Abstract
We report the first case of disseminated infection with both Actinomyces graevenitzii and Mycobacterium tuberculosis and review the medical literature. Concomitant actinomycosis and tuberculosis is very rare. The potential of the facultatively aerobic, newly described A. graevenitzii for disseminated invasive infection needs to be evaluated.
Most infections with Actinomyces spp. are polymicrobial (19). The copathogens are most commonly colonizers of the respective involved organ systems. They act synergistically by inhibiting host defense mechanisms and/or reducing oxygen tension in the affected tissue, which enhances growth of Actinomyces spp. (19). We present a unique case of concomitant disseminated actinomycosis and tuberculosis and a review of the medical literature.
A 46-year-old African-American male presented with a 4-week history of fever, night sweats, a productive cough, and a 30-pound weight loss. He denied any chest pain, shortness of breath, or hemoptysis. He was not aware of any sick contacts, and he had not been incarcerated or homeless.
His past medical history was significant for coronary artery disease, hypertension, and chronic congestive heart failure. There were no known drug allergies and no current drug, tobacco, or alcohol use. He admitted to smoking crack cocaine years ago. There was no travel history nor exposure to animals nor recreational or professional outdoor activities.
Three weeks prior to this admission, he had been seen for the same symptoms and was discharged after computed tomography (CT) of the chest with a presumptive diagnosis of community-acquired pneumonia and treated with doxycycline.
His physical exam on admission was within normal limits except for a temperature of 39.1°C and severe periodontal disease. Abnormal laboratory parameters were a sodium level of 129 mmol/liter, an albumin level of 2.8 g/dl, microcytic anemia with a hemoglobin level of 10.4 g/dl (MCV, 72.6 fl), and a platelet count of 596,000/μl. The human immunodeficiency virus type 1 (HIV-1) and HIV-2 serologies were negative. Urine and several blood cultures remained without growth throughout the hospital stay.
Computed tomography of the thorax revealed a large right-upper-lobe cavity with surrounding airspace disease (Fig. 1B). For comparison, a CT 3 weeks prior to admission had shown a right paratracheal mass (Fig. 1A). A tuberculin skin test was not performed.
FIG. 1.
CT scans of the thorax. A: 3 weeks prior to admission, showing a right paratracheal mass. B: on admission, showing a right-upper-lobe cavernous lesion with surrounding airspace disease. C: complete resolution of all pulmonary lesions after 6 months of antibacterial and tuberculostatic therapy.
Treatment was started empirically with rifampin, isoniazid, pyrazinamide, and ethambutol for presumed tuberculosis, which was later confirmed by direct smear (1 day after admission) and culture (11 days after admission). Upon notification of the presence of Actinomyces spp. in the sputum (48 h after admission), treatment was extended to intravenous ampicillin for suspected actinomycosis. Again, a tuberculin skin test was not performed due to poor predictive values in the special patient population served in our institution (indigenous urban population with high rates of HIV infection).
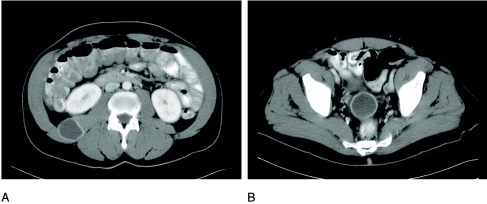
After 10 days of treatment, the patient complained of right flank pain and constipation. A CT of the abdomen showed fluid collections with contrast enhancement in the right perilumbar area (Fig. 2A) and in the cul de sac between rectum and bladder (Fig. 2B). The liver did not show any lesions on CT.
FIG. 2.
CT of the abdomen, revealing fluid collections with contrast enhancement in the right quadratus lumborum muscle (A) and in the cul de sac between rectum and bladder (B).
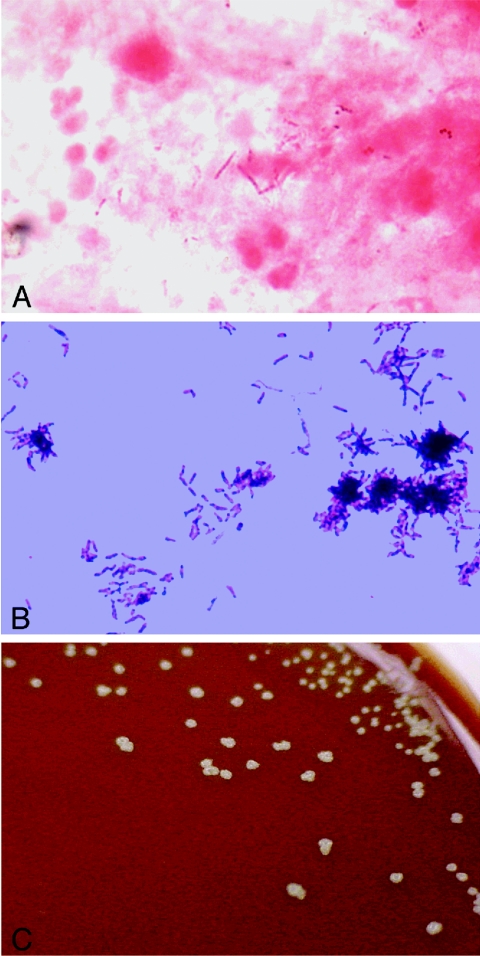
Needle aspirates from both abscesses again showed numerous acid-fast bacilli, identified as M. tuberculosis, upon Ziehl-Neelsen staining (Fig. 3A) and many filamentous gram-positive rods (Fig. 3B). Aerobic and anaerobic cultures remained without growth.
FIG. 3.
Microphotographs and colony morphology of aspirate from the right flank abscess. Panel A shows numerous acid-fast bacilli (Ziehl-Neelsen stain). Panel B shows numerous filamentous, branching gram-positive rods (Gram stain). C shows the typical “molar tooth” appearance of colonies on chocolate agar.
After 6 months of antituberculous therapy and oral ampicillin, the patient underwent a repeat CT that showed complete resolution of all lesions in the lung (Fig. 1C) and abdomen.
The Gram stain of the expectorated sputum sample on admission was read as normal oropharyngeal flora, with >25 leukocytes and 10 to 25 epithelial cells per low-power field (grade 4 according to the Barlett Grading System) (11). The aerobic culture (37°C at 5% CO2) showed heavy growth of gram-positive rods in long chains. The colonies on the chocolate agar plate had a characteristic “molar tooth” appearance (Fig. 3C). No sulfur granules were seen in the sputum. The organism was initially identified by the hospital laboratory as Actinomyces spp. on the basis of Gram stain characteristics, colony morphology, and commercial biochemical testing (RapID ANA II; Innovative Diagnostic Systems, Inc., Atlanta, GA). The isolate was then sent to a reference laboratory. Upon repeat biochemical testing, the isolate was reidentified as a Bifidobacterium spp.
For definitive identification, the DNA of the isolate was subjected to 16S rRNA gene sequencing via PCR. The sequence data were analyzed by assembling the forward and reverse sequences into a consensus sequence. This consensus sequence was edited to resolve discrepancies between the two strands by evaluation of the electropherogram. For an accurate determination of species similarities, the 5′ and 3′ ends were cut at identical positions along the gene. Finally, the consensus sequence was compared with a database available on MicroSeq 1.4 (Applied Biosystems, Inc.) and also a Mayo Clinic Foundation database containing wild-type strains and well-characterized patient specimens. The patient's isolate sequence was aligned with its related type strain sequences using BIOEDIT v. 5.0.9 (Department of Microbiology, North Carolina State University; http://www.mbio.ncsu.edu/bioedit/bioedit.html). The resulting multiple sequence alignment was used to construct the phylogenetic tree with the unweighted pair group method using arithmetic averages algorithm and a distance matrix estimate with WET (Windows Easy Tree 1.31, developed by J. Dopazo; available at http://www.tdi.es/programas/WET.html). As shown in Table 1, the isolate is most closely aligned with Actinomyces graevenitzii, with 1.3% divergence from a reference strain.
TABLE 1.
Comparison of 16S rRNA sequence differences of the patient specimen with those of other members of the Actinomyces genusa
| Species no. | Species | % Difference
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
| 1 | A. bovis C867 | 0.0 | 13.3 | 15.1 | 10.0 | 13.4 | 13.7 | 9.6 | 17.7 | 13.9 | 19.4 | 15.7 | 6.8 | 10.5 |
| 2 | A. georgiae TS49285 | 0.0 | 17.3 | 13.1 | 16.6 | 3.4 | 15.5 | 16.7 | 4.6 | 14.1 | 6.5 | 12.9 | 13.8 | |
| 3 | A. gerencseriae TS23860 | 0.0 | 17.0 | 9.4 | 18.7 | 11.6 | 19.1 | 18.7 | 17.6 | 18.3 | 14.0 | 18.1 | ||
| 4 | A. graevenitzii (clinical) | 0.0 | 14.5 | 13.7 | 15.0 | 17.0 | 13.7 | 18.1 | 13.3 | 11.8 | 1.3 | |||
| 5 | A. israelii TS12012 | 0.0 | 17.9 | 10.8 | 19.7 | 18.3 | 18.1 | 17.9 | 12.4 | 15.7 | ||||
| 6 | A. meyeri TS35568 | 0.0 | 16.6 | 16.0 | 2.1 | 12.5 | 6.3 | 13.2 | 14.4 | |||||
| 7 | A. naeslundii TS12104 | 0.0 | 20.7 | 16.8 | 19.8 | 17.3 | 5.3 | 16.1 | ||||||
| 8 | A. neuii TS51849 | 0.0 | 16.1 | 14.8 | 17.3 | 18.1 | 17.8 | |||||||
| 9 | A. odontolyticus TS17929 | 0.0 | 13.6 | 6.1 | 13.4 | 14.5 | ||||||||
| 10 | A. radingae TS51856 | 0.0 | 15.4 | 18.7 | 19.0 | |||||||||
| 11 | A. turicensis TS51857 | 0.0 | 15.2 | 14.2 | ||||||||||
| 12 | A. viscosus TS15987 | 0.0 | 13.0 | |||||||||||
| 13 | Patient sample | 0.0 | ||||||||||||
Species numbers were arbitrarily assigned.
The mycobacterial sputum culture on admission eventually grew Mycobacterium tuberculosis (identification by Accuprobe, GenProbe Inc., San Diego, California). Standard susceptibility testing showed that it was fully susceptible to isoniazid, rifampin, ethambutol, and pyrazinamide.
Actinomyces spp. are anaerobic to capnophilic or aerotolerant (facultatively anaerobic), nonsporulating, gram-positive bacteria that tend to form branching rods and filaments and have a fermentative type of carbohydrate metabolism (19). They are normal inhabitants of the buccal cavity and human stool, and there is no environmental reservoir.
Coinfection of other pathogens with Actinomycosis spp. has been previously described for 954 of 960 Swedish isolates (2). The suspected pathogenesis is a synergistic effect: oxygen deprivation through other bacteria leads to growth enhancement of the microaerophilic Actinomyces species (1). Enhancement of infection with Actinomyces spp. by coinoculation of Eikenella corrodens in an animal model has been reported (3). Coaggregation of Actinomyces and Streptococcus spp. leads to increased resistance to phagocytosis in a mouse peritonitis model (13, 14).
The most common copathogens for thoracic actinomycosis are Actinobacillus actinomycetemcomitans, Streptococcus spp., and Haemophilus spp. (19).
Disseminated actinomycosis presents a special challenge to clinicians by presenting with prolonged, multisystem manifestations mimicking other diseases. In a recent review, predominantly, A. meyeri, A. israeli, and A. odontolyticus were identified in cases of disseminated disease (4).
A. graevenitzii was first isolated from four clinical human specimens (three respiratory and one bone sample) in 1997 by a Swedish group (18). Like the other Actinomyces spp., it is a nonmotile, branched, and nonsporulating gram-positive rod which is catalase negative and facultatively anaerobic and has a distinct biochemical profile (18, 21). It has been recently identified in the saliva of infants (20).
In contrast to other microorganisms, M. tuberculosis seems to play only a minor role as a copathogen in actinomycosis. We performed a PubMed search with the term “actinomyces” or “actinomycosis” combined with the term “tuberculosis.” Additionally, we searched review articles and medical textbooks on actinomycosis.
The clinical features of the cases found in the literature are shown in Table 2. In total, seven cases could be located in the English literature. Of note, all isolates with reported species information were A. israelii, but information about the exact method of identification was often lacking. All patients had fever and thoracic infection, and most of the isolates were recovered from respiratory specimens. None of the cases had disseminated disease. Actinomycosis coinfection with M. tuberculosis was “rarely encountered” in Holm's series of 960 clinical isolates (7).
TABLE 2.
Overview of present case and seven reported cases with clinical informationa
| Characteristic | Present case | Stein et al. (22) | Chakravarty and Fernandez (2)
|
Lee (9) | Bates and Cruickshank (1)
|
von Arnim (23) | ||
|---|---|---|---|---|---|---|---|---|
| Patient 1 | Patient 2 | Patient 1 | Patient 2 | |||||
| Age (yr) | 43 | 12 | 22 | 30 | 35 | Unknown | Unknown | 42 |
| City and state or country | New Orleans, La. | Bronx, N.Y. | Delhi, India | Delhi, India | New York, N.Y. | Leicester, UK | Leicester, UK | Berlin, Germany |
| Ethnicity | African-American | African-American | Asian Indian | Asian Indian | African-American | Caucasian | Caucasian | Caucasian |
| Comorbidity | Coronary artery disease, hypertension | None | None | None | None | Unknown | Unknown | None |
| HIV infection | No | No | Unknown | Unknown | Unknown | Not applicable | Not applicable | Not applicable |
| Fever | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Site(s) of infection | Lung cavity, soft tissue | Lung cavity, costal osteitis | Lung cavity | Bilateral lung cavities | Lung cavity | Empyema | Empyema | Lung cavity, substernal abscess |
| Identification on Gram stain | Yes (only soft tissue) | Yes (from thoracic wall abscess) | Unknown | Unknown | Yes (from pleural empyema) | Yes | Yes | Yes (from wall abscess) |
| Identification by culture | Yes (only lung) | Yes (from thoracic wall abscess) | Yes (from sputum) | Yes (from sputum) | Yes (from pleural empyema) | Unknown | Unknown | Yes |
| Actinomyces species | A. graevenitzii | A. israelii | A. israelii | A. israelii | Not reported | A. israelii | A. israelii | Not reported |
| Treatment for actinomycosis | Amoxicillin for 6 mo | Penicillin IV for 2 mo, PO for 1 mo | Penicillin IV for 3 mo | Penicillin IV for 3 mo | Penicillin IV for a total of 3 mo | Unknown | Unknown | Neoarsephenamine (Neosalvarsan) |
| Treatment for tuberculosis | RIPE for 2 mo, RI for 4 mo | INH, ethambutol, rifampin | Streptomycin and INH for 3 mo, INH and PAS for 18 mo | Streptomycin and INH for 10 wk | Unknown tuberculosis treated 4 yr before diagnosis of actinomycosis | Unknown | Unknown | Sulfonamides (symptomatic) |
| Surgery | No | No | No | No | Lung resection | Thoracoplasty | No | Incision and drainage of abscesses |
| Outcome | Healed | Recovered | Recovered | Recovered | Recovered | Recovered | Died from amyloidosis | Died of pulmonary hemorrhage |
Abbreviations: RIPE, rifampin-isoniazid-pyrazinamide-ethambutol; IV, intravenously; PO, orally; INH, isoniazid; PAS, para-aminosalicylic acid; UK, United Kingdom.
Other than these seven cases in the English literature, there are scattered case reports of coinfection from Russia and Poland (3, 5, 6, 8, 10, 15-17). These journals were not available for review.
To our knowledge, this case represents the first report of coinfection with A. graevenitzii and M. tuberculosis. It is also the first clinical description of disseminated infection with A. graevenitzii.
The presence of both organisms was well documented in a respiratory specimen of the diseased lung as well as in distant metastatic abscesses, defining this as disseminated infection. Although A. graevenitzii did not grow in the abscess fluid or in the blood culture, a typical morphology was seen on the Gram stain from the abscess fluid. Growth of microorganisms seen on the Gram stain can be significantly impeded after 10 days of appropriate therapy. Molecular diagnostic techniques would have been needed as evidence for true disseminated infection with this organism. The presence of a coinfection was recognized in a timely fashion, preventing further, possibly invasive diagnostic studies. Without the addition of a β-lactam antibiotic, the patient would most likely have suffered a prolonged hospital course.
The rarity of actinomycotic and tuberculous coinfection reports in the literature is striking and gives rise to several questions. Firstly, respiratory specimens are most likely cultured aerobically, which will negatively select most Actinomyces spp. In the original study of A. graevenitzii, isolates grew on blood agar at 37°C with 5 to 10% CO2 (18), like the specimen from our patient.
Second, Actinomyces spp. are commensals of the mouth cavity and the upper respiratory tract. Their presence in respiratory specimens does not necessarily signify clinical disease and may often not be reported. In our case and the cases described in the literature, a significant disease process was identified. We postulate that preexisting periodontal disease was the source of infection, with spread to the lungs by aspiration and subsequent hematogenous dissemination to distant soft tissues. M. tuberculosis was most likely acquired by contact with an infected individual in the community.
Third, the disseminated nature of the coinfection makes our case somewhat unique. Since little is known about the pathophysiology of A. graevenitzii infection, we can only speculate about factors that explain its dissemination. From the host perspective, our patient did not show any key conditions, such as severe immunosuppression or malnutrition, predisposing to overwhelming disease.
The fourth point of discussion is the identification of clinically important Actinomyces species. As pointed out by Sarkonen et al. (21), differentiation of these bacteria is a difficult and costly process which is most likely not done in the routine laboratory. Also, many of the recently discovered species included in the genus Actinomyces are not included in most commercial identification kits.
An interesting theory for the rarity of actinomycotic and tuberculous coinfection was pointed out by Nikiforchin (12), who suggested that there are properties of Actinomyces spp. that are inhibitory to growth characteristics of M. tuberculosis. This has not been confirmed in other studies.
Resistance to antimycobacterial drugs is a common cause of therapeutic failure in cases of tuberculosis. In the setting of full susceptibility, other entities such as coinfection might be suspected and appropriate cultures obtained. Coinfection of M. tuberculosis and Actinomyces spp. is rare and therefore presents a diagnostic challenge in clinical practice. Early identification prevents costly and prolonged diagnostic and therapeutic interventions.
Acknowledgments
We have no financial or other conflicts of interest to disclose. No financial support was granted for the study.
We thank Lynne Sloan and Jon Rosenblatt of the Mayo Clinic for help and advice in establishing phylogenetic dendrograms and distance matrix analyses.
Footnotes
Present address: University Hospital Basel, Basel, Switzerland.
REFERENCES
- 1.Bates, M., and G. Cruickshank. 1957. Thoracic actinomycosis. Thorax 12:99-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chakravarty, S. C., and J. Fernandez. 1977. Co-existence of actinomycosis of lungs with pulmonary tuberculosis. J. Indian Med. Assoc. 69:89-90. [PubMed] [Google Scholar]
- 3.Czyzewska, J., T. Owinski, and B. Remion. 1967. [Tuberculosis of the peripheral lymph nodes with coexistent actinomycosis]. Gruzlica 35:165-168. (In Polish.) [PubMed] [Google Scholar]
- 4.Felz, M. W., and M. R. Smith. 2003. Disseminated actinomycosis: multisystem mimicry in primary care. South. Med. J. 96:294-299. [DOI] [PubMed] [Google Scholar]
- 5.Goldshtein, V. D., and G. B. Mirinov. 1962. [On the combination of tuberculosis of the lungs and actinomycosis]. Klin. Med. (Mosc.) 40:107-110. (In Russian.) [PubMed] [Google Scholar]
- 6.Gondzik, M., and Z. Jasiewicz. 1975. [Case of pulmonary tuberculosis complicated by actinomycosis of the paravesical region]. Wiad. Lek. 28:1869-1871. (In Polish.) [PubMed] [Google Scholar]
- 7.Holm, P. 1950. Studies on aetiology of human actinomycosis. 1. The “other” microbes of actinomycosis and their importance. Acta Pathol. Microbiol. Scand. 28:391. [DOI] [PubMed] [Google Scholar]
- 8.Krakowka, P., K. Traczyk, and B. Ginterowa. 1962. [A case of co-existing pulmonary tuberculosis and primary actinomycosis]. Gruzlica 30:1095-1100. (In Polish.) [PubMed] [Google Scholar]
- 9.Lee, B. Y. 1966. Actinomycosis of the lung coexisting with pulmonary tuberculosis. Report of a case. Dis. Chest 50:211-213. [DOI] [PubMed] [Google Scholar]
- 10.Morozova, O. V., B. D. Girshov, and I. L. Barkan. 1966. [Tuberculosis actinomycosis and candidiasis and candidiasis in a patient with diabetes mellitus]. Klin. Med. (Mosc.) 44:122-124. (In Russian.) [PubMed] [Google Scholar]
- 11.Murray, P. R., and J. A. Washington. 1975. Microscopic and bacteriologic analysis of expectorated sputum. Mayo Clin. Proc. 50:339-344. [PubMed] [Google Scholar]
- 12.Nikiforchin, R. N. 1968. [Antagonistic properties of actinomyces isolated from patients with fibrous-cavernous pulmonary tuberculosis]. Probl. Tuberk. 46:61-65. (In Russian.) [PubMed] [Google Scholar]
- 13.Ochiai, K., K. Kikuchi, K. Fukushima, and T. Kurita-Ochiai. 1999. Co-aggregation as a virulent factor of Streptococcus sanguis isolated from infective endocarditis. J. Oral Sci. 41:117-122. [DOI] [PubMed] [Google Scholar]
- 14.Ochiai, K., T. Kurita-Ochiai, Y. Kamino, and T. Ikeda. 1993. Effect of co-aggregation on the pathogenicity of oral bacteria. J. Med. Microbiol. 39:183-190. [DOI] [PubMed] [Google Scholar]
- 15.Pellar, J., and M. Przystawa. 1968. [On the problem of coexistence of tuberculosis and actinomycosis of lymph nodes]. Wiad. Lek. 21:564-569. (In Polish.) [PubMed] [Google Scholar]
- 16.Pliner, M. A. 1977. [Simultaneous lesion of the lymph nodes of the submandibular region and neck from actinomycosis and tuberculosis]. Stomatologiya (Mosc.) 56:34-37. (In Russian.) [PubMed] [Google Scholar]
- 17.Pliner, M. A., G. V. Dymchenko, and L. S. Kalachev. 1971. [A case of combined lesions of the cervical lymph nodes from actinomycosis and tuberculosis]. Probl. Tuberk. 49:78-80. (In Russian.) [PubMed] [Google Scholar]
- 18.Ramos, C. P., E. Falsen, N. Alvarez, E. Akervall, B. Sjoden, and M. D. Collins. 1997. Actinomyces graevenitzii sp. nov., isolated from human clinical specimens. Int. J. Syst. Bacteriol. 47:885-888. [DOI] [PubMed] [Google Scholar]
- 19.Russo, T. A. 2000. Agents of actinomycosis, p. 2645-2654. In G. L. Mandell, J. E. Bennett, and R. Dolin (ed.), Principles and practices of infectious diseases. Chrchill Livingstone, Philadelphia, Pa.
- 20.Sarkonen, N., E. Kononen, P. Summanen, A. Kanervo, A. Takala, and H. Jousimies-Somer. 2000. Oral colonization with Actinomyces species in infants by two years of age. J. Dent. Res. 79:864-867. [DOI] [PubMed] [Google Scholar]
- 21.Sarkonen, N., E. Kononen, P. Summanen, M. Kononen, and H. Jousimies-Somer. 2001. Phenotypic identification of Actinomyces and related species isolated from human sources. J. Clin. Microbiol. 39:3955-3961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stein, C. A., J. Ernst, M. Stern, T. J. Daley, and W. B. Caspe. 1983. Thoracic actinomycosis in a recent tuberculin converter. Pediatr. Infect. Dis. 2:52-55. [DOI] [PubMed] [Google Scholar]
- 23.von Arnim, H. H. 1949. On a case of simultaneous thoracic actinomycosis and tuberculosis of the lung. Beitr. Klin. Tuberk. Spezif. Tuberk.-Forsch. 101:595-607. (In German.)