ABSTRACT
The history of the founding of the Cuban Skull Base Surgery Group is reported. Under the author's supervision and coordination, the group has managed more than 100 major skull base cases over a 6-year period. The mortality rate was 13% and the rate of permanent morbidity was 23%. In the last 2 years, the mortality rate decreased to 8%. These results reflect the group's enthusiasm pitted against the obvious challenges associated with economic constraints. The present experience may be instructive for neurosurgeons interested in exporting their expertise, with the goal of helping colleagues in developing countries to broaden their professional experience.
Keywords: Developing country, skull base surgery, Republic of Cuba
Establishing a new subspecialty in an already well-established professional neurosurgical environment is challenging. It requires strong motivation and a certain amount of good luck. Although a developing country, the Republic of Cuba has a remarkably well-developed health-care system. A neurological unit has been available, but expertise in skull base surgery was lacking. I had the opportunity to organize a cranial base surgery program, which allowed the cranial base surgery group, developed by the Ministry of Public Health of Cuba, to operate on more than 104 difficult skull base tumors with promising results.
INITIAL CONTACTS AND ORIGINAL PLANNING
The first meeting, which involved a high official of the Cuban Ministry of Public Health, was organized in 1996. The official was Dr. Julian Alvarez, who had just moved to the internationally recognized leading center in neuro-augmentation, CIREN (Centro Internacional de Restauracion Neurologica), as its Director from his previous position as Vice Minister of Public Health. Dr. Alvarez had been promoting the development of several health-care issues in Cuba, including biotechnology.1,2 At the same time he also reorganized CIREN after a period of mismanagement.
In June 1996, I gave my first technical demonstration on a cadaveric head at the CIREN, where I found a modern operating room with a Leica microscope, Aesculap drill, and adequate microinstrumentation. I later learned that microneurosurgery had been introduced in Cuba in the early 1970s and that craniobasal lesions had been routinely operated on using conventional approaches, with acceptable results if compared with the international standard. In 1 day, working diligently from 8 am to 7 pm, I was able to demonstrate an entire family of skull base approaches,3 from the fronto-orbitozygomatic craniotomy with clinoidectomy to the anterior and posterior petrosal approaches, ending with the far-lateral approach. All procedures were filmed for later demonstration to residents and interested neurosurgeons. Subsequently, we planned future visits to establish a skull base laboratory.
When I returned to Italy, an agreement was signed between the University of Rome “Tor Vergata,” where I worked as an Assistant Professor of Neurosurgery, and CIREN. The project was financed with a basic research grant from the Italian Ministry of Scientific Investigation, which totaled $2000 a year. I then began traveling to Havana three or four times a year for 1 or 2 weeks each time.
The Cubans were more interested in promoting a clinically oriented program than in pursuing anatomic-surgical research. Given their limited budget, which had to include all requirements for both clinical and scientific work, their choice was sound. In fact, skull base techniques had not yet been introduced because of economic difficulties related to the embargo of Cuba and to the collapse of the Soviet Union. However, the idea of performing cadaveric dissections was not abandoned.
The first patient treated had a 2 × 3 cm tuberculum sellae meningioma, which was removed successfully. Following cases were not always so straightforward. However, subsequent experience allowed complex cases to be managed according to contemporary criteria.
ESTABLISHMENT OF THE SKULL BASE GROUP
During the course of my visits, I had strengthened my personal relationship with Professor Roger Figueredo, the founder of modern Cuban neurosurgery. I had become acquainted with Dr. Figueredo when he had referred some difficult cases to me in early 1998. Professor Figueredo had observed almost all cranial base demonstrations and offered us the chance to work in the modern-equipped operating theater of the CIMEQ (Centro de Investigaciones Médico Quirúrgico). The twin hospital of CIREN, CIMEQ is located in the same modern building where Dr. Figueredo managed the neurosurgical unit. Unlike CIREN, which is a neurological research institution, CIMEQ is a general hospital and research center. The two institutions have separate neurosurgical units and operating rooms. CIREN has one each and CIMEQ has four units and one operating room. The two centers share certain expensive facilities, such as the diagnostic imaging department, to minimize costs.
With the help and wise suggestions of Professor Figueredo, we created a pilot program of the skull base group and began to systematize organizational aspects and clinical work. We also began to stage the most demanding surgical cases to minimize the demands on the involved personnel by avoiding excessively lengthy operations. At the end of 1999 CIMEQ hosted the Cuban Neurosurgical Congress. Several foreign colleagues participated in the meeting. My presentation on the local skull base experience raised considerable interest among the participants (unpublished data).
During the same period, the high officials of the Ministry of Health agreed to organize a meeting to review past clinical work and to create an official Cuban Skull Base Group. The meeting was scheduled for December 1999, with the participation of the Minister, the first Vice Minister, Professor Figueredo, and the directors of the leading Havana hospitals. Doctor Dotres, a pediatrician and the Cuban Minister of Public Health, expressed interest in promoting the development of skull base surgery in Cuba. He agreed that a national skull base group should be organized under his auspices. The group was directed by myself as a Foreign Consultant and by Professor Figueredo as the Director.
The group decided that CIMEQ would host the clinical work of the skull base group in its operating facilities and that a network would be created among interested neurosurgeons. A skull base laboratory was also planned. MINSAP (Ministerio de la Salud Publica [Ministry of Public Health]) delivered $200,000 so that technology could be updated immediately. I was unable to obtain concrete financial support in Italy. However, I did obtain an agreement between MINSAP and the Nuova Clinica Latina in Rome (where I had worked part time as a neurosurgical supervisor) that allowed select Cuban patients with difficult skull base lesions to be operated on in Italy with the help of Cuban professionals. The Cuban neurosurgeons and paramedical staff could thereby benefit by the experience of working in a different environment.
PRESENT SITUATION AND PERSPECTIVES
Unfortunately, Professor Figueredo died suddenly at the age of 74 in March 2000. Not unexpectedly, his death posed problems to the process of implementing the skull base project. Thanks to his strong motivation, experience, and personal prestige, he had resolved many difficult situations. His death led me to devote myself almost “full time” to the project by taking a leave of absence from my university. At the same time, we reinforced the Italian side of the agreement and began operating on Cuban cases in Rome on a regular basis.
A few months later, MINSAP decided to involve, officially, the leading La Habana Clinic Institution, the Hermanos Ameijeiras Hospital, in the program (Fig. 1). The 30-bed neurosurgical units of this hospital had been a major case contributor to the clinical work of the skull base group. After my official return to Italy, neurosurgeons from this institute began spending 1 or 2 months with me in Rome. There they had the opportunity to be fully involved in the clinical management of several cases, including some Cuban patients with major skull base tumors. Eventually, MINSAP decided to renovate the neurosurgical operating rooms of the Hermanos Ameijeiras Hospital to implement a brand-new operating room dedicated to skull base surgery by the year 2004.
Figure 1.
Front view of the 24-floor multispecialty Hermanos Ameijeiras Hospital.
A modern, fully equipped, skull base laboratory is also being implemented; it may be functional sometime in 2004. The new facility will allow young specialists to be trained in modern techniques, including minimally invasive, endoscopic-assisted skull base procedures, which are likely to be used extensively in the near future. Residents will rotate through the laboratory every 6 months to guarantee both their clinical training and exposure to research. Scientific activity is under way, as testified by (admittedly) the few papers recently submitted for possible publication to relevant international journals.4,5
Neurosurgical instrumentation is being upgraded. Investments, excluding renovation of facilities, have totaled about $400,000. Priority was given to obtaining an operating microscope, video-recording technology, and microsurgical instrumentation. European-produced, high-power drills were purchased for both the operating room and laboratory. The second priority was given to ultrasonic aspiration devices. Laser technology, which was already available at the CIMEQ, was given a low priority.
The group, which is now based in the Hermanos Ameijeiras Hospital, includes three full-time neurosurgeons (whom I supervise), two part-time neurosurgeons, one rotating neurosurgical resident fully devoted to skull base surgery, one ear-nose-throat specialist with an interest and experience in lateral skull base surgery, one maxillofacial surgeon, two dedicated anesthesiologists (assisted by other colleagues if necessary), and a strongly motivated nursing staff. Part-time consultants include an extremely experienced oncological craniofacial surgeon and a plastic surgeon. A limited number of intensive care unit (ICU) specialists work routinely with the patients treated by the skull base group (Fig. 2). At CIMEQ, patients are operated on by three neurosurgeons who trained with me between 1996 and 2000. In these cases, the team discusses operative strategy. In some cases I supervise the operations.
Figure 2.
The Cuban Skull Base Group pictured in front of the Hermanos Ameijeiras Hospital. From left to right: Felicia Montes de Oca Fernandez, M.D., neurosurgeon; Justo Gonzalez Gonzalez, M.D., neurosurgeon; Lilian Moroño Guerrero, M.D., anesthesiologist; Aldo Spallone, M.D., neurosurgeon; Lazaro Alvarez Acosta, head nurse; Irasema Bezares Ramos, M.D., plastic surgeon; Enrique de Jongh Cobo, M.D., neurosurgeon; Carlos Croaña Soospedra, M.D., maxillofacial surgeon; Alexei Villegas Achon, M.D., anesthesiologist; and Antonio Paz Cordovez, M.D., ENT surgeon.
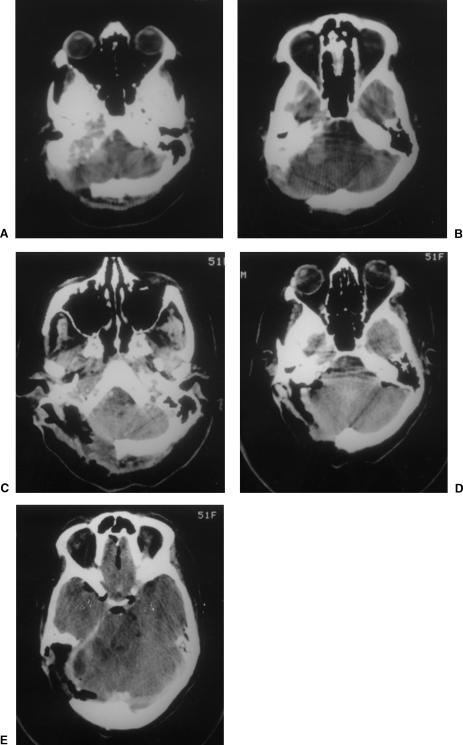
Presently, all patients undergo a strict preoperative protocol that includes MRI, CT, MRI angiography, and angiography with balloon test occlusion. Demanding cases are treated in a two-stage procedure. The craniobasal approach is performed 2 to 3 days before microsurgical removal of the lesion (Fig. 3). Cuban patients who are treated in Italy are accompanied by a young neurosurgeon and an ICU or operating room nurse. These cases are part of my teaching duties as Professor of Neurosurgery at the University of La Havana.
Figure 3.
(A, B) Postcontrast CT showing a lesion extending from the right lateral craniocervical region to the cerebellopontine angle. (C–E) Following surgery via a combined right extreme lateral-retrolabyrinthine approach, the lesion was totally removed.
At the end of 2002 I began to decrease my professional activity in Cuba, and I stopped performing surgery in mid-2003. My Cuban colleagues, however, have accumulated significant experience with skull base surgery.
RESULTS OF CLINICAL MANAGEMENT
As of November 2002, 104 patients with skull base lesions have been treated (Table 1). About a third of the cases had undergone a previous surgery with incomplete tumor resection. By the end of 2000, 55 patients had undergone surgery (3 in Italy). Of these 55 patients, 9 died and 14 had permanent complications for a mortality rate of 16% and a permanent morbidity rate of 25%. From January 2001 to November 2002, 49 patients were treated (20 in Italy); 4 (8%) died and 10 (20%) had permanent postoperative morbidity. LINAC radiosurgery has now been introduced in the clinical routine. Typically, it is given 10 days to 2 months after surgery to patients who underwent incomplete resection of skull base tumors (5 cases in 2001 and 2002). Of the entire 104 patients, 13 (12.5%) have died and 24 (23.1%) have permanent morbidity.
Table 1.
Type of Tumor and Location in 104 Cuban Patients
| Tumor | Location | No. |
|---|---|---|
| Meningiomas | Subfrontal; cavernous sinus | 8 |
| Petroclival | 22 | |
| Foramen magnum | 1 | |
| Neurinomas | V | 2 |
| VIII (giant) | 10 | |
| Foramen magnum | 2 | |
| Cholesteatomas | 10 | |
| Adenomas | Giant extending to the middle fossa | 5 |
| Cavernous sinus | 13 | |
| Craniopharyngiomas | 4 | |
| Chordomas | Cavernous sinus | 2 |
| Clival | 2 | |
| Glomus jugulare tumors | 4 | |
| Aneurysms | 5 | |
| Others | Petroclival | 5 |
| Subfrontal; cavernous sinus | 5 | |
| Foramen magnum | 4 |
The mean hospital stay of Cuban patients in Italy has been 13 ± 5.6 days.
CONCLUSION
As stated, establishing a new subspecialty program in an already well-established professional environment is challenging. Several factors are needed for an initiative of this kind to succeed: strong personal motivation, good integration with the new environment (which necessitates thoughtful consideration and knowledge of the local culture, psychology, habits, and character of the involved people), a strong rationale (including professional, organizational, clinical, and scientific aspects), definition of the minimum necessary technological standard to realistically initiate the work, willingness to grow, and a strong dose of good luck.
In terms of my professional experience in Cuba, the latter involved meeting Professor Roger Figueredo (Fig. 4) and building friendly personal relationships with some of the leading figures of MINSAP at the proper time. Professor Figueredo actively and enthusiastically promoted this work by constantly speaking with the high officials of the Ministry of Public Health to solve problems that could affect my life, both professional and personal while in Cuba. As founder of the Havana Neurological Institute in late 1960s, his experience was fundamental to the success of the project, and his friendly and constant assistance was extremely helpful in several difficult moments.
Figure 4.
Professor Roger Figueredo (1926–2000).
This experience has been exceptional because, in terms of its health-care systems, Cuba is almost unique as a developing country. Despite many economic constraints, their system approaches the best world standards.
My hope is that the international neurosurgical community will benefit from this report by utilizing it when implementing neurosurgical programs in other developing countries.
Footnotes
Dedicated to Professor Roger Figueredo.
REFERENCES
- Pilling D. Cuba's medical revolution. 2001. F T Weekend Jan 13–14.
- Tamayo J O. Advanced therapy, low cost lure patients to Cuba. 1996. pp. 19A–21A. Miami Herald Feb 15.
- Spallone A, Rizzo A, Konovalov A N, Giuffre' R. Fronto-orbito-zygomatic approach: a technical modification. Skull Base Surg. 1996;6:125–128. doi: 10.1055/s-2008-1058904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spallone A, Flores G L, Zaldivar L O, Estupinan B. Giant cell tumor (osteoclastoma) of the petrous bone: case report. Skull Base Surg. 1999;9:155–159. doi: 10.1055/s-2008-1058163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spallone A, Gonzalez J L, Montes De Oca F. Intradural cervical herniated disk: report of two cases and review of the literature. In press.