Abstract
Background and study aims Killian-Jamieson diverticulum (KJD) is a rare type of esophageal diverticulum that occurs in a specific area called the Killian-Jamieson space. Although surgery has been the conventional treatment for symptomatic KJD, minimally invasive endoscopic techniques, particularly Killian-Jamieson per-oral endoscopic myotomy (KJ-POEM), have emerged as an alternative. The aim of the study was to evaluate the effectiveness and safety of KJ-POEM in treating KJD.
Patients and methods This was an international, multicenter, retrospective study that included patients who underwent KJ-POEM for symptomatic KJD from October 16, 2018 to April 12,2023. The primary outcome was clinical success, defined as complete or near-complete resolution of symptoms (i.e., post-procedure Kothari-Haber Score ≤ 2). Secondary outcomes were technical success (defined as successful completion of all procedural steps), rate and severity of adverse events (AEs), total procedure duration, and symptom recurrence during follow-up.
Results A total of 13 patients (mean age 65.23 years, 6 female) with KJD and a mean pre-procedure Kothari-Haber Score of 6 (standard deviation [SD] 2.16) underwent KJ-POEM across 10 participating centers. Clinical success and technical success were achieved in all cases (100%) with a mean post-procedure Kothari-Haber Score of 0.91 (SD 0.99). There were no AEs and no cases of injury to the recurrent laryngeal nerve. Mean length of hospital stay was 1.09 days (SD 0.74). Mean follow-up time was 9.41 months (SD 10.07) post-procedure. There was no post-procedure symptom recurrence any patient.
Conclusions KJ-POEM is a safe and effective alternative treatment for symptomatic KJD with excellent short/mid-term outcomes.
Keywords: Endoscopy Upper GI Tract
Introduction
Killian-Jamieson diverticulum (KJD) is a rare form of esophageal diverticulum that occurs in a specific region of the esophagus known as the Killian-Jamieson space. Unlike other types of esophageal diverticula, such as Zenker’s diverticulum (ZD) which typically occur in the upper part of the esophagus above the cricopharyngeal muscle, Killian-Jamieson diverticula originate on the anterolateral wall of the cervical esophagus below the cricopharyngeal muscle. Most patients with KJD are asymptomatic; however, some patients may develop symptoms like those in ZD, such as globus sensation, halitosis, dysphagia, regurgitation, cough, epigastric pain, and rarely hoarseness 1 . Although surgical intervention has traditionally been the mainstay of treatment for symptomatic Killian-Jamieson diverticula, endoscopic techniques have emerged as a minimally invasive alternative. Although per-oral endoscopic myotomy is an effective treatment for ZD (Z-POEM), its role in management of KJD (KJ-POEM) is not well defined. There are limited published data on KJ-POEM for treatment of KJD, with only a few case reports/case series available in the literature 2 3 4 5 6 7 8 9 . Because of the proximity of KJD to the recurrent laryngeal nerve, safety concerns have been raised about KJ-POEM. The aim of this study was to assess the efficacy and safety of KJ-POEM for treatment of KJD.
Patients and methods
This was an international, multicenter, retrospective study that included 11 centers from six countries including Romania, Italy, Ecuador, Japan, India, and the United States. The study was approved by individual institutional review boards at all participating centers.
Patients who underwent KJ-POEM for symptomatic KJD between October 16, 2018 and April 12, 2023 were enrolled in the study. Diagnosis of KJD was based on results of a barium swallow test and/or computed tomography (CT) scan that were confirmed endoscopically.
Patient symptoms were quantified using the Kothari-Haber score. This scoring system is mainly used for ZD and is based on seven parameters, including dysphagia, weight loss, regurgitation, halitosis, cough, hoarseness, and pneumonia 10 . It ranges from a minimum of 0 to a maximum of 16 points, with higher scores indicating more severe symptoms. Patient dysphagia scores were collected from chart reviews of clinical follow-ups.
Patients were identified using center-specific endoscopic or billing databases. Electronic records were reviewed to capture the following variables: demographic data, dysphagia score, additional symptoms (aspiration, choking, halitosis, regurgitation, weight loss, and others), imaging findings, prior surgical or endoscopic interventions, type of KJ-POEM technique used, total procedure duration, clinical success, technical success, type of knife and number of clips used, length of hospital stay, symptom recurrence at follow-up, adverse events (AEs) with severity graded according to the American Society for Gastrointestinal Endoscopy (ASGE) lexicon 11 , and follow-up duration. None of the participants in this study have been included in another publication.
KJ-POEM technique
Informed consent was obtained from all patients before KJ-POEM was performed. All KJ-POEMs were carried out by therapeutic endoscopists with patients under deep sedation or general anesthesia. Most procedures were done under general anesthesia instead of deep sedation to reduce risk of aspiration. The exception was that in some centers and certain cases, deep sedation was done due to patient preference, mainly for those with very minimal comorbidities. The gastroscope was advanced to the previously identified location of the KJD in the patient’s esophagram or CT scan. Similar to the Z-POEM technique, a submucosal bleb was created and an incision was made in the mucosal lining of the septum. Through the initial mucosal incision, the submucosal fibers were dissected and the endoscope entered the submucosal space. Following submucosal tunneling on both sides of the septum, myotomy/septotomy was performed and the septum that separates the diverticulum and the esophageal proper was dissected down to the base. A complete myotomy was performed, extending beyond the distal extent of the diverticulum to ensure complete dissection and prevent recurrence. We identified the end point of myotomy when the muscular septum thinned to the expected esophageal muscle layer width.
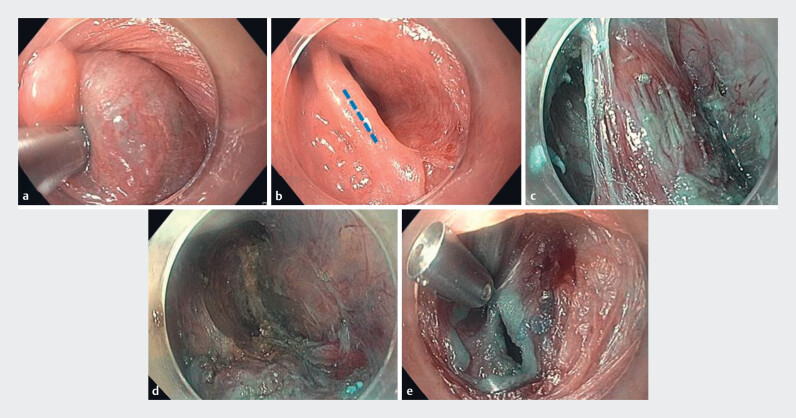
Following the initial cut to the myotomy, a split between the diverticular and esophageal muscles became apparent. The esophageal muscle was cut until the diverticular muscle was completely incised. Precautions taken to avoid leaks, perforation, and injury to surrounding structures, particularly the recurrent laryngeal nerve, included frequent submucosal injection during tunneling to assess methylene blue staining luminally at the base of the diverticulum, gentle blunt dissection as the muscular septum thinned, focused dissection at the base of the myotomy, slow and careful tunneling/myotomy, and avoidance of tunneling/myotomy beyond the bottom of the diverticulum. Finally, the mucosal incision was closed with through-the-scope clips ( Fig. 1 a-e ).
Fig. 1.
Killian-Jamieson per-oral endoscopic myotomy (KJ-POEM) technique. a Submucosal injection is performed over the septum. b Mucosal incision is performed (along the blue dashed line). c Submucosal tunneling is performed until the septum is reached and the septum is completely exposed as submucosal dissection is carried out on either side of the septum. d Complete myotomy. e Mucosal closure using through-the-scope clips.
The approach involves a longitudinal incision along the septum, followed by diverticulum tunnel dissection and myotomy. The differences, as mentioned previously, include extra-luminal inspection during tunnel injection and dissection. In Z-POEM, dissections are performed slightly further down compared with KJ-POEM to avoid potential recurrent laryngeal nerve injury, which can make KJ-POEM more challenging. Using a smaller-diameter cap and occasionally employing underwater tunneling may help overcome some of these challenges. The same technique is used. The only differences are the different location of diverticula and septum and the theoretical risk of recurrent laryngeal nerve injury.
Post-procedure, patients were admitted to the hospital and kept nil per os (NPO) overnight. On postoperative day 1, a barium esophagram was performed as a routine test to make sure no leak was detected. Patients then were started on a soft diet and treated with oral antibiotics for a couple of days. They were kept on a soft diet for 1 to 2 weeks before starting a normal diet. Follow-up appointments were made 2 to 4 weeks post-procedure to assess patient clinical response and to evaluate for any potential delayed AEs.
Outcomes
The primary outcome was clinical success (defined as complete or near-complete resolution of symptoms, i.e., post-procedure Kothari-Haber score ≤ 2). Patients who did not achieve clinical success at follow-up were considered to have “clinical failure”. Patients who attained clinical success at the initial follow-up visit but had recurrence of symptoms at later visits were classified as having “clinical recurrence”. Secondary outcomes included technical success (defined as successful completion of all procedure steps), rate and severity of AEs (per ASGE lexicon) 11 , total procedure duration, and symptom recurrence during follow-up.
Statistical analysis
Continuous variables are presented as the mean (SD). Categorical data are presented as number (percent). Dysphagia score was analyzed as a continuous variable. Paired student’s t test was used to compare pre-procedure and post-procedure results. P < 0.05 was considered statistically significant. All statistical analyses were conducted using STATA version 18.0 (StataCorp LLC, College Station, Texas, United States).
Results
Thirteen patients (mean age 65.23 years [SD 11.41]; 6 female) underwent KJ-POEM during the study period ( Table 1 ). The most common presenting symptoms at the time of diagnosis were dysphagia (n = 13; 100%) and regurgitation (n = 13; 100%). Mean duration of symptoms was 3.30 years (SD 2.69). Mean Kothari-Haber score at baseline was 6 (SD 2.16). None of the patients had prior treatment for esophageal diverticulum or a history of antiplatelet therapy. American Society of Anesthesiologists (ASA) physical status classification of the patients ranged from I to III. Mean ASA score was 1.0 (SD 0.57). Mean size of the diverticula was 21.68 mm (SD 9.61).
Table 1 Baseline, procedure details, and post-procedure KJ-POEM outcomes.
| ASA, American Society of Anesthesiologists; KJ-POEM, Killian-Jamieson per-oral endoscopic myotomy; NPO, nil per os; PS, physical status; SD, standard deviation. | |
| Baseline characteristics | n = 13 |
| Age, mean (SD), years | 65.23 (11.41) |
| Female sex, n (%) | 6 (46.15) |
| ASA PS classification (I/II/III), n | 2/9/2 |
| Prior treatment, n (%) | 0 (0) |
| Symptom duration, mean (SD), years | 3.30 (2.69) |
| Diverticulum size, mean (SD), mms | 21.68 (9.61) |
| Position (left/right/mid), n | 6/4/3* |
| Pre-procedure Kothari-Haber score, mean (SD) | 6 (2.16) |
| Procedure characteristics | |
| Technical success, n (%) | 13 (100%) |
| KJ-POEM technique, (n, %) | |
| Direct septotomy | 8 (61.54%) |
| Tunnel starting in hypopharynx | 0 (0) |
| Tunnel starting at septum | 5 (38.46) |
| Length of tunnel/septotomy, mean (SD), cm | 2.11 (1.19) |
| Number of clips used, mean (SD) | 4 (1.58) |
| Total procedure duration, mean (SD), minutes | 42.92 (21.78) |
| Type of knife used, (n, %) | |
| T-type hybrid knife | 6 (46.15) |
| I-Type hybrid knife | 4 (30.76) |
| Triangular tip knife | 3 (23.07) |
| Intraprocedural adverse events, n (%) | 0 (0) |
| Post-procedure outcomes | |
| Length of hospital stay, mean (SD), days | 1.09 (0.74) |
| Delayed (< 30 days after the procedure) adverse events, n (%) | 0 (0) |
| Post-procedure Kothari-Haber score, mean (SD) | 0.91 (0.99) |
| Length of post-procedure NPO time, mean (SD), hours | 19.07 (8.02) |
| Clinical success (number, %) | 13 (100) |
| Follow-up period, mean (SD), months | 9.41 (10.07) |
Eight patients (61.54%) underwent over-the-septum diverticulotomy, while five patients (38.46%) underwent proximal submucosal tunneling diverticulotomy. Mean total procedure time was 42.92 minutes (SD 21.78). The mean number of clips used for mucosal closure was four (SD 1.58). The most common type of knife used was triangular tip knife (Olympus; Tokyo, Japan) in six patients (46.15%).
Primary and secondary outcomes
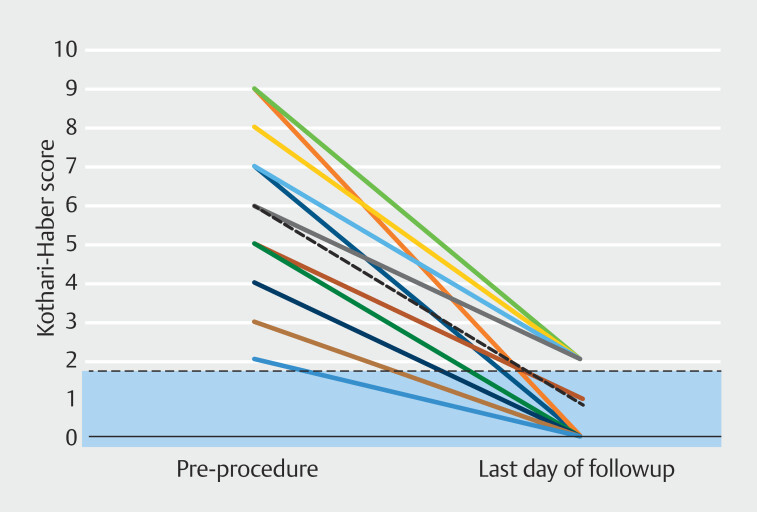
Clinical and technical success was achieved in all cases (100%) with a mean post-procedure Kothari-Haber score of 0.91 (SD 0.99). There was a significant reduction in the Kothari-Haber score after KJ-POEM ( P < 0.001; Table 2 ; Fig. 2 ). There were no AEs and no cases of injury to the recurrent laryngeal nerve. Mean length of hospital stay was 1.09 days (SD 0.74). Mean follow-up time was 9.41 months (SD 10.07) post-procedure. There was no post-procedure symptom recurrence in any of the patients.
Table 2 Pre and post-KJ-POEM Kothari-Haber score.
| Variable | Pre-KJ-POEM, mean (SD) |
Post-KJ-POEM, mean (SD) |
P value |
| One patient had bilateral diverticula, one on left, and one on right side. KJ-POEM, Killian-Jamieson per-oral endoscopic myotomy; SD, standard deviation. | |||
| Kothari-Haber score | 6 (2.16) | 0.91(0.99) | < 0.001 |
Fig. 2.
Pre- and post-procedure Kothari-Haber scores.
Discussion
Because of the rarity of the condition and limited number of reported cases, optimal management of KJD has not been adequately reported. Currently, available endoscopic techniques include direct septotomy 6 7 , tunneling diverticulotomy (tunnel starting in the hypopharynx proximal to the septum of the diverticulum) 5 6 7 , and ultra-short tunnel technique (tunnel at the septum of the diverticulum) 12 .
One retrospective review by Modayi et al. examined outcomes and complication rates of direct and tunneling diverticulotomy (with hypopharyngeal tunnel or ultra-short tunnel) in 13 patients with KJD 12 . Results showed a 92% (12/13) clinical success rate with complete symptom resolution. They reported no incidence of bleeding, mediastinitis, or sign of recurrent laryngeal nerve (RLN) injury. In 2019, Haddad et al. reported a literature review of 68 KJD cases, of which only 10 patients had an endoscopic procedure. The endoscopic approaches comprised a variety of techniques, such as flexible endoscopic diverticulotomy and rigid endoscopic laser diverticulotomy. Two of the 10 patients who had endoscopic procedures experienced recurrence. One was managed with transcervical surgery and the other with repeat endoscopic surgery 13 .
More recently, there have been published case reports about the efficacy of endoscopic management of KJD, particularly KJ-POEM 2 3 4 5 6 7 8 9 . All the case reports showed promising clinical outcomes with no complications. Our study shows similar safety and efficacy results for KJ-POEM, with a clinical success rate of 100% and no reports of symptom recurrence. There were only two reports of remaining diverticula after KJ-POEM, both asymptomatic. There were no moderate or severe AEs.
The retrospective observations presented in this study carry some expected limitations. Being a multicenter study, there is an inherent variability in techniques and follow-up protocols across multiple centers/providers. The sample size was also relatively small, attributed to the infrequent incidence of symptomatic KJD and the novelty of KJ-POEM procedure.
Even though an endoscopic approach historically has been avoided due to concern for RLN injury 14 15 16 17 18 19 20 21 , KJ-POEM has gained significant traction in recent times 22 23 24 . KJ-POEM appears to be promising as a novel therapeutic avenue for managing KJD. This study cohort includes more direct septotomy – KJ-POEM case experience than other studies, which stands out as a notable strength of this investigation.
Conclusions
In conclusion, this study suggests that KJ-POEM is a safe and effective alternative treatment for symptomatic KJD with excellent long-term outcomes and minimal symptom recurrence. Further prospective studies involving larger patient cohorts and longer follow-up periods are warranted to comprehensively assess its long-term effectiveness in comparison to other treatment modalities.
Footnotes
Conflict of Interest The following authors disclosed financial relationships: M. A. Khashab: Consultant for Boston Scientific, Olympus America, Medtronic, Apollo Endosurgery, Pentax, and GI Supply; royalties from UpToDate and Elsevier. H. Inoue: Advisor for Olympus Corporation and Top Corporation; educational grants from Olympus Corporation and Takeda Pharmaceutical Co. All other authors disclosed no financial relationships.
References
- 1.Alnimer L, Zakaria A, Piper M. Killian Jamieson diverticulum: a rare cause of dysphagia. Cureus. 2021;13:e13654. doi: 10.7759/cureus.13654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Félix C, Barreiro P, Rodrigues J et al. A rare case of bilateral Killian-Jamieson diverticula treated endoscopically. Endoscopy. 2022;54:E283–E284. doi: 10.1055/a-1517-6390. [DOI] [PubMed] [Google Scholar]
- 3.Lee CK, Chung IK, Park JY et al. Endoscopic diverticulotomy with an isolated-tip needle-knife papillotome (Iso-Tome) and a fitted overtube for the treatment of a Killian-Jamieson diverticulum. World J Gastroenterol. 2008;14:6589. doi: 10.3748/wjg.14.6589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanders D, Murray T, Donnellan F. Endoscopic management of Killian-Jamieson diverticulum. VideoGIE. 2019;4:364–365. doi: 10.1016/j.vgie.2019.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shimamura Y, Fujiyoshi MRA, Fujiyoshi Y et al. Per-oral endoscopic myotomy as treatment for Killian–Jamieson diverticulum. DEN Open. 2022;2:e27. doi: 10.1002/deo2.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka I, Shimamura Y, Inoue H et al. Feasibility and safety of per-oral endoscopic septotomy for Killian-Jamieson diverticulum: a case series with video. Dig Endosc. 2024;36:895–903. doi: 10.1111/den.14738. [DOI] [PubMed] [Google Scholar]
- 7.Tang SJ, Tang L, Chen E et al. Flexible endoscopic Killian-Jamieson diverticulotomy and literature review (with video) Gastrointest Endosc. 2008;68:790–793. doi: 10.1016/j.gie.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Yang D, Draganov PV. Endoscopic Killian–Jamieson diverticulotomy using a scissor-type electrosurgical knife. Endoscopy. 2018;50:E175–E176. doi: 10.1055/a-0601-6467. [DOI] [PubMed] [Google Scholar]
- 9.Yun PJ, Huang HK, Chang H et al. Endoscopic diverticulotomy with a stapler can be an effective and safe treatment for Killian-Jamieson diverticulum. J Thorac Dis. 2017;9:E787. doi: 10.21037/jtd.2017.08.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kothari TH, Kothari S, Bittner K et al. The “Kothari-Haber” scoring system: a prospective evaluation of pre-and post-procedure outcomes for patients undergoing endoscopic myotomy for Zenker’s diverticulum. Gastrointest Endosc. 2018;87:AB289–AB290. [Google Scholar]
- 11.Cotton PB, Eisen GM, Aabakken L et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454. doi: 10.1016/j.gie.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 12.Modayil RJ, Zhang X, Ali M et al. Endoscopic diverticulotomy for Killian-Jamieson diverticulum: mid-term outcome and description of an ultra-short tunnel technique. Endosc Int Open. 2022;10:E119–E126. doi: 10.1055/a-1548-5552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haddad N, Agarwal P, Levi JR et al. Presentation and management of Killian Jamieson diverticulum: a comprehensive literature review. Ann Otol Rhinol Laryngol. 2020;129:394–400. doi: 10.1177/0003489419887403. [DOI] [PubMed] [Google Scholar]
- 14.Ataka R, Tsunoda S, Goto S et al. Killian-Jamieson diverticulum safely resected using a manual intraoperative neural monitoring system: a case report. Surg Case Rep. 2020;6:1–5. doi: 10.1186/s40792-020-00805-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang YC, Chi CY, Lee CJ. Rigid endoscopic LASER diverticulotomy for lateral pharyngoesophageal diverticuli: cases presentation and discussion. Eur Arch Otorhinolaryngol. 2016;273:4637–4642. doi: 10.1007/s00405-016-4080-8. [DOI] [PubMed] [Google Scholar]
- 16.Howell R, Tang A, Allen J et al. Killian Jamieson Diverticulum, the great mimicker: A Case series and contemporary review. Laryngoscope. 2022;133:2110–2115. doi: 10.1002/lary.30508. [DOI] [PubMed] [Google Scholar]
- 17.Jeismann VB, Bianchi ET, Szachnowicz S et al. Surgical treatment of Killian‐Jamieson diverticulum: A case report and literature review. Clin Case Rep. 2019;7:1374. doi: 10.1002/ccr3.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim DC, Hwang JJ, Lee WS et al. Surgical treatment of Killian-Jamieson diverticulum. Korean J Thorac Cardiovasc Surg. 2012;45:272. doi: 10.5090/kjtcs.2012.45.4.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kohei S, Satoru M, Tanaka T et al. Surgery for Killian-Jamieson diverticulum: a report of two cases. Surg Case Rep. 2020;6:17. doi: 10.1186/s40792-020-0789-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurahashi Y, Hojo Y, Nakamura T et al. Endoscopic observation of the palisade vessels in Killian–Jamieson diverticulum was useful for diagnosis and surgical treatment: a case report. Surg Case Rep. 2020;6:1–4. doi: 10.1186/s40792-020-00949-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oh J, Norris A, Artigue M et al. Killian-Jamieson Diverticulum: Management of a rare esophageal diverticula. Cureus. 2021;13:e17820. doi: 10.7759/cureus.17820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saito T, Ogawa T, Kurahashi S et al. A novel Killian–Jamieson diverticulectomy using a thyroid gland flap: a case report. Surg Case Rep. 2020;6:1–5. doi: 10.1186/s40792-020-01060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stavropoulos SN, Ali MF, Zhang X et al. Endoscopic direct and tunneling diverticulotomy techniques for Killian Jamieson diverticulum: Report of twelve cases. Gastrointest Endosc. 2019;89:AB180. [Google Scholar]
- 24.Zakaria A, Barawi M. Endoscopic treatment of Killian-Jamieson diverticulum using submucosal tunneling diverticulotomy technique. VideoGIE. 2020;5:525–526. doi: 10.1016/j.vgie.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]