Abstract
Background
Adult day programs aim to facilitate aging in place by supporting the health and well-being of persons with dementia and providing respite to their caregivers. However, studies on the effects of day programs are inconclusive, and we especially lack insights into the context conditions and mechanisms of day programs that may produce different outcomes for different groups of persons with dementia and their caregivers. Our objective was to conduct a realist review, synthesizing research on day programs to develop program theories explaining how and why day programs do or do not produce positive or negative outcomes for different groups of persons with dementia, and caregivers.
Methods
We identified 14 literature reviews (including 329 references published between 1975 and 2021) on adult day programs. From this initial pool of studies, we will include those that focused on day program attendees with dementia or meaningful cognitive impairment, and/or their caregivers, and that report how day program contexts (C) and mechanisms (M) bring about outcomes (O) for attendees and caregivers. We will extract CMO statements (i.e., narratives that explain how and why day programs do or do not bring about certain outcomes for whom and under what circumstances). Using additional focused searches, citation mapping, citation tracking, and discussions with our researcher and expert team members, we will identify additional references. CMO statements will be synthesized, transformed into hypotheses, and linked and visualized to form program theories. Using focus groups and the James Lind Alliance Priority Setting Partnership method, we will discuss and prioritize our CMO statements and refine our program theories with 32 experts (older adults, caregivers, Alzheimer societies, caregiver organizations, day program staff and managers, and health system and policy decision makers).
Discussion
By identifying essential elements and processes of day programs and related knowledge gaps, this study will generate much-needed knowledge to leverage the full potential of day programs so they can provide appropriate care, preventing premature institutionalization, and unnecessary acute and primary care use. This will ultimately improve the quality of life of persons with dementia and their caregivers, alleviate caregiver burden, and reduce social costs.
Systematic review registration
PROSPERO CRD42024504030
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-024-02683-1.
Keywords: Realist review, Adult day programs, Persons living with dementia, Family/friend caregivers
Background
The health and well-being of people living with dementia and their family/friend caregivers (herein referred to as caregivers) are essential areas of healthcare reform in Canada and globally [1–5]. Caring for someone with dementia often causes distress, diminishing the health and well-being of the person with dementia and increasing costs to society incurred by potentially unwarranted emergency and hospital visits and/or premature admissions to residential long-term care (LTC) [6–14]. Addressing these challenges and prioritizing the care, health, and well-being of those with dementia and their caregivers is pivotal in the development of public health policy and resource distribution at the community level [1, 15–17].
In 2020, almost 600,000 individuals lived with dementia in Canada, 62% of whom were women and 21% of whom were newly diagnosed in that year [1]. By 2030, these numbers will nearly double, and by 2050 almost triple [1]. This matches global trends, with an estimated 57.4 million people living with dementia in 2019 and a predicted increase of this number to 153 million in 2050 [18]. Global spending attributable to dementia was $263 billion in 2019 with an expected exponential growth to $1.6 trillion by 2050 (11% of total healthcare expenditures) [19]. Dementia is caused by a number of neurodegenerative, vascular, or other diseases [20, 21], often linked with multiple pathologies. It is progressive, irreversible, and associated with neuropsychiatric symptoms (e.g., delusions, aggression, wandering) [22], and declining cognitive and functional abilities [20, 21]. Persons with dementia are at high risk for social isolation and loneliness due to interpersonal stigma, exclusionary continuing care services and policies, and increased support needs, negatively affecting their human rights, health, and well-being [23]. Persons living with dementia in the community often have multiple chronic conditions and complex care needs [24, 25]. 25% have a severe cognitive impairment, 28% require extensive assistance with activities of daily living, 25% exhibit behavioral symptoms and 25% have signs of depression [26], all of which increase the risk for admissions to long-term institutional care [27–29]. Healthcare systems across the globe have implemented aging-in-place policies, aiming to reduce admissions to LTC and to increase the time spent in the community [3, 30–33]. However, 10% of admissions to LTC in Canada (up to 30% in some places) have care needs that could have potentially been met in the community [34–36], highlighting the critical role of caregivers and appropriate community-based services.
Worldwide, 84% of those with dementia (almost 40 million people) live at home, largely supported by caregivers providing a total of 82.1 billion care hours per year (5.7 h/day and 2089 h/year for every person with dementia) [37]. While caregiving can be highly rewarding, caregivers are at high risk of caregiver burden. For example, 70% of Canadian caregivers report negative effects of caregiving, including feeling tired (55.5%), worried/anxious (44%), overwhelmed (36.9%), short-tempered/irritable (30.8%), or having disturbed sleep (29.1%) [11]. In the USA, 59% of caregivers of persons with dementia report high or very high emotional stress, and 30–40% have symptoms of depression [38]. Worldwide, 71% of unpaid care of persons with dementia is provided by women [37], and women, as well as racialized caregivers, are at significantly higher risk for caregiver burden [39, 40]. With health system efforts to retain older adults in the community longer, combined with increasingly complex care needs, caregiver burden has substantially increased [6–10]. At the same time, the number of available caregivers has declined and is expected to do so further in the future [13, 38, 40]. Therefore, to enable older adults with dementia to remain in the community safely and well for as long as possible, we urgently need support (especially those supporting social inclusion) that targets both, persons with dementia and their caregivers.
Adult day programs are one of the few continuing care options designed to meet these dual demands. Day programs are care settings that employ care staff and admit people with some support needs [41, 42], setting them apart from senior or community centers [43] and creative arts programs [44]. Unlike home care [45] or in-home respite [46], day programs serve groups of individuals in a setting external to the person’s home [41, 42] supporting social interactions and caregiver respite [47]. Unlike geriatric day hospitals, which provide medical, therapeutic, and rehabilitative care for a few weeks [48], day programs prioritize social and recreational activities, and they do so long-term (for months or years) [41, 42]. Since their origins (e.g., 1950s in the UK, 1960s in the Netherlands, and 1970s in the USA) and since the initial research studies in the 1970s [49, 50], day programs have received increasing attention for their potential to support aging in place [42, 49, 51]. An initial literature search on adult day programs identified 14 systematically conducted literature reviews [41, 42, 46, 47, 49, 52–60], including 329 international studies (most from the USA), published between 1975 and 2021 (most > 10 years old). These largely quasi-experimental studies mostly focus on older adult day program attendees in general, and rarely on those with dementia specifically. They suggest that, compared to non-attendees, attendees had fewer mental health issues (e.g., depression, loneliness), better cognition, quality of life (QoL), subjective health, physical health, and physical functioning. Attendees took fewer medications, entered care homes later, were hospitalized less frequently, and had lower mortality. Positive effects on caregivers included reduced stress, conflicts, worries, and depression, improved mental health, well-being, and confidence in managing behavioral symptoms. However, the findings were inconsistent. For example, two quasi-experimental studies found decreased levels of depression among day program attendees [61, 62], while a randomized controlled study found no such effect [63]. Some studies suggested delayed admissions to care homes [64, 65], while others found they accelerated this outcome [47].
Traditional day program research has mostly followed a causal XO-model, assuming that an intervention (X) (day programs) leads to an outcome (O) (e.g., less depression, caregiver distress, public costs). However, XO-models do not account for the complexity of day programs, nor do they explain “how” or “why” a particular day program works (or fails to work)—a major knowledge gap of current day program research [42, 44, 52]. Expanding the traditional XO-model, realist reviews ask what contexts (C) and mechanisms (M) explain how and why X does or does not lead to O, so the XO-model becomes a CMO model [66–69]. Context refers to the social conditions in which day programs operate (e.g., social/economic/political structures, geographical location, historical developments, day program characteristics and processes, characteristics/roles/relationships of day program clients, caregivers, and staff) [66–70]. Mechanisms produce outcomes within particular contexts [66–69, 71]. They do so, for example, through individual or collective reasoning, choices, and (re)actions that are not directly observable, but accessible through theory building and testing [66–69, 71]. For example, an ethnographic study [72] found that a home-like environment that reminded individuals with dementia of their past (and staff dressing and acting accordingly) (C) helped clients feel comfortable, safe, and calm (M), reducing the outcome (O) of behavioral symptoms. In contrast, a hospital-like environment (with staff dressed in care uniforms and enacting a nurse-patient relationship) (C) led to feelings of discomfort and anxiety (M), increasing behavioral symptoms (O). Concerns have also been raised about access barriers, especially for equity-deserving groups (e.g., sexual and gender minorities, racialized individuals, immigrants) [52, 54, 56, 58], and about a disconnect between day programs and other continuing care options [42], yet such contexts and mechanisms remain under-explored. The purpose of our realist review is to synthesize such studies into program theories on how and why day programs bring about different effects on different groups of people with dementia, caregivers, and health systems, which—to the best of our knowledge—has not been done before. Day program research, policy, and practice are under-theorized, but such theory is required to better understand and improve the effects of day programs.
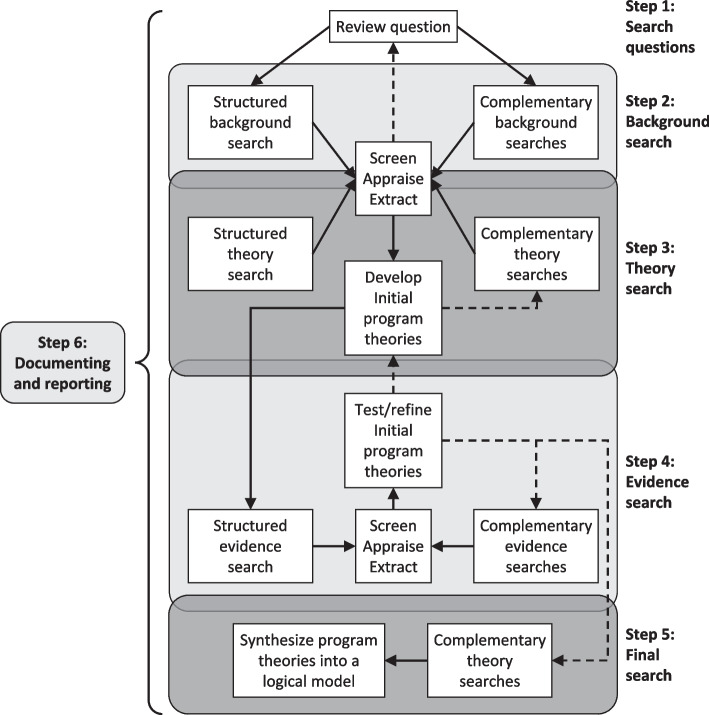
Design and methods
In this 2-year project (August 2023 to July 2025), we will apply a realist approach [66–69] to synthesizing evidence and developing and testing program theories on day programs. Realist reviews are specifically designed to overcome the limitations of traditional systematic reviews [66–69, 73]. Systematic reviews are challenged to account for the complexity of dynamic, multi-faceted social interventions (such as day programs), they typically evaluate (and are better suited to evaluate) “if” an intervention works, rather than “how” and “why”. Rooted in critical realism, the realist approach assumes that (1) causal explanations are achievable, (2) social reality is mainly an interpretative reality of social actors, and (3) social actors evaluate and act upon their social reality [73]. Guided by these assumptions, realist reviews differ from systematic reviews in several important ways [73]. Experts (i.e., people with lived experience and knowledge users) are involved in all stages of the review. In our review, using an integrated knowledge translation (iKT) approach [74, 75], we have collaborated with a cross-Canadian group of 32 experts in preparing this protocol, and we will continue to do so throughout the project. Experts include older adults, some of them living with dementia, their caregivers, representatives of Alzheimer Societies and caregiver organizations, day program staff and managers, and government and health system decision-makers. Evidence searches and appraisals are purposive, theoretically driven, interpretive, and cyclical, aiming to develop and refine theory. Evidence includes a broad range of sources, such as peer-reviewed research, grey literature, theory, and expert knowledge. This protocol was guided by the sections applicable to realist reviews of the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P, Additional file 1) [76], and it is registered with PROSPERO (CRD42024504030). Following well-established realist review guidelines [69, 77], our study will include six iterative and overlapping steps (Fig. 1).
Fig. 1.
Six iterative and overlapping steps
Step 1: formulate specific questions as lines of enquiry
In collaboration with our experts, we have completed this step. Settings will include adult day programs that care for individuals with dementia exclusively (dementia-specific) or in addition to other attendees (dementia-inclusive). Populations will be day program attendees with dementia or meaningful cognitive impairment and their caregivers. Our team has agreed on two specific research questions:
In what contexts and by what mechanisms do day programs produce (or not produce) which kinds of positive or negative outcomes for which groups of persons with dementia, and caregivers?
What theories underlie these CMO constellations and are they able to explain how and why contexts and mechanisms do or do not produce outcomes?
These lines of enquiry will be refined and extended as needed, based on the subsequent steps.
Step 2: conduct a background search to scope the international literature
This preliminary work is critical to prepare for the subsequent steps of a realist review. Its purpose is to “scope” the international literature and to develop an understanding of its quantity and quality [77]. With the assistance of a librarian scientist, we searched the database of MEDLINE via Ovid® in August 2023 for systematically conducted literature reviews, combining various search terms related to the concepts (and various synonyms) of day programs, older adults, dementia, and caregivers (see Additional file 2 for detailed information on the search). Systematic inclusion/exclusion screening and quality appraisal are not usually part of a realist review background search [77], but we will conduct systematic focused searches at a later stage and evaluate the methodological quality of included studies (step 4). Applying our definitions of adult day programs, attendees with dementia and their caregivers, two team members independently screened titles, abstracts, and if needed, full-texts of 892 references and resolved discrepancies by consensus (August–September 2023). They identified 14 relevant reviews [41, 42, 46, 47, 49, 52–60] that included a total of 329 references (Additional file 3). These references cover a breadth of approaches and perspectives, including integrative [52, 54, 55], systematic [46, 47, 49, 57, 59, 60], problematization-based [42], and scoping [41, 53, 56, 58] reviews, as well as original studies applying quantitative, qualitative, and mixed methods designs.
Using Covidence for managing our references, our team is currently mapping this initial pool of studies to identify the diverse perspectives, theories, and approaches to examining day programs, as well as key papers [77]. To identify additional references, we will employ strategies commonly used in realist background searches, including citation mapping, citation tracking, and discussions with our researcher and expert team members [78]. Using Zoom, we are meeting with our researchers every 2 weeks, and with our experts in the alternating weeks to discuss the progress, key references and their implications, our state of knowledge, and important gaps. Separate meetings increase the feasibility and give room to different perspectives. We are meeting with the whole team every 8 weeks to ensure an exchange of perspectives. This helps to refine and extend the initial research questions (see step 1).
Step 3: develop initial program theories
Since January 2024 (to be completed in August 2024), we have screened references identified in step 2 for suitable CMO statements and for formal theories that can explain how and why day programs do or do not work for who and under what circumstances [77]. These CMO statements and formal theories will be the basis for our initial program theories (to be refined in the subsequent steps). CMO statements are hypotheses (framed as if–then-statements) on what contexts trigger what types of mechanisms, leading to which kinds of outcomes [69]. An example of a proposed CMO statement focusing on an outcome for a day program attendee with dementia might be:
If space in day programs is designed to resemble a home-like (vs a hospital-like) environment (C), then attendees with dementia are comforted by feelings of familiarity and safety (M), leading to reduced responsive behaviors (O).
An example, focusing on a caregiver outcome could be:
If social workers in a day program provide counseling, guidance, and support in navigating the continuing care system and in accessing resources to caregivers (C), then they feel more supported and less overwhelmed by the complexities of navigating continuing care systems (M), leading to reduced caregiver distress (O).
A statement focusing on health system outcomes could be:
If day program costs are publicly subsidized (vs privately paid in full) (C), then more people can access these services (M), increasing the number of people whose physical, emotional, and social care needs are addressed (O), reducing the risk of adverse events associated with unmet care needs (O), eventually leading to reduced acute, primary, and long-term institutional care use, and reduced public spending (O).
A program theory links multiple CMO statements, attempting to explain how different mechanisms are triggered in different contexts, generating different outcomes [69]. Often, more than one program theory is needed to cover all relevant aspects of an intervention. Program theories are different from “formal” or “substantive” theories. The latter include established theories of different domains or disciplines, aiming to explain certain phenomena in general (e.g., incentives theory in economics, constructivist learning theory in education, or complex adaptive systems theory in social sciences) [79]. In contrast, our program theories will specifically aim to explain how day program contexts and mechanisms bring about day program outcomes. Formal theory can help identify important contexts, mechanisms, and their linkages to outcomes (translating into CMO statements that are part of our program theories) and they can help explain how findings (especially those that seem disparate) fit together to inform program theories [79].
Data have been extracted on key realist components of contexts, mechanisms, and outcomes (each color-coded), with added levels of granularity supplied by the included literature [80]. We have developed definitions of CMO elements, examples of CMO statements, and instructions for identifying and extracting CMO statements and trained our team members using these resources (Additional file 4). Training included several calibration exercises [81] in which all team members extracted CMO statements of the same study with subsequent meetings to reconcile the statements, address any questions team members had, and refine guiding documents as needed. Subsequently, each of the two team members was assigned a study, extracted CMO statements from that study, and reconciled discrepancies by consensus. Difficult decisions have been brought forward to the larger research team for discussion and resolution.
In addition to the references identified in our initial search, we will conduct several focused searches to determine how each identified mechanism influences outcomes in various contexts. We will develop and use a meta-framework for data synthesis. This framework will ensure that data are collected and synthesized in a consistent way to maximize the value of comparisons between day programs [80]. Data synthesis will also involve reflection and intensive discussion within the team. We will explore how different CMO statements may be linked, and how similar CMO statements can be combined, and we will synthesize linked CMO statements into initial program theories. We will continue the Zoom meetings with researchers and experts to discuss and refine the emerging list of CMO statements and initial program theories.
Step 4: test and refine the program theories
This step (September to November 2024) will start with a series of Zoom-based focus groups with our experts, in which we will apply realist interviewing [82–86] to discuss, further test, refine, and extend the initial program theories derived in the previous step. We will conduct a separate focus group with each (1) older adults (some with dementia) and caregivers, (2) day program staff and managers, and (3) advocates and decision-makers. In an iterative process, we will incorporate findings from these focus groups into our program theories, determine additional needs for information, and then conduct additional focus groups. We will use semi-structured focus group guides, record focus groups, and transcribe them verbatim via Zoom. Focus group guides will be similar across groups but use group-specific questions and wording as needed, and—for the later focus groups—guides will be adjusted to include revised or additional questions informed by the previous work)We will start by asking some general questions about the participants’ backgrounds and roles, followed by presenting visuals of our initial program theories to participants [82, 83, 86]. We will then discuss these program theories with participants, using a set of basic questions, which were adapted from Westhorp and Manzano’s [87] recommendations. Examples of these questions include.
What do you consider an outcome of the day program you have been attending (or that the person you care for has been attending, or that you work in, or that you are overseeing—depending on the group of persons participating in the focus group)?
Can you give an example of such an outcome (or outcomes)?
Are the outcomes different for different groups of day program attendees, caregivers, staff, managers?
What do you think has caused, or helped to cause the outcome you just identified, and how has that happened?
In an iterative process, called the teacher-learner cycle [82–86], participants will confirm, deny, or refine elements of the theory (i.e., contexts, mechanisms, outcomes), and the proposed relationships among these elements. Using NVivo software and applying configure realist analysis [85, 88–90], we will identify and code participant statements that reflect CMO elements and their linkages. Memos will elaborate on each of the identified CMO configurations. Based on these findings, we will update the list of CMO statements and resulting initial program theories generated in step 3.
Using the studies identified in the background search and conducting additional systematic searches in the databases of Embase, MEDLINE, ProQuest, CINAHL, Web of Science, and Scopus, we will then explore to what extent empirical evidence supports or refutes each of our CMO statements and program theories. Guided by a research librarian, we will develop purposeful search strategies and extend the search described in step 2 to identify additional evidence related to each CMO statement and program theory. We will also use CLUSTER searching (Citation tracking, tracing Lead authors, identifying Unpublished materials, Google Scholar searching, Theory tracking, ancestry searching for Early examples, and follow-up of Related projects). This strategy is specifically designed for searches at advanced stages of a realist review [91]. We will also retrieve grey literature and regulatory/policy documents, and examine white papers, editorials, reports, and guidelines describing the operations, policies, practice, and scheduling of day programs, through diverse approaches: searches in bibliographic databases, web engine searches, and examination of websites of organizations. The librarian will facilitate access to the bibliographic databases that index grey literature. Our partners may grant access to their organizations’ program materials. These search approaches will continue until theoretical saturation is met. We will identify “landmark” texts and main research traditions associated with day programs, and then annotate selected texts to create an evidence framework. Iterative, explicit searching will create a pool of data extensive enough to support CMO statements and program theories [92].
Quality appraisal in realist reviews is primarily interpretive [69, 77]. It includes an assessment of the source’s relevance, richness, and rigor [93]. A source’s relevance to this realist synthesis will depend on whether information can be extracted on contexts and mechanisms of day programs (even though the reference may not explicitly use this terminology) and how they produce outcomes for persons with dementia and/or their caregivers [93]. A source’s richness refers to the degree to which this source (a) can theoretically and conceptually explain how day programs are expected to work (conceptual richness), and (b) provides sufficient details to establish what is occurring in day programs and in their wider context, and whether these findings can be generalized across people, places, situations, or environments (contextual thickness) [93]. Finally, rigor refers to the quality of the study design and methods, and the trustworthiness of the study findings [93]. To assess relevance and richness, we will adapt study appraisal questions previously employed in realist syntheses [94]. To assess the rigor of theories, theoretical models/frameworks, theoretical discussions, etc. we will assess the logical coherence of the theoretical elements discussed. To assess the rigor of empirical studies, we will use traditional methodological quality checklists. Rather than determining a study’s rigor based on traditional (and outdated) evidence hierarchy considerations (which usually consider meta-analyses of randomized control trials, followed by individual randomized controlled trials the highest level of evidence), we will use checklists that were specifically developed and validated to assess quality criteria relevant to specific study designs: (1) Quality Assessment Tool for Quantitative Studies (QATQS) for intervention studies with or without a control group and with or without randomized allocation of participants [95, 96], (2) The Newcastle–Ottawa Scale (NOS) for cohort studies or case–control studies [97], (3) Appraisal tool for Cross-Sectional Studies (AXIS) [98], (4) Critical Appraisal Skills Program (CASP) Qualitative Studies Checklist [99], (5) Mixed Methods Appraisal Tool (MMAT) [100]. Since even studies with some methodological issues may contain important “nuggets of wisdom” [94], we will not exclude studies based on their level of rigor, but rather use that information to contextualize CMO statements (e.g., to tone down the strength of a conclusion proposed by a study whose rigor does not support such a strong conclusion). Each relevance, richness, and rigor will be independently assessed by two team members, discrepancies will be reconciled by consensus, and difficult decisions will be brought forward to the larger research team. The research team will discuss the relevance, richness, and rigor of sources for each identified CMO statement and program theory [67]. This will allow us to explore confirmatory and contradictory findings in relation to our hypotheses [101]. We will calibrate the relevance, richness, and rigor of about 5% of the papers retrieved to ensure accuracy and consistency before breaking into dyads. In our team discussions, we will question the integrity of each CMO statement and program theory by examining the degree to which it is supported by evidence. We may also adjudicate between competing CMO statements and program theories, consider the same-day program in different contexts, or ask our experts to reflect on a CMO statement or program theory based on their lived experiences [102]. Through this iterative synthesis process, our initial program theories will be condensed and refined.
Step 5: finalize program theories and derive priority recommendations for research, policy, and practice
In this step (December 2024 to April 2025) we will prioritize and further contextualize our refined program theories generated in step 4, and discuss and agree on priority recommendations for research, policy, and practice. We will use an adapted version of the James Lind Alliance Priority Setting Partnership method [103–106], which—unlike other consensus methods (e.g., Delphi panels) —is specifically designed to engage individuals with lived experience (including persons with dementia and their caregivers) in prioritizing and contextualizing research findings. First, we will develop and disseminate an online survey, asking each of our researchers and expert team members to rate (1) the perceived relevance of each of the CMO statements on a 5-point Likert scale from not relevant at all to highly relevant, and (2) the perceived actionability (how easily can the issue be addressed/improved) on a 5-point Likert scale from not actionable at all to highly actionable. We will descriptively analyze and visualize the survey results and we will share the results with team members ahead of our final workshop. In a 4-h Zoom-based workshop, facilitated by the York University Centre for Aging Research and Education, we will discuss, contextualize, and prioritize the findings. The workshop agenda will be highly structured, and we will prioritize CMO statements, using the Nominal Group Technique [107]. To allow each group member to express their views and to minimize the risk of individual members dominating the discussion, each group member will state their opinion, without justification or explanation. Once each team member has had a turn, we will follow up with a moderated discussion, concluded by voting or ranking with structured group discussions. We will first give a summary presentation on the project overall, on the project findings (CMO statements, program theories) and on the ranking results. Then we will divide participants into small groups, in which participants will share their top and bottom three CMO-statements and the respective rationales. Groups will include individuals of similar backgrounds to minimize power imbalances. This will ensure that each person has dedicated time to talk and feels comfortable sharing their views. Each group will then rank the list of CMO statements. During a break we will aggregate these rankings and, after the break, share and discuss these results with the group. Any changes will be voted on electronically and anonymously with majority decision. We will conclude with a discussion of possible gaps in our program theories and recommendations for research policy and practice, focusing on the top 5 CMO statements. After the workshop, we will use intensity sampling through focused searches to identify where robust research is available for particular contexts (e.g., day programs in a particular jurisdiction or day programs with a particular focus such as dementia care) to explore whether we can address any final gaps identified in the workshop [108]. We will synthesize the final program theories into a logical model (a visualization of the linkages of all the CMO statements).
Step 6: document the research process and disseminate findings
Throughout the research project, we will thoroughly document each process step, all decisions made, the searches conducted, and any findings. We will make all searches publicly available, and, using the open-source software Zotero to manage our references, we will share our reference libraries publicly. Project outputs will include (1) a non-technical report directed at lay audiences (experts will be involved in producing and disseminating this report), (2) a policy brief for health policy makers (our policy experts will be involved in producing and disseminating this report), (3) a list of recommendations for policy and practice on how to improve the impact of day programs on clients with dementia, their caregivers and health systems, (4) presentations at 2–4 peer-reviewed Canadian and international conferences, (5), webinars to the public (e.g., via brainXchange or our collaborators’ platforms), co-presented by researchers and experts, (6) a peer-reviewed open access paper in a journal focused on patient/expert engagement on the methods and results of the priority setting workshop, and (7) a peer-reviewed open access publication of the realist review.
Discussion
This study will make several critical contributions, given our aging population and our health systems’ ongoing struggles to care well for people with dementia and their caregivers. Day programs have the potential to constrain public healthcare costs (compared to long-term institutional care) and to support individuals with dementia and their caregivers to age in the community safely and well for as long as possible [41, 47, 52–55]. However, day programs are variable in funding models and programming, posing challenges for evaluation and improvement [41, 42]. By identifying essential elements and processes of day programs (and how they can be improved for whom) or knowledge gaps related to these essential elements, this study will generate much-needed knowledge to leverage the full potential of day programs so they can provide appropriate care, preventing premature institutionalization, unnecessary acute and primary care use. This will ultimately improve the quality of life of persons with dementia and their caregivers, alleviate caregiver burden, and reduce social costs associated with the aforementioned undesirable outcomes. Our close and continued collaboration with experts (iKT) is critical in generating knowledge relevant to day program practice and policy. Our experts are highly committed to this research and have highlighted its high priority, and they intend to use our findings to inform improvements to their day program policies and practices. Therefore, our study will enable health system and policy decision-makers, and day program teams to take our evidence to practice quickly to benefit older adults with dementia and their caregivers. Finally, this study will inform future research on day programs, including our own program of research. Our own research (including two cohort studies) and that of others will empirically test and further refine our program theories.
Limitations of this review may include those associated with the available literature and those related to realist approaches. Many of the available day program studies will have methodological limitations, limiting our ability to draw strong conclusions from these studies. Sources may also have a low degree of richness, making it difficult to identify and extract CMO statements and to understand the proposed linkages between the CMO elements. We will address these issues by rigorously assessing the relevance, richness, and rigor of included sources, comprehensively training our team members in identifying CMO elements (especially when they are hidden and not well described), excluding sources that do not include the required information (no relevance), transparently reporting on the quality of each included source, and on the challenges and mitigation strategies associated with extracting CMO statements. Generally, realist reviews are complex and resource-intensive [67, 73]. Finding a balance between capturing every detail in the literature and an abstraction level that is too high and unspecific can be difficult [73, 109]. Various of our team members have extensive experience in conducting realist syntheses, which will assist us in mitigating these challenges.
Supplementary Information
Additional file 1. PRISMA-P 2015 Checklist.
Additional file 3. Systematically conducted literature reviews on adult day programs and studies included in these reviews.
Additional file 4. Training and calibration materials.
Acknowledgements
We would like to thank all members of the Helen Carswell Chair in Dementia Care Advisory Committee, who helped us identify this realist synthesis as one of the major research priorities of our program of research, and who gave valuable input that helped us to design this study. We would also like to thank Jennifer Baumbusch, Whitney Berta, Jennifer Bethell, Greta Cummings, Tamara Daly, Malcolm Doupe, Liane Ginsburg, David Hogan, Kimberlyn McGrail, and Adrian Wagg for their advice and general support of this work.
Abbreviations
- AXIS
Appraisal tool for Cross-Sectional Studies
- CASP
Critical Appraisal Skills Program
- CLUSTER searching
Citation tracking, tracing Lead authors, identifying Unpublished materials, Google Scholar searching, Theory tracking, ancestry searching for Early examples, and follow-up of Related projects
- CMO
Contexts, Mechanisms, Outcomes
- iKT
integrated Knowledge Translation
- LTC
Long-Term Care
- MMAT
Mixed Methods Appraisal Tool
- NOS
Newcastle-Ottawa Scale
- QATQS
Quality Assessment Tool for Quantitative Studies
Authors’ contributions
MH is the lead of this study, AU is the co-chair of the Helen Carswell Chair in Dementia Care Advisory Committee, and co-lead of the CIHR grant funding this study. MH, HN, AR, AU, ZG, CJM, SA, KT, HSB, LW, SC, and JM contributed to the design and conception of this realist synthesis. MH and HN drafted this manuscript. AR, AU, ZG, CJM, SA, KT, HSB, LW, SC, and JM commented on and substantially revised various iterations of the manuscript.
Funding
This study is funded by the Carswell Family Foundation, funding the Helen Carswell Chair in Dementia Care, held by the corresponding author Matthias Hoben. In addition, the corresponding author holds a Canadian Institutes of Health Research (CIHR) Knowledge Synthesis and Mobilization Grant (510336), funding this study. The funders had no role in developing this protocol.
Data availability
Not applicable.
Declarations
Ethics approval and consent to participate
We obtained ethics approval for the focus groups and semi-structured interviews in this study from the Human Participants Review Committee, Office of Research Ethics, York University (2023–247), the Health Research Ethics Board-Health Panel, University of Alberta (Pro00137008), the Behavioural Research Ethics Board, University of British Columbia (H23-03918), and the Health Research Ethics Board, University of Manitoba (HS26361 (H2024:085)). Participants will complete written informed consent for participation in the focus groups or semi-structured interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alzheimer Society of Canada. Navigating the path forward for dementia in Canada: The landmark study, report 1. Toronto, ON: Alzheimer Society of Canada; 2022. [Google Scholar]
- 2.Gauthier S, Webster C, Servaes S, Morais JA, Rosa-Neto P. World Alzheimer Report 2022: Life after diagnosis: Navigating treatment, care and support. London, UK: ADI; 2022. [Google Scholar]
- 3.Organization for Economic Cooperation and Development (OECD). Care needed: improving the lives of people with dementia. Paris: OECD Publishing; 2018. [Google Scholar]
- 4.Alzheimer’s Association. 2023 Alzheimer’s disease facts and figures: special report, the treatment journey in an era of new treatments. Chicago, IL: Alzheimer’s Association; 2023. [Google Scholar]
- 5.Alzheimer Europe. Dementia in Europe Yearbook 2022: Employment and related social protection for people with dementia and their carers. Luxembourg: Alzheimer Europe; 2022. [Google Scholar]
- 6.Canadian Institute for Health Information (CIHI). Quick stats - Home Care Reporting System (HCRS) profile of clients in home care 2020–2021. Available from: https://www.cihi.ca/en/quick-stats. Cited 2022 Sep 2
- 7.Morgan T, Ann Williams L, Trussardi G, Gott M. Gender and family caregiving at the end-of-life in the context of old age: a systematic review. Palliat Med. 2016;30:616–24 2016/01/28 ed. [DOI] [PubMed] [Google Scholar]
- 8.Quesnel-Vallée A, Willson A, Reiter-Campeau S. Health inequalities among older adults in developed countries: reconciling theories and policy approaches. In: George L, Ferraro K, editors. Handbook of aging – social sciences. 8th ed. London: Elsevier; 2016. [Google Scholar]
- 9.Quesnel-Vallée A, Farrah J-S, Jenkins T. Population aging, health systems, and equity: Shared challenges for the United States and Canada. In: Settersten RA Jr, Angel JL, editors. Handbook of sociology of aging. New York, Dordrecht, Heidelberg, London: Springer; 2011. [Google Scholar]
- 10.Canadian Insitute for Health Information (CIHI). Your Health System: Caregiver Distress. Available from: https://yourhealthsystem.cihi.ca/hsp/inbrief?lang=en#!/indicators/081/caregiver-distress/;mapC1;mapLevel2. Cited 2023 Jun 5
- 11.Statistics Canada. The Daily — More than half of women provide care to children and care-dependent adults in Canada, 2022. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/221108/dq221108b-eng.htm. Cited 2023 Jun 5
- 12.Canadian Insitute for Health Information (CIHI). 1 in 3 unpaid caregivers in Canada are distressed. Available from: https://www.cihi.ca/en/1-in-3-unpaid-caregivers-in-canada-are-distressed. Cited 2023 Jun 5
- 13.MacDonald B-J, Wolfson M, Hirdes JP. The future co$t of long-term care in Canada. Toronto, ON: National Institute on Aging; 2019. Available from: https://www.nia-ryerson.ca/reports
- 14.Canadian Insitute for Health Information (CIHI). Unpaid caregiver challenges and supports. Available from: https://www.cihi.ca/en/dementia-in-canada/unpaid-caregiver-challenges-and-supports. Cited 2023 Jun 5
- 15.Public Health Agency of Canada. A Dementia Strategy for Canada: Together We Aspire. Ottawa, ON: Public Health Agency of Canada; 2019. [Google Scholar]
- 16.Public Health Agency of Canada. A Dementia Strategy for Canada: Together We Achieve - 2021 Annual Report. Ottawa, ON: Public Health Agency of Canada; 2021. [Google Scholar]
- 17.CanAge. Dementia in Canada: Cross-Country Report 2022. Toronto, ON: CanAge; 2022. p. 2022. [Google Scholar]
- 18.Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7:e105–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pedroza P, Miller-Petrie MK, Chen C, Chakrabarti S, Chapin A, Hay S, et al. Global and regional spending on dementia care from 2000–2019 and expected future health spending scenarios from 2020–2050: An economic modelling exercise. eClinicalMedicine. 2022;45. Available from: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00067-0/fulltext. Cited 2023 Sep 7 [DOI] [PMC free article] [PubMed]
- 20.Haaksma ML, Leoutsakos JS, Bremer JAE, Aalten P, Ramakers I, Verhey FRJ, et al. The clinical course and interrelations of dementia related symptoms. Int Psychogeriatr. 2018;30:859–66 2017/03/14 ed. [DOI] [PubMed] [Google Scholar]
- 21.Kua EH, Ho E, Tan HH, Tsoi C, Thng C, Mahendran R. The natural history of dementia. Psychogeriatrics. 2014;14:196–201 2014/10/18 ed. [DOI] [PubMed] [Google Scholar]
- 22.Borsje P, Wetzels RB, Lucassen PL, Pot AM, Koopmans RT. The course of neuropsychiatric symptoms in community-dwelling patients with dementia: a systematic review. Int Psychogeriatr. 2015;27:385–405. [DOI] [PubMed] [Google Scholar]
- 23.Pinkert C, Köhler K, von Kutzleben M, Hochgräber I, Cavazzini C, Völz S, et al. Social inclusion of people with dementia – an integrative review of theoretical frameworks, methods and findings in empirical studies. Ageing Soc. 2021;41:773–93. [Google Scholar]
- 24.The Academy of Medical Sciences. Multimorbidity: a priority for global health research. London: The Academy of Medical Sciences; 2018. [Google Scholar]
- 25.Nguyen H, Manolova G, Daskalopoulou C, Vitoratou S, Prince M, Prina AM. Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. J Comorb. 2019;9:2235042X19870934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Canadian Insitute for Health Information (CIHI). Dementia in home and community care. Available from: https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-home-and-community-care. Cited 2023 Jun 5
- 27.Tate K, Bailey S, Deschenes S, Grabusic C, Cummings GG. Factors influencing older persons’ transitions to facility-based care settings: a scoping review. Gerontologist. 2023;3(7):211–1227. [DOI] [PubMed]
- 28.Duan-Porter W, Ullman K, Rosebush C, McKenzie L, Ensrud KE, Ratner E, et al. Systematic review: risk factors and interventions to prevent or delay long-term nursing home placement for adults with impairments. Washington (DC): Department of Veterans Affairs (US); 2019. Available from: http://www.ncbi.nlm.nih.gov/books/NBK553430/. Cited 2023 Jun 5 [PubMed]
- 29.Toot S, Swinson T, Devine M, Challis D, Orrell M. Causes of nursing home placement for older people with dementia: a systematic review and meta-analysis. Int Psychogeriatr. 2017;29:195–208. [DOI] [PubMed] [Google Scholar]
- 30.Hoben M, Chamberlain SA, Gruneir A, Knopp-Sihota JA, Sutherland JM, Poss JW, et al. Nursing home length of stay in in three Canadian health regions: temporal trends, jurisdictional differences and associated factors. J Am Med Directors Assoc. 2019;20:1121. [DOI] [PubMed] [Google Scholar]
- 31.Young Y, Kalamaras J, Kelly L, Hornick D, Yucel R. Is aging in place delaying nursing home admission? J Am Med Dir Assoc. 2015;16(900):e1-6. [DOI] [PubMed] [Google Scholar]
- 32.Alders P, Schut FT. Trends in ageing and ageing-in-place and the future market for institutional care: scenarios and policy implications. Health Econ Policy Law. 2019;14:82–100. [DOI] [PubMed] [Google Scholar]
- 33.Vasunilashorn S, Steinman BA, Liebig PS, Pynoos J. Aging in place: evolution of a research topic whose time has come. J Aging Res. 2011;2012:e120952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iciaszczyk N, Arulnamby A, Brydges M, Marshall M, Cheng SM, Feil C, et al. Ageing in the right place: supporting older canadians to live where they want. Toronto, ON: National Institute on Ageing (NIA); 2022. [Google Scholar]
- 35.Canadian Insitute for Health Information (CIHI). 1 in 9 new long-term care residents potentially could have been cared for at home. Available from: https://www.cihi.ca/en/1-in-9-new-long-term-care-residents-potentially-could-have-been-cared-for-at-home. Cited 2023 Jun 5
- 36.Canadian Insitute for Health Information (CIHI). Your health system: new long-term care residents who potentially could have been cared for at home. Available from: https://yourhealthsystem.cihi.ca/hsp/inbrief?lang=en#!/indicators/082/new-long-term-care-residents-who-potentially-could-have-been-cared-for-at-home/;mapC1;mapLevel2. Cited 2023 Jun 5
- 37.Wimo A, Gauthier S, Prince M. Global estimates of informal care. London and Huddinge: Alzheimer’s Disease International and Karolinska Institutet; 2018. [Google Scholar]
- 38.Alzheimer’s Association. Alzheimer’s disease facts and figures. Alzheimer’s & Dementia. 2023;2023(19):1598–695. [DOI] [PubMed] [Google Scholar]
- 39.Liu R, Chi I, Wu S. Caregiving burden among caregivers of people with dementia through the lens of intersectionality. Gerontologist. 2022;62:650–61. [DOI] [PubMed] [Google Scholar]
- 40.Rocard E, Llena-Nozal A. Supporting informal carers of older people: Policies to leave no carer behind. Paris: Organization for Economic Cooperation and Development (OECD); 2022. [Google Scholar]
- 41.Ellen ME, Demaio P, Lange A, Wilson MG. Adult day center programs and their associated outcomes on clients, caregivers, and the health system: a scoping review. Gerontologist. 2017;57:e85-94. [DOI] [PubMed] [Google Scholar]
- 42.Symonds-Brown H, Ceci C, Duggleby W, Purkis ME. Re-thinking the nature of day programs for people with dementia: Implications for research. Dementia (London). 2021;20:326–47. [DOI] [PubMed] [Google Scholar]
- 43.Song M, Seo K, Choi S, Choi J, Ko H, Lee SJ. Seniors centre-based health intervention programmes in the United States and South Korea: a systematic review. Int J Nurs Pract. 2017;23:e12568. [DOI] [PubMed] [Google Scholar]
- 44.Bellazzecca E, Teasdale S, Biosca O, Skelton DA. The health impacts of place-based creative programmes on older adults’ health: a critical realist review. Health Place. 2022;76:102839. [DOI] [PubMed] [Google Scholar]
- 45.Johnson S, Bacsu J, Abeykoon H, McIntosh T, Jeffery B, Novik N. No place like home: a systematic review of home care for older adults in Canada. Can J Aging. 2018;37:400–19. [DOI] [PubMed] [Google Scholar]
- 46.Vandepitte S, Van Den Noortgate N, Putman K, Verhaeghe S, Faes K, Annemans L. Effectiveness of supporting informal caregivers of people with dementia: a systematic review of randomized and non-randomized controlled trials. J Alzheimer’s Dis. 2016;52:929–65. [DOI] [PubMed] [Google Scholar]
- 47.Lunt C, Dowrick C, Lloyd-Williams M. What is the impact of day care on older people with long-term conditions: a systematic review. Health Soc Care Community. 2021;29:1201–21. [DOI] [PubMed] [Google Scholar]
- 48.Hoe J, Ashaye K, Orrell M. Don’t seize the day hospital! Recent research on the effectiveness of day hospitals for older people with mental health problems. Int J Geriatr Psychiatry. 2005;20:694–8. [DOI] [PubMed] [Google Scholar]
- 49.Harder WP, Gornick JC, Burt MR. Adult day care: substitute or supplement? Milbank Q. 1986;64:414–41. [PubMed] [Google Scholar]
- 50.Nies H, Tester S, Nuijens JM. Day Care in the United Kingdom and the Netherlands: a comparative study. Ageing Soc. 1991;11:245–73. [Google Scholar]
- 51.Gutman GM, Milstein S, Killam J, Lewis D, Hollander MJ. Adult day care centres in British Columbia: models, characteristics and services. Health Rep. 1993;5:189–207. [PubMed] [Google Scholar]
- 52.Li Y, Liu J, Sun F, Xu L. Adult day service use among minority older adults: facilitators, barriers, and outcomes from an updated integrative literature review between 2010 to 2021. J Appl Gerontol. 2022;41:2253–63. [DOI] [PubMed] [Google Scholar]
- 53.Orellana K, Manthorpe J, Tinker A. Day centres for older people: a systematically conducted scoping review of literature about their benefits, purposes and how they are perceived. Ageing Soc. 2020;40:73–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sadarangani TR, Murali KP. Service Use, Participation, experiences, and outcomes among older adult immigrants in American adult day service centers: an integrative review of the literature. Res Gerontol Nurs. 2018;11:317–28. [DOI] [PubMed] [Google Scholar]
- 55.Tretteteig S, Vatne S, Rokstad AMM. The influence of day care centres for people with dementia on family caregivers: an integrative review of the literature. Aging Ment Health. 2016;20:450–62. [DOI] [PubMed] [Google Scholar]
- 56.Manthorpe J, Moriarty J. Examining day centre provision for older people in the UK using the Equality Act 2010: findings of a scoping review. Health Soc Care Community. 2014;22:352–60. [DOI] [PubMed] [Google Scholar]
- 57.Fields NL, Anderson KA, Dabelko-Schoeny H. The effectiveness of adult day services for older adults: a review of the literature from 2000 to 2011. J Appl Gerontol. 2014;33:130–63. [DOI] [PubMed] [Google Scholar]
- 58.Manthorpe J, Moriarty J. Opportunity knocks: exploring the links between day opportunities and equal opportunities. Practice. 2013;25:317–33. [Google Scholar]
- 59.Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al. A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers. Health Technol Assess. 2007;11(1–157):iii. [DOI] [PubMed] [Google Scholar]
- 60.Gaugler JE, Zarit SH. The effectiveness of adult day services for disabled older people. J Aging Soc Policy. 2001;12:23–47. [DOI] [PubMed] [Google Scholar]
- 61.Seddigh M, Hazrati M, Jokar M, Mansouri A, Bazrafshan M-R, Rasti M, et al. A comparative study of perceived social support and depression among elderly members of senior day centers, elderly residents in nursing homes, and elderly living at home. Iran J Nurs Midwifery Res. 2020;25:160–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shapira N, Barak A, Gal I. Promoting older adults’ well-being through Internet training and use. Aging Ment Health. 2007;11:477–84. [DOI] [PubMed] [Google Scholar]
- 63.Bøen H, Dalgard OS, Johansen R, Nord E. A randomized controlled trial of a senior centre group programme for increasing social support and preventing depression in elderly people living at home in Norway. BMC Geriatr. 2012;12:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dröes R-M, Breebaart E, Meiland FJM, Van Tilburg W, Mellenbergh GJ. Effect of Meeting Centres Support Program on feelings of competence of family carers and delay of institutionalization of people with dementia. Aging Ment Health. 2004;8:201–11. [DOI] [PubMed] [Google Scholar]
- 65.Kelly R, Puurveen G, Gill R. The effect of adult day services on delay to institutional placement. J Appl Gerontol. 2016;35:814–35. [DOI] [PubMed] [Google Scholar]
- 66.Pawson R, Tilley N. Realistic evaluation. Sage; 1997. Available from: https://login.ezproxy.library.ualberta.ca/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=cat03710a&AN=alb.1992254&site=eds-live&scope=site
- 67.Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review–a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(Suppl 1):21–34. [DOI] [PubMed] [Google Scholar]
- 68.Pawson R. Evidence-based Policy. London and others: SAGE; 2006. Available from: https://methods.sagepub.com/book/evidence-based-policy
- 69.Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med. 2013;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Greenhalgh J, Manzano A. Understanding ‘context’ in realist evaluation and synthesis. Int J Soc Res Methodol. 2022;25:583–95. [Google Scholar]
- 71.Lacouture A, Breton E, Guichard A, Ridde V. The concept of mechanism from a realist approach: a scoping review to facilitate its operationalization in public health program evaluation. Implement Sci. 2015;10:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liou C, Jarrott SE. Dementia and dementia care in Asia-Taiwanese experiences: elders with dementia in two different adult day service (ADS) environments. Aging Ment Health. 2013;17:942–51. [DOI] [PubMed] [Google Scholar]
- 73.Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci. 2012;7:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Leggat FJ, Wadey R, Day MC, Winter S, Sanders P. Bridging the know-do gap using integrated knowledge translation and qualitative inquiry: a narrative review. Qual Res Sport, Exerc Health. 2023;15:188–201. [Google Scholar]
- 75.Boyko JA, Riley BL, Willis CD, Stockton L, Zummach D, Kerner J, et al. Knowledge translation for realist reviews: a participatory approach for a review on scaling up complex interventions. Health Res Pol Syst. 2018;16:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Booth A, Wright J, Briscoe S. Scoping and Searching to Support Realist Approaches. Doing Realist Research. Los Angeles and others: SAGE; 2018. p. 147–66. Available from: https://methods.sagepub.com/book/ng-realist-research
- 78.Booth A, Carroll C. Systematic searching for theory to inform systematic reviews: is it feasible? Is it desirable? Health Info Libr J. 2015;32:220–35. [DOI] [PubMed] [Google Scholar]
- 79.Greenhalgh T, Pawson R, Wong G, Westhorp G, Greenhalgh J, Manzano A, et al. “Theory” in realist evaluation: The RAMESES II Project. Oxford: The RAMESES Projects; 2017. Available from: https://www.ramesesproject.org/media/RAMESES_II_Theory_in_realist_evaluation.pdf
- 80.Bunn F, Goodman C, Reece Jones P, Russell B, Trivedi D, Sinclair A, et al. What works for whom in the management of diabetes in people living with dementia: a realist review. BMC Med. 2017;15:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kneale D, Thomas J, Harris K. Developing and optimising the use of logic models in systematic reviews: exploring practice and good practice in the use of programme theory in reviews. PLoS One. 2015;10:e0142187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Manzano A. The craft of interviewing in realist evaluation. Evaluation. 2016;22:342–60. [Google Scholar]
- 83.Greenhalgh T, Pawson R, Wong G, Westhorp G, Greenhalgh J, Manzano A, et al. The Realist Interview: The RAMESES II Project. Oxford: RAMESES projects, University of Oxford; 2017. [Google Scholar]
- 84.Wong G, Westhorp G, Greenhalgh J, Manzano A, Jagosh J, Greenhalgh T. Quality and reporting standards, resources, training materials and information for realist evaluation: the RAMESES II project. Health Serv Deliver Res. 2017;5:1–108. [PubMed] [Google Scholar]
- 85.Rees CE, Davis C, Nguyen VNB, Proctor D, Mattick KL. A roadmap to realist interviews in health professions education research: recommendations based on a critical analysis. Med Educ. 2024;58:697–712. [DOI] [PubMed] [Google Scholar]
- 86.Mukumbang FC, Marchal B, Van Belle S, van Wyk B. Using the realist interview approach to maintain theoretical awareness in realist studies. Qual Res. 2020;20:485–515. [Google Scholar]
- 87.Westhorp G, Manzano A. Realist evaluation interviewing – a ‘starter set’ of questions: the RAMESES II Project. Oxford: RAMESES projects, University of Oxford; 2017. [Google Scholar]
- 88.Dalkin S, Forster N, Hodgson P, Lhussier M, Carr SM. Using computer assisted qualitative data analysis software (CAQDAS; NVivo) to assist in the complex process of realist theory generation, refinement and testing. Int J Soc Res Methodol. 2021;24:123–34. [Google Scholar]
- 89.Bergeron DA, Gaboury I. Challenges related to the analytical process in realist evaluation and latest developments on the use of NVivo from a realist perspective. Int J Soc Res Methodol. 2020;23:355–65. [Google Scholar]
- 90.Gilmore B, McAuliffe E, Power J, Vallières F. Data analysis and synthesis within a realist evaluation: toward more transparent methodological approaches. Int J Qual Methods. 2019;18:1609406919859754. [Google Scholar]
- 91.Booth A, Harris J, Croot E, Springett J, Campbell F, Wilkins E. Towards a methodology for cluster searching to provide conceptual and contextual “richness” for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol. 2013;13:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dada S, Dalkin S, Gilmore B, Hunter R, Mukumbang FC. Applying and reporting relevance, richness and rigour in realist evidence appraisals: advancing key concepts in realist reviews. Res Synth Methods. 2023;14:504–14. [DOI] [PubMed] [Google Scholar]
- 94.Jagosh J, Pluye P, Macaulay AC, Salsberg J, Henderson J, Sirett E, et al. Assessing the outcomes of participatory research: protocol for identifying, selecting, appraising and synthesizing the literature for realist review. Implement Sci. 2011;6:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1:176–84. [DOI] [PubMed] [Google Scholar]
- 96.Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract. 2012;18:12–8. [DOI] [PubMed] [Google Scholar]
- 97.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2024. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Cited 2024 May 1
- 98.Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. 2016;6:e011458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Critical Appraisal Skills Programme (CASP). CASP Qualitative Studies Checklist. CASP - Critical Appraisal Skills Programme. 2024. Available from: https://casp-uk.net/casp-tools-checklists/. Cited 2024 May 1
- 100.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34:285–91. [Google Scholar]
- 101.Booth A, Carroll C, Ilott I, Low LL, Cooper K. Desperately seeking dissonance: identifying the disconfirming case in qualitative evidence synthesis. Qual Health Res. 2013;23:126–41. [DOI] [PubMed] [Google Scholar]
- 102.Kantilal K, Hardeman W, Whiteside H, Karapanagiotou E, Small M, Bhattacharya D. Realist review protocol for understanding the real-world barriers and enablers to practitioners implementing self-management support to people living with and beyond cancer. BMJ Open. 2020;10:e037636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Petit-Zeman S, Firkins L, Scadding JW. The James Lind Alliance: tackling research mismatches. Lancet. 2010;376:667–9. [DOI] [PubMed] [Google Scholar]
- 104.Chamberlain SA, Estabrooks CA, Keefe JM, Hoben M, Berendonk C, Corbett K, et al. Citizen and stakeholder led priority setting for long-term care research: identifying research priorities within the Translating Research in Elder Care (TREC) Program. Res Involve Engage. 2020;6:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bethell J, Pringle D, Chambers LW, Cohen C, Commisso E, Cowan K, et al. Patient and public involvement in identifying dementia research priorities. J Am Geriatr Soc. 2018;66:1608–12. [DOI] [PubMed] [Google Scholar]
- 106.Bethell J, Puts MTE, Sattar S, Andrew MK, Choate AS, Clarke B, et al. The Canadian frailty priority setting partnership: research priorities for older adults living with frailty. Can Geriatr J. 2019;22:23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.James Lind Alliance. The James Lind Alliance Guidebook. 6th ed. London: National Institutes for Health Research; 2016. [Google Scholar]
- 108.Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Syst Rev. 2016;5:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Flynn R, Schick-Makaroff K, Levay A, Greenhalgh J. Developing an initial program theory to explain how patient-reported outcomes are used in health care settings: methodological process and lessons learned. Int J Qual Methods. 2020;19:1609406920916299. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. PRISMA-P 2015 Checklist.
Additional file 3. Systematically conducted literature reviews on adult day programs and studies included in these reviews.
Additional file 4. Training and calibration materials.
Data Availability Statement
Not applicable.