Abstract
With medical technology development, endovascular intervention has been widely used in clinical practice, and the establishment of surgical access through the femoral artery, where most vascular interventions are performed, is a common method. Postoperative hemostasis at the femoral artery puncture site is a key part of interventional procedures and is particularly important to ensure the safety and effectiveness of hemostasis. Some patients undergoing interventional therapy also use anticoagulant and antiplatelet drugs preoperatively and undergo systemic heparin session intraoperatively, which leads to abnormal coagulation, thus increasing the difficulty of hemostasis at the puncture point postoperatively. Certain patients with specific conditions, such as combined vascular calcification, obesity, diabetes mellitus, and renal impairment, present more challenging cases for postoperative puncture point hemostasis. Femoral artery puncture site hemostasis methods include manual compression, arterial compression devices, and vascular closure devices, which are a kind of equipment that helps interventional doctors stop bleeding quickly at the femoral artery puncture site. From the 1990s to the present, vascular occluders with many different concepts and mechanisms have emerged. Based on different hemostatic principles and materials, the mechanisms and principles of action are varied and include sealant occlusion, collagen patch embolization, polyester suture closure, absorbable polyethanol embolic agents, nickel-titanium alloy clips, polydiethanol sealant embolization, and suture bioabsorbable patches. Many studies have compared the hemostatic effect of vascular closure devices with those of manual compression. In this article, we review the hemostatic effects of the 2 modalities and the advances in the use of vascular closure devices in vascular intervention.
Keywords: Femoral Artery; Postoperative Complications; Radiography; Radiography, Interventional; Vascular Closure Devices
Introduction
With the development of medical technology, endovascular interventions are widely used in clinics due to their minimally invasive nature and safety [1]. According to statistics, more than 7 million interventional procedures are completed annually worldwide [2,3], and the number and complexity of their applications are increasing yearly. Currently, endovascular interventions include invasive cardiac examinations, interventional procedures for cardiovascular diseases, peripheral vascular interventions, and neurointerventional procedures [4–8]. Intraoperative puncture approaches are often used, including the radial artery approach and femoral artery approach [2]. The radial artery approach is mostly used in diagnostic and interventional cardiology and a small number of cerebral vascular interventional therapies to reduce the patient’s postoperative adverse reactions and discomfort to a certain extent. However, due to the anatomical conditions of the limitations, or the need to retain the radial artery for coronary artery bypass grafting surgery, the radial artery needs to be protected, and puncture cannot be arbitrarily used [9]. The femoral artery approach is more widely used in interventional procedures, including cardiac, neurological, oncological, and peripheral vascular procedures [2,9–12]. Postoperative hemostasis of the puncture site is an important part of interventional procedures, and effective and safe hemostatic techniques are essential to minimize patient discomfort and complications in the postoperative period [13]. When patients receive vascular interventional therapy, more discomfort occurs during long-term bed rest after surgery [14]. Some patients undergoing interventional therapy also use anticoagulant and antiplatelet drugs preoperatively and undergo systemic heparin session intraoperatively, which leads to abnormal coagulation, thus increasing the difficulty of hemostasis at the puncture point postoperatively [3,15]. Certain patients with specific problems, such as combined vascular calcification, obesity, diabetes mellitus, and renal impairment, present more challenging cases for postoperative puncture point hemostasis [7,16]. Therefore, a hemostatic method with a low complication rate, high comfort, high success rate of hemostasis, proven operating technique, and ease of postoperative care is essential.
The Seldinger percutaneous arterial puncture technique was first proposed by interventional radiologist Sven Ivar Seldinger in 1953 [3]. In 1974, Driscol improved the technique, which was called the modified Seldinger technique [17]. This technique is the most commonly used method to establish access for percutaneous vascular interventions, where the anterior or anterior-posterior wall of the vessel is first penetrated with a puncture needle with a cannula, and then the core is withdrawn; if the posterior wall is penetrated, the cannula is required to be slowly retreated into the lumen of the vessel until there is a jet of blood. Then, the guidewire is inserted into the vessel via the cannula, which is withdrawn and exchanged for insertion of the vascular sheath. This technique is now widely used for the puncture of various types of blood vessels, including peripherally inserted central catheters and implantable venous access ports, in addition to vascular interventional procedures [18,19]. The confirmation of the puncture site can be performed by human anatomical landmarks, fluoroscopic guidance, or ultrasound guidance. Studies have shown that ultrasound-guided femoral artery puncture has a high success rate and significantly reduces the number of repeated punctures, the risk of mispuncturing the vein, puncture time, and the risk of vascular complications [20]. The femoral artery is characterized by its superficial anatomical location and large diameter, which allows it to pass retrogradely through the iliac arteries to reach the aorta directly, and to easily reach the blood vessels of various organs and the lower limbs [17]. The femoral artery is the most commonly used access route for vascular interventions, including cardiac interventional procedures, neurological interventions, oncological interventions, and peripheral vascular interventions [2,9–12]. Compared with the radial artery, the femoral artery has a minimal possibility of anatomical variability, allowing for the creation of larger caliber accesses with a lower risk of thrombus dislodgement into the intracranial vasculature, but a more complex hemostatic approach with a higher risk of hemorrhage, retroperitoneal hematoma, and pseudoaneurysm [20].
Currently, the commonly used hemostatic methods for femoral artery puncture points include manual compression, arterial compression devices, and vascular closure devices [5,16,21–24]. In comparison, manual compression takes longer, the operator’s workload increases, and the patient’s postoperative discomfort, time to ambulation, and complication rates increase [1,3,21,23]. The use of manual compression increases operator workload, compared with vascular closure devices, and patients are also bedridden for longer periods of time, which can lead to lower limb ischemia and vasovagal reflexes [10]. Compared with manual compression, the use of vascular closures can shorten the hemostasis time and the patient’s time to ambulation, improve patient comfort, and reduce the incidence of complications at the puncture site [2,8]. The use of vascular closures can also reduce the workload of the operator [14]. Vascular closure devices first appeared in the mid-1990s and are a common modality used in vascular puncture point closure [24]. This class of devices was designed with the aim of helping interventionalists to quickly perform vascular puncture point closure and hemostasis after the procedure [21]. The mechanisms and principles of action are varied and include sealant occlusion, collagen patch embolization, polyester suture closure, absorbable polyethanol embolic agents, nickel-titanium alloy clips, polydiethanol sealant embolization, and suture bioabsorbable patches [3,16,23]. With the development of interventional radiology, the new instruments and techniques used in interventional therapy have also undergone radical changes. From the 1990s to the present, vascular closure devices have emerged with many different concepts and different mechanisms of action, after close to 30 years of development. Based on different hemostatic principles and materials, they are categorized into 5 main groups: suture-mediated closure devices, mechanical non-suture closure devices, intra-vascular sealant devices, extra-vascular sealant devices, and manual compression assistance devices [25]. Table 1 lists all the types of vascular closure devices.
Table 1.
Vascular closure devices list.
| Device type | Device name | Manufacturer | Materials | Puncture size, F |
|---|---|---|---|---|
| Intra-vascular sealant devices | Angio-Seal | St. Jude Medical (USA) | Absorbable bovine collagen bolus | 6F-8F |
| FemoSeal | St. Jude Medical (USA) | Absorbable biopolymer disk | 5F-7F | |
| Extra-vascular sealant devices | MynxGrip | Access Closurre (USA) | Polyethene glycol | 5F-7F |
| Exoseal | Cordis (USA) | Polyglycolic acid | 5F-7F | |
| Manual compression assistance device | Vascade | Cardiva Medical (USA) | Absorbable collagen plug | 5F-7F |
| Mechanical non-suture closure devices | Celt | Vasorum Limited (Ireland) | Biocompatible metal stainless steel wing | 5F-7F |
| StarClose | Abbott (USA) | Nickel-titanium alloy clip | 5F-8F | |
| Suture-mediated closure device | Perclose ProGlide | Abbott (USA) | Polypropylene thread | 5F-8F |
Systematic evaluations of the safety and efficacy of vascular closures were reported as early as 2004, but have changed dramatically over these 2 decades [14]. A comparison of the safety and effectiveness of manual compression and vascular closure use was analyzed in a systematic evaluation in 2022, but the authors selected only data on use in cardiac interventional procedures [14]. In the present article, we aim to review the hemostatic effects of the 2 modalities and the advances in the use of vascular closure devices in vascular intervention.
Application Principle and Research Progress of the Angio-Seal Vascular Closure Device
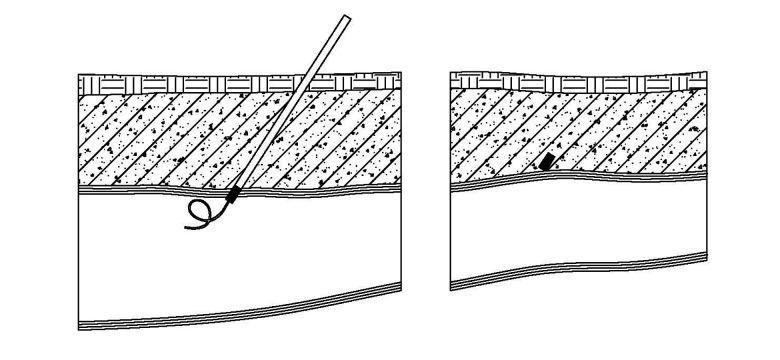
The primary mechanism of action of the Angio-Seal vascular closure device (Figure 1) is embolic sealing of the femoral artery puncture site using an absorbable bovine collagen bolus, which can be used for access portals created by 6F and 8F vascular sheaths [26,27]. The embolization system first opens a rectangular anchor in the lumen of the vessel to determine the location of the puncture port, and the anchor is connected to the embolus by a thin wire. When the thin wire is pulled back, the anchor and the embolus are deployed tightly against the inside and outside of the vessel wall, respectively, to form a sandwich shape. The embolus undergoes a coagulation reaction when it comes into contact with the blood and surrounding tissues, and it acts as an embolization hemostasis for the puncture site.
Figure 1.

Angio-Seal vascular closure device. The rectangular anchor is deployed in the vascular lumen. Embolus is deployed close to the outer wall of blood vessels. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
In a study by Wong HF et al [28], 153 patients who underwent neurointerventional therapy were reported, all of whom had prolonged activated clotting time values after systemic heparinization, and 104 patients were occluded with Angio-Seal, and 70 patients with manual compression. The results of the study showed that the hemostasis time was shorter in the vascular occluded group, and hematomas in the vascular occluded group incidence was lower (1% in the vascular closure group and 20% in the manual compression group). In patients who underwent significantly prolonged activated clotting time with systemic heparinization, closure with the Angio-Seal resulted in a somewhat lower incidence of inguinal hematoma and rapid and effective hemostasis, relative to manual compression. In a retrospective cohort study by Emced [29], 81 patients who underwent peripheral interventions were included, of which 41 in the manual compression group and 40 in the vascular closure device group underwent hemostasis using Angio-Seal. It was found that hemostasis time in the vascular closure device group was significantly faster than that of the manual compression group, and time between removal of the sheath and standing or walking 20 feet without bleeding was significantly faster in the vascular closure device group than in the manual compression group. Also, there were no major complications in the vascular closure device group, whereas there were 5 major complications in the manual compression group (6.2%), including arteriovenous fistula, retroperitoneal hemorrhage, hematoma >6 cm in diameter, and lower extremity arterial embolism, and 2 of these patients also underwent intravenous transfusion therapy. Therefore, the use of Angio-Seal for hemostasis in peripheral interventions is safe and can shorten hemostasis time, hospitalization time, and time to ambulation, and has significant advantages in reducing serious complications. Kim et al [2] published a retrospective study of 2072 patients, of which 818 patients who underwent interventional diagnosis and treatment had Angio-Seal for femoral artery hemostasis. The results of this study showed that Angio-Seal had a higher deployment success rate than did the vascular closure device called Perclose. Elmasri et al [30] compared the safety and efficacy of 5 vascular closure systems vs that of manual compression in percutaneous arterial interventions. A total of 907 procedures were included in the study, and the 5 vascular closure devices included the Angio-Seal vascular closure device, FISH (femoral introducer sheath and hemostasis) vascular closure device, Mynx vascular closure device, Perclose vascular closure device, and StarClose vascular closure device. The results of the study showed that Angio-Seal had the highest hemostatic success rate. There was no statistically significant difference in complications between the groups.
Application Principle and Research Progress of MynxGrip Vascular Closure Device
The primary mechanism of action of the MynxGrip vascular closure device (Figure 2) is embolic sealing of the femoral artery puncture site using a polyethene glycol sealant, which can be used for access portals established by 5F to 7F vascular sheaths [26,27]. The embolization system first fills a semi-compliant balloon in the lumen of the vessel to determine the location of the puncture site, then deploys the sealant on the outer wall of the vessel at the puncture site according to the anchored position. The balloon is retrieved and removed after deployment is completed. The sealant rapidly expands upon contact with surrounding blood and body fluids to achieve hemostasis of the puncture. MynxGrip can be used for arterial and venous hemostasis.
Figure 2.
MynxGrip vascular closure device. A semi-compliant balloon is deployed in blood vessels. The sealant is deployed on the outer wall of blood vessels. The balloon is retrieved and removed after deployment is completed. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
In a randomized controlled study by Jakobsen et al [23] comparing the safety and efficacy of using MynxGrip hemostasis and manual compression hemostasis at femoral artery puncture sites during coronary angiography, there was no statistically significant difference between the 2 groups in the incidence of major adverse vascular events at 30 days. The median time to hemostasis in the vascular closure device group was significantly less than that of the manual compression group, and 7% of the patients in the vascular closure device group were converted to manual compression hemostasis because of hemostatic failure. Song et al [31] included 304 patients undergoing interventional diagnosis or treatment via femoral artery access who were randomly assigned to the MynxGrip group and the manual compression group. It was found that the use of the MynxGrip closure significantly reduced hemostasis time and patient time to ambulation, but did not provide any significant advantage over manual compression in terms of reducing complication rates. Moreover, in the report of Resnic et al [32] on the safety study of MynxGrip, it was shown that the risk of vascular complications, risk of bleeding at the puncture site, and risk of needing transfusion therapy were significantly increased with MynxGrip, compared with other types of vascular closure devices, with patients with diabetes, women, and elderly patients being at greater risk.
The MynxControl is the next generation of the MynxGrip, which is technically easier to control and operate and which received Conformité Européenne marking in 2019 [33]. Noory et al [34] reported a study comparing the safety and efficacy of 2 vascular closure systems, the MynxControl vascular closure device and the FemoSeal vascular closure device, for hemostasis at femoral artery puncture sites. There was a significant difference in the rate of hemostatic failure between the 2 groups, which was higher in the MynxControl group (7.7%) than in the FemoSeal group (4.0%), and the incidence of pseudoaneurysms was also higher in the MynxControl group (6.6%) than in the FemoSeal group (2.2%). One case of femoral artery puncture site stenosis requiring only conservative treatment occurred in the MynxControl group. Risk factors for puncture site closure failure in both groups were related to the use of anticoagulants or antiplatelet agents. In a prospective study, Diamantopoulos et al [33] reported the results of the MynxControl vascular closure device in peripheral arterial interventions. A total of 91 patients were included in the study, including 62 (62%) antegrade punctures of the femoral artery and 38 (38%) retrograde punctures of the femoral artery, with 5F vascular sheaths in 43 (43%) patients, 6F vascular sheaths in 36 (36%), and 7F vascular sheaths in 21 (21%). Four minor complications occurred, including pseudoaneurysms and hematomas. No major complications were noted in the postoperative and 30-day follow-up data. The study demonstrates the safe and effective use of this vascular closure in peripheral vascular arterial interventions.
Application Principle and Research Progress of Exoseal Vascular Closure Device
The embolization principle of the Exoseal vascular closure device (Figure 3) is similar to that of the MynxGrip in that an absorbable sealant consisting of polyglycolic acid is deployed on the outer wall of the vessel at the puncture site, which absorbs blood and tissue fluids to rapidly expand and seal the puncture site. It is suitable for puncture sites created by vascular sheaths ranging from 5F to 7F [26,27]. The sealant is guided into position by means of a nitinol guidewire. The sealant does not bond immediately to the vessel wall, and manual compression is still required for 4 min after device deployment until hemostasis is complete.
Figure 3.
Exoseal vascular closure device. The sealant is guided into position by means of a nitinol guidewire. After the deployment is completed, the guidewire needs to be evacuated. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
Pieper et al [35] reported a prospective study aimed at comparing the level of patient discomfort and satisfaction after femoral artery puncture site hemostasis using the Exoseal vascular closure device and manual compression. They analyzed data from a total of 44 samples. The study showed that vascular closure with the Exoseal was enough to reduce time to ambulation, decrease the pain level, and increase the comfort level, which in turn increased patient satisfaction. A study by Wong et al [36] compared the effectiveness of the Exoseal with that of manual compression for coronary or peripheral arterial interventions, and between the 2 groups, the mean time to hemostasis and mean time to ambulation were significantly lower in the vascular closure device group than in the manual compression group. Complication rates were low in both groups, with no serious femoral arterial complications in the 30-day follow-up results. The safety and efficacy of the vascular closure device and manual compression for hemostasis at the brachial artery puncture site were compared in a study by Wei et al [37]. The results of the study showed that brachial artery closure hemostasis with the vascular closure device had a significantly lower time to hemostasis in patients receiving adequate anticoagulation therapy, and manual compression was safer and more convenient, although it had a high rate of minor complications.
Application Principle and Research Progress of the FemoSeal Vascular Closure Device
The FemoSeal vascular closure device (Figure 4) consists of 2 absorbable biopolymer disks, one acting as an anchor in position within the lumen of the vessel and the other affixed to the outer wall of the vessel. The 2 bio-disks are connected by an absorbable wire to form a sandwich with the vessel wall at the site of the puncture, to achieve hemostasis [38]. Schulz-Schüpke et al [39] compared the efficacy of using FemoSeal and manual compression for hemostasis at femoral artery puncture sites during diagnostic coronary angiography. Two types of vascular closure devices were used in the study, FemoSeal and Exoseal. Hemostasis time was observed to be significantly greater in the manual compression group than in the vascular closure device group. The comparison of 2 vascular closure devices showed that the hemostasis time in the FemoSeal group was faster than that in the Exoseal group. The device failure rate was significantly lower in the FemoSeal group than in the Exoseal group. Gewalt et al [40] compared the effects of FemoSeal, Exoseal, and manual compression. Consistent with the findings of Schulz-Schüpke et al, hemostasis time was shorter in the vascular closure device groups than in the manual compression group. Compared with the Exoseal group, the FemoSeal group had more significant advantages in terms of complication rate, device failure rate, and shorter hemostasis time. The probability of closure failure to change manual compression was higher in the Exoseal group, and the sandwich closure technique was safer and more effective in the FemoSeal group. The risk of puncture site complications was found to be higher in women than in men in the study, probably related to the smaller diameter and length of the femoral artery in women, older age of onset in women, and greater sensitivity of women to anticoagulant dosage, inflammatory components, and mechanical injury. However, the sex factor is not a specific influence on the effectiveness of the vascular closure device and manual compression, and the use of the vascular closure device in women is also safe. The results of a study by Mankerious et al [38] on femoral artery puncture site closure during cardiac catheterization interventions showed that the use of the FemoSeal decreased the incidence of hematoma at the entrance site, in addition to shortening the time to hemostasis. Gabrielli et al [41] retrospectively analyzed the use of the FemoSeal in 114 patients undergoing peripheral arterial interventions. The sample in the study had femoral arterial access established using a vascular sheath ranging from 6F to 8F, and all of the patients were treated with antiplatelet therapy and systemic heparinization. Critical limb ischemia was found to be a predictor of the development of vascular closure device complications in this study.
Figure 4.

FemoSeal vascular closure device. Two absorbable biopolymer disks are deployed: one inside and one outside the blood vessel wall. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
Application Principle and Research Progress of Vascade Vascular Closure Device
The embolization principle of the Vascade vascular closure device (Figure 5) is to deploy an absorbable collagen plug in the outer wall of the vessel to seal the puncture opening. The device is indicated for femoral arterial access established by 5F to 7F vascular sheaths [26,27]. The operator uses the original vascular sheath to place the Vascade and deploys a nickel-titanium alloy disk on the inner wall of the vessel to determine the location of the puncture opening and temporarily seal the puncture opening. The operator then retracts the metal disk after releasing the collagen plug on the outer wall of the vessel to stop bleeding, and manual compression is still required for 4 min after device deployment until hemostasis is complete. The Vascade leaves no material in the lumen of the vessel and does not interfere with secondary puncture of the site.
Figure 5.
Vascade vascular closure device. Deploys a nickel-titanium alloy disk on the inner wall of the vessel to determine the location of the puncture opening, temporarily seals the puncture opening, and retracts the metal disk after releasing the collagen plug on the outer wall of the vessel to stop bleeding. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
In a study by Kulangara et al [42], the differences between the Vascade and manual compression in percutaneous endovascular interventions were compared. The study included 522 interventional treatments for 396 patients with complications including hypertension and diabetes. There was a significant difference in complication rates between the 2 groups, with complications in the Vascade group being significantly lower than those in the manual compression group. Serious complications, such as acute arterial ischemia of the lower extremity on the puncture side, were also observed in the manual compression group. In a single-center retrospective study by Nagpal et al [43] the efficacy and safety of the Vascade and manual compression were compared for use in patients with moderate stenosis of the femoral artery. Two hundred patients were included in the study, of which 2.5% had an antrograde puncture of the femoral artery and 97.5% had a retrograde puncture of the femoral artery; there were 103 patients in the vascular closure device group and 97 patients in the manual compression group. The study collected outcome metrics at 48 h and 30 days after the procedure. There was a difference in mean activated clotting time between the 2 groups, which was significantly shorter in the vascular closure device group (198 s) than in the manual compression group (213 s), P=0.019. Increasing the frequency of use of the external compression device was not different between the 2 groups (19% vs 28.1%, P=0.15).There was no statistically significant difference in the incidence of retroperitoneal hemorrhage and pseudoaneurysm, or in the incidence of hematoma after 30 days between the 2 groups. One patient in both groups received blood transfusion within 30 days; the incidence of thrombus in the lower limb on the side of the puncture was 1% in both groups; 1 case of limb ischemia was found in the manual compression group, and 1 case of aortic dissection was found in the vascular closure device group. Clinical use of vascular closure devices for patients with femoral artery disease is generally done cautiously because of the increased risk of vascular complications. The results of this study suggest that the fluoroscopically guided use of this vascular closure system is also safe and effective when dealing with high-risk patients, provided that the technician is skilled and experienced.
Application Principle and Research Progress of Celt Vascular Closure Device
The principle of the Celt vascular closure device (Figure 6) is to deploy a biocompatible metal stainless steel wing on the inside and outside of the vessel wall at the puncture site, forming a sandwich with the vessel wall to achieve hemostasis. The system is suitable for vascular access established by 5F to 7F vascular sheaths [16,44].
Figure 6.
Celt vascular closure device. Deploys a biocompatible metal stainless steel wing on the inside and outside of the vessel wall at the puncture site. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
Wong SC et al [45] compared the safety and efficacy of the Celt vascular closure device and manual compression for hemostasis at the femoral artery puncture site in 181 patients undergoing percutaneous coronary intervention, all of whom received anticoagulation. The results of the study showed that the median time to hemostasis was significantly shorter in the vascular closure device group than in the manual compression group. There was no difference in the rate of major complications within 30 days between the 2 groups. In 1 case, the embolic wing was dislodged due to inaccurate positioning of the femoral artery puncture site, and was successfully removed by percutaneous endovascular intervention without sequelae. Among the minor complications observed within 30 days, the incidence of hematoma with a diameter of >6 cm was 1 in the vascular closure device group and 3 in the manual compression group. Three patients in the vascular closure device group bled from the puncture site, and the time required to re-establish hemostasis was >30 min. The secondary complication rate was lower in the vascular closure device group (4.1%) than in the manual compression group (6.8%). At 30-day ultrasound follow-up, the difference of femoral artery diameter before and after surgery in the vascular closure device group was 1.2 mm, and that in the manual compression group was 0.5 mm. The peak systolic femoral artery decreased by 10 cm/s in the vascular closure device group and 6.3 cm/s in the manual compression group, which was not statistically significant between the 2 groups (P=0.86). In the previous study by Wong SC et al, there was a mention of dislodgment of embolic wings in the Celt vascular closure system. Two similar cases were reported by Hart and Hans, in which dislodgement of the embolic wing of the Celt vascular closure device into the lumen of the vessel was reported as a specific complication of this system, which increased the risk of complications at the puncture site and the length of hospitalization of the patient [44].
Application Principle and Research Progress of StarClose Vascular Closure Device
The StarClose vascular closure device (Figure 7) principle involves hemostasis by clamping a puncture in the outer wall of the vessel with a nickel-titanium alloy clip [26]. The StarClose requires the use of a system-specific working sheath to deliver a release device into the vessel, which is released by a positioner that releases the nickel-titanium alloy clip. This type of closure is suitable for vascular access established by a 5F to 8F vascular sheath. The clips do not damage the intima but do carry the risk of causing stenosis of the femoral artery.
Figure 7.
StarClose vascular closure device. The exclusive positioner determines the location of the blood vessel puncture site. A nickel-titanium alloy clip is deployed on the outer wall of the blood vessels. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
A study by Iqtidar et al [46] compared the effect of the use of StarClose and manual compression during percutaneous coronary intervention on vascularity and complication rates. The study included 8615 patients who underwent percutaneous coronary intervention using vascular closure devices, including the Perclose Proglide vascular closure device, Angio-Seal vascular closure device, and StarClose vascular closure device. The results of the study showed that the incidence of hematomas >10 cm in diameter was lower in the vascular closure device group than in the manual compression group (1.1% vs 2.1%, P<0.01), but the length of hospitalization did not differ significantly between the 2 groups. When compared within the group of vascular closure devices, the StarClose had the most vascular- and bleeding-related complications (Perclose 5.6%, Angio-Seal 9.0%, StarClose 10.2%, P<0.0001), but there was no difference in the length of hospitalization among the 3 groups. The advantages of the vascular closure device in terms of time to hemostasis, patient time to ambulation, and time in bed were reported in a study of the StarClose vs femoral artery compression hemostats [47]. Two other studies comparing the StarClose with the Angio-Seal demonstrated comparable safety and efficacy in femoral artery puncture site hemostasis [48,49]. In a study on the incidence and risk factors of puncture site pseudoaneurysms in peripheral interventions, it was found that the interventional doctors preferred manual compression for hemostasis when there was calcification at the puncture site. However, there was variability in the incidence of pseudoaneurysms between the 2 groups, with that in the vascular closure device group being lower than that in the manual compression group [50]. In this study, the interventional doctors used the Perclose ProGlide, FemoSeal, StarClose, and Mynx according to the patient’s condition and personal preference, and no pseudoaneurysms were found in the StarClose group. The investigators concluded that the use of vascular closure device can reduce the incidence of pseudoaneurysms when calcification occurs at the femoral artery puncture site.
Application Principle and Research Progress of Perclose Proglide Vascular Closure Device
The Perclose Proglide (Figure 8) is a suture-mediated vascular closure device based on a core component of 1 polypropylene thread that can be sutured to the vessel. It is typically used for femoral artery access established by 5F to 8F vascular sheaths, and can be used to suture vascular sheath puncture openings up to 21F when 2 suture devices are used for the pre-positioning suture technique [26,27,51]. The operator uses a guidewire to exchange the suture device with the vascular sheath in situ, placing it to a depth that is as deep as the bleeding from the marked hole on the suture device, and then suturing the vascular wall puncture site to achieve hemostasis by operating the wrench and needle system on the suture device, which is a more complex procedure, with a strong stretching force of polypropylene thread, and an accurate suture; however, there is a risk of stenosis of the femoral artery after the suture is applied.
Figure 8.

Perclose Proglide vascular closure device. Operates the wrench and sewing needle system on the vascular closure device and sews the vascular puncture site with 1 polypropylene thread. (Software name: AutoCAD; Version: 2022 edition; Manufacturer: Autodesk).
The PETRONIO registry [52], an observational study on the introduction of ultrasound guidance and vascular closure device in percutaneous transfemoral puncture cardiac interventions, found that the use of ultrasound-guided puncture of the femoral artery and vascular closure device in a number of procedures requiring large-bore puncture sheaths reduces the risk of complications at the puncture site. Increased operator experience and knowledge over time are equally important in reducing complications. Ultrasound guidance improves puncture accuracy under visualization conditions, reduces the number of successful attempts at femoral artery puncture, decreases puncture time, and reduces the risk of the risk of wrong venipuncture and complications. Sekhar et al [51] conducted a prospective, single-center study aimed at comparing the use of the Perclose Proglide with manual compression in cardiac interventions for femoral artery puncture site hemostasis in terms of early (within 30 min) efficacy and economic benefits. The vascular closure device group experienced significantly less pain than the manual compression group. Patients using the Perclose Proglide were found to have a direct reduction in the total cost of the procedure in a cost analysis, due to the reduced length of hospitalization and nursing care. In a review of the Perclose Proglide, its advantages were reported in procedures with large-caliber accesses, such as aortic coarctation or endoluminal repair of aortic aneurysms [53]. The safety and efficacy of the Perclose Proglide is superior to that of manual compression and other vascular closure devices when the device is deployed by experienced and skilled operators. The Perclose Proglide has been well facilitated in reducing time to ambulation and discharge time, decreasing complication rates, and improving patient comfort. Iacovelli et al [54] reported that the use of Perclose Proglide can obviously shorten the total time taken for the procedure, time to ambulation, and time to discharge after the procedure and reduce the demand for general anesthesia and the cost of treatment. A study by Kwak et al [55] showed that the introduction of ultrasound guidance while using the Perclose Proglide significantly reduced the incidence of puncture site complications and decreased the incidence of frequency of additional manual compression with the vascular closure device.
Recommendations
Although there have been many clinical studies on vascular closure devices, most of them have been done on general patients. Not many studies have been done on patients with special risks, such as those with a combination of vascular calcification, femoral artery stenosis, obesity, diabetes mellitus, renal impairment, and other special conditions. The use of vascular closure devices in these special patients is more challenging and potentially advantageous. Enhancing the exploration in this direction can effectively expand the scope of clinical use of vascular closure devices and promote their technical improvement. In addition, some visualization techniques can effectively improve the success rate of vascular closure device use, such as ultrasound guidance. Research in this direction is also more meaningful.
Conclusions
Vascular closure devices have an excellent operational success rate, a low rate of vascular and puncture site complications, reduce patient time to ambulation, and increase patient comfort and satisfaction. In addition, ultrasound-guided maneuvers contribute to improving safety when using vascular closure devices.
Footnotes
Conflict of interest: None declared
Declaration of Figures’ Authenticity: All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Kobayashi T, Hamamoto M, Okazaki T, et al. Efficacy and safety of ultrasound-guided repeat access and repeat closure with an exoseal vascular closure system in patients with peripheral arterial disease. Vasc Endovascular Surg. 2022;56(1):24–28. doi: 10.1177/15385744211045508. [DOI] [PubMed] [Google Scholar]
- 2.Kim E, Sebastiao BG, Lee A, et al. Safety and effectiveness of vascular closure devices in interventional radiological procedures. Interv Neuroradiol. 2023;29(5):525–31. doi: 10.1177/15910199221100628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noori VJ, Eldrup-Jørgensen J. A systematic review of vascular closure devices for femoral artery puncture sites. J Vasc Surg. 2018;68(3):887–99. doi: 10.1016/j.jvs.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 4.Luo J, Liao W, Lei D, et al. Transcarotid versus transfemoral access for cerebrovascular intervention: Protocol for a systematic review and meta-analysis. BMJ Open. 2023;13(6):e071820. doi: 10.1136/bmjopen-2023-071820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagpal S, Scierka LE, Castro-Dominguez Y, et al. Real-world VASCADE closure device versus manual compression use and outcomes in patients with severe common femoral artery disease. Catheter Cardiovasc Interv. 2022;100(5):776–84. doi: 10.1002/ccd.30405. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhuri A. ‘Post-close’ femoral arterial haemostasis at endovascular aneurysm repair using a dedicated large-bore vascular closure device: A prospective real-world audit. Cardiovasc Intervent Radiol. 2023;46(7):835–43. doi: 10.1007/s00270-023-03437-7. [DOI] [PubMed] [Google Scholar]
- 7.Yan H, Guo YQ, Zhou YM, et al. [Construction and validation of a prediction model for complications of femoral artery puncture intervention with Angio-Seal vascular closure application]. Journal of Nursing. 2021;36(04):46–49. [in Chinese] [Google Scholar]
- 8.Shi SL, Long SH, Yu Z, et al. [Comparative study on the clinical application of different vascular suture, closure and blocking devices in femoral artery puncture hemostasis after neurointervention]. Chinese Journal of Radiology. 2024;58(1):71–78. [in Chinese] [Google Scholar]
- 9.Papoutsis D, Mourouzis K, Bozini N, et al. Ultrasonographic assessment and clinical outcomes after deployment of a suture-mediated femoral vascular closure device. Cardiovasc J Afr. 2023;34:1–6. doi: 10.5830/CVJA-2023-054. [DOI] [PubMed] [Google Scholar]
- 10.Zhou Y, Xu C. Comparison of application effects of different hemostasis methods after ischemic cerebrovascular intervention. Front Surg. 2022;9:850139. doi: 10.3389/fsurg.2022.850139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee MO, Jeong KU, Kim KM, Song YG. Risk factors affecting complications of access site in vascular intervention through common femoral artery. Niger J Clin Pract. 2022;25(1):85–89. doi: 10.4103/njcp.njcp_37_21. [DOI] [PubMed] [Google Scholar]
- 12.Feng YP, Huo XR, Zhang HM, et al. [Evidence-based care for perioperative femoral artery puncture site monitoring and management in interventional radiography patients]. Journal of Interventional Radiology. 2023;32(3):272–77. [in Chinese] [Google Scholar]
- 13.Wang SJ, Zu SW, Liu CF, et al. [A multicenter controlled study of simulator training in performing the operation of ExoSeal™ blocking hemostasis system at the femoral artery puncture point]. Chinese Journal of General Surgery. 2021;30(6):693–99. [in Chinese] [Google Scholar]
- 14.Pang N, Gao J, Zhang B, et al. Vascular closure devices versus manual compression in cardiac interventional procedures: systematic review and meta-analysis. Cardiovasc Ther. 2022;2022:8569188. doi: 10.1155/2022/8569188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kmiec L, Zerdzitzki M, Schmid C, et al. Evaluation of the MANTA vascular closure device in transfemoral TAVI. Thorac Cardiovasc Surg. 2023;71(2):84–93. doi: 10.1055/s-0041-1730972. [DOI] [PubMed] [Google Scholar]
- 16.Thurner A, Heuer A, Augustin AM, et al. A novel double clip-based vascular closure device in antegrade and retrograde femoral punctures: A single-center experience in peripheral non-cardiac procedures. J Vasc Access. 2022;23(5):778–87. doi: 10.1177/11297298211012829. [DOI] [PubMed] [Google Scholar]
- 17.Dongmei S, Jiancong Research progress on postoperative nursing of patients undergoing vascular intervention with different approaches and puncture points. Chinese Nursing Research. 2020;34(20):3661–64. [in Chinese] [Google Scholar]
- 18.Millington SJ, Hendin A, Shiloh AL, Koenig S. Better with ultrasound: Peripheral intravenous catheter insertion. Chest. 2020;157(2):369–75. doi: 10.1016/j.chest.2019.04.139. [DOI] [PubMed] [Google Scholar]
- 19.Hüttner FJ, Bruckner T, Hackbusch M, et al. Primary open versus closed implantation strategy for totally implantable venous access ports: The multicentre randomized controlled PORTAS-3 trial (DRKS 00004900) Ann Surg. 2020;272(6):950–60. doi: 10.1097/SLA.0000000000003705. [DOI] [PubMed] [Google Scholar]
- 20.Rao SV, Stone GW. Arterial access and arteriotomy site closure devices. Nat Rev Cardiol. 2016;13(11):641–50. doi: 10.1038/nrcardio.2016.133. [DOI] [PubMed] [Google Scholar]
- 21.Diamantopoulos A, Nourzaie R, Mulholland D, et al. Safety and efficacy of the Mynx Control vascular closure device in peripheral arterial procedures: A prospective study. Vascular. 2023;31(2):369–74. doi: 10.1177/17085381211062745. [DOI] [PubMed] [Google Scholar]
- 22.Bhogal S, Waksman R. Vascular Closure: The ABC’s. Curr Cardiol Rep. 2022;24(4):355–64. doi: 10.1007/s11886-022-01654-z. [DOI] [PubMed] [Google Scholar]
- 23.Jakobsen L, Holm NR, Maeng M, et al. Comparison of MynxGrip vascular closure device and manual compression for closure after femoral access angiography: A randomized controlled trial: The closure devices used in every day practice study, CLOSE-UP III trial. BMC Cardiovasc Disord. 2022;22(1):68. doi: 10.1186/s12872-022-02512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sun LX, Yang XS, Zhang DW, et al. Flip-over of blood vessel intima caused by vascular closure device: A case report. World J Clin Cases. 2022;10(7):2247–52. doi: 10.12998/wjcc.v10.i7.2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saleem T, Baril DT. StatPearls. Treasure Island (FL): StatPearls Publishing; Apr 26, 2023. Vascular access closure devices. [PubMed] [Google Scholar]
- 26.Hao J, Shuyang L, Yong S, et al. [The application and progress of vascular closure devices]. Chinese Journal of Clinical Thoracic and Cardiovascular Surgery. 2023;30(12):1791–96. [in Chinese] [Google Scholar]
- 27.Rumeng W, Kunshan Y, Sha L, et al. [Research progress of vascular closure devices]. Chinese Journal of Interventional Imaging and Therapy. 2020;17(07):438–41. [in Chinese] [Google Scholar]
- 28.Wong HF, Lee CW, Chen YL, et al. Prospective comparison of angio-seal versus manual compression for hemostasis after neurointerventional procedures under systemic heparinization. Am J Neuroradiol. 2013;34(2):397–401. doi: 10.3174/ajnr.A3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Emced K. Comparison of manual compression with a new bioabsorbable vascular closure device in percutaneous peripheral procedures. Ann Clin Anal Med. 2022;13(1):109–13. [Google Scholar]
- 30.Elmasri MA, Kee ST, Moriarty JM, et al. Single-center comparison of the efficacy and complications of arterial vascular closure devices in interventional radiology. J Vasc Access. 2017;18(4):339–44. doi: 10.5301/jva.5000623. [DOI] [PubMed] [Google Scholar]
- 31.Song L, Zhao J, Xiong F, et al. Use of the MynxGrip vascular closure device in patients undergoing interventional diagnosis or treatment: The PANDA multicenter, open-label, randomized controlled trial. J Vasc Access. 2024;25(5):1610–17. doi: 10.1177/11297298231183730. [DOI] [PubMed] [Google Scholar]
- 32.Resnic FS, Majithia A, Marinac-Dabic D, et al. Registry-based prospective, active surveillance of medical-device safety. N Engl J Med. 2017;376(6):526–35. doi: 10.1056/NEJMoa1516333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Diamantopoulos A, Nourzaie R, Mulholland D, et al. Safety and efficacy of the Mynx Control vascular closure device in peripheral arterial procedures: A prospective study. Vascular. 2023;31(2):369–74. doi: 10.1177/17085381211062745. [DOI] [PubMed] [Google Scholar]
- 34.Noory E, Böhme T, Krause L, et al. Evaluation of the MYNX CONTROL™ arterial closure system for achieving primary hemostasis after arterial femoral access following peripheral arterial interventions, compared to the FemoSealTM closure system. J Clin Med. 2023;12(16):5255. doi: 10.3390/jcm12165255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pieper CC, Thomas D, Nadal J, et al. Patient satisfaction after femoral arterial access site closure using the ExoSeal(®) vascular closure device compared to manual compression: A prospective intra-individual comparative study. Cardiovasc Intervent Radiol. 2016;39(1):21–27. doi: 10.1007/s00270-015-1204-2. [DOI] [PubMed] [Google Scholar]
- 36.Wong SC, Bachinsky W, Cambier P, et al. A randomized comparison of a novel bioabsorbable vascular closure device versus manual compression in the achievement of hemostasis after percutaneous femoral procedures: The ECLIPSE (Ensure’s Vascular Closure Device Speeds Hemostasis Trial) JACC Cardiovasc Interv. 2009;2(8):785–93. doi: 10.1016/j.jcin.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 37.Wei X, Han T, Sun Y, et al. A retrospective study comparing the effectiveness and safety of EXOSEAL vascular closure device to manual compression in patients undergoing percutaneous transbrachial procedures. Ann Vasc Surg. 2020;62:310–17. doi: 10.1016/j.avsg.2019.06.031. [DOI] [PubMed] [Google Scholar]
- 38.Mankerious N, Mayer K, Gewalt SM, et al. Comparison of the FemoSeal vascular closure device with manual compression after femoral artery puncture – post-hoc analysis of a large-scale, randomized clinical trial. J Invasive Cardiol. 2018;30(7):235–39. [PubMed] [Google Scholar]
- 39.Schulz-Schüpke S, Helde S, Gewalt S, et al. Comparison of vascular closure devices vs manual compression after femoral artery puncture: The ISAR-CLOSURE randomized clinical trial. JAMA. 2014;312(19):1981–87. doi: 10.1001/jama.2014.15305. [DOI] [PubMed] [Google Scholar]
- 40.Gewalt SM, Helde SM, Ibrahim T, et al. Comparison of vascular closure devices versus manual compression after femoral artery puncture in women. Circ Cardiovasc Interv. 2018;11(8):e006074. doi: 10.1161/CIRCINTERVENTIONS.117.006074. [DOI] [PubMed] [Google Scholar]
- 41.Gabrielli R, Rosati MS, Millarelli M, et al. FemoSeal® device use for femoral artery closure by different techniques. Ann Vasc Surg. 2018;51:18–24. doi: 10.1016/j.avsg.2018.02.016. [DOI] [PubMed] [Google Scholar]
- 42.Kulangara R, Bystrom P, Piel M, et al. Extravascular access artery closure following percutaneous peripheral intervention. J Vasc Surg. 2022;76(4):e73. [Google Scholar]
- 43.Nagpal S, Scierka LE, Castro-Dominguez Y, et al. Real-world VASCADE closure device versus manual compression use and outcomes in patients with severe common femoral artery disease. Catheter Cardiovasc Interv. 2022;100(5):776–84. doi: 10.1002/ccd.30405. [DOI] [PubMed] [Google Scholar]
- 44.Hart B, Hans SS. Maldeployment of Celt ACD vascular closure device. J Vasc Surg Cases Innov Tech. 2021;8(1):39–41. doi: 10.1016/j.jvscit.2021.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wong SC, Laule M, Turi Z, et al. A multicenter randomized trial comparing the effectiveness and safety of a novel vascular closure device to manual compression in anticoagulated patients undergoing percutaneous transfemoral procedures: The CELT ACD trial. Catheter Cardiovasc Interv. 2017;90(5):756–65. doi: 10.1002/ccd.26991. [DOI] [PubMed] [Google Scholar]
- 46.Iqtidar AF, Li D, Mather J, McKay RG. Propensity matched analysis of bleeding and vascular complications associated with vascular closure devices vs standard manual compression following percutaneous coronary intervention. Conn Med. 2011;75(1):5–10. [PubMed] [Google Scholar]
- 47.Dan-dan L, Long C. [Comparison of the hemostatic effect of StarClose vascular closure and femoral artery compression hemostat on femoral artery puncture after cerebral angiography]. China Medical Device Information. 2021;27(14):7–8. [in Chinese] [Google Scholar]
- 48.Kim SH, Behnes M, Baron S, et al. Extravascular compared to intravascular femoral closure is associated with less bleeding and similar MACE after percutaneous coronary intervention. Int J Med Sci. 2019;16(1):43–50. doi: 10.7150/ijms.29253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lucatelli P, Fanelli F, Cannavale A, et al. Angioseal VIP® vs. StarClose SE® closure devices: A comparative analysis in non-cardiological procedures. J Cardiovasc Surg (Torino) 2017;58(1):80–86. doi: 10.23736/S0021-9509.16.07654-0. [DOI] [PubMed] [Google Scholar]
- 50.Eleshra A, Kim D, Park HS, Lee T. Access site pseudoaneurysms after endovascular intervention for peripheral arterial diseases. Ann Surg Treat Res. 2019;96(6):305–12. doi: 10.4174/astr.2019.96.6.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sekhar A, Sutton BS, Raheja P, et al. Femoral arterial closure using ProGlide® is more efficacious and cost-effective when ambulating early following cardiac catheterization. Int J Cardiol Heart Vasc. 2016;13:6–13. doi: 10.1016/j.ijcha.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Iannopollo G, Nobile G, Lanzilotti V, et al. Percutaneous artErial closure devices and ultrasound-guided Trans-femoRal puncture ObservatioNal InvestigatiOn: Insights from the PETRONIO registry. Catheter Cardiovasc Interv. 2022;99(3):795–803. doi: 10.1002/ccd.29828. [DOI] [PubMed] [Google Scholar]
- 53.Del Prete A, Della Rocca DG, Calcagno S, et al. Perclose Proglide™ for vascular closure. Future Cardiol. 2021;17(2):269–82. doi: 10.2217/fca-2020-0065. [DOI] [PubMed] [Google Scholar]
- 54.Iacovelli F, Burattini O, Sturdà F, et al. Single suture-mediated closure system after transfemoral transcatheter aortic valve implantation: A single-center real-world experience. Catheter Cardiovasc Interv. 2024;103(7):1125–37. doi: 10.1002/ccd.31054. [DOI] [PubMed] [Google Scholar]
- 55.Kwak J, Bum Cho S. Real-time ultrasound-guided hemostasis using suture-mediated closure device. J Vasc Access. 2023 doi: 10.1177/11297298231215843. [Online ahead of print] [DOI] [PubMed] [Google Scholar]