Abstract
Sabin strains of poliovirus used in the manufacture of oral poliovirus vaccine (OPV) are prone to genetic variations that occur during growth in cell cultures and the organisms of vaccine recipients. Such derivative viruses often have increased neurovirulence and transmissibility, and in some cases they can reestablish chains of transmission in human populations. Monitoring for vaccine-derived polioviruses is an important part of the worldwide campaign to eradicate poliomyelitis. Analysis of vaccine-derived polioviruses requires, as a first step, their isolation in cell cultures, which takes significant time and may yield viral stocks that are not fully representative of the strains present in the original sample. Here we demonstrate that full-length viral cDNA can be PCR amplified directly from stool samples and immediately subjected to genomic analysis by oligonucleotide microarray hybridization and nucleotide sequencing. Most fecal samples from healthy children who received OPV were found to contain variants of Sabin vaccine viruses. Sequence changes in the 5′ untranslated region were common, as were changes in the VP1-coding region, including changes in a major antigenic site. Analysis of stool samples taken from cases of acute flaccid paralysis revealed the presence of mixtures of recombinant polioviruses, in addition to the emergence of new sequence variants. Avoiding the need for cell culture isolation dramatically shortened the time needed for identification and analysis of vaccine-derived polioviruses and could be useful for preliminary screening of clinical samples. The amplified full-length viral cDNA can be archived and used to recover live virus for further virological studies.
Live trivalent oral poliovirus vaccine (OPV) prepared from attenuated Sabin strains is highly efficacious, and its worldwide use resulted in eradication of poliomyelitis in the United States (41) and most other countries (37, 38). Roughly half of the approximately eight cases reported yearly in the United States involved immunodeficient individuals. Vaccine-derived poliovirus (VDPV) strains isolated from stools of individuals with vaccine-associated paralytic poliomyelitis (VAPP) have been found to contain a number of mutations and exhibit increased neurovirulence. While some of the mutations occurring in VDPV strains restore the sequences present in the wild-type progenitors of the vaccine strains (direct reversions), other mutations either are incidental or are second-site suppressors of attenuated phenotype. All three Sabin strains contain a single base change in the same domain of the 5′ untranslated region (5′-UTR) that contributes to the attenuated phenotype, as indicated by increased neurovirulence in strains where this base change is reversed or altered by a compensating mutation (17, 31). Such Sabin strain variants with reversion in the 5′-UTR have been identified in type 3 (5, 17), type 2 (30), and type 1 (9, 24) isolates from patients with VAPP, as well as from healthy vaccine recipients (1, 11, 16, 42). Isolation of such variants from both VAPP cases and healthy vaccinees (5, 17, 19, 35) makes the cause-effect relationship between these mutations and paralytic disease less apparent and suggests that development of paralytic disease may involve both viral and host factors. Nevertheless, the emergence of these poliovirus variants can be a necessary first step in the development of paralytic disease in vaccinees or their contacts. Prolonged circulation of VDPVs in inadequately immunized populations has led to outbreaks of poliomyelitis in Egypt (49, 54), the Philippines (48), the Dominican Republic and Haiti (25, 29), and Madagascar (40), which were caused by highly divergent VDPV strains. These outbreaks, attributable to VDPVs, illustrate a serious challenge to development of a safe strategy for phasing out OPV use after global eradication is achieved. This can be done only by gaining a better understanding of the driving forces and the mechanisms behind the emergence of the newly virulent VDPVs. Important questions about the emergence of VDPV can be answered only by conducting a large-scale worldwide screening of poliovirus isolates and by studying genetic stability of vaccine strains in vaccine recipients. As part of the global eradication effort, genetic analysis of thousands of poliovirus isolates from stool samples from acute flaccid paralysis (AFP) cases, their contacts, and the environment is being done by the global laboratory network supported by the World Health Organization.
Presently, identification and characterization of polioviruses in stool specimens collected from OPV vaccinees and VAPP patients require virus isolation in susceptible tissue cultures (33, 52). More that one cell culture is typically used, because the strains have often-unpredictable preferences for growth in different cell substrates. A second cell culture passage, in the presence of specific neutralizing antisera, is usually required to identify the viral serotypes in the isolate. One shortcoming of this approach is that viruses isolated after passages in cell culture may not be representative of the viral diversity in the original stool specimen (13, 15). Another disadvantage of the culture method is that it can take anywhere from 1 to 3 weeks to obtain a result. Finally, this method requires high level of biological containment in thousands of laboratories around the world that are involved in this effort.
Recently we have shown that viral cDNA prepared from highly purified viral RNA can be PCR amplified to generate complete infectious copies of viral genome. These full-length PCR (FL-PCR) amplicons can be subsequently used for analysis by hybridization and sequencing. They can also be used for rederivation of infectious virus by transfecting susceptible cell cultures with RNA transcripts of the cDNA amplicon, a procedure that was shown to preserve heterogeneity of the original viral populations (10). Here we describe modifications of the protocol that enabled us to amplify the entire genome of poliovirus starting from viral RNA isolated directly from stool specimens. We also describe development of oligonucleotide microarray technique for determination and quantification of reversions in the 5′-UTRs of vaccine-derived strains and the use of another microarray method for screening of viral mutations and analysis of the overall genomic organization of recombinant strains. The entire analysis can be performed within a few days and provides comprehensive information about the genetic diversity of polioviruses in the sample. This new method offers an attractive shortcut that eliminates the need for virus cultivation in cell cultures and enables rapid identification and genotyping of polioviruses in clinical and environmental samples, and it can also be adapted for other viruses.
MATERIALS AND METHODS
Specimen collection.
Subjects consisted of infants from a poliovirus vaccine study performed in mid-1990s at St. Louis University and at the University of Maryland (39). The study was designed to analyze reversion of Sabin strains in vaccine recipients after OPV vaccination of subjects previously immunized with inactivated polio virus vaccine (IPV); the study was approved by the institutional review boards of the participating institutions. Group 1 samples included stool specimens collected 1 week after the first OPV dose. Group 2 included stool specimens collected 1 week after the third dose of OPV. Group 3 included stool specimens collected 1 week after the first IPV dose. Group 4 included stool specimens collected 1 week after an OPV dose that came after two doses of IPV. Group 5 included stool specimens collected 3 weeks after an OPV dose that came after two doses of IPV. The specimens were kept frozen until processing. Two stool specimens from patients with AFP were also used in this study. Specimen 18050 was collected at day 7 after onset of AFP and 10 days after OPV vaccination. Specimen 18058 was collected at day 3 after onset of AFP and 11 days after OPV vaccination.
Viruses.
Sabin strains of types 1, 2, and 3 (GenBank accession numbers AY184219, AY1842120, and AY184221, respectively) were U.S. neurovirulence reference samples. Stocks of VDPV isolate 11262 (99/056-252-14; GenBank accession number AF462418) and of wild-type Mahoney and Leon/37 strains (GenBank accession numbers NC002058 and K01392, respectively), as well as VDPV isolate 154, were grown in HEp-2 cells. Viral RNA was extracted from clarified cell culture supernatant, converted to cDNA by using SuperScript II reverse transcriptase and primers complementary to the 3′ end of poliovirus RNA, and amplified by FL-PCR as described below for stool samples.
Stool sample preparation and extraction of viral RNA.
One gram of frozen stool was vortexed in 10 ml of Dulbecco's phosphate-buffered saline and centrifuged at 325 × g for 10 min, and the supernatants were aliquoted (1.5 ml per vial). A total of 140 μl of the stool supernatant was added to the QIAamp viral RNA minikit (QIAGEN) for isolation of RNA according to the manufacturer's protocol. The extracted RNA was eluted in a final volume of 60 μl of sterile RNase-free water.
Determination of FL-PCR sensitivity for detection of OPV in stool samples.
A series of 10-fold dilutions (0.14 × 10−1 to 0.14 × 10−7) of Sabin 1 virus suspension containing 107 50% tissue culture infectious doses (TCID50) per ml was prepared, spiked into poliovirus-free stool supernatant, and processed as described above.
Reverse transcription.
Viral cDNA was prepared by reverse transcription of viral RNA. Ten microliters of RNA was added to a reaction mixture that contained 1 mM dithiothreitol, 2.5 μg/ml of each primer (A7-Sabin1,3 and A7-Sabin2) (Table 1), 0.5 mM of deoxynucleoside triphosphate mix, and 1× first-strand reverse transcription buffer (50 mM Tris-HCl, pH 8.3, 75 mM KCl, 3 mM MgCl2) (Life Technologies Inc., Gaithersburg, MD). The final volume of the reaction mix was 50 μl. The mixture was heated for 5 min at 65°C and quickly chilled on ice. Superscript II at 12 U/μl was added to the mixture and incubated for 2 hours at 42°C, and then and additional 4 U/μl Superscript II was added and the mixture was incubated for another 2 to 3 h at 42°C. Tubes were then held at 4°C until PCR amplification.
TABLE 1.
Primers used to specifically amplify the 5′-UTR, VP1 sequence, and full-length genome of OPV from stool
| Genomic regions | OPV strain | Primer | Sequence (5′→3′) | Tm (°C) |
|---|---|---|---|---|
| 5′-UTR | Sabin 1 | S1F3 | TGCGTGGTTGAAAGCGACG | 53 |
| S1R3 | ATAACTGTTGAAATTGTACTT | 43 | ||
| Sabin 2 | S2F3 | GAAAAGCCTAGTATCGCCTT | 50 | |
| S2R4 | TGAGAAGTAAAGCTAACAC | 45 | ||
| Sabin 3 | S3-F | CATGTACTTCGAGAAGCCTAGTATCGCTC | 62 | |
| S3-R | AACAAACAAGGGAGTAATTAATCTGATTCA | 55 | ||
| VP1 | Sabin 1 | VP1-s1f | GAGATACCACACATATAGAG | 48 |
| VP1-s1rT7P | ACGCGTTAATACGACTCACTATAGGCAAATCTTCCTGAGTGGCCAA | 69 | ||
| Complete genome | Sabin 1 and 3 | A7-Sabin 1,3 | ACGCGTTAATACGACTCACTATAGGCCTCCGAATTAAAGAAAAATT | 65 |
| Sabin 2 | A7-Sabin2 | ACGCGTTAATACGACTCACTATAGGCCCCGAATTAAAGAAAAATTT | 65 | |
| Universal | U-S7 | ACCGGACGATTTAGGTGACACTATAGTTAAAACAGCTCTGGGGTTG | 69 | |
| Universal | U-A3 | ATGACCCAATCCAATTCGACTG | 53 | |
| Universal | U-S5 | CCCACCCCAGAGGCCCAC | 59 |
FL-PCR.
Ten microliters of cDNA was used for full-length PCR amplification of the poliovirus genome. The reaction was performed according to the manufacturer's manual for the XL-PCR kit (Perkin-Elmer/ABI, Alameda, CA) and as described before (10). Sense primer U-S7 and antisense primers A7-Sabin2 and A7-Sabin1,3 were used (Table 1).
The FL-PCR procedure was performed using a GeneAmp 9700 thermocycler (ABI, Foster City, CA) with the following conditions: incubation for 30 s at 94°C followed by 35 cycles, each consisting of 15 s at 94°C and 10 min at 65°C, and then incubation for 30 min at 72°C.
Nested FL-PCR.
Sense primer U-A3 and antisense primer U-A5 for nested FL-PCR were located within the first amplicon at the regions conserved among all poliovirus serotypes (Table 1). The nested FL-PCR procedure included amplification of 10 μl of the first FL-PCR product in a final volume of 100 μl under the same conditions as described above for FL-PCR except with a slight change in the temperature regimen: incubation for 30 s at 94°C followed by 35 cycles, each consisting of 15 s at 94°C, 15 s at 55°C, and 10 min at 65°C, and then incubation for 30 min at 72°C.
Design and fabrication of microchips.
For quantification of reversions in the 5′-UTR, we designed specific primers to amplify this region separately for each attenuated poliovirus strain (Table 1). Oligonucleotide probes for microarray hybridization were synthesized based on the analysis of previously published genomic sequences of Sabin and wild-type poliovirus strains. Sequences were aligned using the Clustal X program (43), and specific oligonucleotide probes for individual detection of mutations of interest were selected by using the custom OligoScan program developed in our lab (Table 2). The melting temperatures (Tms) of oligonucleotides were chosen to be between 44 to 51°C (calculated by using the nearest-neighbor algorithm) so that the mutation of interest was located close to the center of each oligonucleotide. Oligonucleotides with the 5′ end modified by addition of an aminolink group were synthesized with an automated oligonucleotide synthesizer and purified as described previously (8, 28). Microchips were printed on silylated (aldehyde-coated) glass slides (Cell Associate, Inc., TX) using contact a microspotting robot (Cartesian Technologies, Inc., CA) equipped with a CMP-7 microspotting pin (ArrayIt, CA) as described previously (28). Ten individual microarrays for 5′-UTR analysis were spotted on each slide. The unit microarray contained 10 spots of oligonucleotide probe for specific Sabin strain and 10 spots of oligonucleotide probe specific for revertant virus. Microarrays also contained two oligonucleotides specific to a conserved region (control); each of the controls spotted five times in the last row (see Fig. 2). The redundant spotting was used to increase quantification accuracy.
TABLE 2.
Oligonucleotide probes for detection and differentiation of revertant mutations in the 5′-UTR of OPV extracted from stool specimens
| OPV strain | Mutation position | Probe | Oligonucleotide probe sequences | Tm (°C) |
|---|---|---|---|---|
| Sabin 1 | 480 | 480-A oligo | ACCTCGGAGCAGGTG (Revetant) | 46 |
| 480-G oligo | ACCTCGGGGCAGGTG | 49 | ||
| 525 | 525-C oligo | CGCAAGCCCGTGGC (Revertant) | 51 | |
| 525-T oligo | CGCAAGTCCGTGGC | 47 | ||
| Sabin 2 | 481 | 481-G oligo | ACCACGGAGCAGGCG (Revertant) | 50 |
| 481-A oligo | ACCACGGAACAGGCG | 48 | ||
| Sabin 3 | 472 | 472-C oligo | GGCTAATCCTAACCATGG (Revertant) | 46 |
| 472-T oligo | GGCTAATTCTAACCATGG | 44 | ||
| Sabin 1 | Positive control | S1F | TACTTCGAGAAGCCCAGTACCACCTC | 61 |
| Sabin 2 | Positive control | S2F | TGTGTACTTCGAAAAGCCTAGTATCGCCTT | 60 |
| Sabin 3 | Positive control | S3F | CATGTACTTCGAGAAGCCTAGTATCGCTC | 62 |
| Universal | UF | GGTGTGAAGAGCCTATTGAGCTACAT | 58 |
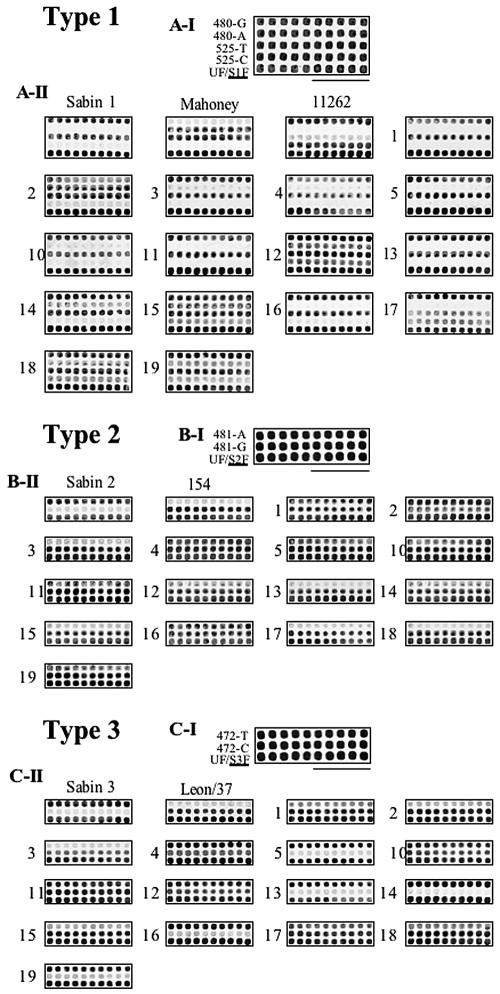
FIG. 2.
Hybridization of samples amplified from stool samples of vaccine recipients with microarrays containing oligonucleotide probes discriminating mutations in the 5′-UTRs of attenuated polioviruses. A: Detection of 480 G→A and 525 T→C mutations in the 5′-UTRs of Sabin 1 poliovirus and its revertants. The upper part of the panel shows the layout of oligonucleotide probes. Ten spots each of four allele-specific oligonucleotide probes were spotted into the top four rows; the bottom row contains five spots each of universal oligonucleotide probe UF and Sabin 1-specific oligonucleotide probe S1F. The lower part shows patterns of hybridization of, respectively, Sabin1, Mahoney, revertant strain 11262, and stool samples 1 to 5 and 10 to 19. B: Detection of the 481 A→G mutation in the 5′-UTRs of Sabin 2 poliovirus and its revertants. The upper part of the panel shows the layout of oligonucleotide probes. Ten spots each of two allele-specific oligonucleotide probes were spotted into the top two rows; the bottom row contains five spots each of universal oligonucleotide probe UF and Sabin 2-specific oligonucleotide probe S2F. The lower part shows patterns of hybridization of, respectively, Sabin2, revertant strain 154, and stool samples 1 to 5 and 10 to 19. C: Detection of the 472 T→Cmutation in the 5′-UTRs of Sabin 3 poliovirus and its revertants. The upper part of the panel shows the layout of oligonucleotide probes. Ten spots each of two allele-specific oligonucleotide probes were spotted into the top two rows; the bottom row contains five spots each of universal oligonucleotide probe UF and Sabin 3-specific oligonucleotide probe S3F. The lower part shows patterns of hybridization of, respectively, Sabin 3, Leon/37, and stool samples 1 to 5 and 10 to 19.
To analyze the variability in the VP1 genes of attenuated polioviruses PCR amplified directly from stool specimens, we used the microarray for resequencing and heterogeneity analysis (MARSH), previously developed in our lab (7). Briefly, three sets of overlapping oligonucleotides corresponding to genomic sequences of three OPV strains and covering the VP1-coding region were synthesized. Four MARSH arrays were spotted on each slide, and each set of oligonucleotide probes was printed with a fourfold redundancy, so that each microarray contained four identical subarrays. On each slide, two out of four microarrays were hybridized with reference DNA, and two remaining arrays were hybridized with sample DNAs. This allowed the hybridization signals obtained for test samples to be normalized by the fluorescence intensity produced by the respective oligonucleotides hybridized with the homogeneous reference (7).
For analysis of viral recombination, we used the microarray analysis of virus recombination (MAVR) assay, which was developed previously (7). Briefly, genotype-specific oligonucleotide probes for identification of Sabin strains were selected and printed in three rows according to their location in the genome. Five individual microarrays for MAVR analysis were spotted on each slide.
Preparation of samples for hybridization.
For the analysis of the 5′-UTR, we designed primers in variable regions at the ends of this segment in order to specifically amplify a single poliovirus genotype from the mixture (Table 1). The specific amplification of 5′-UTR for each OPV strain was performed by PCR, and the synthesis of single-stranded DNA was performed by asymmetric PCR using a Perkin-Elmer PCR kit as described previously (28). The single-stranded DNA was purified with the QIAquick PCR purification kit (QIAGEN, Chatsworth, CA) and diluted in 50 μl of water.
Aliquots containing 0.2 μM of single-stranded DNA were labeled using the Cy5 or Cy3 Micromax ASAP RNA labeling kit (Perkin-Elmer, Boston, MA) and purified using CENTRI-SEP (Princeton Separation, Adelphia, NJ) spin columns.
The VP1-coding region was PCR amplified with specific Sabin 1 specific primers. Reverse primers contained a T7 RNA polymerase promoter (Table 1), and preparation of sample for hybridization with microarrays for mutations screening in VP1 or for analysis of viral recombinants was done as described previously (7).
Microarray hybridization, scanning, and data analysis.
Fluorescently labeled samples were dried immediately prior to hybridization, reconstituted in ASAP hybridization buffer III, (for hybridization to the 5′-UTR microarray, 0.5 μM Cy5-quality control of oligonucleotide was also added), and denatured by incubating for 1 min at 95°C. The final concentration of each probe in the hybridization solution did not exceed 0.2 μM. Five-microliter aliquots were applied to the MARSH and MAVR microarrays, and 2 μl was applied to the 5′-UTR microarray; each aliquot was covered with an individual plastic coverslip. Hybridization was performed for at least 30 min at 45°C. The microarray was then washed as described previously (28).
Microarray images were taken using a ScanArray 5000 confocal fluorescent scanner (GSI Lumonics, MA) equipped with green and red HeNe lasers (543 nm and 632 nm for excitation of Cy3 and Cy5, respectively). Images were then analyzed using QuantArray software (Packard BioScience, MA). The MARSH assay results were analyzed as described before (7). The values obtained from 5′-UTR microchips were normalized and analyzed as described before (28).
RESULTS
PCR amplification of a full-length genome of poliovirus from stool specimens.
Amplification of full-length cDNA of poliovirus starting from purified poliovirus RNA was previously described (10), opening an intriguing possibility of using this approach for analysis of clinical specimens. There are numerous reports that inhibitory substances that interfere with PCR can be present in stool specimens (12, 23, 44, 45). To eliminate these inhibitors, we used the QIAamp viral RNA minikit for isolation of viral RNA and further modified the highly efficient protocol (4, 25). To increase the sensitivity of the amplification, we increased the quantity of source RNA to 1 to 1.5 μg, extended the time of the reverse transcription reaction to 3 to 5 h, and added Superscript II reverse transcriptase twice in the course of reaction: first at 12 U/μl at the beginning, and then at 4 U/μl after 2 hours.
Next, we altered FL-PCR protocol by increasing the length of the polymerase extension step and by increasing the number of amplification cycles. The PCR primers used for this protocol are listed in Table 1. Increasing the concentration of rTth DNA polymerase from 1 unit to 1.5 units significantly increased the yields of specific amplification product. To determine the sensitivity of the protocol, we spiked decreasing amounts of virus suspension containing 107 TCID50 into a control stool sample and performed the complete cycle of isolation and amplification. Using our modified protocol, we were able to detect 470 TCID50 in one milliliter of stool.
To further increase the sensitivity of detection, we used nested FL-PCR in which XL-PCR with different primers that were located in highly conserved regions flanked by the primers was used to generate first amplicons. The nested FL-PCR allowed us to detect about 47 TCID50 of poliovirus in 1 ml of stool.
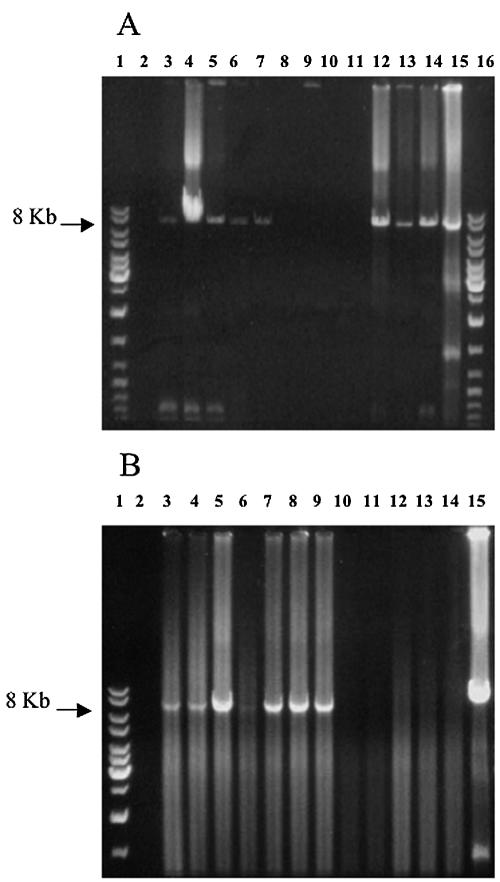
FL-PCR amplification from stool specimens collected from healthy vaccine recipients.
To test the ability of FL-PCR to amplify poliovirus cDNA from stool specimens, we used samples collected from healthy children 1 week after immunization with OPV. The stool was diluted to 10% in Dulbecco's phosphate-buffered saline, the RNA was extracted with the QIAamp viral RNA minikit and reverse transcribed, and the cDNA was amplified by FL-PCR as described above. The results of this amplification are shown in Fig. 1A and B. Fifteen out of the total of 24 samples were positive in the FL-PCR amplification, which demonstrated that the product was full-length cDNA of poliovirus. All samples collected 1 week after the first dose of OPV and most samples collected 1 week after an OPV dose given after two IPV doses were positive, while only two out of three samples collected 1 week after three OPV doses appeared to contain poliovirus. No PCR amplification was observed in stool samples collected from children immunized with IPV only or in stool samples collected 3 weeks after an OPV dose given after two doses of IPV. This result is in complete agreement with the expectation that prior immunization reduces the amount of excreted virus. The virus titration (Table 3) demonstrated that the limit of detection was 158 TCID50/ml.
FIG. 1.
Amplification of full-length genome of attenuated poliovirus directly from stool samples. Panel A: lanes 1 and 16, DNA ladder mix; lane 2, negative reverse transcription-PCR control; lanes 3 to 14, stool samples 1 to 12, respectively; lane 15, Sabin 1 positive control. Panel B: lane 1, DNA ladder mix; lane 2, negative control; lanes 3 to 14, stool samples 13 to 24, respectively; lane 15, Sabin 1 positive control.
TABLE 3.
Titers of virus in stool samples and results of FL-PCR amplification
| Sample | Log10 TCID50 | FL-PCR |
|---|---|---|
| 1 | 10,000 | + |
| 2 | 794,328 | + |
| 3 | 39,811 | + |
| 4 | 3,162 | + |
| 5 | 316 | + |
| 6 | <158 | − |
| 7 | <158 | − |
| 8 | <158 | − |
| 9 | <158 | − |
| 10 | 398,107 | + |
| 11 | 39,811 | + |
| 12 | 199,526 | + |
| 59 | 5,012 | + |
| 60 | 50,119 | + |
| 61 | 39,811 | + |
| 62 | 7,943 | + |
| 63 | 31,623 | + |
| 64 | 3,162 | + |
| 65 | 316,228 | + |
| 66 | <158 | − |
| 67 | <158 | − |
| 68 | <158 | − |
| 69 | <158 | − |
| 70 | <158 | − |
Quantification of mutations in the 5′-UTR by oligonucleotide microarray hybridization.
The ability to prepare viral cDNA directly from stool samples opens the possibility of rapid genetic characterization of virus in in vivo samples. To determine whether viral genomes recovered from the stool specimens contained mutations in the 5′-UTR, we developed oligonucleotide microarrays and hybridized them with the DNA amplified with primers specific to each of the three genotypes of poliovirus (Table 1). To detect and quantify each mutation of interest, two oligonucleotides were synthesized and spotted on the microchip. One oligonucleotide probe was specific to the vaccine sequence, and the other was specific to the revertant. These oligonucleotide probes were 15 to 18 nucleotides long, ensuring that their binding was critically affected by a single-nucleotide mismatch (Table 2). The following mutations were tested: 480 G→A and 525 T→C in Sabin 1, 481 A→G in Sabin 2, and 472 U→C in Sabin 3-derived viruses.
Fluorescent single-stranded DNA samples were generated from test and control samples and hybridized with the chip as described above. The percentage of reversion was calculated by dividing the normalized signal from each revertant oligonucleotide probe by the total signal (signal obtained from both revertant and vaccine oligonucleotide probes). The numbers obtained from 10 replicates of each oligonucleotide probe (vaccine and revertant) were averaged, and the standard deviation was calculated (Table 4). These data show that many stool samples taken from healthy children 1 week after OPV immunization contained reversions, consistent with classical observations (5, 16, 17). The hybridization patterns for each OPV strain are shown in Fig. 2A-II, B-II, and C-II. These results demonstrate that the oligonucleotide microarrays simultaneously and unambiguously detected and discriminated vaccine and revertant sequences and allowed us to perform quantification of reversions in the 5′-UTRs of all three genotypes of poliovirus.
TABLE 4.
Percentage of revertants in the 5′-UTR of poliovirus determined directly in stool specimens
| Stool sample | % (mean ± SD)
|
|||
|---|---|---|---|---|
| Sabin 1
|
Sabin 2, 481-G | Sabin 3, 472-C | ||
| 480-A | 525-C | |||
| 1 | 2 ± 0.03 | 0 | 68 ± 0.20 | 74 ± 0.05 |
| 2 | 53 ± 0.22 | 3 ± 0.03 | 33 ± 0.30 | 93 ± 0.04 |
| 3 | 2 ± 0.02 | 0 | 97 ± 0.04 | 93 ± 0.03 |
| 4 | 2 ± 0.02 | 0 | 55 ± 0.20 | 26 ± 0.05 |
| 5 | 0 | 0 | 66 ± 0.10 | 6 ± 0.03 |
| 10 | 0 | 0 | 64 ± 0.10 | 36 ± 0.07 |
| 11 | 2 ± 0.02 | 0 | 63 ± 0.20 | 63 ± 0.05 |
| 12 | 21 ± 0.09 | 24 ± 0.03 | 74 ± 0.15 | 47 ± 0.05 |
| 13 | 0 | 0 | 97 ± 0.10 | 30 ± 0.23 |
| 14 | 20 ± 0.11 | 0 | 77 ± 0.07 | 22 ± 0.20 |
| 15 | 18 ± 0.14 | 26 ± 0.05 | 92 ± 0.05 | 95 ± 0.05 |
| 16 | 0 | 0 | 46 ± 0.09 | 36 ± 0.32 |
| 17 | 3 ± 0.04 | 68 ± 0.05 | 87 ± 0.20 | 65 ± 0.10 |
| 18 | 12 ± 0.05 | 26 ± 0.05 | 96 ± 0.17 | 88 ± 0.08 |
| 19 | 24 ± 0.20 | 15 ± 0.03 | 85 ± 0.11 | 29 ± 0.21 |
Screening for mutations in the VP1-coding region by using the MARSH oligonucleotide microarray.
Viral replication in vitro or in vivo results in accumulation of mutations and leads to increased heterogeneity of viral populations. To detect these mutations in stool specimens, we used MARSH assay as previously described (6). This microarray contains specific oligonucleotides overlapping at half length and covering the region coding for VP1, the poliovirus capsid protein exhibiting the greatest variability. This method has been shown to be sufficiently sensitive to detect small differences in mutational profiles of poliovirus (6).
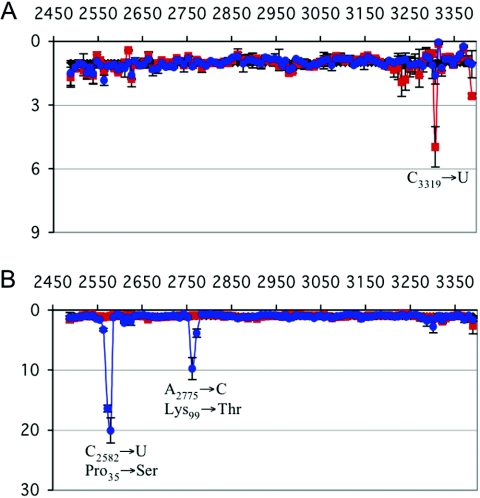
The hybridization of PCR-amplified DNAs derived from stool samples on this chip and the comparison of their fluorescent signals with that of the prototype Sabin 1 showed that there were two mutations in stool sample 2, one in an oligonucleotide centered around genomic position 2579 and the second in an oligonucleotide located at position 2762 (Fig. 3B). Sequencing of the VP1-coding region confirmed the presence of mutations C2582→U, coding for a Pro35→Ser change, and A2775→C, coding for Lys99→Thr. The latter amino acid substitution affects antigenic site 1 (amino acids 91 to 102 of VP1) (18, 34).
FIG. 3.
Mutational profiles of the VP1-coding region of Sabin 1 virus extracted from stool specimens. A: The ratios of signals obtained from DNA microarray hybridization with reference sample (Sabin 1) and stool samples 18 (red) and 19 (blue). B: The ratios of signals obtained from DNA microarray hybridization with reference sample (Sabin 1) and stool samples 1 (red) and 2 (blue). The peaks indicate the locations of mutations that disrupt binding of respective oligonucleotide probes.
Analysis of stool sample 18 showed the presence of a peak located in oligonucleotide 3308 (Fig. 3A). Sequencing of this region showed the presence of a silent mutation, C3319→U. MARSH analysis of other stool samples did not identify additional mutations in the VP1 region. This was confirmed by the results of nucleotide sequencing. These results demonstrate that MARSH analysis can reveal mutations regions in viral genomes amplified directly from stool samples.
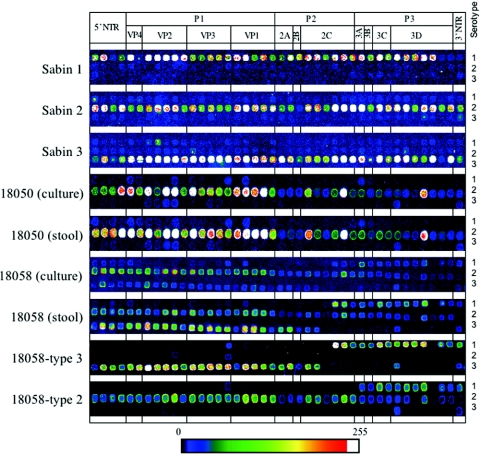
Analysis of poliovirus genome structure in cDNAs prepared from stool samples taken from AFP cases.
Genetic characterization of poliovirus strains isolated from cases of AFP is an essential part of laboratory diagnosis. The ability to perform this analysis directly on the samples prepared from stool specimens could allow us to reduce the time needed for obtaining results from several weeks to few days. Therefore, we analyzed FL-PCR amplicons obtained from stool samples taken from AFP cases by MAVR, a method recently created in our laboratory (6). Figure 4 shows the result of analysis of samples (18050 and 18058) prepared from stool specimens and respective isolates obtained by a conventional scheme (50). Sample 18058 contained a mixture of Sabin 2 and Sabin 3 viruses, one or both of them being recombinants with Sabin 1 virus. Growing this virus in cell culture in the presence of antisera against these serotypes allowed us to separate viral genomes with type 2 capsid sequences from those with type 3 sequences; their hybridization pattern in MAVR analysis shows that Sabin 3 is a recombinant with Sabin 1 (Fig. 4, 18058-type 3), and there are at least two type 2 polioviruses present in this sample, one nonrecombinant and another recombinant with Sabin 1 (Fig. 4, 18058-type 2). Therefore, microarray analysis of cDNAs amplified directly from stool samples by using the MAVR protocol allowed us to perform rapid overall characterization of strains present in the in vivo specimens and to significantly decrease the analysis time.
FIG. 4.
Genome structure analysis of poliovirus in stool samples from AFP, cases using DNA oligonucleotide microarray hybridization. Three rows of oligonucleotide probes in each microarray are specific to three serotypes of poliovirus and are spotted according to their location in the genome. Sample names are shown on the left.
DISCUSSION
The worldwide poliomyelitis eradication campaign resulted in stopping of wild-type poliovirus circulation in much of the world, with the exceptions of south-central Asia and some regions in Africa. Because the ultimate goal of eradication seems to be within reach, development of a rational “endgame” strategy and vaccination policies for the posteradication period has become a high priority (14). The original assumption was that after cessation of circulation and containment of wild-type polioviruses, worldwide immunization against poliomyelitis would eventually be stopped (46, 47), similar to the strategy employed in the smallpox eradication campaign (20-22). However, recent discoveries of long-term circulation of VDPV that may cause outbreaks of paralytic disease in communities with inadequate immunity (25, 48, 49, 51) raise questions about the prudence of this approach (7, 22, 27, 37). Long-term persistence of poliovirus and its excretion by immunocompromised individuals (26, 32) suggest that some form of protection from the threat of reemergence of poliomyelitis may be needed even after the transmission of wild-type poliovirus has been eliminated. Some countries have already announced their intention to continue to use IPV at least until the situation with VDPV has been studied in more detail. To develop a rational posteradication immunization strategy, extensive surveillance coupled with detailed genomic characterization to identify the level of divergence of circulating VDPV strains must be urgently performed. The rigorous global monitoring of poliovirus circulation should also continue after the eradication is complete and until we determine that the environment is clear of all polioviruses and that the risk of their reemergence is negligible.
Currently, laboratory diagnosis of AFP cases and environmental monitoring are carried out by conventional procedures based on poliovirus isolation in several types of cell cultures followed by intratypic differentiation or serotyping (52). This traditional approach requires several weeks and also carries a risk of missing some of the components that may be present in highly heterogeneous and dynamic natural populations of these viruses.
In this communication we describe a rapid method for amplification of complete copies of poliovirus cDNA directly from stool samples. The FL-PCR amplification method was originally proposed in our laboratory (10) and was recently used for discrimination between wild-type and attenuated polioviruses (3). In this study we adapted the protocol to prepare cDNA directly from stool samples, eliminating the need to grow virus in vitro. The materials obtained directly from the clinical samples were used for genetic analysis using microarray hybridization. Together, these two approaches produce a snapshot of genomic analysis of the entire viral population without resorting to more laborious techniques. This simple analysis can be completed within few days for a large number of viral isolates simultaneously. The method does not require cloning of the test samples, thus preserving the natural compositions of viral populations. Unlike PCR techniques relying on amplification of short segments of viral genome that were previously used for characterization of viruses in clinical samples (36), full-length PCR amplification allows investigators to reasonably suggest that its results reflect the presence of live virus rather than fragments. Therefore, the results of this method may be more clinically relevant. Use of the proposed shortcut opens the possibility of a large-scale full-genome screening of viral isolates from clinical samples, which is needed for thorough epidemiological surveillance, vaccine quality control, and analysis of genetic changes in response to drug treatment.
We used the microarray methods that have been described here for quantification of the known reversions in the 5′-UTR of live poliovirus vaccine at the level of point mutation, based on the ability of oligonucleotide microarrays to distinguish single-nucleotide polymorphism (6, 8, 28). We also used other microarray methods recently created in our lab (6). We analyzed both stool samples obtained from healthy vaccinees and samples taken from cases of adverse reactions (AFP) linked to OPV immunization. The proposed protocol is rapid, highly sensitive, and robust. It allowed us to perform characterization of complex mixtures of viral recombinants within few working days, as opposed to several weeks for the conventional protocol. We also demonstrate that it can be used for characterization of the overall genomic structure, identification of random mutations, and quantification of particular mutations causing increased neurovirulence.
The use of an improved viral RNA isolation procedure and the larger total quantity of RNA used for reverse transcription (1 to 1.5 μg) allowed us to consistently amplify full-length viral cDNA from stool samples. The sensitivity of the optimized assay for detection of attenuated poliovirus in stool specimens determined in spiking experiments using FL-PCR is roughly equal to what could be determined by direct virus titration of stool samples (the limit of detection in our protocol was 158 TCID50 per ml), and a sample with a titer of 316 TCID50/ml was positive. The direct FL-PCR amplification protocol can yield results in 1 to 2 days, while traditional cell culture-based assay requires at least 2 to 3 weeks. Another advantage of FL-PCR is that it can be performed in laboratories without tissue culture capabilities and at a lower expense. The ability to perform large-scale screening of environmental and clinical samples without resorting to traditional cell culture methods might have additional value after polio eradication is achieved. According to the current World Health Organization guidelines (53), all work with live poliovirus in the posteradication period must be performed in laboratories having a biosafety 3 level of containment. Screening of clinical and environmental samples for possible reemergence of poliovirus would therefore be subject to similar levels of containment. Direct screening of RNAs isolated from stool samples and from the environment by using the molecular method proposed in this communication will help solve this critical dilemma.
Many samples obtained from healthy vaccine recipients 1 week after immunization contained reversions in the 5′-UTR, consistent with previously published data (5, 17). Some samples also contained reversions inside the VP1 capsid protein-coding region, including the locus coding for a major antigenic site, consistent with the pattern observed for other VDPVs that gradually regain their ability to circulate in human communities (2, 7). These results as well as the data from hundreds of other stool specimens from vaccine recipients analyzed by the technique described here will be discussed in detail elsewhere.
Terminal regions of genomes of most RNA viruses are highly conserved, which opens the possibility of using the same approach for direct analysis of other viruses. Screening of clinical and environmental samples by using the FL-PCR amplification protocol coupled with microarray analysis of the resulting amplicons can be used for surveillance of emerging pathogens, including those viruses that are difficult to grow in cell culture. It can also be used for creation of archival DNA samples prepared from clinical and environmental specimens. Such samples can be easily stored and then used for retrospective analysis and screening for the presence of particular pathogens.
Finally, incorporation of RNA polymerase promoters suitable for in vitro transcription into the PCR primers allowed us to obtain infectious RNA transcripts from the FL amplicons and to recover live virus from these archived samples (not shown). Therefore, use of FL-PCR as the first step in characterization of viruses directly in clinical samples, without cultivating them in cell culture, could become a new paradigm in virus isolation and epidemiological surveillance for emerging and reemerging viruses.
Acknowledgments
We thank Vladimir Chizhikov for help and advice on using microarray hybridization, Roland Lundquist and Elena Cherkasova for suggestions and critical review of the manuscript, and Stanley Plotkin for discussions and encouragement.
This work was supported in part by a grant to K.C. from the Defense Advanced Research Projects Agency (DARPA) and by NIAID contracts NO1-AI-45250 and NO1-AI-45251 to R.B.
REFERENCES
- 1.Abraham, R., P. Minor, G. Dunn, J. F. Modlin, and P. L. Ogra. 1993. Shedding of virulent poliovirus revertants during immunization with oral poliovirus vaccine after prior immunization with inactivated polio vaccine. J. Infect. Dis. 168:1105-1109. [DOI] [PubMed] [Google Scholar]
- 2.Blomqvist, S., C. Savolainen, P. Laine, P. Hirttio, E. Lamminsalo, E. Penttila, S. Joks, M. Roivainen, and T. Hovi. 2004. Characterization of a highly evolved vaccine-derived poliovirus type 3 isolated from sewage in Estonia. J. Virol. 78:4876-4883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boot, H. J., R. M. Schepp, F. J. van Nunen, and T. G. Kimman. 2004. Rapid RT-PCR amplification of full-length poliovirus genomes allows rapid discrimination between wild-type and recombinant vaccine-derived polioviruses. J. Virol. Methods 116:35-43. [DOI] [PubMed] [Google Scholar]
- 4.Burgener, M., U. Candrian, and M. Gilgen. 2003. Comparative evaluation of four large-volume RNA extraction kits in the isolation of viral RNA from water samples. J. Virol. Methods 108:165-170. [DOI] [PubMed] [Google Scholar]
- 5.Cann, A. J., G. Stanway, P. J. Hughes, P. D. Minor, D. M. Evans, G. C. Schild, and J. W. Almond. 1984. Reversion to neurovirulence of the live-attenuated Sabin type 3 oral poliovirus vaccine. Nucleic Acids Res. 12:7787-7792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cherkasova, E., M. Laassri, V. Chizhikov, E. Korotkova, E. Dragunsky, V. I. Agol, and K. Chumakov. 2003. Microarray analysis of evolution of RNA viruses: evidence of circulation of virulent highly divergent vaccine-derived polioviruses. Proc. Natl. Acad. Sci. USA 100:9398-9403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cherkasova, E. A., E. A. Korotkova, M. L. Yakovenko, O. E. Ivanova, T. P. Eremeeva, K. M. Chumakov, and V. I. Agol. 2002. Long-term circulation of vaccine-derived poliovirus that causes paralytic disease. J. Virol. 76:6791-6799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chizhikov, V., M. Wagner, A. Ivshina, Y. Hoshino, A. Z. Kapikian, and K. Chumakov. 2002. Detection and genotyping of human group A rotaviruses by oligonucleotide microarray hybridization. J. Clin. Microbiol. 40:2398-2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christodoulou, C., F. Colbere-Garapin, A. Macadam, L. F. Taffs, S. Marsden, P. Minor, and F. Horaud. 1990. Mapping of mutations associated with neurovirulence in monkeys infected with Sabin 1 poliovirus revertants selected at high temperature. J. Virol. 64:4922-4929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chumakov, K. M. 1996. PCR engineering of viral quasispecies: a new method to preserve and manipulate genetic diversity of RNA virus populations. J. Virol. 70:7331-7334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Contreras, G., K. Dimock, J. Furesz, C. Gardell, D. Hazlett, K. Karpinski, G. McCorkle, and L. Wu. 1992. Genetic characterization of Sabin types 1 and 3 poliovaccine virus following serial passage in the human intestinal tract. Biologicals 20:15-26. [DOI] [PubMed] [Google Scholar]
- 12.De Leon, R., S. M. Matsui, R. S. Baric, J. E. Herrmann, N. R. Blacklow, H. B. Greenberg, and M. D. Sobsey. 1992. Detection of Norwalk virus in stool specimens by reverse transcriptase-polymerase chain reaction and nonradioactive oligoprobes. J. Clin. Microbiol. 30:3151-3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Domingo, E., E. Martinez-Salas, F. Sobrino, J. C. de la Torre, A. Portela, J. Ortin, C. Lopez-Galindez, P. Perez-Brena, N. Villanueva, R. Najera, et al. 1985. The quasispecies (extremely heterogeneous) nature of viral RNA genome populations: biological relevance. Gene 40:1-8. [DOI] [PubMed] [Google Scholar]
- 14.Dowdle, W. R., E. De Gourville, O. M. Kew, M. A. Pallansch, and D. J. Wood. 2003. Polio eradication: the OPV paradox. Rev. Med. Virol. 13:277-291. [DOI] [PubMed] [Google Scholar]
- 15.Duarte, E. A., I. S. Novella, S. C. Weaver, E. Domingo, S. Wain-Hobson, D. K. Clarke, A. Moya, S. F. Elena, J. C. de la Torre, and J. J. Holland. 1994. RNA virus quasispecies: significance for viral disease and epidemiology. Infect. Agents Dis. 3:201-214. [PubMed] [Google Scholar]
- 16.Dunn, G., N. T. Begg, N. Cammack, and P. D. Minor. 1990. Virus excretion and mutation by infants following primary vaccination with live oral poliovaccine from two sources. J. Med. Virol. 32:92-95. [DOI] [PubMed] [Google Scholar]
- 17.Evans, D. M., G. Dunn, P. D. Minor, G. C. Schild, A. J. Cann, G. Stanway, J. W. Almond, K. Currey, and J. V. Maizel, Jr. 1985. Increased neurovirulence associated with a single nucleotide change in a noncoding region of the Sabin type 3 poliovaccine genome. Nature 314:548-550. [DOI] [PubMed] [Google Scholar]
- 18.Evans, D. M., P. D. Minor, G. S. Schild, J. W. Almond, G. C. Schild, J. Bootman, M. Ferguson, P. Reeve, M. Spitz, G. Stanway, A. J. Cann, R. Hauptmann, L. D. Clarke, and R. C. Mountford. 1983. Critical role of an eight-amino acid sequence of VP1 in neutralization of poliovirus type 3. Location and primary structure of a major antigenic site for poliovirus neutralization. Nature 304:459-462. [DOI] [PubMed] [Google Scholar]
- 19.Friedrich, F. 1996. Genomic modifications in Sabin vaccine strains isolated from vaccination-associated cases, healthy contacts and healthy vaccinees. Acta Virol. 40:157-170. [PubMed] [Google Scholar]
- 20.Fulginiti, V. A., A. Papier, J. M. Lane, J. M. Neff, and D. A. Henderson. 2003. Smallpox vaccination. I. Background, vaccination technique, normal vaccination and revaccination, and expected normal reactions. Clin. Infect. Dis. 37:241-250. [DOI] [PubMed] [Google Scholar]
- 21.Fulginiti, V. A., A. Papier, J. M. Lane, J. M. Neff, and D. A. Henderson. 2003. Smallpox vaccination. II. Adverse events. Clin. Infect. Dis. 37:251-271. [DOI] [PubMed] [Google Scholar]
- 22.Henderson, D. A. 2002. Countering the posteradication threat of smallpox and polio. Clin. Infect. Dis. 34:79-83. [DOI] [PubMed] [Google Scholar]
- 23.Jiang, X., J. Wang, D. Y. Graham, and M. K. Estes. 1992. Detection of Norwalk virus in stool by polymerase chain reaction. J. Clin. Microbiol. 30:2529-2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kawamura, N., M. Kohara, S. Abe, T. Komatsu, K. Tago, M. Arita, and A. Nomoto. 1989. Determinants in the 5′ noncoding region of poliovirus Sabin 1 RNA that influence the attenuation phenotype. J. Virol. 63:1302-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kew, O., V. Morris-Glasgow, M. Landaverde, C. Burns, J. Shaw, Z. Garib, J. Andre, E. Blackman, C. J. Freeman, J. Jorba, R. Sutter, G. Tambini, L. Venczel, C. Pedreira, F. Laender, H. Shimizu, T. Yoneyama, T. Miyamura, H. van Der Avoort, M. S. Oberste, D. Kilpatrick, S. Cochi, M. Pallansch, and C. deq Uadros. 2002. Outbreak of poliomyelitis in Hispaniola associated with circulating type 1 vaccine-derived poliovirus. Science 296:356-359. [DOI] [PubMed] [Google Scholar]
- 26.Khetsuriani, N., D. R. Prevots, L. Quick, M. E. Elder, M. Pallansch, O. Kew, and R. W. Sutter. 2003. Persistence of vaccine-derived polioviruses among immunodeficient persons with vaccine-associated paralytic poliomyelitis. J. Infect. Dis. 188:1845-1852. [DOI] [PubMed] [Google Scholar]
- 27.Korotkova, E. A., R. Park, E. A. Cherkasova, G. Y. Lipskaya, K. M. Chumakov, E. V. Feldman, O. M. Kew, and V. I. Agol. 2003. Retrospective analysis of a local cessation of vaccination against poliomyelitis: a possible scenario for the future. J. Virol. 77:12460-12465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Laassri, M., V. Chizhikov, M. Mikheev, S. Shchelkunov, and K. Chumakov. 2003. Detection and discrimination of orthopoxviruses using microarrays of immobilized oligonucleotides. J. Virol. Methods 112:67-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Landaverde, M., L. Venczel, and C. A. deq Uadros. 2001. Poliomyelitis outbreak caused by vaccine-derived virus in Haiti and the Dominican Republic. Rev. Panam. Salud Publ. 9:272-274. [DOI] [PubMed] [Google Scholar]
- 30.Macadam, A. J., S. R. Pollard, G. Ferguson, R. Skuce, D. Wood, J. W. Almond, and P. D. Minor. 1993. Genetic basis of attenuation of the Sabin type 2 vaccine strain of poliovirus in primates. Virology 192:18-26. [DOI] [PubMed] [Google Scholar]
- 31.Macadam, A. J., D. M. Stone, J. W. Almond, and P. D. Minor. 1994. The 5′ noncoding region and virulence of poliovirus vaccine strains. Trends Microbiol. 2:449-454. [DOI] [PubMed] [Google Scholar]
- 32.Martin, J., G. Dunn, R. Hull, V. Patel, and P. D. Minor. 2000. Evolution of the Sabin strain of type 3 poliovirus in an immunodeficient patient during the entire 637-day period of virus excretion. J. Virol. 74:3001-3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Melnick, J. L. 1996. Current status of poliovirus infections. Clin. Microbiol. Rev. 9:293-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Minor, P. D., G. C. Schild, J. Bootman, D. M. Evans, M. Ferguson, P. Reeve, M. Spitz, G. Stanway, A. J. Cann, R. Hauptmann, L. D. Clarke, R. C. Mountford, and J. W. Almond. 1983. Location and primary structure of a major antigenic site for poliovirus neutralization. Nature 301:674-679. [DOI] [PubMed] [Google Scholar]
- 35.Ogra, P. L., H. S. Faden, R. Abraham, L. C. Duffy, M. Sun, and P. D. Minor. 1991. Effect of prior immunity on the shedding of virulent revertant virus in feces after oral immunization with live attenuated poliovirus vaccines. J. Infect. Dis. 164:191-194. [DOI] [PubMed] [Google Scholar]
- 36.Old, M. O., C. V. Martinez, D. Kwock, J. Garcia, G. Martin, C. Chan, and Y. A. Maldonado. 2003. Direct extraction of Sabin poliovirus genomes from human fecal samples using a guanidine thiocyanate extraction method. J. Virol. Methods 110:193-200. [DOI] [PubMed] [Google Scholar]
- 37.Paul, Y., B. D. Schoub, J. Martin, G. Dunn, R. Hull, V. Patel, P. D. Minor, and S. C. Arya. 2001. Medical negligence and vaccine associated paralytic poliomyelitis. Indian Pediatr. 38:1068-1069. [PubMed] [Google Scholar]
- 38.Prevots, D. R., and P. M. Strebel. 1997. Poliomyelitis prevention in the United States: new recommendations for routine childhood vaccination place greater reliance on inactivated poliovirus vaccine. Pediatr. Ann. 26:378-383. [DOI] [PubMed] [Google Scholar]
- 39.Rennels, M. B., J. A. Englund, D. I. Bernstein, G. A. Losonsky, E. L. Anderson, M. E. Pichichero, F. M. Munoz, and M. C. Wolff. 2000. Diminution of the anti-polyribosylribitol phosphate response to a combined diphtheria-tetanus-acellular pertussis/Haemophilus influenzae type b vaccine by concurrent inactivated poliovirus vaccination. Pediatr. Infect. Dis. J. 19:417-423. [DOI] [PubMed] [Google Scholar]
- 40.Rousset, D., M. Rakoto-Andrianarivelo, R. Razafindratsimandresy, B. Randriamanalina, S. Guillot, J. Balanant, P. Mauclere, and F. Delpeyroux. 2003. Recombinant vaccine-derived poliovirus in Madagascar. Emerg. Infect. Dis. 9:885-887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Strebel, P. M., R. W. Sutter, S. L. Cochi, R. J. Biellik, E. W. Brink, O. M. Kew, M. A. Pallansch, W. A. Orenstein, and A. R. Hinman. 1992. Epidemiology of poliomyelitis in the United States one decade after the last reported case of indigenous wild virus-associated disease. Clin. Infect. Dis. 14:568-579. [DOI] [PubMed] [Google Scholar]
- 42.Tatem, J. M., C. Weeks-Levy, S. J. Mento, S. J. DiMichele, A. Georgiu, W. F. Waterfield, B. Sheip, C. Costalas, T. Davies, M. B. Ritchey, et al. 1991. Oral poliovirus vaccine in the United States: molecular characterization of Sabin type 3 after replication in the gut of vaccinees. J. Med. Virol 35:101-109. [DOI] [PubMed] [Google Scholar]
- 43.Thompson, J. D., D. G. Higgins, and T. J. Gibson. 1994. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 22:4673-4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Widjojoatmodjo, M. N., A. C. Fluit, R. Torensma, G. P. Verdonk, and J. Verhoef. 1992. The magnetic immuno polymerase chain reaction assay for direct detection of salmonellae in fecal samples. J. Clin. Microbiol. 30:3195-3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wilde, J., J. Eiden, and R. Yolken. 1990. Removal of inhibitory substances from human fecal specimens for detection of group A rotaviruses by reverse transcriptase and polymerase chain reactions. J. Clin. Microbiol. 28:1300-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wood, D. J. 2001. The scientific basis for stopping polio immunisation—issues and challenges. Dev. Biol. (Basel) 105:69-72. [PubMed] [Google Scholar]
- 47.Wood, D. J., R. W. Sutter, and W. R. Dowdle. 2000. Stopping poliovirus vaccination after eradication: issues and challenges. Bull. W. H. O. 78:347-357. [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization. 2001. Acute flaccid paralysis associated with circulating vaccine-derived poliovirus, Philippines, 2001. Wkly. Epidemiol. Rec 76:319-320. [PubMed] [Google Scholar]
- 49.World Health Organization. 2001. Circulation of a type 2 vaccine-derived poliovirus—Egypt, 1982-1993. Morb. Mortal. Wkly. Rep. 50:41-42, 51. [PubMed] [Google Scholar]
- 50.World Health Organization. 1997. Manual for the virologic investigation of poliomyelitis. W.H.O./EPI/GEN/97.1. World Health Organization, Geneva, Switzerland.
- 51.World Health Organization. 2002. Paralytic poliomyelitis in Madagascar, 2002. Wkly. Epidemiol. Rec. 77:241-242. [PubMed] [Google Scholar]
- 52.World Health Organization. 2001. Polio laboratory manual. World Health Organization, Geneva, Switzerland.
- 53.World Health Organization. 2002. W.H.O. global action plan for laboratory containment of wild polioviruses, 2nd ed. World Health Organization, Geneva, Switzerland.
- 54.Yang, C. F., T. Naguib, S. J. Yang, E. Nasr, J. Jorba, N. Ahmed, R. Campagnoli, H. van der Avoort, H. Shimizu, T. Yoneyama, T. Miyamura, M. Pallansch, and O. Kew. 2003. Circulation of endemic type 2 vaccine-derived poliovirus in Egypt from 1983 to 1993. J. Virol. 77:8366-8377. [DOI] [PMC free article] [PubMed] [Google Scholar]