the rural Chinese cohort study. Diabetes Metab. 2021;47(4):101246–52. [DOI] [PubMed] [Google Scholar]
- 17.Wang A, Wang G, Liu Q, et al. Triglyceride-glucose index and the risk of stroke and its subtypes in the general population: an 11-year follow-up. Cardiovasc Diabetol. 2021;20(1):46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang L, Cong HL, Zhang JX, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. 2020;19(1):80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong S, Han K, Park CY. The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study. BMC Med. 2020;18(1):361–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miao M, Zhou G, Bao A, et al. Triglyceride-glucose index and common carotid artery intima-media thickness in patients with ischemic stroke. Cardiovasc Diabetol. 2022;21(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nukata M, Taguchi A, Kitagawa K, et al. Association of plasma homocysteine concentration with atherosclerotic carotid plaques and Lacunar Infarction. Stroke. 2002;33:1493–6. [DOI] [PubMed] [Google Scholar]
- 22.Dietrich M, Jacques PF, Polak JF, et al. Segment-specific association between plasma homocysteine level and carotid artery intima-media thickness in the Framingham offspring Study. J Stroke Cerebrovasc Dis. 2011;20:155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adachi H, Hirai Y, Fujiura Y, Matsuoka H, Satoh A, Imaizumi T. Plasma homocysteine levels and atherosclerosis in Japan: epidemiological study by use of carotid ultrasonography. Stroke. 2002;33:2177–81. [DOI] [PubMed] [Google Scholar]
- 24.Alsulaimani S, Gardener H, Elkind MS, et al. Elevated homocysteine and carotid plaque area and densitometry in the Northern Manhattan Study. Stroke. 2013;44(2):457–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang X, Zhou Y, Liu C, et al. Homocysteine and carotid plaque stability: a cross-sectional study in Chinese adults. PLoS ONE. 2014;9(4):e94935. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available due to the privacy of the research subjects, but can be obtained from the corresponding author upon reasonable request.