Abstract
Background
Female sex workers are disproportionately affected by sexual violence, which is associated with an increased risk of poor mental health outcomes, substance use, and decreased access to health resources. Understanding the pathways through which sexual violence impacts these outcomes can inform strategies that appropriately and effectively meet the health needs of sex workers.
Methods
This study investigated the prevalence of sexual violence among female sex workers in Côte d’Ivoire, and the relationship between sexual violence and adverse mental health and substance use outcomes. We examined survey data from female sex workers recruited between November 2019 and May 2020 across five regions of Côte d’Ivoire using respondent driven sampling (RDS), as part of an integrated bio-behavioral survey. The primary exposure of interest was self-reported lifetime experience of sexual violence, and the main outcomes of interest included depression, suicidal ideation, counselling seeking, alcohol consumption, and substance use. Multivariable logistic regression models investigated associations between exposure to sexual violence and the key mental health and substance use outcomes of interest. For each outcome, a directed acyclic graph was developed to identify a minimally sufficient set of covariates for adjustment. Additional sociodemographic characteristics, experiences, and sex work-related behaviors were explored in descriptive analyses using crude and RDS adjusted estimates.
Results
Out of 1,177 participants, 376 (31.9%; RDS weighted: 30.5%; 95% CI: 24.7, 36.3) reported having experienced sexual violence in their lifetime, and of those 31.9% (RDS weighted: 31.2%; 95% CI: 21.3, 41.1) had experienced sexual violence within the previous 12 months. Experience of sexual violence was associated with an increased odds of suicidal ideation (aOR: 1.95; 95% CI: 1.48, 2.55), illicit drug use in the last 12 months (aOR: 2.40; 95% CI: 1.50, 3.86), daily alcohol use (aOR: 1.63; 95% CI: 0.99, 2.67), and having spoken to a counselor or confidant (aOR: 1.90; 95% CI: 1.34, 2.68).
Conclusion
Findings confirm a high burden of sexual violence among female sex workers in Côte d’Ivoire, and a need to implement large structural changes that enable female sex workers to seek protection as well as health resources after experiencing sexual violence. This may include reform in the form of targeted social, clinical and mental health resources, along with community development opportunities.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20177-6.
Keywords: Sexual violence, Intimate partner violence, Sex work, Substance use, Mental health
Background
Globally, female sex workers experience a high burden of gender-based violence and other forms of sexual violence [1–9]. Lifetime prevalence of workplace violence affecting sex workers ranges from 45 to 75% [6], but has been shown to be greater in settings where sex work is highly stigmatized [9]. In Côte d’Ivoire, the lifetime prevalence of sexual violence affecting female sex workers in urban settings like Abidjan is estimated to be more than 40% [10]. This is significantly higher than what is estimated among the general population. In the 2021 Demographic and Health Survey, around 7% of women surveyed aged 15–49 reported having experienced some form of sexual violence [11].
Violence against female sex workers is not routinely monitored, reported, or acted upon in most settings, resulting in limited recourse and few legal protections for women who experience violence [6]. In settings where sex work is illegal or criminalized, clients may be more empowered to perpetrate violence given legal impunity, and female sex workers may be more reluctant to report these incidents of violence [6, 12, 13]. Moreover, a lack of legal protections means that women may be forced to work in dangerous conditions, for example by soliciting or meeting clients on secondary streets or other isolated locations, where they may be less likely to be observed by law enforcement and more likely to experience violence [14, 15].
The environment within which female sex workers sell sex can also shape their ability to access resources such as social support and health services after experiencing violence [12, 13]. Sexual violence is associated with both depression and substance use [2, 9, 16], which drive decisions around condom use and increase the risk of acquiring HIV and other sexually transmitted infections (STI) in the absence of comprehensive preventative healthcare. Previous studies have found that sex workers who reported working in an environment where police refused to protect them had more than twice the odds of acquiring HIV [16].
In Côte d’Ivoire, survey data suggest that there are many barriers to female sex workers seeking protection from violence and accessing healthcare resources after violence occurs [1]. Although exchanging sex for money is legal in Côte d’Ivoire, it is illegal to solicit to sell sex in public spaces and to pander or operate dedicated sex work venues [17]. The criminalization of particular aspects of sex work, even if sex work itself is not illegal, means that sex workers are often not registered and not able to seek the resources they need due to fear of arrest and other police actions after experiencing violence [7]. This environment may also make reporting instances of violence challenging for many sex workers, suggesting that the burden of sexual and physical violence in Côte d’Ivoire is underreported.
This study used data from an integrated bio-behavioral survey which was administered by Enda Santé Côte d’Ivoire. The survey aimed widely to provide factual and contextual data on sex worker populations in Côte d’Ivoire in order to improve targeted HIV prevention and treatment programs. This analysis aimed to better characterize and contextualize the burden of sexual violence affecting female sex workers in Côte d’Ivoire. Furthermore, the study investigated the relationship between sexual violence among female sex workers and adverse health outcomes such as poor mental health and substance use, which have not been fully explored in this context [10, 18].
Methods
Study design
Data for these analyses were collected among female sex workers between November 2019 and May 2020 in five regions of Côte d’Ivoire as part of an integrated bio-behavioral survey (IBBS) and population size estimation study. The aims of this original study were to estimate HIV prevalence and associated risk factors for female sex workers in Côte d’Ivoire, including experiences of sex work, access to health resources, and stigma and discrimination [19]. Regions were prioritized for inclusion based on their high overall prevalence of HIV or their population size (> 100,000), and included Aboisso, Soubré, Agboville, Yamoussoukro, and Katiola. Once recruited, participants were asked to complete a cross-sectional quantitative survey and HIV testing; participants living with HIV were referred for treatment as per Côte d’Ivoire national guidelines. All participants were also given information about HIV and other STIs more widely.
Study population and sampling
Participants were eligible for inclusion if they identified as women, were assigned female sex at birth, were currently practicing sex work, were 16 years or older, had lived in the study region for at least three months, and provided informed consent to participate in the study. Participants were excluded from the study if they had a health condition that impeded their full understanding of the study and the informed consent process, were under the influence of substances, or had previously participated in the study. Participants were given information regarding HIV prevention, and those that were living with HIV were referred for treatment. Participants were also referred for other resources as needed, including counseling in the case of reporting experiences of sexual violence or suicidal ideation.
Participants were recruited within each region using respondent driven sampling (RDS) [20–22]. RDS is a network-based recruitment method which facilitates reaching and estimating the size of populations for which a reliable sampling frame does not exist [23]. This methodology enabled researchers to reach a diverse group of female sex workers within different demographic and social groups in Côte d’Ivoire. An initial set of female sex worker seeds were recruited and given coupons to recruit further participants within their communities. Seed selection was led by community organization ENDA Santé and local community leaders. Seeds were intentionally diverse in sociodemographic characteristics, including age, education, marital status, and sex work registration status in order to maximize the range of lived experience among those who were recruited into the study. Participants were eligible for inclusion if they presented a valid RDS coupon at the study site. A total of 1,177 participants were ultimately enrolled into the study.
Measures
Primary exposure
The primary outcome of interest in this analysis was self-reported lifetime sexual violence, measured as having ever been forced to have sexual relations when the participant did not want to. Experiences of sexual violence were recorded by asking participants if they had “ever been forced to have sexual relationships without wanting to (by ‘forced’, we mean physically forced, coerced to have sexual relations, or penetration with an object when you did not want to).”
Primary outcomes
This analysis aimed to characterize the association of sexual violence with self-reported mental health and substance use outcomes. Primary outcomes of interest were measured categorically, and included:
Depression
Participants who reported depression were those who reported having experienced depression or sadness for more than two weeks. This was captured by asking participants if they had “ever felt sad or depressed during more than two weeks at a time.”
Suicidal ideation
Participants who had at some point experienced suicidal ideation. This was captured by asking participants if they had ever wanted to end their life.
Spoken to a counselor or confidant
Participants who had experienced depression or suicidal ideation were also asked whether they had ever spoken to a counselor or confidant about those feelings.
Alcohol consumption
Alcohol consumption was measured by regular use. Participants were asked “with what frequency they had consumed alcohol over the previous 30 days”, and reported whether they had never, sometimes, or regularly (on a daily basis) consumed alcohol.
Substance use
Use of illegal substances captured whether participants had never used drugs, used drugs more than 12 months ago, or had used drugs within the last 12 months. The question asked participants if they had “ever consumed drugs, including marijuana, glue, powdered cocaine, crack, heroine, narcotics, codeine, or other drugs.”
Additional measures
In descriptive analyses, the following measures were also explored to characterize patterns of physical and sexual violence among female sex workers:
Sociodemographic characteristics
Sociodemographic characteristics of interest included age, country of origin, years living in Côte d’Ivoire, education level, marital status, weekly income, and employment status outside of sex work. The analysis also included years spent in sex work.
Sexual violence experiences and reporting practices
Granular measures related to sexual violence included the number of experiences of sexual violence, whether the last experience of sexual violence had taken place within the previous 12 months, age at first experience of sexual violence, type of perpetrator, whether the perpetrator(s) had been reported, and whether the perpetrator(s) were arrested. The last three variables referred to the latest instance of sexual violence, and respondents were able to select perpetrator type from a list of options comprising: regular clients; occasional or new clients; spouse or other non-paying partner; manager (related to sex work); police or other security; teacher, friend or co-worker; family member; neighbor; or stranger.
Physical violence
The analysis included an exploration of physical violence and its relation to sexual violence through the following variables: lifetime experiences of physical violence during sex work, number of experiences of physical violence, perpetrator of physical violence, and whether the respondent believed that this violence was linked to their sex worker status.
HIV and condom use
Two main self-reported variables related to HIV were analyzed: lifetime HIV testing and last HIV test result. The analysis also included six self-reported variables used to characterize condom use. These six variables were: condom use during sex work (never, frequent, or always); condom use during last sexual encounter with a client; difficulty of persuading a new client to use a condom; difficulty of persuading a regular client to use a condom; and difficulty of persuading a non-paying partner to use a condom. The variables assessing persuasion power had three response options: difficult, neither difficult nor easy, and easy. Finally, the analysis included participant reports of ever having avoided carrying condoms out of fear of issues with police.
Statistical analyses
We conducted a descriptive analysis assessing frequencies, proportions, and RDS adjusted estimates for sociodemographic characteristics, sexual violence prevalence and reporting practices, physical violence experiences, mental health, substance use, HIV testing and status, and condom use. We then compared differences in these characteristics between women who reported having experienced sexual violence and those that did not using a Pearson’s chi-squared test. The RDS adjusted estimates allowed us to account for the sampling method and the probability of being sampled based on network size.
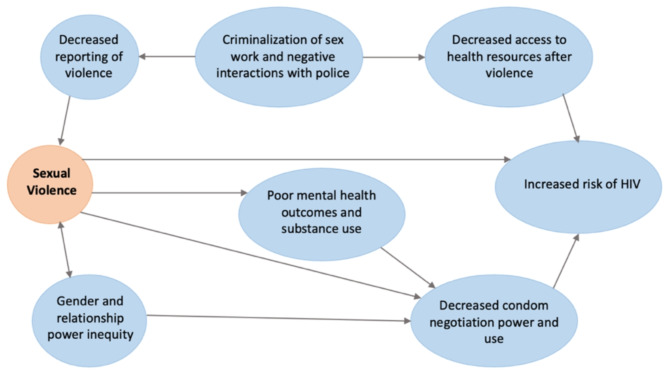
Associations between lifetime sexual violence and a priori-specified mental health and substance use outcomes were estimated using unadjusted and adjusted logistic regression models. A conceptual model informed our understanding of potential pathways through which sexual violence may lead to an increased risk of suboptimal mental health outcomes, risky sexual practices, and HIV among female sex workers (Fig. 1). For each outcome, we subsequently developed a directed acyclic graph (DAG) to identify a minimally sufficient set of covariates for adjustment (Supplementary material 1). Covariates included for adjustment in these models included age, educational level, income, country of origin, and years lived in Côte d’Ivoire. Unadjusted and adjusted Odds Ratios (aOR) were calculated with their associated 95% confidence intervals (CI). Odds ratios were not weighted, as the utility of RDS weights for this purpose is debated, and a standard methodology for use of RDS-adjusted estimates in regression models has not been well-established [24–26].
Fig. 1.
Pathways through which sexual violence may lead to an increased risk of suboptimal mental health outcomes, risky sexual practices, and HIV among female sex workers
All analyses were conducted using Stata, version 15.0 [27]. Stata’s RDS package was used for RDS adjustment, using RDS II estimator [28].
Results
Sample characteristics
A total of 1,177 participants were included in this analysis, including 200 (24.1%; 95% CI: 20.5, 27.7) in Aboisso, 230 (24.1%; 95% CI: 17.6, 30.6) in Agboville, 347 (13.1%; 95% CI: 6.2, 20.0) in Katiola, 200 (20.5%; 95% CI: 16.5, 24.5) in Soubré, and 200 (18.2%; 95% CI: 13.7, 22.7) in Yamoussoukro (Table 1). Most participants were single (81.7%; 95% CI: 76.6, 86.8) and between 19 and 29 years of age (70.2%; 95% CI: 64.2, 76.1). Nearly all (93.9%; 95% CI: 91.6, 96.3) reported Côte d’Ivoire as their country of origin. Half (52.2%; 95% CI: 45.8, 58.7) reported some secondary school education and 37.3% (95% CI: 31.5, 43.2) were informally employed outside of sex work.
Table 1.
Demographic characteristics and experiences of sexual violence of female sex workers in Côte d’Ivoire participating in the study, n (%)+
| Total (N = 1,177) |
RDS adjusted proportion (N = 902)‡ |
Sexual Violence | |||
|---|---|---|---|---|---|
| Yes (N = 376) |
Chi squared p value** | RDS Adjusted Yes (N = 297) |
|||
| n (%) | % (95% CI) | n (%) | % (95% CI) | ||
| SOCIODEMOGRAPHIC VARIABLES | |||||
| Age | |||||
| 16–18 | 77 (6.5) | 4.7 (2.6, 6.8) | 22 (5.9) | 0.896 | 3.3 (1.8, 4.8) |
| 19–29 | 832 (70.7) | 70.2 (64.2, 76.1) | 265 (70.5) | 67.8 (57.6, 77.9) | |
| 30–39 | 220 (18.7) | 20.6 (15.3, 26.0) | 73 (19.4) | 23.6 (14.4, 32.9) | |
| 40+ | 48 (4.1) | 4.5 (1.5, 7.5) | 16 (4.3) | 5.3 (0.0, 11.0) | |
| REGION OF RESIDENCE | |||||
| Aboisso | 200 (17.0) | 24.1 (20.5, 27.7) | 57 (15.2) | 0.006* | 22.4 (16.8, 28.0) |
| Agboville | 230 (19.5) | 24.1 (17.6, 30.6) | 84 (22.3) | 29.2 (16.9, 41.4) | |
| Katiola | 347 (29.5) | 13.1 (6.2, 20.0) | 88 (23.4) | 8.1 (0.0, 18.3) | |
| Soubré | 200 (17.0) | 20.5 (16.5, 24.5) | 74 (19.7) | 20.7 (14.4, 27.0) | |
| Yamoussoukro | 200 (17.0) | 18.2 (13.7, 22.7) | 73 (19.4) | 19.6 (11.9, 27.3) | |
| Country of origin | |||||
| Côte d’Ivoire | 1,110 (94.3) | 93.9 (91.6, 96.3) | 362 (96.3) | 0.068 | 97.2 (96.0, 98.3) |
| Other | 52 (4.4) | 4.5 (0.8, 8.0) | 9 (2.4) | 1.6 (1.1, 2.1) | |
| No response | 15 (1.3) | 1.6 (0.4, 2.9) | 5 (1.3) | 1.2 (0.3, 2.1) | |
| Years lived in Côte d’Ivoire | |||||
| 0–10 | 56 (4.8) | 5.1 (2.7, 7.4) | 12 (3.2) | 0.084 | 2.1 (1.4, 2.8) |
| > 10 | 1,121 (95.2) | 94.9 (92.6, 97.3) | 364 (96.8) | 97.9 (97.2, 98.6) | |
| Education | |||||
| Primary or less | 492 (41.8) | 41.4 (34.7, 48.0) | 161 (42.8) | 0.799 | 44.5 (33.1, 55.9) |
| Secondary | 614 (52.2) | 52.2 (45.8, 58.7) | 191 (50.8) | 48.9 (37.8, 59.9) | |
| University | 71 (6.0) | 64.1 (49.7, 78.6) | 24 (6.4) | 6.6 (3.9, 9.3) | |
| Marital status | |||||
| Single | 896 (76.1) | 81.7 (76.6, 86.8) | 287 (76.3) | 0.862 | 81.6 (74.1, 89.1) |
| Married or cohabitating | 59 (5.0) | 5.6 (2.6, 8.6) | 19 (5.1) | 5.4 (2.4, 8.3) | |
| Divorced or widowed | 49 (4.2) | 3.4 (0.8, 5.9) | 13 (3.5) | 4.8 (0.0, 10.2) | |
| No response | 173 (14.7) | 9.3 (5.6, 13.1) | 57 (15.2) | 8.3 (3.6, 13.0) | |
| Employment outside of sex work | |||||
| Student | 274 (23.3) | 19.9 (15.6, 24.2) | 81 (21.5) | 0.357 | 42.7 (32.1, 53.4) |
| Unemployed | 252 (21.4) | 24.0 (17.8, 30.1) | 73 (19.4) | 18.9 (8.5, 29.2) | |
| Informally employed*** | 420 (35.7) | 37.3 (31.5, 43.2) | 145 (38.6) | 15.4 (8.8, 22.0) | |
| Other/No response | 231 (19.6) | 18.8 (13.2, 24.5) | 77 (20.5) | 23.1 (12.6, 33.6) | |
| PHYSICAL VIOLENCE | |||||
| Has experienced non-sexual physical violence since practicing sex work | |||||
| No | 794 (67.5) | 69.8 (63.6, 76.0) | 175 (46.5) | < 0.001* | 47.4 (36.5, 58.3) |
| Yes | 381 (32.4) | 30.1 (23.9, 36.3) | 200 (53.2) | 52.4 (41.5, 63.3) | |
+ Some variables have instances of missing values not shown in Table 1 (< 2% in all cases)
‡ The RDS adjusted sample size corresponds to those who completed the coupon data for RDS adjustment
* Statistically significant (p < 0.05)
** Chi-squared test of differences in sexual violence experiences across variable categories
***Informal employment refers to work conducted within the informal economy (neither taxed nor monitored by any form of government)
A smaller sample of participants had RDS weight data available (N = 902 compared to the overall sample of N = 1,177). However, a comparison of the participants with RDS weights available showed that they did not differ in terms of any relevant sociodemographic characteristics or outcomes of interest from the overall sample (Supplementary material 2).
Experiences of sexual violence were common; 31.9% (RDS adjusted: 30.5%; 95% CI: 24.7, 36.3) reported experiencing sexual violence at some point in their lives. Among participants that had experienced sexual violence, 53.2% (200/376) had also experienced physical violence as compared to 22.6% (181/801) of those who had not experienced sexual violence (p < 0.001). Sociodemographic characteristics were generally similar irrespective of past experiences of sexual violence, with the exception of a higher burden of physical violence reported among participants who had experienced sexual violence. RDS-adjusted characteristics among women reporting sexual violence are included in Supplementary material 3.
Experiences, perpetrators, and reporting of sexual and physical violence
Of the 376 participants who reported past experiences of sexual violence, 31.2% (95% CI: 21.3, 41.1; 120/376) had experienced sexual violence in the last 12 months and 66.6% (95% CI: 56.3, 76.8; 248/376) had experienced sexual violence more than 12 months ago (Table 2). Perpetrators of sexual violence at the most recent instance of abuse were most commonly occasional or new clients (23.4%; 95% CI: 12.5, 34.2; 98/376). For 22.2% (95%CI: 13.5, 30.9; 89/376) of participants, the perpetrator was a spouse or other non-paying partner; 22.0% (95% CI: 14.1, 30.0; 73/376) reported the perpetrator was a regular client. Only 7.6% (95% CI: 0.6, 14.4; 26/376) of women that had experienced sexual violence reported their abuse to the authorities and of those, 53.2% (95% CI: 17.7, 88.6; 14/26) reported that their abusers had not been arrested. No incidents of violence were formally reported for those that said their perpetrator was their manager, their teacher, friend, co-worker or classmate, or family member.
Table 2.
Sexual violence (SV) experiences and reporting practices among 376 female sex workers in Côte d’Ivoire, n (%)
| Total sample un-adjusted, n = 376 n (%) or median (IQR) |
RDS adjusted, n = 297* % (95% CI) |
||
|---|---|---|---|
| Last experience of sexual violence | |||
| Less than 12 months ago | 120 (31.9) | 31.2 (21.3, 41.1) | |
| More than 12 months ago | 248 (66.0) | 66.6 (56.3, 76.8) | |
| No response/does not know | 8 (2.1) | 2.2 (0, 5.3) | |
| Age at first experience of sexual violence | |||
| 19.3 (16, 22) | 19.7 (18.5, 20.9) | ||
| Number of experiences of sexual violence | |||
| 2 (1, 3) | 2 (2,3) | ||
| Most recent perpetrator of sexual violence | |||
| Regular client | 73 (19.4) | 22.0 (14.1, 30.0) | |
| Occasional or new client | 89 (23.7) | 23.4 (12.5, 34.2) | |
| Spouse or another partner | 98 (26.1) | 22.2 (13.5, 30.9) | |
| Manager (related to sex work) | 2 (0.5) | 0.6 (0, 1.5) | |
| Police, military, other security | 7 (1.9) | 1.1 (0, 2.4) | |
| Teacher, friend, co-worker, etc. | 22 (5.9) | 6.0 (1.1, 10.9) | |
| Family member | 14 (3.7) | 4.0 (0, 8.1) | |
| Neighbor | 33 (8.9) | 10.4 (2.5, 18.2) | |
| Stranger | 38 (10.1) | 10.4 (3.7, 17.0) | |
| Reported instance of sexual violence to the authorities | |||
| No | 349 (92.8) | 92.4 (85.5, 99.3) | |
| Yes | 26 (6.9) | 7.6 (0.6, 14.4) | |
| No response | 1 (0.3) | 0 (0, 0) | |
| Perpetrator of sexual violence was arrested | |||
| No, none were arrested | 14 (53.8) | 53.2 (17.7, 88.6) | |
| Yes, all were arrested | 8 (30.8) | 26.1 (8.9, 43.3) | |
| Yes, but not all perpetrators | 4 (15.4) | 20.8 (0, 52.3) | |
A total of 381 participants (30.1%; 95% CI: 23.9, 36.3; 381/1,177) reported that they had experienced non-sexual physical violence (Table 3). Of these, 299 responded to a question about who the perpetrator of that physical violence was. The most common perpetrators of physical violence were occasional or new clients (24.6%; 95% CI: 14.1, 35.1; 96/299), strangers (24.6%; 95% CI: 12.9, 36.3; 74/299), and non-paying partners (23.8%; 95% CI: 15.6, 31.9; 61/299). More than half (52.9%; 95% CI: 41.4, 64.5; 185/381) of participants who had experienced physical violence believed this abuse was related to their status as a sex worker.
Table 3.
Experiences of non-sexual physical violence (PV) among female sex workers in Côte d’Ivoire (n = 1,177)
| Total sample un-adjusted, n = 1,177 n (%) or median (IQR) |
RDS adjusted, n = 902 % (95% CI) |
||
|---|---|---|---|
| Has experienced physical violence since practicing sex work | |||
| No | 794 (67.5) | 69.8 (63.6, 76.0) | |
| Yes | 381 (32.4) | 30.1 (23.9, 36.3) | |
| Number of experiences of physical violence | |||
| 2 (1, 3) | 3 (2,3) | ||
| Perpetrator of physical violence ( n = 299)* | |||
| Regular client | 61 (20.4) | 14.8 (8.0, 21.6) | |
| Occasional or new client | 74 (24.7) | 24.6 (14.1, 35.1) | |
| Spouse or another partner | 96 (32.1) | 23.8 (15.6, 31.9) | |
| Manager (related to sex work) | 5 (1.7) | 1.0 (0, 2.2) | |
| Police, military, other security | 1 (0.3) | 0.2 (0, 0.5) | |
| Family member | 9 (3.0) | 2.0 (0, 4.5) | |
| Neighbor | 14 (4.7) | 3.0 (0, 8.7) | |
| Stranger | 22 (7.4) | 24.6 (12.9, 36.3) | |
| Other | 17 (5.7) | 4.5 (0, 5.6) | |
| Believes violence was linked to sex worker status | |||
| No | 140 (36.8) | 33.7 (22.4, 45.0) | |
| Yes, some experiences | 45 (11.8) | 9.7 (2.4, 17.1) | |
| Yes, all experiences | 185 (48.6) | 52.9 (41.4, 64.5) | |
| No response | 1 (0.3) | 0.1 (0, 0.1) | |
| Doesn’t know | 10 (2.6) | 3.6 (0, 9.3) | |
*Of the 381 participants who had experienced physical violence, 299 responded to this question
A greater proportion of participants who had experienced sexual violence (Table 4) had been engaged in sex work for more than 5 years compared to participants who had not experienced sexual violence (31.9% vs. 26.1%, p = 0.038). Suicidal ideation was also more common among participants who had experienced violence compared to those that had not (35.6% vs. 22.4%, p < 0.001). Among those who had experienced depression or suicidal ideation, having sought counseling was less common among those who had experienced sexual violence compared to those who had not. (44.7% vs. 55.3%, p < 0.001). Similarly, those who had experienced sexual violence reported daily alcohol consumption more frequently than those who had not experienced sexual violence (30.3% vs. 19.8%, p = 0.003). Illegal drug consumption in the previous 12 months was also more common among those that had experienced sexual violence than those that had not (10.5% vs. 4.9%, p = 0.001).
Table 4.
Sex work conditions, mental health outcomes, HIV and condom use, and experiences of sexual violence of female sex workers in Côte d’Ivoire participating in the study, n(%)
| Total (N = 1,177)+ |
RDS adjusted proportion (N = 902) ‡ |
Sexual Violence | ||||
|---|---|---|---|---|---|---|
| Yes (N = 376) |
Chi squared p value** | RDS Adjusted Yes (N = 297) |
||||
| n (%) | % (95% CI) | n (%) | % (95% CI) | |||
| SEX WORK CONDITIONS | ||||||
| Years spent in sex work | ||||||
| 0–5 | 848 (72.0) | 71.5 (57.6, 77.3) | 256 (68.1) | 0.038* | 67.4 (57.6, 77.3) | |
| > 5 | 329 (28.0) | 28.5 (22.5, 34.5) | 120 (31.9) | 32.6 (22.8, 42.5) | ||
| Weekly income (CFA francs) | ||||||
| Less than 50,000 | 626 (53.2) | 73.5 (68.4, 78.6) | 197 (52.4) | 0.709 | 74.5 (66.2, 82.8) | |
| 50,000 or more | 551 (46.8) | 26.5 (21.4, 31.6) | 179 (47.6) | 25.5 (17.3, 33.8) | ||
| MENTAL HEALTH | ||||||
| Has experienced depression or sadness for more than 2 weeks | ||||||
| No | 572 (48.6) | 44.3 (37.8, 50.8) | 178 (47.3) | 0.554 | 45.5 (34.4, 56.7) | |
| Yes | 605 (51.4) | 55.7 (49.2, 62.2) | 198 (52.7) | 54.5 (43.3, 65.6) | ||
| Suicidal ideation | ||||||
| No | 864 (73.4) | 72.0 (66.3, 77.8) | 242 (64.4) | < 0.001* | 60.9(49.8, 72.1) | |
| Yes | 313 (26.6) | 28.0 (22.2, 33.7) | 134 (35.6) | 39.1 (27.9, 50.3) | ||
| Has spoken to counselor or confidant (if has experienced depression or suicidal ideation, n = 696) | ||||||
| No | 497 (71.4) | 52.8 (42.6, 63.0) | 150 (62.8) | < 0.001* | 39.1 (22.3, 56.0) | |
| Yes | 199 (28.6) | 47.2 (37.0, 57.4) | 89 (37.2) | 60.9 (44.0,77.7) | ||
| SUBSTANCE USE | ||||||
| Alcohol consumption ( n = 827) + | ||||||
| Never | 114 (13.8) | 15.0 (10.4, 19.6) | 36 (12.5) | 0.003* | 13.2 (6.5, 20.0) | |
| Sometimes | 519 (62.8) | 64.6 (58.0, 71.1) | 164 (57.1) | 57.3 (45.8, 68.7) | ||
| Regularly (every day) | 194 (23.5) | 20.4 (14.6, 26.3) | 87 (30.3) | 29.5 (18.6, 40.5) | ||
| Illegal drug consumption ( n = 1139) + | ||||||
| No | 1,030 (90.4) | 91.3 (88.2, 94.4) | 309 (85.6) | 0.001* | 85.8 (78.2, 93.4) | |
| Yes, more than 12 months ago | 33 (2.9) | 2.4 (1.2, 3.5) | 14 (3.9) | 3.6 (1.3, 5.8) | ||
| Yes, in the last 12 months | 76 (6.7) | 6.3 (3.4, 9.3) | 38 (10.5) | 10.6 (3.3, 17.9) | ||
| HIV AND CONDOM USE | ||||||
| Lifetime HIV testing ( n = 1175) + | ||||||
| No | 227 (19.3) | 17.0 (12.4, 21.6) | 67 (17.8) | 0.372 | 14.5 (7.0, 22.1) | |
| Yes | 948 (80.7) | 82.9 (78.3, 87.5) | 309 (82.2) | 85.5 (78.0, 93.0) | ||
| Reported last HIV test result ( n = 670) + | ||||||
| Negative | 648 (96.7) | 95.9 (92.0, 99.9) | 227 (96.6) | 0.897 | 96.9 (95.0, 98.7) | |
| Positive | 22 (3.3) | 4.1 (0.1, 8.0) | 8 (3.4) | 3.1 (1.3, 5.0) | ||
| Condom use frequency during sex work ( n = 1174) + | ||||||
| Never | 90 (7.7) | 7.8 (4.7, 10.9) | 29 (7.7) | 0.036* | 7.4 (1.2, 13.5) | |
| Frequently | 278 (23.7) | 25.4 (20.0, 30.9) | 106 (28.3) | 33.4(22.9, 43.9) | ||
| Always | 806 (68.7) | 66.8 (60.9, 72.6) | 240 (64.0) | 59.3(48.3, 70.3) | ||
| Condom during last sexual encounter (vaginal or anal) with a client ( n = 825) + | ||||||
| No | 160 (19.4) | 20.1 (15.1, 26.7) | 69 (24.0) | 0.014* | 27.7 (16.5, 39.0) | |
| Yes | 665 (80.6) | 79.1 (73.3, 84.9) | 218 (76.0) | 72.3 (61.0, 83.5) | ||
| Difficulty of persuading a new client to use a condom ( n = 1172) + | ||||||
| Difficult | 230 (19.6) | 19.6 (14.9, 24.3) | 90 (24.0) | 0.035* | 27.8 (17.0, 38.6) | |
| Neither difficult nor easy | 136 (11.6) | 12.6 (8.2, 16.9) | 41 (10.9) | 10.3 (4.8, 15.8) | ||
| Easy | 806 (68.8) | 67.9 (62.1, 73.7) | 244 (65.1) | 61.9 (51.0, 72.9) | ||
| Difficulty of persuading a regular client to use a condom ( n = 1172) + | ||||||
| Difficult | 178 (15.2) | 15.0 (10.6, 19.4) | 65 (17.3) | 0.387 | 20.1 (11.9, 28.3) | |
| Neither difficult nor easy | 129 (11.0) | 11.8 (7.8, 15.8) | 40 (10.6) | 11.6 (5.1, 18.0) | ||
| Easy | 865 (73.8) | 73.2 (67.7, 78.7) | 271 (72.1) | 68.3 (58.6, 78.1) | ||
| Difficulty of persuading a non-paying partner to use a condom ( n = 1052) + | ||||||
| Difficult | 355 (33.8) | 34.0 (27.3, 40.7) | 129 (37.8) | 0.142 | 42.5 (30.6, 54.4) | |
| Neither difficult nor easy | 161 (15.3) | 14.4 (10.4, 18.3) | 47 (13.8) | 11.7 (7.1, 16.3) | ||
| Easy | 536 (51.0) | 51.6 (45.0, 58.4) | 165 (48.4) | 45.8 (34.6, 57.1) | ||
| Has avoided carrying condoms out of fear of issues with police ( n = 1165) + | ||||||
| No | 1,066 (91.5) | 97.6 (95.3, 99.9) | 320 (86.3) | < 0.001* | 97.6 (96.0, 99.3) | |
| Yes | 99 (8.5) | 2.4 (0.1, 4.7) | 51 (13.8) | 2.4 (0.7, 4.0) | ||
+Where denominator varies due to missing values, alternative denominator is listed
‡ The RDS adjusted sample size corresponds to those who completed the coupon data for RDS adjustment
* Statistically significant (p < 0.05)
** Chi-squared test of differences in sexual violence experiences across variable categories
Participants who had experienced sexual violence were less likely to have used a condom during their last sexual encounter than those who had not experienced sexual violence (76.0% vs. 83.1%, p = 0.014) and more frequently reported having difficulty in persuading a new client to use a condom compared to those who had not experienced sexual violence (24.0% vs. 17.6%, p = 0.035). Those who had experienced sexual violence were also more likely to have at some point avoided carrying condoms out of fear of facing issues with the police as compared to those that had not experienced sexual violence (13.8% vs. 6.1%, p < 0.001).
Sexual violence and associated mental health and substance use outcomes
In multivariable analyses of mental health and substance use outcomes and their association with sexual violence (Table 5), those that had experienced sexual violence were more likely to report having at some point experienced suicidal ideation (aOR: 1.95; 95% CI: 1.48, 2.55) and having spoken to a counselor or confidant about their feelings (aOR: 1.90, 95% CI: 1.34, 2.68) compared to participants that had not experienced sexual violence. They were also more likely to report having consumed illegal drugs within the last 12 months (aOR: 2.40, 95% CI: 1.50, 3.86) and to report more daily alcohol use (aOR: 1.63; 95% CI: 0.99, 2.67) compared to participants that had not experienced sexual violence.
Table 5.
Associations of lifetime sexual violence with mental health and substance use outcomes. For each outcome, the exposure of interest is experience of sexual violence compared to those who reported not having experienced sexual violence
| Unadjusted OR | OR 95% CI | Adjusted OR* | Adjusted OR 95% CI* | |
|---|---|---|---|---|
| Experiences of depression or sadness (Ref: No experiences of depression/sadness) | 1.08 | (0.84–1.38) | 1.09 | (0.85–1.40) |
| Suicidal ideation (Ref: No history of suicidal ideation) | 1.92** | (1.47–2.52) | 1.95** | (1.48–2.55) |
| Having spoken to a counselor or confidant (Ref: Did not speak to counselor/confidant) | 1.87** | (1.33–2.63) | 1.90** | (1.34–2.68) |
| Consuming alcohol occasionally (sometimes) (Ref: Never) | 1.00 | (0.65–1.55) | 0.94 | (0.60–1.46) |
| Consuming alcohol regularly (daily) (Ref: Never) | 1.76** | (1.08–2.86) | 1.63 | (0.99–2.67) |
| Having consumed illegal drugs more than 12 months ago (Ref: Never) | 1.72 | (0.85–3.47) | 1.81 | (0.89–3.69) |
| Having consumed illegal drugs within the last 12 months (Ref: Never) | 2.33** | (1.46–3.73) | 2.40** | (1.50–3.86) |
Each outcome was assessed through a separate model evaluating sexual violence as the exposure
CI = Confidence Interval
*Adjusted for: age, educational level, income, country of origin, years lived in Côte d’Ivoire (all as categorical variables). Covariates were selected using a DAG for each model (Supplementary material 1)
**Statistically significant (p < 0.05)
Discussion
This study aimed to describe the prevalence of sexual violence among female sex workers in Côte d’Ivoire, and to investigate the relationship between experiences of sexual violence and adverse mental health and substance use outcomes. Findings confirm that sexual violence is common and widespread among female sex workers in Côte d’Ivoire. Within our study population, nearly one in three participants had experienced sexual violence at some point in their lives, with many having experienced it within the last year. Women who had experienced sexual violence were more likely to report suicidal ideation, as well as substance use in the form of daily alcohol use and illegal drug use within the last 12 months.
The high prevalence of sexual violence found in this study reflects a similarly high burden of violence reported previously among female sex workers in Côte d’Ivoire and in neighboring countries such as Togo and Burkina Faso [1, 10]. These high rates of sexual violence pose a great threat to the sexual autonomy and human rights of sex workers, and are likely in part due to the social, legal, and economic environment within which sex workers practice [10]. Previously, interventions focusing on generating empathy towards sex workers among police, the legal system and the media, and on mobilizing sex workers to form communities and learn about their legal rights resulted in a reduction in violence [8]. Similarly, decriminalization reforms in other countries have been found to reduce violence against sex workers and to increase the rates of reporting this violence [14]. Sex workers in Côte d’Ivoire may benefit from similar structural changes within their legal and social environment, which could enable them to seek additional protections, legal resources, and social support [6, 16, 29].
Women who experienced sexual violence were more likely to report illicit substance use within the past 12 months, which may be a downstream consequence of mental health outcomes, further reinforcing the known harms of sexual violence in this community. Daily alcohol consumption was also more frequent among those that reported experiences of sexual violence, although this association did not remain significant in adjusted analyses. Across sub-Saharan Africa, research has shown significant substance use among the female sex worker community, with alcohol and other substances being recognized as a way in which women are able to cope with day-to-day stressors associated with sex work [30–33]. Among female sex workers who experience violence, this may be one factor leading to increased alcohol consumption.
This relationship between sexual violence and substance use outcomes has important implications for support service needs and indicates that substance use counseling efforts should target this population. Effective harm-reduction strategies may include initiatives such as safe support spaces and support groups, providing women with spaces where they can come together as a community and seek mutual support [34]. Providing female sex workers, and particularly those who are survivors of sexual violence, with targeted mental health, social, and clinical services is also key in addressing these mental health and downstream substance use outcomes [2, 34].
The association between sexual violence perpetrated towards sex workers and the resulting decreased access to support and health resources highlights the importance of targeting female sex workers with violence prevention and substance use support services as a human rights concern. It has previously been widely explored how fear of stigma and shame can detrimentally affect women’s likelihood to report sexual violence [35]. It is likely that these factors are also negatively affecting female sex workers’ ease of accessing preventative healthcare and support services.
Sexual violence may also lead to an increased risk of HIV acquisition for sex workers [29, 36]. This could partially be due to sexual violence and substance use often being linked to decreased protective behaviors such as condom use [37]. Studies performed in Kenya estimated that eliminating sexual violence could help avert up to 17% of HIV infections in the country through its effect on condom use among female sex workers and their clients [29]. This result together with previous research, shows the importance of targeting female sex workers with violence prevention and substance use support services as part of efforts to curb the global HIV epidemic. Other types of interventions, such as cash transfers and peer health initiatives or other programs incentivizing condom use and creating support systems and safe medical spaces, may also help address the decreased rates of condom use reported among those who had experienced sexual violence and among all sex workers more generally [38–40].
Participants who had experienced sexual violence also had increased odds of reporting a history of suicidal ideation, further suggesting an acute need for mental health resources geared towards female sex workers. This group of participants was also significantly more likely to have spoken to a counselor or confidant about their feelings, signifying women’s prioritization of social support over criminal justice support after sexual violence experiences. These mental health issues may also impede female sex workers’ ability to seek HIV prevention and treatment services [9]. Sexual violence is also linked to gender and relationship power inequity, which in turn often leads to psychological distress and a set of control dynamics that diminish a person’s ability to negotiate for safer sex [36]. A study conducted in South Africa established a temporal relationship between intimate partner violence and increased HIV risk, suggesting that violence and the associated power inequity precede the increased risk for unsafe practices such as condomless sex among sex workers [36]. This may in part be explained by the mental health and substance use associations with sexual violence that were found in this analysis.
Limitations
This study had several limitations. Recruitment was conducted using respondent-driven sampling, a methodology that relies on social networks. It is possible that some groups of female sex workers may have been excluded if they were not a part of the social networks reached. However, similar methodologies and questionnaires have been used successfully within similar populations [10, 41, 42]. Furthermore, not all participants in the survey had RDS weight data available, and thus were excluded from the weighted analysis. This may have led to bias in the weighted results. However, a comparison of the participants with RDS weights available to the overall sample showed that these two groups did not differ significantly in terms of any relevant variables (including sociodemographic, experiences of sexual and physical violence, sex work conditions, mental health, substance use, and HIV and condom use variables). Thus, the potential bias from the missing RDS weights is likely minimal. The only characteristic in which the two groups varied was region of residence, indicating potential challenges with recruitment in certain regions (notably Katiola).
Data were collected cross sectionally, and we were unable to determine whether experiences of sexual violence preceded other health outcomes, including mental health and substance use. This lack of temporality between the exposure and the outcomes means that additional pathways not described here may play a role in the relationships found, including the possibility for a reverse relationship between mental health and substance use, and violence outcomes. Further, effect estimates may be biased due to unmeasured confounding. Additionally, this study did not use a formal AUDIT score or depression scale to evaluate substance use and mental health outcomes, which may have introduced some measurement error. The stigma and legal environment surrounding sex work may have affected participants’ willingness to respond to certain questions and thus the reliability of these data. This is exacerbated by the personal and sensitive nature of much of the data collected. Further, survivorship bias may be affecting the results related to suicidal ideation and depression, given that we are only able to survey those that survived these mental health conditions. This could be leading to an underestimate of adverse mental health outcomes in this population.
Conclusion
The results of this study indicate that it is crucial for future violence prevention agendas to focus on constructing a legal and social environment that allows sex workers to seek protection, health resources, and social support after experiencing sexual violence. The high prevalence of sexual violence among female sex workers in Côte D’Ivoire and the associations of sexual violence with poor mental health and substance use outcomes has important human rights and public health implications. Poor mental health and substance use have also previously been found to be associated with inconsistent condom use, and thus have important implications for sexual health outcomes and HIV acquisition risk [9]. Taken together, these findings highlight the need for programmatic and legal changes to mitigate the risks of sexual and gender-based violence affecting sex workers.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to acknowledge the contributions of the women who participated in this study.
Abbreviations
- aOR
Adjusted Odds Ratio
- AUDIT
Alcohol Use Disorders Identification Test
- CI
Confidence Interval
- DAG
Directed Acyclic Graph
- HIV
Human Immunodeficiency Virus
- IBBS
Integrated Bio-Behavioral Survey
- IQR
Interquartile Range
- OR
Odds Ratio
- PV
Physical Violence
- RDS
Respondent-Driven Sampling
- SV
Sexual Violence
- STI
Sexually Transmitted Infection
Author contributions
NGM, SB, KR, and CL contributed to the design of this analysis. NGM and HM conducted data analyses. NGM, CL, and KR were major contributors in writing this manuscript. NGM, NE, CL, GT, SB, and KR made substantial contributions to drafting and revising the work. SB, GT, IB, NT, EG, EO, and DD made substantial contributions to the acquisition of the data and design of the work. All authors read and approved the final manuscript.
Funding
This study was funded by the Global Fund and led by ENDA Santé Côte d’Ivoire, with technical assistance provided by ENDA Santé and Johns Hopkins University. KR was supported by an award from the National Institute of Mental Health (K01MH129226). SB was supported by an award from the National Institute of Allergy and Infectious Diseases (R01AI170249). The content is solely the responsibility of the authors and does not necessarily reflect the official views of the funding agencies.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All data were collected in accordance to established national ethical guidelines set by the Côte d’Ivoire National Ethics Committee (Comité National d’Ethique des Sciences de la Vie et de la Santé la de Côte d’Ivoire). Ethical approval for data collection and processing was obtained from the Côte d’Ivoire National Ethics Committee (Comité National d’Ethique des Sciences de la Vie et de la Santé la de Côte d’Ivoire). This secondary analysis used only anonymized data at all stages, and the authors conducting the analysis did not have access to identifiable data. Written informed consent was obtained from all participants of the study. As part of the informed consent process, participants were informed of their rights, including their right to withdraw from the study at any point.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wirtz AL, Schwartz S, Ketende S, Anato S, Nadedjo FD, Ouedraogo HG et al. Sexual Violence, Condom Negotiation, and Condom Use in the Context of Sex Work. JAIDS J Acquir Immune Defic Syndr. 2015 Mar 1 [cited 2021 Feb 11];68(Supplement 2):S171–9. https://journals.lww.com/00126334-201503011-00014 [DOI] [PubMed]
- 2.Sherwood JA, Grosso A, Decker MR, Peitzmeier S, Papworth E, Diouf D et al. Sexual violence against female sex workers in the Gambia: A cross-sectional examination of the associations between victimization and reproductive, sexual and mental health. BMC Public Health. 2015 [cited 2021 Feb 11];15(1). /pmc/articles/PMC4375842/ [DOI] [PMC free article] [PubMed]
- 3.Shannon K, Goldenberg SM, Deering KN, Strathdee SA. HIV infection among female sex workers in concentrated and high prevalence epidemics: Why a structural determinants framework is needed. Vol. 9, Current Opinion in HIV and AIDS. NIH Public Access; 2014 [cited 2021 Feb 11]. pp. 174–82. /pmc/articles/PMC4286412/ [DOI] [PMC free article] [PubMed]
- 4.Schwitters A, Swaminathan M, Serwadda D, Muyonga M, Shiraishi RW, Benech I et al. Prevalence of Rape and Client-Initiated Gender-Based Violence Among Female Sex Workers: Kampala, Uganda, 2012. AIDS Behav. 2015 [cited 2021 Feb 11];19(1):68–76. Available from: http://www.pmc/articles/PMC4724433/ [DOI] [PMC free article] [PubMed]
- 5.Mendoza C, Barrington C, Donastorg Y, Perez M, Fleming PJ, Decker MR et al. Violence From a Sexual Partner is Significantly Associated With Poor HIV Care and Treatment Outcomes Among Female Sex Workers in the Dominican Republic. JAIDS J Acquir Immune Defic Syndr. 2017 Mar 1 [cited 2021 Feb 11];74(3):273–8. https://journals.lww.com/00126334-201703010-00005 [DOI] [PubMed]
- 6.Deering KN, Amin A, Shoveller J, Nesbitt A, Garcia-Moreno C, Duff P, American Journal of Public Health. A systematic review of the correlates of violence against sex workers. Vol. 104,. American Public Health Association Inc.; 2014 [cited 2021 Feb 11]. p. e42. /pmc/articles/PMC3987574/ [DOI] [PMC free article] [PubMed]
- 7.Decker MR, Crago AL, Chu SKH, Sherman SG, Seshu MS, Buthelezi K et al. Human rights violations against sex workers: Burden and effect on HIV. Vol. 385, The Lancet. Lancet Publishing Group; 2015 [cited 2021 Feb 11]. pp. 186–99. 10.1016/S0140-6736(14)60800-X [DOI] [PMC free article] [PubMed]
- 8.Beattie TS, Bhattacharjee P, Ramesh B, Gurnani V, Anthony J, Isac S et al. Violence against female sex workers in Karnataka state, south India: Impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010 [cited 2021 Feb 11];10:476. /pmc/articles/PMC2931467/ [DOI] [PMC free article] [PubMed]
- 9.Abelson A, Lyons C, Decker M, Ketende S, Mfochive Njindam I, Fouda G et al. Lifetime experiences of gender-based violence, depression and condom use among female sex workers in Cameroon. Int J Soc Psychiatry. 2019 Sep 1 [cited 2021 Feb 11];65(6):445–57. http://journals.sagepub.com10.1177/0020764019858646 [DOI] [PubMed]
- 10.Lyons CE, Grosso A, Drame FM, Ketende S, Diouf D, Ba I et al. Physical and sexual violence affecting female sex workers in Abidjan, côte d’ivoire: Prevalence, and the relationship with the work environment, HIV, and access to health services. J Acquir Immune Defic Syndr. 2017 [cited 2021 Feb 11];75(1):9–17. https://pubmed.ncbi.nlm.nih.gov/28169873/ [DOI] [PMC free article] [PubMed]
- 11.Institut National de la Statistique-INS, ICF. Enquête Démographique et de Santé de Côte d’Ivoire, 2021. Rockville, Maryland, USA. 2023. https://dhsprogram.com/publications/publication-FR385-DHS-Final-Reports.cfm
- 12.Erausquin JT, Reed E, Blankenship KM. Police-related experiences and HIV risk among female sex workers in Andhra Pradesh, India. J Infect Dis. 2011 Dec 1 [cited 2021 Feb 11];204(SUPPL. 5):S1223. http://www.pmc/articles/PMC4565555/ [DOI] [PMC free article] [PubMed]
- 13.Sirotin N, Strathdee SA, Lozada R, Abramovitz D, Semple SJ, Bucardo J et al. Effects of government registration on unprotected sex amongst female sex workers in Tijuana; Mexico. Int J Drug Policy. 2010 Nov [cited 2021 Feb 11];21(6):466–70. Available from: http://www.pmc/articles/PMC2991616/. [DOI] [PMC free article] [PubMed]
- 14.Decker MR, Crago A-L, Ka S, Chu H, Sherman SG, Seshu MS, The lancet series on HIV in sex workers; Paper 4 burden and HIV impact of human rights violations against sex workers HHS Public Access, et al. Lancet. 2015;385(9963):186–99. [DOI] [PMC free article] [PubMed]
- 15.Shannon K, Strathdee SA, Shoveller J, Rusch M, Kerr T, Tyndall MW. Structural and environmental barriers to condom use negotiation with clients among female sex workers: Implications for HIV-prevention strategies and policy. Am J Public Health. 2009 Apr 1 [cited 2021 Feb 11];99(4):659–65. Available from: http://www.pmc/articles/PMC2661482/. [DOI] [PMC free article] [PubMed]
- 16.Lyons CE, Schwartz SR, Murray SM, Shannon K, Diouf D, Mothopeng T et al. The role of sex work laws and stigmas in increasing HIV risks among sex workers. Nat Commun. 2020 Dec 1 [cited 2021 Feb 11];11(1). http://www.pmc/articles/PMC7028952/ [DOI] [PMC free article] [PubMed]
- 17.Institute of Development Studies. Sex Work Law - Countries. [cited 2021 Feb 11]. http://spl.ids.ac.uk/sexworklaw/countries
- 18.Namey E, Perry B, Headley J, Yao AK, Ouattara ML, Shighata C et al. Understanding the financial lives of female sex workers in Abidjan, Côte d’Ivoire: implications for economic strengthening interventions for HIV prevention. AIDS Care. 2018 Jul 25 [cited 2021 Feb 11];30(sup3):6–17. https://www.tandfonline.com/doi/full/10.1080/09540121.2018.1479031
- 19.Enda Santé Côte d’Ivoire. Etude, surveillance biologique et comportementale et cartographie en direction des ts À katiola agboville. yamoussoukro, soubré et divo, 2019. [cited 2021 Apr 15]. https://endasanteci.org/rechibbsts2019.php
- 20.Badowski G, Somera LP, Simsiman B, Lee H-R, Cassel K, Yamanaka A, et al. The efficacy of respondent-driven sampling for the health assessment of minority populations HHS Public Access. Cancer Epidemiol. 2017;50:214–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greiner AL, Albutt K, Rouhani SA, Scott J, Dombrowski K, Vanrooyen MJ et al. Practice of Epidemiology Respondent-Driven Sampling to Assess Outcomes of Sexual Violence: A Methodological Assessment. Am J Epidemiol. 2014 [cited 2022 Oct 14];180(5):536–44. http://www.kobotoolbox.org [DOI] [PubMed]
- 22.Mccreesh N, Frost S, Seeley J, Katongole J, Tarsh MN, Ndunguse R et al. Evaluation of Respondent-Driven Sampling. http://links.lww.com [DOI] [PMC free article] [PubMed]
- 23.Heckathorn D. Respondent Driven Sampling. Cornell University Department of Sociology. http://www.respondentdrivensampling.org/
- 24.Avery L, Rotondi N, McKnight C, Firestone M, Smylie J, Rotondi M. Unweighted regression models perform better than weighted regression techniques for respondent-driven sampling data: results from a simulation study. BMC Med Res Methodol. 2019;19(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sperandei S, Bastos LS, Ribeiro-Alves M, Reis A, Bastos FI. Assessing logistic regression applied to respondent-driven sampling studies: a simulation study with an application to empirical data. Int J Soc Res Methodol. 2023;26(3):319–33. 10.1080/13645579.2022.2031153
- 26.Schonlau M, Liebau E. Respondent-driven sampling. Stata J. 2012;12(1):72–93. [Google Scholar]
- 27.StataCorp. Stata statistical software: Release 15. College Station, TX: StataCorp LLC; 2017. https://www.stata.com/
- 28.Wirtz AL, Mehta SH, Latkin C, Zelaya CE, Galai N, Peryshkina A, et al. Comparison of respondent driven sampling estimators to determine HIV prevalence and population characteristics among men who have sex with men in Moscow, Russia. PLoS ONE. 2016;11(6):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shannon K, Strathdee SA, Goldenberg SM, Duff P, Mwangi P, Rusakova M et al. Global epidemiology of HIV among female sex workers: Influence of structural determinants. Vol. 385, The Lancet. Lancet Publishing Group; 2015 [cited 2021 Feb 11]. pp. 55–71. http://www.pmc/articles/PMC4297548/ [DOI] [PMC free article] [PubMed]
- 30.Nelson EUE. Structural inequities, HIV vulnerability and women’s agency: Street-based sex workers in Nigeria. Glob Public Health. 2020;1800–9. 10.1080/17441692.2020.1791211 [DOI] [PubMed]
- 31.Panneh M, Gafos M, Nyariki E, Liku J, Shah P, Wanjiru R, et al. Mental health challenges and perceived risks among female sex workers in Nairobi, Kenya. BMC Public Health. 2022;22(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parmley LE, Comins CA, Young K, Mcingana M, Phetlhu DR, Guddera V, et al. Occupational barriers to accessing and adhering to antiretroviral therapy for female sex workers living with HIV in South Africa. Occup Env Med. 2020;77(2):100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lancaster KE, Go VF, Lungu T, Mmodzi P, Hosseinipour MC, Chadwick K et al. Substance use and HIV infection awareness among HIV-infected female sex workesr in Lilongwe, Malawi. Int J Drug Policy. 2016;(30):124–31. [DOI] [PMC free article] [PubMed]
- 34.Lim S, Peitzmeier S, Cange C, Papworth E, LeBreton M, Tamoufe U et al. Violence Against Female Sex Workers in Cameroon. JAIDS J Acquir Immune Defic Syndr. 2015 Mar 1 [cited 2021 Feb 11];68(Supplement 2):S241–7. https://journals.lww.com/00126334-201503011-00022 [DOI] [PubMed]
- 35.Dessalegn Muluneh M, Stulz V, Francis L, Agho K. Gender based violence against women in Sub-saharan Africa: a systematic review and Meta-analysis of cross-sectional studies. [cited 2021 Feb 11]; Available from: http://www.mdpi.com/journal/ijerph [DOI] [PMC free article] [PubMed]
- 36.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. Lancet. 2010 Jul 3 [cited 2021 Feb 11];376(9734):41–8. Available from: http://www.thelancet.com. [DOI] [PubMed]
- 37.Onyango MA, Adu-Sarkodie Y, Agyarko-Poku T, Asafo MK, Sylvester J, Wondergem P et al. It’s All About Making a Life. JAIDS J Acquir Immune Defic Syndr. 2015 Mar 1 [cited 2021 Feb 11];68(Supplement 2):S131–7. https://journals.lww.com/00126334-201503011-00009 [DOI] [PubMed]
- 38.Packel LJ, de Walque D, Feeney KC, Balampama MP, Cooper JE, Kalolella A et al. A randomized trial of cash incentives for sexual behavior change among female sex workers in Dar es Salaam. Soc Sci Med. 2021;272. [DOI] [PubMed]
- 39.Stoner MCD, Kilburn K, Hill LM, Macphail C, Kimaru L, Khoza N, et al. The effects of a cash transfer intervention on sexual partnerships and HIV in the HPTN 068 study in South Africa. Cult Heal Sex. 2020;22(10):1112–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson L, Potter LC, Beeching H, Bradbury M, Matos B, Sumner G et al. Interventions to improve health and the determinants of health among sex workers in high-income countries: a systematic review. Lancet Public Heal. 2023;8(2):e141–54. 10.1016/S2468-2667(22)00252-3 [DOI] [PMC free article] [PubMed]
- 41.Gorin EM, Lyons CE, Jarrett BA, Djalo MA, Barreto K, Drame FM et al. Mobility and HIV vulnerabilities among female sex workers in Guinea-Bissau: findings from an integrated bio-behavioral survey. BMC Public Health. 2023;23(1):1–12. 10.1186/s12889-023-16744-y [DOI] [PMC free article] [PubMed]
- 42.Rao A, Schwartz S, Billong SC, Bowring A, Fouda G, Ndonko F, et al. Predictors of early childhood HIV testing among children of sex workers living with HIV in Cameroon. BMC Public Health. 2019;19(Suppl 1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.