Cardiac herniation and contrast leakage from the left pulmonary artery.
Central Message.
Cardiac herniation must not be forgotten as a potential complication after intrapericardial pneumonectomy. Emergency chest compression can exacerbate heart malposition and cause fatal hemorrhage.
This is a case of 74-year-old woman diagnosed with squamous cell carcinoma of the right upper bronchus. Computed tomography showed a 44 × 40 × 25-mm solid tumor in the right upper lobe, which invaded to the right main bronchus. Preoperative staging was cT2bN1M0, stage IIB. Because of interstitial pneumonia, surgery was chosen as the treatment. Right upper lobe sleeve lobectomy and S6 sleeve segmentectomy were performed. Due to intraoperative suspicion of pericardial tumor invasion, the pericardium was also resected from the superior vena cava inflow area to the periphery of the right main pulmonary artery. Because the pericardiectomy was small and the residual lung volume was large, no repair was performed. Pathology revealed a squamous cell carcinoma without pericardial invasion. The tumor measured 44 × 40 × 35 mm, and a mediastinal lymph node was positive. Pathological staging was pT2bN2M0, stage IIIA.
Although the anastomosis was wrapped with pericardial fat, dehiscence occurred, necessitating a right intrapericardial sleeve pneumonectomy 4 weeks after the initial surgery. The pericardial incision was extended to secure the right main pulmonary artery in the pericardial sac, between the superior vena cava and the ascending aorta, and to ensure safe visualization due to adhesions around the right main pulmonary artery. The pericardial defect was reinforced with a pericardial fat to avoid the risk of myocardial injury associated with adhesion within the pericardium.
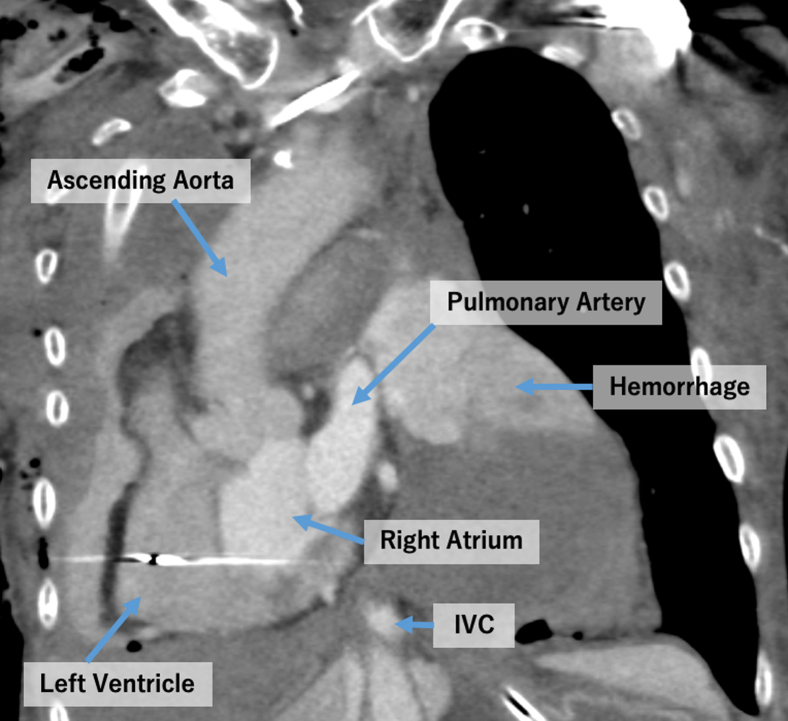
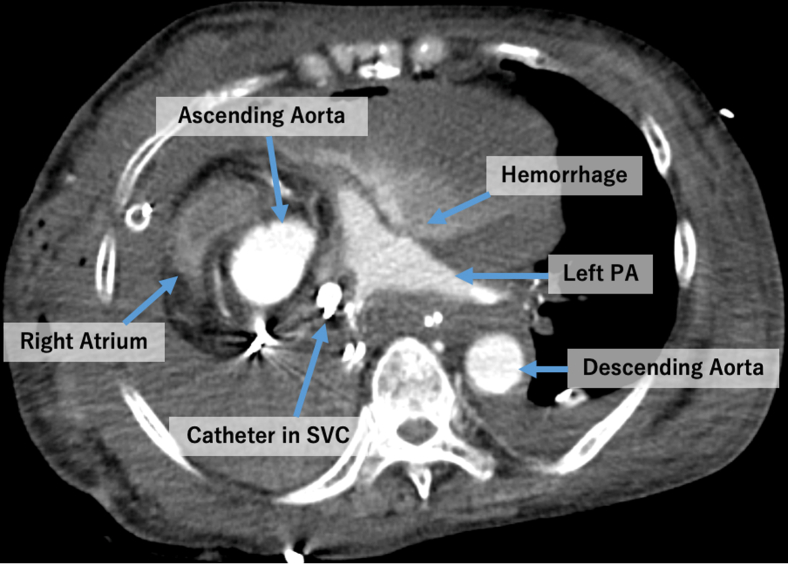
One hour after the end of the reoperation, the patient had a sudden cardiac arrest and underwent immediate cardiopulmonary resuscitation (CPR). There was no response to CPR, and venoarterial extracorporeal membrane oxygenation was initiated. An urgent chest computed tomography scan revealed horizontal rotation of the heart around the superior and inferior vena cava with significant contrast leakage from the left main pulmonary artery (Figures 1 and 2). These findings led to a diagnosis of right-sided cardiac herniation and pulmonary artery hemorrhage as a result of external cardiac massage. CPR was discontinued, and the patient was pronounced dead.
Figure 1.
Cardiac herniation and contrast leakage from the left pulmonary artery. IVC, Inferior vena cava.
Figure 2.
Cardiac herniation and contrast leakage from the left pulmonary artery. PA, Pulmonary artery; SVC, superior vena cava.
Cardiac herniation is rare but must be considered as a potential complication after intrapericardial pneumonectomy, with an incidence rate of 0.2% to 0.5%.1 Immediate diagnosis is essential because the mortality is 100% in unrecognized cases and 50% in cases in which the diagnosis is made.2
In this case, 2 critical mistakes were made. First, the pericardial defect was reinforced with pericardial fat, but the reinforcement was insufficient to prevent cardiac herniation. A biological patch would have been more appropriate in this infected area to prevent cardiac herniation. Second, an emergency thoracotomy should have been performed instead of obtaining a computed tomography scan and performing chest compressions. Thoracotomy is the only effective treatment for cardiac herniation, and the external force applied during chest compressions exacerbates the heart malposition and can cause catastrophic hemorrhage. If necessary, an emergency thoracotomy should have been performed in the recovery room, not in the operating room. Therefore, it is crucial to provide strong pericardial reinforcement to prevent cardiac herniation and not to hesitate to perform an emergency thoracotomy in case of a sudden change after an intrapericardial pneumonectomy.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Informed consent for publication was obtained, and this research received Institutional Review Board approval on October 24, 2023, Number S23-086.
References
- 1.Tschersich H.U., Skorapa V., Fleming W.H. Acute cardiac herniation following pneumonectomy. Radiology. 1976;120(3):546. doi: 10.1148/120.3.546. [DOI] [PubMed] [Google Scholar]
- 2.Veronesi G., Spaggiari L., Solli P.G. Cardiac dislocation after extended pneumonectomy with pericardioplasty. Eur J Cardiothorac Surg. 2001;19(1):89–91. doi: 10.1016/s1010-7940(00)00612-6. [DOI] [PubMed] [Google Scholar]